Abstract
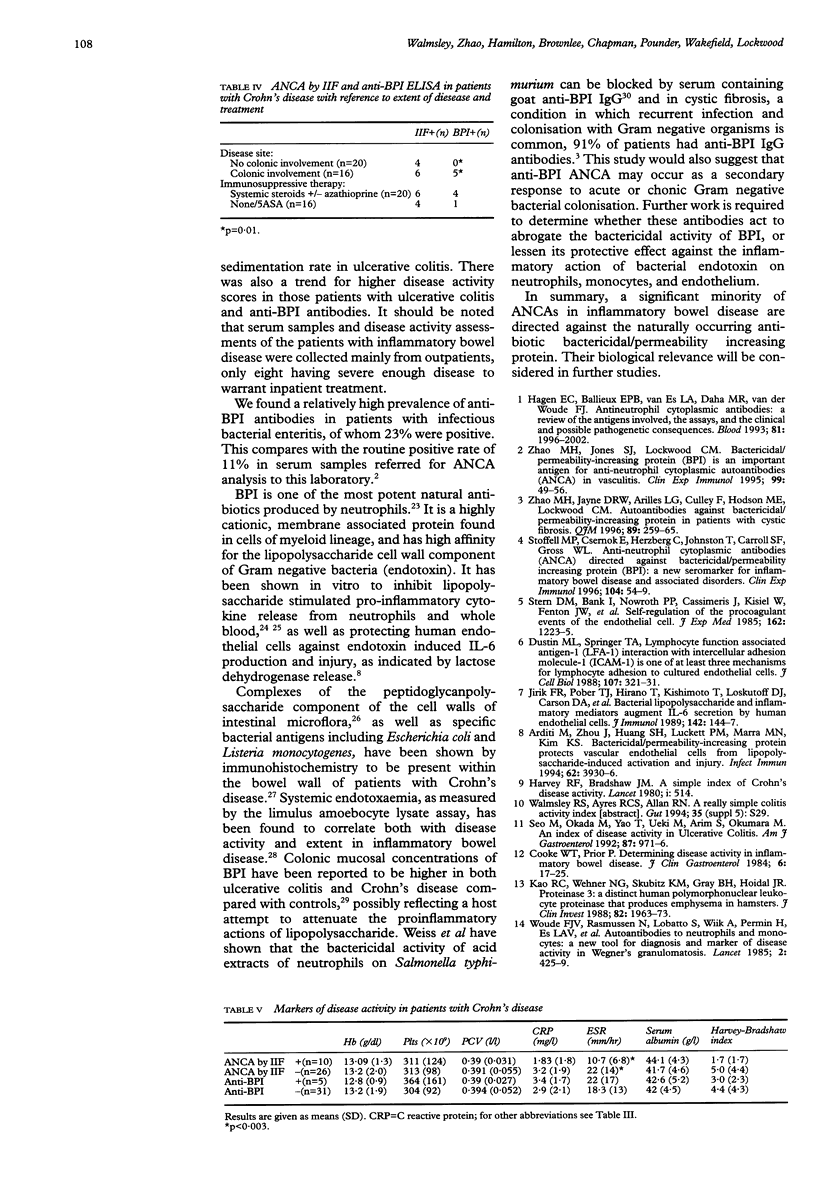
BACKGROUND: Bactericidal/permeability-increasing protein (BPI), a constituent of primary neutrophil granules, is a potent natural antibiotic and an antineutrophil cytoplasm antibody (ANCA) antigen in cases of vasculitis in which the target antigen is neither myeloperoxidase (MPO) nor proteinase-3 (PR3). AIM: To investigate BPI as a possible target antigen for ANCAs in inflammatory bowel disease. METHODS: ANCAs were detected by routine immunofluorescence (IIF) and solid phase enzyme linked immunosorbent assay (ELISA) performed for antibodies to the purified neutrophil granule proteins; MPO, PR3, cathepsin-G, lactoferrin, and BPI in serum samples from 88 patients with inflammatory bowel disease (36 with Crohn's disease, 52 with ulcerative colitis). Thirty patients with bacterial enteritis acted as controls. RESULTS: Significantly more patients with ulcerative colitis were ANCA positive by IIF (60%) than patients with Crohn's disease (28%) or infectious enteritis (23%) (p < 0.001). IgG anti-BPI antibodies were present in 29% of patients with ulcerative colitis, 14% of patients with Crohn's disease, and 23% of patients with infectious enteritis, occurring in 44% of those patients with inflammatory bowel disease who were ANCA positive by IIF. Antibodies to other ANCA antigens were rare. The presence of ANCAs was not related to either disease activity or extent; presence of anti-BPI antibodies was significantly related to both a lower serum albumin concentration (p = 0.001) and a higher erythrocyte sedimentation rate (p = 0.02) in patients with ulcerative colitis, and to colonic involvement in patients with Crohn's disease (p = 0.01). CONCLUSION: BPI is a significant minority target antigen for ANCAs in inflammatory bowel disease that seems related to colonic Crohn's disease and disease activity in ulcerative colitis. Anti-BPI antibodies occur in infectious enteritis.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Arditi M., Zhou J., Huang S. H., Luckett P. M., Marra M. N., Kim K. S. Bactericidal/permeability-increasing protein protects vascular endothelial cells from lipopolysaccharide-induced activation and injury. Infect Immun. 1994 Sep;62(9):3930–3936. doi: 10.1128/iai.62.9.3930-3936.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cambridge G., Rampton D. S., Stevens T. R., McCarthy D. A., Kamm M., Leaker B. Anti-neutrophil antibodies in inflammatory bowel disease: prevalence and diagnostic role. Gut. 1992 May;33(5):668–674. doi: 10.1136/gut.33.5.668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooke W. T., Prior P. Determining disease activity in inflammatory bowel disease. J Clin Gastroenterol. 1984 Feb;6(1):17–25. [PubMed] [Google Scholar]
- Desch C. E., Kovach N. L., Present W., Broyles C., Harlan J. M. Production of human tumor necrosis factor from whole blood ex vivo. Lymphokine Res. 1989 Summer;8(2):141–146. [PubMed] [Google Scholar]
- Duerr R. H., Targan S. R., Landers C. J., Sutherland L. R., Shanahan F. Anti-neutrophil cytoplasmic antibodies in ulcerative colitis. Comparison with other colitides/diarrheal illnesses. Gastroenterology. 1991 Jun;100(6):1590–1596. doi: 10.1016/0016-5085(91)90657-7. [DOI] [PubMed] [Google Scholar]
- Dustin M. L., Springer T. A. Lymphocyte function-associated antigen-1 (LFA-1) interaction with intercellular adhesion molecule-1 (ICAM-1) is one of at least three mechanisms for lymphocyte adhesion to cultured endothelial cells. J Cell Biol. 1988 Jul;107(1):321–331. doi: 10.1083/jcb.107.1.321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gardiner K. R., Halliday M. I., Barclay G. R., Milne L., Brown D., Stephens S., Maxwell R. J., Rowlands B. J. Significance of systemic endotoxaemia in inflammatory bowel disease. Gut. 1995 Jun;36(6):897–901. doi: 10.1136/gut.36.6.897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagen E. C., Ballieux B. E., van Es L. A., Daha M. R., van der Woude F. J. Antineutrophil cytoplasmic autoantibodies: a review of the antigens involved, the assays, and the clinical and possible pathogenetic consequences. Blood. 1993 Apr 15;81(8):1996–2002. [PubMed] [Google Scholar]
- Harvey R. F., Bradshaw J. M. A simple index of Crohn's-disease activity. Lancet. 1980 Mar 8;1(8167):514–514. doi: 10.1016/s0140-6736(80)92767-1. [DOI] [PubMed] [Google Scholar]
- Jirik F. R., Podor T. J., Hirano T., Kishimoto T., Loskutoff D. J., Carson D. A., Lotz M. Bacterial lipopolysaccharide and inflammatory mediators augment IL-6 secretion by human endothelial cells. J Immunol. 1989 Jan 1;142(1):144–147. [PubMed] [Google Scholar]
- Kao R. C., Wehner N. G., Skubitz K. M., Gray B. H., Hoidal J. R. Proteinase 3. A distinct human polymorphonuclear leukocyte proteinase that produces emphysema in hamsters. J Clin Invest. 1988 Dec;82(6):1963–1973. doi: 10.1172/JCI113816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klasen I. S., Melief M. J., van Halteren A. G., Schouten W. R., van Blankenstein M., Hoke G., de Visser H., Hooijkaas H., Hazenberg M. P. The presence of peptidoglycan-polysaccharide complexes in the bowel wall and the cellular responses to these complexes in Crohn's disease. Clin Immunol Immunopathol. 1994 Jun;71(3):303–308. doi: 10.1006/clin.1994.1090. [DOI] [PubMed] [Google Scholar]
- Levy O., Ooi C. E., Elsbach P., Doerfler M. E., Lehrer R. I., Weiss J. Antibacterial proteins of granulocytes differ in interaction with endotoxin. Comparison of bactericidal/permeability-increasing protein, p15s, and defensins. J Immunol. 1995 May 15;154(10):5403–5410. [PubMed] [Google Scholar]
- Liu Y., van Kruiningen H. J., West A. B., Cartun R. W., Cortot A., Colombel J. F. Immunocytochemical evidence of Listeria, Escherichia coli, and Streptococcus antigens in Crohn's disease. Gastroenterology. 1995 May;108(5):1396–1404. doi: 10.1016/0016-5085(95)90687-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ooi C. E., Weiss J., Doerfler M. E., Elsbach P. Endotoxin-neutralizing properties of the 25 kD N-terminal fragment and a newly isolated 30 kD C-terminal fragment of the 55-60 kD bactericidal/permeability-increasing protein of human neutrophils. J Exp Med. 1991 Sep 1;174(3):649–655. doi: 10.1084/jem.174.3.649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oudkerk Pool M., Ellerbroek P. M., Ridwan B. U., Goldschmeding R., von Blomberg B. M., Peña A. S., Dolman K. M., Bril H., Dekker W., Nauta J. J. Serum antineutrophil cytoplasmic autoantibodies in inflammatory bowel disease are mainly associated with ulcerative colitis. A correlation study between perinuclear antineutrophil cytoplasmic autoantibodies and clinical parameters, medical, and surgical treatment. Gut. 1993 Jan;34(1):46–50. doi: 10.1136/gut.34.1.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saxon A., Shanahan F., Landers C., Ganz T., Targan S. A distinct subset of antineutrophil cytoplasmic antibodies is associated with inflammatory bowel disease. J Allergy Clin Immunol. 1990 Aug;86(2):202–210. doi: 10.1016/s0091-6749(05)80067-3. [DOI] [PubMed] [Google Scholar]
- Seibold F., Weber P., Klein R., Berg P. A., Wiedmann K. H. Clinical significance of antibodies against neutrophils in patients with inflammatory bowel disease and primary sclerosing cholangitis. Gut. 1992 May;33(5):657–662. doi: 10.1136/gut.33.5.657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seo M., Okada M., Yao T., Ueki M., Arima S., Okumura M. An index of disease activity in patients with ulcerative colitis. Am J Gastroenterol. 1992 Aug;87(8):971–976. [PubMed] [Google Scholar]
- Stern D. M., Bank I., Nawroth P. P., Cassimeris J., Kisiel W., Fenton J. W., 2nd, Dinarello C., Chess L., Jaffe E. A. Self-regulation of procoagulant events on the endothelial cell surface. J Exp Med. 1985 Oct 1;162(4):1223–1235. doi: 10.1084/jem.162.4.1223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stoffel M. P., Csernok E., Herzberg C., Johnson T., Carroll S. F., Gross W. L. Anti-neutrophil cytoplasmic antibodies (ANCA) directed against bactericidal/permeability increasing protein (BPI): a new seromarker for inflammatory bowel disease and associated disorders. Clin Exp Immunol. 1996 Apr;104(1):54–59. doi: 10.1046/j.1365-2249.1996.d01-654.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss J., Victor M., Stendhal O., Elsbach P. Killing of gram-negative bacteria by polymorphonuclear leukocytes: role of an O2-independent bactericidal system. J Clin Invest. 1982 Apr;69(4):959–970. doi: 10.1172/JCI110535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao M. H., Jayne D. R., Ardiles L. G., Culley F., Hodson M. E., Lockwood C. M. Autoantibodies against bactericidal/permeability-increasing protein in patients with cystic fibrosis. QJM. 1996 Apr;89(4):259–265. doi: 10.1093/qjmed/89.4.259. [DOI] [PubMed] [Google Scholar]
- Zhao M. H., Jones S. J., Lockwood C. M. Bactericidal/permeability-increasing protein (BPI) is an important antigen for anti-neutrophil cytoplasmic autoantibodies (ANCA) in vasculitis. Clin Exp Immunol. 1995 Jan;99(1):49–56. doi: 10.1111/j.1365-2249.1995.tb03471.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Woude F. J., Rasmussen N., Lobatto S., Wiik A., Permin H., van Es L. A., van der Giessen M., van der Hem G. K., The T. H. Autoantibodies against neutrophils and monocytes: tool for diagnosis and marker of disease activity in Wegener's granulomatosis. Lancet. 1985 Feb 23;1(8426):425–429. doi: 10.1016/s0140-6736(85)91147-x. [DOI] [PubMed] [Google Scholar]



