Abstract
The reporting case is a 27 year-old woman. She was admitted with complaints of clumsy gait and dysesthesia over her upper limbs and spasticity in the legs. The investigations revealed a long segment cervical intramedullary tumor, associated with whole cord syringomyelia. The superior part of syringomyelia image intensity matched intramedullary lipoma completely. C1–C5 intramedullary tumor was resected grossly under microscopic view, and a fat-containing liquid exited the syringomyelia cavity at its superior pole. After a transient paresis just following the surgery, neurological condition was improved. The follow-up imaging showed that the fatty syringomyelia reduced in dimensions. Conclusion. According to this case and another similar case due to instability, it appears that as a rare phenomenon, syringomyelia liquid content sometimes could have fatty droplets which could mimic intramedullary lipoma with an unknown mechanism. It seems these fat droplets in syringomyelia would not change its natural history.
Keywords: Syringomyelia, lipoma, astrocytoma, spinal cord neoplasms
Introduction
Syringohydromyelia has been used for description of pathologic accumulation of cerebrospinal fluid (CSF) within the central canal or the spinal cord due to CSF circulation disturbance. 1 Therefore, its radiological characteristic findings should be similar to CSF.
Nonetheless, in this case of intramedullary cervical pilocytic astrocytoma which was associated with entire cord syrinx, the upper part of syrinx had imaging features that completely matched intramedullary lipoma.2, 3
The diagnostic and management issues in this rare clinical condition were reported. According to our literature review, this is the first report of spinal cord neoplasm associated with fatty syringomyelia. There is only one similar fatty syringomyelia case due to instability. 4
Case report
History and physical examination
A 27 year-old woman presented with a history of progressive neck pain and dysesthesia and tingling in the shoulders and upper limbs for 1.5 years. The symptoms were progressive in intensity and had worsened over the last 3 months.
In addition, she developed difficulty in the gait and reported some falling down episodes. It was difficult for her to put clothes on. Recently, she developed urinary urgency but no bowel complaint. She also noticed the wasting of shoulder pads. Neurological examination revealed upper motor signs in the upper (Hoffman test) and lower limbs (upward plantar reflex). There was mild spasticity in the hands and both legs and mild quadriparesis. She had decreased sensations of pain and temperature.
Imaging
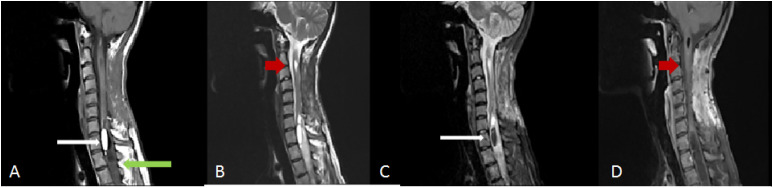
Magnetic resonance imaging (MRI) of the spine showed a central intramedullary tumor with hypo and hyper signal intensities in T1 and T2, respectively, and fine enhancement at contrast T1-weighted images extending from C1 down to C5 (Figure 1). There was associated heterogeneous expansive syringomyelia occupying the entire length of the cord and also inferior part of the medulla.
Figure 1.
White long arrows show intramedullary hypersignal lesions (fatty syrinx), and green long arrow shows hyposignal lesion (syrinx) on T1-weighted image (a). Red arrow shows intramedullary hypersignal lesion (tumor), and green long arrow shows hyposignal lesion (syrinx) on T2-weighted image (b). White long arrows show intramedullary hyposignal lesions (fatty syrinx), and red arrow shows intramedullary hypersignal lesion (tumor) on T2 fat suppression-weighted image (c). Red arrow shows enhancement of intramedullary lesion (tumor) on postcontrast T1-weighted image (d).
The syringomyelia at the inferior part of the medulla, superior to the tumor, and C5-T2 inferior to the tumor was hyperintense on both T1-weighted and T2-weighted images (Figure 1). These imaging features were suggestive of an intramedullary lipoma. Fat suppression images confirmed that the lesion matched with a lipoma in imaging.
Cervical computed tomography (CT) confirmed a fat-containing lesion in the cord at the two mentioned parts. There were hemivertebrae with kyphosis at T9 and cystic dilation at conus medullaris of the spinal cord suggestive of cystic dilation of a ventriculus terminalis 5 or focal entrapped syrinx (Figure 2).
Figure 2.
Blue long arrows show T9 hemivertebra, and orange arrow shows cystic dilation at conus medullaris on T2-weighted image.
Treatment
The patient underwent an operation for microscopic tumor resection. C2–C5 laminectomy was performed and the dura was opened. Under microscopic view, after midline myelotomy, the tumor was found with yellow-gray color and firm consistency. There was a distinct plane between the tumor and normal cord tissue; therefore, it was dissected completely and resected grossly. Then, at the inferior limit of tumor bed resection, the superior pole of fatty syringomyelia opened and a yellow-colored liquid with fatty mixed appearance exited (Figure 3). It was compatible with imaging findings; however, there was no solid lipoma. No adjuvant treatment was applied.
Figure 3.
White long arrow shows fatty liquid (fatty droplets on pathology) of intramedullary fatty syrinx under microscopic view (a). Pathologic evaluation shows pilocytic astrocytoma infiltrated with inflammatory cells including lipid-laden macrophage and cholesterol deposits (b).
Histopathology
Tumor pathologic examination revealed pilocytic astrocytoma infiltrated with inflammatory cells including lipid-laden macrophages and cholesterol deposits (Figure 3).
Follow-up
After a transient paresis, the patient had a remarkable improvement in the pain and gait. The spasticity decreased and the leg force became better. At a follow-up of 18 months, she was relieved of her major symptoms. Motor force examination was normal. Control MRI showed significant regression of intramedullary fatty syringomyelia dimensions and gross total tumor resection (Figure 4).
Figure 4.
Postoperative MRI: White long arrow shows intramedullary hypersignal lesion (fatty syrinx) remnant, and green long arrow shows hyposignal lesion (syrinx) remnant on T1-weighted image (a). Red arrow shows intramedullary lesion (tumor) resection on T2-weighted image (b). White long arrow shows intramedullary hyposignal lesion (fatty syrinx) remnant on T2 fat suppression-weighted image (c). Red arrow shows complete intramedullary lesion (tumor) resection on postcontrast T1-weighted image (d).
Discussion
In this case, there was an intramedullary pilocytic astrocytoma tumor with fine central enhancement associated with the entire cord syringomyelia and cystic dilation of conus medullaris. Syringomyelia imaging findings just above the tumor (the inferior part of medulla and C1) and below the tumor (C5-T2) were radiologically characteristic of lipoma. Nonetheless, considering the existence of the tumor at C2–C5, lipoma-mimicking lesions’ shape (completely intramedullary) and extension, and a more possible clinical entity, it was assumed to be fatty or fat-containing syringomyelia. Although according to the literature review, there was no similar reported case at the time.
Surgical findings and pathologic examination and control MRI confirmed lipid-containing syringomyelia and ruled out the intramedullary lipoma.
Until now, according to our literature review, there is no reported case of a similar case as an association of spinal cord neoplasm and fat-containing syringomyelia mimicking lipoma. There was only one report by Atul Goel et al. 4 in 2020 suggesting lipoma-like syringomyelia fading after treatment of instability without any intervention to syringomyelia. 4
They described that “the reduction of lipoma on delayed postoperative imaging,” similar to the reduction in the syringomyelia cavity, was a surprising observation. 4 Multiple types are described for spinal cord lipoma from complete intraspinal to lipomyelomeningocele 3 and fatty filum terminale 6 according to the embryonic background of spinal lipoma. It is nearly impossible to have a circumscribed lipoma in a fused spinal cord, and spinal cord lipoma almost always has to be associated with an open, unfused, and tethered cord.
Regarding the pathogenesis and the treatment, no definite conclusions can be drawn from a single or two clinical reports. However, these reports show that syringomyelia content could contain cholesterol or fatty macrophages with unknown mechanisms. Therefore, it could mimic the intramedullary lipoma radiologically. We suggest the term “fatty syringomyelia” for a better description of this rare entity to distinguish it from intramedullary lipoma.
According to Goel’s reported case, both typical and fatty syringomyelia are similar, and the existence of these fats in syringomyelia would not change the natural history. More importantly, surgical management is similar, and if the underlying pathology is treated, fatty syringomyelia would disappear spontaneously as well.
Due to the different underlying pathology of these two reported cases (tumor vs instability), it is unlikely for the fat content to be related to the tumor pathogenesis. Hence, fatty syringomyelia could occur in other pathologies like typical syringomyelia, and its natural history is not much different. Pathogenesis and etiology for this entity need further investigation.
Conclusion
This is the first report of fatty syringomyelia in association with spinal cord astrocytoma. The diagnosis and differentiation of fatty syringomyelia from lipoma are important from radiological point of view and even more critical in making surgical decisions. The natural history appears to be similar to typical syringomyelia.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Consent for publication: Informed consent was taken from the patient whose identifying information is included in this article.
ORCID iD
Mahdi Arjipour http://orcid.org/0000-0002-0261-1492
References
- 1.Guinto G, Abdo M, Aréchiga N, et al. Different types of syringomyelia and their management: part I. Contemp Spine Surg 2010; 11(6): 1–7. [Google Scholar]
- 2.Khoshnevisan A, Mirkoohi M, Arjipour M. Tectal lipoma: a case report and review of literature. Tehran Univ Med Sci 2012; 70(3). [Google Scholar]
- 3.Esmaeili A, Hanaei S, Fadakar K, et al. Risk factors associated with lipomyelomeningocele: a case-control study. Pediatr Neurosurgery 2013; 49(4): 202–207. [DOI] [PubMed] [Google Scholar]
- 4.Goel A, Patil A, Shah A, et al. Central atlantoaxial instability as a cause of syringomyelia mimic intramedullary lipoma. J Craniovertebral Junction Spine 2020; 11(2): 152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zeinali M, Safari H, Rasras S, et al. Cystic dilation of a ventriculus terminalis: case report and review of the literature. Br J Neurosurg 2017; 33: 294–298. [DOI] [PubMed] [Google Scholar]
- 6.Morota N, Ihara S, Ogiwara H. New classification of spinal lipomas based on embryonic stage. J Neurosurg Pediatr 2017; 19(4): 428–439. [DOI] [PubMed] [Google Scholar]