Abstract
Although neurocognitive deficits have been documented in adolescents with suicidal ideation (SI) and suicide attempts (SA), it is unclear whether certain impairments differentiate these groups, potentially suggesting heightened risk for SA. Focus on specific facets of impulsivity and cognitive control may indicate distinctions between adolescents with SA vs. SI. The current study examined dimensions of impulsivity and cognitive control in 141 adolescents with SA (n=41) vs. SI without SA (n=49) vs. typically-developing controls (TDCs; n=51). Adolescents completed cross-sectional neurocognitive tasks via the Cambridge Neuropsychological Testing Automated Battery, in addition to demographic and clinical measures. Analyses involved ANOVAs and ANCOVAs. Results indicated that adolescents with SA demonstrated less set shifting/cognitive flexibility (reduced ability to adapt to/disengage from stimuli) and greater impulsive decision making (reduced ability to collect/evaluate information before making decisions) compared to TDCs. In addition, both TDCs and adolescents with SA had greater response inhibition (increased ability to stop motor responses that have begun/become prepotent) than those with SI. Similar results were found when analyzing female adolescents separately. There were no significant differences for male adolescents, potentially due to the small subsample (n=40). There were no significant findings for spatial planning/problem solving or visuospatial working memory. Findings suggest: 1) less set shifting/cognitive flexibility and greater impulsive decision making for adolescents with SA vs. TDCs; and 2) greater response inhibition for TDCs and adolescents with SA vs. SI. Such information may be useful for improving risk assessments (adding neurocognitive tasks) and targeted treatments (incorporating cognitive remediation) for this impaired population.
Keywords: adolescents, suicide attempt, suicidal ideation, cognitive flexibility, impulsive decision making, response inhibition
Introduction
Suicide is the second leading cause of death among youth ages 10–24 years old, and suicide rates have increased nearly 50% over the past decade among this age group (Centers for Disease Control and Prevention, 2021a, 2021b). In addition, 7% of high school students report having made a suicide attempt (SA) in the past year (Kann et al., 2018) and prior SA is among the strongest predictors of future SA and death by suicide (Bridge et al., 2006).
Despite mounting concerns and ongoing research, suicide risk assessments lack specificity and sensitivity (Franklin et al., 2017). Though several sociodemographic and clinical risk factors have been identified, these have proven to be weak and inconsistent predictors of suicidality and their predictive ability has not improved over the past 50+ years (Franklin et al., 2017). Of utmost importance is differentiating risk factors for suicidal ideation (SI) vs. SA (Klonsky & May, 2014). Indeed, only one-third of those with SI go on to make a SA (Nock et al., 2013). Furthermore, many of the risk factors for suicidality, such as depression and hopelessness, do not differentiate those with SI vs. SA (May & Klonsky, 2016). Another concern is that suicide risk assessments largely utilize self-report methods (e.g., questionnaires, clinical interviews), which are subject to self-preservation biases (e.g., minimizing suicidality to avoid hospitalization) (Stewart et al., 2017). Thus, it is essential to study and identify novel and objective risk factors differentiating SI vs. SA in youth, which can inform both assessment and intervention efforts.
Neurocognitive testing may offer an innovative and objective method of detecting adolescents vulnerable to SA. Indeed, examination of neurocognitive deficits has been the focus of recent empirical work in the adult suicide literature, which is in line with the NIMH’s Research Domain Criteria (RDoC) approach to suicidality (Glenn et al., 2017). However, few studies have specifically focused on neurocognitive deficits in adolescents with SA, thereby underscoring the need for additional research (Stewart et al., 2019). Two neurocognitive constructs particularly relevant to adolescent SA both conceptually and empirically, and thus warrant future examination, include impulsivity (Liu et al., 2017) and cognitive control (Stewart et al., 2019).
Impulsivity, broadly defined as impaired self-control, is a multi-faceted construct that includes behaviors and responses that are not deliberately planned and thus may result in unwanted or negative outcomes (Chamberlain & Sahakian, 2007; Hamilton, Littlefield, et al., 2015; Hamilton, Mitchell, et al., 2015). Specifically, impulsivity is thought to involve several processes, including: 1) reduced ability to collect and evaluate information before reaching decisions (i.e., impulsive decision making); and 2) reduced ability to stop motor responses that have already begun or become prepotent (i.e., response inhibition). In the context of SA, adolescents with greater impulsive decision making may demonstrate impairments in their ability to brainstorm and evaluate different options for tolerating distress, and instead quickly opt for SA. Adolescents with less response inhibition may have difficulty refraining from suicidal acts amid high levels of distress and stopping these behaviors once they have started. Thus, greater impulsive decision making and less response inhibition may be particularly problematic for suicidal adolescents, and such deficits have been found in empirical work comparing adolescents with SA vs. non-suicidal self-injury (Dougherty et al., 2009; Ruch et al., 2020; Zelazny et al., 2019), SA vs. psychiatric comparisons (Ackerman et al., 2015; Bridge et al., 2012), and in a recent meta-analysis (Liu et al., 2017).
The second neurocognitive construct of interest, cognitive control, refers to an individual’s ability to adapt their thoughts, attention, and/or behavior to changing environmental circumstances to achieve goals (Gläscher et al., 2012; Stewart et al., 2019). Several specific facets of cognitive control include set shifting/cognitive flexibility, sustained attention, spatial planning/problem solving, and working memory. These abilities are essential to critical thinking and future planning, and if impaired in suicidal adolescents, may contribute to difficulties coping with distress other than through suicide. According to the cognitive model of suicide (Wenzel & Beck, 2008) and other escape theories of suicide (Baumeister, 1990; Linehan, 1993), when negative life events generate emotional distress in the context of poor cognitive control, such individuals may become preoccupied with suicide as their only escape or option. In addition, they may be unable to execute effective coping strategies, leading to further distress and eventual SA.
Importantly, ideation-to-action frameworks have suggested that the predictors and correlates of SI are distinct from SA (Klonsky et al., 2018), and cognitive control has been found to differentiate adolescents with SA vs. SI, particularly when emotional- and suicide-related stimuli are used (Stewart et al., 2017). Regarding specific facets of cognitive control, studies evaluating sustained attention and/or spatial planning/problem solving have demonstrated mixed findings (Horesh, 2001; Ruch et al., 2020; Sommerfeldt et al., 2016; Stewart et al., 2015; Zelazny et al., 2019). However, in studies with null findings, some found deficits were associated with SA among adolescents with histories of maltreatment (Stewart et al., 2015; Zelazny et al., 2019), suggesting there may be meaningful subgroup differences. In addition, male adolescents with SA have been found to demonstrate impaired spatial working memory (Ruch et al., 2020). Thus, current studies indicate deficits across domains of cognitive control among adolescents with SA.
Set shifting/cognitive flexibility, defined as the behavioral adaptation to changing rewards and punishments, is another domain of cognitive control potentially relevant to suicidal adolescents (Gläscher et al., 2012). However, this has rarely been examined in suicidal youth, with one study reporting null findings (Ruch et al., 2020). Set shifting/cognitive flexibility may be crucial for suicidal individuals, representing the ability to disengage from emotionally evocative or suicide-relevant stimuli to more effective coping strategies. Though, studies examining the association between set shifting/cognitive flexibility and suicide often focus on omnibus variables, like total errors and/or trials required to complete a task. This approach has the potential to miss interesting intricacies of multi-stage tasks. For instance, the first time participants are required to adapt to changing rewards/punishments in the context of a task may be particularly meaningful because it highlights raw/true set shifting/cognitive flexibility deficits before any learning/adaptation occurs in subsequent, similar stages of a task. Indeed, deficits during initial stages of reversal tasks have been associated with set shifting/cognitive flexibility impairments in pediatric bipolar disorder (Dickstein et al., 2016; Dickstein et al., 2007; Dickstein et al., 2004; Wegbreit et al., 2016) and worsening trajectory of SI (MacPherson et al., 2021). However, the relevance of initial stages of reversal tasks to adolescents with SI and SA has not been examined.
To address these gaps in the literature, the current study investigated neurocognitive functioning, including facets of impulsivity (response inhibition and impulsive decision making) and cognitive control (set shifting/cognitive flexibility, spatial planning/problem solving, visuospatial working memory), in three groups of adolescents: 1) those with SA; 2) those with SI without SA; and 3) typically-developing controls (TDCs). We hypothesized that adolescents with SA would display greater impulsivity and less cognitive control than those with SI and TDCs, and those with SI would display greater impulsivity and less cognitive control than TDCs only. Based on research highlighting differences in neurocognitive deficits among suicidal female adolescents vs. male adolescents (i.e., cognitive control and affective bias impairments in suicidal female adolescents; spatial working memory impairments in suicidal male adolescents) (Ruch et al., 2020), exploratory post-hoc analyses were conducted, stratified by sex.
Method
Participants
Participants (N=141) were adolescents ages 12–19, including TDCs (n=51) and those with a psychiatric history (n=90). Adolescents with a psychiatric history were recruited from an inpatient unit or partial hospitalization program in a psychiatric hospital in the Northeastern United States. For this study, youth were divided into two groups: those with a history of SA (n=49) and those with SI but without a history of SA (n=41). These youth participated in either an RCT, whose primary clinical results have been previously reported (Esposito-Smythers et al., 2019), or an assessment study. TDCs were recruited from the community as part of a different study.
Inclusion criteria for participants with a psychiatric history were: 1) English fluency; 2) hospitalized for SI or SA; and 3) completed neurocognitive tasks at baseline as part of the main study. Exclusion criteria were: 1) cognitive or developmental delays; 2) autism spectrum disorder; 3) a primary diagnosis of a psychotic disorder, obsessive-compulsive disorder, or an eating disorder; 4) used “hard” illicit substances, such as opiates; and 5) full-scale intelligent quotient (FSIQ) < 70 on the Wechsler Abbreviated Scale of Intelligence (WASI) (Wechsler, 1999).
Inclusion criteria for TDCs were: 1) English fluency; and 2) no current/lifetime psychiatric illness or substance abuse/dependence in participants or first-degree relatives. Exclusion criteria were: 1) FSIQ < 70 on the WASI (Wechsler, 1999); and 2) medical/neurological conditions potentially mimicking/confounding psychiatric illness.
Procedures
All study procedures were approved by the Institutional Review Boards of Lifespan Corporation and Brown University. Participants with a psychiatric history were identified through clinical team referrals or electronic health record review and invited to participate in the study if they met the inclusion and exclusion criteria. TDCs were recruited via community outreach efforts (e.g., advertising at primary care offices, local schools, and shops). After written informed consent and assent, parents and adolescents completed a baseline assessment consisting of clinical interviews and questionnaires. Adolescents also completed a battery of cross-sectional neurocognitive tasks. Longitudinal data from the RCT were not included in the current study, and aforementioned interviews, questionnaires, and tasks were completed prior to randomization to treatment condition.
Measures
Neurocognitive tasks measuring domains of cognitive control.
Tasks from the Cambridge Neuropsychological Testing Automated Battery (CANTAB, 2021) were administered.
Set shifting/cognitive flexibility.
Participants’ set shifting/cognitive flexibility was assessed using the Intra-Dimensional/Extra-Dimensional Shift Task (ID/ED) (CANTAB, 2021), which is modeled after the Wisconsin Card Sorting Task. This task has nine stages. Depending on the stage, each trial displays two simple shapes or two compound shapes with overlaid white lines. Participants use feedback during trial-and-error learning to determine which of two stimuli is rewarded (earning points) and move onto the next stage after completing six consecutive correct trials (maximum 50 attempts). During reversal stages (stages 2, 5, 7, 9) the stimulus/reward association switches, such that the previously rewarded stimulus becomes punished, and vice versa. Based on prior research examining the association between cognitive flexibility deficits and suicidality using the ID/ED or similar tasks (Gifuni et al., 2020; MacPherson et al., 2021; Ruch et al., 2020), variables of interest included: 1) ID/ED total errors and trials; and 2) simple reversal stage 2 total errors and trials. The simple reversal stage 2 was of particular interest, as this represents the first time participants are required to adapt to the reversal of the prior stage 1 stimulus/reward relationship.
Spatial planning/problem solving.
Participants’ spatial planning/problem solving ability was assessed with the Stockings of Cambridge Task (SOC) (CANTAB, 2021). The task displays two arrangements of three colored balls, and participants must move the balls in the bottom set to match the top set. Each trial requires two to five moves. If participants make double the necessary moves, the trial terminates. The task ends after three consecutive terminations. Performance was assessed via total moves, number of problems solved with minimum moves, thinking time before starting each problem, and thinking time after starting. In this study, a single score for each variable was created by summing across problems (weighting by number of each type).
Visuospatial working memory.
Participants’ visuospatial working memory was assessed with the Spatial Span Task (SSP) (CANTAB, 2021). Participants watch nine squares displayed on a screen sequentially change colors and then are asked to touch the squares in the order in which they changed color. The number of squares increases from two to nine across trials. If participants are unsuccessful on their first try on a level, they receive two more attempts. After three failed attempts on a level, the task terminates. Outcome measures in this study included span length, total errors, and usage errors.
Neurocognitive tasks measuring domains of impulsivity.
Tasks from the Cambridge Neuropsychological Testing Automated Battery (CANTAB, 2021) were administered.
Response inhibition.
Participants’ response inhibition was assessed via the Stop Signal Task (SST) (CANTAB, 2021). Participants are instructed to push the button on the right side of the push pad when the arrow points to the right and the left button when the arrow points to the left. They are told to stop pressing either button when they hear a tone. After a practice trial, the task persists for 16 trials. Data is collected on stop signal response time, number of correct directional pushes, and number of successful stops. Outcome measures in this study included directional errors, proportion of successful stops, median correct reaction time on Go trials, and stop signal reaction time.
Impulsive decision making.
Participants’ impulsive decision making was assessed via the Information Sampling Task (IST) (CANTAB, 2021). On each trial, participants are presented with a 5 × 5 matrix of grey boxes on the computer screen, and two larger colored panels at the bottom of the screen. The participant can win points by making a correct decision about which color is in the majority under the gray boxes. Touching a grey box would immediately open that box to reveal one of the two colors displayed at the bottom of the screen. Participants can open boxes at their own rate with no time limit before deciding between one of the two colors, indicating their decision by touching one of the two panels at the bottom of the screen. At this point, the remaining boxes are uncovered, and a message is displayed to inform the participant whether or not they were correct. In the ‘fixed win’ condition, participants are awarded 100 points for a correct decision regardless of the number of boxes opened. In the ‘decreasing win’ condition, the participant loses 10 points for every box opened. In both conditions, they lose 100 points for an incorrect decision. The task starts with a single practice trial, followed by ten trials in each of the two conditions. The primary outcome measures were the average number of boxes opened and the probability (P) of the participant being correct at the point of decision in each condition.
Demographic and Clinical Measures.
Demographic information and psychiatric diagnoses were assessed in the entire sample. SI and SA were assessed in those with a psychiatric history (n=90), which included those recruited from an inpatient unit or partial hospitalization program.
Demographic information.
Participants reported on their age, sex, race, and ethnicity. Adolescents were administered the WASI (Wechsler, 1999) by research assistants to measure FSIQ.
Psychiatric diagnoses.
The Kiddie Schedule for Affective Disorders and Schizophrenia-Present Version (K-SADS-P) (Kaufman et al., 1997), a semi-structured diagnostic interview based on DSM-IV criteria, was used to assess adolescents’ psychiatric and substance use diagnoses. Interviews were conducted by trained masters’ level clinicians, postdoctoral fellows, and licensed clinical psychologists and psychiatrists with established inter-rater reliability (κ>.85).
Suicidal ideation and suicide attempts.
The Columbia-Suicide Severity Rating Scale (C-SSRS), a semi-structured interview, was used to assess SI and history of SA (Posner et al., 2011). The C-SSRS defines any self-injurious act with at least some intent/desire to die as a SA, and has demonstrated good reliability with adolescent psychiatric samples (κ=.88). Aborted and interrupted attempts were not included in the SA group. Research assistants who underwent extensive training by a licensed clinical psychologist (3–4 months) administered the C-SSRS to adolescents. Interviews were reviewed by a licensed clinical psychologist. A third rater was added for disagreements.
Analytic Strategy
Analyses were implemented in SPSS 25 with two-tailed comparisons. Descriptive statistics were calculated to characterize the sample. Specifically, a series of one-way analysis of variance (ANOVAs) and chi-square tests were used to compare SA vs. SI vs. TDCs on demographic variables. For psychiatric diagnoses (comparing SA vs. SI groups only), chi-square tests were used.
Our analytic strategy attempted to balance potential for Type I and Type II errors in this unique dataset examining neurocognitive performance in adolescents with SA vs. SI. vs. TDCs. As such, primary analyses involved a series of 19 one-way analysis of covariance (ANCOVAs) for different variables measuring: 1) set shifting/cognitive flexibility via the ID/ED (simple reversal stage 2 trials, simple reversal stage 2 errors, total trials, total errors); 2) spatial planning/problem solving via the SOC (total moves, problems solved in minimum moves, total initial thinking time, total subsequent thinking time); 3) visuospatial working memory on the SSP (length, errors, usage errors); 4) response inhibition on the SST (directional errors, proportion of successful stops, median reaction time on Go trials, stop signal reaction time); and 5) impulsive decision making on the IST (average number of boxes opened—win condition fixed, probability of being correct—win condition fixed, average number of boxes opened—win condition decreasing, probability of being correct—win condition decreasing). These were followed by Bonferroni-corrected post-hoc tests of pairwise comparisons within each ANCOVA, and Cohen’s d effect sizes for significant values. The Bonferroni correction for post-hoc pairwise comparisons was calculated in SPSS by multiplying each observed (uncorrected) p-value by the number of comparisons conducted. Covariates in ANCOVAs for primary analyses included demographic characteristics that significantly differed across groups (i.e., sex). Covariates in ANCOVAs for supplemental analyses included additional demographic features (i.e., sex, age, FSIQ).
In line with recent research demonstrating differences in suicidal female adolescents vs. male adolescents on neurocognitive variables (Ruch et al., 2020), and based on demographic characteristics found to differ between groups in the current study, exploratory post-hoc analyses involved one-way ANOVAs (followed by Bonferroni-corrected post-hoc tests for pairwise comparisons and Cohen’s d effect sizes for significant values) to compare SA vs. SI vs. TDCs on neurocognitive variables, stratified by sex.
Results
Sample Composition
Adolescents in this study were 15.31 (SD=1.51) years old on average. The majority of the sample was female (82%) and White (77%), with one-fifth (20%) identifying as Latinx. The mean FSIQ fell within the average range (M=104.30±11.71). There were no significant differences in age, race, ethnicity, and FSIQ across groups of SA vs. SI vs. TDCs, though there was a significant sex difference (Table 1). Bonferroni-corrected post-hoc chi-square tests revealed that the proportion of female adolescents to male adolescents was significantly higher in those with SA vs. TDCs [χ2(1)=7.88, p=.015, V=0.28].
Table 1.
Between-Group Demographic Characteristics in Participants with a History of a Suicide Attempt vs. Suicidal Ideation without a Suicide Attempt vs. Typically-Developing Controls
| Demographic Variables | History of Suicide Attempt (n=49) | Suicidal Ideation without a Suicide Attempt (n=41) | Typically-Developing Controls (n=51) | Statistic F/χ2 | p | / Cramer’s V |
|---|---|---|---|---|---|---|
| Age, M(SD) | 15.28(1.54) | 15.24(1.59) | 15.39(1.45) | F(2,138)=0.13 | .883 | =0.00 |
| Sex | χ2(2)= 7.96 | .019 | V=0.24 | |||
| Female, n(%) | 42(86%) | 28(68%) | 31(61%) | |||
| Male, n(%) | 7(14%) | 13(32%) | 20(39%) | |||
| Race | χ2(2)= 2.12 | .347 | V=0.13 | |||
| White, n(%) | 38(83%) | 33(89%) | 37(77%) | |||
| Black or African American, n(%) | 1(2%) | 2(5%) | 5(10%) | |||
| Multiracial, n(%) | 5(11%) | 2(5%) | 4(8%) | |||
| Asian, n(%) | 1(2%) | 0(0%) | 1(2%) | |||
| Native Hawaiian or Pacific Islander, n(%) | 1(2%) | 0(0%) | 0(0%) | |||
| Other, n(%) | 0(0%) | 0(0%) | 1(2%) | |||
| Ethnicity | χ2(2)= 2.79 | .248 | V=0.15 | |||
| Hispanic or Latino, n(%) | 13(28%) | 6(16%) | 6(15%) | |||
| Not Hispanic or Latino, n(%) | 34(72%) | 31(84%) | 35(85%) | |||
| Full-Scale IQ, M(SD) | 106.36(10.35) | 100.60(12.80) | 105.31(11.55) | F(2,135)=3.00 | .053 | =0.04 |
Note. The chi-square test for Race compared White versus Minority status.
The most common psychiatric diagnoses in those with SA and SI were major depressive disorder (78%), generalized anxiety disorder (41%), social anxiety disorder (22%), oppositional defiant disorder (22%), and attention-deficit/hyperactivity disorder (18%). There were no significant differences in diagnostic categories across SA and SI groups (Table 2). In addition, 82% (n=32) of those with SI and 81% (n=39) of those with SA were diagnosed with any depressive disorder (including major depressive disorder, dysthymia, and depressive disorder not otherwise specified), with no significant difference between groups [χ2(1)=0.01, p=.924, V=0.07].
Table 2.
Psychiatric Diagnoses among Participants with a History of a Suicide Attempt vs. Suicidal Ideation without a Suicide Attempt
| K-SADS-P DSM-IV Diagnoses | History of Suicide Attempt (n=49) | Suicidal Ideation without a Suicide Attempt (n=41) | Statistic χ2(1) | p | Cramer’s V |
|---|---|---|---|---|---|
|
|
|
||||
| n(%) | n(%) | ||||
| Mood Disorders | 40(83%) | 32(82%) | 0.03 | .875 | 0.02 |
| Major Depressive Disorder | 38(79%) | 30(77%) | |||
| Dysthymia | 1(2%) | 2(5%) | |||
| Depressive Disorder NOS | 2(4%) | 2(5%) | |||
| Bipolar I Disorder | 0(0%) | 1(3%) | |||
| Bipolar II Disorder | 1(2%) | 0(0%) | |||
| Bipolar Disorder NOS | 0(0%) | 1(3%) | |||
| Anxiety Disorders | 32(67%) | 19(49%) | 2.86 | .091 | 0.18 |
| Generalized Anxiety Disorder | 24(50%) | 12(31%) | |||
| Social Anxiety Disorder | 13(27%) | 6(15%) | |||
| Panic Disorder without Agoraphobia | 9(19%) | 5(13%) | |||
| Agoraphobia | 4(8%) | 3(8%) | |||
| Obsessive-Compulsive Disorder | 2(4%) | 1(3%) | |||
| Specific Phobia | 3(6%) | 4(10%) | |||
| Post-Traumatic Stress Disorder | 7(15%) | 6(15%) | 0.01 | .917 | 0.01 |
| Disruptive Behavior Disorders | 17(35%) | 15(39%) | 0.09 | .770 | 0.03 |
| ADHD | 9(19%) | 7(18%) | |||
| Oppositional Defiant Disorder | 9(19%) | 10(26%) | |||
| Conduct Disorder | 3(6%) | 0(0%) | |||
| Substance Abuse/Dependence | 6(13%) | 5(13%) | 0.002 | .964 | 0.01 |
| Alcohol Abuse | 2(4%) | 1(3%) | |||
| Alcohol Dependence | 1(2%) | 0(0%) | |||
| Substance Abuse | 5(10%) | 4(10%) | |||
| Substance Dependence | 3(6%) | 2(5%) | |||
| Eating Disorders | 1(2%) | 1(3%) | 0.02 | .882 | 0.02 |
| Anorexia | 0(0%) | 1(3%) | |||
| Bulimia | 1(2%) | 0(0%) |
Note. K-SADS-P=Kiddie Schedule for Affective Disorders and Schizophrenia-Present Version; DSM-IV=Diagnostic and Statistical Manual of Mental Disorders, 4th Edition; NOS=Not Otherwise Specified; ADHD=Attention/Deficit-Hyperactivity Disorder.
Between-Group Differences on CANTAB Neurocognitive Tasks
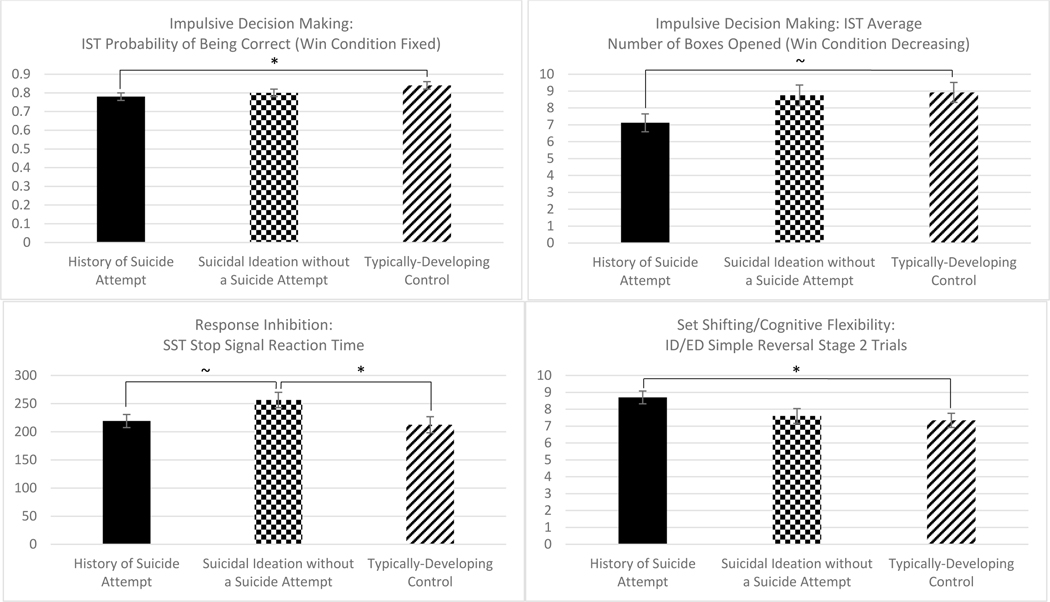
Primary analyses involved one-way ANCOVAs with the entire sample, including a covariate for sex, given a significant between-group difference on this demographic variable. On CANTAB neurocognitive tasks, there were significant between-group effects for: 1) set shifting/cognitive flexibility on the ID/ED simple reversal stage 2 trials [F(2,137)=3.50, p=.033, =0.05]; 2) response inhibition on the SST stop signal reaction time [F(2,121)=3.56, p=.031, =0.06]; and 3) impulsive decision making on the IST mean probability of being correct (win condition fixed) [F(2,132)=3.13, p=.047, =0.05] and mean number of boxes opened per trial (win condition decreasing) [F(2,133)=3.40, p=.036, =0.05]. There were no significant between-group effects for spatial planning/problem solving on the SOC and visuospatial working memory on the SSP (Table 3). Similar results were found in supplemental analyses involving one-way ANCOVAs including covariates for sex, age, and FSIQ, except two findings were no longer significant: 1) response inhibition on the SST stop signal reaction time [F(2,117)=2.09, p=.129, =0.03]; and 2) impulsive decision making on the IST mean probability of being correct (win condition fixed) [F(2,128)=2.97, p=.055, =0.04] (Supplemental Table 1).
Table 3.
ANCOVAs Examining Between-Group Neurocognitive Characteristics in Participants with a History of a Suicide Attempt vs. Suicidal Ideation without a Suicide Attempt vs. Typically-Developing Controls, Controlling for Biological Sex
| Variables | History of Suicide Attempt (n=49) M(SD) | Suicidal Ideation without a Suicide Attempt (n=41) M(SD) | Typically-Developing Controls (n=51) M(SD) | Statistic F | p | |
|---|---|---|---|---|---|---|
| Set Shifting/Cognitive Flexibility (ID/ED Task) | ||||||
| Simple Reversal Stage 2 Trials | 8.82(3.86) | 7.85(1.92) | 7.65(1.45) | F(2,137)=3.50 | .033 | 0.05 |
| Simple Reversal Stage 2 Errors | 1.59(1.21) | 1.37(0.77) | 1.25(0.48) | F(2,137)=2.11 | .125 | 0.03 |
| ID/ED Total Trials | 84.35(22.13) | 83.51(19.95) | 82.94(22.82) | F(2,137)=0.08 | .921 | 0.00 |
| ID/ED Total Errors | 19.04(12.90) | 19.56(11.97) | 18.25(13.06) | F(2,137)=0.11 | .892 | 0.00 |
| Spatial Planning/Problem Solving (SOC Task) | ||||||
| Total Moves | 17.93(1.65) | 18.27(2.47) | 17.87(1.90) | F(2,137)=0.70 | .498 | 0.01 |
| Problems Solved in Minimum Moves | 8.33(1.60) | 7.73(1.82) | 8.22(1.72) | F(2,137)=1.33 | .268 | 0.02 |
| Total Initial Thinking Time | 16452.63(10989.47) | 15357.43(9444.22) | 14563.15(11160.43) | F(2,137)=0.32 | .728 | 0.01 |
| Total Subsequent Thinking Time | 1678.60(1559.24) | 1547.84(1883.67) | 1427.50(1607.85) | F(2,137)=0.19 | .830 | 0.00 |
| Visuospatial Working Memory (SSP Task) | ||||||
| Length | 6.63(1.41) | 6.50(1.13) | 6.84(1.33) | F(2,136)=0.79 | .457 | 0.01 |
| Errors | 16.37(8.49) | 15.73(6.42) | 14.18(5.87) | F(2,136)=1.12 | .328 | 0.02 |
| Usage Errors | 2.10(1.39) | 2.35(1.42) | 2.12(1.57) | F(2,136)=0.39 | .676 | 0.01 |
| Response Inhibition (SST Task) | ||||||
| Directional Errors | 7.35(8.26) | 8.34(8.18) | 6.30(8.10) | F(2,123)=0.59 | .554 | 0.01 |
| Proportion of Successful Stops | 0.47(0.10) | 0.66(1.10) | 0.47(0.08) | F(2,122)=1.37 | .258 | 0.02 |
| Median Correct Reaction Time on Go Trials | 422.00(138.99) | 473.13(149.07) | 410.11(77.79) | F(2,122)=2.69 | .072 | 0.04 |
| Stop Signal Reaction Time | 217.04(77.77) | 251.07(90.93) | 206.70(66.03) | F(2,121)=3.56 | .031 | 0.06 |
| Impulsive Decision Making (IST Task) | ||||||
| Average # Boxes Opened (win condition fixed) | 14.74(6.15) | 14.90(6.27) | 16.11(6.24) | F(2,133)=0.84 | .433 | 0.01 |
| Probability of Being Correct (win condition fixed) | 0.78(0.11) | 0.79(0.11) | 0.83(0.11) | F(2,132)=3.13 | .047 | 0.05 |
| Average # Boxes Opened (win condition decreasing) | 6.94(3.23) | 8.36(4.30) | 8.48(3.50) | F(2,133)=3.40 | .036 | 0.05 |
| Probability of Being Correct (win condition decreasing) | 0.67(0.07) | 0.68(0.08) | 0.69(0.08) | F(2,132)=1.99 | .141 | 0.03 |
Note. ID/ED=Intra-Dimensional/Extra-Dimensional Shift Task; SOC=Stockings of Cambridge Task; SSP=Spatial Span Task; SST=Stop Signal Task; IST=Information Sampling Task.
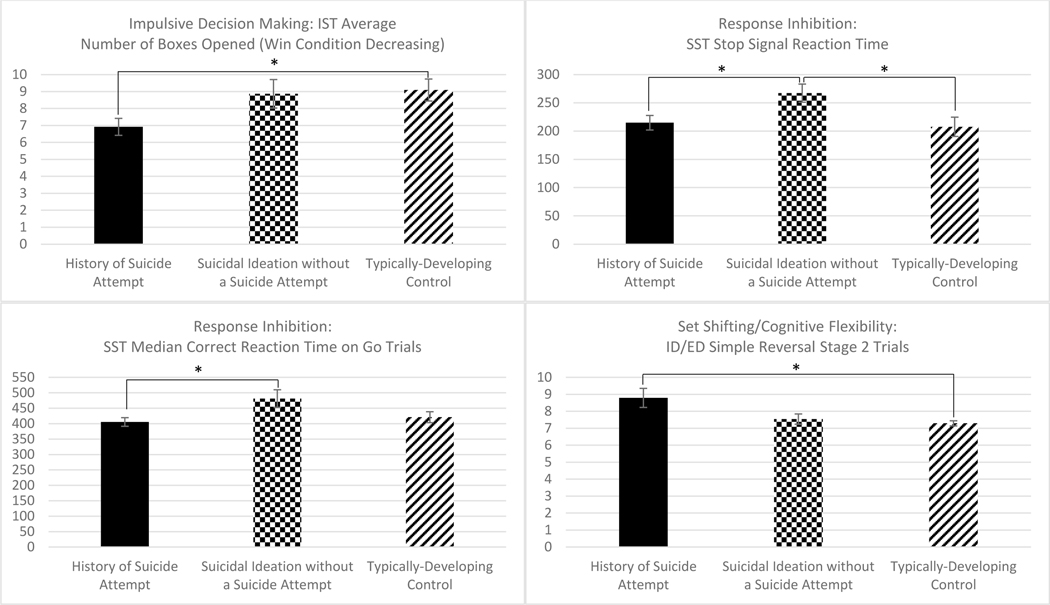
Exploratory post-hoc analyses involved one-way ANOVAs, stratified by sex, given a significant between-group difference on this demographic variable, and in line with prior research (Ruch et al., 2020). For female adolescents (n=101) on CANTAB neurocognitive tasks, there were significant between-group effects for: 1) set shifting/cognitive flexibility on the ID/ED simple reversal stage 2 trials [F(2,98)=3.67, p=.029, =0.07]; 2) response inhibition on the SST median correct reaction time on Go trials [F(2,91)=4.01, p=.021, =0.08] and stop signal reaction time [F(2,90)=4.20, p=.018, =0.09]; and 3) impulsive decision making on the IST mean probability of being correct (win condition decreasing) [F(2,97)=3.80, p=.026, =0.07]. There were no significant between-group effects for spatial planning/problem solving on the SOC or visuospatial working memory on the SSP for female adolescents (Supplemental Table 2). Similar results were found involving one-way ANCOVAs including covariates for age and FSIQ, except response inhibition on the SST stop signal reaction time was no longer significant [F(2,87)=2.92, p=.059, =0.06]. For male adolescents (n=40) on CANTAB neurocognitive tasks, there were no significant between-group effects for any variables. However, these analyses were underpowered (Supplemental Table 3).
Set shifting/cognitive flexibility.
Post-hoc pairwise Bonferroni-corrected tests with the entire sample for set shifting/cognitive flexibility indicated that participants with SA (M=8.82±3.86) required significantly more ID/ED simple reversal stage 2 trials than TDCs (M=7.65±1.45, p=.039, d=0.40, small-to-medium effect) (Table 3, Figure 1). This indicated less set shifting/cognitive flexibility in participants with SA vs. TDCs. There were no significant differences between SA vs. SI and between SI vs. TDCs. In addition, there were no significant between-group effects for ID/ED simple reversal stage 2 errors and ID/ED total trials and errors.
Figure 1.
Between-Group Differences in Impulsive Decision Making, Response Inhibition, and Set Shifting/Cognitive Flexibility in Participants with a History of a Suicide Attempt vs. Suicidal Ideation without a Suicide Attempt vs. Typically-Developing Controls. ID/ED=Intra-Dimensional/Extra-Dimensional Shift Task; SST=Stop Signal Task; IST=Information Sampling Task. Estimated means and standard errors were used. Estimated means were adjusted for biological sex. Error bars represent the standard error. *p<.05; ~ p<.10
Post-hoc pairwise Bonferroni-corrected tests with the female subsample for set shifting/cognitive flexibility indicated that female adolescents with SA (M=8.79±3.65) required significantly more ID/ED simple reversal stage 2 trials than TDCs (M=7.29±0.82, p=.044, d=0.53, medium effect) (Supplemental Table 2, Figure 2). This indicated less set shifting/cognitive flexibility in female adolescents with SA vs. TDCs. There were no significant differences between SA vs. SI and SI vs. TDCs. In addition, there were no significant between-group effects for ID/ED simple reversal stage 2 errors and ID/ED total trials and errors.
Figure 2.
Between-Group Differences in Impulsive Decision Making, Response Inhibition, and Set Shifting/Cognitive Flexibility in Female Participants with a History of a Suicide Attempt vs. Suicidal Ideation without a Suicide Attempt vs. Typically-Developing Controls. ID/ED=Intra-Dimensional/Extra-Dimensional Shift Task; SST=Stop Signal Task; IST=Information Sampling Task. Estimated means and standard errors were used. Error bars represent the standard error. *p<.05
Response inhibition.
Post-hoc pairwise Bonferroni-corrected tests with the entire sample for response inhibition indicated that participants with SI (M=251.07±90.93) had a significantly longer SST stop signal reaction time than TDCs (M=206.70±66.03, p=.049, d=0.56, medium effect) (Table 3, Figure 1). Although not significant, participants with SI (M=251.07±90.93) also had a longer SST stop signal reaction time than those with SA (M=217.04±77.77, p=.098, d=0.41, small-to-medium effect). Of note, the 95% CI was −4.62, 79.22. This indicated greater response inhibition in TDCs vs. SI and SA vs. SI. There were no significant differences between TDCs vs. SA. In addition, there were no significant between-group effects for median correct reaction time on Go trials, SST directional errors, and proportion of successful stops.
Post-hoc pairwise Bonferroni-corrected tests with the female subsample for response inhibition indicated that female adolescents with SI (M=481.00±152.27) had a significantly longer SST median correct reaction time on Go trials than those with SA (M=405.33±90.32, p=.020, d=0.64, medium effect) (Supplemental Table 2, Figure 2). This indicated greater response inhibition in female adolescents with SA vs. SI. There were no significant differences between SA vs. TDCs and SI vs. TDCs. Female adolescents with SI (M=267.20±101.51) also had a significantly longer SST stop signal reaction time than TDCs (M=207.69±71.43, p=.038, d=0.67, medium effect) and than those with SA (M=214.83±76.94, p=.038, d=0.60, medium effect). This indicated greater response inhibition in female TDCs vs. SI and SA vs. SI. There were no significant differences between TDCs vs. SA. In addition, there were no significant between-group effects for SST directional errors and proportion of successful stops.
Impulsive decision making.
Post-hoc pairwise Bonferroni-corrected tests with the entire sample for impulsive decision making indicated that participants with SA (M=0.78±0.11) had a significantly lower probability of being correct (win condition fixed) on the IST than TDCs (M=0.83±0.11, p=.049, d=0.45, small-to-medium effect) (Table 3, Figure 1). There were no significant differences between SA vs. SI and SI vs. TDCs. Although not significant, participants with SA (M=6.94±3.23) had a lower average number of boxes opened (win condition decreasing) on the IST than TDCs (M=8.48±3.50, p=.057, d=0.46, small-to-medium effect). Of note, the 95% CI was −0.04, 3.65. There were no significant differences between SA vs. SI and SI vs. TDCs. Both IST findings indicated greater impulsive decision making in participants with SA vs. TDCs. In addition, there were no significant between-group effects for IST probability of being correct (win condition decreasing) and average number of boxes opened (win condition fixed).
Post-hoc pairwise Bonferroni-corrected tests with the female subsample for impulsive decision making indicated that female adolescents with SA (M=6.92±3.26) had a significantly lower average number of boxes opened (win condition decreasing) on the IST vs. TDCs (M=9.09±3.56, p=.048, d=0.64, medium effect) (Supplemental Table 2, Figure 2). This indicated greater impulsive decision making in female adolescents with SA vs. TDCs. There were no significant differences between SA vs. SI and SI vs. TDCs. In addition, there were no significant between-group effects for IST probability of being correct (win condition decreasing), average number of boxes opened (win condition fixed), and probability of being correct (win condition fixed).
Discussion
This study adds to the literature on neurocognitive functioning in suicidal adolescents. Findings indicated that participants with SA demonstrated less set shifting/cognitive flexibility and greater impulsive decision making compared to TDCs. In addition, both TDCs and participants with SA had greater response inhibition than participants with SI. Similar results were found when analyzing the female adolescent subsample separately. There were no significant differences in neurocognitive functioning for male adolescents. In addition, there were no significant findings for spatial planning/problem solving or visuospatial working memory. Future research is needed to confirm whether such deficits are also seen in male adolescents, given sample size restrictions in this study. Nevertheless, current findings may be useful to consider in efforts towards improving evidence-based assessments and treatments for suicidal adolescents.
As hypothesized, female adolescents with SA demonstrated less set shifting/cognitive flexibility compared to TDCs. This finding advances the literature, as set shifting/cognitive flexibility has not commonly been examined in suicidal adolescents, with one study reporting null findings (Ruch et al., 2020). However, this prior study examined omnibus variables, and similarly, our examination of total trials and errors on the ID/ED task yielded null results. However, those with SA required significantly more trials than TDCs on the simple reversal stage 2, which is relevant because this represents the first time participants are required to adapt to the reversal of the prior stage 1 stimulus/reward relationship. Indeed, deficits in this stage have been associated with cognitive flexibility impairments in pediatric bipolar disorder (Dickstein et al., 2016; Dickstein et al., 2007; Dickstein et al., 2004) and worsening trajectory of SI (MacPherson et al., 2021). Thus, findings suggest that the simple reversal stage 2 may be sensitive to detecting cognitive flexibility deficits, and therefore may be a useful adjunct to the assessment of suicidal youth and important to target in treatment. In line with the cognitive model of suicide (Wenzel & Beck, 2008) and other escape theories of suicide (Baumeister, 1990; Linehan, 1993), if suicidal individuals become preoccupied with suicide as their only option and are unable to disengage from emotionally evocative or suicide-relevant stimuli to more effective coping strategies, this may lead to further distress and eventual SA. Thus, enhancing cognitive flexibility in suicidal female adolescents (e.g., via cognitive restructuring) appears important.
Female adolescents with SA also demonstrated greater impulsive decision making compared to TDCs. This is consistent with prior research linking different facets of impulsivity to SA (Ackerman et al., 2015; Bridge et al., 2012; Dougherty et al., 2009; Liu et al., 2017; Ruch et al., 2020; Zelazny et al., 2019). From a clinical perspective, suicidal adolescents with greater impulsive decision making may lack the ability to effectively brainstorm and evaluate different options for tolerating distress, and instead quickly opt for SA. Thus, study findings underscore the importance of assessing impulsive decision making in suicidal female adolescents and addressing these impairments in treatment via established therapeutic techniques (e.g., problem solving) and/or novel paradigms (detailed below).
Significant differences were also found for response inhibition. Female TDCs had greater response inhibition than female adolescents with SI, which was expected. Clinically, this may suggest those with SI have difficulty refraining from and/or stopping engagement in certain behaviors, which would be problematic in the context of risky behaviors (e.g., conflict, risky sexual behavior, non-suicidal self-injury), and which may increase risk for SA. However, female adolescents with SA demonstrated greater response inhibition than those with SI, which was unexpected. It is also curious that those with SA and TDCs did not differ. We hypothesized that those with SA would demonstrate less response inhibition, signifying a potential difficulty in refraining from suicidal acts and stopping these behaviors once they have started. One consideration is that response inhibition was measured using routine neurocognitive tasks, as opposed to tasks with emotional content—impaired response inhibition may be more apparent in those with SA amid distress (Stewart et al., 2017). Thus, response inhibition may be sensitive to differentiating TDCs vs. SI and SA vs. SI in female adolescents, though further research is needed to determine the nature of this relationship.
Notably, most of the significant between-group differences in neurocognitive functioning were found in female adolescents; none were identified in male adolescents. Although additional research will be needed to examine whether true sex differences exist in neurocognitive functioning among female adolescents vs. male adolescents, prior research has documented differences in risk for SA among female vs. male adolescents and young adults in terms of demographic, socioeconomic, parent/family, and clinical factors (Navarro et al., 2021). In addition, rumination, or the tendency to passively and repetitively focus on one’s dysphoric mood, is more common in female adolescents and associated with increased risk for depression (Alloy et al., 2016). Impaired cognitive flexibility, or an inability to adapt to or disengage from stimuli, is related to rumination. Thus, findings suggest that a multi-level approach to assessing inflexible thinking may enhance our understanding of the clinical manifestation and neurocognitive deficits associated with increased risk for SA in female adolescents, thus informing treatment efforts.
Prior literature also suggests that impulsivity deficits may differ among suicidal female adolescents vs. male adolescents. For instance, SI and SA are more common in female adolescents, though death by suicide is more common in male adolescents (Fox et al., 2018). In addition, male adolescents who died by suicide may be different than those who attempted; for instance, they may have greater deficits in impulsivity and cognitive flexibility. However, the reverse could be true, as highly planned attempts tend to be more lethal (Dombrovski et al., 2011; Nakagawa et al., 2009). Thus, the methods more likely to be used by male adolescents may not require as much planning to be fatal. Also, and as aforementioned, facets of impulsive decision making and response inhibition are related to suicide (Ackerman et al., 2015; Bridge et al., 2012; Dougherty et al., 2009; Liu et al., 2017; Ruch et al., 2020; Zelazny et al., 2019). Thus, it is possible that greater impulsivity in female adolescents may confer increased risk facilitating progression from SI to SA, indicating an important area of further investigation.
Notably, and contrary to hypotheses, there were no significant group differences in SA vs. SI vs. TDCs on indices of spatial planning/problem solving or visuospatial working memory, despite the apparent clinical relevance of these constructs to SI and SA, and prior research documenting such differences in these and related indices (Horesh, 2001; Ruch et al., 2020; Sommerfeldt et al., 2016). Thus, future research should continue to evaluate these constructs.
Finally, findings should be interpreted within the context of study design elements. For instance, the sample represented a high level of acuity and severity of SI and SA, requiring treatment at a psychiatric hospital via an inpatient unit or partial hospitalization program. Those requiring hospitalization for SI are often at imminent risk for making a SA, as opposed to adolescents with SI not requiring hospitalization, who may not be as impaired on neurocognitive constructs. Thus, the severity of SI may have contributed to limited differences in SI vs. SA in this study. While the current study sheds light on neurocognitive deficits in suicidal adolescents, it also identifies many areas for future research.
Clinical Implications
Findings indicate that the specific neurocognitive constructs of set shifting/cognitive flexibility and impulsive decision making may be effective for identifying female adolescents with SA, while response inhibition may be relevant for those with SI. To augment existing suicide risk assessments, which currently lack specificity and sensitivity (Franklin et al., 2017) and largely utilize self-report methods that are subject to self-preservation biases (Stewart et al., 2017), the addition of neurocognitive tasks may offer a brief and objective indicator for assessing risk.
Similarly, despite growing evidence-based treatments for this population (Glenn et al., 2019), rates of suicide have increased nearly 50% over the past 10 years for youth ages 10–24, making suicide the second leading cause of death for this age group (Centers for Disease Control and Prevention, 2021a, 2021b). Thus, novel intervention strategies are needed. Cognitive remediation paradigms that specifically target neurocognitive deficits in suicidal adolescents may serve as useful adjuncts to existing treatments to enhance the uptake of therapeutic skills while targeting neurocognitive impairments. Indeed, cognitive remediation has proven effective for other disorders, including pediatric bipolar disorder (Dickstein et al., 2015), depression (Thérond et al., 2021), and schizophrenia (Wykes et al., 2011). Attention bias modification training has also shown promise for anxiety symptoms (White et al., 2017). In addition, evaluative conditioning paradigms via phone apps have proven effective for reducing suicidal thoughts and behaviors (Franklin et al., 2016). Thus, pending replication of findings, future research should develop and test the efficacy and effectiveness of cognitive remediation interventions for suicidal youth targeting set shifting/cognitive flexibility, impulsive decision making, and response inhibition.
Limitations
Study findings should be interpreted within the context of limitations. First, the sample was drawn from a psychiatric inpatient unit or partial hospitalization program, suggesting a high level of acuity and severity of SI and SA. Thus, findings may not generalize to community samples or those with a less severe presentation. Second, some might speculate about potential referral bias in the sample due to response inhibition deficits (i.e., whether adolescents with suicidality and impaired response inhibition are more likely to seek care in an emergency psychiatric setting). However, it is often the parents, not the adolescent, who seek care for mental health and other issues. Thus, it is unlikely response inhibition affected our sampling, though examining parental cognitive attributes of adolescents with suicidality would be worth further study.
Third, the sample size was modest, and the design was cross-sectional, which limited our ability to examine temporal relationships between neurocognitive constructs, SI, and SA. Fourth, the sample was comprised predominantly of female adolescents and inadequately powered to detect true sex differences, given the small male subsample (n=7 SA, n=13 SI, n=20 TDCs). Fifth, the proportion of female adolescents to male adolescents was significantly higher in those with SA vs. TDCs, which may have contributed to different findings between sexes. Sixth, several variables within each neurocognitive construct were examined, and while some variables within the same construct demonstrated significant differences, others did not. This may be a result of the modest sample size or an indication of the unique predictive power of certain variables over others. Seventh, in an effort to balance between Type I and Type II errors in this unique dataset, we applied a more liberal analytic approach to explore associations between neurocognitive constructs and suicidality in adolescents, though multiple comparisons may have led to spurious findings.
Eighth, all tasks were administered without emotional content, and therefore assessed cold cognition, which may have influenced the limited significant findings in adolescents with SI vs. SA. However, prior research has documented that cognitive control deficits are exacerbated in adolescents with SI vs. SA when emotional- and suicide-related stimuli are used (Stewart et al., 2017). Thus, the use of tasks without emotional content may have contributed to limited differences in SI vs. SA groups in the current study, with most significant findings emerging for SA vs. TDCs. It may be that those with a history of SA are particularly impaired under the conditions of emotional arousal, but not during general neurocognitive tasks.
Thus, future research should address these shortcomings. Importantly, studies should be replicated in different settings (e.g., community, outpatient), use a larger sample with a higher proportion of male adolescents adequately powered to detect potential sex differences, and examine longitudinal and directional relationships between neurocognitive constructs with SA and SI in adolescents. In addition, it will be important for future research to incorporate neurocognitive tasks with emotional content, examine parental cognitive attributes of adolescents with suicidality, and investigate the robustness and predictive validity of certain neurocognitive variables over others in their association with SI and SA using stringent methodology.
Conclusions
Suicidal adolescents exhibit unique neurocognitive deficits that may be important to consider in assessment and treatment. Findings indicated that female adolescents with SA demonstrated less set shifting/cognitive flexibility and greater impulsive decision making compared to TDCs. In addition, both female adolescent TDCs and those with SA had greater response inhibition than female adolescents with SI. Future research should investigate whether similar or different impairments are apparent in suicidal male adolescents. Nevertheless, these neurocognitive constructs may be important to assess in suicide risk evaluations, to augment existing assessment strategies, and to target in intervention efforts for suicidal female adolescents via novel cognitive remediation paradigms.
Supplementary Material
Acknowledgements
We gratefully acknowledge and thank the adolescent participants and their families for their time and effort participating in this study, without which this research would not be possible.
Funding
Primary funding for this research was from the National Institute of Mental Health grant R01MH097703 (PIs: Esposito-Smythers/Spirito). Additional funding sources included the National Institute of Mental Health grants R01MH110379 (PI: Dickstein), R01MH111542 (PI: Dickstein), and K24MH110402 (PI: Dickstein). The funders had no role in the study design; in the collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
Footnotes
Declarations
Ethics Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This study was approved by the Institutional Review Boards of Lifespan Corporation and Brown University.
Informed Consent
Parents and adolescent participants provided written informed consent and assent, respectively.
Conflicts of Interest
The authors have no financial relationships or conflicts of interest related to this study to disclose.
References
- Ackerman JP, McBee-Strayer SM, Mendoza K, Stevens J, Sheftall AH, Campo JV, & Bridge JA (2015). Risk-sensitive decision-making deficit in adolescent suicide attempters. Journal of Child and Adolescent Psychopharmacology, 25(2), 109–113. 10.1089/cap.2014.0041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alloy LB, Hamilton JL, Hamlat EJ, & Abramson LY (2016). Pubertal development, emotion regulatory styles, and the emergence of sex differences in internalizing disorders and symptoms in adolescence. Clinical Psychological Science, 4(5), 867–881. 10.1177/2167702616643008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baumeister RF (1990). Suicide as escape from self. Psychological Review, 97(1), 90–113. 10.1037/0033-295x.97.1.90 [DOI] [PubMed] [Google Scholar]
- Bridge JA, Goldstein TR, & Brent DA (2006). Adolescent suicide and suicidal behavior. Journal of Child Psychology and Psychiatry, 47(3–4), 372–394. 10.1111/j.1469-7610.2006.01615.x [DOI] [PubMed] [Google Scholar]
- Bridge JA, McBee-Strayer SM, Cannon EA, Sheftall AH, Reynolds B, Campo JV, Pajer KA, Barbe RP, & Brent DA (2012). Impaired decision making in adolescent suicide attempters. Journal of the American Academy of Child and Adolescent Psychiatry, 51(4), 394–403. 10.1016/j.jaac.2012.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- CANTAB. (2021). Neuropsychological Tests from Cambride Cognition. Retrieved from https://www.cambridgecognition.com/cantab/
- Centers for Disease Control and Prevention. (2021a). WISQARS Fatal Injury Reports, National, Regional, and State, 1981–2019. Retrieved March 10, 2021 from https://webappa.cdc.gov/sasweb/ncipc/mortrate.html
- Centers for Disease Control and Prevention. (2021b). WISQARS Leading Causes of Death Reports, 1981–2019. Retrieved March 10, 2021 from https://webappa.cdc.gov/sasweb/ncipc/leadcause.html
- Chamberlain SR, & Sahakian BJ (2007). The neuropsychiatry of impulsivity. Current Opinions in Psychiatry, 20(3), 255–261. 10.1097/YCO.0b013e3280ba4989 [DOI] [PubMed] [Google Scholar]
- Dickstein DP, Axelson D, Weissman AB, Yen S, Hunt JI, Goldstein BI, Goldstein TR, Liao F, Gill MK, Hower H, Frazier TW, Diler RS, Youngstrom EA, Fristad MA, Arnold LE, Findling RL, Horwitz SM, Kowatch RA, Ryan ND, Strober M, Birmaher B, & Keller MB (2016). Cognitive flexibility and performance in children and adolescents with threshold and sub-threshold bipolar disorder. European Child and Adolescent Psychiatry, 25(6), 625–638. 10.1007/s00787-015-0769-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickstein DP, Cushman GK, Kim KL, Weissman AB, & Wegbreit E (2015). Cognitive remediation: Potential novel brain-based treatment for bipolar disorder in children and adolescents. CNS Spectrums, 20(4), 382–390. 10.1017/s109285291500036x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickstein DP, Nelson EE, McClure EB, Grimley ME, Knopf L, Brotman MA, Rich BA, Pine DS, & Leibenluft E (2007). Cognitive flexibility in phenotypes of pediatric bipolar disorder. Journal of the American Acadademy of Child and Adolescent Psychiatry, 46(3), 341–355. 10.1097/chi.0b013e31802d0b3d [DOI] [PubMed] [Google Scholar]
- Dickstein DP, Treland JE, Snow J, McClure EB, Mehta MS, Towbin KE, Pine DS, & Leibenluft E (2004). Neuropsychological performance in pediatric bipolar disorder. Biological Psychiatry, 55(1), 32–39. 10.1016/s0006-3223(03)00701-7 [DOI] [PubMed] [Google Scholar]
- Dombrovski AY, Szanto K, Siegle GJ, Wallace ML, Forman SD, Sahakian B, Reynolds CF 3rd, & Clark L (2011). Lethal forethought: Delayed reward discounting differentiates high- and low-lethality suicide attempts in old age. Biological Psychiatry, 70(2), 138–144. 10.1016/j.biopsych.2010.12.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dougherty DM, Mathias CW, Marsh-Richard DM, Prevette KN, Dawes MA, Hatzis ES, Palmes G, & Nouvion SO (2009). Impulsivity and clinical symptoms among adolescents with non-suicidal self-injury with or without attempted suicide. Psychiatry Research, 169(1), 22–27. 10.1016/j.psychres.2008.06.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esposito-Smythers C, Wolff JC, Liu RT, Hunt JI, Adams L, Kim K, Frazier EA, Yen S, Dickstein DP, & Spirito A (2019). Family-focused cognitive behavioral treatment for depressed adolescents in suicidal crisis with co-occurring risk factors: a randomized trial. Journal of Child Psychology and Psychiatry, 60(10), 1133–1141. 10.1111/jcpp.13095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox KR, Millner AJ, Mukerji CE, & Nock MK (2018). Examining the role of sex in self-injurious thoughts and behaviors. Clinical Psychology Review, 66, 3–11. 10.1016/j.cpr.2017.09.009 [DOI] [PubMed] [Google Scholar]
- Franklin JC, Fox KR, Franklin CR, Kleiman EM, Ribeiro JD, Jaroszewski AC, Hooley JM, & Nock MK (2016). A brief mobile app reduces nonsuicidal and suicidal self-injury: Evidence from three randomized controlled trials. Journal of Consulting and Clinical Psychology, 84(6), 544–557. 10.1037/ccp0000093 [DOI] [PubMed] [Google Scholar]
- Franklin JC, Ribeiro JD, Fox KR, Bentley KH, Kleiman EM, Huang X, Musacchio KM, Jaroszewski AC, Chang BP, & Nock MK (2017). Risk factors for suicidal thoughts and behaviors: A meta-analysis of 50 years of research. Psychological Bulletin, 143(2), 187–232. 10.1037/bul0000084 [DOI] [PubMed] [Google Scholar]
- Gifuni AJ, Perret LC, Lacourse E, Geoffroy MC, Mbekou V, Jollant F, & Renaud J (2020). Decision-making and cognitive control in adolescent suicidal behaviors: A qualitative systematic review of the literature. European Child and Adolescent Psychiatry, 30(12), 1839–1855. 10.1007/s00787-020-01550-3 [DOI] [PubMed] [Google Scholar]
- Gläscher J, Adolphs R, Damasio H, Bechara A, Rudrauf D, Calamia M, Paul LK, & Tranel D (2012). Lesion mapping of cognitive control and value-based decision making in the prefrontal cortex. Proceedings of the National Academy of Sciences of the United States of America, 109(36), 14681–14686. 10.1073/pnas.1206608109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glenn CR, Cha CB, Kleiman EM, & Nock MK (2017). Understanding suicide risk within the Research Domain Criteria (RDoC) framework: Insights, challenges, and future research considerations. Clinical Psychological Science, 5(3), 568–592. 10.1177/2167702616686854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glenn CR, Esposito EC, Porter AC, & Robinson DJ (2019). Evidence base update of psychosocial treatments for self-injurious thoughts and behaviors in youth. Journal of Clinical Child and Adolescent Psychology, 48(3), 357–392. 10.1080/15374416.2019.1591281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton KR, Littlefield AK, Anastasio NC, Cunningham KA, Fink LHL, Wing VC, Mathias CW, Lane SD, Schütz CG, Swann AC, Lejuez CW, Clark L, Moeller FG, & Potenza MN (2015). Rapid-response impulsivity: Definitions, measurement issues, and clinical implications. Personality Disorders, 6(2), 168–181. 10.1037/per0000100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton KR, Mitchell MR, Wing VC, Balodis IM, Bickel WK, Fillmore M, Lane SD, Lejuez CW, Littlefield AK, Luijten M, Mathias CW, Mitchell SH, Napier TC, Reynolds B, Schütz CG, Setlow B, Sher KJ, Swann AC, Tedford SE, White MJ, Winstanley CA, Yi R, Potenza MN, & Moeller FG (2015). Choice impulsivity: Definitions, measurement issues, and clinical implications. Personality Disorders, 6(2), 182–198. 10.1037/per0000099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horesh N (2001). Self-report vs. computerized measures of impulsivity as a correlate of suicidal behavior. Crisis, 22(1), 27–31. 10.1027//0227-5910.22.1.27 [DOI] [PubMed] [Google Scholar]
- Kann L, McManus T, Harris WA, Shanklin SL, Flint KH, Queen B, Lowry R, Chyen D, Whittle L, Thornton J, Lim C, Bradford D, Yamakawa Y, Leon M, Brener N, & Ethier KA (2018). Youth Risk Behavior Surveillance - United States, 2017. MMWR: Surveillance Summaries, 67(8), 1–114. 10.15585/mmwr.ss6708a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, Williamson D, & Ryan N (1997). Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): Initial reliability and validity data. Journal of the American Academy of Child and Adolescent Psychiatry, 36(7), 980–988. 10.1097/00004583-199707000-00021 [DOI] [PubMed] [Google Scholar]
- Klonsky ED, & May AM (2014). Differentiating suicide attempters from suicide ideators: A critical frontier for suicidology research. Suicide and Life-Threatening Behavior, 44(1), 1–5. 10.1111/sltb.12068 [DOI] [PubMed] [Google Scholar]
- Klonsky ED, Saffer BY, & Bryan CJ (2018). Ideation-to-action theories of suicide: A conceptual and empirical update. Current Opinions in Psychology, 22, 38–43. 10.1016/j.copsyc.2017.07.020 [DOI] [PubMed] [Google Scholar]
- Linehan MM (1993). Cognitive behavioral treatment of borderline personality disorder. New York, NY: Guilford Press. [Google Scholar]
- Liu RT, Trout ZM, Hernandez EM, Cheek SM, & Gerlus N (2017). A behavioral and cognitive neuroscience perspective on impulsivity, suicide, and non-suicidal self-injury: Meta-analysis and recommendations for future research. Neuroscience and Biobehavioral Reviews, 83, 440–450. 10.1016/j.neubiorev.2017.09.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacPherson HA, Kudinova AY, Schettini E, Jenkins GA, Gilbert AC, Thomas SA, Kim KL, Radoeva PD, Fenerci RLB, Yen S, Hower H, Hunt J, Keller MB, & Dickstein DP (2021). Relationship between cognitive flexibility and subsequent course of mood symptoms and suicidal ideation in young adults with childhood-onset bipolar disorder. European Child and Adolescent Psychiatry, 31(2), 299–312. 10.1007/s00787-020-01688-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- May AM, & Klonsky ED (2016). What distinguishes suicide attempters from suicide ideators? A meta-analysis of potential factors. Clinical Psychology: Science and Practice, 23(1), 5–20. 10.1111/cpsp.12136 [DOI] [Google Scholar]
- Nakagawa A, Grunebaum MF, Oquendo MA, Burke AK, Kashima H, & Mann JJ (2009). Clinical correlates of planned, more lethal suicide attempts in major depressive disorder. Journal of Affective Disorders, 112(1–3), 237–242. 10.1016/j.jad.2008.03.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Navarro MC, Ouellet-Morin I, Geoffroy MC, Boivin M, Tremblay RE, Côté SM, & Orri M (2021). Machine learning assessment of early life factors predicting suicide attempt in adolescence or young adulthood. JAMA Network Open, 4(3), e211450. 10.1001/jamanetworkopen.2021.1450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Green JG, Hwang I, McLaughlin KA, Sampson NA, Zaslavsky AM, & Kessler RC (2013). Prevalence, correlates, and treatment of lifetime suicidal behavior among adolescents: Results from the National Comorbidity Survey Replication Adolescent Supplement. JAMA Psychiatry, 70(3), 300–310. 10.1001/2013.jamapsychiatry.55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Posner K, Brown GK, Stanley B, Brent DA, Yershova KV, Oquendo MA, Currier GW, Melvin GA, Greenhill L, Shen S, & Mann JJ (2011). The Columbia-Suicide Severity Rating Scale: Initial validity and internal consistency findings from three multisite studies with adolescents and adults. American Journal of Psychiatry, 168(12), 1266–1277. 10.1176/appi.ajp.2011.10111704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruch D, Sheftall AH, Heck K, McBee-Strayer SM, Tissue J, Reynolds B, Ackerman J, Brent DA, Campo JV, & Bridge JA (2020). Neurocognitive vulnerability to youth suicidal behavior. Journal of Psychiatric Research, 131, 119–126. 10.1016/j.jpsychires.2020.08.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sommerfeldt SL, Cullen KR, Han G, Fryza BJ, Houri AK, & Klimes-Dougan B (2016). Executive attention impairment in adolescents with major depressive disorder. Journal of Clinical Child and Adolescent Psychology, 45(1), 69–83. 10.1080/15374416.2015.1072823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart JG, Glenn CR, Esposito EC, Cha CB, Nock MK, & Auerbach RP (2017). Cognitive control deficits differentiate adolescent suicide ideators From attempters. Journal of Clinical Psychiatry, 78(6), e614–e621. 10.4088/JCP.16m10647 [DOI] [PubMed] [Google Scholar]
- Stewart JG, Kim JC, Esposito EC, Gold J, Nock MK, & Auerbach RP (2015). Predicting suicide attempts in depressed adolescents: Clarifying the role of disinhibition and childhood sexual abuse. Journal of Affective Disorders, 187, 27–34. 10.1016/j.jad.2015.08.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart JG, Polanco-Roman L, Duarte CS, & Auerbach RP (2019). Neurocognitive processes implicated in adolescent suicidal thoughts and behaviors: Applying an RDoC framework for conceptualizing risk. Current Behavioral Neuroscience Reports, 6(4), 188–196. 10.1007/s40473-019-00194-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thérond A, Pezzoli P, Abbas M, Howard A, Bowie CR, & Guimond S (2021). The efficacy of cognitive remediation in depression: A systematic literature review and meta-analysis. Journal of Affective Disorders, 284, 238–246. 10.1016/j.jad.2021.02.009 [DOI] [PubMed] [Google Scholar]
- Wechsler D (1999). Wechsler Abbreviated Scale of Intelligence (WASI) Subtests: Matrix Reasoning and Vocabulary. San Antonio, TX: The Psychological Corporation. [Google Scholar]
- Wegbreit E, Cushman GK, Weissman AB, Bojanek E, Kim KL, Leibenluft E, & Dickstein DP (2016). Reversal-learning deficits in childhood-onset bipolar disorder across the transition from childhood to young adulthood. Journal of Affective Disorders, 203, 46–54. 10.1016/j.jad.2016.05.046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wenzel A, & Beck AT (2008). A cognitive model of suicidal behavior: Theory and treatment. Applied and Preventive Psychology, 12(4), 189–201. 10.1016/j.appsy.2008.05.001 [DOI] [Google Scholar]
- White LK, Sequeira S, Britton JC, Brotman MA, Gold AL, Berman E, Towbin K, Abend R, Fox NA, Bar-Haim Y, Leibenluft E, & Pine DS (2017). Complementary features of attention bias modification therapy and cognitive-behavioral therapy in pediatric anxiety disorders. American Journal of Psychiatry, 174(8), 775–784. 10.1176/appi.ajp.2017.16070847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wykes T, Huddy V, Cellard C, McGurk SR, & Czobor P (2011). A meta-analysis of cognitive remediation for schizophrenia: Methodology and effect sizes. American Journal of Psychiatry, 168(5), 472–485. 10.1176/appi.ajp.2010.10060855 [DOI] [PubMed] [Google Scholar]
- Zelazny J, Melhem N, Porta G, Biernesser C, Keilp JG, Mann JJ, Oquendo MA, Stanley B, & Brent DA (2019). Childhood maltreatment, neuropsychological function and suicidal behavior. Journal of Child Psychology and Psychiatry, 60(10), 1085–1093. 10.1111/jcpp.13096 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.