Abstract
BACKGROUND
Knee pain is one of the main problems associated with knee osteoarthritis. The peak external knee adduction moment (KAM) in gait is commonly used to estimate medial knee loading, and elevated KAM has been related to a higher risk of developing knee pain in older adults. Although knee flexion moment (KFM) also contributes to medial knee loading, its role in the development of knee pain remains unclear.
AIM
To investigate the association between knee moments and the incidence of knee pain in 24 months in asymptomatic older adults.
DESIGN
Prospective cohort study.
SETTING
University laboratory.
POPULATION
Community-dwelling adults aged 60-80 years were recruited. We excluded participants with knee pain/known arthritis, knee injury, knee/hip joint replacement, cognitive impairment, or neurological conditions.
METHODS
Three-dimensional gait analysis was conducted to compute the peak KFM and KAM. Telephone surveys were conducted 12 and 24 months after the baseline assessment. Self-reported knee pain and its intensity and frequency were captured. Logistic regression with generalized estimating equations was used to examine associations between knee moments and the risk of knee pain.
RESULTS
Of the 162 eligible participants who completed the baseline assessment (age: 65.8±4.0 years, 61.1% females), 157 and 138 were also assessed for incident knee pain after 12 and 24 months, respectively. Compared with the lowest tertile, the highest tertile of KFM was significantly related to a lower incidence of frequent knee pain (RR=0.25, 95% CI: 0.08-0.85, P=0.027) in 24 months. In addition, a higher KFM was significantly associated with the lower intensity of incident knee pain after 24 months (β=-1.513; 95% CI: -2.879, -0.147; P=0.030). We also observed trends showing that a higher peak KAM was related to higher risks of developing any (RR=2.48, 95% CI: 0.99-6.20, P=0.053) and frequent (RR=3.82, 95% CI: 0.96-15.1, P=0.057) knee pain in 24 months.
CONCLUSIONS
A higher sagittal knee moment is associated with a lower risk of knee pain developing in 24 months in older adults.
CLINICAL REHABILITATION IMPACT
Interventions for promoting sagittal knee moment may be considered in preventative training programs for reducing knee pain among older adults.
Key words: Gait analysis, Knee, Pain, Aged
Knee pain is one of the main problems associated with knee osteoarthritis (OA). The annual prevalence of persistent knee pain is 25% among adults aged above 55 years.1 The prevalence of painful disabling knee OA is 10%, with a quarter of these individuals being severely disabled.1 More essentially, knee pain is found as a precursor to cartilage defects,2-4 suggesting that knee pain can be present before the occurrence of irreversible cartilage damage or osteophyte formation associated with knee osteoarthritis. Thus, it is important to identify factors related to the development of knee pain such that preventive measures can be implemented before structural changes.
Increase in mechanical loading in stance phase, particularly during the loading response, induces an abrupt and large impact load on the knee joints.5 The peak external knee adduction moment (KAM) is a surrogate measure of the sharing of medial to lateral knee joint loading during the stance phase of gait.6-8 Subjects with higher peak KAM had higher chance to develop frequent knee pain in 3-4 years9 and moderate knee OA in 7.5 years.10 Although the external knee flexion moment (KFM) also contributes to medial knee joint loading,7, 11 its role in knee health remains controversial.7, 11, 12 A lower KFM in the early stance phase is commonly observed in subjects with knee OA than the healthy controls.13-15 In contrast, a more recent study observed a higher KFM in the midstance phase of gait in knee OA patients with moderate/severe knee pain compared to the asymptomatic patients.16 Such phenomenon might relate to pain avoidance strategy in subjects with knee OA. In addition, inconsistent results about the peak KFM on the disease progression were reported.17, 18 In patients with knee OA, Chehab et al. found that a higher stance phase peak KFM was associated with greater medial tibial cartilage loss over 5 years,17 while a later study from Chang et al. could not detect associations between the change in KFM during the loading response phase and the exacerbation of cartilage damage or bone marrow lesions over 2 years.18
In subjects with knee OA, peak knee flexion angle (KFA) and knee flexion excursion (KFE) during the early stance phase were reduced13, 19 and that contribute to a lower stance phase KFM.20, 21 It is unclear whether such relationship was due to the avoidance of pain associated with knee flexion reductions in subjects with knee OA.22 If similar association could be detected in pain-free knees, modulation on knee flexion could be one of the strategies used to alleviate joint loadings, and thus to prevent knee symptoms.
The incidence of knee pain has been reported in previous prospective observations with 12-18 months’ follow-ups.23, 24 The primary aim of this study was to examine whether stance phase peak KFM and KAM were associated with the development of knee pain in asymptomatic older adults in 12 and 24months. Our secondary aim was to examine the relationships between knee flexions (peak KFA and KFE) and peak KFM in subjects without knee pain. We hypothesized that (1) higher peak KFM in addition to peak KAM would be related to higher risk of developing knee pain; and (2) lower sagittal knee motions (peak KFA and KFE) would be associated with lower peak KFM.
Materials and methods
Study design and sample
This was a prospective cohort study. Participants were recruited from local communities from November 2018 to October 2019. Potential participants were included if they were: 1) aged 60-80 years; 2) able to walk 10 m without using an assistive device. Potential participants were excluded if they had 1) knee pain or known arthritis; 2) a history of knee injury; 3) knee or hip joint replacement; 4) cognitive impairment; or 5) a neurological condition (e.g., stroke or Parkinson’s disease). All potential participants underwent a face-to-face interview to be screened against the inclusion and exclusion criteria. Study size was reached according to the availability of the eligible subjects during the study period. The study was approved by the human subject ethics sub-committee of the administering institution (ID no.: HSEARS20180110001). All eligible participants provided their written informed consent prior to data collection.
Demographics
At baseline, age, sex, and body mass, and body height were collected from all eligible participants. Known comorbidities (hypertension, diabetes, cardiopulmonary disease, and dyslipidemia) were also documented. Each participant was categorized as having a sedentary or active lifestyle based on the type and duration of physical exercises they undertook, as recommended by the U.S. Department of Health and Human Services.25 The Montreal Cognitive Assessment was used to screen for the presence of mild cognitive impairment (MCI), based on a cut-off score of 22.26
Gait analysis at baseline
The gait analysis was conducted at a motion and gait laboratory. An eight-camera (MX T40) Motion Analysis System (Vicon, Oxford, UK) with two floor-mounted force plates (Advanced Mechanical Technology Inc., Watertown, MA, USA) were used to capture three-dimensional motion and knee moments. Sampling rates of 1,000 and 100 Hz were used to capture the kinetic and kinematic data, respectively. The standard Plug-In-Gait marker set (Marker diameter: 14 mm) was applied to the pelvic, hip, knee, and ankle joints of both lower limbs.27 Marker trajectory data were digitally filtered using a Woltring quintic spline filter with a low-pass cut-off frequency of 10 Hz.28, 29 Each participant walked unshod and without any assistive device on a 10-m walkway at a self-selected comfortable speed. After three practice trials, data were collected. Five successful trials with a clean foot strike on the force plates of each leg were captured and saved for off-line analyses.
Nexus software (Version 2.5, Vicon) was used to analyze the knee joint kinetic and kinematic data for both limbs. A vertical ground reaction force threshold of 20 N was used to identify heel contact and toe-off events.11 A custom MATLAB program (MathWorks, Inc, Natick, MA, USA) was used to compute knee biomechanical outcomes. Early stance phase is identified as the initial 15–40% of the stance phase, and this is the period when the first peak of knee flexion occurs.30 Walking speed, peak values of knee flexion moment (KFM) and KAM during the stance phase; and peak KFA and KFE (i.e., the KFE from initial heel contact to its peak) during the early stance phase of the gait cycle were analyzed. Knee kinetic parameters were normalized to body mass. Each parameter was averaged over five successful trials for analysis.
Incidence of knee pain at follow-up
Telephone interviews were conducted 12 and 24 months after the baseline measurements, to define the incidence of knee pain. In telephone interviews, the following questions were asked for each participant: 1) during the past 1 month, have you experienced any knee pain at any of your knee joints during weight-bearing activities? (If yes) 2) If “0” represents no symptoms and “10” represents “the worst pain ever possible”, which number from 0 to 10 best indicates the level of knee pain you have experienced? 3) How many days have you experienced the knee pain during the past 1 month?
Knee pain was defined as pain perceived during weight-bearing activities with an intensity at or above 4 out of a score of 10 on Numeric Rating Scale (NRS).31 As the patient acceptable symptom state (PASS: a value of knee symptom below which patients consider their knee symptoms as acceptable) for OA patients was 32.3 of 100 mm on visual analog scale,32 a cut-off of ≥4 on NRS was used for the definitive knee pain above the APSS.31 In addition, the perceived pain during weight-bearing activities is a typical OA-related knee symptom.33 These approaches were chosen to improve the validity of outcome measures on the incidence of OA-related knee pain with clinical relevance at the telephone follow-ups. Subjects reported knee pain on at least 1 day in the previous month were classified as having “any knee pain” and those who had knee pain for more than 15 days (most days) during the previous month were classified as having “frequent knee pain”.34 The presence of knee pain on most days in the preceding month (i.e.,>15 days) is a widely used method to define the frequent, persistent, or chronic knee pain in OA studies.9, 34-36
Statistical analysis
In the primary analyses, the tertiles of peak KAM and peak KFM (using the total sample of 324 knees assessed at baseline) were computed to define the higher and lower cut-off values. The participants were grouped into the lowest, middle, and highest tertiles. Logistic regression was used to examine the associations between knee loading (categorical variables: peak KAM and peak KFM) and knee pain (dichotomous outcomes: any and frequent knee pain) adjusted by age, sex, body height, comorbidities, activity level, and walking speed. Generalized estimating equations (GEE) were used to control for between-knee correlations within each participant. The body mass was not entered into the regression models, as knee moments (Nm/kg) have been normalized by body mass.
In the secondary analyses, the associations of baseline knee moments (continues variables: KAM and KFM) with the intensity of incident knee pain and days with knee pain were assessed using linear regressions with GEE (account for the correlation between the two limbs of each participant), adjusted by age, sex, body height, comorbidities, activity level, and walking speed. Sensitivity analyses were conducted by entering both peak KFM and peak KAM into the same logistic or linear regression model to examine their associations with knee pain, adjusted by each other and the covariates.
The relationships between sagittal knee motions (continuous variables: peak KFA and KFE) and peak KFM (continuous outcome) were also examined using linear regressions with GEE, by controlling for age, sex, body height, comorbidities, activity level, and walking speed.
Adjusted relative risk (RR) with 95% confidence interval (95% CI) and corresponding P value were reported for each logistic regression model. Adjusted unstandardized regression coefficients (β) with 95% CI and corresponding P value were reported for each linear regression model. Statistical significance was preset at P<0.05 (two-tailed). Data analyses were conducted using SPSS 23.0 (IBM Corp., Armonk, NY, USA).
Results
Baseline cohort descriptions
Two hundred and twenty-five potential participants were screened, and 63 were excluded because of knee pain, known arthritis, knee injury, joint replacement, mild cognitive impairment, or stroke. Baseline gait analyses were conducted for the 162 eligible participants (61.1% females, age: 65.8±4.0 years) from November 2018 to October 2019. The participant inclusion diagram is shown in Figure 1. The demographics and descriptive data from baseline measurements are presented in Table I. No significant differences in demographic data or gait measurements were found between those who completed the study and those who dropped out.
Figure 1.
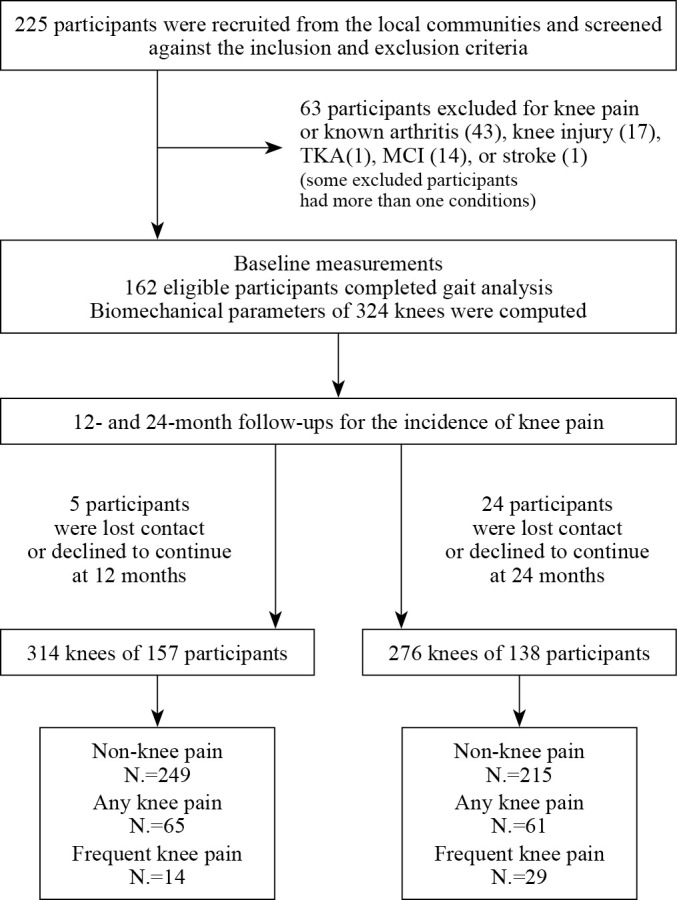
—Participant inclusion diagram. N.: number of knees; TKA: total knee arthroplasty; MCI: mild cognitive impairment.
Table I. —Baseline characteristics.
| Participants tested at baseline (N.=162) | Participants joining 12-month telephone survey (N.=157) | Participants joining 24-month telephone survey (N.=138) | |
|---|---|---|---|
| Demographics | |||
| Age (years) | 65.8±4.0 | 65.8±4.0 | 65.7±4.1 |
| Gender (females: males) | 99:63 | 95:62 | 84:54 |
| Body mass (kg) | 58.7±10.0 | 58.9±10.1 | 59.1±10.0 |
| Body height (m) | 1.59±0.08 | 1.59±0.08 | 1.59±0.08 |
| Activity level (N. of sedentary) | 83 | 82 | 69 |
| N. of comorbidities:* N. of participants | 0:92 1:44 >1:26 |
0:88 1:43 >1:26 |
0:78 1:36 >1:24 |
| Walking speed (m/s) | 1.19±0.18 | 1.19±0.18 | 1.18±0.17 |
| Knee loading (Nm/kg) | |||
| KAM | 0.66±0.17 | 0.66±0.17 | 0.66±0.16 |
| KFM | 0.30±0.25 | 0.29±0.25 | 0.29±0.24 |
| Knee flexions (degree) | |||
| KFA | 17.7±6.9 | 17.6±7.0 | 17.7±7.1 |
| KFE | 8.4±3.8 | 8.3±3.7 | 8.3±3.8 |
Values are mean±SD or numbers (N.) unless other indicates. *Including hypertension, diabetes, cardiopulmonary disease, and dyslipidemia. KAM: peak knee adduction moment; KFM: peak knee flexion moment; KFA, and KFE: peak knee flexion angle and knee flexion excursion during the early stance phase.
Knee loading and the risk of knee pain at 12 months
At the 12-month follow-up, 157 participants (97%) were contacted via telephone (age: 65.8±4.0 years, 60.5% females). The remaining 5 participants were either lost to follow-up or declined to continue with the study. Based on the telephone survey, 65 knees (20.7%) were identified as having any pain (NRS: 5.3±1.4). The incidence of frequent knee pain was 4.5% (N.=14/314 knees) (NRS: 5.3±1.2; painful days: 27.2±4.6). The results from logistic regression analyses showed that peak KAM and peak KFM were not associated with any knee pain (P=0.325-0.855; Table II) or frequent knee pain (P=0.254-0.990; Table II) over the 12-month study period.
Table II. —Relative risk of knee pain between different tertiles of knee loading in 12 months.
| Knee loading | Tertiles | Range in each tertile | Total knees | Risk of any knee pain | Risk of frequent knee pain | ||||
|---|---|---|---|---|---|---|---|---|---|
| Knees with any pain * | RR (95% CI)** |
P value | Knees with frequent pain * | RR (95% CI)** |
P value | ||||
| KAM (Nm/kg) |
Low (reference) | ≤0.596 | 103 | 18 (17.5%) | 1.00 | - | 2 (1.9%) |
1.00 | - |
| Medium | 0.597-0.722 | 104 | 25 (24.0%) | 1.49 (0.68, 3.27) |
0.325 | 5 (4.8%) |
2.38 (0.17, 34.1) |
0.523 | |
| High | ≥0.723 | 107 | 22 (20.6%) | 1.34 (0.58, 3.08) |
0.498 | 7 (6.5%) |
4.49 (0.34, 59.0) |
0.254 | |
| KFM (Nm/kg) |
Low (reference) | ≤0.175 | 104 | 21 (20.2%) | 1.00 | - | 5 (4.8%) |
1.00 | - |
| Medium | 0.176-0.383 | 107 | 25 (23.4%) | 1.31 (0.62, 2.77) |
0.484 | 5 (4.7%) |
1.01 (0.22, 4.60) |
0.990 | |
| High | ≥0.384 | 103 | 19 (18.4%) | 0.91 (0.35, 2.39) |
0.855 | 4 (3.9%) |
0.89 (0.14, 5.71) |
0.900 | |
*Number (%) of knees; **controlling for age, gender, body height, comorbidities, activity level, and walking speed; RR: adjusted relative risk; 95% CI: 95% confidence interval of RR. KAM: peak knee adduction moment; KFM: peak knee flexion moment.
Secondary analyses included 120 knees developed NRS pain (NRS: 4.1±1.8; painful days: 7.9±9.4) in 12 months. No significant relationship was found between knee moments and the intensity of knee pain or days with knee pain (P=0.236-0.766; Supplementary Digital Material 1: Supplementary Figure 1).
Similarly, no significant relationship between knee moments and knee pain in 12 months was observed in the sensitivity analyses by entering peak KFM and peak KAM into the same regression models.
Knee loading and the risk of knee pain at 24 months
At the 24-month telephone follow-up, 138 participants (85.2%) were contacted (age: 65.7±4.1 years, 60.9% females), and 24 participants were not able to be contacted or declined to continue participating in the study. The 24-month incidences of any knee pain and frequent knee pain were 22.1% (N.=61/276 knees) and 10.5% (N.=29/276 knees), respectively. The pain intensity for those with any knee pain was 5.2±1.4 on the numeric rating scale. For those with frequent knee pain, the pain intensity, and the number of days with pain were 5.2±1.5 and 21.9±5.8, respectively. Compared with the lowest tertile, the highest tertile of the peak KFM was significantly associated with a lower incidence of frequent knee pain (RR = 0.25, 95% CI: 0.08-0.85, P=0.027; Table III, Figure 2B). In contrast, there were trends showing that a higher peak KAM was associated with higher risks of developing any (RR=2.48, 95% CI: 0.99-6.20, P=0.053, Table III, Figure 2A) and frequent (RR=3.82, 95% CI: 0.96-15.1, P=0.057, Table III, Figure 2B) knee pain in 24 months. When peak KFM and peak KAM were entered into the same logistic model, similar results were found for the associations of peak KFM (RR=0.25, 95% CI: 0.07-0.89, P=0.031) and peak KAM (RR=3.71, 95% CI: 0.96-14.4, P=0.058) with the incidence of frequent knee pain in 24 months.
Table III. —Relative risk of knee pain between different tertiles of knee loading in 24 months.
| Knee loading | Tertiles | Range in each tertile | Total knees | Risk of any knee pain | Risk of frequent knee pain | ||||
|---|---|---|---|---|---|---|---|---|---|
| Knees with any pain * | RR (95% CI) ** |
P value |
Knees with frequent pain * | RR (95% CI) ** |
P value | ||||
| KAM (Nm/kg) |
Low (reference) | ≤0.596 | 93 | 15 (16.1%) | 1.00 | - | 6 (6.5%) |
1.00 | - |
| Medium | 0.597-0.722 | 92 | 21 (22.8%) | 1.69 (0.76, 3.79) |
0.201 | 10 (10.9%) |
2.33 (0.73, 7.45) |
0.152 | |
| High | ≥0.723 | 91 | 25 (27.5%) | 2.48 (0.99, 6.20) |
0.053 | 13 (14.3%) |
3.82 (0.96, 15.1) |
0.057 | |
| KFM (Nm/kg) |
Low (reference) | ≤0.175 | 92 | 24 (26.1%) | 1.00 | - | 15 (16.3%) |
1.00 | - |
| Medium | 0.176-0.383 | 94 | 21 (22.3%) | 0.79 (0.36, 1.72) |
0.555 | 9 (9.6%) |
0.50 (0.17, 1.43) |
0.196 | |
| High | ≥0.384 | 90 | 16 (17.8%) | 0.57 (0.24, 1.33) |
0.194 | 5 (5.6%) |
0.25 (0.08, 0.85) | 0.027 | |
*Number (%) of knees; **controlling for age, gender, body height, comorbidities, activity level, and walking speed. KAM: peak knee adduction moment; KFM: peak knee flexion moment; RR: adjusted relative risk; 95% CI: 95% confidence interval of RR.
Figure 2.
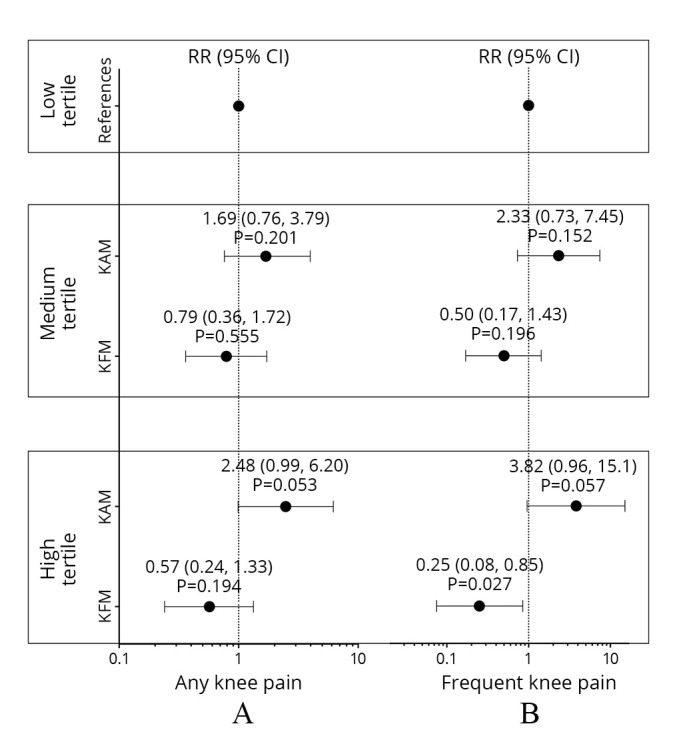
—Relative risk of knee pain between different tertiles of knee loading in 24 months. KAM: peak knee adduction moment; KFM: peak knee flexion moment; RR: adjusted relative risk; 95% CI: 95% confidence interval of RR.
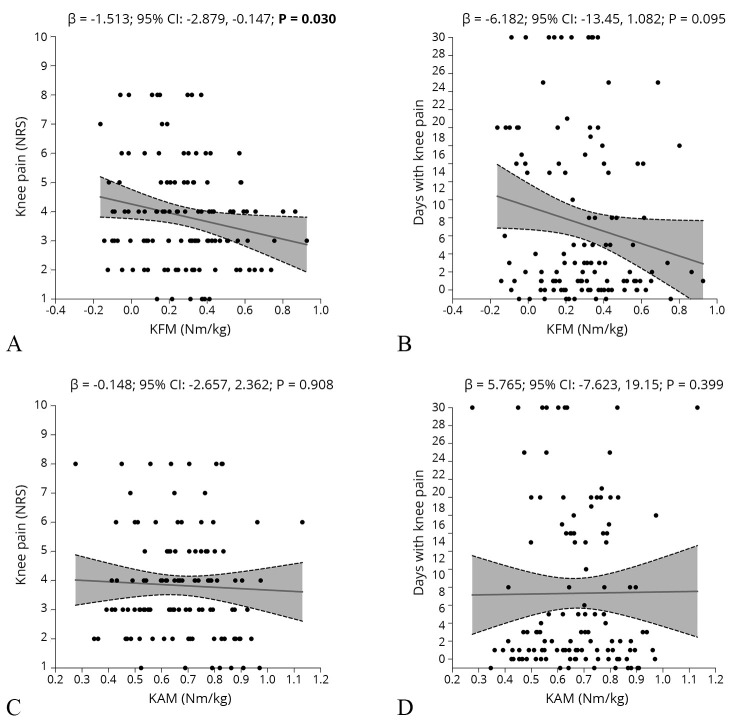
Secondary analyses were conducted among 120 knees developed NRS pain (NRS: 3.8±1.8; painful days: 9.3±9.1) in 24 months. A lower KFM was significantly associated with a higher intensity of knee pain with the adjustment of age, sex, body height, comorbidities, activity level, and walking speed (β=-1.513; 95% CI: -2.879, -0.147; P=0.030; Figure 3A). In addition, a trend of association could be seen between the lower KFM and more painful days (β=-6.182; 95% CI: -13.45, 1.082; P=0.095; Figure 3B). No significant relationship was found between peak KAM and the intensity of knee pain (P=0.908; Figure 3C) or days with knee pain (P=0.399; Figure 3D). Sensitivity analyses were conducted by adding peak KAM into the linear regression models, with a significant relationship persisted between baseline peak KFM and the intensity of NRS knee pain (β=-1.512; 95% CI: -2.883, -0.141; P=0.031); a similar trend remained for the association between baseline peak KFM and the painful days (β=-6.223; 95% CI: -13.38, 0.933; P=0.088).
Figure 3.
—Relationships between knee moments and (A and C) the intensity of knee pain and (B and D) days with knee pain among knees developed any NRS pain in 24 months, adjusted by age, sex, body height, comorbidities, activity level, and walking speed. β: adjusted regression coefficients; 95% CI: 95% confidence interval of β. KFM: peak knee flexion moment; KAM: peak knee adduction moment; NRS: Numeric Rating Scale.
Relationships between knee flexions and KFM
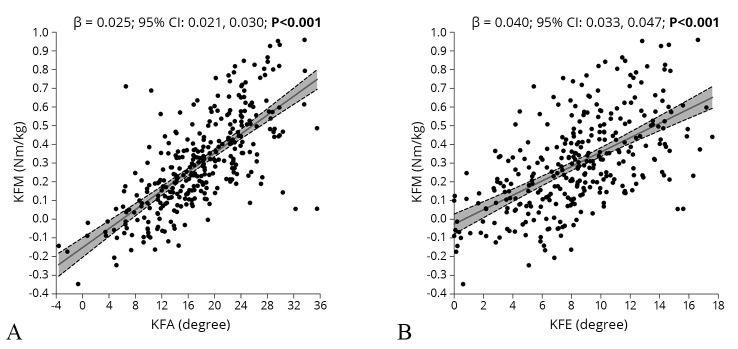
A larger peak KFA (β=0.025; 95% CI: 0.021, 0.030; P<0.001; Figure 4A) and a larger KFE (β = 0.040; 95% CI: 0.033, 0.047; P<0.001; Figure 4B) were associated with a higher peak KFM, adjusted by age, sex, body height, comorbidities, activity level, and walking speed.
Figure 4.
—Relationships between knee flexion moment and sagittal knee motions during the early stance phase, adjusted by age, sex, body height, comorbidities, activity level, and walking speed. KFM: peak knee flexion moment; KFA and KFE: peak knee flexion angle and knee flexion excursion during the early stance phase. β: adjusted regression coefficients; 95% CI: 95% confidence interval of β.
Discussion
Our findings indicated that a higher peak knee flexion moment during the stance phase of gait was associated with a lower incidence of frequent knee pain in 24 months in asymptomatic older adults. In addition, a higher peak KFM at baseline was associated with the lower intensity of the incident knee pain after 24 months. Furthermore, a higher peak knee flexion moment was related to larger peak KFE and KFE during the early stance phase in these subjects.
This study identified the 12- and 24-month incidence of knee pain in older adults with no prior complaints of knee pain. The 12-month incidences were 20.7% and 4.5%; and the 24-month incidences were 22.1% and 10.5% for any knee pain and frequent knee pain, respectively, in older adults aged between 60 and 80 years. Miranda et al. documented the 12-month incidence of knee pain, defined as having knee pain on more than 7 days, as 10.1% in middle-aged adult workers.23 Also, in subjects with a mean age of 49 years, Palmer et al. found that the 18-month incidences of any knee pain and frequent knee pain (i.e., pain happened at least once or 14 days in the past month, respectively) were 15.1% and 3.8%, respectively.24 In this study, we recruited older adults with a mean age of 65 years and found a relatively higher incidence of knee pain.
The results from regression analyses showed that baseline knee moments were not associated with the risk of knee pain in 12 months. It may suggest that the accumulative mechanical effects of knee moments on the risk of knee pain could not be detected in a relatively short-term observation. We observed trends showing that a higher peak KAM during the stance phase of walking was related to higher risks of developing any and frequent knee pain in 24 months. This finding partially echoed with the previous report from Amin et al. who observed associations between greater peak KAMs and the development of chronic knee pain after 3-4 years.9 However, the accumulative effects of KAM on the development of knee symptoms may be more obvious in a relatively longer period (e.g. >3 years). Moreover, the authors assessed peak KAM during different weight-bearing activities, including standing, chair rise, walking, and stair descent, and found that the participants who developed weight-bearing chronic knee pain exhibited higher peak KAM than those who did not, especially in standing and stair descent (by 35-39%), followed by walking and chair rise (by 8-13%).9 Thus, the mechanical impacts of KAM on the development of knee symptoms may be more obvious in other weight-bearing tasks (e.g., stair climbing). The KAM is regarded as a surrogate measure of the sharing of medial to lateral knee joint loading,6-8 and the elevated medial knee load would induce excessive mechanical loading on the cartilage and subchondral bone,37 which plays a crucial role in the pathogenesis of knee symptoms.38, 39 Hence, aside from the two abovementioned cohorts, more studies in the future are needed to confirm the role of KAM (measured during different weight-bearing tasks) in the pathogenesis of knee symptoms or OA.
This was the first prospective study to explore the role of KFM in the development of knee pain in asymptomatic population. We found that a higher peak KFM during the stance phase of gait reduced the likelihood of developing frequent knee pain in 24 months. In addition, a higher peak KFM at baseline was associated with the lower intensity of the incident knee pain after 24 months. Moreover, there was a trend showing a higher peak KFM may be related to less painful days. These findings were against our initial hypothesis that higher peak KFM might be associated with a higher risk of developing knee pain. The peak KFM contributes to 13-22% of the medial knee loading7, 11 and a higher peak KFM was found associated with greater cartilage degeneration in people with knee OA.17 There exit two possible explanations for our results. First, a higher peak KFM was associated with a lower peak KAM in patients with established knee OA.40, 41 These authors proposed that the redistribution of mechanical knee load from the frontal to the sagittal planes might be a protective strategy for pain avoidance associated with mechanical irritation in individuals with established knee OA.40, 41 However, the inverse relationships between the stance phase peak KAM and KFM could not be detected in our subjects.
Second, it could be explained by the interplays between knee motions and moments in the sagittal plane. Reduced knee flexions during the loading response phase of gait are commonly observed in persons with knee OA,13, 19 which often occurs concomitantly with a reduction in KFM acting to flex the knee joint.13-15 Our study indicated that smaller peak KFE (peak KFA) and KFE were associated lower peak KFM during the early stance phase of gait. Similar observations have been observed in individuals with established knee OA.20, 21 During the loading response, sufficient flexion of the knee joint is required to modulate the intensity21, 42, 43 and rate44, 45 of joint loading. A higher loading rate is related to early OA-related adverse effects on cartilage.46 In addition, reduced knee motions may shift the load-bearing contact area to the less-adapted regions of the knee joint.47 Taken together, reduced knee flexion motion might lead to a reduction in peak KFM as well as a high loading rate and a shifting of loading area, which might cause the incidence of knee pain. As such, a higher peak knee flexion motion may be beneficial for the prevention of knee pain in the aging population. Future clinical trials may further investigate whether the promotion of knee flexions would decrease the risk of developing knee pain via the resultant increase in sagittal knee moment. Sensitivity analyses by further entering peak KAM to the regression models showed that the associations of peak KFM with the incidence and intensity of the incident knee pain in 24 months were persisted, with KAM remained as a non-significant contributor. It may suggest that compared with the increased peak KAM, the decreased peak KFM could be a more sensitive biomechanical marker related to knee pain developing in the elderly.
Limitations of the study
The limitations of this study include the relatively weak way of assessing knee pain based the telephone interviews and the absence of a validated questionnaire to screen participants with knee pain related to inflammatory joint diseases.48 However, participants’ medical histories were reviewed to exclude those with known inflammatory joint diseases. This was important, as such inflammatory diseases may cause knee pain by other (non-OA) mechanisms. In addition, our follow-up surveys showed that no participant had newly diagnosed inflammatory diseases or knee injury. Furthermore, the incidence of knee pain was defined as perceived pain during weight-bearing activities, which is a typical OA-related knee symptoms.33 More importantly, we used a cut-off of NRS≥4 for the definitive knee pain (above PASS for knee OA patients)31, 32 and a commonly used definition for frequent knee pain in patients with knee OA (i.e., pain on >15 days during the past month).9, 34-36 However, a validated questionnaire optimally conducted in a daily manner will surely strengthen the outcome measures in OA-related knee pain. Second, according to our prior power analysis based on the previous study,9 the estimated sample size was 157 subjects (314 knees) to achieve a moderate effect with 80% study power. After considering the expected 20% dropouts, over 200 eligible participants (>400 knees) were originally planned to be recruited. Unfortunately, our baseline tests were interrupted in January 2020 by the COVID-19. As this was the first study to prospectively examine the association between KFM and the risk of knee pain developing. Future studies with larger sample size are expected to further confirm our findings. Another possible limitation was that the incidence of knee pain in the past one month was asked.34 This decision was made to minimize the potential recall bias, as those with more advanced age may have difficulty to recall of the knee symptoms in the past 12 or 24 months. However, it is possible that some participants may have developed knee pain earlier, and the symptom has been alleviated (NRS<4) or disappeared at the follow-up month. In this scenario, we would expect our results to be biased towards the null. Because if the true effects exist, we may miss out those participants with incidence of knee pain, and thus underestimate the effects. Moreover, the using of pain killers or other treatments for reducing knee pain was not considered in our analyses. We acknowledged this should be a strong factor related to knee pain. It is possible that some participants may have developed knee pain prior to the telephone interview, which may have been cured by using medications and/or other treatments by the follow-ups. In this case, we may miss out those subjects with incidence of knee pain. Similarly, if the true effects exist, our results may underestimate the effects of peak KFM on pain developing. Considering the above-mentioned potential limitations, the findings of our study may need to be interpreted with caution. Hence, future studies are expected to further investigate the role of KFM in the development of knee pain or OA in the elderly.
Conclusions
To conclude, a higher sagittal knee moment is associated with a lower risk of knee pain developing in 24 months in asymptomatic older adults. Such finding suggests that the lower knee flexion moment may be another risk factor related to the pathogenesis of knee pain. As larger sagittal knee motions are linked with the higher knee flexion moment, promoting knee flexions and maintaining a higher knee flexion moment may be beneficial for the prevention of knee pain in the aging population.
Supplementary Digital Material 1
Supplementary Figure 1
Relationships between knee moments and (A and C) the intensity of knee pain and (B and D) days with knee pain among knees developed NRS pain in 12 months, adjusted by age, sex, body height, comorbidities, activity level, and walking speed.
Acknowledgements
The authors thank all the study participants.
Footnotes
Conflicts of interest: The authors certify that there is no conflict of interest with any financial organization regarding the material discussed in the manuscript.
Funding: Special thanks to Dr. Roy Chung for the funding support on Mobile imaging of knee motion in early detection of knee osteoarthritis in adults (POO31011). The authors declare that the study sponsor was not involved in the study design; collection, analysis, and interpretation of the data; in the writing of the manuscript; or in the decision to submit the manuscript for publication.
References
- 1.Peat G, McCarney R, Croft P. Knee pain and osteoarthritis in older adults: a review of community burden and current use of primary health care. Ann Rheum Dis 2001;60:91–7. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=11156538&dopt=Abstract 10.1136/ard.60.2.91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Eckstein F, Cotofana S, Wirth W, Nevitt M, John MR, Dreher D, et al. Osteoarthritis Initiative Investigators Group . Greater rates of cartilage loss in painful knees than in pain-free knees after adjustment for radiographic disease stage: data from the osteoarthritis initiative. Arthritis Rheum 2011;63:2257–67. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=21520009&dopt=Abstract 10.1002/art.30414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang Y, Teichtahl AJ, Abram F, Hussain SM, welletier JP, Cicuttini FM, et al. Knee pain as a predictor of structural progression over 4 years: data from the Osteoarthritis Initiative, a prospective cohort study. Arthritis Res Ther 2018;20:250. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=30400973&dopt=Abstract 10.1186/s13075-018-1751-4 [DOI] [PMC free article] [PubMed]
- 4.Saunders J, Ding C, Cicuttini F, Jones G. Radiographic osteoarthritis and pain are independent predictors of knee cartilage loss: a prospective study. Intern Med J 2012;42:274–80. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=21299779&dopt=Abstract 10.1111/j.1445-5994.2011.02438.x [DOI] [PubMed] [Google Scholar]
- 5.Perry J, Burnfield J. Kinetics of Gait Ground Reaction Forces, Vectors, Moments, Power, and Pressure. In: Perry J, Burnfield J (editors). Gait analysis: normal and pathological function. Thorofare, NJ: Slack Incorporated; 2010. p. 457-69. [Google Scholar]
- 6.Zhao D, Banks SA, Mitchell KH, D’Lima DD, Colwell CW, Jr, Fregly BJ. Correlation between the knee adduction torque and medial contact force for a variety of gait patterns. J Orthop Res 2007;25:789–97. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=17343285&dopt=Abstract 10.1002/jor.20379 [DOI] [PubMed] [Google Scholar]
- 7.Richards RE, Andersen MS, Harlaar J, van den Noort JC. Relationship between knee joint contact forces and external knee joint moments in patients with medial knee osteoarthritis: effects of gait modifications. Osteoarthritis Cartilage 2018;26:1203–14. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=29715509&dopt=Abstract 10.1016/j.joca.2018.04.011 [DOI] [PubMed] [Google Scholar]
- 8.Birmingham TB, Hunt MA, Jones IC, Jenkyn TR, Giffin JR. Test-retest reliability of the peak knee adduction moment during walking in patients with medial compartment knee osteoarthritis. Arthritis Rheum 2007;57:1012–7. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=17665490&dopt=Abstract 10.1002/art.22899 [DOI] [PubMed] [Google Scholar]
- 9.Amin S, Luepongsak N, McGibbon CA, LaValley MP, Krebs DE, Felson DT. Knee adduction moment and development of chronic knee pain in elders. Arthritis Rheum 2004;51:371–6. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=15188321&dopt=Abstract 10.1002/art.20396 [DOI] [PubMed] [Google Scholar]
- 10.Lynn SK, Reid SM, Costigan PA. The influence of gait pattern on signs of knee osteoarthritis in older adults over a 5-11 year follow-up period: a case study analysis. Knee 2007;14:22–8. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=17092727&dopt=Abstract 10.1016/j.knee.2006.09.002 [DOI] [PubMed] [Google Scholar]
- 11.Manal K, Gardinier E, Buchanan TS, Snyder-Mackler L. A more informed evaluation of medial compartment loading: the combined use of the knee adduction and flexor moments. Osteoarthritis Cartilage 2015;23:1107–11. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=25862486&dopt=Abstract 10.1016/j.joca.2015.02.779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Creaby MW. It’s not all about the knee adduction moment: the role of the knee flexion moment in medial knee joint loading. Osteoarthritis Cartilage 2015;23:1038–40. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=25865394&dopt=Abstract 10.1016/j.joca.2015.03.032 [DOI] [PubMed] [Google Scholar]
- 13.Astephen JL, Deluzio KJ, Caldwell GE, Dunbar MJ. Biomechanical changes at the hip, knee, and ankle joints during gait are associated with knee osteoarthritis severity. J Orthop Res 2008;26:332–41. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=17960658&dopt=Abstract 10.1002/jor.20496 [DOI] [PubMed] [Google Scholar]
- 14.Landry SC, McKean KA, Hubley-Kozey CL, Stanish WD, Deluzio KJ. Knee biomechanics of moderate OA patients measured during gait at a self-selected and fast walking speed. J Biomech 2007;40:1754–61. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=17084845&dopt=Abstract 10.1016/j.jbiomech.2006.08.010 [DOI] [PubMed] [Google Scholar]
- 15.Astephen JL, Deluzio KJ, Caldwell GE, Dunbar MJ, Hubley-Kozey CL. Gait and neuromuscular pattern changes are associated with differences in knee osteoarthritis severity levels. J Biomech 2008;41:868–76. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=18078943&dopt=Abstract 10.1016/j.jbiomech.2007.10.016 [DOI] [PubMed] [Google Scholar]
- 16.O’Connell M, Farrokhi S, Fitzgerald GK. The role of knee joint moments and knee impairments on self-reported knee pain during gait in patients with knee osteoarthritis. Clin Biomech (Bristol, Avon) 2016;31:40–6. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=26527453&dopt=Abstract 10.1016/j.clinbiomech.2015.10.003 [DOI] [PubMed] [Google Scholar]
- 17.Chehab EF, Favre J, Erhart-Hledik JC, Andriacchi TP. Baseline knee adduction and flexion moments during walking are both associated with 5 year cartilage changes in patients with medial knee osteoarthritis. Osteoarthritis Cartilage 2014;22:1833–9. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=25211281&dopt=Abstract 10.1016/j.joca.2014.08.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chang AH, Chmiel JS, Almagor O, Guermazi A, Prasad PV, Moisio KC, et al. Association of baseline knee sagittal dynamic joint stiffness during gait and 2-year patellofemoral cartilage damage worsening in knee osteoarthritis. Osteoarthritis Cartilage 2017;25:242–8. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=27729289&dopt=Abstract 10.1016/j.joca.2016.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schmitt LC, Rudolph KS. Influences on knee movement strategies during walking in persons with medial knee osteoarthritis. Arthritis Rheum 2007;57:1018–26. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=17665469&dopt=Abstract 10.1002/art.22889 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fukaya T, Mutsuzaki H, Mori K. Relations between external moment and movement of the knee joint during the stance phase in patients with severe knee osteoarthritis. J Orthop 2019;16:101–4. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=30655656&dopt=Abstract 10.1016/j.jor.2018.12.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Creaby MW, Hunt MA, Hinman RS, Bennell KL. Sagittal plane joint loading is related to knee flexion in osteoarthritic gait. Clin Biomech (Bristol, Avon) 2013;28:916–20. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=23938182&dopt=Abstract 10.1016/j.clinbiomech.2013.07.013 [DOI] [PubMed] [Google Scholar]
- 22.Henriksen M, Graven-Nielsen T, Aaboe J, Andriacchi TP, Bliddal H. Gait changes in patients with knee osteoarthritis are replicated by experimental knee pain. Arthritis Care Res (Hoboken) 2010;62:501–9. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=20391505&dopt=Abstract 10.1002/acr.20033 [DOI] [PubMed] [Google Scholar]
- 23.Miranda H, Viikari-Juntura E, Martikainen R, Riihimäki H. A prospective study on knee pain and its risk factors. Osteoarthritis Cartilage 2002;10:623–30. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=12479384&dopt=Abstract 10.1053/joca.2002.0796 [DOI] [PubMed] [Google Scholar]
- 24.Palmer KT, Reading I, Calnan M, Linaker C, Coggon D. Does knee pain in the community behave like a regional pain syndrome? Prospective cohort study of incidence and persistence. Ann Rheum Dis 2007;66:1190–4. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=17114191&dopt=Abstract 10.1136/ard.2006.061481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Physical Activity Guidelines for Americans. Physical Activity Guidelines Advisory Committee of U.S. Department of Health and Human Services; 2008. p. 29-34. [Google Scholar]
- 26.Lee JY, Cho SJ, Na DL, Kim SK, Youn JH, Kwon M, et al. ; Dong Woo Lee; Hong Jin Jeon; You Ra Lee; Maeng Je Cho. Brief screening for mild cognitive impairment in elderly outpatient clinic: validation of the Korean version of the Montreal Cognitive Assessment. J Geriatr Psychiatry Neurol 2008;21:104–10. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=18474719&dopt=Abstract 10.1177/0891988708316855 [DOI] [PubMed] [Google Scholar]
- 27.Dixon SJ, Hinman RS, Creaby MW, Kemp G, Crossley KM. Knee joint stiffness during walking in knee osteoarthritis. Arthritis Care Res (Hoboken) 2010;62:38–44. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=20191489&dopt=Abstract 10.1002/acr.20012 [DOI] [PubMed] [Google Scholar]
- 28.Woltring HJ. A Fortran package for generalized, cross-validatory spline smoothing and differentiation. Adv Eng Softw 1986;8:104–13. 10.1016/0141-1195(86)90098-7 [DOI] [Google Scholar]
- 29.Esrafilian A, Karimi MT, Amiri P, Fatoye F. Performance of subjects with knee osteoarthritis during walking: differential parameters. Rheumatol Int 2013;33:1753–61. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=23292190&dopt=Abstract 10.1007/s00296-012-2639-2 [DOI] [PubMed] [Google Scholar]
- 30.Heiden TL, Lloyd DG, Ackland TR. Knee joint kinematics, kinetics and muscle co-contraction in knee osteoarthritis patient gait. Clin Biomech (Bristol, Avon) 2009;24:833–41. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=19765867&dopt=Abstract 10.1016/j.clinbiomech.2009.08.005 [DOI] [PubMed] [Google Scholar]
- 31.Ruhdorfer A, Wirth W, Dannhauer T, Eckstein F. Longitudinal (4 year) change of thigh muscle and adipose tissue distribution in chronically painful vs painless knees—data from the Osteoarthritis Initiative. Osteoarthritis Cartilage 2015;23:1348–56. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=25887367&dopt=Abstract 10.1016/j.joca.2015.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tubach F, Ravaud P, Baron G, Falissard B, Logeart I, Bellamy N, et al. Evaluation of clinically relevant states in patient reported outcomes in knee and hip osteoarthritis: the patient acceptable symptom state. Ann Rheum Dis 2005;64:34–7. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=15130902&dopt=Abstract 10.1136/ard.2004.023028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhang W, Doherty M, Peat G, Bierma-Zeinstra MA, Arden NK, Bresnihan B, et al. EULAR evidence-based recommendations for the diagnosis of knee osteoarthritis. Ann Rheum Dis 2010;69:483–9. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=19762361&dopt=Abstract 10.1136/ard.2009.113100 [DOI] [PubMed] [Google Scholar]
- 34.Soni A, Kiran A, Hart DJ, Leyland KM, Goulston L, Cooper C, et al. Prevalence of reported knee pain over twelve years in a community-based cohort. Arthritis Rheum 2012;64:1145–52. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=22180258&dopt=Abstract 10.1002/art.33434 [DOI] [PubMed] [Google Scholar]
- 35.Carlesso LC, Segal NA, Frey-Law L, Zhang Y, Na L, Nevitt M, et al. Pain susceptibility phenotypes in those free of knee pain with or at risk of knee osteoarthritis: the multicenter osteoarthritis study. Arthritis Rheumatol 2019;71:542–9. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=30307131&dopt=Abstract 10.1002/art.40752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Englund M, Niu J, Guermazi A, Roemer FW, Hunter DJ, Lynch JA, et al. Effect of meniscal damage on the development of frequent knee pain, aching, or stiffness. Arthritis Rheum 2007;56:4048–54. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=18050201&dopt=Abstract 10.1002/art.23071 [DOI] [PubMed] [Google Scholar]
- 37.Trepczynski A, Kutzner I, Bergmann G, Taylor WR, Heller MO. Modulation of the relationship between external knee adduction moments and medial joint contact forces across subjects and activities. Arthritis Rheumatol 2014;66:1218–27. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=24470261&dopt=Abstract 10.1002/art.38374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Perry TA, Parkes MJ, Hodgson RJ, Felson DT, Arden NK, O’Neill TW. Association between Bone marrow lesions & synovitis and symptoms in symptomatic knee osteoarthritis. Osteoarthritis Cartilage 2020;28:316–23. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=31877381&dopt=Abstract 10.1016/j.joca.2019.12.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Felson DT, Chaisson CE, Hill CL, Totterman SM, Gale ME, Skinner KM, et al. The association of bone marrow lesions with pain in knee osteoarthritis. Ann Intern Med 2001;134:541–9. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=11281736&dopt=Abstract 10.7326/0003-4819-134-7-200104030-00007 [DOI] [PubMed] [Google Scholar]
- 40.Huang C, Chan PK, Chiu KY, Yan CH, Yeung SS, Fu SN. Exploring the relationship between pain intensity and knee moments in participants with medial knee osteoarthritis: a cross-sectional study. BMC Musculoskelet Disord 2021;22:685. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=34384397&dopt=Abstract 10.1186/s12891-021-04587-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Asay JL, Erhart-Hledik JC, Andriacchi TP. Changes in the total knee joint moment in patients with medial compartment knee osteoarthritis over 5 years. J Orthop Res 2018;36:2373–9. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=29611879&dopt=Abstract 10.1002/jor.23908 [DOI] [PubMed] [Google Scholar]
- 42.Kawaji H, Kojima S. Effect of altered sagittal-plane knee kinematics on loading during the early stance phase of gait. Gait Posture 2019;74:108–13. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=31499404&dopt=Abstract 10.1016/j.gaitpost.2019.08.021 [DOI] [PubMed] [Google Scholar]
- 43.Luc-Harkey BA, Harkey MS, Stanley LE, Blackburn JT, Padua DA, Pietrosimone B. Sagittal plane kinematics predict kinetics during walking gait in individuals with anterior cruciate ligament reconstruction. Clin Biomech (Bristol, Avon) 2016;39:9–13. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=27614716&dopt=Abstract 10.1016/j.clinbiomech.2016.08.011 [DOI] [PubMed] [Google Scholar]
- 44.Riskowski JL. Gait and neuromuscular adaptations after using a feedback-based gait monitoring knee brace. Gait Posture 2010;32:242–7. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=20558068&dopt=Abstract 10.1016/j.gaitpost.2010.05.002 [DOI] [PubMed] [Google Scholar]
- 45.Cook TM, Farrell KP, Carey IA, Gibbs JM, Wiger GE. Effects of restricted knee flexion and walking speed on the vertical ground reaction force during gait. J Orthop Sports Phys Ther 1997;25:236–44. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=9083942&dopt=Abstract 10.2519/jospt.1997.25.4.236 [DOI] [PubMed] [Google Scholar]
- 46.Nia HT, Bozchalooi IS, Li Y, Han L, Hung HH, Frank E, et al. High-bandwidth AFM-based rheology reveals that cartilage is most sensitive to high loading rates at early stages of impairment. Biophys J 2013;104:1529–37. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=23561529&dopt=Abstract 10.1016/j.bpj.2013.02.048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Andriacchi TP, Mündermann A, Smith RL, Alexander EJ, Dyrby CO, Koo S. A framework for the in vivo pathomechanics of osteoarthritis at the knee. Ann Biomed Eng 2004;32:447–57. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=15095819&dopt=Abstract 10.1023/B:ABME.0000017541.82498.37 [DOI] [PubMed] [Google Scholar]
- 48.Barbour JA, Binding J, Bridges M, Kelly C. Evaluation of a screening tool for inflammatory joint disease. Ann Rheum Dis 2003;62:187–8. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=12525396&dopt=Abstract 10.1136/ard.62.2.187 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Figure 1
Relationships between knee moments and (A and C) the intensity of knee pain and (B and D) days with knee pain among knees developed NRS pain in 12 months, adjusted by age, sex, body height, comorbidities, activity level, and walking speed.