Abstract
Artificial intelligence (AI) is currently integrated into many medical services. AI is utilized in many aspects of orthopedic surgery. The scope ranges from diagnosis to complex surgery. To evaluate the perceptions, attitudes, and interests of Sudanese orthopedic surgeons regarding the different applications of AI in orthopedic surgery. This qualitative questionnaire-based study was conducted through an anonymous electronic survey using Google Forms distributed among Sudanese orthopedic surgeons. The questionnaire entailed 4 sections. The first section included the participants’ demographic data. The remaining 3 sections included questions for the assessment of the perception, attitude, and interest of surgeons toward (AI). The validity and reliability of the questionnaire were tested and piloted before the final dissemination. One hundred twenty-nine surgeons responded to the questionnaires. Most respondents needed to be more aware of the basic concepts of AI. However, most respondents were aware of its use in spinal and joint replacement surgeries. Most respondents had doubts regarding the safety of (AI). However, they were highly interested in utilizing (AI) in many orthopedic surgical aspects. Orthopedic surgery is a rapidly evolving branch of surgery that involves adoption of new technologies. Therefore, orthopedic surgeons should be encouraged to enroll in research activities to generate more studies and reviews to assess the usefulness and safety of emerging technologies.
Keywords: artificial intelligence, attitude, orthopedic surgeons, perception, Sudan
Key Points:
-
•
Artificial intelligence is rapidly incorporated into many aspects of orthopedic surgical care.
-
•
Majority of surgeons needed to be more aware of the basic terminologies of AI.
-
•
Orthopedic surgeons should be more involved in research to investigate the usefulness, practicality, and safety of artificial intelligence utilization in their practice.
1. Introduction
Artificial intelligence (AI) has a plethora of definitions. Nevertheless, it is defined as the ability of machines to perform complex tasks such as intelligent beings.[1] Currently, (AI) is an integral part of many machines and devices that are used daily. These include the smart voice assistants used in smartphones, automobiles, and navigation devices. Machine learning (ML) is a form of (AI) in which algorithms are used via computers to learn and acquire experience in performing specific tasks.[2]
ML can be subdivided into several categories. The 2 main types are supervised learning, in which the computer uses labeled examples or specific roles to predict future patterns and events such as disease outcomes. The second ML type is unsupervised learning, in which computer algorithms are not equipped with prelabeled data. Therefore, they can explore data and identify specific patterns and common characteristics.[2] Deep learning (DL) is an advanced and complex form of unsupervised ML. It uses multiple levels of neural networks to mimic the analysis and processing of human brain data analysis and processing. DL has shown good results in exploring and finding the common characteristics of large datasets, such as medical information, and it can also improve itself through learning.[3]
AI has been utilized in healthcare since the 1980s as a diagnostic tool for identifying patients at risk of developing myocardial infarction in emergency departments.[4] In dermatology, (AI) has been used to categorize skin lesions using DL neural networks, which integrate patient medical information and digital lesion images with high sensitivity and specificity.[5] In musculoskeletal radiology, DL neural networks have been utilized in many aspects, such as improving appointment scheduling, which was achieved by reducing the number of missed appointments, especially for advanced imaging modalities, such as CT scans and MRI.[6] Moreover, ML showed a marked improvement in the image acquisition and reconstruction speed. Furthermore, ML shows promising results in reducing the CT radiation dose, which is highly desirable during the procedure.[6] Another area in which (AI) is showing promise is enhancing the interpretation of musculoskeletal MRI scans.[7] AI powered systems can use ML to observe and analyze subtle patterns and minor changes that humans may miss. AI can provide a higher level of accuracy, speed, and efficiency by leveraging previous imaging studies, scans, and results from similar patients.[8] AI can act as a “second pair of eyes” for radiologists, increasing the diagnostic accuracy and reducing the risk of delayed diagnosis. AI technology has vast potential in the field of musculoskeletal radiology and has already contributed significantly to diagnosis, treatment, and patient care. As capabilities continue to improve, AI is expected that AI will become an even more impactful tool for supporting radiologists in identifying musculoskeletal abnormalities and addressing patients’ individual needs, ultimately leading to a more efficient, cost-effective, and personalized healthcare system.[6,9]
AI has been used in many aspects of orthopedic surgical care. (AI) was incorporated in the diagnosis and classification of fractures, risk assessment and prediction of outcomes, intraoperative navigation in joint replacement and spinal surgery, and robot-assisted surgery.
ML was used for risk stratification and to predict outcomes in patients with fractures. For example, in hip fractures in geriatric patients, ML can predict which patients are more likely to develop delirium; therefore, preventive measures could be taken earlier,[10] and ML has been used to predict the most suitable surgical tactics for certain fractures, such as distal radius fractures, to improve outcomes.[11] However, the prediction of outcomes requires high-quality data to be used by ML prediction models to increase the accuracy of risk stratification. Multicentric collaboration is therefore necessary to achieve this goal.[11] Nevertheless, this collaboration can be complex due to many ethical, legal, political, and administrative obstacles.
ML has also been used in emergency departments to help doctors avoid missing significant fractures due to lack of experience or exhaustion at the end of the shift.[11] One approved application is OsteoDetect, which uses computer vision (a type of ML) to diagnose fractures.[12]
In joint replacement surgery(arthroplasty), (AI) was used in preoperative planning by utilizing a specific patient CT scan to develop 3D models of the joint,[13] which helped in proper sizing and placement of the implants with an accuracy >90%.[14] The use of robots and navigation systems in joint replacement surgery has shown promising results by improving the accuracy of bone cuts and ligament balancing (particularly in total knee replacement).[15]
In spinal surgery, AI has been applied to many aspects of patient care, such as selecting cases, classifying spinal diseases, classifying deformities, and predicting outcomes.[16] Intraoperatively, robot-assisted surgery significantly improves outcomes using minimally invasive techniques and accurate placement of pedicle screws with the aid of navigation systems.[17]
Few studies have addressed the magnitude of knowledge about (AI) among health professionals.[18,19] They revealed a lack of knowledge regarding the basic concepts of (AI). Although the early results of (AI) utilization in health services are promising, many scientific communities have been concerned that ML might disturb the doctor-patient relationship.[20] However, some scholars have postulated that proper utilization of (AI) in medical services may improve it.[21] Although the use of AI in orthopedics seems promising, there are some limitations to this technology, including the following:
-
1.
Lack of clinical experience: Although AI can analyze massive amounts of data and spot patterns, it lacks the clinical expertise of doctors. As a result, AI algorithms may not always reach the same conclusions as subject matter expert.[22,23]
-
2.
Data bias: The quality of the data that AI algorithms are trained on to determine the accuracy of the data. AI systems produce biased results if the data used for training are biased. For instance, if the algorithm was developed using data from a particular demographic group, it might not be as effective at forecasting results for other groups.[23,24]
-
3.
Lack of empathy: AI algorithms are ill-suited to comprehending the psychological and emotional facets of patient care. This may restrict their ability to offer individualized care that considers the unique circumstances and preferences of each patient.[20,25]
-
4.
Legal and ethical issues: Concerns about data privacy, informed consent, and liability for incorrect diagnoses or treatments are among the legal and ethical issues raised by the use of AI in orthopedics.[26]
-
5.
Cost: The cost of creating and implementing AI systems makes it challenging for small healthcare facilities to use this technology. Accessibility to these cutting-edge diagnostic and treatment options may be hampered by their high cost.[9,14]
Many previous studies have elaborated on the applications of (AI) in arthroplasty and spine and musculoskeletal trauma[10,13,16,17,24]; however, to the best of our knowledge, no published studies have measured orthopedic surgeons’ knowledge of and attitudes toward the utilization of (AI) in orthopedic practice. This study aimed to evaluate the perceptions, attitudes, and interests of Sudanese orthopedic surgeons regarding different applications of (AI) in orthopedic surgery.
2. Materials & methods
2.1. Study design
This descriptive, qualitative, cross-sectional, survey-based study was conducted among Sudanese orthopedic surgeons. It was conducted from the 1st of September 2022 to the 31st of January 2023.
2.2. Study population and sample size
An electronic survey link was sent to 4 official WhatsApp groups of the Sudanese Orthopedic Surgeons Association (SOSA). According to information from the deputy secretary general of the SOSA, 687 surgeons have been officially registered with the organization as of January 2023. The Social Affairs Secretary manages these 4 official SOSA WhatsApp groups, which are the primary means of communication between the SOSA and its members. To join one of these groups, a member must be a registered specialist with Sudan Medical Council. In total, 664 participants were included in each group. The author sent a reminder to participate in the survey every 2 weeks to increase the response rate. Of the 664 participants, 78 responded initially (1st wave) to the survey, resulting in a response rate of 11.75%. From November 2022 to January 2023, an additional 50 responses were received, totaling 128 responses, increasing the response rate to 19.42%. Successive wave analysis was used to estimate the nonresponse bias. This technique is based on the response continuum theory, which states that late respondents or those who participated after 1 or 2 reminders were more likely to be non-responders than those who reacted,[27,28] after November, all replies were deemed to be subsequent wave (2nd wave).
2.3. The questionnaire
The questionnaire was designed using google forms. It was in English and composed of 4 sections. The first section concerned demographics (age, subspecialty, years of experience, work institutions, and sex). The second section assessed the level of knowledge of the basic concepts of AI, which was composed of 3 questions. Each question had 4 responses, ranging from complete awareness to lack of knowledge about the primary (AI) concepts. The third section was mainly intended to assess knowledge about the applications of (AI) in trauma (three questions), spine (two questions), and arthroplasty (two questions), with each question having 3 responses (yes, no, and I do not know). The final section contained 4 questions (statements) to assess the attitudes of surgeons toward (AI); it contained 4 questions(statements), and each question had 4 responses (ranging from strongly agree to strongly disagree). Moreover, 3 questions were intended to assess surgeons’ interest in (AI), each with 4 responses (ranging from strongly interested to strongly not interested). All questions were closed and are summarized in Table 1. Responses were coded into numbers from 1 to 4; responses that indicated a higher level of knowledge, positive attitude, or high interest were assigned higher values in the coding process. A complete questionnaire was required for submission.
Table 1.
Shows the summary of the survey questions and the domains which they are intended to measure.
| Domain | Questions | No. of responses | |
|---|---|---|---|
| Basic concepts | •Do you know the difference between machine learning and deep learning? | 4 | |
| •Do you know the difference between supervised and unsupervised machine learning? | 4 | ||
| •Do you know the difference between computer vision and natural language processing? | 4 | ||
| Orthopedic application of AI | •Reading radiographs | Trauma | 3 |
| •Patients risk stratification and prediction of the outcome | 3 | ||
| •Planning and execution of surgical tactics in fracture surgery | 3 | ||
| •Selecting the proper implant size in arthroplasty | Arthroplasty | 3 | |
| •Intraoperative proper implant positioning in arthroplasty | 3 | ||
| •Intraoperative navigation in spinal surgery | Spine | 3 | |
| •Deformity correction planning in spinal surgery | 3 | ||
| Attitude | •I think there may be serious privacy issues with the use of AI? | 4 | |
| •I think AI can replace my job? | 4 | ||
| •I think AI can improve my practice | 4 | ||
| •I think AI is dangerous | 4 | ||
| Interest | •Are you interested to search for scientific articles or courses on artificial intelligence (AI)? | 4 | |
| •Are you Interested to use AI in your practice? | 4 | ||
| •I think artificial intelligence applications in orthopedic surgery are useful for: Tick all that apply | 5 | ||
2.4. Validation of the questionnaire
English language experts checked the questionnaire linguistic clarity. Four senior orthopedic consultants checked the face validity of the different questionnaire constructs.
A Pilot study was performed to check the validity and reliability of the questionnaire, which was distributed to a group of 25 orthopedic surgeons who were omitted in the final study.
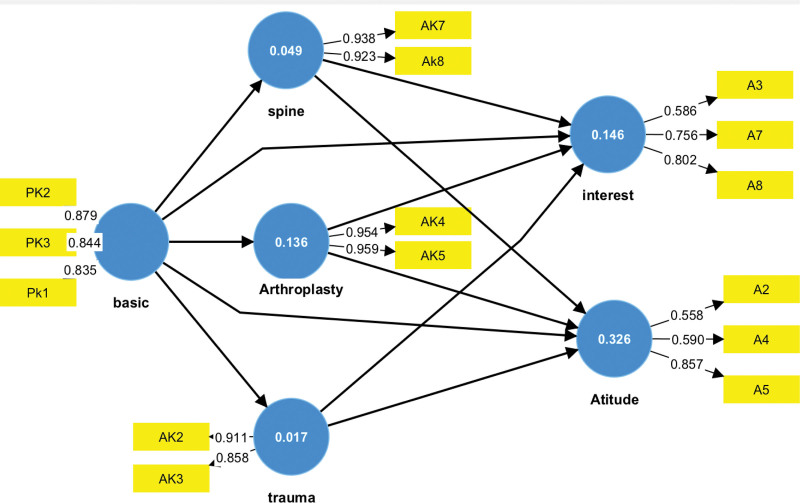
Factor analysis was performed using the SmartPLS software version 4 (SmartPLS GmbH, D-22114 Oststeinbek, Germany). The partial least squares structural equation modeling (PLS-SEM) algorithm was used to determine the factor loadings for each domain to assess validity (convergent and discernment) and reliability (internal consistency). Using the measurement model, as shown in Figure 1, all constructs had composite reliability (rho-c) values not <0.7, indicating that internal consistency was established. The average variance extracted for all constructs was >0.5; thus, convergent validity was established (Table 2). Discernment validity was checked using the Fornell and Larker criteria, which showed that every construct average variance extracted square root was higher than its correlation with other constructs. Moreover, the Heterotrait-Monotrait Ratio was <0.85 in all constructs and this indeed signified construct validity (Table 3).
Figure 1.
Figure 1 shows the measurement model and factor loadings for each questionnaire construct. Yellow rectangular shapes represent questions (factors), while blue circular shapes represent constructs (latent variables). Large arrows between circles represent the relationship between latent variables, while small arrows between rectangles and circles represent factor loadings in latent variables (Using smartPLS® v.4.).
Table 2.
Shows the values of composite reliability (rho_c) as an indicator for constructs reliability and the AVE as an indicator for convergence validity.
| Composite reliability (rho_c) | Average variance extracted (AVE) | |
|---|---|---|
| Arthroplasty | 0.956 | 0.915 |
| Attitude | 0.714 | 0.464 |
| Basic K. | 0.889 | 0.728 |
| Interest | 0.761 | 0.519 |
| Spine | 0.928 | 0.866 |
| Trauma | 0.878 | 0.783 |
Table 3.
Showing discriminant validity measures using Furnell and Larker criteria & HTMT ratio.
| Fornell and Larker criteria | ||||||
|---|---|---|---|---|---|---|
| Arthroplasty | Attitude | Basic K. | Interest | Spine | Trauma | |
| Arthroplasty | 0.957 | |||||
| Attitude | 0.500 | 0.681 | ||||
| Basic K. | 0.369 | 0.383 | 0.853 | |||
| Interest | 0.088 | 0.257 | 0.119 | 0.721 | ||
| Spine | 0.333 | 0.185 | 0.222 | 0.114 | 0.931 | |
| Trauma | 0.322 | 0.329 | 0.131 | 0.358 | 0.068 | 0.885 |
| Heterotrait-Monotrait Ratio (HTMT) | ||||||
| Arthroplasty | Attitude | Basic k. | Interest | Spine | Trauma | |
| Arthroplasty | ||||||
| Attitude | 0.607 | |||||
| Basic k. | 0.429 | 0.443 | ||||
| Interest | 0.111 | 0.381 | 0.202 | |||
| Spine | 0.384 | 0.236 | 0.261 | 0.190 | ||
| Trauma | 0.403 | 0.322 | 0.189 | 0.546 | 0.160 | |
2.5. Ethical considerations
Ethical approval for this study was granted by the Research Ethics Committee of King Faisal University (KFU-REC-2022-DEC-ETHICS411). The survey was optional and all respondent information was kept anonymous. No private information is available for this study. Once participants completed the survey, they consented to participate in the study.
2.6. Statistical analysis
Data were analyzed using IBM SPSS version 25 (IBM Corp., Armonk, NY). Frequency tables and percentages were used for the descriptive statistics. Data exploration revealed that the data were not normally distributed; therefore, nonparametric tests were used. Spearman rank correlation coefficient was used to determine the relationships between continuous variables. The Mann–Whitney U test and Kruskal–Wallis test with post hoc analysis for independent samples were used to determine the relationships between continuous and categorical variables. Successive wave analysis to estimate non-response bias was performed using the chi-square test (χ2) and Mann–Whitney U test to determine the differences between 1st wave and 2nd wave responses. A P value of <.05 for 95% confidence interval was considered significant.
3. Results
3.1. Demographics
Initially, 78 surgeons completed the survey, followed by a second wave of 50 respondents, with a response rate of 19.42% for 128 participants. Successive wave analysis was conducted by comparing the initial and late respondents’ characteristics, and the (χ2) test revealed no significant differences in demographic variables between the early and late participants (see Table 4). Using the Mann–Whitney U test and adopting response time as a grouping variable (wave1, wave2), there were no significant differences in knowledge, attitude, and interest mean rank scores between early and late respondents (Table 5). Therefore, no significant variations were observed in any of the factors studied throughout the waves, suggesting that individuals who needed more reminders shared comparable characteristics with the early participants. Although the response rate was low, these findings suggest no evidence of non-response bias.
Table 4.
Shows frequencies and chi-square (χ2) test result for early (wave1) and late (wave2) respondants demogrhaphic varibles (N = 128).
| Variable | Frequency of respondants Wave1 (N78) | Frequency of respondants Wave2 (N51) | Total number of respondanats | χ2 (df) | P value |
|---|---|---|---|---|---|
| Age | 0.155 (2) | .925 | |||
| 30–40 | 21 | 14 | 35 | ||
| 41–50 | 52 | 32 | 84 | ||
| 51–60 | 5 | 4 | 9 | ||
| Gender | 0.009 (1) | .925 | |||
| Male | 73 | 47 | 120 | ||
| Female | 5 | 3 | 8 | ||
| Rank | |||||
| Specialist | 14 | 9 | 23 | 4.037 (3) | .257 |
| Senior specialist | 22 | 12 | 34 | ||
| Consultant | 35 | 24 | 59 | ||
| Senior consultant | 7 | 5 | 12 | ||
| Years of experience | 0.968 (3) | .809 | |||
| <5 | 12 | 9 | 21 | ||
| 6–10 | 32 | 20 | 52 | ||
| 11–20 | 22 | 11 | 33 | ||
| >20 | 12 | 10 | 22 | ||
| 0 | |||||
| Subspecialty/practice | 2.82 (8) | .945 | |||
| Pediatrics | 12 | 9 | 21 | ||
| Sports | 5 | 4 | 9 | ||
| Arthroplasty | 10 | 5 | 15 | ||
| Spine | 5 | 5 | 10 | ||
| Ankle and foot | 5 | 2 | 7 | ||
| Limb deformity correction | 1 | 1 | 2 | ||
| Trauma | 29 | 20 | 49 | ||
| Upper limb | 6 | 3 | 9 | ||
| Hand | 5 | 1 | 6 | ||
| Work institution | 0.817 (3) | .845 | |||
| Private practice | 10 | 10 | 20 | ||
| Community hospital | 28 | 28 | 56 | ||
| Academic hospital | 29 | 29 | 58 | ||
| Specialized center | 11 | 11 | 22 |
Table 5.
Show the differences in mean rank scores in basic knowledge, applied knowledge (Trauma, Arthroplasty, Spine), attitude and interest between early (wave1) and late (wave2) respondents using the Mann–Whitney U test for independent samples (N = 128).
| Domain | Grouping variable | N | Mean Rank | Mann–Whitney U | P value |
|---|---|---|---|---|---|
| wave | |||||
| Basic k. | 1 | 78 | 64.36 | 1939 | .955 |
| 2 | 50 | 64.72 | |||
| Attitude | 1 | 78 | 63.46 | 1869 | .688 |
| 2 | 50 | 66.12 | |||
| Interest | 1 | 78 | 65.06 | 1906 | .825 |
| 2 | 50 | 63.62 | |||
| Arthroplasty K. | 1 | 78 | 66.29 | 1810.5 | .451 |
| 2 | 50 | 61.71 | |||
| Trauma K. | 1 | 78 | 66.22 | 1815.5 | .483 |
| 2 | 50 | 61.81 | |||
| Spine K. | 1 | 78 | 64.46 | 1947 | .987 |
| 2 | 50 | 64.56 |
The majority of participants were male (93.8%) and 6.3% were female; most of them were between 41 and 50 years old (65.7%); most were consultants (46.1%); most of the participants had 6 to 10 years of experience (40.6%); the most frequent subspecialty or the main practice area was trauma (38.3%); and most surgeons were practicing in academic hospitals (39.1%), followed by community hospitals (33.6%) (Table 4).
3.2. Perceptions of (AI) among surgeons
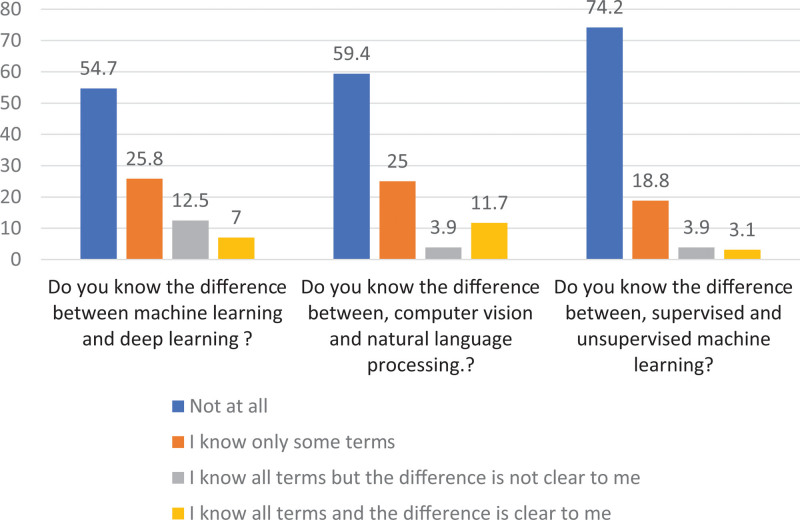
Regarding awareness of the basic concepts in (AI), 57.7% were not familiar with the types of ML, 59.4% did not know the difference between supervised and unsupervised ML, and 74.2%were not aware of terminologies such as computer vision and natural language processing (Fig. 2).
Figure 2.
Bar chart showing the percentages of responses to the questions about the basic concepts of artificial intelligence (N = 128).
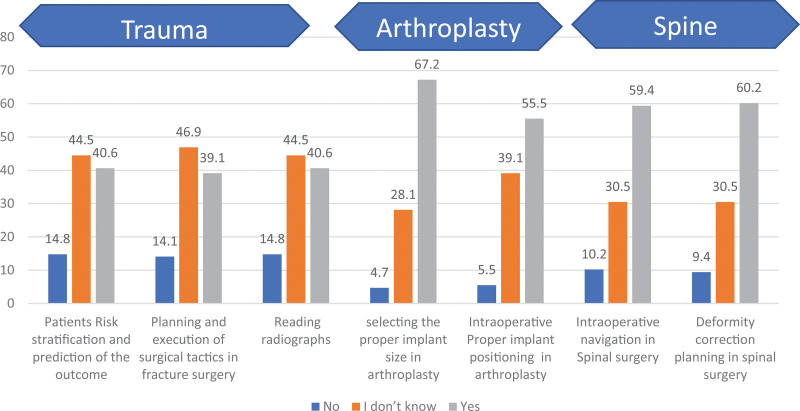
Regarding the knowledge about the applications of (AI) in different orthopedic subspecialities, most of the participants were aware of (AI) applications in arthroplasty (67.2% and 55.5% responded “yes”) and spinal surgery (59.4%,60.2% responded “yes”). However, they were less aware of the use of (AI) in trauma surgery (44.5%,44.5%, and 46.9.3% responded, “I do not know”) (Fig. 3). Spearman rank correlation revealed that surgeons with higher mean rank scores for knowledge of the basic concepts of (AI), were significantly more knowledgeable about the use of (AI) in arthroplasty (rs = 0.478; P < .01) and spine surgery (rs = 0.224; P = .011) but not in trauma (rs = 0.124; P = .164). There were no statistically significant differences in the knowledge mean rank scores (MR) across all demographic factors.
Figure 3.
Bar chart showing the percentages of responses of surgeons to questions about the applications of AI in orthopedics (N = 128). AI = artificial intelligence.
3.3. Surgeon attitudes toward (AI)
Regarding the surgeon attitude toward (AI), 64.1% of the respondents agreed that (AI) will improve their practice, and 64.1% completely disagreed that (AI) can replace their jobs. In contrast, only 32.8% of surgeons completely disagreed that AI is dangerous and only,10.9% thought that (AI) would not cause any serious privacy issues (Table 6). Spearman rank correlation revealed that surgeons with higher mean rank scores of knowledge about (AI) basic concepts (rs = 0.339; P < .01) and application in arthroplasty (rs = 0.433; P < .01) showed significantly positive attitudes toward (AI).
Table 6.
Shows the surgeons’ attitude toward (AI) (N = 128).
| Responses Questions | Completely agree (%) | Partially agree (%) | Partially disagree (%) | Completely disagree (%) |
|---|---|---|---|---|
| I think there may be serious privacy issues with the use of AI? | 17.2 | 49.2 | 22.7 | 10.9 |
| I think AI can replace my job? | 8.6 | 15.6 | 11.7 | 64.1 |
| I think AI can improve my practice | 64.1 | 35.2 | 0.8 | 0 |
| I think AI is dangerous | 4.7 | 21.9 | 40.6 | 32.8 |
AI = artificial intelligence.
3.4. Surgeons’ interest in (AI)
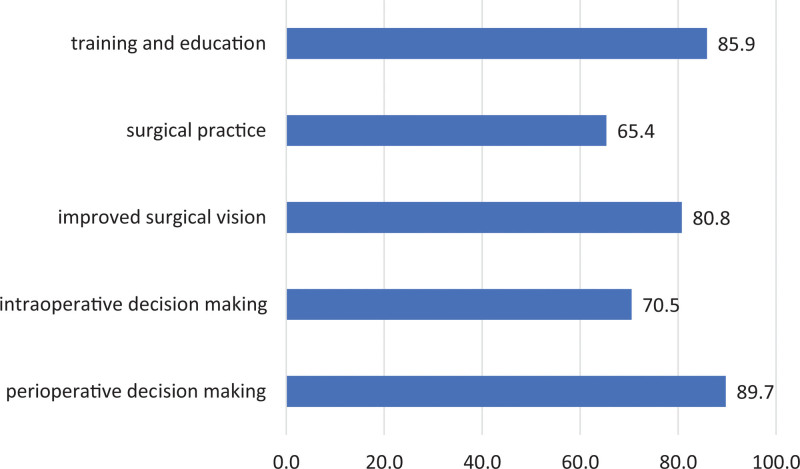
Regarding the surgeons’ interest in (AI), 47.7% of respondents were interested in searching for scientific articles or courses addressing (AI), followed by 41.4% who were strongly interested. Sixty-eight percent of the respondents were interested in using (AI) in their practice, followed by 26.6%, who were strongly interested (Table 7). Most respondents thought that (AI) can be helpful in preoperative decision-making (89.7%), training and education (85.9%), and improved surgical vision (80.8%) (Fig. 4).
Table 7.
Shows the interest of surgeons in (AI) (N = 128).
| Responses questions | Strongly not interested (%) | Not interested (%) | Interested (%) | Strongly interested (%) |
|---|---|---|---|---|
| Are you interested to search for scientific articles or courses on artificial intelligence (AI)? | 2.3 | 8.6 | 47.7 | 41.4 |
| Are you interested to use AI in your practice? | 1.6 | 3.1 | 68.8 | 26.6 |
Figure 4.
Bar chart showing the percentages of responses of surgeons to what they thought AI is useful for in orthopedics (N = 128). AI = artificial intelligence.
Female surgeons showed lower interest mean rank scores (MR = 9.63) than male surgeons (MR = 68.16), which was statistically significant according to the Mann–Whitney U test (U = 44, P < .01). Surgeons with 11–20 years of experience showed higher interest mean rank scores (MR = 84.97) than those with <5 years of experience (MR = 44.76) and >20 years of experience (MR = 52.2), which were found to be significant using the Kruskal–Wallis test (H (3) = 19.3; P < .01) with post hoc analysis using the Dunn test and Bonferroni adjustment for the P value. There were no statistically significant differences in mean interest rank scores among the other demographic variables.
4. Discussion
To the best of our knowledge, this is the first survey to assess the depth of knowledge, attitude, and interest toward (AI) among Sudanese orthopedic surgeons. The survey revealed a lack of knowledge about the basic concepts of AI; more than 50% of respondents needed to be made aware of basic terms like ML and DL. These results are in line with those of previous studies conducted among healthcare professionals.[18,19,29] Although there was a general lack of knowledge about the basic concepts of (AI), most respondents in our study were aware of the utilization of (AI) in arthroplasty and spine surgery, which could be justified by the early introduction of advanced technologies, such as robotic surgery and computer navigation systems, since the 1990s in arthroplasty and spine surgery.[13,30] Regarding the utilization of (AI) in trauma surgery, there was a lower level of knowledge among the respondents, which could be due to the late introduction of deep ML in fracture management, such as fracture detection, classification,[31,32] and prediction of outcomes.[10,33] Although early results are promising, additional research is required to assess the usefulness and cost-effectiveness of employing (AI) in fracture treatment. In our study, the level of knowledge of the basic concepts of (AI) was found to positively impact the level of awareness of (AI) in spinal surgery and arthroplasty.
Only (32%) of the respondents ultimately agreed that (AI) is not dangerous, and 50% of the respondents thought there might be privacy issues with the use of (AI), which means most respondents had doubts regarding the safety of (AI). This was in agreement with the findings of studies conducted by Castagno et al,[18] Codari et al,[34] and Lai et al[35] In the contrast, most respondents (64%) completely agreed that (AI) can improve their practice, and (64%) also not think that (AI) could replace their jobs. These results are in agreement with the results reported by Castagno et al[18] among doctors, but they were not in line with the public survey conducted by Smith and Aaron[36] among Americans, which reported that 2-thirds of the respondents expected that their jobs would be taken by robots and computers in 50 years, which could be justified because in medicine, empathy is crucial for the doctor-patient relationship, and this part of our practice is difficult to replace by machines. In our study, surgeons with 11 to 20 years of practice, those with higher basic knowledge scores, and those with higher scores on knowledge of (AI) application in arthroplasty showed a significantly positive attitude toward using (AI) in their practice.
Most surgeons in our study were willing to use (AI) in their practice, which is in agreement with the study conducted by De Simone,[19] and most respondents were willing to search for articles and courses on (AI). Although most respondent needed more knowledge about the basic concepts of (AI), they are willing to explore and adopt (AI) technologies in their practice, and this was reflected in their response to the last question of the survey “what do you think (AI) is useful for in orthopedics?” which had 5 choices that were designed to cover the significant areas of orthopedic surgical practices, most respondents 47% had checked all the 5 choices which shows a high magnitude of interests among the surgeons. Nevertheless, female surgeons showed a significantly lower interest than male surgeons; however, it could be argued that the number of females was small in this study group (only 7 females).
5. Limitations of the study
One of the limitations of this study was its small sample size. However, the response rate to the survey was much higher (19.42%) than that reported by De Simone et al (2%) and Castagno et al (1.3%),[18,19] and successive wave analysis revealed no evidence of nonresponse bias. Moreover, the survey was self-administered; therefore, self-selection bias was possible, and multiple reminders were sent to minimize this bias. Another limitation was that the survey did not contain personal data or less-detailed questions, which increased the possibility of information bias. Therefore, all survey questions were closed to minimize information bias. Therefore, the results should be cautiously generalized. The justification for these limitations is to ease the survey format and encourage more respondents to complete it.
6. Conclusion
AI is becoming an integral part of our daily practice, and the same is valid for medical practice. Although Sudanese orthopedic surgeons need to be more knowledgeable about the basic concepts of (AI), most are aware of its use in spine surgery and arthroplasty. There were trust issues toward (AI) among the surgeons; however, most respondents were willing to learn more about (AI) and to utilize it in practice. Orthopedic surgery is a rapidly evolving branch of surgery that involves adoption of new technologies. Therefore, orthopedic surgeons should be encouraged to enroll in research activities to generate more studies and reviews for assessing the usefulness and safety of emerging technologies.
Acknowledgments
I would like to thank Professor Ali AL Tayeb, Professor Osman Bakri, Dr Azar Abbas, and Dr Mohammed Khalid for their contribution to the validation of the questionnaire. I would like to express my gratitude to Professor Ali Adam for his efforts in revising the language of the questionnaire. I would like to extend my thanks to my fellow surgeons at SOSA for responding to the survey.
Author contributions
Conceptualization: Ahmed Hassan Kamal.
Data curation: Ahmed Hassan Kamal.
Formal analysis: Ahmed Hassan Kamal, El Walid Fadul Nasir.
Investigation: Rabab Abbas Majzoub.
Methodology: Ossama Mohammed Zakaria.
Software: Ahmed Hassan Kamal, El Walid Fadul Nasir.
Supervision: Ahmed Hassan Kamal.
Visualization: Rabab Abbas Majzoub.
Writing – original draft: Ossama Mohammed Zakaria, El Walid Fadul Nasir.
Writing – review & editing: Ossama Mohammed Zakaria, El Walid Fadul Nasir.
Abbreviations:
- AI
- artificial intelligence
- DL
- deep learning
- ML
- machine learning
- SOSA
- Sudanese orthopedic surgeons association
The authors have no conflicts of interest to disclose.
The research was supported by the Deanship of Scientific Research, Vice Presidency for Graduate Studies and Scientific Research, King Faisal University, Saudi Arabia.
Informed consent: Not applicable.
Institutional Ethical Committee Approval: Ethical approval for this study was granted by the Research Ethics Committee of the King Faisal University.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
How to cite this article: Kamal AH, Zakaria OM, Majzoub RA, Nasir EWF. Artificial intelligence in orthopedics: A qualitative exploration of the surgeon perspective. Medicine 2023;102:24(e34071).
Contributor Information
Ossama Mohammed Zakaria, Email: ossamaz2004@gmail.com.
Rabab Abbas Majzoub, Email: dr.rabababbas@hotmail.com.
El Walid Fadul Nasir, Email: mamlakatnoonn@gmail.co.
References
- [1].Oxford Languages and Google - English | Oxford Languages. 2022.
- [2].Deo RC. Machine learning in medicine. Circulation. 2015;132:1920–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Esteva A, Robicquet A, Ramsundar B, et al. A guide to deep learning in healthcare. Nat Med. 2019;25:24–9. [DOI] [PubMed] [Google Scholar]
- [4].Goldman L, Cook EF, Johnson PA, et al. Prediction of the need for intensive care in patients who come to emergency departments with acute chest pain. N Engl J Med. 1996;334:1498–504. [DOI] [PubMed] [Google Scholar]
- [5].De A, Sarda A, Gupta S, et al. Use of artificial intelligence in dermatology. Indian J Dermatol. 2020;65:352–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Gyftopoulos S, Lin D, Knoll F, et al. Artificial intelligence in musculoskeletal imaging: current status and future directions. Am J Roentgenol. 2019;213:506–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Štern D, Payer C, Lepetit V, et al. Automated age estimation from hand mri volumes using deep learning. In: Cham, 2016, pp.194–202. Springer International Publishing. [Google Scholar]
- [8].Jamaludin A, Lootus M, Kadir T, et al. ISSLS PRIZE IN BIOENGINEERING SCIENCE 2017: automation of reading of radiological features from magnetic resonance images (MRIs) of the lumbar spine without human intervention is comparable with an expert radiologist. Eur Spine J. 2017;26:1374–83. 20170206. [DOI] [PubMed] [Google Scholar]
- [9].Wuni AR, Botwe BO, Akudjedu TN. Impact of artificial intelligence on clinical radiography practice: futuristic prospects in a low resource setting. Radiography (Lond). 2021;27 Suppl 1:S69–s73. 20210813 [DOI] [PubMed] [Google Scholar]
- [10].Oosterhoff JHF, Oberai T, Karhade AV, et al. Does the SORG orthopaedic research group hip fracture delirium algorithm perform well on an independent intercontinental cohort of patients with hip fractures who are 60 years or older? Clin Orthop Relat Res. 2022;480:2205–13. 20220510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Oosterhoff JHF, Doornberg JN; Machine Learning Consortium. Artificial intelligence in orthopaedics: false hope or not? A narrative review along the line of Gartner’s hype cycle. EFORT Open Rev. 2020;5:593–603. 20201026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Voelker R. Diagnosing fractures with AI. JAMA. 2018;320:23. [DOI] [PubMed] [Google Scholar]
- [13].Jassim SS, Benjamin-Laing H, Douglas SL, et al. Robotic and navigation systems in orthopaedic surgery: how much do our patients understand? Clin Orthop Surg. 2014;6:462–7. 20141110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Han XG, Tian W. Artificial intelligence in orthopedic surgery: current state and future perspective. Chin Med J (Engl). 2019;132:2521–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Harris AHS, Kuo AC, Bowe TR, et al. Can machine learning methods produce accurate and easy-to-use preoperative prediction models of one-year improvements in pain and functioning after knee arthroplasty? J Arthroplasty. 2021;36:112–117.e6. 20200720 [DOI] [PubMed] [Google Scholar]
- [16].Kamalapathy PN, Karhade AV, Tobert D, et al. Artificial intelligence in adult spinal deformity. Acta Neurochir Suppl. 2022;134:313–8. [DOI] [PubMed] [Google Scholar]
- [17].Rasouli JJ, Shao J, Neifert S, et al. Artificial intelligence and robotics in spine surgery. Global Spine J. 2021;11:556–64. 20200401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Castagno S, Khalifa M. Perceptions of artificial intelligence among healthcare staff: a qualitative survey study. Front Artif Intell. 2020;3:578983. 20201021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].De Simone B, Abu-Zidan FM, Gumbs AA, et al. Knowledge, attitude, and practice of artificial intelligence in emergency and trauma surgery, the ARIES project: an international web-based survey. World J Emerg Surg. 2022;17:10. 20220210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Karches KE. Against the iDoctor: why artificial intelligence should not replace physician judgment. Theor Med Bioeth. 2018;39:91–110. [DOI] [PubMed] [Google Scholar]
- [21].McDonald L, Ramagopalan SV, Cox AP, et al. Unintended consequences of machine learning in medicine? F1000Res. 2017;6:1707. 20170919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Oliveira ECL, van den Merkhof A, Olczak J, et al. An increasing number of convolutional neural networks for fracture recognition and classification in orthopaedics: are these externally validated and ready for clinical application? Bone Jt Open. 2021;2:879–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Innocenti B, Radyul Y, Bori E. The use of Artificial Intelligence in orthopedics: applications and limitations of machine learning in diagnosis and prediction. Appl Sci. 2022;12:10775. [Google Scholar]
- [24].Lee LS, Chan PK, Wen C, et al. Artificial intelligence in diagnosis of knee osteoarthritis and prediction of arthroplasty outcomes: a review. Arthroplasty. 2022;4:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Martin RK, Ley C, Pareek A, et al. Artificial intelligence and machine learning: an introduction for orthopaedic surgeons. Knee Surg Sports Traumatol Arthrosc. 2022;30:361–4. [DOI] [PubMed] [Google Scholar]
- [26].Naik N, Hameed BMZ, Shetty DK, et al. Legal and ethical consideration in artificial intelligence in healthcare: who takes responsibility? Front Surg. 2022;9:862322. 20220314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Armstrong JS, Overton TS. Estimating nonresponse bias in mail surveys. J Mark. 1977;14:396–402. [Google Scholar]
- [28].Duszynski TJ, Fadel W, Dixon BE, et al. Successive wave analysis to assess nonresponse bias in a statewide random sample testing study for SARS-CoV-2. J Public Health Manag Pract. 2022;28:E685–91. 20220209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Yu K-H, Beam AL, Kohane IS. Artificial intelligence in healthcare. Nat Biomed Eng. 2018;2:719–31. [DOI] [PubMed] [Google Scholar]
- [30].Lang JE, Mannava S, Floyd AJ, et al. Robotic systems in orthopaedic surgery. J Bone Joint Surg Br. 2011;93:1296–9. [DOI] [PubMed] [Google Scholar]
- [31].Hirschmann A, Cyriac J, Stieltjes B, et al. Artificial Intelligence in musculoskeletal imaging: review of current literature, challenges, and trends. Semin Musculoskelet Radiol. 2019;23:304–11. 20190604 [DOI] [PubMed] [Google Scholar]
- [32].Soffer S, Ben-Cohen A, Shimon O, et al. Convolutional neural networks for radiologic images: a radiologist’s guide. Radiology. 2019;290:590–606. 20190129 [DOI] [PubMed] [Google Scholar]
- [33].Oosterhoff JHF, Karhade AV, Oberai T, et al. Prediction of postoperative delirium in geriatric hip fracture patients: a clinical prediction model using machine learning algorithms. Geriatric Orthopaedic Surg Rehabil. 2021;12:215145932110622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Codari M. Impact of artificial intelligence on radiology: a EuroAIM survey among members of the European Society of Radiology. Insights Imag. 2019;10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Laï MC, Brian M, Mamzer MF. Perceptions of artificial intelligence in healthcare: findings from a qualitative survey study among actors in France. J Transl Med. 2020;18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Smith A. Public Predictions for the Future of Workforce Automation. 2016. Washington: Pew Research Center. [Google Scholar]