Abstract
The β-hemoglobinopathies, such as sickle cell disease and β-thalassemia, are one of the most common genetic diseases worldwide and are caused by mutations affecting the structure or production of β-globin subunits in adult hemoglobin. Many gene editing efforts to treat the β-hemoglobinopathies attempt to correct β-globin mutations or increase γ-globin for fetal hemoglobin production. δ-globin, the subunit of adult hemoglobin A2, has high homology to β-globin and is already pan-cellularly expressed at low levels in adult red blood cells. However, upregulation of δ-globin is a relatively unexplored avenue to increase the amount of functional hemoglobin. Here, we use CRISPR-Cas9 to repair non-functional transcriptional elements in the endogenous promoter region of δ-globin to increase overall expression of adult hemoglobin 2 (HbA2). We find that insertion of a KLF1 site alone is insufficient to upregulate δ-globin. Instead, multiple transcription factor elements are necessary for robust upregulation of δ-globin from the endogenous locus. Promoter edited HUDEP-2 immortalized erythroid progenitor cells exhibit striking increases of HBD transcript, from less than 5% to over 20% of total β-like globins in clonal populations. Edited CD34 +hematopoietic stem and progenitors (HSPCs) differentiated to primary human erythroblasts express up to 46% HBD in clonal populations. These findings add mechanistic insight to globin gene regulation and offer a new therapeutic avenue to treat β-hemoglobinopathies.
Research organism: Human
Introduction
Red blood cells, also known as erythrocytes, are packed with hemoglobin and circulate the body to supply all organs with oxygen. Hemoglobin is a hetero-tetrameric protein made up of two α-like and two β-like subunits. Hemoglobin A1 (HbA1) accounts for approximately 97% of the hemoglobin expressed in adults and is composed of two α-globin subunits (HBA) and two β−globin (HBB) subunits. Hemoglobin A2 (HbA2) accounts for the remaining 2–3% of hemoglobin expressed in adults and is composed of two α-globin subunits and two δ-globin (HBD) subunits Steinberg and Rodgers, 2015.
The β-hemoglobinopathies, such as sickle cell disease (SCD) and β-thalassemia, are caused by mutations in HBB that effect the structure or expression of β-globin. The clinical hallmarks include hemolytic anemia and vaso-occlusion, which can lead to acute and chronic pain and organ damage. Clinical management is limited to frequent blood transfusions and life-long treatment of anemia and pain crises. The only curative approach is allogeneic stem cell transplantation, which is dependent upon HLA-identical donor availability Locatelli et al., 2013. Fetal hemoglobin (HbF), which is the predominant hemoglobin expressed before birth, has anti-sickling properties and its re-expression is frequently pursued as a treatment for β-hemoglobinopathies Wienert et al., 2018. While increasing HbF has shown to be clinically effective to combat SCD, studies have also validated the in vitro and in vivo anti-sickling abilities of δ-globin using a humanized mouse model of SCD Nagel et al., 1979; Poillon et al., 1993; Porcu et al., 2021; Waterman et al., 1979.
Increased HbA2 expression has some potential advantages over HbF that suggests it could provide an alternative avenue for ameliorating the β-hemoglobinopathies. HbA2 is weakly transcriptionally active and expressed pancellularly in all adult red blood cells Heller and Yakulis, 1969; Steinberg, 2021. Additionally, δ-globin shares 93% amino acid homology to β-globin, suggesting that HbA2 may be a better replacement relative to HbF, whose γ-globin subunit shares 73% amino acid homology to β-globin. Finally, HbF is known to bind oxygen more tightly than HbA1, an evolutionary advantage for the fetus to draw oxygen from the maternal blood source, while HbA2 has a similar oxygen-binding capacity as HbA1 Di Cera et al., 1989; Inagaki et al., 2000. On-going clinical trials re-express HbF to extremely high levels not commonly seen even in individuals with Hereditary Persistence of Fetal Hemoglobin Frangoul et al., 2021. The effect of extreme maternal HbF re-expression during pregnancy is currently unknown.
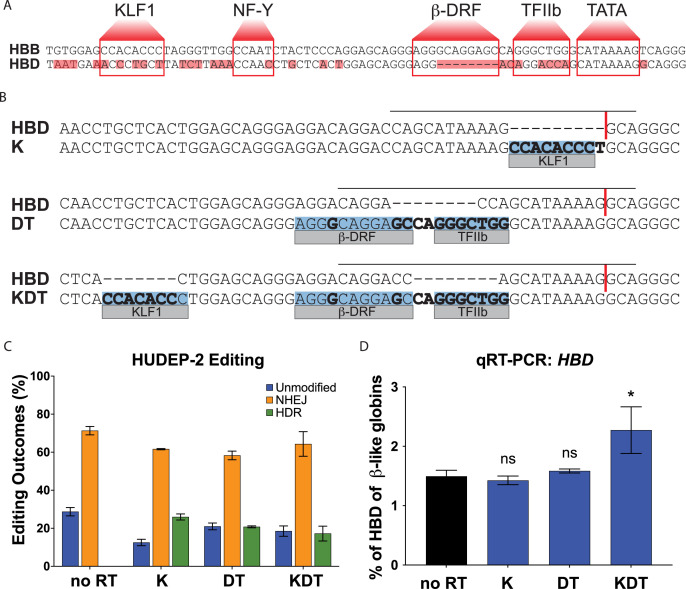
The genes for β−globin (HBB) and δ-globin (HBD) are located in the β-like globin cluster and regulated by the same control region. The β-like globin cluster is located on chromosome 11, and harbors the five β-like genes: HBB (β-globin gene), HBD (δ-globin gene), HBG1 and HBG2 (γ-globin genes), and HBE (ε-globin gene). β-globin and δ-globin both comprise 147 amino acids and differ at only 10 positions Moleirinho et al., 2013. The extreme difference in expression levels between these two globins is not due to protein instability or differences in translation, but instead results from a lower transcription rate Steinberg and Rodgers, 2015. The globin genes are arranged in order of their expression during development and regulated by contact to a distal enhancer called the Locus Control Region that contains five active DNase Hypersensitivity Sites Li et al., 2002. A comparative genomics study has shown that, compared to the HBB promoter, the HBD promoter has mutations in multiple transcriptional elements including a KLF1, NF-Y, β-DRF, and TFIIB binding site (Figure 1A) Zaldívar-López et al., 2017.
Figure 1. Targeting and design of the endogenous HBD promoter.
(A) Alignment of the HBB and HBD promoter sequences. Transcription factor binding sequences for KLF1, NF-Y, β-DRF, TFIIb, and TATA are shown in boxes and base pair mismatches between HBB and HBD are highlighted in red. (B) The repair template designs for insertions of KLF1 (K), β-DRF and TFIIb (DT), and KLF1, β-DRF, and TFIIb (KDT) directly compared to the HBD promoter. The inserted transcription factor binding sequences are highlighted in blue. Any base pair changes are in bold. The gRNA is indicated by a black horizontal line and the cut site is indicated by a red vertical line. (C) HUDEP-2 editing efficiencies showing percentages of unmodified, NHEJ, or HDR alleles. Conditions tested were Cas9 and sgRNA RNP with no repair template (no RT), K, DT, and KDT repair templates. This experiment was performed three times and the data is presented as mean ± SD of three biological replicates. (D) qRT-PCR of HBD after pooled editing of HUDEP-2 cells with no RT, K, DT, and KDT and 5 days of differentiation. Data is plotted as % of all β-like globins (HBB, HBG1/2, HBD). The three biological replicates from the editing experiment in (C) were each differentiated and the data is presented as mean ± SD of three biological replicates. p Value indicates paired, two-tailed student t test (ns, non-significant; *, p≤0.05; **, p≤0.01).
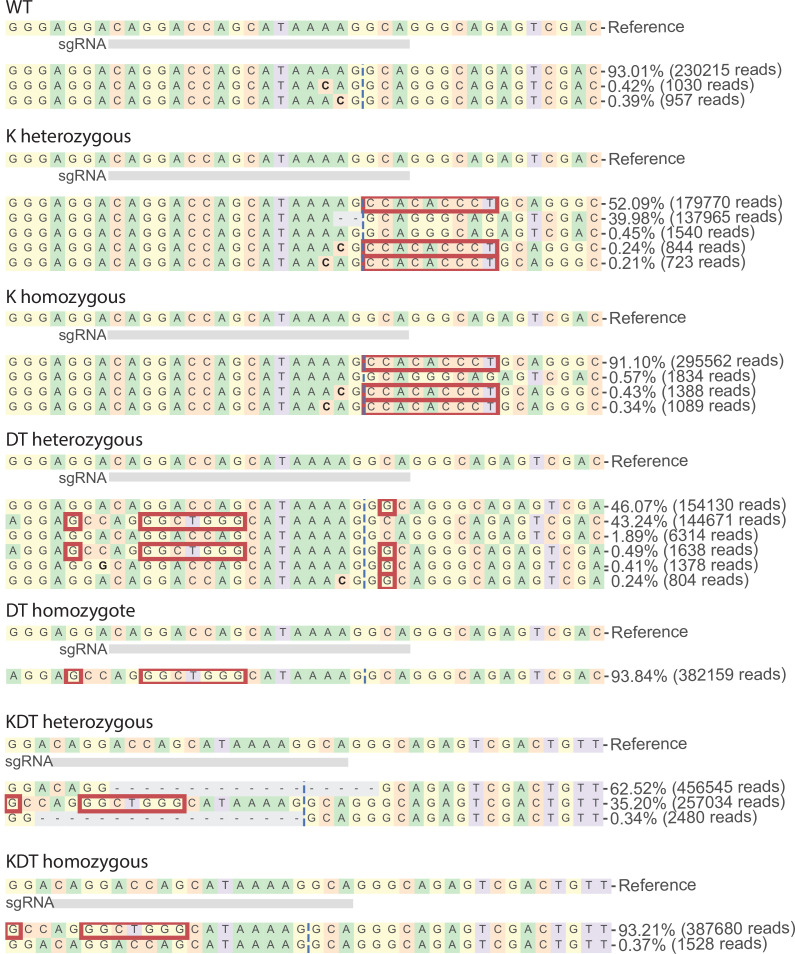
Figure 1—figure supplement 1. Genotypes of HUDEP-2 clones with heterozygous or homozygous knock-ins of KLF1, β-DRF, and TFIIb sequences.
Previous studies using transgenic approaches have shown that inclusion of a KLF1 motif in the HBD promoter can drive exogenous expression of δ-globin Porcu et al., 2021; Donze et al., 1996; Ristaldi et al., 1999. However, these studies do not reflect the complex chromosomal context and extensive epigenetic regulation at the β-like globin cluster. Due to the large size of the β-like globin locus, transgenic studies have mostly included only a subset of the genes of the β-like globin locus and a minimal region of the LCR. They therefore do not necessarily predict the biological outcomes of perturbations at the native β-globin locus Woodard et al., 2022.
The expression of globin genes is a tightly regulated developmental process. There are currently no drugs or therapeutic approaches to increase HbA2 for the β-hemoglobinopathies. Using CRISPR-Cas9 genome editing, we used homology directed repair at the endogenous HBD promoter to engineer the transcriptional elements present in HBB. We find that insertion of single transcriptional elements to the endogenous promoter is insufficient for δ-globin upregulation. However, insertion of KLF1, β-DRF, and TFIIB motifs drive high expression of δ-globin from the endogenous locus in clonal populations of HUDEP-2 cells and primary erythroblasts. This leads to reconstitution of high levels of HbA2, over 10-fold increase compared to WT unedited cells. Our work adds mechanistic insight to the globin gene regulation at the β-like globin cluster and suggests a potential therapeutic avenue to upregulate HbA2 for the β-hemoglobinopathies.
Results
Targeting the endogenous HBD promoter to introduce functional HBB promoter elements
We aligned the promoter sequences of HBB and HBD to identify transcriptional elements missing in the HBD promoter (Figure 1a). This highlighted multiple mutations and deletions in the KLF1, NF-Y, β-DRF, and TFIIB binding motifs. To re-engineer the endogenous HBD promoter, we employed CRISPR-Cas9 induced homology directed repair (HDR) gene editing Jinek et al., 2012; Yeh et al., 2019.
We designed and tested three sgRNAs targeting the HBD promoter (Supplementary file 1) and three HDR templates that would incorporate base pairs needed to complete the transcriptional element motifs (Figure 1b). The HDR templates were designed as single stranded oligo donor nucleotides (ssODN) to either insert a KLF1 (K) sequence, a β-DRF and TFIIB (DT) sequence, or all three elements (KDT). A previous transgenic study showed that the NF-Y site has a lesser impact on HBB transcription in comparison to KLF1 Tang et al., 1997. Therefore, in order to minimize the number of transcription element iterations for testing, we omitted NF-Y from our designs. For the K repair template, the KLF1 sequence was inserted adjacent to the cut site, after the TATA box sequence, in order to disrupt the seed sequence of the sgRNA to reduce subsequent cutting post HDR repair. For the DT repair template, β-DRF and TFIIB motifs were designed into a single template as they are separated by only 2 base pairs. For the KDT repair template, we maintained the ordering between motifs KLF1, β-DRF and TFIIB to mimic the HBB promoter and limited the number of mutated base pairs to increase the likelihood of successful HDR editing. For both the K and KDT repair template, the KLF1 motifs inserted are not designed in the homologous position to the KLF1 site in the HBB promoter. The homologous site is considerably upstream of the sgRNA cut site and therefore more difficult to integrate given the relatively short conversion tracts of HDR in human cells.
We performed editing in HUDEP-2 cells, an immortalized cell line capable of differentiating into hemoglobin-producing erythroid cells Kurita et al., 2013, using Cas9 ribonucleoprotein (RNP) and an ssODN. After optimizing conditions and testing multiple sgRNAs (Supplementary file 1; data not shown), we found that the sgRNA g1 had the highest editing efficiency, and proceeded to use sgRNA g1 for all further experiments. Editing resulted in NHEJ rates ranging from 56% to 74% and HDR efficiencies from 13% to 27% as measured by next generation sequencing (NGS; Figure 1c). The edited pools were differentiated to erythroblasts and qRT-PCR measurements were taken to assess the effects on HBD expression (Figure 1d). Despite roughly equal HDR rates between all promoter designs, we observed a statistically significant increase in HBD only for the KDT design with three elements.
Homozygous knock-in of KLF1, TFIIB, and β-DRF leads to robust increase of HBD in HUDEP-2 cells
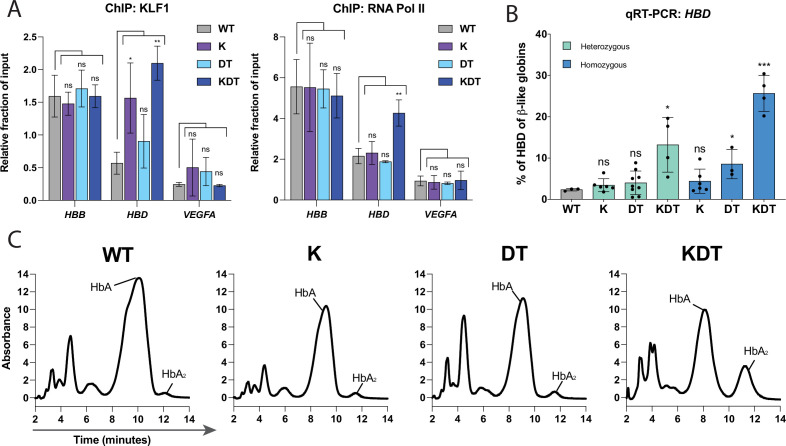
Heterogeneously edited pools of cells, containing a mixture of alleles, can mask large effects at a clonal level. We isolated heterozygous and homozygous HDR clones to more accurately assess the effect of each motif edit on HBD expression. We obtained at least three heterozygotes and homozygotes for each knock-in construct, as verified by amplicon NGS sequencing of the HBD promoter (Figure 1—figure supplement 1). We used ChIP-qPCR to test whether the inserted motifs were functional in recruiting KLF1 and RNA Pol II to the HBD promoter, comparing to the HBB promoter and VEGFA as a positive and negative control, respectively. Due to the unavailability of a TFIIB antibody suitable for ChIP, we performed ChIP for RNA Pol II (Figure 2a). While Pol II is a binding partner of TFIIB in the pre-initiation complex, this ChIP does have the limitation of indirectly immunoprecipitating other factors in the transcriptional pre-initiation complex and might also reflect general promoter activity. The β-DRF motif has been shown to be important for high transcription of HBB, but its bona fide binding factor has not yet been identified Stuve and Myers, 1990. In the homozygous clones K and KDT, which harbor the edited KLF1 sequence, we observed increased binding of KLF1 to the HBD promoter relative to unedited WT HUDEP-2 cells. However, we found RNA Pol II binding at the HBD promoter binding only in the homozygous KDT clone. The homozygous DT clone, which harbors a TFIIB site, did not show significant binding of RNA Pol II. Taken together, our data show that three transcription factor binding sites are necessary to recruit the transcriptional machinery to the HBD promoter Gillinder et al., 2018.
Figure 2. Characterization of HUDEP-2 clones with heterozygous or homozygous knock-ins of KLF1, β-DRF, and TFIIb sequences.
(A) ChIP-qPCR of KLF1 and RNA Pol II performed on WT HUDEP-2 cells and homozygous clones of K, DT, and KDT. Data is shown as relative fraction of input and normalized to SP1. The genes targeted are HBD, HBB, and VEGFA as a negative control. Cells from WT, one K homozygous clone, one DT homozygous clone, and one KDT homozygous clone were grown and harvested separately and on different days for each biological replicate. The data is presented as mean ± SD of three biological replicates. P value indicates paired, two-tailed student t test (ns, non-significant; *, p≤0.05; **, p≤0.01). (B) qRT-PCR of HBD of HUDEP-2 heterozygous and homozygous clones with K, DT, and KDT knock-in and 5 days of differentiation. Each dot represents an individual clonal population, each validated by NGS. Data is plotted as % of β-like globins (HBB, HBG1/2, HBD). Each clone was differentiated and the data is presented as one replicate for each clonal population. p Value indicates paired, two-tailed student t test (ns, non-significant; *, p≤0.05; **, p≤0.01). (C) HPLC of of HUDEP-2 homozygous clones with K, DT, and KDT knock-in and 5 days of differentiation. Hemoglobin A (HbA) and Hemoglobin A2 (HbA2) peaks are annotated. HPLC of one homozygous clone of K, DT, and KDT was performed in triplicate, with a representative dataset of one replicate shown.
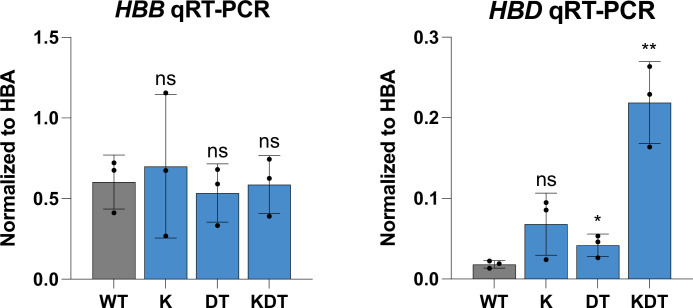
Figure 2—figure supplement 1. qRT-PCR of HUDEP-2 clones with homozygous knock-ins of KLF1, β-DRF, and TFIIb sequences.
We next performed qRT-PCR on all differentiated heterozygous and homozygous clones to look at percentage of HBD produced compared to total β-like globins (Figure 2b). HBB expression was unaffected by the K, DT, and KDT knock-ins (Figure 2—figure supplement 1). Like the pooled editing results, we found that clones with single knock-ins of KLF1 or β-DRF and TFIIB motifs alone did not show increased HBD. Strikingly, we observed a significant increase in HBD for KDT clones harboring all three motifs. Wildtype clones showed HBD expression less than 5% of β-like globins, while heterozygous KDT clones had increased HBD expressions ranging from 5% to 19% and homozygous KDT clones showed increases in HBD to ranges of 20–30% of β-like globins.
Next, hemoglobin protein levels were measured using high pressure liquid chromatography (HPLC) for the differentiated homozygous clones (Figure 2c). Peaks were assigned to hemoglobin complexes based on previous work that performed mass-spectrometry on each globin peak fraction Boontanrart et al., 2020. We found that the transcript-level results are further supported at the protein level. The KLF1 and the β-DRF and TFIIB clones did not show any measurable increase in HbA2, while the KDT homozygous showed a large increase in HbA2.
Endogenous editing of the HBD promoter increases HBD in CD34+ derived erythroblasts
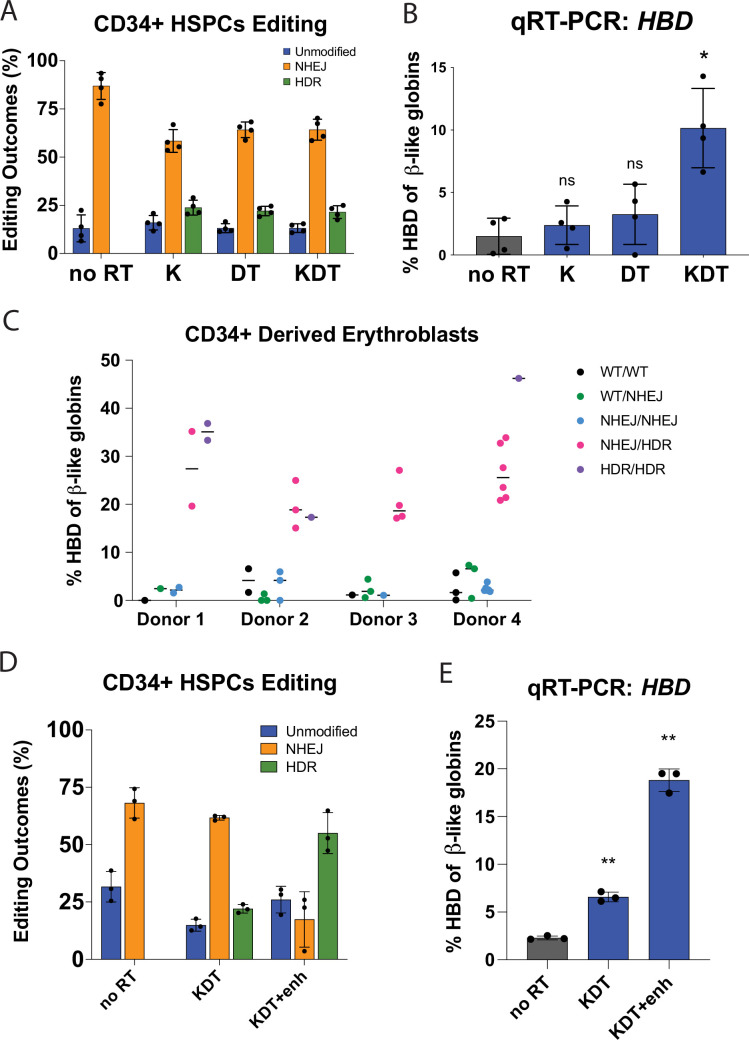
To test the effects of HBD promoter engineering in a more clinically relevant cell type for a potential ex vivo therapy to treat β-hemoglobinopathies, we edited human CD34 +derived erythroblasts. We used CRISPR-Cas9 to perform pooled knock-in at the HBD promoter in mobilized peripheral blood CD34 +human hematopoietic stem and progenitor cells (HSPCs) with the K, DT, and KDT RNP and ssODNs. We found HDR rates ranging from 18% to 25% for all promoter knock-ins (Figure 3a). We differentiated the edited HSPC pools and performed qRT-PCR to measure HBD expression levels. As in HUDEP-2 cells, there was no statistically significant increase in HBD levels for K and DT, and a slight increase in four different donors in the KDT knock-in condition (Figure 3b).
Figure 3. Endogenous editing of the HBD promoter in HSPCs.
(A) Editing efficiencies showing percentages of unmodified, NHEJ, or HDR alleles. Conditions tested were Cas9 and sgRNA RNP with no repair template (no RT), K, DT, and KDT repair templates. The data is presented as independent editing experiments with four different donor samples. (B) qRT-PCR of HBD after pooled editing of HSPCs with no RT, K, DT, and KDT. Cells were expanded in erythroid expansion conditions and differentiated for 5 days. Data is plotted as % of all β-like globins (HBB, HBG1/2, HBD). The data is presented as independent editing experiments with four different donor samples. (C) qRT-PCR of HBD of clonal erythroblast populations after 5 days of differentiation. Genotypes were determined by NGS. Data is plotted as % of β-like globins (HBB, HBG1/2, HBD). The data is presented as independent editing experiments with four different donor samples and each dot denotes an individual clonal population. (D) Editing efficiencies showing percentages of unmodified, NHEJ, or HDR alleles. Conditions tested were Cas9 and sgRNA RNP with no repair template (no RT), KDT repair template, and KDT repair template with AZD-7648 (KDT +enh). The data is presented as one editing experiment with three different donor samples. (E) qRT-PCR of HBD after pooled editing of HSPCs with no RT, KDT, or KDT +enh. Cells were expanded in erythroid expansion conditions and differentiated for 5 days. Data is plotted as % of all β-like globins (HBB, HBG1/2, HBD). The data is presented as one editing experiment with three different donor samples.
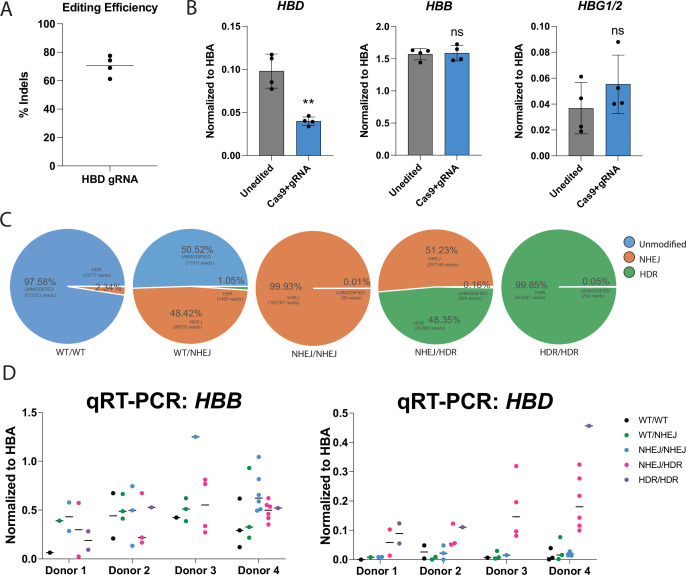
Figure 3—figure supplement 1. Characterization of HBD promoter edited CD34 +HSPCs.
Overall, we observed high editing rates in HSPCs using our CRISPR-Cas9 editing reagents. Cas9 editing can sometimes be accompanied by large deletions Shin et al., 2017, which in the case of editing the HBD promoter might impinge upon the neighboring gene for β-globin. To test if editing at the HBD promoter leads to decrease of other β-like globins, we edited four different HSPC donors with Cas9 and the HBD gRNA alone, mimicking a ‘worst case’ scenario of only NHEJ with no HDR alleles. We observed indel efficiencies ranging from 61% to 78% in the various donors (Figure 3—figure supplement 1a). We differentiated these edited pools into erythroblasts and performed qRT-PCR on the β-like globins HBB, HBD, and HBG1/2 and normalized their expressions to HBA (Figure 3—figure supplement 1b). The HBA gene, which is present in a different locus from the β-like genes, should be unaffected by editing at the β-globin locus. We observed that HBD expression decreased by approximately 50%, while the expression of HBB and HBG1/2 were not significantly changed. While we cannot rule out a small percentage of large deletions among the indel alleles, we do conclude that indel-based targeting of the HBD promoter decreases HBD, as expected, without grossly affecting the expression of the other β-like globins.
To test the effect of KDT editing on a single-cell level, we isolated and grew colonies from HSPCs under erythroid expansion conditions. Each colony was genotyped and their alleles classified as either unmodified, NHEJ, or HDR (Figure 3—figure supplement 1c). These CD34 +derived clonal erythroblasts were differentiated and qRT-PCR was performed to determine HBD expression relative to total β-like globins (Figure 3D). HBB transcript levels remain similar between unedited or NHEJ clones and KDT knock-in clones (Figure 3—figure supplement 1d). We observed that colonies with unedited or all NHEJ alleles had an average expression of lower than 3% HBD of total β-like globins. Heterozygous KDT knock-ins from multiple donors increased HBD expression dramatically, between 15–35% of total β-like globins in heterozygous knock-ins and between 17–46% of total β-like globins in homozygous knock-ins.
Clonal erythroblasts harboring either a heterozygous or homozygous knock-in of KDT expressed significantly increased HBD. However, the edited pools of HSPCs had only a slight increase in HBD, far below the level required to be clinically relevant. We hypothesized that increased HDR efficiency in the pool could lead to higher HBD levels. Small molecule drugs, most notably DNA-PKcs inhibitors that effectively inhibit NHEJ, have shown to shift editing outcomes in CRISPR-Cas9 induced double-stranded break to favor HDR Lee et al., 2022; Peterka et al., 2022. We tested the DNA-PKcs inhibitor AZD-7648 on HSPCs using our editing conditions for KDT knock-in. In three different HSPC donors, we observed an increase from 20% to 24% HDR alleles to 47–65% when we used AZD-7648. We differentiated the edited HSPC pools and performed qRT-PCR to measure HBD expression levels. In these edited erythroblast pools, the KDT-editing pool expressed 6–7% HBD of total β-like globins, while the pools edited with KDT along with HDR enhancer showed increased HBD expression to 17–19%, confirming that increasing the HDR efficiency of KDT knock-in can increase HBD levels within edited pools of HSPCs.
Discussion
Current gene editing efforts to treat the β-hemoglobinopathies include correcting individual HBB mutations DeWitt et al., 2016, a method which would be limited to specific types of patient mutations, or increasing fetal hemoglobin Wienert et al., 2018, which has different oxygen-binding capacities than HbA1. In this study, we describe a path to upregulating HbA2, which shares high similarity to HbA1 and is applicable to all β-hemoglobinopathy disease mutations.
Previous transgenic studies have shown that insertion of KLF1 alone to the HBD promoter sequence is sufficient to drive expression of HBD Porcu et al., 2021; Donze et al., 1996. In our study, we found that endogenous insertion of a KLF1 motif is insufficient to drive HBD expression. One explanation of this discrepancy could be that previous transgenic studies do not reflect the complex chromatin context and regulation at the β-like globin locus. Another explanation could be the importance of the KLF1 motif placement. To ablate re-recognition of the HDR alleles by Cas9, we inserted the KLF1 motif in the K repair template after the TATA box, while the DT and KDT repair templates inserted all motifs upstream of the TATA box. In the HBB promoter, the KLF1 motif is upstream of the TATA box. In a previous study using a HBD promoter luciferase reporter system, they found the highest luciferase activity when the KLF1 motif was upstream of the TATA box, in the homologous position to the HBB promoter Donze et al., 1996. In another study, it was shown that insertion of the KLF1 motif in varying positions resulted in differences in luciferase activity Ristaldi et al., 1999. The placement of transcription factor binding sites can play a crucial role in promoter activity and follow-up studies of our work should further test the spacing and positioning of these various promoter elements, as well as include the NF-Y motif that was not explored in this study.
We have shown that insertion of three motifs, KLF1, β-DRF, and TFIIB, is necessary to recruit RNA Pol II and induce high expression of HBD. In CD34 + derived erythroblasts, homozygous knock-in of KLF1, β-DRF, and TFIIB leads to increases in HBD up to 46% of total β-like globins in clonal populations. To our knowledge, this is the first genomic editing of the HBD promoter that results in increased HbA2. Bulk editing of HBD through insertion of multiple transcriptional elements will rely on high levels of HDR. Increasing HDR outcomes might be achieved in CD34 + cells by a variety of methods such as controlled cell-cycling or modulation of DNA repair factors Howden et al., 2016; Charpentier et al., 2018; Schiroli et al., 2019; Shin et al., 2018. In this study, we found that AZD-7648 increased HDR outcomes in pooled edited HSPCs with concomitant increases in HBD expression. Further work should assess the safety and the effects of the AZD-7648 or other HDR-enhancing in HSPCs if they are to be pursued in a clinical context.
We observed high editing efficiencies when targeting CD34 + HSPCs. When editing targets HBB, NHEJ alleles that co-occur with HDR alleles can cause reductions in overall β-globin levels DeWitt et al., 2016. When targeting HBD, HBB might also be inadvertently affected by large deletions that extend into neighboring β-like globin genes. However, we using qRT-PCR experiment we found that HBB and HBG1/2 mRNA expression were unaffected in our edited populations of HSPCs, suggesting that large deletions were not occurring with enough frequency to grossly affect β-like globin expression. However, some studies have shown that large deletions can occur at low levels, which might be detected by very sensitive tests such as long-range next-generation sequencing or ddPCR.
It is estimated that roughly 30% of beneficial hemoglobin (10 pg per cell) is sufficient to ameliorate β-hemoglobinopathy symptoms Steinberg, 2021. There are currently many gene editing approaches being explored for the β-hemoglobinopathies, mainly focused on increasing fetal hemoglobin or directly correcting the SCD mutation Wienert et al., 2018. A recent study reversed the SCD mutation using CRISPR-Cas9 prime-editing Everette et al., 2023. They showed SCD mutation reversion rates of 17–41% in 4 SCD patient donors and resulted in expression of HbA1 to 10–45% of total hemoglobins. Sickling decreased proportionally to editing efficiencies, with an average of 63% sickled cells for untreated samples and decreasing to 37% in treated samples. Another strategy utilizes CRISPR-Cas9 base-editing to disrupt the LRF repressor binding site within HBG1/2 and observed an upregulation of HbF to over 20% of total hemoglobins in SCD HSPCs Antoniou et al., 2022. When disrupting the LRF site by insertion of a KLF1 site, HbF levels increased to 65–77%. All edited cell populations showed a therapeutically relevant reduction in the number of sickling cells. Another approach utilizes CRISPR-Cas9 to disrupt the enhancer region of BCL11A, a repressor of fetal hemoglobin Frangoul et al., 2021. In an on-going clinical trial, BCL11A enhancer targeting yields editing efficiencies of 80–93% in four SCD patients and HbF upregulation to over 30% of total hemoglobins, with no vaso-occlusive crises 3 months post-transfusion of edited cells. These studies support the curative effect of increasing functional hemoglobin levels on β-hemoglobinopathies. In our study using CRISPR-Cas9 and a DNAPKcs inhibitor to knock the KDT promoter into HBD, we observed increased HbA2 to 17–19% of total hemoglobins in CD34+-derived erythroblasts. Further studies will need to be done to achieve even higher levels of HbA2 expression or test whether this lower expression of HbA2 is sufficient to ameliorate a disease phenotype.
In our experiments, heterozygous and homozygous knock-in of KDT in CD34+ erythroblasts led to 15–46% HBD relative to total β-like globins. Interestingly, in edited CD34+ erythroblasts, we observed that heterozygous and homozygous KDT populations expressed similar increases in HBD. Further studies should investigate whether heterozygous knock-in of KDT in β-hemoglobinopathy cells is sufficient to ameliorate disease phenotypes. For example, one could knock-in KDT to the HBD promoter of SCD patient HSPCs and perform HPLC or microscopy assays to determine the anti-sickling effects of a heterozygous or homozygous knock-in. If heterozygous knock-in of KDT is sufficient, one would see a decrease in sickle hemoglobin produced, or a decreased percentage of sickled red blood cells.
In summary, our presented study provides a novel strategy to increase levels of HbA2 from the endogenous HBD locus that could potentially be applicable as an ex vivo gene therapy. In pre-clinical studies, it will be important to quantitatively investigate the amount of HBD that is optimal for improving the function and health of patient red blood cells and explore the overall potential and safety of increasing HbA2 as a therapeutic option for the β-hemoglobinopathies.
Materials and methods
Cas9 RNP nucleofection
Cas9 RNP was performed as described previously (Lingeman et al., 2017). Briefly, either IVT guides are purified or chemically protected guides were ordered from Synthego and complexed with purified Cas9-NLS protein. The nucleofection was performed using Lonza 4D-Nucleofector and using the P3 Primary Cell 96-well NucleofectorTM Kit (V4SP-3096) following manufacturer’s instructions. The HUDEP-2 nucleofector code used was DD-100 and for primary HSPCs ER-100.
IVT sgRNA
Guide RNAs (Supplementary file 1) were in vitro transcribed as described previously (Lingeman et al., 2017). Briefly, guide sequences were ordered as oligonucleotides and formed into duplexes using a PCR thermocycler. The DNA template was transcribed to RNA using HiScribe T7 High Yield RNA Synthesis Kit (E2040S) following manufacturer protocol. The resulting RNA was purified using RNeasy Mini kit (74104) and Rnase-Free DnaseI Kit (79254).
High-pressure liquid chromatography and mass Spectrometry
HUDEP-2 cells or HSPCs were differentiated and harvested for lysis in hemolysate reagent containing 0.005 M EDTA and 0.07% KCN at 10,000 cells per microliter. The lysis was incubated at room temperature for 10 min and then centrifuged at max speed for 5 min. The supernatant was collected and run on Agilent 1260 Infinity II using a PolyCAT A column from PolyLC, 35x4.6 mm (3 µm;1500 Å) Serial# B19916E. The following Buffer compositions were used: Mobile Phase A: 20 mM Bis-tris, 2 mM NaCN pH 6.8 and Mobile Phase B: 20 mM Bis-tris, 2 mM NaCN, 200 mM NaCl, pH 6.9. The following flow settings were used: Gradient: 0–8’ 2–25% Phase B, 8–18’ 25–100% Phase B, 18–23’ 100–2% Mobile Phase B using a Flow Rate: 1.5 mL/min and measuring detection of 415 nm Diode Array.
HUDEP-2 cell culture and differentiation
All cell culture was performed at 37 °C in a humidified atmosphere containing 5% CO2. HUDEP-2 cells (RRID: CVCL_VI06), obtained from the Riken Institute Kurita et al., 2013, were tested negative for mycoplasm and the cell line was authenticated by STR profiling. HUDEP-2 cells were cultured in a base medium of SFEM (Stemcell Technologies 9650) containing to a final concentration of dexamethasone 1 µM (Sigma D4902-100MG), doxycycline 1 µg/ml (Sigma D9891-1G), human stem cell factor 50 ng/ml (PeproTech 300–07), erythropoietin 50 ng/ml (Peprotech 100–64), and penstrept 1%. Cells were cultured at a density of 2e5 – 1e6 cells/ml. For differentiation, HUDEP-2 cells are centrifuged at 500 g for 5 min, media is removed and replaced with differentiation media. Differentiation media consists of a base media of IMDM + Glutamax (ThermoFisher 31980030) containing to a final concentration human serum 5% (Sigma H4522-100mL), heparin 2 IU/ml (Sigma H3149-25KU), insulin 10 µg/ml (Sigma I2643-25mg), erythropoietin 50 ng/ml (Peprotech 100–64), holo-transferrin 500 µg/ml (Sigma T0665-100mg), mifepristone 1 µM (Sigma M8046-100MG), and doxycyline 1 µg/ml (Sigma D9891-1G). Cells are differentiated for 5 days and then harvested for analysis.
mPB-HSPCs cell culture and differentiation
For editing for human CD34 + cells, CD34 + mobilized peripheral blood HSPCs were thawed and cultured in SFEM containing CC110 supplement (Stemcell Technologies 02697) for 2 days. CD34 + cells were then electroporated and transferred into erythroid expansion media containing SFEM and erythroid expansion supplement (Stemcell Technologies 02692) for 7 days and cultured at a density of 2e5-1e6 cells/ml. The resulting early erythroblasts were transferred to differentiation media containing SFEM with 50 ng/ml erythropoietin, 3% normal human serum, and 1 µM mifepristone. The resulting late erythroblasts were harvested for analysis after 5 days of differentiation. For generation of clonal erythroblasts, CD34 + cells were then electroporated and transferred into erythroid expansion media containing SFEM and erythroid expansion supplement (Stemcell Technologies 02692) for 4 days. The early erythroblasts were then single cell seeded and cultured for 7 days. After 7 days, the cells are transferred into differentiation media containing SFEM with 50 ng/ml erythropoietin, 3% normal human serum, and 1 µM mifepristone. The resulting late erythroblasts were harvested for analysis after 5 days of differentiation.
qRT-PCR
RNA was harvested from cells using Qiagen RNeasy Mini Kit and Rnase-Free DnaseI Kit following manufacturer’s instructions. RNA was reverse transcribed to cDNA using Iscript Reverse Transcription Supermix (Bio-Rad) and qRT-PCR reactions were set up using SsoAdvanced Universal SYBR Green or SsoFast EvaGreen Supermix (Bio-Rad). Reactions were run on the StepOne Plus Real-Time PCR System (Applied Biosystems) or the QuantStudio 6 Flex (Thermo Fisher). Samples were analyzed using a two-step amplification and melt curves were obtained after 40 cycles. The Ct values for genes of interest were normalized to GAPDH, and expressions of genes are represented as 2-[ΔCt] or 2-[ΔΔCt] for fold change over control condition. All primers used for qRT-PCR are listed in Supplementary file 1.
ChIP-qPCR
ChIP was performed as done previously Boontanrart et al., 2020. Briefly, 10 million cells per sample were harvested and cross-linked in 1% Formaldehyde. Cross-linking was quenched with the addition of 1.5 M glycine. Samples were then lysed for 10 min at 4 °C in 50 mM Hepes–KOH, pH 7.5; 140 mM NaCl; 1 mM EDTA; 10% glycerol; 0.5% NP-40 or Igepal CA-630; 0.25% Triton X-100. Cells were then centrifuged at 1500 g for 3 min and the supernatant was discarded. The pellet was resuspended in 10 mM Tris–HCl, pH8.0; 200 mM NaCl; 1 mM EDTA; 0.5 mM EGTA and incubated for 5 min at 4 °C. The cells were then centrifuged at 1500 g for 3 min and the supernatant was discarded. The pellet was resuspended in 10 mM Tris–HCl, pH 8; 100 mM NaCl; 1 mM EDTA; 0.5 mM EGTA; 0.1% Na–Deoxycholate; 0.5% N-lauroylsarcosine and sonicated using the Covaris S220 following manufacturer’s instructions. Protein G beads (ThermoFisher) were complexed with antibody and the antibody-bead complexes were incubated with cell lysates at 4 C overnight with rotation. The antibodies used were mouse anti-RNA Pol II (Diagenode C15100055-100 RRID: AB_2750842) and goat anti-KLF1 (Origene TA305808). The beads were retrieved using a magnetic stand and rinsed with RIPA buffer. Elution buffer containing 50 mM Tris–HCl, pH 8; 10 mM EDTA; 1% SDS was added to the beads for reverse crosslinking at 65 °C overnight with shaking. After reverse crosslinking, the beads were removed. The eluted DNA was treated with RNaseA and Proteinase K and then purified using Qiagen MinElute PCR Purification Kit, following the manufacturer’s instructions. qPCR reactions were set up using SsoAdvanced Universal SYBR Green or SsoFast EvaGreen Supermix (BioRad). Reactions were run on the StepOne Plus Real-Time PCR System (Applied Biosystems) or the QuantStudio 6 Flex (Thermo Fisher). The Ct values were analyzed by the relative fraction of input method.
Next-Generation Sequencing (NGS) amplicon preparation and analysis
To confirm homozygosity/heterozygosity of the HBD clones, samples’ gDNA extracted with QuickExtract DNA Kit was first amplified by PCR. The primers were designed specifically for NGS, spanning a region of <200 bp (including the primers sequences) in which the cutsite is asymmetrically placed (e.g., 30–80 bp from the forward or the reverse primer) to capture the edited region. Subsequently, two stubber sequences are added, one for the forward primer (5‘– CTTTCCCTACACGACGCTCTTCCGATCT –3‘) and one for the reverse (5‘– GGAGTTCAGACGTGTGCTCTTCCGATCT –3‘). After running the first PCR to amplify the genetic region of interest, the overhanging stubber sequences are used to run a second PCR with indexing primers (forward and reverse primers are premixed at 5 M). Samples are pooled and purified with SPRIselect beads, 5 mL (Beckman Coulter, B23317) using a DynaMag–2 Magnet magnetic stand (Thermo Fisher Scientific, 12321D). NGS is performed by the Genome Engineering and Measurement Lab (GEML, ETH Zürich) using a NovaSeq 6000 Sequencing System (Illumina, 20012850) or MiSeq. Sequencing mode used was either 100 or 150 PE (paired end). Editing efficiencies were determined using CRISPResso Pinello et al., 2016.
Acknowledgements
We thank laboratory members for helpful discussions and support; D Fercher and M Zenobi-Wong for help with HPLC; R Kurita and Y Nakamura for their contribution of HUDEP-2 cells; Genome Engineering Measurement Lab and Functional Genomics Center Zurich (ETH Zurich/University of Zurich) for help in running NGS samples. We also acknowledge the Cooperative Centers of Excellence in Hematology NIDDK Grant # DK106829 for CD34 +HSPCs. JEC is supported by the NOMIS Foundation and the Lotte and Adolf Hotz-Sprenger Stiftung. MYB is supported by ETH Foundation’s ETH Pioneer Fellowship and the SNSF BRIDGE Foundation.
Funding Statement
The funders had no role in study design, data collection and interpretation, or the decision to submit the work for publication.
Contributor Information
Mandy Y Boontanrart, Email: mandy.boontanrart@biol.ethz.ch.
Jacob E Corn, Email: jacob.corn@biol.ethz.ch.
Kate Quinlan, UNSW Sydney, Australia.
Didier YR Stainier, Max Planck Institute for Heart and Lung Research, Germany.
Funding Information
This paper was supported by the following grants:
ETH Zürich Foundation ETH Pioneer Fellowship to Mandy Y Boontanrart.
SNSF BRIDGE Proof of Concept to Mandy Y Boontanrart.
Additional information
Competing interests
No competing interests declared.
No competing interests declared.
Author contributions
Conceptualization, Formal analysis, Supervision, Investigation, Visualization, Writing – original draft.
Investigation.
Investigation.
Investigation.
Investigation.
Supervision, Writing – review and editing.
Additional files
Data availability
All data generated are included in the manuscript. All DNA sequences and oligo information are listed in Supplemental Table 1.
References
- Antoniou P, Hardouin G, Martinucci P, Frati G, Felix T, Chalumeau A, Fontana L, Martin J, Masson C, Brusson M, Maule G, Rosello M, Giovannangeli C, Abramowski V, de Villartay JP, Concordet JP, Del Bene F, El Nemer W, Amendola M, Cavazzana M, Cereseto A, Romano O, Miccio A. Base-editing-mediated dissection of a γ-globin cis-regulatory element for the therapeutic reactivation of fetal hemoglobin expression. Nature Communications. 2022;13:6618. doi: 10.1038/s41467-022-34493-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boontanrart MY, Schröder MS, Stehli GM, Banović M, Wyman SK, Lew RJ, Bordi M, Gowen BG, DeWitt MA, Corn JE. ATF4 regulates MYB to increase γ-globin in response to loss of β-globin. Cell Reports. 2020;32:107993. doi: 10.1016/j.celrep.2020.107993. [DOI] [PubMed] [Google Scholar]
- Charpentier M, Khedher AHY, Menoret S, Brion A, Lamribet K, Dardillac E, Boix C, Perrouault L, Tesson L, Geny S, De Cian A, Itier JM, Anegon I, Lopez B, Giovannangeli C, Concordet JP. CtIP fusion to Cas9 enhances transgene integration by homology-dependent repair. Nature Communications. 2018;9:1133. doi: 10.1038/s41467-018-03475-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeWitt MA, Magis W, Bray NL, Wang T, Berman JR, Urbinati F, Heo S-J, Mitros T, Muñoz DP, Boffelli D, Kohn DB, Walters MC, Carroll D, Martin DIK, Corn JE. Selection-free genome editing of the sickle mutation in human adult hematopoietic stem/progenitor cells. Science Translational Medicine. 2016;8:360ra134. doi: 10.1126/scitranslmed.aaf9336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Cera E, Doyle ML, Morgan MS, De Cristofaro R, Landolfi R, Bizzi B, Castagnola M, Gill SJ. Carbon monoxide and oxygen binding to human hemoglobin F0. Biochemistry. 1989;28:2631–2638. doi: 10.1021/bi00432a041. [DOI] [PubMed] [Google Scholar]
- Donze D, Jeancake PH, Townes TM. Activation of Δ-globin gene expression by erythroid Krupple-like factor: A potential approach for gene therapy of sickle cell disease. Blood. 1996;88:4051–4057. doi: 10.1182/blood.V88.10.4051.bloodjournal88104051. [DOI] [PubMed] [Google Scholar]
- Everette KA, Newby GA, Levine RM, Mayberry K, Jang Y, Mayuranathan T, Nimmagadda N, Dempsey E, Li Y, Bhoopalan SV, Liu X, Davis JR, Nelson AT, Chen PJ, Sousa AA, Cheng Y, Tisdale JF, Weiss MJ, Yen JS, Liu DR. Ex vivo prime editing of patient haematopoietic stem cells rescues sickle-cell disease phenotypes after engraftment in mice. Nature Biomedical Engineering. 2023;7:616–628. doi: 10.1038/s41551-023-01026-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frangoul H, Ho TW, Corbacioglu S. CRISPR-Cas9 Gene editing for Sickle cell disease and Β-Thalassemia. The New England Journal of Medicine. 2021;384:e91. doi: 10.1056/NEJMc2103481. [DOI] [PubMed] [Google Scholar]
- Gillinder KR, Magor G, Bell C, Ilsley MD, Huang S, Perkins A. KLF1 acts as a pioneer transcription factor to open Chromatin and facilitate recruitment of GATA1. Blood. 2018;132:501. doi: 10.1182/blood-2018-99-119608. [DOI] [Google Scholar]
- Heller P, Yakulis V. The distribution of hemoglobin A1. Annals of the New York Academy of Sciences. 1969;165:54–59. doi: 10.1111/j.1749-6632.1969.tb27776.x. [DOI] [PubMed] [Google Scholar]
- Howden SE, McColl B, Glaser A, Vadolas J, Petrou S, Little MH, Elefanty AG, Stanley EG. A Cas9 variant for efficient generation of indel-free knockin or gene-corrected human pluripotent stem cells. Stem Cell Reports. 2016;7:508–517. doi: 10.1016/j.stemcr.2016.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inagaki K, Inagaki J, Dumoulin A, Padovan JC, Chait BT, Popowicz A, Manning LR, Manning JM. Expression and properties of recombinant HbA2 (alpha2delta2) and hybrids containing delta-beta sequences. Journal of Protein Chemistry. 2000;19:649–662. doi: 10.1023/a:1007196118200. [DOI] [PubMed] [Google Scholar]
- Jinek M, Chylinski K, Fonfara I, Hauer M, Doudna JA, Charpentier E. A programmable dual-RNA – guided DNA endonuclease S figs. Science. 2012;337:816–822. doi: 10.1126/science.1225829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurita R, Suda N, Sudo K, Miharada K, Hiroyama T, Miyoshi H, Tani K, Nakamura Y. Establishment of immortalized human erythroid progenitor cell lines able to produce enucleated red blood cells. PLOS ONE. 2013;8:e59890. doi: 10.1371/journal.pone.0059890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee ABC, Tan MH, Chai CLL. Small-molecule enhancers of CRISPR-induced homology-directed repair in gene therapy: A medicinal chemist’s perspective. Drug Discovery Today. 2022;27:2510–2525. doi: 10.1016/j.drudis.2022.06.006. [DOI] [PubMed] [Google Scholar]
- Li Q, Peterson KR, Fang X, Stamatoyannopoulos G. Locus control regions. Blood. 2002;100:3077–3086. doi: 10.1182/blood-2002-04-1104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lingeman E, Jeans C, Corn JE. Production of purified Casrnps for efficacious genome editing. Current Protocols in Molecular Biology. 2017;120:31. doi: 10.1002/cpmb.43. [DOI] [PubMed] [Google Scholar]
- Locatelli F, Kabbara N, Ruggeri A, Ghavamzadeh A, Roberts I, Li CK, Bernaudin F, Vermylen C, Dalle JH, Stein J, Wynn R, Cordonnier C, Pinto F, Angelucci E, Socié G, Gluckman E, Walters MC, Rocha V, Eurocord and European Blood and Marrow Transplantation (EBMT) group Outcome of patients with hemoglobinopathies given either cord blood or bone marrow transplantation from an HLA-identical sibling. Blood. 2013;122:1072–1078. doi: 10.1182/blood-2013-03-489112. [DOI] [PubMed] [Google Scholar]
- Moleirinho A, Seixas S, Lopes AM, Bento C, Prata MJ, Amorim A. Evolutionary constraints in the β-globin cluster: The signature of purifying selection at the δ-globin (HBD) locus and its role in developmental gene regulation. Genome Biology and Evolution. 2013;5:559–571. doi: 10.1093/gbe/evt029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagel RL, Bookchin RM, Johnson J, Labie D, Wajcman H, Isaac-Sodeye WA, Honig GR, Schilirò G, Crookston JH, Matsutomo K. Structural bases of the inhibitory effects of hemoglobin F and hemoglobin A2 on the polymerization of hemoglobin S. PNAS. 1979;76:670–672. doi: 10.1073/pnas.76.2.670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterka M, Akrap N, Li S, Wimberger S, Hsieh P-P, Degtev D, Bestas B, Barr J, van de Plassche S, Mendoza-Garcia P, Šviković S, Sienski G, Firth M, Maresca M. Harnessing DSB repair to promote efficient homology-dependent and -independent prime editing. Nature Communications. 2022;13:1240. doi: 10.1038/s41467-022-28771-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinello L, Canver MC, Hoban MD, Orkin SH, Kohn DB, Bauer DE, Yuan GC. Analyzing CRISPR genome-editing experiments with CRISPResso. Nature Biotechnology. 2016;34:695–697. doi: 10.1038/nbt.3583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poillon WN, Kim BC, Rodgers GP, Noguchi CT, Schechter AN. Sparing effect of hemoglobin F and hemoglobin A2 on the polymerization of hemoglobin S at physiologic ligand saturations. PNAS. 1993;90:5039–5043. doi: 10.1073/pnas.90.11.5039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Porcu S, Simbula M, Marongiu MF, Perra A, Poddie D, Perseu L, Kowalik MA, Littera R, Barella S, Caria CA, Demartis FR, Ristaldi MS. Delta-globin gene expression improves sickle cell disease in a humanised mouse model. British Journal of Haematology. 2021;193:1228–1237. doi: 10.1111/bjh.17561. [DOI] [PubMed] [Google Scholar]
- Ristaldi MS, Casula S, Porcu S, Marongiu MF, Pirastu M, Cao A. Activation of the delta-globin gene by the beta-globin gene CACCC motif. Blood Cells, Molecules & Diseases. 1999;25:193–209. doi: 10.1006/bcmd.1999.0245. [DOI] [PubMed] [Google Scholar]
- Schiroli G, Conti A, Ferrari S, Della Volpe L, Jacob A, Albano L, Beretta S, Calabria A, Vavassori V, Gasparini P, Salataj E, Ndiaye-Lobry D, Brombin C, Chaumeil J, Montini E, Merelli I, Genovese P, Naldini L, Di Micco R. Precise gene editing preserves hematopoietic stem cell function following transient p53-mediated DNA damage response. Cell Stem Cell. 2019;24:551–565. doi: 10.1016/j.stem.2019.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shin HY, Wang C, Lee HK, Yoo KH, Zeng X, Kuhns T, Yang CM, Mohr T, Liu C, Hennighausen L. CRISPR/Cas9 targeting events cause complex deletions and insertions at 17 sites in the mouse genome. Nature Communications. 2017;8:15464. doi: 10.1038/ncomms15464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shin J, Wyman SK, Dewitt MA, Bray NL, Vu J, Corn JE. Controlled cycling and quiescence enables homology directed repair in engraftment-enriched adult hematopoietic stem and progenitor cells. bioRxiv. 2018 doi: 10.1101/301176. [DOI] [PMC free article] [PubMed]
- Steinberg MH, Rodgers GP. HbA2: biology, clinical relevance and a possible target for ameliorating sickle cell disease. British Journal of Haematology. 2015;170:781–787. doi: 10.1111/bjh.13570. [DOI] [PubMed] [Google Scholar]
- Steinberg MH. HbA2 induction: the merit of pancellularity in sickle cell disease. British Journal of Haematology. 2021;193:1032–1033. doi: 10.1111/bjh.17562. [DOI] [PubMed] [Google Scholar]
- Stuve LL, Myers RM. A directly repeated sequence in the beta-globin promoter regulates transcription in murine erythroleukemia cells. Molecular and Cellular Biology. 1990;10:972–981. doi: 10.1128/mcb.10.3.972-981.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang DC, Ebb D, Hardison RC, Rodgers GP. Restoration of the CCAAT box or insertion of the CACCC motif activate Δ-Globin gene expression. Blood. 1997;90:421–427. doi: 10.1182/blood.V90.1.421. [DOI] [PubMed] [Google Scholar]
- Waterman MR, Cottam GL, Shibata K. Inhibitory effect of deoxyhemoglobin A2 on the rate of deoxyhemoglobin S polymerization. Journal of Molecular Biology. 1979;129:337–341. doi: 10.1016/0022-2836(79)90287-0. [DOI] [PubMed] [Google Scholar]
- Wienert B, Martyn GE, Funnell APW, Quinlan KGR, Crossley M. wake-up sleepy gene: reactivating fetal globin for β-hemoglobinopathies. Trends in Genetics. 2018;34:927–940. doi: 10.1016/j.tig.2018.09.004. [DOI] [PubMed] [Google Scholar]
- Woodard KJ, Doerfler PA, Mayberry KD, Sharma A, Levine R, Yen J, Valentine V, Palmer LE, Valentine M, Weiss MJ. Limitations of mouse models for sickle cell disease conferred by their human globin transgene configurations. Disease Models & Mechanisms. 2022;15:dmm049463. doi: 10.1242/dmm.049463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeh CD, Richardson CD, Corn JE. Advances in genome editing through control of DNA repair pathways. Nature Cell Biology. 2019;21:1468–1478. doi: 10.1038/s41556-019-0425-z. [DOI] [PubMed] [Google Scholar]
- Zaldívar-López S, Rowell JL, Fiala EM, Zapata I, Couto CG, Alvarez CE. Comparative genomics of canine hemoglobin genes reveals primacy of beta subunit delta in adult carnivores. BMC Genomics. 2017;18:141. doi: 10.1186/s12864-017-3513-0. [DOI] [PMC free article] [PubMed] [Google Scholar]