Abstract
Question
Alexithymia has been found to be modifiable through treatment, with associated clinical benefits. Recent studies have begun to test the potential of mindfulness-based interventions to reduce alexithymia, using skills-based, group training to improve non-judgemental, present-moment awareness. The objective of this review therefore was to conduct a systematic synthesis to assess the current state of knowledge about the effect of mindfulness-based interventions on alexithymia to inform clinical practice.
Study selection and analysis
We carried out a systematic review of the literature and found four randomised controlled trials of the effect of mindfulness-based interventions on alexithymia, with a combined total of 460 participants.
Findings
A random-effects meta-analysis, combining study endpoint data, showed a statistically significant effect of mindfulness-based treatment on alexithymia (Toronto Alexithymia Scale) compared with the control group (mean difference=−5.28, 95% CI −9.28 to −1.28, p=0.010). Subgroup analysis was conducted to investigate sources of heterogeneity (I2=52%). Heterogeneity was reduced when the meta-analysis was restricted to interventions of a similar duration (3 months or less).
Conclusions
Findings from our study should be replicated in further research with larger samples; however, the results indicate that mindfulness-based interventions may be an effective treatment in reducing alexithymia.
Keywords: adult psychiatry
Background
Alexithymia is a trait characterised by difficulties in identifying and communicating emotions, and by an externally orientated thinking style,1 arising from a deficiency in the neural processing of emotions.2 Prevalence rates range from 7% to 13% in community samples, but can be several times higher in clinical samples.3 Alexithymia has been found to be associated with psychological disorders, such as anxiety,4 depression5 6 and general psychopathological distress,7 and with maladaptive behaviours including alcohol dependence,8 eating disorders9 and self-harm.10 The presence of alexithymia can present a barrier to psychotherapeutic treatment,11 because the inability of the patient to communicate emotions may induce a negative reaction in the therapist.12
There has been a debate as to whether alexithymia is a state-dependent response to trauma or depression13 14 or a stable personality trait.15 16 The growing consensus is that alexithymia is a trait with relative, rather than absolute, stability, which means that it can be modified through treatment, but that differences between individuals remain largely the same over time.17 A further consideration is whether any reduction in alexithymia as a result of treatment has any effect on the individual’s health or well-being. There is some indicative evidence that decreases in alexithymia may be beneficial: one study found that reduced alexithymia following therapy was significantly associated with a reduction in cardiac events in patients with coronary heart disease18 and a second study reported an association between reduced alexithymia and improvements in interpersonal problems.19 Taken together, this evidence suggests both that it is possible to reduce alexithymia through treatment and also that a reduction in alexithymia may be of positive benefit to the individual. Identifying effective treatment for alexithymia is therefore an important area for further investigation.
A systematic review assessing changes in alexithymia found that studies involving psychological interventions that targeted alexithymic symptoms directly were more likely to report significant reductions in alexithymia than those studies where the intervention was not specifically designed for alexithymia.20 The interventions that resulted in significant falls in alexithymia tended to use skills-based training designed to increase awareness of bodily sensations and associated emotions. In addition, they often involved group therapy, which may allow alexithymic participants to observe and mirror the way others describe their feelings and experiences.11 These elements are core to mindfulness-based training courses, such as mindfulness-based stress reduction (MBSR)21 and mindfulness-based cognitive therapy,22 in which participants are taught to pay attention to whatever is happening in the present moment, through exercises designed to increase awareness of bodily sensation and non-judgemental observation of thoughts and feelings. Mindfulness-based training has been found to be effective against depression, anxiety and stress in clinical samples23 24 and against psychological distress in community samples.25 Although mindfulness and alexithymia have been shown to be related constructs, with high alexithymia significantly correlated with low levels of mindfulness,26 27 Cameron et al’s20 review did not identify any study that explicitly tested mindfulness-based interventions on alexithymia. However, a small number of studies published since Cameron et al’s20 review in 2014 indicate that mindfulness-based training might be also effective in reducing alexithymia,28 29 possibly through the mechanism of enhanced neural processing associated with the identification of bodily sensations, termed interoception.30 31
Objective
We therefore aimed to carry out a systematic review and meta-analysis of randomised controlled trials (RCTs) of mindfulness-based interventions to provide a quantitative assessment of the effect of mindfulness-based training on alexithymia.
Study selection and analysis
The protocol for this systematic review was registered on PROSPERO (CRD42017071924).
Search strategy
Electronic databases (PsycINFO, Medline, Web of Science and Cochrane CENTRAL) were searched from inception until 25 September 2017, using the following terms: ‘affective symptoms’ (MeSH) OR ‘alexithymi*’ AND mindful* AND (intervention* OR random* OR ‘clinical trial*’ OR training*). No restrictions were applied regarding language or date of publication, but we considered only articles published in peer-reviewed journals to increase the quality of the included studies. Abstracts were screened independently by two reviewers and disagreements were solved via discussion with a third member of the review team. The same two reviewers independently extracted the data from the included studies.
Study selection
We included only RCTs of any duration comparing mindfulness-based interventions with any control condition (pharmacological or psychological intervention, wait-list, treatment as usual), in which alexithymia was measured in both the experimental and control groups, using a validated measure. To be included, mindfulness training had to be a component or the whole of the intervention. No exclusion criteria were set regarding age, diagnosis or other participant demographics.
Outcomes
The primary outcome was the severity of alexithymia symptoms at study endpoint. We also carried out secondary analyses of severity of alexithymia symptoms within 3 months. We decided to choose this time point because it is common to the included studies and is closest to the standard length of an MBSR programme.21 Additional analyses at other time points were conducted where the study period exceeded 3 months.
Data extraction
Data from the studies were extracted using a standardised form. Extracted information included study sample characteristics, details of the intervention (such as duration, activities undertaken and method of delivery and number), severity of symptoms and timings of measurement.
Risk of bias assessment
The risk of bias was assessed using the Cochrane tool as reported in the Cochrane handbook.32 This enables researchers to assess as high, low or unclear seven different types of risk that might cause the effect of treatment in individual studies to be overestimated or underestimated. Risk of bias assessment was carried out independently by two reviewers and any disagreement resolved through consensus or by discussion with another member of the review team.
Statistical analysis
As our outcomes were continuous, we calculated the pooled mean difference (MD) with corresponding 95% CIs, as appropriate. We considered a p value of less than 0.05 and a 95% CI that does not cross the line of no effect as statistically significant. The standardised mean difference (SMD) was also calculated as a measure of the effect size. In accordance with the study protocol, we used a random-effects model because it has the highest generalisability for empirical examination of summary effect measures in meta-analyses.33 However, as recommended by the Cochrane Handbook for Systematic Reviews of Interventions32 (10.4.4.1) when concerned about the influence of small study effects on the results of a meta-analysis with between-study heterogeneity, we examined the robustness by comparing the fixed-effect model and the random-effects model. We reported any material differences between the models. In the case that a study included multiple intervention cohorts, we decided to combine the outcome data from all the intervention cohorts, using the method recommended by Higgins and Green.32 We planned to conduct subgroup analyses if there were large differences between the interventions or between participant characteristics. All analyses were carried out using RevMan V.5.3.34
Findings
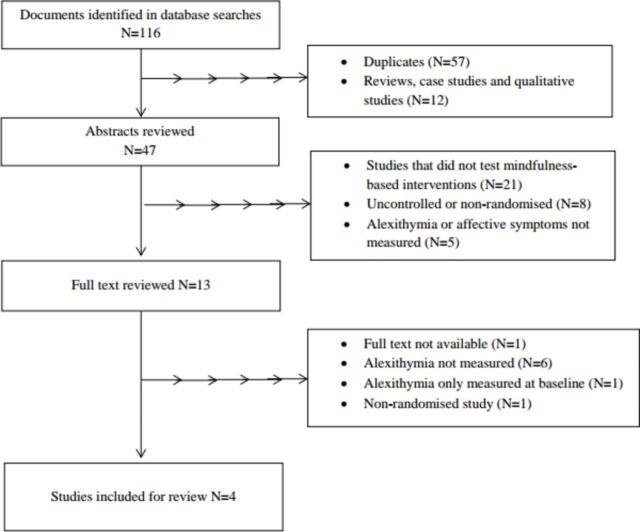
In total, 116 articles were retrieved from the database search, which resulted in 59 individual studies after duplicates were removed (figure 1). After screening, a total of four studies met the criteria, all published since 2010, with a combined total sample of 460 participants.35–38 A full description of the four studies is given in table 1.
Figure 1.
Flow chart of the study selection process.
Table 1.
Results of systematic review of literature on the effect of mindfulness-based interventions on alexithymia
| Author | Study type | Population (N) | Age and sex | Intervention | Control | Measures | Time measurements taken | Results |
| Bornemann and Singer35 | RCT | Volunteers from the general public in Germany in good health and with no prior meditation experience. People with TAS20 scores of >60 were excluded n=318 |
Mean=40.8 (9.3) 59% Female |
Three mental training modules, each 3 months long, involving a 3-day silent retreat, 13 weeks of weekly 2-hour group sessions and 30 min of daily practice. The Presence module was about directing attention to the present moment, the Affect module about approaching difficult emotions with acceptance and the Perspective module about metacognition, observing thoughts and reframing experiences. There were three intervention groups: groups 1 and 2 did all three modules over 9 months but in a different order, group 3 did just the Affect module for 3 months | No training | TAS20 and subscales1
Heartbeat perception task and ECG |
Before the intervention and at 3, 6 and 9 months (after each module) | Alexithymia decreased more in the intervention groups than the control group from T0 to T3 (p<0.001, d=−0.331) and T0 to T2 (p=0.026, d=−0.155) but not T0 to T1 (p=0.143, d=−0.166). The effect at T3 was significant for all TAS subscales. Post hoc tests showed that the decreases in TAS scores were caused by the Presence and Affect modules but not the Perspective module Heartbeat perception accuracy increased more in the intervention groups than the control group from T0 to T3 (p=0.017, d=0.273) and T0 to T2 (p=0.020, d=0.173) but not T0 to T1 (p=0.220, d=0.111) Change in heartbeat perception accuracy between T0 and T1 were negatively correlated with changes in TAS20 (p=0.002). The correlation was significant for those who had taken the Presence training but not for those who had taken the Affect training |
| de la Fuente Arias et al 36 | RCT | Students from the University of Almeria with no experience of meditation or yoga n=46 |
M=23.47 (6.34) 85% F |
10 weekly 1.5-hour mindfulness/meditation training sessions adapted from the MBSR programme,21 combined with individual practice | Wait-list | TAS20 and subscales1
Social skills scale51 |
Before and after the intervention | Pre/post tests show significant changes in TAS20 in the intervention group (DIF p<0.001, DDF, EOT and Total TAS p<0.01). The size of the change was 20% decrease in DIF (d=0.32) and DDF (d=0.39), 22.2% in EOT (d=0.55) and 20.60% in total TAS (d=0.47). The control group’s TAS20 did not change significantly. The difference in TAS20 scores between the groups was not significant at baseline (p=0.321) or post intervention (t=0.600, p=0.552) There were no significant differences in social skills in the experimental and control groups at baseline, but post intervention social skills were significantly higher (p≤0.001) in the experimental group and there was a significant pre/post increase in social skills in the experimental group (total social skills, p≤0.001) |
| Santarnecchi et al 37 | RCT and MRI study |
Right-handed members of the public in Italy, with no prior meditation or mindfulness experience and in good physical and mental health n=48 |
Intervention group: 31 (±4) Control group: 30 (±4) 52% F |
8-week MBSR programme21 involving weekly 2.5-hour group sessions and daily individual practice | Wait-list | TAS201
Penn State Worry Questionnaire52 State-Trait Anxiety Inventory53 Beck Depression Inventory II54 Mindfulness Attention Awareness Scale39 MRI scans measured grey matter volume and cortical thickness |
Before and after the intervention | There was a significant reduction in TAS20 in the intervention group (p=0.004) and no significant change in the control group. There was no significant change in MAAS in either group There was a significant negative correlation between alexithymia level and insula cluster thickness values (r=−0.712, p<0.01) in the intervention group post training There were significant reductions in the intervention group in worry (p=0.012), state anxiety (p=0.031) and depression (p=0.046) but not in the control group |
| Viding et al 38 | RCT | Adult women attending any of 4 healthcare centres in Sweden with burnout/exhaustion symptoms, excluding individuals with drug or alcohol abuse or severe depression n=48 |
M=53.8 (8.15) 100% F |
A package of six cultural activities, including mindfulness (focused on breathing, body awareness and awareness of thoughts and feelings), dance, theatre, film and drawing, each delivered in two 90 min sessions | Standard care involving physiotherapy | TAS20 and subscales1
Karolinska Exhaustion Disorder Scale55 Sense of Coherence56 Single item measure of self-rated health |
Baseline, 3 months (the length of the programme) and 6 months (follow-up) | There was a significantly greater decrease in the intervention group compared with the control group in total TAS (p=0.007), DDF (p=0.004) and DIF (p=0.051) at 6 months relative to baseline There was a significant decrease in exhaustion and self-reported health (p≤0.001) in the intervention group compared with the control group, but not in sense of coherence |
MAAS, Mindful Attention Awareness Scale; MBSR, Mindfulness-Based Stress Reduction; RCT, randomised controlled trial; TAS20, 20-item Toronto Alexithymia Scale; DIF, Difficulty Identifying Feelings subscale of the TAS20; DDF, Difficulty Describing Feelings subscale of the TAS20; EOT, Externally Orientated Thinking subscale of the TAS20.
Sixty-five per cent of the total sample was female. The mean age ranged from 23.5 to 53.8, with one study restricting the age range of eligible participants to between 20 and 55.35 Three studies were drawn from non-clinical samples35–37 and two studies35 37 additionally excluded individuals in poor psychological health. Participants in the fourth study were women with symptoms of burnout or exhaustion.38 Three of the studies explicitly excluded people with prior experience of meditation.35–37
Two studies compared mindfulness-based interventions based on the MBSR programme, delivered over 8 weeks37 and 10 weeks,36 with wait-list. A third study tested a bespoke mindfulness-based programme of contemplative mental training delivered in three different 3-month modules.35 In this study, two intervention cohorts participated in all three modules in a different order, one intervention cohort only took one 3-month module and a control group had no training. Finally, the fourth study tested a 3-month package of six different cultural activities (including mindfulness training, and also dance, theatre and art).38 This was compared with standard care, consisting of physiotherapy and light physical exercise. This was the only study to include a follow-up assessment at 6 months, 3 months after the end of the intervention.38 All four studies measured alexithymia using the Toronto Alexithymia Scale (TAS20).1 In one study,35 individuals with a TAS20 score of over 60 were excluded. Other variables measured are described in table 1. Only one study37 measured mindfulness, using the Mindful Attention Awareness Scale (MAAS).39
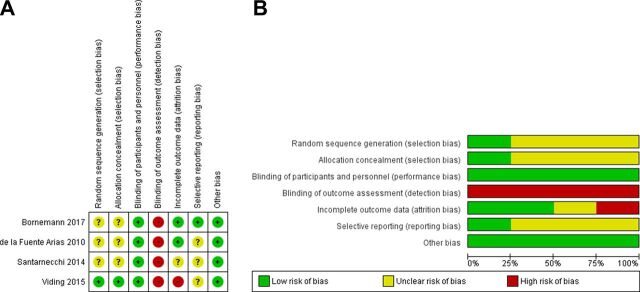
The assessment of risk of bias is set out in figure 2. The main risk of bias was considered to be in the blinding of outcome assessment, which is difficult to achieve with a self-report outcome measure.
Figure 2.
(A) Risk of bias summary: review authors’ judgements about each risk of bias item for each included study. (B) Risk of bias graph: review authors’ judgements about each risk of bias item presented as percentages across all included studies.
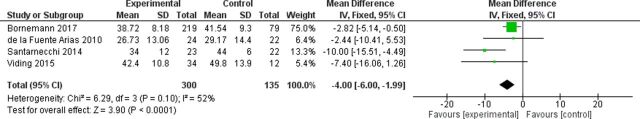
A random-effects meta-analysis was carried out to assess mean difference in TAS20 scores between the experimental and control groups at study endpoint. Study endpoint was interpreted as the final data collection. In two studies, the study endpoint coincided with the end of treatment for all participants.36 37 In Bornemann and Singer,35 data from the three experimental cohorts at the end of their respective treatment periods were combined. In the case of Viding et al,38 the study endpoint occurred at the 6-month follow-up assessment. In order to make use of all the available evidence, subgroup analyses were carried out to assess mean difference in TAS20 scores between the experimental and control groups at different time points post baseline: at T1 (within 3 months post baseline), T2 (6 months post baseline) and T3 (9 months post baseline). The results are set out in figure 3.
Figure 3.
Random-effects meta-analysis of mean and standardised mean difference in alexithymia at study end and at different time points.
Combining the results from all studies at study endpoint resulted in a significant model (MD=−5.28, 95% CI −9.28 to −1.28, p=0.010, 435 participants). This difference corresponded to a SMD of −0.48, indicating a moderate effect size (figure 3), but the heterogeneity between the studies was moderate to high (I2=52%). At T1, the results from the four studies show that although alexithymia levels were lower in the experimental group than the control group, the overall effect of treatment was not significant, with significant heterogeneity (MD=−4.59, 95% CI −9.31 to 0.12, p=0.06; I2=64%, 441 participants). Excluding Bornemann and Singer,35 on the grounds that the intervention was not complete for most participants at T1, produced a significant model (MD=−6.91, 95% CI −11.52 to −2.30, p=0.003, 134 participants), and reduced heterogeneity to I2=19%. The difference between experimental and control groups at T2, based on two studies, was not significant (MD=−3.04, 95% CI −7.24 to 1.16, p=0.16, 276 participants). Finally, Bornemann and Singer,35 the only study to take measurements at T3, reported a significant difference between the experimental and control groups at that time point (MD=−2.84, 95% CI −5.30 to −0.38, p=0.02, 226 participants).
One possible cause of heterogeneity is the difference between the interventions. While three of the interventions tested centred on mindfulness-based training, in Viding et al 38 the mindfulness element accounted for only one-sixth of the total intervention. A sensitivity analysis was conducted on the primary outcome of mean alexithymia at study endpoint, excluding Viding et al.38 This exclusion increased the heterogeneity of the model, but it remained significant (I2=65%, MD=−4.99, 95% CI −9.84 to −0.13, p=0.04, 389 participants).
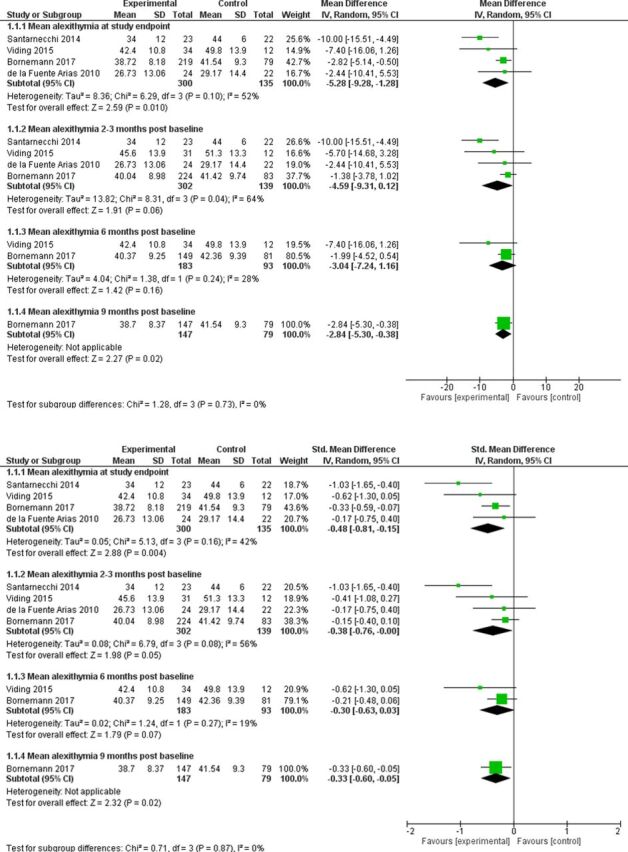
Finally, for comparison purposes, a fixed-effects meta-analysis was carried out on the primary outcome of the mean difference in TAS20 scores between the experimental and control groups at study endpoint (figure 4). This resulted in a significant model (MD=−4.00, 95% CI −6.00 to −1.99, p<0.0001, I2=52%, 435 participants).
Figure 4.
Fixed-effects meta-analysis of mean difference of alexithymia at study endpoint.
Conclusions and clinical implications
This systematic review and meta-analysis examined the effect of mindfulness-based interventions on alexithymia. The combined results from the four RCTs found in the literature indicate that mindfulness-based interventions significantly reduce alexithymia, compared with a control condition, at the end of the study period. It is not clear if the observed effect can last beyond 9 months (ie, the length of the longest intervention in the included trials).
Nature of the intervention
The studies differed in the length of the intervention offered, with Bornemann and Singer’s35 9-month programme considerably longer than the interventions tested in the other studies and also the conventional length of a MBSR programme. However, excluding Bornemann and Singer35 from the meta-analysis of outcomes at 3 months, on the grounds that the intervention was not complete for most participants at that point, produced a significant effect of mindfulness-based training, suggesting that it is the content of the intervention rather than its length that is important for alexithymia. This is in line with non-randomised evidence, which suggests that even a short intervention can have a positive effect. Byrne et al 28 tested a 2-week mindfulness-based intervention on a group of sex offenders in prison and found that alexithymia decreased significantly in the intervention group compared with the control group over the short period of the intervention.
Mechanisms
The intervention tested by Bornemann and Singer35 gives an opportunity to deconstruct the elements of a mindfulness-based intervention since it was explicitly divided into three modules covering awareness of the present moment and particularly of bodily sensations (Presence), accepting difficult emotions with loving kindness (Affect) and observing thoughts and learning reappraisal skills (Perspective). The authors found that a significant decrease in alexithymia was attributable only to the Presence and Affect modules, and not to the Perspective module. The mindfulness-based class that formed part of the intervention tested in Viding et al 38 would appear to be similar in content to the Presence module in Bornemann and Singer’s35 study, as it was focused on breathing and awareness of the body, thoughts and feelings. Taken together, these studies may indicate that increased awareness of present experience, particularly awareness of bodily sensations, may be one mechanism by which alexithymia is reduced. Alexithymia (awareness of emotional experience) has been found to be strongly related to interoception (awareness of bodily experience)40 and improvement in alexithymia symptoms has been associated with increased heartbeat perception accuracy.35 Furthermore, Santarnecchi et al 37 reported a significant correlation between the decrease in alexithymia and an increase in right insula thickness, an area of the brain, which is involved in both emotional and bodily awareness.41 Interestingly, however, Bornemann and Singer35 found that the significant correlation between the decrease in alexithymia and increased heartbeat awareness was only observed among those who had taken part in the Presence training module and not among those who had taken the Affect training module. The authors conclude that the significant decrease in alexithymia observed among participants in the Presence module may be attributable to an increase in interoception, but that reduction in alexithymia in participants in the Affect module, which focused on the acceptance of difficult emotions, may be attributable to a different mechanism.
It might be assumed that another mechanism by which alexithymia is reduced following mindfulness-based training is an increase in trait mindfulness. In fact, the only one of the four studies included in this review to measure trait mindfulness37 reported no significant change in mindfulness as a result of the intervention, a surprising finding that runs counter to other evidence.24 The authors attribute this result to the use of the MAAS.39 The items in the MAAS focus on the respondent’s ability to pay attention to what is happening in the present moment (eg, “I drive places on automatic pilot and then wonder why I went there”) rather than the emotional and non-judgemental aspect of mindfulness captured in other measures.42 This conception of mindfulness, which places little emphasis on identifying or describing feelings, might explain the lower correlations between the MAAS and the TAS20 than between the TAS20 and other measures of mindfulness, such as the Kentucky Inventory of Mindfulness Skills and the Five Facet Mindfulness Questionnaire.26 43 Santarnecchi et al’s37 findings might imply that the mechanism of change through which mindfulness-based interventions operate on trait mindfulness and alexithymia is not based on the attentional aspect of mindfulness, but more research and larger study samples are needed to test this hypothesis further.
Comparison with other interventions
One question that arises from the results of this review is how a combined mean difference of five points on the TAS20 scale between intervention and control groups post mindfulness-based training compares with the effect of other types of intervention on alexithymia. There is some evidence from uncontrolled pre–post studies to support the use of other therapies in treating alexithymia, including cognitive behavioural therapy (CBT),44 45 psychodynamic group therapy7 and voice movement therapy.46 An RCT comparing the effect of a psychoeducation and cognitive restructuring programme for patients with cancer with standard medical care resulted in a much greater difference in mean TAS20 between the groups after treatment than found in the current meta-analysis (MD=−17.29, CI −22.52 to −12.06).17 However, the difference was due in large part to a significant increase in TAS20 in the control group, which may be a specific feature of the oncological population or, as the authors suggest, may have been a secondary effect of the increase in anxiety associated with illness.
Clinical implications
This review has identified a statistically significant effect of mindfulness-based interventions on alexithymia. It is worth noting that in all the studies, the baseline level of alexithymia was relatively low and below the clinical threshold.47 It is possible that the effect of a mindfulness-based intervention might be still greater in clinical populations where baseline alexithymia may be higher.3 Bornemann and Singer35 observed larger falls in TAS20 scores among those who had higher alexithymia at baseline (above 51) than those with low alexithymia.
Alexithymia has been described as a transdiagnostic factor associated with a range of disorders.48 Using mindfulness-based training to reduce alexithymia might therefore be a means of improving the efficacy of subsequent condition-specific treatments. An increased awareness of, and ability to talk about, emotions might, for example, enable better engagement with psychotherapy.12 More evidence is needed to establish whether a reduction in alexithymia is directly and causally related to improvements in health. The studies reviewed here reported significant improvements post intervention in some measures of psychological health (eg, worry, anxiety and depression37; exhaustion and self-reported health38) but not others (eg, sense of coherence38). Where improvements were observed, it is not possible to say whether they are related to the changes in alexithymia or merely concurrent. Further research is needed, particularly to test the implications of a decrease in alexithymia on psychological health.
As far as non-clinical populations are concerned, mindfulness-based interventions may be effective in reducing alexithymia as a preventative measure. One advantage of mindfulness-based interventions is that they can be delivered in community settings and are becoming increasingly popular as a means of reducing non-clinical levels of stress.25 High alexithymia per se is unlikely to be an explicit reason someone might seek treatment but is rather a comorbid, and potentially causal, feature of many other presenting behaviours or psychological features.47 Community-based, universal interventions, therefore, may be a means of preventing future problems by improving alexithymic symptoms.
Limitations
There were several limitations in this review. First, the conclusions are based on a combined sample size of just 460 participants. We focused only on RCTs, excluding other, non-randomised28 and uncontrolled29 49 trials of the effect of mindfulness-based interventions on alexithymia. Although this limited the number of included studies to four, it meant that the conclusions were based on the highest quality evidence available. Second, the heterogeneity between the studies was found to be moderate to high. We conducted sensitivity analysis to assess whether this was due to the differences in either the content or the length of the interventions. The results showed that heterogeneity was higher when studies with interventions of different lengths were combined. It should be noted, however, that the only study that tested an intervention of over 3 months’ duration35 accounted for nearly 70% of the combined sample. The observed heterogeneity, therefore, may be due to the inclusion of studies with small sample sizes in the meta-analysis.50 Future RCTs with larger samples could usefully explore further whether the content or the duration of an intervention affects the outcome.
A third limitation is the absence of an active control group. A meta-analysis of mindfulness-based therapy found no significant difference in outcomes between mindfulness therapy and other therapeutic interventions such as CBT.24 None of the studies in the current review included an active control group, which would have allowed the effect of mindfulness-based interventions to be compared with other types of active treatment. However, Bornemann and Singer35 found that two of their training modules resulted in reduced alexithymia, while the third, which focused on observing thoughts and learning reappraisal skills, did not. This finding appears to suggest the reduction in alexithymia is attributable to the content of that particular training module, rather than other aspects of the intervention such as the method of delivery.
Finally, while two of the interventions were based on the MBSR programme,36 37 two tested bespoke interventions,35 38 which may limit the conclusions that can be drawn for clinical practice. In one of these studies38 mindfulness training comprised only one-sixth of the intervention, and therefore it is not possible to attribute the effect of the intervention to the mindfulness component with any certainty. To address this limitation, we conducted subgroup analysis excluding this study and found that the model remained significant, although the heterogeneity increased.
Conclusions
Participation in mindfulness-based interventions led to significantly lower alexithymia at the study end compared with a control group. The literature on which these conclusions are based is limited, and further RCTs with larger clinical and non-clinical samples and longer follow-up are required. However, the findings indicate that mindfulness-based interventions may be an effective means of reducing alexithymia.
Compliance with ethical standards
Research involving human or animal participants: This article does not contain any studies with human participants or animals performed by any of the authors.
Acknowledgments
The authors would like to thank Paula Garrido for translating one of the studies into English. The authors would like to thank Professor Andrea Cipriani for his expert advice during this project.
Footnotes
Contributors: HN designed the study and wrote the protocol with input from LM, AO and MC. Literature searches were carried out by HN. HN, LM, AO and MC screened abstracts against inclusion criteria. HN and LM conducted data extraction and risk of bias assessment. HN conducted the statistical analysis. HN wrote the first draft of the manuscript. LM, AO and MC reviewed subsequent drafts. All authors have contributed to and have approved the final manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Bagby RM, Parker JD, Taylor GJ. The twenty-item Toronto Alexithymia Scale—I. Item selection and cross-validation of the factor structure. J Psychosom Res 1994;38:23–32. 10.1016/0022-3999(94)90005-1 [DOI] [PubMed] [Google Scholar]
- 2. van der Velde J, Gromann PM, Swart M, et al. Alexithymia influences brain activation during emotion perception but not regulation. Soc Cogn Affect Neurosci 2015;10:285–93. 10.1093/scan/nsu056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. McGillivray L, Becerra R, Harms C. Prevalence and demographic correlates of alexithymia: a comparison between Australian psychiatric and community samples. J Clin Psychol 2017;73:76–87. 10.1002/jclp.22314 [DOI] [PubMed] [Google Scholar]
- 4. Paniccia MF, Gaudio S, Puddu A, et al. Alexithymia in parents and adolescents with generalised anxiety disorder. Clin Psychol 2017;38. 10.1111/cp.12134 [DOI] [Google Scholar]
- 5. Honkalampi K, Hintikka J, Tanskanen A, et al. Depression is strongly associated with alexithymia in the general population. J Psychosom Res 2000;48:99–104. [DOI] [PubMed] [Google Scholar]
- 6. Son SH, Jo H, Rim HD, et al. A comparative study on alexithymia in depressive, somatoform, anxiety, and psychotic disorders among Koreans. Psychiatry Investig 2012;9:325–31. 10.4306/pi.2012.9.4.325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Grabe HJ, Frommer J, Ankerhold A, et al. Alexithymia and outcome in psychotherapy. Psychother Psychosom 2008;77:189–94. 10.1159/000119739 [DOI] [PubMed] [Google Scholar]
- 8. Thorberg FA, Young RM, Sullivan KA, et al. A longitudinal mediational study on the stability of alexithymia among alcohol-dependent outpatients in cognitive-behavioral therapy. Psychol Addict Behav 2016;30:64–72. 10.1037/adb0000135 [DOI] [PubMed] [Google Scholar]
- 9. Westwood H, Kerr-Gaffney J, Stahl D, et al. Alexithymia in eating disorders: systematic review and meta-analyses of studies using the Toronto Alexithymia Scale. J Psychosom Res 2017;99:66–81. 10.1016/j.jpsychores.2017.06.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Norman H, Borrill J. The relationship between self-harm and alexithymia. Scand J Psychol 2015;56:405–19. 10.1111/sjop.12217 [DOI] [PubMed] [Google Scholar]
- 11. Lumley MA, Neely LC, Burger AJ. The assessment of alexithymia in medical settings: implications for understanding and treating health problems. J Pers Assess 2007;89:230–46. 10.1080/00223890701629698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ogrodniczuk JS, Piper WE, Joyce AS. Effect of alexithymia on the process and outcome of psychotherapy: a programmatic review. Psychiatry Res 2011;190:43–8. 10.1016/j.psychres.2010.04.026 [DOI] [PubMed] [Google Scholar]
- 13. Söndergaard HP, Theorell T, Alexithymia TT. Alexithymia, emotions and PTSD; findings from a longitudinal study of refugees. Nord J Psychiatry 2004;58:185–91. 10.1080/08039480410006214 [DOI] [PubMed] [Google Scholar]
- 14. Honkalampi K, Hintikka J, Laukkanen E, et al. Alexithymia and depression: a prospective study of patients with major depressive disorder. Psychosomatics 2001;42:229-34. [DOI] [PubMed] [Google Scholar]
- 15. Salminen JK, Saarijärvi S, Aäirelä E, et al. Alexithymia—state or trait? One-year follow-up study of general hospital psychiatric consultation out-patients. J Psychosom Res 1994;38:681–5. [DOI] [PubMed] [Google Scholar]
- 16. Tolmunen T, Heliste M, Lehto SM, et al. Stability of alexithymia in the general population: an 11-year follow-up. Compr Psychiatry 2011;52:536–41. 10.1016/j.comppsych.2010.09.007 [DOI] [PubMed] [Google Scholar]
- 17. Porcelli P, Tulipani C, Di Micco C, et al. Temporal stability of alexithymia in cancer patients following a psychological intervention. J Clin Psychol 2011;67:1177–87. 10.1002/jclp.20839 [DOI] [PubMed] [Google Scholar]
- 18. Beresnevaite M. Exploring the benefits of group psychotherapy in reducing alexithymia in coronary heart disease patients: a preliminary study. Psychother Psychosom 2000;69:117–22. 10.1159/000012378 [DOI] [PubMed] [Google Scholar]
- 19. Ogrodniczuk JS, Sochting I, Piper WE, et al. A naturalistic study of alexithymia among psychiatric outpatients treated in an integrated group therapy program. Psychol Psychother 2012;85:278–91. 10.1111/j.2044-8341.2011.02032.x [DOI] [PubMed] [Google Scholar]
- 20. Cameron K, Ogrodniczuk J, Hadjipavlou G. Changes in alexithymia following psychological intervention: a review. Harv Rev Psychiatry 2014;22:162–78. 10.1097/HRP.0000000000000036 [DOI] [PubMed] [Google Scholar]
- 21. Kabat-Zinn J, Lipworth L, Burney R. The clinical use of mindfulness meditation for the self-regulation of chronic pain. J Behav Med 1985;8:163–90. 10.1007/BF00845519 [DOI] [PubMed] [Google Scholar]
- 22. Teasdale JD, Segal ZV, Williams JM, et al. Prevention of relapse/recurrence in major depression by mindfulness-based cognitive therapy. J Consult Clin Psychol 2000;68:615–23. 10.1037/0022-006X.68.4.615 [DOI] [PubMed] [Google Scholar]
- 23. Gotink RA, Chu P, Busschbach JJ, et al. Standardised mindfulness-based interventions in healthcare: an overview of systematic reviews and meta-analyses of RCTs. PLoS One 2015;10:e0124344. 10.1371/journal.pone.0124344 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 24. Khoury B, Lecomte T, Fortin G, et al. Mindfulness-based therapy: a comprehensive meta-analysis. Clin Psychol Rev 2013;33:763–71. 10.1016/j.cpr.2013.05.005 [DOI] [PubMed] [Google Scholar]
- 25. Galante J, Dufour G, Vainre M, et al. A mindfulness-based intervention to increase resilience to stress in university students (the Mindful Student Study): a pragmatic randomised controlled trial. Lancet Public Health 2018;3:e72–81. 10.1016/S2468-2667(17)30231-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Baer RA, Smith GT, Hopkins J, et al. Using self-report assessment methods to explore facets of mindfulness. Assessment 2006;13:27–45. 10.1177/1073191105283504 [DOI] [PubMed] [Google Scholar]
- 27. Teixeira RJ, Pereira MG. Examining mindfulness and its relation to self-differentiation and alexithymia. Mindfulness 2015;6:79–87. 10.1007/s12671-013-0233-7 [DOI] [Google Scholar]
- 28. Byrne G, Bogue J, Egan R, et al. "Identifying and describing emotions": measuring the effectiveness of a brief, alexithymia-specific, intervention for a sex offender population. Sex Abuse 2016;28:599–619. 10.1177/1079063214558940 [DOI] [PubMed] [Google Scholar]
- 29. Haase L, May AC, Falahpour M, et al. A pilot study investigating changes in neural processing after mindfulness training in elite athletes. Front Behav Neurosci 2015;9. 10.3389/fnbeh.2015.00229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Ernst J, Böker H, Hättenschwiler J, et al. The association of interoceptive awareness and alexithymia with neurotransmitter concentrations in insula and anterior cingulate. Soc Cogn Affect Neurosci 2014;9:857–63. 10.1093/scan/nst058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Fissler M, Winnebeck E, Schroeter T, et al. An investigation of the effects of brief mindfulness training on self-reported interoceptive awareness, the ability to decenter, and their role in the reduction of depressive symptoms. Mindfulness 2016;7:1170–81. 10.1007/s12671-016-0559-z [DOI] [Google Scholar]
- 32. Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0, 2011. [Google Scholar]
- 33. Furukawa TA, Guyatt GH, Griffith LE. Can we individualize the ’number needed to treat'? An empirical study of summary effect measures in meta-analyses. Int J Epidemiol 2002;31:72–6. [DOI] [PubMed] [Google Scholar]
- 34. The Cochrane Collaboration. RevMan 5 | Cochrane Community. Cochrane Community 2014. [Google Scholar]
- 35. Bornemann B, Singer T. Taking time to feel our body: steady increases in heartbeat perception accuracy and decreases in alexithymia over 9 months of contemplative mental training. Psychophysiology 2017;54:469–82. 10.1111/psyp.12790 [DOI] [PubMed] [Google Scholar]
- 36. de la Fuente Arias M, Justo CF, Granados MS. Efectos de un programa de meditación (mindfulness) en la medida de la alexitimia y las habilidades sociales. Psicothema 2010;22:369–75. [PubMed] [Google Scholar]
- 37. Santarnecchi E, D’Arista S, Egiziano E, et al. Interaction between neuroanatomical and psychological changes after mindfulness-based training. PLoS One 2014;9. 10.1371/journal.pone.0108359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Vinding C, Osika W, Theorell T, et al. “The Culture palette”—a randomized intervention study for women with burnout symptoms in Sweden. Br J Med Pract 2015;8. [Google Scholar]
- 39. Brown KW, Ryan RM. The benefits of being present: mindfulness and its role in psychological well-being. J Pers Soc Psychol 2003;84:822–48. [DOI] [PubMed] [Google Scholar]
- 40. Murphy J, Brewer R, Catmur C, et al. Interoception and psychopathology: a developmental neuroscience perspective. Dev Cogn Neurosci 2017;23:45–56. 10.1016/j.dcn.2016.12.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Craig AD. How do you feel—now? The anterior insula and human awareness. Nat Rev Neurosci 2009;10:59–70. 10.1038/nrn2555 [DOI] [PubMed] [Google Scholar]
- 42. Sauer S, Walach H, Schmidt S, et al. Assessment of mindfulness: review on state of the art. Mindfulness 2013;4:3–17. 10.1007/s12671-012-0122-5 [DOI] [Google Scholar]
- 43. Stasiewicz PR, Bradizza CM, Gudleski GD, et al. The relationship of alexithymia to emotional dysregulation within an alcohol dependent treatment sample. Addict Behav 2012;37:469–76. 10.1016/j.addbeh.2011.12.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Rufer M, Albrecht R, Zaum J, et al. Impact of alexithymia on treatment outcome: a naturalistic study of short-term cognitive-behavioral group therapy for panic disorder. Psychopathology 2010;43:170–9. 10.1159/000288639 [DOI] [PubMed] [Google Scholar]
- 45. Spek V, Nyklícek I, Cuijpers P, et al. Alexithymia and cognitive behaviour therapy outcome for subthreshold depression. Acta Psychiatr Scand 2008;118:164–7. 10.1111/j.1600-0447.2008.01199.x [DOI] [PubMed] [Google Scholar]
- 46. Martin S, Martin G, Lequertier B, et al. Voice movement therapy: evaluation of a group-based expressive arts therapy for nonsuicidal self-injury in young adults. Music Med 2013;5:31–8. 10.1177/1943862112467649 [DOI] [Google Scholar]
- 47. Taylor GJ, Bagby RM, Parker JDA, et al. Disorders of affect regulation: alexithymia in medical and psychiatric illness: Cambridge University Press, 1997. [Google Scholar]
- 48. Valdespino A, Antezana L, Ghane M, et al. Alexithymia as a transdiagnostic precursor to empathy abnormalities: the functional role of the insula. Front Psychol 2017;8. 10.3389/fpsyg.2017.02234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Bouvet C, Grignon C, Zachariou Z, et al. Liens entre le développement de la pleine conscience et l’amélioration de la dépression et de l’anxiété. Ann Med Psychol 2015;173:54–9. [Google Scholar]
- 50. Turner RM, Bird SM, Higgins JP. The impact of study size on meta-analyses: examination of underpowered studies in Cochrane reviews. PLoS One 2013;8:e59202. 10.1371/journal.pone.0059202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Gismero E. EHS Escala de Habilidades Sociales. Madrid TEAPublicaciones Psicol Apl 2000. [Google Scholar]
- 52. Meyer TJ, Miller ML, Metzger RL, et al. Development and validation of the Penn State Worry Questionnaire. Behav Res Ther 1990;28:487–95. [DOI] [PubMed] [Google Scholar]
- 53. Vigneau F, Cormier S. The factor structure of the State-Trait Anxiety Inventory: an alternative view. J Pers Assess 2008;90:280–5. 10.1080/00223890701885027 [DOI] [PubMed] [Google Scholar]
- 54. Beck AT, Steer RA, Ball R, et al. Comparison of Beck Depression Inventories -IA and -II in psychiatric outpatients. J Pers Assess 1996;67:588–97. 10.1207/s15327752jpa6703_13 [DOI] [PubMed] [Google Scholar]
- 55. Besèr A, Sorjonen K, Wahlberg K, et al. Construction and evaluation of a self rating scale for stress-induced exhaustion disorder, the Karolinska Exhaustion Disorder Scale. Scand J Psychol 2014;55:72–82. 10.1111/sjop.12088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Langius A, Lind MG. Well-being and coping in oral and pharyngeal cancer patients. Eur J Cancer B Oral Oncol 1995;31B:242-9. [DOI] [PubMed] [Google Scholar]