Summary
A large number of multidisciplinary, qualitative and quantitative research suggests that providing care for family members with mental health illnesses can have both positive and negative effects on the carers’ wellbeing. However, to date a comprehensive overview and synthesis of literature that compares and contrasts positive and negative effects of family-caregiving on the carer is missing. To address this gap, this scoping review examines the effects of family-caregiving on carers’ wellbeing. A Boolean search generated a total of 92 relevant articles that were included in the analysis. The results suggest that, to understand the effects of family-caregiving on the carer’s mental and physical wellbeing, it is necessary to take a combination of situational and sociodemographic characteristics into consideration. Elderly, female, spousal-carers and primary-carers may be a group that is at risk of suffering from a lack of positive mental and physical wellbeing as a result of caring. However, the negative effects of caregiving can be balanced by extraversion, social support and religious or spiritual beliefs. Therefore, future interventions that aim to promote family caregivers’ wellbeing may need to take personality, particular circumstances as well as cultural and personal beliefs into consideration.
Keywords: family caregiving, scoping review, mental health, family carers
INTRODUCTION
According to recent studies, an increasing number of people experience mental health disorders (Fernando, 2014; Bruffaerts et al., 2015; Polanczyk et al., 2015; Hanna et al., 2018). Due to a global deinstitutionalization of the treatment of mental illnesses, only a low proportion of those suffering from mental illnesses are admitted to hospitals (WHO, 2017). Of those who are hospitalized, ∼30–50% experience a relapse of symptoms within the first 6 months and 50–70% in the first 5 years after being discharged (Chang and Chou, 2015; Ali et al., 2017; Sadock et al., 2017). Comorbidity with other mental illness, non-adherence to medication, shorter duration on treatment and experiencing stressful life events as well as high disability score, and a single admission history are significant predictors of mental health relapse (Agenagnew and Kassaw, 2020; Moges et al., 2021). Patients with psychotic disorders who also experience common mental health disorders such as depression and anxiety are more likely to experience a relapse (Ali et al., 2017; Moges et al., 2021). Some novel approaches such as receiving low-intensity personalized advice via text-messages post-treatment (Malins et al., 2020) and specific forms of therapy such as Acceptance and Commitment Therapy (Østergaard, 2020), mind–body relaxation and therapies that allow the patient to develop healthy coping skills (Melemis, 2015) can be particularly beneficial in relapse prevention. However, as family and spousal carers live with patients and are usually the first to recognize behavioural changes, they play an increasingly important role in supporting and rehabilitating those who suffer from mental health illnesses.
The challenges that family members who care for those with mental health illnesses face are well documented in the literature. Family caregivers are at an increased risk of suffering physically, psychologically and socially while providing care for family members with mental health conditions (Sharma et al., 2016; Akbari et al., 2018; Norris et al., 2018; Özgönül and Bademli, 2022). Specifically, studies have shown that caring for family members with mental health problems can lead to social isolation, financial difficulties, occupational restrictions and negative emotions such as anger, aggression, frustration, low self-esteem, constant worry and feelings of helplessness (van der Sanden et al., 2013, 2015; Yin et al., 2014; Lamont and Dickens, 2021). In addition, there is an increased risk of reduced life-expectancy, lower wellbeing and mastery of life skills, and less time spent doing leisure activities for family caregivers (Akbari et al., 2018; Hsiao et al., 2020; McKee, 2020; Dadalto and Cavalcante, 2021).
Yet, research also shows that caring for a family member may also affect the caregivers in positive ways (Roth et al., 2015). For example, literature suggests that some family carers can become more resilient over time (Crellin et al., 2014; Donnellan et al., 2015; Ong et al., 2018; Post et al., 2021). While there are different definitions for caregiver resilience in the literature, they all share similar descriptions for the characteristics for overcoming adversity. This is explained as not only being about surviving the burden associated with caring for a mentally ill family member, but also growing into a stronger, more adaptable and healthier person (Amagai et al., 2016; Pione et al., 2021). In addition, family caregiving can improve the relationship between the caregiver and the person they care for, while also providing a sense of inner strength and satisfaction (Kate et al., 2013; Roth et al., 2015; Grover et al., 2017; Shiraishi and Reilly, 2019).
While previous research examined possible challenges and advantages of caring for family members with mental health problems, a comprehensive overview and synthesis of the literature appears to be missing. This is problematic, as there is a need to understand the unique challenges that family carers face and determine possible sources of help and support that would allow for implementation of informed strategies to meet the carers’ needs. The present study addresses this gap by reviewing empirical studies and scientific evidence to capture both the challenges and positive aspects of caregiving in the family context.
METHODS
A scoping review was used to synthesize the relevant literature on family caregiving (Arksey and O’Malley, 2005; Levac et al., 2010). Scoping reviews are a ‘useful way of mapping fields of study where it is difficult to visualize the range of material that might be available’ [(Arksey and O’Malley, 2005), p. 21]. They allow for a synthesis of the literature across different academic disciplines. This technique was relevant to the present study as empirical inquiry surrounding positive and negative effects of family caregiving are the subject of interest in various disciplines. For example, clinical studies might examine the physical and mental health effects of family caregiving, and psychological studies observe the severity of caregiver burden or changes in identity formation, whereas sociological studies tend to focus on the effects of family caregiving on social structures such as families or friendship networks. A scoping review utilizes a rigorous methodological framework consisting of five steps, which includes contributions from several disciplines. It maps the terrain of existing research and highlights gaps in knowledge (Arksey and O’Malley, 2005; Levac et al., 2010). As a method for reviewing literature, scoping studies have distinct characteristics (Arksey and O’Malley, 2005). Unlike systematic reviews, they address broader topics and topic areas in which many different study designs might be applicable (Arksey and O’Malley, 2005). Therefore, this approach was suitable to identify relevant themes in family caregiving in relation to caregiver health and wellbeing. The present study utilized Arksey and O’Malley’s (Arksey and O’Malley, 2005) five-step protocol of scoping reviews because this is one of the most frequently utilized and published frameworks in scoping review literature (i.e. Abraham et al., 2010; Halas et al., 2015; O’Flaherty and Phillips, 2015; O’Brien et al., 2016; Walsh et al., 2019). The five steps include: (i) identifying the research question, (ii) identifying relevant studies, (iii) study selection, (iv) charting the data and (v) collating, summarizing and reporting the results. Each step is outlined in more detail below.
Step 1: Identifying the research question
The first methodological step when conducting a scoping review is to determine the focus of the research question (Arksey and O’Malley, 2005; Levac et al., 2010). A research team from Robert Gordon University (Aberdeen), Anglia Ruskin University and the Forces in Mind Research Centre (Chelmsford) considered the appropriate balance of breadth and depth for the research topics (Arksey and O’Malley, 2005; Levac et al., 2010) during the literature review. The following questions were determined in December 2020 and guided the scoping review:
“How does family caregiving affect the caregiver physically, mentally and socially?” and
“How can family carers be best supported?”.
Step 2: Identifying relevant studies
Guidelines concerning the identification of the literature in scoping reviews, include the development of search terms, identification of databases, and the establishment of time frames, were followed (Levac et al., 2010). Therefore, the present review drew on a broad interpretation of search strings related to family caring and wellbeing. The social and health sciences databases APA Psych Articles, Web of Science, Science Direct, Scopus, Springer Link, SAGE Discipline Hub: Psychology and Counselling, Medline, SocINDEX, CINAHL and PTSDpubs were accessed. Additional studies were identified by manual searching the reference lists of the reviewed articles. The selection of articles was limited to peer-reviewed, English-language empirical studies published between January 2001 and March 2021 to ensure the recency of empirical evidence. Databases were searched by combining the search strings on family caregiving and the physical, mental and social consequences of caring. The key words were ‘Mental Health’ with the search strings ‘Mental health problem*’, ‘Mental health issue*’, ‘Ill-mental health’, ‘Mental health disorder*’, ‘Mental Distress’ and ‘Family Care’ with the search strings ‘Spousal carer*/ing’, ‘Informal care*/caring’, ‘Family care*/caring’, ‘Unpaid care*/caring’, ‘Care for family members with –’, ‘Support of family members with’ (cf. Table 1).
Table 1:
Key words and search strings
| Key words | Search strings |
|---|---|
| Mental health |
|
| Family care |
|
Step 3: Study selection
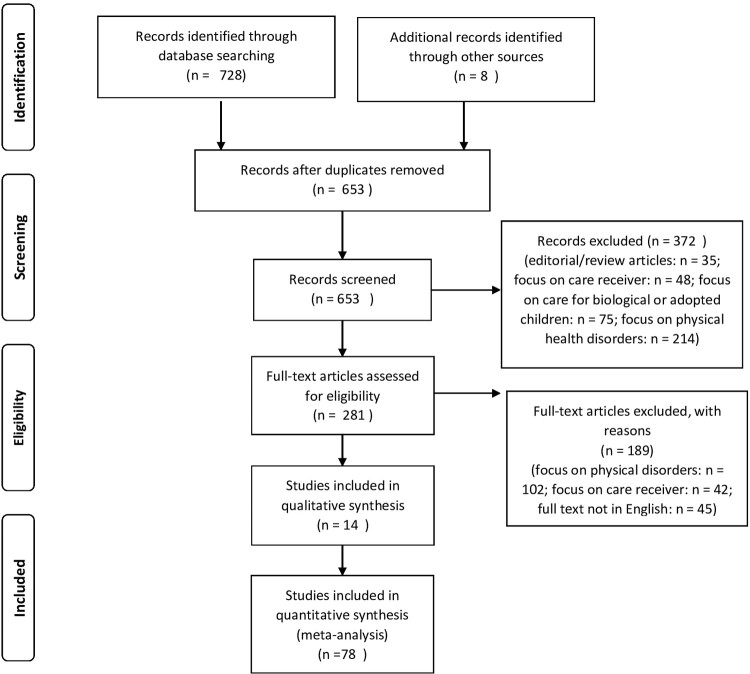
Decisions surrounding the inclusion and exclusion of studies in a scoping review rely upon an iterative and collaborative process involving all members of the researcher team (Levac et al., 2010). To address this we used the Preferred Reporting Items for Systematic Reviews flow diagram (cf. Figure 1; Moher et al., 2009). Databases were searched with a combination of search strings and Boolean operators to ensure the inclusion of at least one search string from the terms listed in Table 1. Both qualitative and quantitative studies were included. The exclusion criteria were the publication being an editorial or review article, studies with a primary focus on the care receiver and not the family carer, the patient being a child or adolescent (under 18 years of age) and studies about caring for physical health disorders. Editorial and review articles were examined to ensure the complete retrieval of relevant primary research noted therein.
Fig. 1:
PRISMA flow diagram (cf. Moher et al., 2009).
Step 4: Charting the data
In scoping reviews, charting the data involves reviewing, documenting and sorting the information that was retrieved in accordance with the key issues and themes (Arksey and O’Malley, 2005). An Excel spreadsheet was used to extract, document and organize the relevant information from each reviewed article (Levac et al., 2010). The spreadsheet included separate columns for article title, authors, database from which the article was drawn, the population and social-cultural background, mental illness of the patient whom family carers supported, methodological framework, instruments used in the study, method of analysis, main findings, implications and any additional information (e.g. screenshots of tables and figures).
Step 5: Collating, summarizing and reporting the results
The articles were read independently by members of the research team and topics relevant to the purpose of the review were identified. The research team compared, summarized and collated the identified preliminary themes. The data were then re-examined and reorganized to reflect deeper and more nuanced perspectives of the studies’ findings. Based on common meanings and central issues, the findings for each study were organized and integrated into categories and themes to highlight prevalent issues and gaps in knowledge. The research team commenced with collating, summarizing and reporting the results in April 2021 and concluded this step in August 2021.
RESULTS
Boolean searches including the string search terms generated a total output of 736 articles. From these 736 articles, 83 were excluded as they were duplicates. The research team examined the remaining 653 articles for inclusion/exclusion independently. Concordance in interrater reliability was high with the researcher team agreeing on inclusion and exclusion of 646 of the 653 articles (98.93%). Arguments for inclusion or exclusion of the remaining seven articles (1.07%) were discussed and consensus on inclusion/exclusion was reached before commencing with further analyses. The initial screening involved reading the abstracts and skimming the tests, which identified 281 articles that could potentially qualify for inclusion in the review. These 281 articles were read in detail. From the 231 articles, a total of 189 were excluded from further review, based on the exclusion criteria (cf. Table 1). Therefore, a total of 92 studies were included in the present review, of which 14 were qualitative and 78 were quantitative studies. Most studies focussed on American or British participants. Other countries represented were Australia, Canada, Chile, China, Colombia, Cyprus, Finland, Germany, Greece, India, Iran, Ireland, Italy, Japan, Malaysia, Malta, New Zealand, Norway, Portugal, Saudi Arabia, Spain and the Netherlands. Various mental health conditions were present in this review, the highest proportion being articles concerning family carers’ experiences with dementia (38 articles, 41.3%), followed by family carer’s experiences handling multiple and/or various mental health conditions (25 articles, 27.18%) and Alzheimer disease (13 articles, 14.13%). A smaller number of articles discussed family carers’ experiences with depression (3 articles, 3.26%), polytrauma in relation to traumatic brain injury (TBI; 3 articles, 3.26%), schizophrenia (2 articles, 2.17%), suicidal ideation (2 articles, 2.17%), post traumatic stress disorder (PTSD; 2 articles, 2.17%), psychosis (1 article, 1.09%), Parkinson disease psychosis (1 article, 1.09%), Postpartum psychiatric disorder (1 article, 1.09%) and bipolar disorder (1 article, 1.09%). An overview of the studies included in the review can be found in Table 2.
Table 2:
Table of articles and papers included in the analysis
| References | Participants | Disease | Method |
|---|---|---|---|
| Hahn, E. A., Boileau, N. R., Hanks, R. A., Sander, A. M., Miner, J. A. and Carlozzi, N. E. (2020). Health literacy, health outcomes, and the caregiver role in traumatic brain injury. Rehabilitation Psychology, 65, 401–408. https://doi-org.ezproxy.rgu.ac.uk/10.1037/rep0000330 | 131 family caregivers | TBI | Quantitative |
| Brickell, T. A., Lippa, S. M., French, L. M., Gartner, R. L., Driscoll, A. E., Wright, M. M. and Lange, R. T. (2019). Service needs and health outcomes among caregivers of service members and veterans following TBI. Rehabilitation Psychology, 64, 72–86. https://doi-org.ezproxy.rgu.ac.uk/10.1037/rep0000249 | 264 caregivers (95.8% female)—veterans/military | TBI | Quantitative |
| Griffin, J. M., Lee, M. K., Bangerter, L. R., Van Houtven, C. H., Friedemann-Sánchez, G., Phelan, S. M., Carlson, K. F. and Meis, L. A. (2017). Burden and mental health among caregivers of veterans with traumatic brain injury/polytrauma. American Journal of Orthopsychiatry, 87, 139–148. https://doi-org.ezproxy.rgu.ac.uk/10.1037/ort0000207 | 564 caregivers—veterans | TBI and Polytrauma | Quantitative |
| Mausbach, B. T., Chattillion, E. A., Ho, J., Flynn, L. M., Tiznado, D., von Känel, R., Patterson, T. L. and Grant, I. (2014). Why does placement of persons with Alzheimer’s disease into long-term care improve caregivers’ well-being? Examination of psychological mediators. Psychology and Aging, 29, 776–786. https://doi-org.ezproxy.rgu.ac.uk/10.1037/a0037626 | 126 spousal caregivers | Alzheimer | Longitudinal, Quantitative |
| Gonçalves-Pereira, M., Zarit, S. H., Cardoso, A. M., Alves da Silva, J., Papoila, A. L. and Mateos, R. (2020). A comparison of primary and secondary caregivers of persons with dementia. Psychology and Aging, 35, 20–27. https://doi-org.ezproxy.rgu.ac.uk/10.1037/pag0000380.supp (Supplemental) | 61 primary and 61 secondary family caregivers | Dementia | Quantitative |
| Meyer, O. L., Nguyen, K. H., Dao, T. N., Vu, P., Arean, P. and Hinton, L. (2015). The sociocultural context of caregiving experiences for Vietnamese dementia family caregivers. Asian American Journal of Psychology, 6, 263–272. https://doi-org.ezproxy.rgu.ac.uk/10.1037/aap0000024.supp (Supplemental) | 10 caregivers | Dementia | Qualitative |
| Otero, P., Torres, Á. J., Vázquez, F. L., Blanco, V., Ferraces, M. J. and Díaz, O. (2019). Does the disease of the person receiving care affect the emotional state of non-professional caregivers? Frontiers in Psychology, 10, 1144. | 491 caregivers | Multiple | Quantitative |
| Alzahrani, S. H., Fallata, E. O., Alabdulwahab, M. A., Alsafi, W. A. and Bashawri, J. (2017). Assessment of the burden on caregivers of patients with mental disorders in Jeddah, Saudi Arabia. BMC Psychiatry, 17, 1–8. | 377 caregivers | Mental health illnesses (various) | Quantitative |
| Chiang, C. Y., Lu, C. Y., Lin, Y. H., Lin, H. Y. and Sun, F. K. (2015). Caring stress, suicidal attitude and suicide care ability among family caregivers of suicidal individuals: a path analysis. Journal of Psychiatric and Mental Health Nursing, 22, 792–800. | 164 family caregivers | Suicidal ideation | Quantitative |
| Unwin, G. and Deb, S. (2011). Family caregiver uplift and burden: Associations with aggressive behavior in adults with intellectual disability. Journal of Mental Health Research in Intellectual Disabilities, 4, 186–205. | 44 family caregivers | Intellectual disability or aggressive behaviour | Quantitative |
| Choi, H. (2018). Giving or receiving spouse care and marital satisfaction among older Korean individuals. Social Science & Medicine. | 3424 spousal caregivers—not specified | Care—not specified | Quantitative |
| Casarez, R. L., Barlow, E., Iyengar, S. M., Soares, J. C. and Meyer, T. D. (2019). Understanding the role of m-Health to improve well-being in spouses of patients with bipolar disorder. Journal of Affective Disorders, 250, 391–396. | 13 spousal caregivers | Bipolar disorder | Qualitative |
| Greenwood, N., Pound, C., Brearley, S. and Smith, R. (2019). A qualitative study of older informal carers’ experiences and perceptions of their caring role. Maturitas, 124, 1–7. | 44 family carers aged 70–87 years | Dementia or other mental illness | Qualitative |
| Alasmee, N. and Hasan (2020). Primary caregivers experience of anti-psychotic medication: a qualitative study. Archives of Psychiatric Nursing, 34, 520–528. | 21 family caregivers | Schizophrenia | Qualitative |
| Colvez, A., Joel, M. E., Ponton-Sanchez, A. and Royer, A. C. (2002). Health status and work burden of Alzheimer patients’ informal caregivers: comparisons of five different care programs in the European Union. Health Policy, 60, 219–233. | 322 spousal caregivers | Alzheimer | Quantitative |
| Anchan, V. and Janardhana, N. (2020). Transformation of attitude through brief psychoeducation program for the husbands of women with postpartum psychiatric disorders. Asian Journal of Psychiatry, 51, 101841. | 21 husbands of women with postpartum psychiatric disorder | Postpartum psychiatric disorders | Quantitative |
| Lai, F. H. Y., Yan, E. W. H., Tsui, W. S. and Yu, K. K. Y. (2020). A randomized control trial of activity scheduling for caring for older adults with dementia and its impact on their spouse care-givers. Archives of Gerontology and Geriatrics, 90, 104167. | 100 spouses | Dementia | Quantitative |
| Van Wijngaarden, B., Koeter, M., Knapp, M., Tansella, M., Thornicroft, G., Vázquez-Barquero, J. L. et al. (2009). Caring for people with depression or with schizophrenia: are the consequences different? Psychiatry Research, 169(1), 62–69. | 252 family/friends/partner caregivers for outpatients with depression and 151 family/friends/partner caregivers for outpatients with schizophrenia | Multiple | Quantitative |
| Dahlrup, B., Ekström, H., Nordell, E. and Elmståhl, S. (2015). Coping as a caregiver: a question of strain and its consequences on life satisfaction and health-related quality of life. Archives of Gerontology and Geriatrics, 61, 261–270. | 369 family carers | Multiple | Quantitative |
| Jones, S. M., Woodward, M. and Mioshi, E. (2019). Social support and high resilient coping in carers of people with dementia. Geriatric Nursing, 40, 584–589. |
|
Dementia | Quantitative |
| Highet, N., Thompson, M. and McNair, B. (2005). Identifying depression in a family member: the carers’ experience. Journal of Affective Disorders, 87(1), 25–33. |
|
Clinical depression | Qualitative |
| Beeson, R. A. (2003). Loneliness and depression in spousal caregivers of those with Alzheimer’s disease versus non-caregiving spouses. Archives of Psychiatric Nursing, 17, 135–143. | 49 caregiving spouses and 52 non-caregiving control individuals | Alzheimer | Quantitative |
| Kabitsi, N. and Powers, D. V. (2002). Spousal motivations of care for demented older adults: a cross-cultural comparison of Greek and American female caregivers. Journal of Aging Studies, 16, 383–399. | 30 American women spousal carers, 44 Greek women spousal carers | Dementia | Quantitative |
| Mills, P. J., Ancoli-Israel, S., von Känel, R., Mausbach, B. T., Aschbacher, K., Patterson, T. L. et al. (2009). Effects of gender and dementia severity on Alzheimer’s disease caregivers’ sleep and biomarkers of coagulation and inflammation. Brain, Behavior, and Immunity, 23, 605–610. | 81 male and female spousal caregiver and 41 non-caregivers | Alzheimer | Quantitative |
| Teles, S., Ferreira, A. and Paúl, C. (2021). Access and retention of informal dementia caregivers in psychosocial interventions: a cross-sectional study. Archives of Gerontology and Geriatrics, 93, 104289. | 179 Portuguese caregivers—unspecified | Dementia | Quantitative |
| Morrison, V. and Williams, K. (2020). Gaining longitudinal accounts of carers’ experiences using IPA and photograph elicitation. Frontiers in Psychology, 11, 521382. | 3 women caregivers | Dementia, stroke and ftd | Qualitative |
| Zwar, L., König, H. H. and Hajek, A. (2020). Psychosocial consequences of transitioning into informal caregiving in male and female caregivers: findings from a population-based panel study. Social Science & Medicine, 264, 113281. | 13 333 informal carers—unspecified | Unspecified | Quantitative |
| Willis, P., Vickery, A. and Symonds, J. (2020). “You have got to get off your backside; otherwise, you’ll never get out”: older male carers’ experiences of loneliness and social isolation. International Journal of Care and Caring, 4, 311–330. | 25 men; British—five distinct sample groups, including: male carers; men who were single and living in urban or rural areas; men who identified as gay and were single or living alone; and men with hearing loss. | Various (including dementia, Alzheimer, physical disabilities) | Qualitative |
| Brites, R., Brandão, T., Moniz Pereira, F., Hipólito, J. and Nunes, O. (2020). Effects of supporting patients with dementia: a study with dyads. Perspectives in Psychiatric Care, 56, 614–620. | 36 informal caregivers and their 36 care receivers | Dementia | Quantitative |
| Mahomed, A. and Pretorius, C. (2020). Availability and utilization of support services for South African male caregivers of people with Alzheimer’s disease in low-income communities. Dementia, 20, 633–652. | 11 adult males who were familial caregivers | Alzheimer | Qualitative |
| Ruisoto, P., Contador, I., Fernandez-Calvo, B., Serra, L., Jenaro, C., Flores, N. et al. (2020). Mediating effect of social support on the relationship between resilience and burden in caregivers of people with dementia. Archives of Gerontology and Geriatrics, 86, 103952. | 283 primary and family caregivers in Spain | Dementia | Quantitative |
| Kamalzadeh, L., Salehi, M., Rashedi, V., Ahmadzad Asl, M., Malakouti, S. K., Seddigh, R. et al. (2020). Perceived burden of dementia care, clinical, psychological and demographic characteristics of patients and primary caregivers in Iran. Applied Neuropsychology Adult. | 60 family caregiver and care-recipient pairs | Dementia | Quantitative |
| Tranvåg, O., Nåden, D. and Gallagher, A. (2019). Dignity work of older women caring for a husband with dementia at home. Health Care for Women International, 40, 1047–1069. | 6 Norwegian women spousal carers | Dementia | Qualitative |
| Hvidsten, L., Engedal, K., Selbæk, G., Wyller, T. B., Benth, J.Š., Kersten, H. | 88 family carers—unspecified | Dementia | Quantitative |
| Avdikou, K., Stefanatos, C., Tsatali, M., Gouva, M. and Tsolaki, M. (2019). The role of gender in shame, hostility, and aggression experienced by caregivers for patients with dementia. American Journal of Alzheimer’s Disease & Other Dementias, 34, 231–235. | 55 family caregivers | Dementia | Quantitative |
| Care recipients’ low level of cognitive function was associated with greater perceived burden. Higher quality of support was associated with lower perceived burden among female and male spouse caregivers, daughter caregivers and mother | 20 207 respondents and 43 262 observations of 50+ carers | Unspecified | Quantitative |
| Mantri, S., Edison, B., Alzyoud, L., Marras, C., Chahine, L. M. | 145 partner caregivers | Parkinson disease psychosis (PDP) | Mixed-methods cross-sectional study |
| Juntunen, K., Salminen, A. L., Törmäkangas, T., Tillman, P., Leinonen, K. and Nikander, R. (2018). Perceived burden among spouse, adult child, and parent caregivers. Journal of Advanced Nursing, 74, 2340–2350. | 4000 family caregivers in Finland | Unspecified | Quantitative |
| Dam, A. E., Boots, L. M., Van Boxtel, M. P., Verhey, F. R. and De Vugt, M. E. (2018). A mismatch between supply and demand of social support in dementia care: a qualitative study on the perspectives of spousal caregivers and their social network members. International Psychogeriatrics, 30, 881–892. | 10 spousal caregivers of people with dementia and 17 network members | Dementia | Qualitative |
| Beks, T. A. and Cairns, S. L. (2018). Contexts precipitating help-seeking among partners of veterans with posttraumatic stress disorder: a qualitative exploration. Traumatology, 24, 313. | 16 Canadian female partners (English-speaking) of male veterans with PTSD | Veterans/PTSD | Qualitative |
| Rahmani, F., Ebrahimi, H., Seyedfatemi, N., Namdar Areshtanab, H., Ranjbar, F. and Whitehead, B. (2018). Trapped like a butterfly in a spider’s web: experiences of female spousal caregivers in the care of husbands with severe mental illness. Journal of Clinical Nursing, 27, 1507–1518. | 14 female spousal caregivers of people with severe mental illness | Mental health illnesses (various) | Qualitative |
| Pattanayak, R. D., Jena, R., Tripathi, M. and Khandelwal, S. K. (2010). Assessment of burden in caregivers of Alzheimer’s disease from India. Asian Journal of Psychiatry, 3, 112–116. | 32 patient–caregiver dyads India | Alzheimer’s disease | Quantitative |
| Gresswell, I., Lally, L., Adamis, D. and McCarthy, G. M. (2018). Widening the net: exploring social determinants of burden of informal carers. Irish Journal of Psychological Medicine, 35, 43–51. | 53 Irish family carers, unspecified | Dementia or other chronic illness | Quantitative |
| McAuliffe, L., Ong, B. and Kinsella, G. (2018). Mediators of burden and depression in dementia family caregivers: kinship differences. Dementia. | 134 family caregivers | Dementia | Quantitative |
| Stadtmann, M. P., Maercker, A., Binder, J. and Schnepp, W. (2018). Mastering life together-symptom management, views, and experiences of relatives of persons with CPTSD: a grounded theory study. Journal of Patient-Reported Outcomes, 2, 1–13. | 17 self-declared ‘relatives’ | Complex posttraumatic stress disorder | Qualitative |
| Viñas‐Diez, V., Turró‐Garriga, O., Portellano‐Ortiz, C., Gascón‐Bayarri, J., Reñé‐Ramírez, R., Garre‐Olmo, J. et al. (2017). Kinship and cohabitation in relation to caregiver burden in the context of Alzheimer's disease: a 24‐month longitudinal study. International Journal of Geriatric Psychiatry, 32, e72–e82. | 275 Alzheimer’s disease family primary caregivers | Alzheimer | Quantitative |
| Chow, E. O. W. and Ho, H. C. (2015). Caregiver strain, age, and psychological well-being of older spousal caregivers in Hong Kong. Journal of Social Work, 15, 479–497. | 112 spousal caregivers aged 55 and over in Hong Kong | Not specified | Quantitative |
| Tuomola, J., Soon, J., Fisher, P. and Yap, P. (2016). Lived experience of caregivers of persons with dementia and the impact on their sense of self: a qualitative study in Singapore. Journal of Cross-Cultural Gerontology, 31, 157–172. | 6 Chinese female spousal caregivers | Dementia | Qualitative |
| Mausbach, B. T., Chattillion, E. A., Ho, J., Flynn, L. M., Tiznado, D., von Känel, R. et al. (2014). Why does placement of persons with Alzheimer’s disease into long-term care improve caregivers’ well-being? Examination of psychological mediators. Psychology and Aging, 29(4), 776. | 126 spousal Alzheimer’s disease family caregivers | Alzheimer | Quantitative |
| Williams, K. L., Morrison, V. and Robinson, C. A. (2014). Exploring caregiving experiences: caregiver coping and making sense of illness. Aging & Mental Health, 18, 600–609. | 13 family caregivers | Stroke and dementia | Qualitative |
| Abu Bakar, S. H., Weatherley, R., Omar, N., Abdullah, F. and Mohamad Aun, N. S. (2014). Projecting social support needs of informal caregivers in Malaysia. Health & Social Care in the Community, 22, 144–154. | 175 family caregivers | Unspecified (chronically ill/disability) | Quantitative |
| Orpin, P., Stirling, C., Hetherington, S. and Robinson, A. (2014). Rural dementia carers: formal and informal sources of support. Ageing & Society, 34(2), 185–208. | 18 rural primary caregivers (unspecified) | Dementia | Qualitative |
| Gibbons, C., Creese, J., Tran, M., Brazil, K., Chambers, L., Weaver, B. and Bédard, M. (2014). The psychological and health consequences of caring for a spouse with dementia: a critical comparison of husbands and wives. Journal of Women & Aging, 26, 3–21. | 65 spouses (husbands/wives) caring for someone with Alzheimer’s disease | Dementia | quantitative |
| Daley, R. T., Sugarman, M. A., Shirk, S. D. and O’Connor, M. K. (2018). Spared emotional perception in patients with Alzheimer’s disease is associated with negative caregiver outcomes. Aging & Mental Health, 22(5), 595–602. | 28 spousal caregivers and 30 controls | Alzheimer’s | Quantitative |
| van Groenou, M. I. B., de Boer, A. and Iedema, J. (2013). Positive and negative evaluation of caregiving among three different types of informal care relationships. European Journal of Ageing, 10, 301–311. | 1685 Dutch family caregivers | Multiple | Quantitative |
| Alpass, F., Pond, R., Stephens, C., Stevenson, B., Keeling, S. and Towers, A. (2013). The influence of ethnicity and gender on caregiver health in older New Zealanders. Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 68, 783–793. | 2155 New Zealand family carers | Unspecified | Quantitative |
| Slachevsky, A., Budinich, M., Miranda-Castillo, C., Núñez-Huasaf, J., Silva, J. R., Muñoz-Neira, C. et al. (2013). The CUIDEME Study: determinants of burden in Chilean primary caregivers of patients with dementia. Journal of Alzheimer’s Disease, 35(2), 297–306. | 292 Chilean family caregivers | Dementia | Quantitative |
| Pöysti, M. M., Laakkonen, M. L., Strandberg, T., Savikko, N., Tilvis, R. S., Eloniemi-Sulkava, U. and Pitkälä, K. H. (2012). Gender differences in dementia spousal caregiving. International Journal of Alzheimer’s Disease, 2012, 162960. | 335 dyads of wife– husband caregivers | Dementia | Quantitative |
| Quinn, C., Clare, L. and Woods, R. T. (2012). What predicts whether caregivers of people with dementia find meaning in their role? International Journal of Geriatric Psychiatry, 27(11), 1195–1202. | 447 informal caregivers | Dementia | Quantitative |
| Lai, D. W. (2012). Effect of financial costs on caregiving burden of family caregivers of older adults. Sage Open, 2(4), 2158244012470467. | 448 informal caregivers | Unspecified | Quantitative |
| Tsai, C.-F., Hwang, W.-S., Lee, J.-J., Wang, W.-F., Huang, L.-C., Huang, L.-K. et al. (2021) Predictors of caregiver burden in aged caregivers of demented older patients. BMC Geriatrics, 21, 1–9. | 328 informal caregiver–patient dyads. | Dementia | Quantitative |
| Papastavrou, E., Charalambous, A., Tsangari, H. and Karayiannis, G. (2012). The burdensome and depressive experience of caring: what cancer, schizophrenia, and Alzheimer’s disease caregivers have in common. Cancer Nursing, 35, 187–194. | 410 family caregivers | Cancer, Schizophrenia, and Alzheimer | Quantitative |
| Clare, L., Nelis, S. M., Whitaker, C. J., Martyr, A., Markova, I. S., Roth, I. et al. (2012). Marital relationship quality in early-stage dementia: perspectives from people with dementia and their spouses. Alzheimer Disease & Associated Disorders, 26, 148–158. | 54 spousal caregivers and 54 control couples | Dementia | Quantitative |
| Shanley, C., Russell, C., Middleton, H. and Simpson-Young, V. (2011). Living through end-stage dementia: the experiences and expressed needs of family carers. Dementia, 10, 325–340. | 15 informal carers | End-stage dementia | Quantitative |
| Papastavrou, E., Tsangari, H., Karayiannis, G., Papacostas, S., Efstathiou, G. and Sourtzi, P. (2011). Caring and coping: the dementia caregivers. Aging & Mental Health, 15, 702–711. | 172 Greek family caregivers | Dementia | Quantitative |
| Innes, A., Abela, S. and Scerri, C. (2011). The organisation of dementia care by families in Malta: the experiences of family caregivers. Dementia, 10, 165–184. | 17 family caregivers from Malta | Dementia | Qualitative |
| Nordtug, B. and Holen, A. (2011). Similarities and differences in caring burden of home dwellers with partners suffering from chronic obstructive pulmonary disease or dementia. Home Health Care Management & Practice, 23, 93–101. | 206 Norwegian spousal carers | Chronic obstructive pulmonary disease (COPD) or dementia | Quantitative |
| Lai, D. W. and Thomson, C. (2011). The impact of perceived adequacy of social support on caregiving burden of family caregivers. Families in Society, 92, 99–106. | 340 Canadian family caregivers aged above 65 | Unspecified | Quantitative |
| Stanley, S., Balakrishnan, S. and Ilangovan, S. (2017). Psychological distress, perceived burden and quality of life in caregivers of persons with schizophrenia. Journal of Mental Health, 26, 134–141. | 75 primary family caregivers of persons with schizophrenia in India | Schizophrenia | Quantitative cross-sectional design and survey |
| Baker, K. L., Robertson, N. and Connelly, D. (2010). Men caring for wives or partners with dementia: masculinity, strain and gain. Aging & Mental Health, 14, 319–327. | 70 male caregivers | Dementia | Quantitative |
| Papastavrou, E., Tsangari, H., Kalokerinou, A., Papacostas, S. S. and Sourtzi, P. (2009). Gender issues in caring for demented relatives. Health Science Journal, 3, 41–53. | 172 Cyprus family primary caregivers | Dementia | Quantitative |
| Arango Lasprilla, J. C., Moreno, A., Rogers, H. and Francis, K. (2009). The effect of dementia patient’s physical, cognitive, and emotional/behavioral problems on caregiver well-being: findings from a Spanish-speaking sample from Colombia, South America. American Journal of Alzheimer's Disease & Other Dementias, 24, 384–395. | 73 Colombian family caregivers | Dementia | Quantitative |
| Sun, F., Lee Roff, L., Klemmack, D. and Burgio, L. D. (2008). The influences of gender and religiousness on Alzheimer disease caregivers’ use of informal support and formal services. Journal of Aging and Health, 20, 937–953. | 720 family caregivers | Alzheimer | Quantitative |
| Quinn, C., Clare, L., Pearce, A. and Van Dijkhuizen, M. (2008). The experience of providing care in the early stages of dementia: an interpretative phenomenological analysis. Aging and Mental Health, 12, 769–778. | 34 spouses or partners of people with a diagnosis of early-stage dementia | Early stages of dementia | Qualitative |
| Brown, J. and Chen, S. L. (2008). Help-seeking patterns of older spousal caregivers of older adults with dementia. Issues in Mental Health Nursing, 29, 839–852. | 20 spousal caregivers | Dementia | Qualitative |
| Dahlberg, L., Demack, S., and Bambra, C. (2007). Age and gender of informal carers: a population‐based study in the UK. Health & Social Care in the Community, 15, 439–445. | a 3% random sample of the 2001 UK Census. The sample size was 1 825 595. Of this sample, 10% were reported to be carers. | Unspecified | Quantitative |
| Ducharme, F., Lévesque, L., Zarit, S. H., Lachance, L. and Giroux, F. (2007). Changes in health outcomes among older husband caregivers: a one-year longitudinal study. The International Journal of Aging and Human Development, 65, 73–96. | 232 older husband caregivers | Unspecified | Quantitative, longitudinal |
| Calasanti, T. and Bowen, M. E. (2006). Spousal caregiving and crossing gender boundaries: maintaining gendered identities. Journal of Aging Studies, 20, 253–263. | 22 primary spousal caregivers | Alzheimer | Qualitative |
| Adams, K. B., Smyth, K. A. and McClendon, M. J. (2005). Psychosocial resources as moderators of the impact of spousal dementia caregiving on depression. Journal of Applied Gerontology, 24, 475–489. | 441 caregivers and 251 Non-caregivers | Alzheimer | Quantitative |
| Malhotra, C., Malhotra, R., Østbye, T., Matchar, D. and Chan, A. (2012). Depressive symptoms among informal caregivers of older adults: insights from the Singapore Survey on Informal Caregiving. International Psychogeriatrics, 24, 1335–1346. | 1190 dyads caregivers and receivers | Multiple | Quantitative |
| Gaugler, J. E., Anderson, K. A., Leach, C. R., Smith, C. D., Schmitt, F. A. and Mendiondo, M. (2004). The emotional ramifications of unmet need in dementia caregiving. American Journal of Alzheimer's Disease & Other Dementias, 19, 369–380. | 694 informal caregivers | Dementia | Quantitative |
| Beeson, R. A. (2003). Loneliness and depression in spousal caregivers of those with Alzheimer’s disease versus non-caregiving spouses. Archives of Psychiatric Nursing, 17, 135–143. | 49 Alzheimer spousal carers (AD) and 52 spousal non-caregivers | Alzheimer | Quantitative |
| Perry, J. (2002). Wives giving care to husbands with Alzheimer’s disease: a process of interpretive caring. Research in Nursing & Health, 25, 307–316. | 20 spousal carers (wives) | Alzheimer | Qualitative |
| Chow, E. O. W. and Ho, H. C. (2015). Caregiver strain, age, and psychological well-being of older spousal caregivers in Hong Kong. Journal of Social Work, 15, 479–497. | 112 spousal caregivers from Hong Kong | Not specified | Quantitative |
| Gonçalves-Pereira, M., Carmo, I., da Silva, J. A., Papoila, A. L., Mateos, R. and Zarit, S. H. (2010). Caregiving experiences and knowledge about dementia in Portuguese clinical outpatient settings. International Psychogeriatrics, 22, 270–280. | 99 primary caregivers | Dementia | Quantitative |
| Gresswell, I., Lally, L., Adamis, D. and McCarthy, G. M. (2018). Widening the net: exploring social determinants of burden of informal carers. Irish Journal of Psychological Medicine, 35, 43–51. | 53 carers Ireland | Not specified | Quantitative |
| Shikimoto, R., Sado, M., Ninomiya, A., Yoshimura, K., Ikeda, B., Baba, T. et al. (2018). Predictive factors associated with psychological distress of caregivers of people with dementia in Japan: a cross-sectional study. International Psychogeriatrics, 30, 1089–1098. | Japan, 1437 people with dementia-caregiver dyads | Dementia | Quantitative |
| Temple, J. B. and Dow, B. (2018). The unmet support needs of carers of older Australians: prevalence and mental health. International Psychogeriatrics, 30, 1849–1860. | 25 555 primary carers Australia | Multiple | Quantitative |
| Collins, C. and Jones, R. (1997). Emotional distress and morbidity in dementia carers: a matched comparison of husbands and wives. International Journal of Geriatric Psychiatry, 12, 1168–1173. | 48 UK spousal carers | Dementia | Quantitative |
| Luderowski, A. and Boden, Z. V. (2020). Love and incomprehensibility: the hermeneutic labour of caring for and understanding a loved one with psychosis. Health, 24, 737–754. | 10 UK informal carer for someone experiencing psychosis | Psychosis | Qualitative |
| Wayland, S., Coker, S. and Maple, M. (2021). The human approach to supportive interventions: the lived experience of people who care for others who suicide attempt. International Journal of Mental Health Nursing, 30, 667–682. | 758 family carers of someone who has attempted suicide | Suicide | Mixed |
| Vasileiou, K., Barnett, J., Barreto, M., Vines, J., Atkinson, M., Lawson, S. et al. (2017) Experiences of loneliness associated with being an informal caregiver: a qualitative investigation. Frontiers in Psychology, 8, 585. | 16 family caregivers | Mixed (dementia, frailty due to old age, multiple sclerosis, depression, autism) | Qualitative |
| Östman, M., Wallsten, T. and Kjellin, L. (2005). Family burden and relatives' participation in psychiatric care: are the patient’s diagnosis and the relation to the patient of importance? International Journal of Social Psychiatry, 51, 291–301. | 455 close relatives caregivers | Psychoses, affective disorders and ‘other diagnoses’ | Quantitative |
| McGaw, V. E., Reupert, A. E. and Maybery, D. (2020). Partners of veterans with PTSD: parenting and family experiences. Families in Society, 101, 456–468. | 8 female partner caregivers of Australian veterans | PTSD | Qualitative |
| Roth, D. L., Dilworth-Anderson, P., Huang, J., Gross, A. L. and Gitlin, L. N. (2015). Positive aspects of family caregiving for dementia: differential item functioning by race. Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 70, 813–819. | 642 family caregivers | Dementia | Quantitative |
| Brown, S. L., Smith, D. M., Schulz, R., Kabeto, M. U., Ubel, P. A., Poulin, M., et al. (2009). Caregiving behavior is associated with decreased mortality risk. Psychological Science, 20, 488–494. | 3376 family caregivers | Multiple | Quantitative |
| O’Reilly, D., Connolly, S., Rosato, M. and Patterson, C. (2008). Is caring associated with an increased risk of mortality? A longitudinal study. Social Science & Medicine, 67, 1282–1290. | Health of caregivers recorded in the 2001 Northern Ireland Census | Multiple | Quantitative |
| Roth, D. L., Perkins, M., Wadley, V. G., Temple, E. M. and Haley, W. E. (2009). Family caregiving and emotional strain: associations with quality of life in a large national sample of middle-aged and older adults. Quality of Life Research, 18, 679–688. | 43 099 family caregivers | Multiple | Quantitative |
| Dilworth-Anderson, P., Brummett, B. H., Goodwin, P., Williams, S. W., Williams, R. B. and Siegler, I. C. (2005). Effect of race on cultural justifications for caregiving. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 60, S257–S262. | 48 African American and 121 White caregivers. | Multiple | Quantitative |
| McCallum, T. J., Sorocco, K. H. and Fritsch, T. (2006). Mental health and diurnal salivary cortisol patterns among African American and European American female dementia family caregivers. The American Journal of Geriatric Psychiatry, 14, 684–693. | 30 African American and 24 European American female dementia family caregivers and 48 African American and 15 European American non-caregivers | Dementia | Quantitative |
As outlined in Table 3, the review identified three main themes: (i) Negative Implications of Caring for Family Members with Mental Health Diseases, (ii) Positive Implications of Caring for Family Members with Mental Health Diseases and (iii) Moderating Factors that can Contribute to the Family Carer’s Wellbeing. We now discuss these three themes in more detail.
Table 3:
Summary of themes and key results
| Theme: name | Theme: description | Theme: prevalence | Example: article |
|---|---|---|---|
| Negative Implications of Caring for Family Members with Mental Health Diseases | Studies that provide qualitative or quantitative evidence for adverse physical and/or psychological consequences of family caregiving are included in this theme. Examples for adverse physical and/or psychological consequences are e.g. depression, burden of care, muscular dystrophy, disc prolapses, increased mortality rates, etc. | 54.24% of articles described adverse physical and/or psychological consequences of family caregiving | Viñas‐Diez, V., Turró‐Garriga, O., Portellano‐Ortiz, C., Gascón‐Bayarri, J., Reñé‐Ramírez, R., Garre‐Olmo, J., et al. (2017). Kinship and cohabitation in relation to caregiver burden in the context of Alzheimer’s disease: a 24‐month longitudinal study. International Journal of Geriatric Psychiatry, 32, e72–e82. |
| Positive Implications of Caring for Family Members with Mental Health Diseases | Studies that provide qualitative or quantitative evidence for beneficial physical and/or psychological consequences of family caregiving are included in this theme. Examples for beneficial physical and/or psychological consequences are e.g. personal growth, maturity, increased resilience, reduced all-cause mortality rates, etc. | 17.39% of articles investigated positive and beneficial effects of family caregiving. | Quinn, C., Clare, L. and Woods, R. T. (2012). What predicts whether caregivers of people with dementia find meaning in their role? International Journal of Geriatric Psychiatry, 27, 1195–1202. |
| Moderating Factors that can Contribute to the Family Carer’s Wellbeing | Studies that examine factors that contribute to family caregivers’ wellbeing and family caregivers’ needs are included in this theme. Examples for unmet needs are physical, social and financial support. | A total of 47.82% examined how moderating factors contribute to family caregivers’ wellbeing. | Temple, J. B. and Dow, B. (2018). The unmet support needs of carers of older Australians: prevalence and mental health. International Psychogeriatrics, 30, 1849–1860. |
Negative implications of caring for family members with mental health diseases
A major theme was the negative impact on the family caregiver’s physical and mental health. Most of the articles included in this review examined clinical levels of psychological distress in family carers (33.7%; 31 studies) and depression and depressive symptoms in relation to family caregiving (21.17%, 20 studies). This indicates that providing primary care for family members can have problematic consequences on the carers’ wellbeing. For example, Mausbach et al.(Mausbach et al., 2014) conducted a longitudinal study comparing the individual experiences of 126 spousal carers for Alzheimer patients. The placement of the care receiver into care homes was associated with significant reductions in depressive symptoms, activity restriction and an increase in personal mastery in caregivers. These results are supported by studies that examined levels of psychological distress and depressive symptoms in primary and secondary caregivers across different mental health diseases and different cultures [i.e. (Colvez et al., 2002; Gonçalves-Pereira et al., 2020; Zwar et al., 2020)].
However, while primary care for family members can have negative consequences on carer wellbeing, sociodemographic factors can also determine the extent to which individuals may be affected by such negative consequences. For example, 32 (34.78%) of the reviewed studies indicated that gender significantly impacts on the care givers self-perceived burden of care. The results from these studies are consistent in suggesting that female family caregivers experience higher levels of psychological distress, shame and caregiver burden [i.e. (Pattanayak et al., 2010; Chiang et al., 2015; Gresswell et al., 2018; Avdikou et al., 2019; Brites et al., 2020)]. This trend was evident across different cultures and applied to various mental health disorders equally (Papastavrou et al., 2009; Nordtug and Holen, 2011; Pöysti et al., 2012). In addition, if wives cared for their husbands, they experienced lower marital satisfaction, while the opposite effect was observed in husbands caring for their wives (Beeson, 2003; Dahlberg et al., 2007; Lai, 2012; Choi, 2018). The literature around this phenomenon suggests that women feel more responsible for providing care and as a result are left with multiple competing roles (Calasanti and Bowen, 2006; Dahlberg et al., 2007). Women are therefore more likely to experience a loss of self and loneliness when caring for a family member making them more susceptible to caregiver depression, whereas men are more comfortable with letting others assume the carer role, and are more self-reliant on themselves and others to provide social support (Calasanti and Bowen, 2006; Brown and Chen, 2008; Sun et al., 2008; Ruisoto et al., 2020).
The role of the carer and their relationship with the care-receiver was also found to impact on individual wellbeing. Specifically, research suggests that close ties such as being a spouse and/or living together with a mentally ill person in an acute setting determines the caregiver’s experiences of burden of care. For example, in their quantitative study with 455 close relatives, found that burden was particularly high among spouses, as they feel more isolated and have less leisure time than other family carers. In addition, findings suggest that spouses who care for partners with mental health disorders are exposed to additional stressors that originate from an internal conflict of roles were they are perceived to ‘hold it all together’ in their relationship [(Casarez et al., 2019), p. 393]. In this sense, spouses need to handle challenging behaviours such as reckless spending or rageful and hypercritical behaviour, minimizing any issues that might arise during social encounters (Casarez et al., 2019). Besides the emotional burden, spousal carers may also experience financial difficulties as they often give up their work to care for their loved ones. This poses additional problems as financial uncertainty contributes to clinically significant levels of distress, caregiver burden and depression among family carers (Lai, 2012; Abu Bakar et al., 2014; Temple and Dow, 2018; Wayland et al., 2021). Therefore, spouses may be at risk of compromising their own wellbeing when delivering primary care, due to greater emotional and financial strain.
Another key determinant in the prediction of family carer’s wellbeing is age. Studies in this review suggest that challenging experiences in relation to family caring were perceived to be more difficult or worse for older carers (Chiang et al., 2015; Chow and Ho, 2015: Tsai et al., 2021). Essentially, elderly family carers may not understand mental health issues or have the stamina required to overcome the challenges of caring, for example accessing formal support (Chiang et al., 2015; Greenwood et al., 2019). In addition, their own health conditions can compromise the ability to perform physical tasks, and thus diminish their social circle. Potential sources of social support can also decrease with age, while their own health conditions can make it harder to leave their home, and engage in leisure activities or make new friends.
Positive implications of caring for family members with mental health diseases
While most literature examines the negative psychological and physical consequences of caregiving on the carer, there is an increasing emphasis on the positives that bring balance to this point of view. A total of 16 studies (17.39%) in this review investigated the full range of caregiving experiences, including potential positive aspects and benefits of caregiving. Essentially, caregiving can be a rewarding experience that facilitates personal growth, maturity and resilience (Netto et al., 2009; Sánchez-Izquierdo et al., 2015; Quinn et al., 2015) with population-based surveys indicating that caregiving may relate to significantly reduced all-cause mortality rates in comparison to a matched sample of non-caregivers (Brown et al., 2009; O’Reilly et al., 2008). Caregivers often report feeling gratitude and a sense of mastery, meaningfulness and coherence in their existence (Cohen et al., 2002; Quinn et al., 2012; Cheng et al., 2017). Therefore, the findings that suggest positive aspects of caregiving to be inversely related to burden and depression are unsurprising [i.e. (Hilgeman et al., 2007)].
Theoretical models offer different explanations to understand these positive changes in the caregiver’s life. For example, the adaption stress and coping model (Folkman, 1997), suggests that positive psychological states are associated with finding positive meaning in adversity, and helping the individual to make sense of the situation. This can result in the caregiver identifying positive changes in their life (Park, 2010). Fredrickson et al.(Fredrickson et al., 2003) take a similar approach in their broaden-and-build theory by suggesting that positive emotions contribute to cognitive broadening, which then widens the individual’s attention, thinking and behaviour. This broadening effect helps foster a range of adaptive and durable personal resources that contribute to the development of resilience (Fredrickson, 2004). Similarly, theories that are based on benefit-finding imply that adaptive coping emerges over time as a way of responding to stressful circumstances. This enables personal growth and fosters resilience.
In addition to situational and personal factors, literature indicates that adaptive coping also depends upon demographic characteristics. For example, caregiver personality characteristics such as extraversion and agreeableness along with social support (especially support from loved ones) are associated with positive aspects of caregiving (Koerner et al., 2009). Ethnicity can also impact on the experience of positive aspects in caregiving. Studies show that African Americans report more positive caregiving outcomes associated with active coping styles and greater resilience in comparison to Caucasians (Dilworth-Anderson et al., 2005; McCallum et al., 2006; Merritt et al., 2011). This is consistent with studies in which African American family caregivers were less affected by depression, caregiver burden and strain than white family caregivers (Haley et al., 2004). A study by Roth et al. (2015) also found that African American family carers felt more capable at appreciating and developing a positive attitude towards life when compared to Caucasians. This positive attitude towards care is explained as a reflection of long-standing traditions of the African American community. This attitude is cultivated in early life through racial socialization and maintained in adulthood life through spiritual and cultural beliefs, especially when facing adversities or overcoming hardships (McLoyd et al., 2005). Roff et al. (2004) outlined similar findings but added that religiosity partially mediates the relationship between ethnicity and the elevated positive attitudes in caregiving among African Americans. Although symptoms of depression were not associated with baseline levels of positive aspects in caregiving, Roff et al.(Roff et al., 2004) found that lower anxiety levels, less worrying and lower socioeconomic status among African American caregivers contributed to higher levels of positive aspects in caregiving. In conclusion, positive aspects of caregiving may be related to coping and having a more optimistic outlook on life.
Moderating factors that can contribute to the family carers’ wellbeing
A total of 44 studies (47.82%) suggest that tailored means of support are pivotal in improving family carers’ physical and mental wellbeing. Here, a particular focus is placed on examining the individual needs of the family caregiver and how these may be addressed (Temple and Dow, 2018). Findings from the review suggest that the most prevalent types of unmet needs include financial, physical and social support [i.e. (Highet et al., 2005; Temple and Dow, 2018; Brickell et al., 2019; Casarez et al., 2019; Jones et al., 2019; Alasmee and Hasan, 2020; Anchan and Janardhana, 2020; Brites et al., 2020; Lai et al., 2020; Teles et al., 2021)]. Temple and Dow’s (2018) findings indicate that having any unmet needs for support increased the likelihood of the carer experiencing psychological distress two-fold. With each successive unmet need for support, the odds of psychological distress increased another 1.37 times. Therefore, besides the previously discussed negative effect of financial burden (7 studies; 7.61%), maintaining social connections (17 studies; 18.48%) and receiving professional or social support (16 studies; 17.39%), unmet needs are key factors in understanding and addressing the carer’s physical and psychological wellbeing.
Increasing social resources was found to reduce the risk of suffering from poor mental health in family caregivers for patients with different mental illnesses (Gaugler et al., 2004; Griffin et al., 2017; Otero et al., 2019). This may be explained by feelings of social connectedness counteracting the effects of loneliness and social isolation that are associated with depression and depressive symptoms in family carers (Beeson, 2003; Vasileiou et al., 2017; McAuliffe et al., 2018). In this sense, empathy and social connections with family and friends as well as healthcare staff can provide a source of strength and a sense of mastery in one’s predicament (Shanley et al., 2011). Peer support groups may be particularly relevant in reducing the burden of care by providing the family carer with a feeling of social connectedness with individuals who share similar experiences (Shanley et al., 2011). In addition, peer support groups give family carers the space and opportunity to reflect on their own caring routine, helping them cope more effectively with the competing demands of care (Stanley et al., 2017).
In addition to peer support groups, research suggests that smartphone technologies (i.e. applications) can help improve and maintain family carers’ physical and mental health. For example, Casarez et al.(Casarez et al., 2019) report that using mental health (mHealth) apps leads to a reduction of carer burden and distress and an increase in social contacts. They not only improve the relationship between carer and care-receiver but help them to manage the administration of medication and contribute to mental health literacy. Specifically, mHealth apps can provide information for family carers on how to manage symptoms of mental health disorders, what to do in difficult situations, provide constructive practices and alert users to the need for professional interventions. This is important because information about mental health symptoms can foster an understanding of the care receivers’ experiences and reduce burden and distress in caregivers [i.e. (Vasileiou et al., 2017; Brickell et al., 2019; Casarez et al., 2019; Jones et al., 2019; Alasmee and Hasan, 2020; Anchan and Janardhana, 2020; Hahn et al., 2020; Lai et al., 2020; McGaw et al., 2020; Wayland et al., 2021)]. However, while mental health literacy is crucial in improving caregiver wellbeing, studies have found that in certain situations, carers are not interested in information about the mental health illness of the care receiver (Williams et al., 2014). Rather, Williams et al.(Williams et al., 2014) suggests that caregivers adopt active information-seeking techniques to not only deal with current problems and to increase their sense of control, but avoid considering future logistics of caregiving when they feel helpless or overwhelmed with stress. Thus, caregiving stressors affect the extent to which caregivers may adequately utilize the information and service provisions available. In conclusion, for them to be effective, resources must be tailored to the caregivers’ individual needs.
Importantly, cultural differences need to be taken into consideration when tailoring support [i.e. (Sun et al., 2008; Chow and Ho, 2015; Meyer et al., 2015; Tuomola et al., 2016; Mahomed and Pretorius, 2020; Kabitsi and Powers, 2002)]. This review suggests that cultural differences impact on patterns of help-seeking behaviour, access to sources of formal and informal support, the search for information about the mental illness and the motivation to provide family care (Kabitsi and Powers, 2002; Mahomed and Pretorius, 2020). For example, Mahomed and Pretorius (Mahomed and Pretorius, 2020) found that male South Africans in low-income communities utilize a collective approach towards caregiving, relying on wider informal social networks instead of institutional and formal care services. Similar results were evident in studies that compared motives for family caregiving in Greece and America (Kabitsi and Powers, 2002). This study found that Greek and American carers were motivated by different factors. Greek families understood themselves in a more relational and largely family-interwoven frame, while American family carers were more motivated by financial reasons to provide family care. It can therefore be concluded that cultural differences in caregiving motivations may result in adaptive or maladaptive outcomes for the caregiver and care receiver. Here, studies suggest that cultural and religious values often correlate and overlap with one another. Several studies outlined the importance of religion and spirituality in helping family caregivers to manage the stress of caregiving [i.e. (Meyer et al., 2015; Robinson-Lane et al., 2021)]. For example, Tuomola et al. (Tuomola et al., 2016), Chan (Chan, 2010) and Hinton et al. (Hinton et al., 2008) outlined how Confucian principles that highlight the importance of closeness between family members are reflected in family carers’ reasoning processes. By drawing on the collectivistic cultures of East Asia that espouse a set of values and beliefs which promote maintenance of harmony with individuals and with the environment, family carers could overcome obstacles and emotional difficulties. Similar results are supported in Meyer et al.’s (Meyer et al., 2015) examination of Christian family carers who relied on their faith to cope with challenging situations. Community support and doctrinal beliefs about God’s will helped caregivers to cope with distress and burden. In conclusion, the studies presented in this review suggest that it may be valuable to include an understanding of cultural values and an individual’s spirituality and religion as components of tailored means of support for family caregivers.
DISCUSSION AND CONCLUSION
This scoping review was conducted to understand the effects of caring for family members with mental health illnesses on caregivers’ wellbeing. The findings suggest that mental and physical wellbeing of family caregivers may depend upon a combination of situational and sociodemographic characteristics.
The review identified elderly, female and spousal primary-caregivers as a group who are at risk of experiencing mental and physical health. Primary caregivers, in comparison to secondary caregivers, suffer higher levels of distress, have less leisure time and smaller social circles. In addition, the findings indicate that there are gender differences that also need to be taken into consideration. The scoping review found that female spousal carers may view caring for their partner as their duty, try to be less dependent on support from others and take on multiple roles to fill the gaps that the mental illness of their partner has caused in comparison to their male counterparts, In doing so, female spousal carers may experience higher levels of distress and caregiver burden than male family caregivers. Spousal family caregivers often give up their work. This is linked to financial uncertainty and elevated levels of distress and depressive symptoms. In this sense, it is possible that some factors associated with caring for family members such as limited temporal resources may contribute to and trigger further stressors such as financial uncertainty. Similarly, elderly family caregivers tend to experience lower levels of wellbeing as they often do not have the stamina required for caring responsibilities, and experience diminishing social circles besides suffering from their own health issues. Therefore, the results suggest that for older caregivers, there are a range of underlying stressors that decrease the individual’s overall quality of life and life satisfaction while increasing the burden of care.
Nevertheless, caregiving can also be a rewarding experience that fosters meaning, resilience and personal growth in the caregiver. Therefore, the present results suggest that the negative effects of caregiving can be balanced by the individuals’ personality, social support, religiosity and culture. Specifically, high levels of agreeableness and extraversion in combination with social support relate to lower levels of caregiver stress and burden. Social resources were found to play a particularly important role because support from peers counteracts the loneliness and isolation that can lead to depression. In this sense, social resources combined with personality traits and social skills may be important in maintaining life satisfaction and quality of life. Also, positive attitudes towards life coupled with religious or spiritual beliefs helped improve the family caregivers’ wellbeing because spirituality and religiosity provide a framework through which caregiving experiences can be interpreted in meaningful ways. This supports the idea that the meaningful interpretation of one’s circumstances is an important skill that can help give family caregivers a positive outlook on their life and understand difficult circumstances through multiple perspectives.
However, despite the findings from this review, several limitations need to be taken into consideration. The present review did not examine demands, capabilities and meaning at the community level, nor did it consider the care receiver’s adaptation and adjustment to their mental illness. The scoping review did not seek to assess the studies included regarding their quality or effect sizes. We also acknowledge that the sample of articles is skewed towards the challenges and demands of family caregivers for dementia (38 articles, 41.3%) and Alzheimer patients (13 articles, 14.13%). While the scholarship reviewed suggests that there is little difference in caregiver experience between conditions, it may still be possible that other unique aspects of the caregiver experiences in relation to other mental health illnesses have not been covered. In this sense, the present review included caregivers of individuals with different pathologies but did not necessarily differentiate between their experiences. Future research may therefore wish to focus on the experiences of family caregivers looking after an individual with specific mental health conditions such as depression or schizophrenia. In addition, as the care receiver’s health can also influence the caregiver’s quality of life, only few studies in the review discussed the caregivers’ overall quality of life. This is problematic as it remains unclear whether the caregiver has lower self-rated quality of life besides scoring high on e.g. caregiver burden, and caregiver distress. This limitation can be addressed in future reviews focussing on examining and comparing specific measures such as self-rated quality of life. In addition, the scope of future reviews could include research that examines interventions intending to improve family caregivers’ wellbeing.
Despite these limitations, the present review achieved its research objective by providing an overview of how family caregiving affects the caregivers physical, mental and social wellbeing, and the best ways to support family carers. While caregiving can have a negative impact on the physical and mental wellbeing of the carer, specific sociodemographic, personal and situational factors can work as a buffer. Therefore, support for family caregivers must be tailored to individual needs, taking into consideration personality, particular circumstances, along with cultural and personal beliefs.
REFERENCES
- Abraham A., Sommerhalder K., Abel T. (2010) Landscape and well-being: a scoping study on the health-promoting impact of outdoor environments. International Journal of Public Health, 55, 59–69. [DOI] [PubMed] [Google Scholar]
- Abu Bakar S. H., Weatherley R., Omar N., Abdullah F., Mohamad Aun N. S. (2014) Projecting social support needs of informal caregivers in Malaysia. Health & Social Care in the Community, 22, 144–154. [DOI] [PubMed] [Google Scholar]
- Agenagnew L., Kassaw C. (2020) The lifetime prevalence and factors associated with relapse among mentally ill patients at Jimma University Medical Center, Ethiopia: cross sectional study. Journal of Psychosocial Rehabilitation and Mental Health, 7, 211–220. [Google Scholar]
- Akbari M., Alavi M., Irajpour A., Maghsoudi J. (2018) Challenges of family caregivers of patients with mental disorders in Iran: a narrative review. Iranian Journal of Nursing and Midwifery Research, 23, 329–337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alasmee N., Hasan A. A. (2020) Primary caregivers experience of anti-psychotic medication: a qualitative study. Archives of Psychiatric Nursing, 34, 520–528. [DOI] [PubMed] [Google Scholar]
- Ali S., Rhodes L., Moreea O., McMillan D., Gilbody S., Leach C.. et al. (2017) How durable is the effect of low intensity CBT for depression and anxiety? Remission and relapse in a longitudinal cohort study. Behaviour Research and Therapy, 94, 1–8. [DOI] [PubMed] [Google Scholar]
- Amagai M., Takahashi M., Amagai F., (2016) Qualitative study of resilience of family caregivers for patients with schizophrenia in Japan. Age (Years), 63, 55–74. [Google Scholar]
- Anchan V., Janardhana N. (2020) Transformation of attitude through brief psychoeducation program for the husbands of women with postpartum psychiatric disorders. Asian Journal of Psychiatry, 51, 101841. [DOI] [PubMed] [Google Scholar]
- Arksey H., O’Malley L. (2005) Scoping studies: towards a methodological framework. International Journal of Social Research Methodology, 8, 19–32. [Google Scholar]
- Avdikou K., Stefanatos C., Tsatali M., Gouva M., Tsolaki M. (2019) The role of gender in shame, hostility, and aggression experienced by caregivers for patients with dementia. American Journal of Alzheimer’s Disease & Other Dementias, 34, 231–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beeson R. A. (2003) Loneliness and depression in spousal caregivers of those with Alzheimer’s disease versus non-caregiving spouses. Archives of Psychiatric Nursing, 17, 135–143. [DOI] [PubMed] [Google Scholar]
- Brickell T. A., Lippa S. M., French L. M., Gartner R. L., Driscoll A. E., Wright M. M.. et al. (2019) Service needs and health outcomes among caregivers of service members and veterans following TBI. Rehabilitation Psychology, 64, 72–86. [DOI] [PubMed] [Google Scholar]
- Brites R., Brandão T., Moniz Pereira F., Hipólito J., Nunes O. (2020) Effects of supporting patients with dementia: a study with dyads. Perspectives in Psychiatric Care, 56, 614–620. [DOI] [PubMed] [Google Scholar]
- Brown J., Chen S. L. (2008) Help-seeking patterns of older spousal caregivers of older adults with dementia. Issues in Mental Health Nursing, 29, 839–852. [DOI] [PubMed] [Google Scholar]
- Brown S. L., Smith D. M., Schulz R., Kabeto M. U., Ubel P. A., Poulin M.. et al. (2009) Caregiving behavior is associated with decreased mortality risk. Psychological Science, 20, 488–494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruffaerts R., Demyttenaere K., Kessler R. C., Tachimori H., Bunting B., Hu C.. et al. (2015) The associations between preexisting mental disorders and subsequent onset of chronic headaches: a worldwide epidemiologic perspective. The Journal of Pain, 16, 42–52. [DOI] [PubMed] [Google Scholar]
- Calasanti T., Bowen M. E. (2006) Spousal caregiving and crossing gender boundaries: maintaining gendered identities. Journal of Aging Studies, 20, 253–263. [Google Scholar]
- Casarez R. L., Barlow E., Iyengar S. M., Soares J. C., Meyer T. D. (2019) Understanding the role of m-Health to improve well-being in spouses of patients with bipolar disorder. Journal of Affective Disorders, 250, 391–396. [DOI] [PubMed] [Google Scholar]
- Chan S. W. C. (2010) Family caregiving in dementia: the Asian perspective of a global problem. Dementia and Geriatric Cognitive Disorders, 30, 469–478. [DOI] [PubMed] [Google Scholar]
- Chang Y. C., Chou F. H. C. (2015) Effects of home visit intervention on re-hospitalization rates in psychiatric patients. Community Mental Health Journal, 51, 598–605. [DOI] [PubMed] [Google Scholar]
- Cheng S. T., Mak E. P., Fung H. H., Kwok T., Lee D. T., Lam L. C. (2017) Benefit-finding and effect on caregiver depression: a double-blind randomized controlled trial. Journal of Consulting and Clinical Psychology, 85, 521–529. [DOI] [PubMed] [Google Scholar]
- Chiang C. Y., Lu C. Y., Lin Y. H., Lin H. Y., Sun F. K. (2015) Caring stress, suicidal attitude and suicide care ability among family caregivers of suicidal individuals: a path analysis. Journal of Psychiatric and Mental Health Nursing, 22, 792–800. [DOI] [PubMed] [Google Scholar]
- Choi H. (2018) Giving or receiving spouse care and marital satisfaction among older Korean individuals. Social Science & Medicine. [DOI] [PubMed] [Google Scholar]
- Chow E. O. W., Ho H. C. (2015) Caregiver strain, age, and psychological well-being of older spousal caregivers in Hong Kong. Journal of Social Work, 15, 479–497. [Google Scholar]
- Cohen C. A., Colantonio A., Vernich L. (2002) Positive aspects of caregiving: rounding out the caregiver experience. International Journal of Geriatric Psychiatry, 17, 184–188. [DOI] [PubMed] [Google Scholar]
- Colvez A., Joel M. E., Ponton-Sanchez A., Royer A. C. (2002) Health status and work burden of Alzheimer patients’ informal caregivers: comparisons of five different care programs in the European Union. Health Policy (Amsterdam, Netherlands), 60, 219–233. [DOI] [PubMed] [Google Scholar]
- Crellin N. E., Orrell M., McDermott O., Charlesworth G. (2014) Self-efficacy and health-related quality of life in family carers of people with dementia: a systematic review. Aging & Mental Health, 18, 954–969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dadalto E. V., Cavalcante F. G. (2021) The place of family caregivers for older adults with Alzheimer’s disease: a literature review in Brazil and the United States. Ciência & Saúde Coletiva, 26, 147–157. [DOI] [PubMed] [Google Scholar]
- Dahlberg L., Demack S., Bambra C. (2007) Age and gender of informal carers: a population‐based study in the UK. Health & Social Care in the Community, 15, 439–445. [DOI] [PubMed] [Google Scholar]
- Dilworth-Anderson P., Brummett B. H., Goodwin P., Williams S. W., Williams R. B., Siegler I. C. (2005) Effect of race on cultural justifications for caregiving. The Journals of Gerontology: Series B, 60, S257–S262. [DOI] [PubMed] [Google Scholar]
- Donnellan W. J., Bennett K. M., Soulsby L. K. (2015) What are the factors that facilitate or hinder resilience in older spousal dementia carers? A qualitative study. Aging & Mental Health, 19, 932–939. [DOI] [PubMed] [Google Scholar]
- Fernando S. (2014) Mental Health Worldwide: Culture, Globalization and Development. Springer, London. [Google Scholar]
- Folkman S. (1997) Positive psychological states and coping with severe stress. Social Science & Medicine (1982), 45, 1207–1221. [DOI] [PubMed] [Google Scholar]
- Fredrickson B. L. (2004) The broaden-and-build theory of positive emotions. Philosophical Transactions of the Royal Society of London. Series B, Biological Sciences, 359, 1367–1378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredrickson B. L., Tugade M. M., Waugh C. E., Larkin G. R. (2003) What good are positive emotions in crises? A prospective study of resilience and emotions following the terrorist attacks on the United States on September 11th, 2001. Journal of Personality and Social Psychology, 84, 365–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaugler J. E., Anderson K. A., Leach C. R., Smith C. D., Schmitt F. A., Mendiondo M. (2004) The emotional ramifications of unmet need in dementia caregiving. American Journal of Alzheimer's Disease & Other Dementias, 19, 369–380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibbons C., Creese J., Tran M., Brazil K., Chambers L., Weaver B.. et al. (2014) The psychological and health consequences of caring for a spouse with dementia: a critical comparison of husbands and wives. Journal of Women & Aging, 26, 3–21. [DOI] [PubMed] [Google Scholar]
- Gonçalves-Pereira M., Zarit S. H., Cardoso A. M., Alves da Silva J., Papoila A. L., Mateos R. (2020) A comparison of primary and secondary caregivers of persons with dementia. Psychology and Aging, 35, 20–27. [DOI] [PubMed] [Google Scholar]
- Greenwood N., Pound C., Brearley S., Smith R. (2019) A qualitative study of older informal carers’ experiences and perceptions of their caring role. Maturitas, 124, 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gresswell I., Lally L., Adamis D., McCarthy G. M. (2018) Widening the net: exploring social determinants of burden of informal carers. Irish Journal of Psychological Medicine, 35, 43–51. [DOI] [PubMed] [Google Scholar]
- Griffin J. M., Lee M. K., Bangerter L. R., Van Houtven C. H., Friedemann-Sánchez G., Phelan S. M.. et al. (2017) Burden and mental health among caregivers of veterans with traumatic brain injury/polytrauma. The American Journal of Orthopsychiatry, 87, 139–148. [DOI] [PubMed] [Google Scholar]
- Grover S., Nehra R., Malhotra R., Kate N. (2017) Positive aspects of caregiving experience among caregivers of patients with dementia. East Asian Archives of Psychiatry, 27, 7178. [PubMed] [Google Scholar]
- Hahn E. A., Boileau N. R., Hanks R. A., Sander A. M., Miner J. A., Carlozzi N. E. (2020) Health literacy, health outcomes, and the caregiver role in traumatic brain injury. Rehabilitation Psychology, 65, 401–408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halas G., Schultz A. S., Rothney J., Goertzen L., Wener P., Katz A. (2015) A scoping review protocol to map the research foci trends in tobacco control over the last decade. BMJ Open, 5, e006643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haley W. E., Gitlin L. N., Wisniewski S. R., Mahoney D. F., Coon D. W., Winter L.. et al. (2004) Well-being, appraisal, and coping in African-American and Caucasian dementia caregivers: findings from the REACH study. Aging & Mental Health, 8, 316–329. [DOI] [PubMed] [Google Scholar]
- Hanna F., Barbui C., Dua T., Lora A., van Regteren Altena M., Saxena S. (2018) Global mental health: how are we doing? World Psychiatry, 17, 367–368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Highet N., Thompson M., McNair B. (2005) Identifying depression in a family member: the carers’ experience. Journal of Affective Disorders, 87, 25–33. [DOI] [PubMed] [Google Scholar]
- Hilgeman M. M., Allen R. S., DeCoster J., Burgio L. D. (2007) Positive aspects of caregiving as a moderator of treatment outcome over 12 months. Psychology and Aging, 22, 361–371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinton L., Tran J. N., Tran C., Hinton D. (2008) Religious and spiritual dimensions of the Vietnamese dementia caregiving experience. Hallym International Journal of Aging: HIJA, 10, 139–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsiao C.-Y., Lu H.-L., Tsai Y.-F. (2020) Caregiver burden and health-related quality of life among primary family caregivers of individuals with schizophrenia: cross-sectional study. Quality of Life Research, 29, 2745–2757. [DOI] [PubMed] [Google Scholar]
- Jones S. M., Woodward M., Mioshi E. (2019) Social support and high resilient coping in carers of people with dementia. Geriatric Nursing, 40, 584–589. [DOI] [PubMed] [Google Scholar]
- Kabitsi N., Powers D. V. (2002) Spousal motivations of care for demented older adults: a cross-cultural comparison of Greek and American female caregivers. Journal of Aging Studies, 16, 383–399. [Google Scholar]
- Kate N., Grover S., Kulhara P., Nehra R. (2013) Caregiving appraisal in schizophrenia: a study from India. Social Science & Medicine (1982), 98, 135–140. [DOI] [PubMed] [Google Scholar]
- Koerner S. S., Kenyon D. B., Shirai Y. (2009) Caregiving for elder relatives: which caregivers experience personal benefits/gains? Archives of Gerontology and Geriatrics, 48, 238–245. [DOI] [PubMed] [Google Scholar]
- Lai D. W. (2012) Effect of financial costs on caregiving burden of family caregivers of older adults. Sage Open, 2, 215824401247046. [Google Scholar]
- Lai F. H. Y., Yan E. W. H., Tsui W. S., Yu K. K. Y. (2020) A randomized control trial of activity scheduling for caring for older adults with dementia and its impact on their spouse care-givers. Archives of Gerontology and Geriatrics, 90, 104167. [DOI] [PubMed] [Google Scholar]
- Lamont E., Dickens G. L. (2021) Mental health services, care provision, and professional support for people diagnosed with borderline personality disorder: systematic review of service-user, family, and carer perspectives. Journal of Mental Health (Abingdon, England), 30, 619–633. [DOI] [PubMed] [Google Scholar]
- Levac D., Colquhoun H., O’Brien K. K. (2010) Scoping studies: advancing the methodology. Implementation Science, 5, 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahomed A., Pretorius C. (2020) Availability and utilization of support services for South African male caregivers of people with Alzheimer’s disease in low-income communities. Dementia, 20, 633–652. [DOI] [PubMed] [Google Scholar]
- Malins S., Biswas S., Patel S., Levene J., Moghaddam N., Morriss R. (2020) Preventing relapse with personalized smart‐messaging after cognitive behavioural therapy: a proof‐of‐concept evaluation. British Journal of Clinical Psychology, 59, 241–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mausbach B. T., Chattillion E. A., Ho J., Flynn L. M., Tiznado D., von Känel R.. et al. (2014) Why does placement of persons with Alzheimer’s disease into long-term care improve caregivers’ well-being? Examination of psychological mediators. Psychology and Aging, 29, 776–786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McAuliffe L., Ong B., Kinsella G. (2018) Mediators of burden and depression in dementia family caregivers: kinship differences. Dementia. [DOI] [PubMed]
- McCallum T. J., Sorocco K. H., Fritsch T. (2006) Mental health and diurnal salivary cortisol patterns among African American and European American female dementia family caregivers. The American Journal of Geriatric Psychiatry, 14, 684–693. [DOI] [PubMed] [Google Scholar]
- McGaw V. E., Reupert A. E., Maybery D. (2020) Partners of veterans with PTSD: parenting and family experiences. Families in Society: The Journal of Contemporary Social Services, 101, 456–468. [Google Scholar]
- McKee R. G. (2020) Exploring Experiences of Family Caregivers: The Relationship between Caregivers Perceived Burden and the Disability of the Care Receiver. Southern Connecticut State University, New Haven, US. [Google Scholar]
- McLoyd V. C., Hill N. E., Dodge K. A. (eds) (2005) African American Family Life: Ecological and Cultural Diversity. Guilford, New York, NY. [Google Scholar]
- Melemis S. M. (2015) Focus: addiction: relapse prevention and the five rules of recovery. The Yale Journal of Biology and Medicine, 88, 325–332. [PMC free article] [PubMed] [Google Scholar]
- Merritt M. M., McCallum T. J., Fritsch T. (2011) How much striving is too much? John Henryism active coping predicts worse daily cortisol responses for African American but not white female dementia family caregivers. The American Journal of Geriatric Psychiatry, 19, 451–460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer O. L., Nguyen K. H., Dao T. N., Vu P., Arean P., Hinton L. (2015) The sociocultural context of caregiving experiences for Vietnamese dementia family caregivers. Asian American Journal of Psychology, 6, 263–272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moges S., Belete T., Mekonen T., Menberu M. (2021) Lifetime relapse and its associated factors among people with schizophrenia spectrum disorders who are on follow up at Comprehensive Specialized Hospitals in Amhara region, Ethiopia: a cross-sectional study. International Journal of Mental Health Systems, 15, 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D., Liberati A. A., Tetzlaff J., Altman D. G.;. PRISMA Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ (Clinical Research ed.), 339, b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Netto N., Jenny G. Y. N., Philip Y. L. K.. (2009) Growing and gaining through caring for a loved one with dementia. Dementia, 8, 245–261. [Google Scholar]
- Nordtug B., Holen A. (2011) Similarities and differences in caring burden of home dwellers with partners suffering from chronic obstructive pulmonary disease or dementia. Home Health Care Management & Practice, 23, 93–101. [Google Scholar]
- Norris D., Eichler M., Cramm H., Tam‐Seto L., Smith‐Evans K. (2018) Operational stress injuries and the mental health and well‐being of veteran spouses: a scoping review. Journal of Family Theory & Review, 10, 657–671. [Google Scholar]
- O’Brien K. K., Colquhoun H., Levac D., Baxter L., Tricco A. C., Straus S.. et al. (2016) Advancing scoping study methodology: a web-based survey and consultation of perceptions on terminology, definition and methodological steps. BMC Health Services Research, 16, 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Flaherty J., Phillips C. (2015) The use of flipped classrooms in higher education: a scoping review. The Internet and Higher Education, 25, 85–95. [Google Scholar]
- O’Reilly D., Connolly S., Rosato M., Patterson C. (2008) Is caring associated with an increased risk of mortality? A longitudinal study. Social Science & Medicine, 67, 1282–1290. [DOI] [PubMed] [Google Scholar]
- Ong H. L., Vaingankar J. A., Abdin E., Sambasivam R., Fauziana R., Tan M. E.. et al. (2018) Resilience and burden in caregivers of older adults: moderating and mediating effects of perceived social support. BMC Psychiatry, 18, 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Østergaard T., Lundgren T., Zettle R. D., Landrø N. I., Haaland V. Ø. (2020) Psychological flexibility in depression relapse prevention: processes of change and positive mental health in group-based ACT for residual symptoms. Frontiers in Psychology, 11, 528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Otero P., Torres Á. J., Vázquez F. L., Blanco V., Ferraces M. J., Díaz O. (2019) Does the disease of the person receiving care affect the emotional state of non-professional caregivers? Frontiers in Psychology, 10, 1144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Özgönül M. L., Bademli K. (2022) Ethical problems experienced by family caregivers of patient with schizophrenia: a hermeneutic phenomenological study. Perspectives in Psychiatric Care. [DOI] [PubMed] [Google Scholar]
- Papastavrou E., Tsangari H., Kalokerinou A., Papacostas S. S., Sourtzi P. (2009) Gender issues in caring for demented relatives. Health Science Journal, 3, 41–53. [Google Scholar]
- Park C. L. (2010) Making sense of the meaning literature: an integrative review of meaning making and its effects on adjustment to stressful life events. Psychological Bulletin, 136, 257–301. [DOI] [PubMed] [Google Scholar]
- Pattanayak R. D., Jena R., Tripathi M., Khandelwal S. K. (2010) Assessment of burden in caregivers of Alzheimer’s disease from India. Asian Journal of Psychiatry, 3, 112–116. [DOI] [PubMed] [Google Scholar]
- Pione R. D., Spector A., Cartwright A. V., Stoner C. R. (2021) A psychometric appraisal of positive psychology outcome measures in use with carers of people living with dementia: a systematic review. International Psychogeriatrics, 33, 385–320. [DOI] [PubMed] [Google Scholar]
- Polanczyk G. V., Salum G. A., Sugaya L. S., Caye A., Rohde L. A. (2015) Annual research review: a meta‐analysis of the worldwide prevalence of mental disorders in children and adolescents. Journal of Child Psychology and Psychiatry, and Allied Disciplines 56, 345–365. [DOI] [PubMed] [Google Scholar]
- Post D., Agteren J., Kasai D., Barrett A., Doyle M., Kernot J.. et al. (2021) Caring for carers: understanding the physical and psychological well‐being of carers of veterans in Australia. Health & Social Care in the Community, 30, e793–e803. [DOI] [PubMed] [Google Scholar]
- Pöysti M. M., Laakkonen M. L., Strandberg T., Savikko N., Tilvis R. S., Eloniemi-Sulkava U.. et al. (2012) Gender differences in dementia spousal caregiving. International Journal of Alzheimer’s Disease, 2012, 162960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quinn C., Clare L., Woods R. T. (2012) What predicts whether caregivers of people with dementia find meaning in their role? International Journal of Geriatric Psychiatry, 27, 1195–1202. [DOI] [PubMed] [Google Scholar]
- Quinn C., Clare L., Woods R. T. (2015) Balancing needs: the role of motivations, meanings and relationship dynamics in the experience of informal caregivers of people with dementia. Dementia (London, England), 14, 220–237. [DOI] [PubMed] [Google Scholar]
- Robinson-Lane S. G., Zhang X., Patel A. (2021) Coping and adaptation to dementia family caregiving: a pilot study. Geriatric Nursing, 42, 256–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roff L. L., Burgio L. D., Gitlin L., Nichols L., Chaplin W., Hardin J. M. (2004) Positive aspects of Alzheimer’s caregiving: the role of race. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 59, P185–P190. [DOI] [PubMed] [Google Scholar]
- Roth D. L., Dilworth-Anderson P., Huang J., Gross A. L., Gitlin L. N. (2015) Positive aspects of family caregiving for dementia: differential item functioning by race. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 70, 813–819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roth D. L., Perkins M., Wadley V. G., Temple E. M., Haley W. E. (2009) Family caregiving and emotional strain: associations with quality of life in a large national sample of middle-aged and older adults. Quality of Life Research, 18, 679–688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruisoto P., Contador I., Fernández-Calvo B., Serra L., Jenaro C., Flores N.. et al. (2020) Mediating effect of social support on the relationship between resilience and burden in caregivers of people with dementia. Archives of Gerontology and Geriatrics, 86, 103952. [DOI] [PubMed] [Google Scholar]
- Sadock B., Sadock V. A., Sussman N. (2017) Kaplan & Sadock’s Pocket Handbook of Psychiatric Drug Treatment. Lippincott Williams & Wilkins, Philadelphia, US. [Google Scholar]
- Sánchez-Izquierdo M., Prieto-Ursúa M., Caperos J. M. (2015) Positive aspects of family caregiving of dependent elderly. Educational Gerontology, 41, 745–756. [Google Scholar]
- Shanley C., Russell C., Middleton H., Simpson-Young V. (2011) Living through end-stage dementia: the experiences and expressed needs of family carers. Dementia, 10, 325–340. [Google Scholar]
- Sharma N., Chakrabarti S., Grover S. (2016) Gender differences in caregiving among family-caregivers of people with mental illnesses. World Journal of Psychiatry, 6, 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiraishi N., Reilly J. (2019) Positive and negative impacts of schizophrenia on family caregivers: a systematic review and qualitative meta-summary. Social Psychiatry and Psychiatric Epidemiology, 54, 277–290. [DOI] [PubMed] [Google Scholar]
- Stanley S., Balakrishnan S., Ilangovan S. (2017) Psychological distress, perceived burden and quality of life in caregivers of persons with schizophrenia. Journal of Mental Health (Abingdon, England), 26, 134–141. [DOI] [PubMed] [Google Scholar]
- Sun F., Lee Roff L., Klemmack D., Burgio L. D. (2008) The influences of gender and religiousness on Alzheimer disease caregivers’ use of informal support and formal services. Journal of Aging and Health, 20, 937–953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teles S., Ferreira A., Paúl C. (2021) Access and retention of informal dementia caregivers in psychosocial interventions: a cross-sectional study. Archives of Gerontology and Geriatrics, 93, 104289. [DOI] [PubMed] [Google Scholar]
- Temple J. B., Dow B. (2018) The unmet support needs of carers of older Australians: prevalence and mental health. International Psychogeriatrics, 30, 1849–1860. [DOI] [PubMed] [Google Scholar]
- Tsai C.-F., Hwang W.-S., Lee J.-J., Wang W.-F., Huang L.-C., Huang L.-K.. et al. (2021) Predictors of caregiver burden in aged caregivers of demented older patients. BMC Geriatrics, 21, 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tuomola J., Soon J., Fisher P., Yap P. (2016) Lived experience of caregivers of persons with dementia and the impact on their sense of self: a qualitative study in Singapore. Journal of Cross-Cultural Gerontology, 31, 157–172. [DOI] [PubMed] [Google Scholar]
- van der Sanden R. L., Bos A. E., Stutterheim S. E., Pryor J. B., Kok G. (2013) Experiences of stigma by association among family members of people with mental illness. Rehabilitation Psychology, 58, 73–80. [DOI] [PubMed] [Google Scholar]
- Van Der Sanden R. L., Bos A. E., Stutterheim S. E., Pryor J. B., Kok G. (2015) Stigma by association among family members of people with a mental illness: a qualitative analysis. Journal of Community & Applied Social Psychology, 25, 400–417. [Google Scholar]
- Vasileiou K., Barnett J., Barreto M., Vines J., Atkinson M., Lawson S.. et al. (2017) Experiences of loneliness associated with being an informal caregiver: a qualitative investigation. Frontiers in Psychology, 8, 585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh K., Grech C., Hill K. (2019) Health advice and education given to overweight patients by primary care doctors and nurses: a scoping literature review. Preventive Medicine Reports, 14, 100812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wayland S., Coker S., Maple M. (2021) The human approach to supportive interventions: the lived experience of people who care for others who suicide attempt. International Journal of Mental Health Nursing, 30, 667–682. [DOI] [PubMed] [Google Scholar]
- WHO (2017) Mental Health Atlas.https://apps.who.int/iris/bitstream/handle/10665/272735/9789241514019-eng.pdf?ua=1 (last accessed 19 March 2022).
- Williams K. L., Morrison V., Robinson C. A. (2014) Exploring caregiving experiences: caregiver coping and making sense of illness. Aging & Mental Health, 18, 600–609. [DOI] [PubMed] [Google Scholar]
- Yin Y., Zhang W., Hu Z., Jia F., Li Y., Xu H.. et al. (2014) Experiences of stigma and discrimination among caregivers of persons with schizophrenia in China: a field survey. PLoS One, 9, e108527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zwar L., König H. H., Hajek A. (2020) Psychosocial consequences of transitioning into informal caregiving in male and female caregivers: findings from a population-based panel study. Social Science & Medicine, 264, 113281. [DOI] [PubMed] [Google Scholar]