Abstract
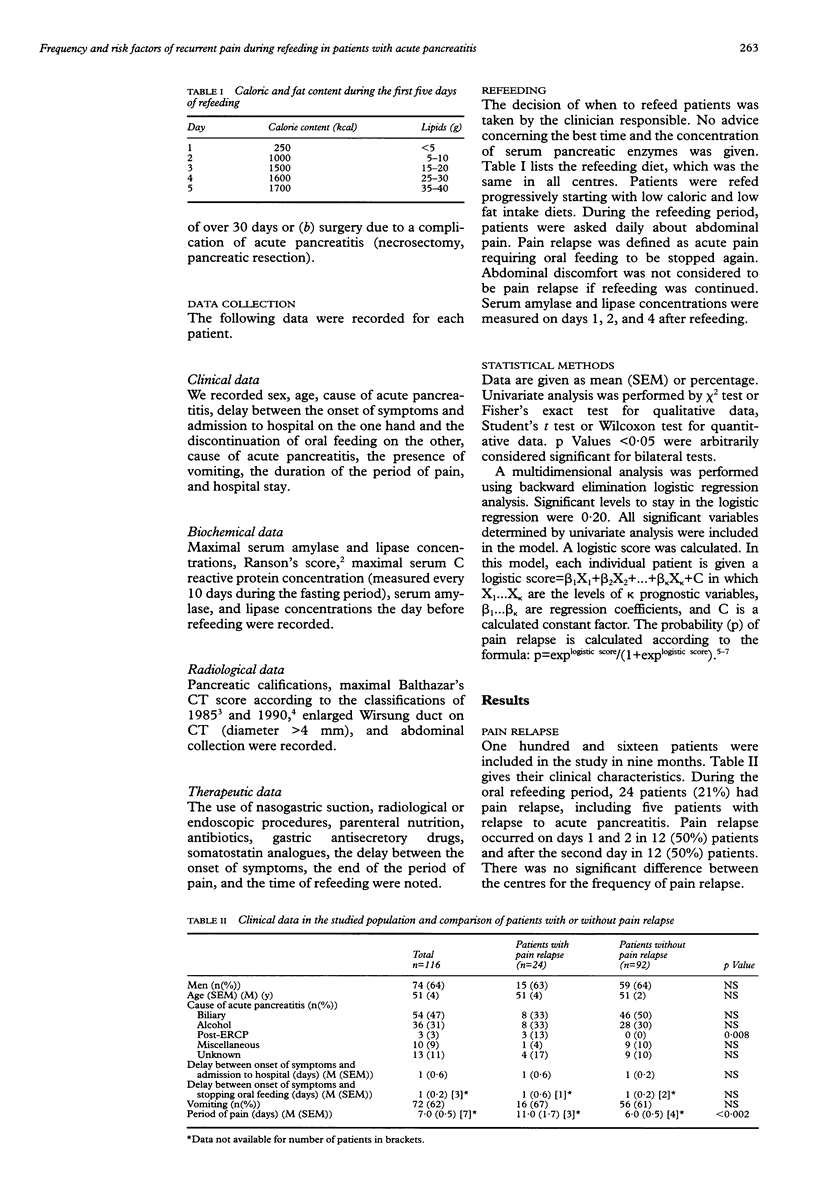
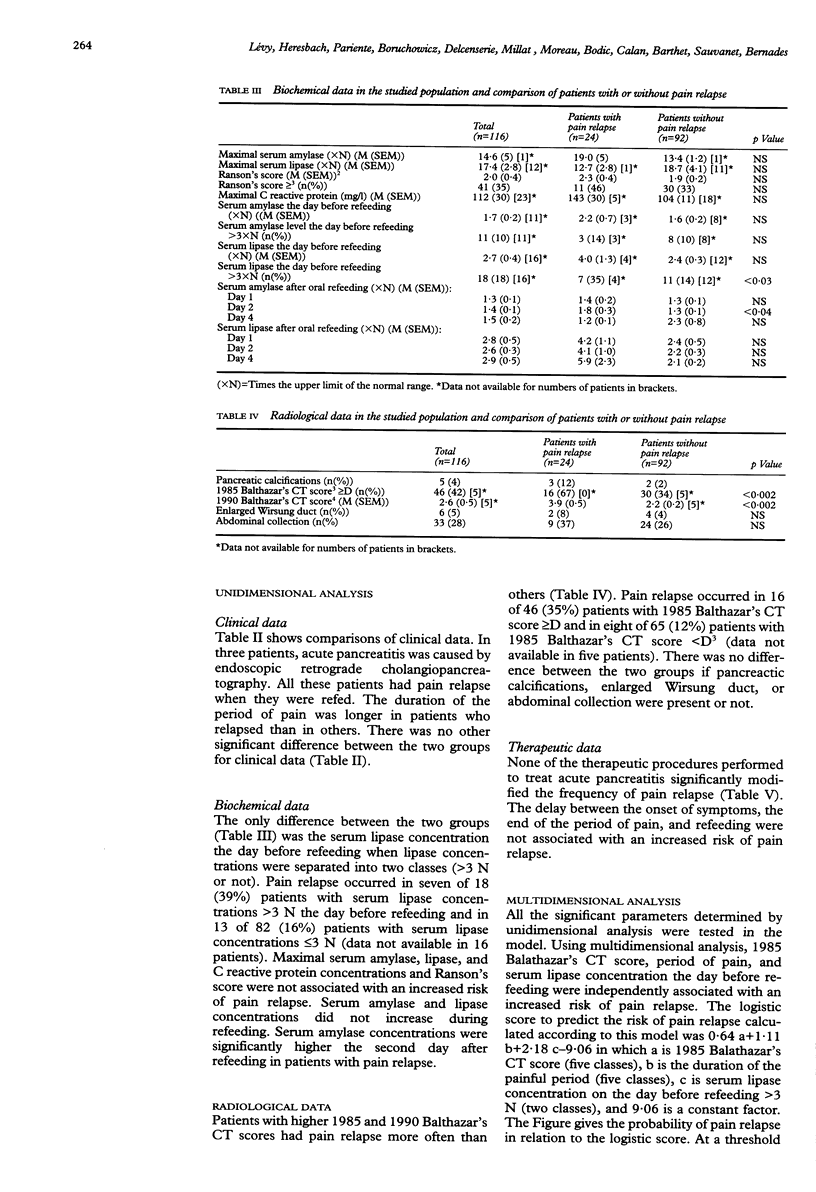
BACKGROUND/AIMS: The period of refeeding in patients with acute pancreatitis is critical because they may have pain relapse. A multicentre, multidimensional, prospective study was performed to assess the frequency and the risk factors of pain relapse in these patients. METHODS: Patients were included if they had acute pancreatitis severe enough to stop oral feeding for more than 48 hours. Clinical, biochemical, radiological, and therapeutic data were prospectively recorded and analysed by unidimensional and multidimensional analysis. The moment to refeed patients was chosen by the clinician but the diet was the same in all centres. RESULTS: A total of 116 patients were included with a Ranson's bioclinical score > or = 3 in 35% and a Balthazar's CT score > or = D in 42%. The cause of acute pancreatitis was biliary in 47% and alcohol misuse in 31%. During the oral refeeding period, 21% of the patients had pain relapse. This occurred on days 1 and 2 in 50% of patients. The duration of the painful period was longer in patients who relapsed than in others (p < 0.002). Pain relapse occurred in 39% of patients with a serum lipase concentration > 3x the upper limit of the normal range the day before refeeding and in 16% of other patients (p < 0.03). Patients with higher Balthazar's CT scores had pain relapse more often than the others (p < 0.002). None of the therapeutic procedures significantly modified the frequency of pain relapse. Using multidimensional analysis, Balathazar's CT score, period of pain, and serum lipase concentration the day before refeeding were independently associated with an increased risk of pain relapse. At a threshold of 0.5, a logistic score had a 37% sensitivity, 95% specificity, and 83% accuracy to predict pain relapse. Pain relapse nearly doubled total hospital stay and hospital stay after the first attempt at oral refeeding. CONCLUSION: Pain relapse occurred in one fifth of the patients with acute pancreatitis during oral refeeding and was more common in patients with necrotic pancreatitis and with longer periods of pain. The results of this study can be used to predict high risk patients and are a first step in the prevention of pain relapse.
Full text
PDF


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Balthazar E. J., Ranson J. H., Naidich D. P., Megibow A. J., Caccavale R., Cooper M. M. Acute pancreatitis: prognostic value of CT. Radiology. 1985 Sep;156(3):767–772. doi: 10.1148/radiology.156.3.4023241. [DOI] [PubMed] [Google Scholar]
- Balthazar E. J., Robinson D. L., Megibow A. J., Ranson J. H. Acute pancreatitis: value of CT in establishing prognosis. Radiology. 1990 Feb;174(2):331–336. doi: 10.1148/radiology.174.2.2296641. [DOI] [PubMed] [Google Scholar]
- Ranson J. H., Rifkind K. M., Roses D. F., Fink S. D., Eng K., Spencer F. C. Prognostic signs and the role of operative management in acute pancreatitis. Surg Gynecol Obstet. 1974 Jul;139(1):69–81. [PubMed] [Google Scholar]
- Ranson J. H. The timing of biliary surgery in acute pancreatitis. Ann Surg. 1979 May;189(5):654–663. doi: 10.1097/00000658-197905000-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viedma J. A., Pérez-Mateo M., Agulló J., Domínguez J. E., Carballo F. Inflammatory response in the early prediction of severity in human acute pancreatitis. Gut. 1994 Jun;35(6):822–827. doi: 10.1136/gut.35.6.822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson C., Heath D. I., Imrie C. W. Prediction of outcome in acute pancreatitis: a comparative study of APACHE II, clinical assessment and multiple factor scoring systems. Br J Surg. 1990 Nov;77(11):1260–1264. doi: 10.1002/bjs.1800771120. [DOI] [PubMed] [Google Scholar]



