Abstract
We aimed to systematically review and meta-analyze the association of employees working in various kinds of open-plan offices with sick leave data, compared to those working in traditional cell offices. Databases of PubMed, PubPsych, and Psyndex were systematically searched following the PRISMA statement. Pooled summary estimates of odds ratio (OR) were calculated comparing sick leave of employees in cell offices with those working in small open-plan offices (4–9 people), and those in various open-plan office solutions (≥4 people). We used Forest plots visualizing study-specific estimates and the pooled fixed and random effects estimators. Five studies were identified (2008–2020) with a total of 13,277 (range 469–6,328) participants. Compared with employees working in cell offices, those working in small open-plan offices were associated with higher odds of sick leave days (OR=1.27; 95% CI 0.99–1.54; p=0.046) as well as those working in various kinds of open-plan offices with ≥4 colleagues (OR=1.24; 95% CI 0.96–1.51; p=0.004). Our results are consistent with those of earlier reviews focusing on other effects of open-plan office solutions such as health and well-being. Different solutions for office design and architectural lay-out should be the focus of future studies to balance pros and cons of open-plan offices.
Keywords: Absenteeism, Activity-based working, Employees, Office type, Open office, Sickness, Sick leave, Workspace
Introduction
Most employees in western countries work in offices1). In the last decades, a worldwide trend has emerged in this regard that the office environment has changed from the traditional provision of individual cell offices to more open designed workspaces. The provision of workspaces ranges from various options of offices with single and shared offices to activity-based flexible offices2) changing the workspace from an exclusive to a more communal area. Although the trend to open-plan offices is becoming increasingly common and should therefore be a growing topic of scientific interest, evidence on the implications on employee health and well-being as well as sick leave is still very limited.
There are large expectations of corporates about the benefits of open-plan office solutions, often driven by building developers and designers, especially regarding communication, collaboration, work satisfaction, and well-being of employees. New specialists are hired by corporates to introduce ideas and solutions for “new ways of working” or “new work”, often combined with the provision of building and office alterations. However, a robust foundation to these expectations is still missing. While some studies found benefits of open-plan office concepts such as improved communication, cooperation, innovation, and performance3,4,5), others reported negative effects for the same study outcomes6,7,8). Others found negative health effects on employees such as infections9) or disturbances by noise10, 11). Recent reviews of the literature have suggested a disruptive effect on employee health and well-being12, 13).
Reduced satisfaction, health and well-being of employees at work might affect productivity by increased sick leave (being absent from work due to sickness) and presenteeism (attending work while being sick). While innovative office concepts may save overall office costs due to higher occupant density as well as lower technical and general service costs and therefore seem to have a high cost-efficiency ratio for corporates, different variables with negative effects will still have a high impact on productivity. Therefore, possible costs for sick leave should be considered when calculating a business case for the introduction of open-plan offices. However, evidence of implications on productivity and on sick leave is still limited11,12,13). To our best knowledge, there is no meta-analysis on the association of open-plan offices and sick leave so far. The aim of this review is therefor to summarize current evidence about this association using statistical methods of meta-analysis.
Subjects and Methods
Search strategy
We searched multiple databases, including PSYNDEX (1981–2021), PubPsych (Leibniz-Zentrum für Psychologische Information und Dokumentation, 1907–2021), and Medline (1966–2021) accessed by PubMed (US National Library of Medicine). Articles eligible for review were those published up to July 31, 2021. Search terms included open-plan, open office, activity-based working, office design, flexible office, open space, AND sick, sick leave, sickness, absenteeism, respectively: (sick leave OR sickness OR absenteeism) AND (open plan OR open office OR activity-based working OR office design OR flex* office OR open space).
Study selection
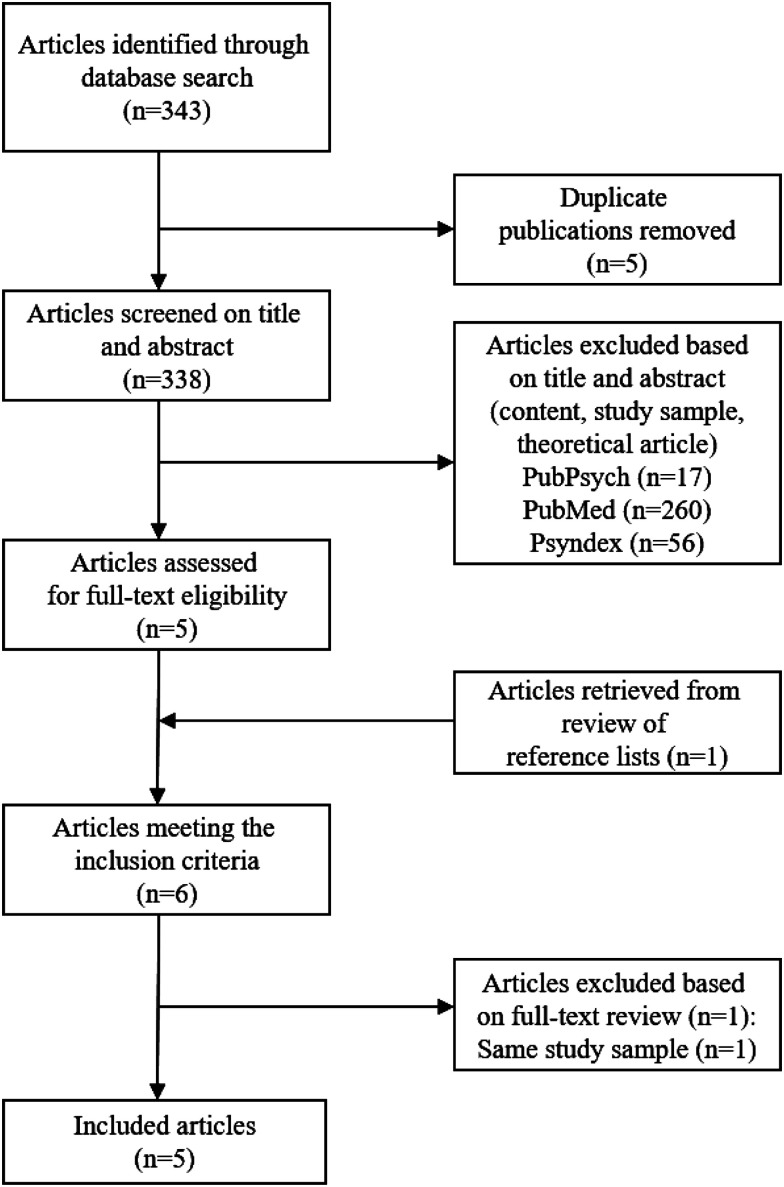
Methods of the analysis and inclusion criteria were specified in advance, following the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analysis) 2020 statement14). At least two review authors (DM, RH) independently read the titles and abstracts of each article to identify whether the respective manuscript met all of the following eligibility criteria: (1) study comparing different office designs; (2) sick leave as study outcome; (3) study conducted in an office environment with working adults; (4) full text article; (5) article written in English or German language; (6) peer-reviewed article. Editorials, book chapters, lectures, and commentaries were excluded from the analysis (Fig. 1). If an abstract was not available or in doubt if the inclusion criteria were met or in case of disagreement between the reviewers, the full text of the article was screened. Reference lists of all included articles were screened to identify potential articles for review. Initial disagreement between the two reviewers was resolved by a third review author (MJ).
Fig. 1.
Study selection.
The search strategy identified 343 articles—265 from PubMed, 21 from PubPsych and 57 from PSYNDEX. After excluding 5 doublets, 338 abstracts were screened. Five full-text articles were reviewed following the initial application of exclusion criteria. Reference list screening identified one additional eligible publication, while one article was excluded due to the exploration of the same study sample15, 16), resulting in a total sample of 5 articles published between 2008 and 2021 (Fig. 1).
Data extraction
A standard data extraction sheet was developed. At least two review authors independently reviewed the full text of each article and extracted the following information from the 5 articles included for review: name of first author, year of publication, country, study period, study design, sample size, age of the study sample, sex (% female), response rate, confounders and study findings. The principal summary measure was the association office design had on sick leave. All results were categorized and are presented descriptively.
Quality assessment/Assessment of potential bias
A standardized checklist was used to identify study features associated with potential sources of bias. According to a recent review on tools to assess the methodological quality of studies17), the Joanna Briggs Institute (JBI) Critical Appraisal Checklist for studies reporting prevalence data18) is the most common tool for quality assessment of cross-sectional studies (Appendix Table 1). We analyzed selection, description and size of the study sample, information on statistical analysis including adjustment for confounding variables, and response rate. When present, each of the nine criterions was scored as “1”, the value “0” was used if data were missing or if specific information was not provided. An overall quality score (0–9) was calculated by summing the ratings. The quality of the study was regarded as high if the quality score was indicated ≥8. This quality assessment led to a judgment about the risk of bias (high quality = low risk of bias).
Statistical analysis
We used meta-analysis to combine the results from the analyses of the estimates from the published studies reported as rate ratio or risk ratio (RR) or odds ratio (OR). We regarded ORs as close approximations of RR resulting in a common estimate of OR. We calculated pooled summary estimates of OR by using fixed effects (the Mantel–Haenszel method19)) and random effects (the DerSimonian and Laird model20)) meta-analysis techniques. We analyzed two calculations. First, we calculated estimates comparing employees working in cell offices (1 employee) with those in small open-plan offices (4–9 employees). Second, we compared employees in cell offices with various kinds of open-plan offices hosting at least 4 employees (small open-plan office, medium sized open-plan office, large open-plan office, flex office, combi office). Standard definitions of these various types of offices are presented in Table 1. Sick leave was defined as being absent from work due to sickness, might that be certified or uncertified by a medical doctor.
Table 1. Definition of various office types.
| Office type | Definition | |
|---|---|---|
| Traditional office types | ||
| Single room office (cell office) | 1 person in an individual office room | |
| Shared room office | 2–3 people sharing an office room | |
| Traditional open-plan offices | ||
| Small open-plan office | 4–9 people sharing an office room | |
| Medium open-plan office | 10–24 people working in one office room | |
| Large open-plan office | >24 people working in one office room | |
| Activity-based office types | ||
| Flex-office | No personal workstations, less workstations than employees (e.g. ratio of 70%), additional space for phone calls, concentrated work, meetings etc. | |
| Combi-office | Mix of individual and shared workstations as well as shared facilities (project rooms, meeting rooms etc.). | |
As we assumed unexplained heterogeneity among studies due to heterogeneous study design we considered the random effects estimate as the preferable approach. To further explore heterogeneity among studies, we calculated I2 statistics. This method quantifies the amount of variation between studies that can be attributed to true variation in effect sizes rather than sampling error. Importantly, I2 does not depend on the number of studies included in the meta-analysis or the metric of the effect size21). An I2 of 25%, 50% and 75% is considered as low, moderate and high heterogeneity, respectively. Heterogeneity was considered to be present if I2 exceeded 25%21). We used Forest plots visualizing study-specific estimates and the pooled fixed and random effects estimators. Statistical hypothesis testing was conducted two sided with a p-value of <0.05 to be considered significant. All statistical analyses were conducted using the statistical software package STATA (Version 16.1 SE, STATA Corporation, College Station, TX, USA).
Results
Study and sample characteristics
Data were presented on a total of 13,277 (range 469–6,328) employees aged 21–70 yr from three Scandinavian countries and various industrial settings. Table 2 summarizes the main study and sample characteristics including the year of publication, name of first author, country in which the study was conducted, study design and period, sample size, response rate as well as age and sex composition. Almost all studies used a cross-sectional study design and one single longitudinal study was identified15, 16).
Table 2. Study characteristics.
| Author & year | Country | Study design | Study period | Sample size (n) | Response rate (%) | Female (%) | Age (yr) |
|---|---|---|---|---|---|---|---|
| Danielsson 2008 | Sweden | Cross-sectional | No data | 469 | 72.5 | 74 | 21–64 |
| Pejtersen 2011 | Denmark | Cross-sectional | 2005 | 2,403 | 62 | 55 | 42.4 (18–59) |
| Danielsson 2014 Danielsson 2016 | Sweden | Longitudinal | 2010–2012 | 1,852 | 57 | 58 | 23–71 |
| Platts 2020 | Sweden | Cross-sectional | 2011–2012 | a: 988 b: 1,237 | 69.5 | a: 61 b: 63 | a: 48.3 b: 47.8 |
| Nielsen 2020 | Norway | Cross-sectional | 2004–2014 | 6,328 | 48 | 57 | 19–70 |
a: employer records; b: self-reported sick leave.
Study findings
Findings of the five included studies indicated effects on sick leave comparing employees working in individual cell offices with those in open-plan offices. Details are presented in Table 3. To summarize, Nielsen and colleagues compared registered sick leave data over 1 yr among 6,328 Norwegian employees who worked in various types of office workspace. Incidence of certified sickness absence was 18% higher in shared offices and 12% higher in open-plan offices, compared to cell offices, independent of age, sex, educational level, and leadership role. Different office types were not related to the number of sick leave days22). Pejtersen found in a Danish sample of 2,403 employees that in offices with more than 6 employees, self-reported average sick days of employees increased by 62% compared to those in cell offices. Employees in shared offices with 2 persons had a 50% increase in sick leave, while an increase of 36% was noted in offices for 3–6 persons23). Bodin Danielsson assessed 469 Swedish employees in 2008 and found a statistically significant difference between the explored office types for the outcome of any sick leave throughout the year2). In addition, her study with 1,852 Swedish employees in 2014 and 2016 described higher absenteeism in small, medium or large open-plan offices, especially in women15). Finally, Platts explored a Swedish sample of 2,225 employees. He found that office type was generally not associated with employer records of number of sickness episodes or days of sickness absence, although the total number of sick leave days was much higher in flex offices than in cell offices24).
Table 3. Studies on various office types and sick leave.
| Author & year | Explored office types | Statistical model | Confounders | Outcome variable | Results |
|---|---|---|---|---|---|
| Danielsson 2008 | Cell office vs. shared (2–3), small open-plan (4–9), medium open-plan (10–24), large open-plan (>24), flex, combi office | Odds ratio | Age, sex, job rank, industry | Any sick leave (self-reported), more than 7 days of sick leave (self-reported), within last 12 months | Sick leave was lower in cell offices and flex offices and highest in medium-sized open-plan offices |
| Pejtersen 2011 | Cell office vs. office with 2, 3–6, >6 employees | Rate ratio | Age, sex, SES, BMI, alcohol, smoking, physical activity | Days of sickness absence within last 12 months (self-reported) | Compared to cell offices, occupants in 2-person offices had 50%, in 3–6-person offices 36%, and in open-plan offices (>6 persons) 62% more sick leave days |
| Danielsson 2014 Danielsson 2016 |
Cell office vs. shared (2–3), small open-plan (4–9), medium open-plan (10–24), large open-plan (>24), flex, combi office | Odds ratio | Age, sex, job rank, industry | ≥2 short sick leave spells of one week or less (self-reported), any long (medically certified) sick leave spell >1 week (self-reported), 7 days of sick leave in total (self-reported), within last 12 months | short sick leave spells were higher in all 3 open-plan offices, especially for men in flex offices. For long sick leave spells, a significantly higher risk was found among women in large open-plan offices and for total number of sick days among men in flex offices. |
| Platts 2020 | Cell office vs. shared (2–3), small open-plan (4–9), medium open-plan (10–24), large open-plan (>24), flex office | Rate ratio | Age, sex, educational level, labour market sector | Number of days and number of episodes of sick leave (employer records), number of days of sick leave (self-reported), within last 12 months | Office type was generally not associated with employer records of number of episodes or days of sick leave, except that the total number of days of leave was higher in flex offices compared to cell offices. In general, office type was not associated with self-reported days of sick leave. |
| Nielsen 2020 | Cell office vs. shared office (2–3), open-plan workspace (>3) | Risk ratio | Survey year, organizational affiliation | ≥1 instance of medically certified sickness absence and the total number of days within last months | employees working in a shared office and an open-plan workspace had significantly higher risk of medically certified sickness absence when compared to employees working in cell offices. Office design was not related to the number of days with absence. |
SES: socioeconomic status: BMI: body mass index.
Quality assessment/Potential bias
Based on the Joanna Briggs Institute (JBI) Critical Appraisal Checklist all five studies were rated with a score of 8 out of 9, indicating a study of high quality (Appendix Table 1). All studies incorporated a wide number and type of potentially confounding characteristics such as age, sex, socio-economic status, BMI, alcohol, smoking, physical activity, and industry. The most frequently used confounder were age and sex (Table 3).
Meta-analysis
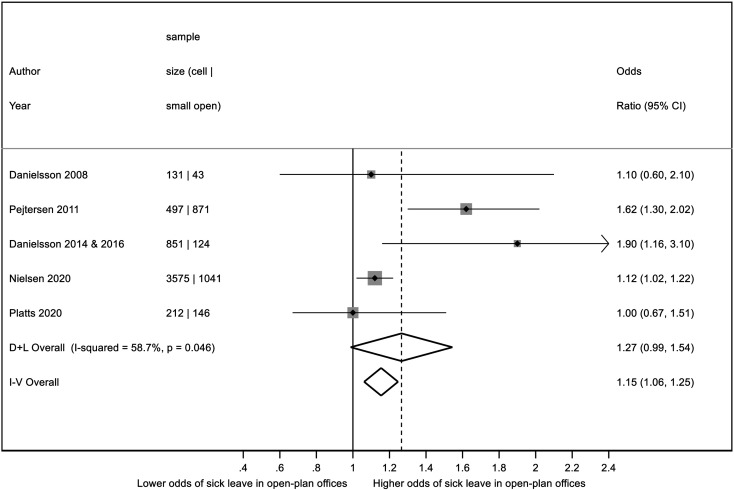
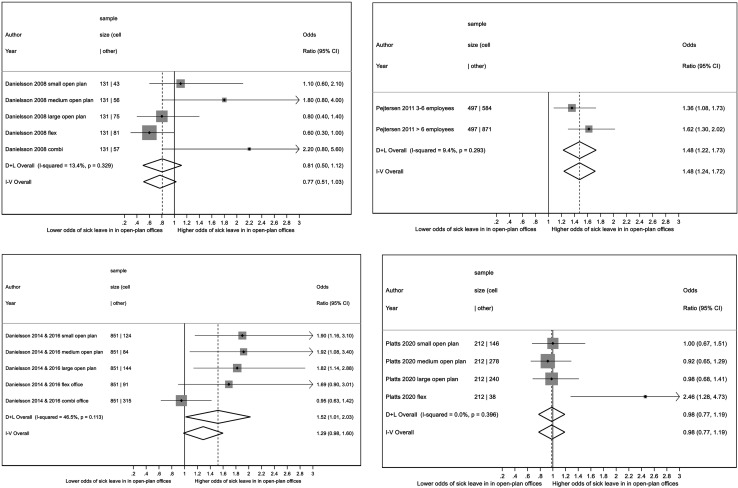
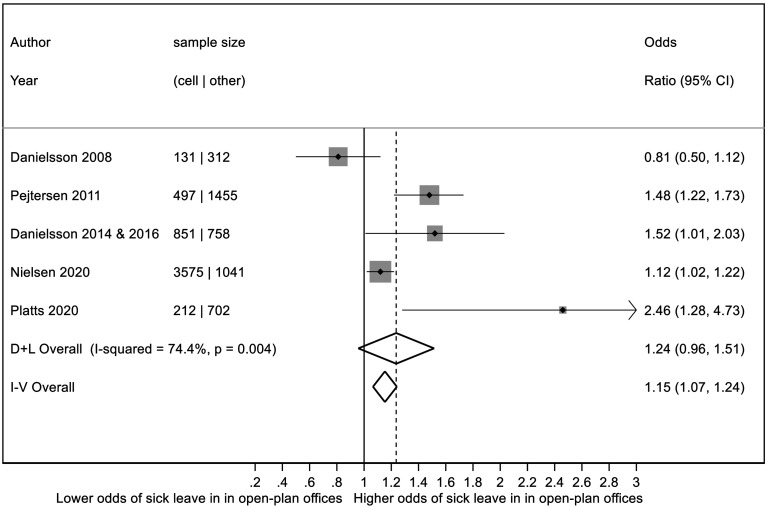
Figures 2, 3, and 4 present the results of the meta-analysis comparing employees in cell offices with those in small open-plan offices (Fig. 2) and those in various kinds of open-plan offices (Figs. 3 and 4).
Fig. 2.
Effect of small open-plan office vs. cell office on total number of sick leave days.
Fig. 3.
Effect of various kinds of open-plan offices (small open-plan office, medium sized open-plan office, large open-plan office, flex office, combi office) vs. cell office on total number of sick leave days, summary estimates for each study separately.
Fig. 4.
Effect of various kinds of open-plan offices (small open-plan office, medium sized open-plan office, large open-plan office, flex office, combi office) vs. cell office on total number of sick leave days, summary estimate over all studies based on within study random effects summary estimates (shown in Fig. 3).
Discussion
This systematic review summarizes current knowledge about the association of open-plan offices and sick leave in the workforce. We meta-analyzed substantial homogeneity in the included articles in terms of the extent to which an open workspace is associated with absence from work. These findings are consistent with the association of open-plan offices and different variables of health and well-being of employees.
Why open-plan offices are associated with higher sickness absence may have several explanations. One reason could be the difference in air-conditioning of offices. While open-plan offices are commonly ventilated by air-condition, single offices might be naturally ventilated by fresh air through the office window which is supported by former studies25, 26). Additionally, air-conditioning is associated with various non-specific symptoms in office workers27, 28). Nevertheless, ventilation status of offices was not assessed as a confounder throughout the included studies. Another reason which is related to the ventilation of offices could be an increased risk for infections in open-plan offices29). This effect is especially very present in the recent corona pandemic particularly for airborne but also for droplet viral infections. A third explanation are acoustic disturbances and noise by colleagues (loud voices, phone calls, talks). In a Danish study, 25% of the participants reported that the noise was so annoying that they had to work overtime to get their tasks done30). Pejtersen and colleagues found out that compared to employees in cell offices, occupants in open-plan offices are more likely to perceive noise, besides thermal discomfort and poor air quality, and they more frequently complain about various symptoms31). Kim et al. explored that the cons of open-plan office layout such as noise outweighed the pros such as better interaction and therefor clearly decreased overall workplace satisfaction of employees10). That association is supported by other studies32) including a higher risk for absenteeism33). A further explanation are different sources of psychosocial stressors including lack of privacy11), lack of autonomy34), or interruptions, among others. Due to the fundamental human desire for privacy35) employees find other strategies to preserve their privacy by choosing other communication channels such as emails. That has clearly an impact on face-to-face communication and collaboration and the desired pros of open office solutions8). Additionally, the fact of more people sharing one office leads to higher peer control, the feeling of reduced personal control and as a consequence to special group dynamics.
These environmental stress factors can be disruptive and contribute to physical and mental health disparities, and may lead to an increasing risk of sick leave in the worst case. Interaction between stress, recovery and immune functions are apparent36,37,38). Thus, a stressful environment may shape short-term and long-term immune response through autonomic function. There are different ways to cope with stress factors. Besides adaption of employees to the strains of open-plan offices, individual strategies such as wearing earphones, working in less busy times, using home office more often, and performing stress-relieving techniques may play an important role to cope with loads and the negative effects24).
In addition, the number of employees per enclosed office space may be a confounding factor as well. The association with adverse health effects and job satisfaction has been explored in cross-sectional and longitudinal study designs before7, 31, 39, 40). Employees in open-plan offices are more often dissatisfied with environmental features than those working in cell offices7, 41) and report lower well-being31). A higher number of employees per enclosed office space is associated with psychosomatic complaints, emotional irritation, and impaired work ability7), which could lead to higher sick leave. Having to deal with all these above mentioned environmental stressors might become a work demand by itself and lead to a dynamic that changes work in open-plan offices itself7).
While the office design is varying regarding the number of employees sharing one room, the architectural and functional features including multiple variables such as thermal conditions, furnishing, IT equipment, lighting, air quality, colors, and textures may influence health, well-being and absenteeism of employees. Especially, participation of employees in designing their own workspace and developing new office concepts as well as taking all these mentioned variables into account may play an additional role to make the implementation successful but is often underrepresented so far.
The recent trend of converting open-plan offices into activity-based flex offices with different facilities and offers to counterbalance the possible negative effects of open-plan offices on employee health and well-being as well as on sick leave should be the focus of further research. The workspace can provide a variety of open, half-open, or enclosed supplemental work areas such as silent areas for concentrated work, project and meeting rooms that enable collaboration, team desks, sit-stand workstations, and telephone rooms as well as break-out and lounge areas for informal meetings. While a recent review found positive outcomes of activity-based flex offices on interaction, communication, control of time and space, and satisfaction with the workspace, limited evidence was seen for the effects on physical and mental health13). The main conclusion of a recent review is that lighting and noise controls are the basic functional, if not humanitarian needs of employees that should be properly managed in open-plan offices42). Additionally, it is important to take into account the status quo of an organization, e.g. if all employees used to work in cell offices before or if shared and open-plan offices were already in place. Finally, the actual needs of employees to sit closer together should be considered. These needs might be different in different job roles, varying from creative jobs that need more interaction to situations when more concentration is needed.
Although open workspaces may be cost-effective, evidence is rising that employees and employers may pay a significant price by reduced well-being, more health disparities and increased sick leave. Due to the fact that many business leaders focus on saving money while introducing open-plan offices, it may be appropriate to consider the possible costs of sick leave associated with these types of office workspace in the business case. Nevertheless, offering employees the opportunity to work in cell offices including the provision of a certain level of privacy and comfort standards may in the end reduce absence rates in certain settings.
Limitations
Our results should be interpreted within the context of several limitations. First, the reported findings have limited generalizability given the small number of eligible studies under review. Nevertheless, other reviews exploring the impact of open-plan offices on employee health and well-being11,12,13) and not on sick leave, have shown similar results Second, the observational nature of the studies in our sample precludes inferences of causality in the instances in which sick leave occurred. Only one single longitudinal study could be found and included in the meta-analysis. Further research should focus on a longitudinal or experimental study design. Third, all five included studies are based on Scandinavian data. That limits generalizability for overall working populations and nationalities. Nevertheless, some sort of generalizability is applicable due to the fact that at least employees of different industries participated. Fourth, besides the study of Platts all findings are based on self-reported data of employees and not on employer-recorded data24). Fifth, no information about office design, besides the number of employees sitting together in one office, was presented. For example, supporting offerings for employees such as health promotion activities, coffee bar, free soft drinks, additional office space, meeting rooms could have an influence on the results and therefore considered as at least confounding variable. Sixth, the results might be biased by quality of the included studies or publication bias. Our quality assessment led to a judgment about the risk of bias. As the assessment showed a high quality on average, the overall risk of bias was seen as being low. In addition, a publication bias should be mentioned as a meta-analysis is often restricted to published data. This is the case in our review as well and therefor our conclusions could be biased due to unpublished nonsignificant studies. The combined effect of significant and nonsignificant studies together, may change the overall conclusions. Nevertheless, both studies of Danielsson2, 15, 16) showed nonsignificant results and the study of Platts24) did not confirm any association of open-plan offices and higher sick leave leading to a well-balanced result of the meta-analysis overall.
Conclusions
There is still a limited number of longitudinal or experimental studies measuring the effects of open-plan offices on sick leave. Variables that might support the well-being of employees in specific job roles should be explored in order to introduce open-plan offices with limited negative effects on health. A “one size fits all” approach will not be the answer to the question if an open-plan office is perceived as resource or as strain.
Appendix Table 1. Joanna Briggs Institute (JBI) Critical Appraisal Checklist for quality assessment
Study characteristics.
| Major components | Danielsson 2008 | Pejtersen 2011 | Danielsson 2014 & 2016 | Platts 2020 | Nielsen 2020 |
|---|---|---|---|---|---|
| 1. Was the sample frame appropriate to address the target population? | yes | yes | yes | yes | yes |
| 2. Were study participants sampled in an appropriate way? | yes | yes | yes | yes | yes |
| 3. Was the sample size adequate? | yes | yes | yes | yes | yes |
| 4. Were the study subjects and the setting described in detail? | no | yes | no | yes | yes |
| 5. Was the data analysis conducted with sufficient coverage of the identified sample? | yes | yes | yes | yes | yes |
| 6. Were valid methods used for the identification of the condition? | yes | yes | yes | yes | yes |
| 7. Was the condition measured in a standard, reliable way for all participants? | yes | yes | yes | yes | yes |
| 8. Was there appropriate statistical analysis? | yes | no | yes | no | yes |
| 9. Was the response rate adequate, and if not, was the low response rate managed appropriately? | yes | yes | yes | yes | no |
| Result (0–9) | 8 | 8 | 8 | 8 | 8 |
References
- 1.Duffy F, Powell K .(1999) The new office, Repr. Conran Octopus, London. [Google Scholar]
- 2.Danielsson CB, Bodin L. (2008) Office type in relation to health, well-being, and job satisfaction among employees. Environ Behav 40, 636–68. [Google Scholar]
- 3.Boutellier R, Ullman F, Schreiber J, Naef R. (2008) Impact of office layout on communication in a science-driven business. R & D Manag 38, 372–91. [Google Scholar]
- 4.Robertson MM, Huang YH, O’Neill MJ, Schleifer LM. (2008) Flexible workspace design and ergonomics training: impacts on the psychosocial work environment, musculoskeletal health, and work effectiveness among knowledge workers. Appl Ergon 39, 482–94. [DOI] [PubMed] [Google Scholar]
- 5.Blok MM, Groenesteijn L, Schelvis R, Vink P. (2012) New ways of working: does flexibility in time and location of work change work behavior and affect business outcomes? Work 41Suppl 1, 5075–80. [DOI] [PubMed] [Google Scholar]
- 6.Nijp HH, Beckers DGJ, van de Voorde K, Geurts SAE, Kompier MAJ. (2016) Effects of new ways of working on work hours and work location, health and job-related outcomes. Chronobiol Int 33, 604–18. [DOI] [PubMed] [Google Scholar]
- 7.Herbig B, Schneider A, Nowak D. (2016) Does office space occupation matter? The role of the number of persons per enclosed office space, psychosocial work characteristics, and environmental satisfaction in the physical and mental health of employees. Indoor Air 26, 755–67. [DOI] [PubMed] [Google Scholar]
- 8.Bernstein ES, Turban S. (2018) The impact of the ‘open’ workspace on human collaboration. Philos Trans R Soc Lond B Biol Sci 373, 373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jaakkola JJK, Heinonen OP. (1995) Shared office space and the risk of the common cold. Eur J Epidemiol 11, 213–6. [DOI] [PubMed] [Google Scholar]
- 10.Kim J, de Dear R. (2013) Workspace satisfaction. The privacy-communication trade-off in open-plan offices. J Environ Psychol 36, 18–26. [Google Scholar]
- 11.De Croon EM, Sluiter JK, Kuijer PP, Frings-Dresen MHW. (2005) The effect of office concepts on worker health and performance: a systematic review of the literature. Ergonomics 48, 119–34. [DOI] [PubMed] [Google Scholar]
- 12.Richardson A, Potter J, Paterson M, Harding T, Tyler-Merrick G, Kirk R, Reid K, McChesney J. (2017) Office design and health: a systematic review. N Z Med J 130, 39–49. [PubMed] [Google Scholar]
- 13.Engelen L, Chau J, Young S, Mackey M, Jeyapalan D, Bauman A. (2019) Is activity-based working impacting health, work performance and perceptions? A systematic review. Build Res Inform 47, 468–79. [Google Scholar]
- 14.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372, n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bodin Danielsson C, Chungkham HS, Wulff C, Westerlund H. (2014) Office design’s impact on sick leave rates. Ergonomics 57, 139–47. [DOI] [PubMed] [Google Scholar]
- 16.Danielsson CB. (2016) Office type’s association to employees’ welfare: three studies. Work 54, 779–90. [DOI] [PubMed] [Google Scholar]
- 17.Ma LL, Wang YY, Yang ZH, Huang D, Weng H, Zeng XT. (2020) Methodological quality (risk of bias) assessment tools for primary and secondary medical studies: what are they and which is better? Mil Med Res 7, 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Munn Z, Moola S, Lisy K, Riitano D, Tufanaru C. (2015) Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. Int J Evid-Based Healthc 13, 147–53. [DOI] [PubMed] [Google Scholar]
- 19.Dickersin K, Berlin JA. (1992) Meta-analysis: state-of-the-science. Epidemiol Rev 14, 154–76. [DOI] [PubMed] [Google Scholar]
- 20.DerSimonian R, Laird N. (1986) Meta-analysis in clinical trials. Control Clin Trials 7, 177–88. [DOI] [PubMed] [Google Scholar]
- 21.Higgins JPT, Thompson SG. (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21, 1539–58. [DOI] [PubMed] [Google Scholar]
- 22.Nielsen MB, Knardahl S. (2020) The impact of office design on medically certified sickness absence. Scand J Work Environ Health 46, 330–4. [DOI] [PubMed] [Google Scholar]
- 23.Pejtersen JH, Feveile H, Christensen KB, Burr H. (2011) Sickness absence associated with shared and open-plan offices—a national cross sectional questionnaire survey. Scand J Work Environ Health 37, 376–82. [DOI] [PubMed] [Google Scholar]
- 24.Platts LG, Seddigh A, Berntson E, Westerlund H. (2020) Sickness absence and sickness presence in relation to office type: an observational study of employer-recorded and self-reported data from Sweden. PLoS One 15, e0231934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Teculescu DB, Sauleau EA, Massin N, Bohadana AB, Buhler O, Benamghar L, Mur JM. (1998) Sick-building symptoms in office workers in northeastern France: a pilot study. Int Arch Occup Environ Health 71, 353–6. [DOI] [PubMed] [Google Scholar]
- 26.Preziosi P, Czernichow S, Gehanno P, Hercberg S. (2004) Workplace air-conditioning and health services attendance among French middle-aged women: a prospective cohort study. Int J Epidemiol 33, 1120–3. [DOI] [PubMed] [Google Scholar]
- 27.Seppänen O, Fisk WJ. (2002) Association of ventilation system type with SBS symptoms in office workers. Indoor Air 12, 98–112. [DOI] [PubMed] [Google Scholar]
- 28.Mendell MJ. (1993) Non-specific symptoms in office workers. A review and summary of the epidemiologic literature. Indoor Air 3, 227–36. [Google Scholar]
- 29.Li Y, Leung GM, Tang JW, Yang X, Chao CY, Lin JZ, Lu JW, Nielsen PV, Niu J, Qian H, Sleigh AC, Su HJ, Sundell J, Wong TW, Yuen PL. (2007) Role of ventilation in airborne transmission of infectious agents in the built environment—a multidisciplinary systematic review. Indoor Air 17, 2–18. [DOI] [PubMed] [Google Scholar]
- 30.Feiring E.(2014) Åpne kontorlandskap stresser hjernen. Tidsskrift for Den norske legeforening. https://tidsskriftet.no/2014/06/legelivet/apne-kontorlandskap-stresser-hjernen. Accessed March 5, 2022 .
- 31.Pejtersen J, Allermann L, Kristensen TS, Poulsen OM. (2006) Indoor climate, psychosocial work environment and symptoms in open-plan offices. Indoor Air 16, 392–401. [DOI] [PubMed] [Google Scholar]
- 32.Passchier-Vermeer W, Passchier WF. (2000) Noise exposure and public health. Environ Health Perspect 108Suppl 1, 123–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Clausen T, Christensen KB, Lund T, Kristiansen J. (2009) Self-reported noise exposure as a risk factor for long-term sickness absence. Noise Health 11, 93–7. [DOI] [PubMed] [Google Scholar]
- 34.Lee RT, Ashforth BE. (1996) A meta-analytic examination of the correlates of the three dimensions of job burnout. J Appl Psychol 81, 123–33. [DOI] [PubMed] [Google Scholar]
- 35.Bernstein ES. (2017) Making transparency transparent. The evolution of observation in management theory. Acad Management Ann 11, 217–66. [Google Scholar]
- 36.Williams DP, Koenig J, Carnevali L, Sgoifo A, Jarczok MN, Sternberg EM, Thayer JF. (2019) Heart rate variability and inflammation: a meta-analysis of human studies. Brain Behav Immun 80, 219–26. [DOI] [PubMed] [Google Scholar]
- 37.Thayer JF, Mather M, Koenig J. (2021) Stress and aging: a neurovisceral integration perspective. Psychophysiology 58, e13804. [DOI] [PubMed] [Google Scholar]
- 38.Peters EMJ, Schedlowski M, Watzl C, Gimsa U. (2021) To stress or not to stress: brain-behavior-immune interaction may weaken or promote the immune response to SARS-CoV-2. Neurobiol Stress 14, 100296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bergström J, Miller M, Horneij E. (2015) Work environment perceptions following relocation to open-plan offices: a twelve-month longitudinal study. Work 50, 221–8. [DOI] [PubMed] [Google Scholar]
- 40.Kaarlela-Tuomaala A, Helenius R, Keskinen E, Hongisto V. (2009) Effects of acoustic environment on work in private office rooms and open-plan offices—longitudinal study during relocation. Ergonomics 52, 1423–44. [DOI] [PubMed] [Google Scholar]
- 41.Bodin C, Danielsson LB. (2009) Difference in satisfaction with office environment among employees in different office types. J Archit Plann Res 26, 3–242. [Google Scholar]
- 42.Lai LWC, Chau KW, Davies SNG, Kwan LML. (2021) Open space office: a review of the literature and Hong Kong case studies. Work 68, 749–58. [DOI] [PubMed] [Google Scholar]