Abstract
Introduction
The objective of this study was to evaluate the economic impact of supply chain investment on the performance of the National Supply System of Essential Medicines in Sudan from 2011 to 2014.
Methods
This is a retrospective cross-sectional study designed from National Medical Supplies Fund documents. The cost-effectiveness analysis involved an economic evaluation of the performance of the supply chain system, with the cost calculated by using the activity-based costing method, by examining a supply chain according to its main components or functions including the cost of procurement, central storage, distribution and management, and administrative function. Effectiveness of supply chain investment was measured as an indicator of supply chain performance, which includes availability, coverage, affordability, and building capacity indicators. Statistical analysis was performed by using Microsoft Excel 2010, STATA (version 14) and the level of statistical significance was set at p < .05 for all analyses.
Results
The new system in 2014 (Model B), which reflects the performance of the system after the NMSF started investing more in the supply chain, will probably be more costly than the baseline system of 2011 (Model A) but will produce a much higher level of performance. The incremental cost-effectiveness ratios of moving from the baseline system of 2011 (Model A) to the new system in 2014 (Model B) were $286,826.02 per percentage of availability of medicines at the central warehouse; $310,728.18 per percentage of medicines procured that have a median price ratio of 1 or less than 1; $149,149.53 per percentage of public health institutions' coverage by National Medical Supplies Fund (NMSF) services; and $12,682.78 per number of NMSF staff trained. A paired t test showed that there was a statistically significant difference between the average cost-effectiveness ratios of the 2 models.
Conclusions
The investment in the supply chain had a significant impact on the performance of the National Supply System of Essential Medicines in Sudan. The new policies and interventions as embedded in the new 2014 model represent a more efficient and cost-effective approach, and a better performing system than the baseline model of 2011.
Keywords: cost-effectiveness analysis, medical supply chain, investment, policies
INTRODUCTION
Since the mid-1980s, research on economic growth has experienced a boom, beginning with the work of Romer in 1986.[1] The concept of capital in the neoclassical model can be usefully broadened from physical goods to include human capital in the form of education, experience, and health.[1] As with physical capital, health in the new growth theory is considered as human capital stock and can be increased through investment. This investment includes education and training, as well as the prevention and treatment of illness.[2] The money invested in the health supply chain has a direct impact on increasing the accessibility and affordability of medicines with an ultimate goal of better health, especially for developing countries that face many challenges in getting the essential drugs to patients at the right quantity and quality, at the right time, and at an affordable price.[3]
The economic objective of a drug supply system is to ensure the supply of safe, effective, good-quality drugs at the least possible cost to the people who need them.[4] An economic evaluation compares both the costs and the consequences of alternative courses of action as a way to guide decisions about the efficient use of scarce resources.[5] Economic evaluation is one of many useful ways to assess the performance of supply chains; it provides tools for analyzing the cost and benefit of a different intervention in the public health supply chain and can help distinguish which of several alternative interventions offers the greatest benefit compared with its cost to the health sector and society.[6]
The National Medical Supplies Fund (NMSF) is the national center for procurement, storage, and distribution of medical supplies in Sudan. NMSF is working on a cost-recovery system, to be in line with the cost-recovery policy implemented by the government at all health facilities in the public health sector in Sudan, since 1992. The range of medical supplies at NMSF includes medicines, vaccines, and other biological and medical consumables and a wide range of medical equipment.
All government medical supply organizations meet their needs from NMSF. The National Health Insurance Fund is one of the health finance mechanisms in Sudan and the main customer of NMSF; other organizations include Military Medical Services, Police Medical Services, and Revolving Drug Funds in Khartoum State.
In 2010, the health supply system at the regional and local levels suffered from inadequacy in its sustainability of supply of medicine and faced high prices as compared with the same medicine at the central level. Inefficiency in procurement systems and regulatory procedures unduly delayed the use of the needed medicines. Average availability in the states was less than 60%, requiring more effort to increase the distribution of essential medicines in the states at that time, and the average coverage was very low.[7] Therefore, in 2011 NMSF implemented a comprehensive reform program by instating new policies to ensure the availability, quality, and affordability of health commodities. It established NMSF branches in 16 states, with increasing geographic and financial access to high-quality drugs through the public sector, to ensure quality medicines across the country and to mandate that medicine prices be the same across the country, regardless of the distance from central stores.
This reform is in line with the national medicine policy, which aims to ensure the availability of safe, efficacious, quality medicines at a reasonable cost to society. According to the World Health Organization (WHO), the public expenditure on medicines is very low (about US $4 per capita per annum)[8]; the efficient use of inadequate resources is considered one of the major policies to increase the accessibility of essential medicines in Sudan. This study describes the performance of 2 health supply systems: the system in 2011, considered as Model A, and the system in 2014, considered as Model B.
The baseline system of 2011 (Model A) describes the performance of the supply chain function before implementation of the NMSF reform. In the selection of procured medicines, NMSF did not use the concept of evidence-based medicine or cost-effectiveness criteria when updating its list of medicines. NMSF procured medicines through a bidding process, concentrating only on low price. It previously distributed medicines from Port Sudan to a central warehouse by using rental vehicles, which were not well suited to ensuring quality and good distribution practices, as medicines were delivered in open trucks with minimum protection from dust and weather conditions. As for storage and inventory, the control of humidity and temperature in its warehouses was managed by manual register twice daily. The model showed absence of an integrated Management Information System (MIS) and described the generation of a general report with procurement and supply management indicators.
For the new system in 2014 (Model B), NMSF started investing more in the supply chain to achieve the desired goal of getting a full and consistent supply of essential medicines to patients at the right quantity and quality, at the right time, and at an affordable price with assured quality. In this system, different approaches to the new policies and interventions were implemented in the supply chain function and cycle. All of the new approaches mentioned are summarized in a report titled Reform of the National Health Supply Chain in Sudan: Achievement, Challenges, Success Factors, and Lesson Learned (2nd edition).[7] In the first intervention for the selection process, NMSF pharmacists updated the NMSF list of medicines according to the criteria of cost-effectiveness, concentrated on the National Essential Drug List, National Health Programs, relied on evidence-based medicine, and implemented WHO essential medicine policy. Secondly, NMSF introduced a new policy in procurement function, aiming to increase the efficiency of procurement and achieve affordable pricing for the patient. This policy involved the reduction of costing and markup of medicines and other health commodities, a cross-subsidization mechanism, long-term contracting, and unified retail prices in all NMSF branches in the state (free cost of transportation), with the establishment of a committee to negotiate with the winner, for further discount and differed payment, to make sure that the supplies meet the stated specifications in the tender document, pooled electronic procurement, and procurement of registered medicines. In the third intervention for transportation function, NMSF contracted with an outsource service for transportation of medical products, which uses temperature-controlled vehicles to ensure the quality of medicines during transportation; these vehicles are equipped with a data logger. Fourth, NMSF invested in storage and inventory control management by introducing a new system to control and measure the humidity and temperature of its warehouses by the second. Fifth, NMSF set up a logistic MIS to coordinate, monitor, and support all logistics activities for the various commodity groups, as well as to improve data and information uses for calculating various indicators to assess the performance of the supply chain in order to achieve better health outcomes. The sixth intervention was conducted when NMSF decided to invest more in human resources to improve capacity building. It established a comprehensive training program with national and international institutions and universities, which specialize in strengthening the health supply chain.
The aim of this research is to evaluate the economic impact of supply chain investment on the performance of the National Supply System of Essential Medicines in Sudan from 2011 to 2014 from a management perspective. Specifically, to determine the cost-effectiveness of investing in supply chain strengthening to enhance the accessibility of essential medicines and to explain the effect that implementing NMSF's reform program had on its performance after increasing its investment in the supply chain.
METHODS
Study Design
This is a retrospective, cross-sectional study based on NMSF's documents, researched with the archives available on hard records; an electronic record was undertaken by the researchers.
In this study, we compared the cost-effectiveness of 2 systems in the National Health Public Supply Chain. The first is considered the baseline system of 2011 (Model A) and the second is the new system of 2014 (Model B).
The baseline system in 2011 (Model A)
The baseline system described the performance of the supply chain function in 2011 before the implementation of the NMSF reform.
The new system in 2014 (Model B)
In the new system of 2014, NMSF started investing more in the supply chain to achieve the desired goal of getting a full and consistent supply of essential medicines to patients. In this system, different approaches to interventions have been implemented in the supply chain function.
Study Instrument and Tools
The research was conducted by using cost-effectiveness analysis for economics evaluation of the performance of the supply system, with the use of the following tools.
Cost-effectiveness analysis
The cost of the supply chain at the central level of the NMSF in Khartoum State was estimated until the point of distribution of medicines to the warehouses of NMSF's branches at the state level. The costs of a supply chain investment included a combination of resources: equipment, labor, supplies, infrastructure, vehicles, and others, in the functions of the supply chain.
The effectiveness of supply chain investment measured as an indicator of supply chain performance includes the core indicators for procurement and supply management systems. The indicators of supply chain performance developed by MSH (2013) and WHO (2011) were selected and used in this study, which include availability, coverage, affordability, and building capacity; these indicators were used as a measure of supply effectiveness.[6,9]
Average cost-effectiveness ratios (ACERs)
ACER divides the total cost by the total effectiveness of an intervention. The ACER is calculated as follows: ACER = (Total Cost of Intervention) ÷ (Total Effectiveness of Intervention).
Incremental cost-effectiveness ratios (ICERs)
The ICER is calculated as follows: ICER = (Cost of Intervention A – Cost of Intervention B) ÷ (Effectiveness of Intervention A – Effectiveness of Intervention B).
Economic Evaluation of Public Health Supply Chain Model
A framework to facilitate the application of economic evaluation to public health supply chains developed by USAID | DELIVER PROJECT for the WHO (2009) was used after introducing a simple modification involving additional costing tools.[6] This framework provided a macroeconomics estimate of supply chain costs and is intended to give an idea of the total costs of the supply chain in delivering essential medicines; it estimated the cost by using the activity-based costing method, by examining a supply chain according to its main components or functions including the cost of procurement, central storage, distribution and management, and administrative support.
Data Collection Procedure
Data were collected for 2 years: 2011 and 2014. The cost was measured from survey data and from a budgetary document and NMSF's automation program (Enterprises Resources Planning), widely known as ERP. Effectiveness in term of availability, affordability, coverage, and quality indicator was measured from a document in the NMSF automation program (ERP) such as stock card, physical count reports, documents and statistical data in NMSF tender reports and NMSF annual reports, which were analyzed to evaluate changes in many areas before and after the intervention in different supply functions such as procurement, storage, distribution, human resources, and finance.
Data were collected from the 2nd edition of the book titled Reform of the National Health Supply Chain in Sudan: Achievement, Challenges, Success Factors, and Lesson Learned,[7] which was published by the authors and their colleagues in 2015; this book has been used as the basis for this study.
Data Analysis
Data for cost and effectiveness were checked to ensure completeness. Data were analyzed with the computer program Microsoft Excel 2010, STATA version 14 (Microsoft, Redmond, Washington, United States); and the level of statistical significance was set at p < .05 for all analyses. Descriptive statistics were used in the form of count, percentage, ratio, and average for the same elements of the 2 models under study.
Inferential statistics as complementary measures were used for informed decision making. A paired 2-sample t test for the average cost-effectiveness ratios as an inferential statistical test was used to determine whether there is a statistically significant difference between the 2 models and to measure the performance of the supply system before and after introducing the new policies and interventions.
RESULTS
Measuring Cost of Supply Chain
The cost was calculated by using the activity-based costing method. ABC assigned the direct cost and indirect cost of each activity to determine the cost of procurement, central storage, distribution, and management and administrative function (Table 1).
Table 1.
Overall cost of supply chain in 2011 and 2014
| Measure |
Model |
|||
| Baseline System in 2011 (Model A) |
New System in 2014 (Model B) |
|||
| Cost: |
Value/US$ |
% |
Value/US$ |
% |
| Procurement cost | 8,057,068.87 | 34% | 6,876,516.99 | 22% |
| Storage cost | 11,029,206.05 | 46% | 12,091,731.02 | 38% |
| Distribution and transportation costs | 1,235,932.17 | 5% | 9,245,819.89 | 29% |
| Management and administrative support cost | 3,493,796.31 | 15% | 3,228,156.69 | 10% |
| Total supply chain cost | 23,816,003.40 | 100% | 31,440,665.87 | 100% |
Procurement costs
These costs include bank charges, salaries and incentives of procurement staff, overtime, tender committee sundries, shortage cost of health commodities, clearance, stationary, computer, and communication.
Storage costs
In this study, storage costs represent the expense of conducting the storage activities at the central level, which include storage space, equipment and machine depreciation, salaries and incentives of warehousing staff, repair and maintenance of warehouses, rented warehouses, depreciation of buildings and instruments (such as forklifts), electricity, insurance (assets and inventory), and the cost of expired and damage medicines.
Distribution and transportation costs
Costs of distribution and transportation include unit between storage points at the central level until distribution of medicines to the warehouses of the NMSF branches at the state level, fuel, depreciation of vehicles and equipment, repair and maintenance of vehicles, shipping and discharge, insurance, and supervision.
Management and administrative support cost
Management operating costs include costs of training, logistics management information system (LMIS), supporting network and ERP systems, salaries and incentives of staff workers in supportive departments in NMSF.
Measuring the Consequences of Supply Chain
Effectiveness of supply chain investment measured as an indicator of supply chain performance includes some of the core indicators for procurement and supply management systems (Table 2).
Table 2.
Procurement and supply indicators
|
Description
|
Indicator
|
References
|
| Procurement efficiency | The ratio between the median price of medicines procured and the international median reference value (target ≤1) | WHO (2011). Harmonized Monitoring and Evaluation Indicators for Procurement and Supply Management Systems: Early-Warning Indicators to Prevent Stock-Outs and Overstocking of Antiretroviral, Antituberculosis and Antimalarial Medicines |
| Availability | Percentage of items available per total number of NMSF items | *MSH. MDS-3: Managing Access to Medicines and Health Technologies. 3rd ed. West Hartford, CT: Kumarian Press; 2013 |
| *WHO (2011). Harmonized Monitoring and Evaluation Indicators for Procurement and Supply Management Systems: Early-Warning Indicators to Prevent Stock-Outs and Overstocking of Antiretroviral, Antituberculosis and Antimalarial Medicines | ||
| Coverage | Percentage of coverage of NMSF services among public institutions | WHO (2007). Operational package for assessing, monitoring, and evaluating country pharmaceutical situations |
| Improving capacity building | Number of staff responsible for PSM who have been trained in PSM | WHO (2008). Harmonized Monitoring and Evaluation Indicators for ARV Procurement and Supply Management Systems |
MSH, Managment Sciences for Health; NMSF, National Medical Supplies Fund; WHO, World Health Organization
Availability of essential medicine
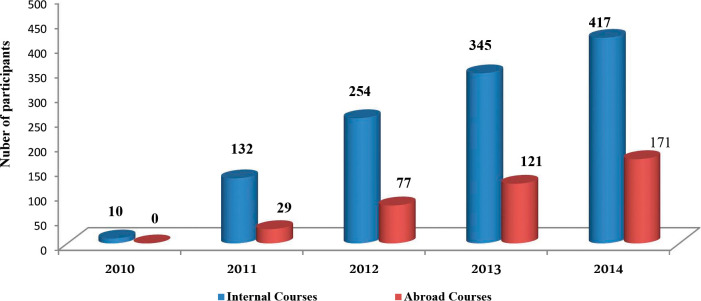
Stock availability is commonly thought of as a bottom-line measure of performance.[3] The availability of essential medicines at central NMSF warehouses increased from 66% in 2011 to 92% in 2014. At the state level, the availability of medicines increased from 66.7% to 86% (Figure 1).
Figure 1.
Availability of medicines at NMSF's central warehouses.
Procurement efficiency: comparison with international price indicator
According to WHO (2007), prices of publicly procured medicines are considered acceptable “if they have a median price ratio of 1 or less than 1, which means that price of the awarded medicine is the same or less than IRP (International Reference Price) of the same medicine.”[9] The analysis of the price of medicines available through NMSF showed that 77% of medicines procured in 2014 had a median price ratio of 1 or less than 1, compared to only 53% of medicines procured in 2011 with a median price ratio of 1 or less than 1.
Coverage of NMSF services among public institutions
As shown in Table 3, the coverage of NMSF services among public institutions in 2011 and 2014 increased by 20% for hospital coverage and by 7% for primary health care coverage.
Table 3.
Coverage of NMSF services among public institutions in 2011 and 2014
| No. |
Name of State |
Hospital Coverage |
Primary Health Care Center Coverage |
||
| 2011 |
2014 |
2011 |
2014 |
||
| 1 | River Nile | 45% | 45% | 52% | 10% |
| 2 | Sennar | 88% | 100% | 21% | 70% |
| 3 | Kassala | 39% | 100% | 65% | 88% |
| 4 | Blue Nile | 53% | 93% | 40% | 24% |
| 5 | White Nile | 86% | 100% | 2% | 42% |
| 6 | North Darfur | 10% | 31% | 1% | 4% |
| 7 | South Darfur | 28% | 35% | 0% | 4% |
| 8 | East Darfur | 50% | 57% | 0% | 0% |
| Average | 50% | 70% | 23% | 30% | |
Improving capacity building
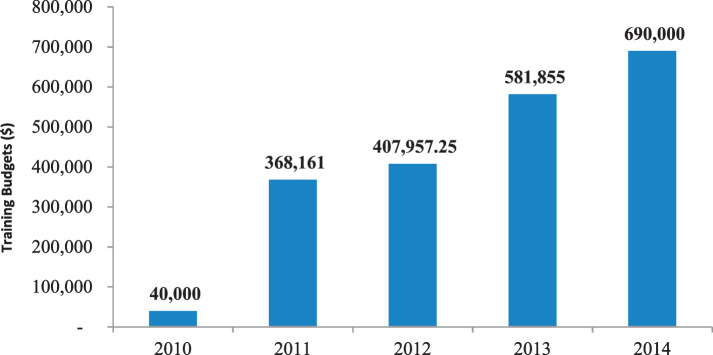
NMSF has started a comprehensive external and internal training program for its staff with different professional disciplines, resulting in an increase in the number of staff trained: from only 10 in 2010 to more than 580 in 2014 (Figure 2).
Figure 2.
Human resource developments in NMSF.
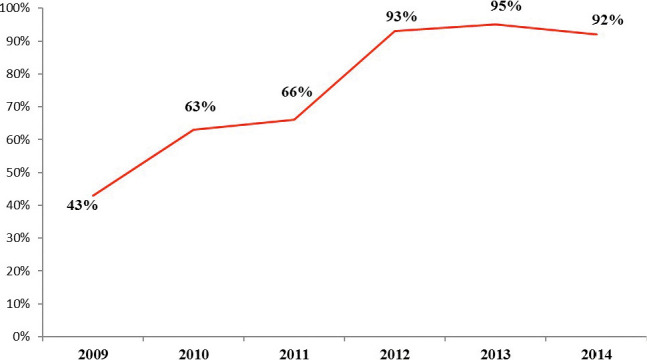
As shown in Figure 3, NMSF increased the training budget: from less than US $40,000 in 2010 to US $690,000 in 2014.
Figure 3.
NMSF training budgets ($) from 2010 to 2014.
Cost-effectiveness Analysis of Health Public Supply Chain Investments
Average cost-effectiveness ratio analysis
To explore and find the most cost-effective system between the baseline system in 2011 and the new system in 2014 after NMSF started investing more in the supply chain, ACER analysis was conducted (Table 4).
Table 4.
Cost-effectiveness analysis of health public supply chain investments
|
Measure
|
Model
|
|
| Baseline system in 2011 (Model A) |
New system in 2014 (Model B) |
|
| Cost | ||
| Total supply chain cost | US $23,816,003.40 | US $31,440,665.87 |
| Effectiveness | ||
| Percentage of availability of medicines at central warehouse | 66% | 92% |
| Percentage of medicines procured that have a median price ratio of 1 or less than 1 | 53% | 77% |
| Percentage of public health institutions' coverage by NMSF services | 36.5% | 50% |
| Number of NMSF staff trained | 161 | 588 |
| Average cost-effectiveness ratios | ||
| Cost per percentage of availability of medicines at central warehouse | $360,848.54 | $341,746.37 |
| Cost per percentage of medicines procured that have a median price ratio of 1 or less than 1 | $449,358.55 | $408,320.34 |
| Cost per percentage of public health institutions' coverage by NMSF services | $652,493.24 | $628,813.32 |
| Cost per number of NMSF staff trained | $147,925.49 | $53,470.52 |
| Incremental cost-effectiveness ratios | ||
| Cost per percentage of availability of medicines at central warehouse | $286,826.02 | |
| Cost per percentage of medicines procured that have a median price ratio of 1 or less than 1 | $310,728.18 | |
| Cost per percentage of public health institutions' coverage by NMSF services | $149,149.53 | |
| Cost per number of NMSF staff trained | $12,682.78 | |
NMSF, National Medical Supplies Fund
Incremental cost-effectiveness ratio
The new system in 2014 was more effective but at a high price; therefore, there is a need to conduct an ICER analysis (Table 4).
DISCUSSION
The main finding of this study was that the new system in 2014 (Model B) will probably be more costly than the baseline system of 2011 (Model A), but will produce a much higher level of performance, as measured by availability, coverage, affordability, and building capacity. A paired t test of the mean showed statistical significance between the average cost-effectiveness ratios for these 2 models. This indicates that the intervention and investment in 2014 by NMSF resulted in a more efficient, better-performing system.
In this study, the cost-effectiveness of 2 systems in the health public supply chain was compared. The first in 2011 is considered a baseline system (Model A), whereas the new system (Model B) in 2014 was implemented after NMSF started investing more in the supply chain to achieve the desired goals of getting a full and consistent supply of essential drugs to patients at the right quantity and quality, at the right time, and at an affordable price with assured quality. Cost-effectiveness was calculated by the 2 principal measures of cost-effectiveness, namely ACER and ICER.
The new system in 2014 (Model B) had lower average cost-effectiveness ratios than the baseline system in 2011 (Model A), as measured by cost per percentage of availability of medicines at the central warehouse ($360,848.54 versus $341,746.37), per percentage of medicines procured that have a median price ratio of 1 or less than 1 ($449,358.55 versus $408,320.34), per percentage of public health institutions' coverage by NMSF services ($652,493.24 versus $628,813.32), and per number of NMSF staff trained ($147,925.49 versus $ 53,470.52) (refer to Table 4).
The incremental cost-effectiveness ratios of moving from the baseline system in 2011 (Model A) to the new system in 2014 (Model B) were $286,826.02 per percentage of availability of medicines at the central warehouse; $310,728.18 per percentage of medicines procured that had a median price ratio of 1 or less than 1; $149,149.53 per percentage of public health institutions' coverage by NMSF services; and $12,682.78 per number of NMSF staff trained.
The cost of the supply chain provides useful information and guidance for policy-makers in order to understand the best way of delivering health commodities to the end point, that is, the service delivery point.[10] The USAID | DELIVER PROJECT has developed a supply chain costing approach with appropriate tools, which has been applied in Nigeria, Rwanda, Zambia, and Zimbabwe.[10]
After obtaining the cost of the supply chain, it is possible to conduct economic evaluations as cost-effectiveness and cost-benefit analysis to analyze supply chain investments. Therefore, better knowledge of costs will lead to stronger and more sustainable public health supply chains.[10]
According to this study, the total cost of health commodities supply chains was US $23,816,003.40 in 2011 and US $31,440,665.87 in 2014. Based on the cost analysis for each supply chain function as a percentage of the total supply-chain cost for NMSF in 2 years, the procurement cost decreased from 34% in 2011 to 22% in 2014, storage cost decreased from 46% to 38%, the cost of administration and management function decreased from 15% in 2011 to 10% in 2014, while the cost of transportation and distribution increased from 5% in 2011 to 29% in 2011. This result complies with NMSF's plan to increase the investment in transportation and distribution, aiming to ensure the quality and increase the accessibility and affordability of their health commodities distributed among different states in Sudan.
As evidenced from the international published literature, the effectiveness of supply chain investment is measured as an indicator of supply chain performance, which includes measuring the indicator of availability, coverage, affordability, and building capacity.[3,9]
Medicine availability and prices in both public and private sectors are key indicators of access to treatment, as low availability and unaffordable prices are a key barrier to access to medicines. According to surveys of medicine prices and availability, conducted by using a standard methodology, public sector availability of generic medicines is less than 60% across WHO regions, ranging from 32% in the Eastern Mediterranean region to 58% in the European region. Availability of generic medicines is higher in the private sector than in the public sector in all regions. However, availability is still less than 60% in the Western Pacific, South-East Asian, and African regions.[11] A study from Sudan in 2014 showed that the availability of key medicines was low in all sectors; it was 40% to 50% as generics, depending on the different sectors in Sudan.[12]
Availability in the NMSF at the central and state level has been increased after increasing the investment in the supply chain function. The percentage of availability of medicines at central NMSF warehouses increased from 66% in 2011 to 92% in 2014, while at the state level the availability of key medicines for 53 items increased from 66.7% to 86%. This remarkable increase in availability was achieved by improving the efficiency and good management of the supply chain cycle in terms of the selection, quantification, procurement, and distribution of health commodities.
One of the most important reasons for improvement in availability is the fact that NMSF established the electronic logistics management information system (e-LMIS). It provided NMSF with adequate data and information for calculating medicine consumption by using an accurate electronic record, and for issuing an alert by sending a message when the stock reaches its reordering point, resulting in better forecasting and better quantification. E-LMIS improves the health system by providing information, knowledge, and tools about all functions in the health supply chain system. It supports investment in and benefits. It is currently being used in other African countries such as Tanzania and Nigeria.[13,14]
The percentage of coverage of NMSF services among public health care facilities varies considerably among the 8 states that were included in the study. Hospital coverage by NMSF services increased on average from 50% in 2011 to 70% in 2014. The coverage of hospitals in the states was found to range from 100% in Kassala, Sennar, and White Nile, to 31% in North Darfur. In the Darfur states (conflict area), the coverage was found to be lower than in other states. However, with respect to NMSF services' coverage in the primary health centers, it increased on average from 23% to 30%; it varies between 88% and 0% in East Darfur. Generally, the percentage of coverage of NMSF services increased among health institutions. Hospital coverage increased by 20% and primary health care coverage increased by 7%, as a consequence of implementing good distribution practices and routine supervision of the states.
The availability of low-priced but effective medicines is important to ensure medicine accessibility and use.[9] The public sector through NMSF procures about 35% of all medicines consumed in Sudan. NMSF aims to procure medicines at prices that will not be an obstacle to preventing accessibility of medicines and aims to ensure high benefit from the budget allocated by the government for public free-medicine projects, that is, NMSF will plan the medicine procurement process in order to achieve its objective: the value of money.
NMSF established a new policy in the procurement process; one of these policies is the implementation of pooled procurement, to encourage generic competition and gain access to cheaper sources of drugs, differential pricing, and creation of high volume or high demand. NMSF has launched a new model for a unified supply system of medicines, to all states.
An efficient program obtains the best prices by using reference price benchmarks and reliable deliveries of good-quality pharmaceuticals from suppliers.[9] NMSF uses an indicator to measure the efficiency of procurement practices by comparing the prices paid for medicines with international price standards. The international price indicator is published by MSH in its methodology. This price indicator is used to compare prices of generic medicines with those of the proprietary medicines and prices of selected medicines with those cited in the International Price Indicator (widely known as IRP), published by Management Sciences for Health. In the case of publicly procured generic medicines, prices were considered “acceptable” if they had a median price ratio of 1 or less, which means that the price of the generic medicine was the same or less than the IRP for the same medicine. The analysis of the price of medicines available by NMSF showed that 77% of medicines procured in 2014 had a price ratio of 1 or less, compared to 53% of medicines procured in 2011 with a price ratio of 1 or less.
Recently, a number of developing countries used the concept of investment in human capital in order to choose between different courses of action in their pursuit of public health goals, including activities to strengthen the health system (Rosen[3]). To this end, the NMSF invested considerable resources in staff development and capacity building, resulting in an increase in the NMSF training budget, from less than US $40,000 to US $670,000 in 2014.
NMSF is keen to provide continuous and effective training inside and outside the country by continuing to participate in regional and international meetings, workshops, and conferences, which will be positively reflected in the development of the workforce, with the number of staff trained increasing from only 10 in 2010 to more than 580 in 2014. The outcomes of the comprehensive training program are clearly reflected in NMSF's performance, which is measured by highly improved supply chain performance indicators such as the indicator of availability, coverage, affordability, and quality of medicines.
Study Limitations
The cost of supply analysis encompassed the central level of the NMSF in Khartoum State until distribution of medicines to the warehouses of the NMSF branches at the state level only, due to lack of information at the time of the study.
Two of the researchers are staff members of NMSF, which raises the possibility of bias; however, the information gathered in the study is taken from documents such as stock records, tender document, and financial reports, all of which are carefully reviewed by governmental committees including representatives from the Ministry of Finance, and general and internal auditors, which increases the credibility of the results presented.
CONCLUSION
The investment in the supply chain had a significant impact on the performance of the National Supply System of Essential Medicines in Sudan. The new policies and interventions as embedded in the new 2014 model represent a more efficient and cost-effective approach, and a better-performing system than the baseline model of 2011.
In conclusion, the study results show that it is worthwhile for the NMSF to invest in supply chain strengthening. The NMSF as the largest public medicine supply agency in Sudan used the concept of the value of money to improve its performance and to ensure more spending and investment in the supply chain, which maximized benefit to the patient in terms of money spent on the supply chain system in Sudan.
This study is the first evaluation of its kind in Sudan. Findings and related considerations will be of interest to policy-makers and researchers. Strategies and interventions that have been adopted in recent years have had a good impact on the current performance of the NMSF, and the study will be used as baseline information to further research and strategies related to the economic evaluation of the health supply system in Sudan.
Funding Statement
Source of Support: None.
Footnotes
Conflict of Interest: None.
References
- 1.Barro R. Health and Economic Growth. Geneva, Switzerland: World Health Organization; 1996. [Google Scholar]
- 2.Gardner H, Gardner D. Health as Human Capital Theory and Implications A New Management Paradigm. Cheyenne, Wyoming: HCMS Group; 2001. [Google Scholar]
- 3.Rosen J. Economic Evaluation Guide to Approaches for Public Health Supply Chains. Arlington, Virginia: USAID; 2014. [Google Scholar]
- 4.Dumoulin J, Kaddar M, Velasquez G. Guide to Drug Financing Mechanisms. Geneva: World Health Organization; 1998. [Google Scholar]
- 5.Drummond MF, Sculpher MJ, Claxton K, Stoddart GL, Torrance GW. Methods for the Economic Evaluation of Health Care Programmes. Oxford, England: Oxford University Press; 2015. [Google Scholar]
- 6.Managment Sciences for Health. MDS3 Managing Access to Medicines and Health Technologies 3rd ed. West Hartford, CT: Kumarian Press; 2013. [Google Scholar]
- 7.National Medical Supplies Fund. Reform of the National Health Supply Chain in Sudan Achievements Challenges Success Factors and Lessons Learned 2nd ed. Khartoum, Sudan: NMSF; 2015. [Google Scholar]
- 8.World Health Organization. The World Health Situation. Geneva: WHO; 2004. [Google Scholar]
- 9.World Health Organization. Harmonized Monitoring and Evaluation Indicators for Procurement and Supply Management Systems EarlyWarning Indicators to Prevent StockOuts and Overstocking of Antiretroviral Antituberculosis and Antimalaria Medicines. Geneva: WHO; 2011. [Google Scholar]
- 10.Sarley D, Allain L, Akkihal A. Estimating the Global InCountry Supply Chain Costs of Meeting the MDGs by 2015. Arlington, VA: USAID | DELIVER PROJECT, Task Order; 2009;1. [Google Scholar]
- 11.Cameron A, Ewen M, Auton M, Abegunde D. The World Medicines Situation 2011 Medicines Prices Availability and Affordability. Geneva: World Health Organization; 2011. [Google Scholar]
- 12.Kheder SI, Ali HM. Evaluating medicines prices, availability, affordability and price components in Sudan. Sudan Med Monit. 2014;9:19. [Google Scholar]
- 13.USAID. Putting Cost Into the Equation Case Examples of Economic Evaluation of Public Health Supply Chains in Three African Countries. Arlington, VA: USAID | DELIVER PROJECT, Task Order 4; 2015. [Google Scholar]
- 14.Kamunyori Joy, Ahmed M. Nigeria Readiness Assessment for an Electronic Logistics Management Information System in Bauchi State. Arlington, VA: USAID | DELIVER PROJECT, Task Order 4; 2012. [Google Scholar]