Abstract
Timely, high-quality mortality data have allowed for assessments of the impact of the novel coronavirus disease 2019 (COVID-19) on life expectancies in upper-middle- and high-income countries. Extant data, though imperfect, suggest that the bulk of the pandemic-induced mortality might have occurred elsewhere. This article reports on changes in life expectancies around the world as far as they can be estimated from the evidence available at the end of 2021. The global life expectancy appears to have declined by 0.92 years between 2019 and 2020 and by another 0.72 years between 2020 and 2021, but the decline seems to have ended during the last quarter of 2021. Uncertainty about its exact size aside, this represents the first decline in global life expectancy since 1950, the first year for which a global estimate is available from the United Nations. Annual declines in life expectancy (from a 12-month period to the next) appear to have exceeded two years at some point before the end of 2021 in at least 50 countries. Since 1950, annual declines of that magnitude had only been observed on rare occasions, such as Cambodia in the 1970s, Rwanda in the 1990s, and possibly some sub-Saharan African nations at the peak of the acquired immunodeficiency syndrome (AIDS) pandemic.
Introduction
Period life expectancy at birth (life expectancy thereafter) is the most frequently used indicator of mortality conditions. More broadly, life expectancy is commonly taken as a marker of human progress, for instance in aggregate indices such as the Human Development Index (United Nations Development Programme 2020). The United Nations (UN) regularly updates and makes available life expectancy estimates for every country, various country aggregates, and the world for every year since 1950 (Gerland, Raftery, Ševčíková et al. 2014), providing a 70-year benchmarkˇ for assessing the direction and magnitude of mortality changes.
Analyses of timely, high-quality vital statistics from about 40 upper-middle- and high-income nations have already demonstrated the impact of COVID-19 mortality on life expectancy in 2020 (Aburto et al. 2021; Islam et al. 2021). Due to the relative efficiency of their mortality reporting, these countries (mostly European, plus the United States and a few countries in East Asia and Oceania) do account for a substantial share of the global deaths attributed to COVID-19 to date. In other countries, however, deaths due to COVID-19 may be more frequently misdiagnosed and underreported, and pandemic-mitigation policies might have induced greater changes in deaths from other causes. Numbers of “excess deaths”—the difference between the actual number of deaths and the number of deaths expected to have occurred in the absence of the pandemic (based on prepandemic trends)—would provide a fuller account of the mortality impact of the pandemic (Helleringer and Lanza Queiroz 2021). While imperfect, extant estimates suggest that the number of excess deaths might be two to four times the number of deaths officially attributed to COVID-19 and that the bulk of these excess deaths likely occurred outside of Europe and the other high-income nations in which the mortality impact of the pandemic has been extensively documented (Adam 2022; The Economist 2022).
This paper presents an attempt to redress this geographical imbalance betweentheseverityofthepandemicandthedepthofthecurrentanalytical record, by providing estimates of changes in life expectancies up to the end of 2021 for the world and for as many countries as even partial data allow. First, to provide a sense of magnitude for the results, past instances of life expectancy declines are provided from a review of the UN time series from 1950 to 2019. Second, for each country and each quarter of 2020 and 2021, numbers of excess deaths are estimated. Used in combination with previously (prepandemic) estimated UN life tables, these numbers yield global and national life expectancies for eight 12-month periods ending each quarter from March 31, 2020, to December 31, 2021. Changes between two consecutive 12-month periods and cumulative 2019–2021 changes are then compared to the UN annual series. The last sections discuss the current data limitations, the estimates’ uncertainty and what might still be reasonably concluded from this still preliminary assessment of global mortality trends between 2019 and 2021.
Background
Global life expectancy and mortality crises
Global and national trends in life expectancies are assessed first to provide context for the pandemic-induced changes. As estimated by the UN, the post-1950 trend in global life expectancy is quite remarkable. The UN estimates that the annual value of the global life expectancy has increased without interruption from 45.7 years in 1950 to 72.6 years in 2019 (United Nations 2019), a 0.39-year gain per year on average. The largest annual gains, more than 0.7 year from 1964 to 1968, reflect the success of global public health campaigns, in particular childhood vaccination programs (Cutler, Deaton, and Lleras-Muney 2006).
The distribution of these mortality declines over the lifespan contributed to reduce the global life table entropy (Keyfitz 1977; Goldman and Lord 1986; Olshansky, Carnes, and Désesquelles 2001). As a result, proportionally larger mortality declines would have been required to maintain the pace of annual gains in life expectancy. Instead, annual gains in global life expectancy have gradually declined below their 1950–2019 average of 0.39 years, dipping below 0.3 years from 2015 to 2018 and below 0.2 years in 2019. Annual gains had previously dropped under 0.2 years between 1990 to 1995 due to AIDS pandemic, with 0.16 years in 1992 being the smallest annual gain of the entire 1950–2019 period.
At the national level, countries did not all enjoy an uninterrupted upward trend in life expectancy. Instances of life expectancy declines, from one calendar year to the next, remain rare in the UN time series and relatively modest though. The main exceptions to this generalization are found for Cambodia (up to −4.63 years per year) and Rwanda (up to −5.02 years per year)—two countries that experienced massive increases in violent mortality, in the late 1970s and early 1990s, respectively—and a few sub-Saharan countries during by the AIDS pandemic. According to the UN estimates, the impact of AIDS mortality on life expectancy was most severe in Eswatini in the late 1990s (up to −2.10 years per year).
The UN annual estimates of life expectancy are derived from five-year period estimates though. This involves a smoothing function that reduces annual variations. The decline in life expectancy in Rwanda between 1993 and 1994, the year of the genocide (Verwimp 2004), is likely much more than five years. National estimates similarly smooth out the impact of mortality crises at the subnational level, such as in Darfur (Hagan and Palloni 2006). Sadly, instances of massive short-term mortality increases driven by violence or famine have not been that uncommon since 1950 (Obermeyer et al. 2008). Contrary to estimates of the number of deaths, however, estimates of life expectancy during these mortality crises remain relatively few. A full reconstruction of demographic changes in China between 1958 and 1961 does suggest that life expectancy may have declined by 12 years between fiscal years 1957–1958 and 1958–1959 (equivalent to a five-level change in Coale–Demeny model life tables, Ashton et al. 1984, 639). Another reconstruction of demographic changes in Cambodia during the “Khmer Rouge” regime (1975–1978) suggests that life expectancy may have fallen to 8.1 years for males and 16.7 years for females (Heuveline 2015, 211), implying a decline from pre-1975 levels that numbers in decades rather than in years. The conclusion from a review of the UN time series that annual declines in life expectancy since 1950 rarely exceeded two years must thus be qualified as not applying to famine- or violence-driven mortality shocks.
Pandemic-induced changes in life expectancy
Besides famines or violent conflicts, pandemics also represent mortality shocks likely to induce increases in the sex- and age-specific rates of all-cause mortality from which life expectancy is derived. The process of verifying and consolidating deaths data to produce these rates is typically a lengthy one. The US Centers for Disease Control and Prevention (CDC), for instance, first produced a provisional estimate of the US life expectancy for 2020 in July 2021 suggesting a decline of 1.5 years, compared to 2019 (Arias et al. 2021). The estimated decline was increased to 1.8 years with the final estimate released in December 2021 (Murphy et al. 2021). Given the urgency to document recent mortality conditions during the pandemic, provisional mortality statistics have been released notably faster than under usual circumstances. Most notably, the Human Mortality Database has released a Short-term Mortality Fluctuations (STMF) data series (Jdanov et al. 2021) that tracks weekly mortality data with a few-week lag for countries with reliable and timely mortality statistics. Analyses of these data have provided estimates of life expectancy change in 2020 for nearly 40 countries, mostly European, with a few additional upper-middle- and high-income nations in North America, East Asia and Oceania (Aburto et al. 2021; Islam et al. 2021). From these analyses, the only country that appears to have experienced a two-year or larger decline in life expectancy between 2019 and 2020 is Russia (Islam et al. 2021 report the difference between the actual and expected 2020 values, 2.33 for males and 2.14 for females, which should be slightly larger than the 2019 to 2020 decline given the expected, counterfactual, upward trend).
For all but a handful of countries, numbers of COVID-19 deaths that are updated at least daily on online dashboards such as Johns Hopkins University’s (JHU) have provided a timelier and, foremost, more global resource to assess the mortality impact of the pandemic (Dong, Du and Gardner 2020). Analyses of these data strongly suggest that the largest declines in life expectancy were not occurring in Europe or the United States, but in countries of Central and South America (Heuveline and Tzen 2021). The life expectancy estimates derived from these data proved unreliable, however, as their validity depends on reported counts of deaths due to COVID-19 that may be inaccurate and an assumption of unchanged rates of mortality from causes other than COVID-19 that may not hold. Cause-specific mortality data reveal increases in US death rates from causes other than COVID-19 during the pandemic for instance (Ahmad and Anderson 2021). Conversely, analyses of STMF data showed that, in a few countries, life expectancy increased more in 2020 than in recent years before, suggesting that public health interventions intended to mitigate the impact on the virus also reduced mortality from other causes. With respect to deaths attributed to COVID-19, protocols that require including all suspected, but unconfirmed, COVID-19 deaths might have produced overcounts in some countries (Beaney et al. 2020). The main concern, however, remains the possibly vast extent to which COVID-19 deaths might have been misdiagnosed or unreported in many parts of the world. Estimates of excess deaths in Central and South America suggest drastically larger reductions in life expectancy than when based on reported COVID-19 deaths, reaching 10.91 years in Peru, 7.91 years in Ecuador, 5.54 years in Mexico, 2.42 years in Brazil, and 2.26 years in Guatemala (Lima et al. 2021).
Data and methods
At this writing, global and national estimates of deaths attributed to COVID-19 were available up to the end of 2021. In this paper, however, I aim to derive global and national estimates of changes in life expectancy between 2019 and 2021 based on excess deaths rather than deaths attributed to COVID-19 alone.
Excess deaths data
The most comprehensive source of excess-death estimates to date is the World Mortality Dataset (WMD), which at the end of 2021 covered over 100 countries (Karlinsky and Kobak 2021). In the combined population of these countries, the WMD suggests there was 60 percent more excess than COVID-19 deaths since the beginning of the pandemic. However, the scope and quality of the mortality data available to estimate excess mortality vary across countries. An analysis by Our World In Data (OWID) suggests that in nearly 60 of these countries, the data did not allow for reliable estimation of the expected number of deaths over time from which estimates of excess deaths are derived (OWID 2021). Reasons include too few years of prepandemic data to estimate the temporal trend, insufficient breakdown over time (within year) to adjust for seasonality, or insufficient age breakdown to adjust for demographic changes.
Even the full WMD still does not cover large swaths of Africa and Asia. The few sub-Saharan African countries that are included (Mauritius, Mayotte, Reunion, Seychelles, and South Africa), for instance, are clearly not representative of the entire region. But the most conspicuous coverage gap and current unknown quantity may be India. A recent study derived from three independent data sources estimated a confidence interval of 2.75 to 12.25 for the ratio of excess to COVID-19 deaths (Anand, Sandefur, and Subramanian 2021). Culling mortality data from several sources, however, the most sophisticated demographic analysis to date suggested the number of excess deaths was likely seven times the official number of COVID-19 deaths at the time (Guilmoto 2022). This ratio is consistent with the largest study of the Civil Registration System that placed the number of excess deaths close to three million by the end of 2021, more than six times the official tally at the time (Jha et al. 2022).
A machine learning algorithm designed to provide estimates of excess deaths for all countries and the whole world suggests that the global number of excess deaths from the start of the pandemic to the end of 2021 is between 2.2 and 4.0 times the reported number of COVID-19 deaths (The Economist 2022). The algorithm (known as “gradient boosting”) is developed by fitting the relationship between excess mortality and a large set of diverse national indicators (including mean elevation, average temperature, and prevalence of human immunodeficiency virus (HIV), tuberculosis (TB) or malaria) on a training sample of about 80 countries. This model provides estimates of excess mortality for many countries where there is no reliable COVID-19 mortality data for such estimation—or only unrepresentative data, typically from small studies conducted in urban centers (e.g., Jakarta, Indonesia: Djaafara et al. 2021; Khartoum, Sudan: Watson et al. 2020; Damascus, Syria: Watson et al. 2021; Lusaka, Zambia: Mwananyanda et al., 2021; Aden, Yemen: Koum Besson et al. 2021). As with any extrapolation strategy, however, the performance of gradient boosting algorithms depends on the degree of similarity between countries included in the training sample and other countries.
An estimate of global excess deaths
The numbers of excess deaths were estimated for each country and each quarter in 2020 and 2021. Different approaches were used depending on the availability and quality of the data in each country. For a first group of 53 WMD countries, data quality was deemed satisfactory per OWID criteria. In these countries, WMD estimates of excess deaths by quarter were used when available for the entire quarter. In the remaining quarters, excess deaths were estimated iteratively based on the relationship between estimates of excess deaths and COVID-19 deaths reported on the JHU dashboard in the past 12 months (JHU 2022). When these excess-death estimates were larger than reported COVID-19 deaths, the ratio of the two was applied to the number of COVID-19 deaths reported on the JHU dashboard for the following quarter. This assumption would fit the situation where excess deaths are mostly due to COVID-19 and the ratio of reported to unreported COVID-19 deaths does not change. When excess-death estimates over the past 12 months were less than reported COVID-19 deaths, or even negative, the average quarterly difference between the two was assumed to remain the same in the next quarter. This assumption would fit the situation where COVID-19 deaths are accurately reported and deaths from other causes are fewer than expected by the same amount each quarter.
The second group of countries includes the remaining WMD countries plus some, like India, for which a national estimate of excess mortality might be available from ancillary sources. For the WMD countries, preliminary quarterly estimates were produced following the same approach as for the first group of countries. The end-of-2021 tallies of excess deaths were then compared to the number derived from the tallies of COVID-19 deaths reported on the JHU dashboard and the percent undercount predicted by The Economist model. In countries for which preliminary estimates already exceeded reported COVID-19 deaths in each quarter, and the predicted undercount suggested an even higher ratio of excess to COVID-19 deaths, the preliminary quarterly estimates were scaled up to match the predicted undercount. In other countries, the under count ratio predicted by the model or provided by ancillary sources was applied to quarterly numbers of COVID-19 deaths reported on the JHU dashboard.
This last approach is the only option to estimate excess deaths in the remaining countries comprising nearly half of the world population. Since the performance of the model remains difficult to assess at this point for countries for which there has been little to no direct data on COVID-19 mortality, an upper limit was placed on the predicted cumulative number of excess deaths. This limit was set by deriving age-standardized rates of excess mortality for the 2020–2021 period for each country within each UN geographic area, and if necessary, scaling down the prediction for a country in this third group so that its rate would not exceed the highest age-standardized rate for countries in the first two groups. The full calculations for each country are provided in Supplementary File (“Excess Deaths”).
Across groups, this estimation yields more than 15 million excess deaths in 2020 and 2021, 2.8 times the global number of COVID-19 deaths reported at the end of 2021 (5.4 million). Figure 1 summarizes the estimated numbers of excess deaths for each group of countries and the global number of reported COVID-19 deaths for each quarter in 2020 and 2021. The figure shows that the exact proportion by which reported COVID-19 deaths underestimate excess deaths worldwide depends largely on the situation in countries where it has only been partially (Group II) or hardly (Group III) documented. As also illustrated in Figure 1, excess mortality trends differ across groups. While 33 percent of excess deaths occurred in Group-I countries in 2020, only 24 percent of 2021 excess deaths occurred in these countries. Global trends cannot be simply extrapolated from the well-documented trends in Group-I countries.
FIGURE 1.
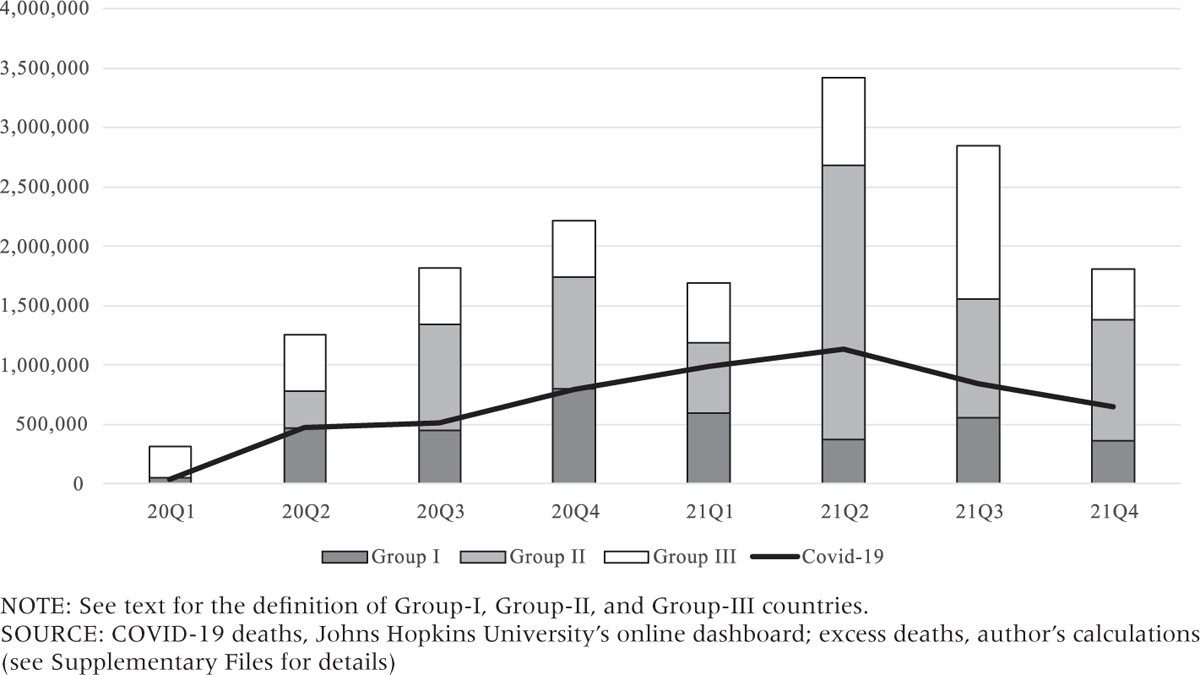
Estimates of excess deaths by country group and reported COVID-19 deaths, 2020–2021, by quarter
Methods: Recalculating period life expectancies
Life expectancies were recalculated for eight 12-month periods, each ending in one of the quarters of 2020 and 2021 (the first period being from April 1, 2019, to April 1, 2020, and the last one being the calendar year 2021). The estimation of global and national life expectancies in each period proceeded in four steps. First, excess deaths were distributed by age and sex. A different sex and age pattern was used in each period, based on the cumulative number of COVID-19 deaths by sex and age group reported by the US CDC at each quarter-end (CDC 2022). The number of excess deaths in each sex and age group was derived from the total number of excess deaths in the world/country during a period, the number of COVID-19 deaths in the same-sex age group and period in the United States and the ratio of sex and age group’s population size in the world/country and in the United States. That last ratio was obtained from the UN projections of national population sizes by sex and age group for mid-2019, -2020, and -2021 (United Nations 2019).
Second, sex- and age-specific mortality rates (nmx) and survival probabilities (npx) for the calendar year 2019 and counterfactual rates and probabilities for each of the eight 12-month periods were derived from the UN 2019 estimates and projections. Period values were obtained by linear (nmx) or exponential (npx) interpolation between the 2015–2020 and 2020–2025 values from the UN. Third, excess mortality rates for each country and the world in each of the eight periods were combined with the counterfactual rates into period life tables by reversing the procedure typically used to “delete” a cause of death from a multiple-decrement life table (Heuveline and Tzen 2021; Preston, Heuveline, and Guillot 2001). Fourth, life expectancies were estimated from the reestimated probabilities and the counterfactual rates and probabilities. Additional details on these four steps are provided in the Appendix (Steps 2 to 5). National life expectancies were only estimated for Group-I and Group-II countries for which the UN estimates life table functions (countries with a population size above a given threshold)—a total of 98 countries. Estimates of excess deaths for Group-III countries were not deemed sufficiently reliable for life expectancy estimation.
Results
The increase in the number of deaths during the pandemic had a substantial impact on the global life expectancy. After 69 years of uninterrupted increase from 1950 to 2019, the global life expectancy is estimated here to have declined by −0.92 years between 2019 and 2020 and by another 0.72 years between 2020 and 2021 (for both sexes, Figure 2). In 2021, the global life expectancy is estimated to have dropped below its 2013 level.
FIGURE 2.
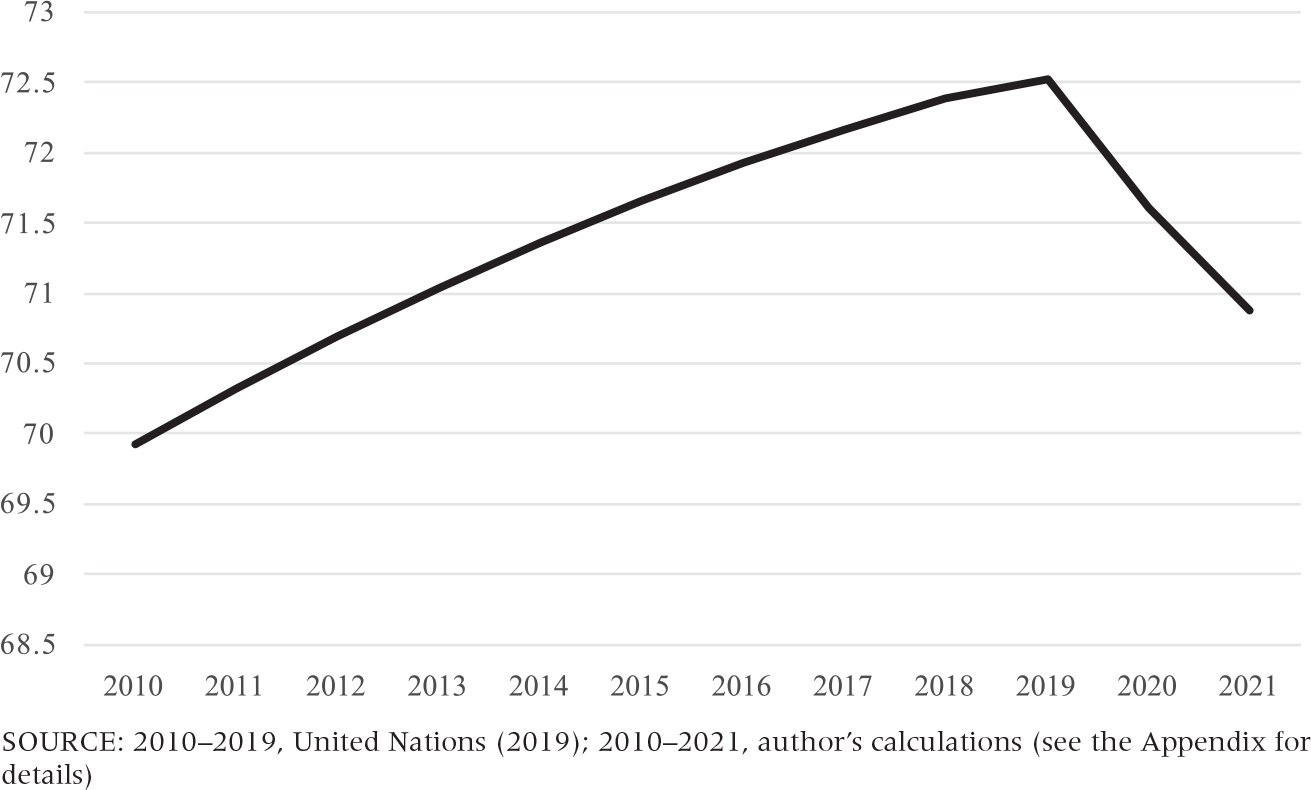
Global life expectancy, 2010–2021 (both sexes, in years)
Comparing life expectancy estimates for each of the eight 12-month periods, however, the decline in global life expectancy appears to have stopped in the last quarter of 2021 (Figure 3). Based on these eight estimates, tracking changes in life expectancy between two consecutive 12-month periods (annual change thereafter) shows that the annual change for the global population is estimated to have peaked at 1.33 years at the end of June 2021 (mid-2020 to mid-2021 vs. mid-2019 to mid-2020).
FIGURE 3.
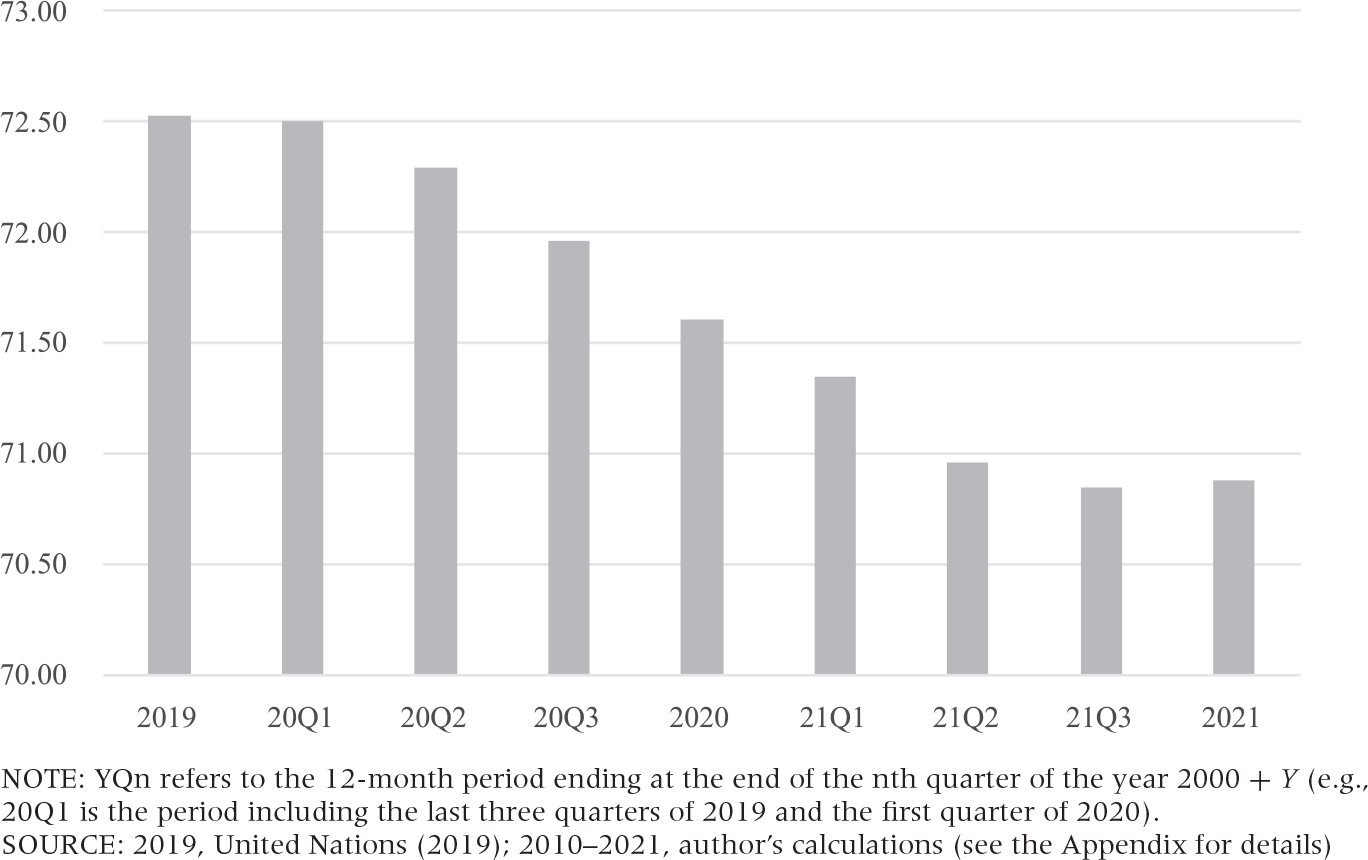
Global life expectancy, by 12-month period ending in each quarter of 2020 and 2021 (both sexes, in years)
At the national level, many countries experienced substantial changes in life expectancy (Figure 4). Between 2019 and 2021, life expectancy is estimated to have declined by more than two years annually (four years overall) in eight countries (Figure 4, Category 3), five in America (Peru, 5.6; Guatemala, 4.8; Paraguay, 4.7; Bolivia, 4.1; and Mexico, 4.0 years) and three in Europe (the Russian Federation, 4.3; Bulgaria, 4.1; and North Macedonia, 4.1 years).
FIGURE 4.
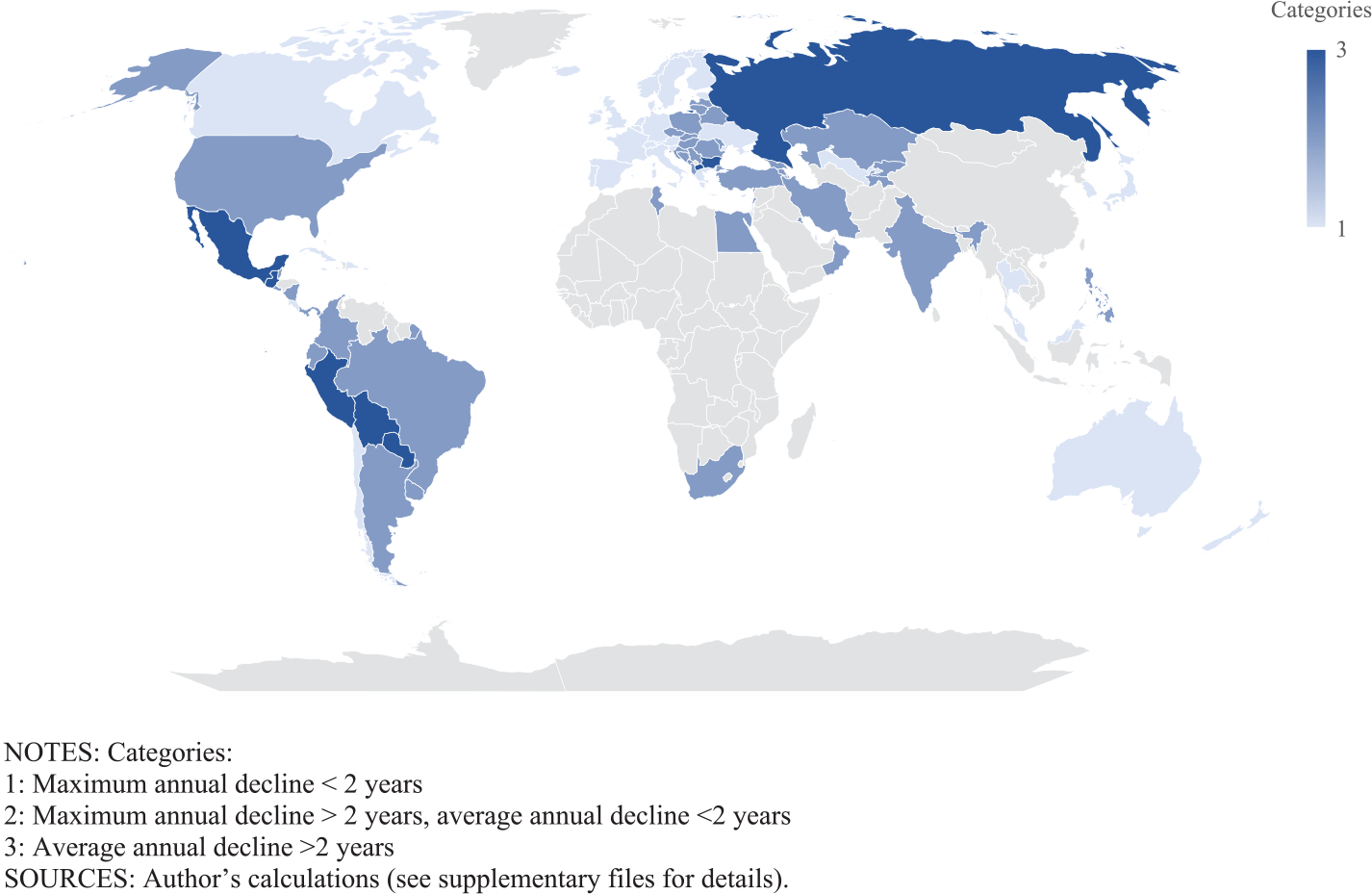
Annual change in life expectancy, 2019–2021 (both sexes, in year)
Tracking annual change at the end of each quarter, however, more than half of the countries for which life expectancies were estimated (53 out of 98) reached an annual change in excess of two years at some point in 2020 or 2021 (Figure 4, Category 2). Annual change even reached seven years in Peru and between four and six years in several other countries in America (Mexico, Nicaragua, Bolivia, Paraguay, Columbia, Ecuador, and French Guiana). In Europe, annual change reached a little over four years in Bosnia and Herzegovina and in North Macedonia and over three years in a few other countries (Montenegro, Bulgaria, Albania, and Poland). Substantial annual changes are also observed throughout Asia, from Southeast Asia (Philippines, 3.0 years) and South Asia (India, 2.6 years) to Central Asia (Kazakhstan, 3.2 years) and Western Asia (Lebanon, 3.4 years), and in the few countries in continental Africa with sufficient data (Tunisia, 3.4 years; South Africa, 3.1 years; and Egypt 2.3 years). Among those with sufficient data, the only countries that did not reach the two-year mark at any point between 2020 and 2021 are countries in Eastern Asia, Australia, New Zealand, and European countries, west of a line running from the Baltic to the Balkans. Together with the United States, which did reach an annual change of just over two years, these are arguably the countries where the impact of the pandemic has been the most extensively studied to date.
Tracking change quarterly also reveals very diverse timing of pandemic impact across countries (see Supplementary File “Life Expectancies”). In some (Nicaragua, Ecuador), annual change peaked in 2020 and life expectancy recovered in 2021. On the contrary, after little change in 2020, the annual change was still increasing in the last quarter of 2021 in the Philippines and Overseas Territories of France (Guyana, Martinique, and Guadeloupe), for instance. The plateau in global life expectancy reached during the last quarter of 2021 (Figure 3) is far from a global trend and results instead from a diminishing impact of the pandemic in some countries and a still increasing impact on some other countries.
Discussion
The results demonstrate that the pandemic had an impact on the global life expectancy that has no precedent since 1950. In more than half of the countries where impacts on national life expectancy could be estimated, they also appear to be of a rare magnitude since 1950. Obviously, there is still substantial uncertainty about the exact size of the declines in life expectancy even in these countries and globally. Estimates of declines in life expectancy were derived here from numbers of excess deaths that in turn must be derived from statistical modeling of what the number of deaths might have been in the absence of the pandemic. Even in countries with the required good-quality data, this modeling involves multiple decisions for which there is no clear rule—regarding the number of past years used to define benchmark mortality conditions, if and how a temporal mortality trend is modeled, and so forth—and which may substantially impact the results (Nepomuceno et al. 2021; Schöley 2021). The main challenge to measuring excess deaths with confidence, however, remains substantial data limitations in many parts of the world.
An additional difficulty for some countries is that only a total number of excess deaths might be derived from the number of deaths attributed to COVID-19 and ancillary data, but the impact of these excess deaths on life expectancy depends on their age and sex distribution. As age-and-sex distributions of excess deaths are only available in a limited number of countries, the results presented here rest on a simplifying assumption that derived the distribution of excess deaths in all countries from a single mortality schedule (US sex- and age-specific mortality rates from COVID-19), albeit different for each period. For countries that have good quality data on excess deaths by age and sex, extant results based on these data should be more reliable than those presented here, the former providing useful benchmarks for assessing the quality of the latter.
In settings where excess deaths consist mostly of reported and unreported COVID-19 deaths, the main issue is expected to be potential differences in sex and age patterns of COVID-19 mortality between countries. Extant reviews suggest that the age patterns are flatter in lower-income countries and at lower life expectancy levels (Demombynes et al. 2021; Guilmoto 2020; Ioannidis, Axfors, and Contopoulos-Ioannidis2021; O’Driscoll et al. 2021). Further evaluations of data quality might be needed to validate that observation, as a higher degree of uncertainty about exact age can also reduce the slope of the mortality schedule (Preston et al 1996). Moreover, even if these observed differences in slope were to be taken at face value, COVID-19 mortality schedules would still be broadly similar (Ohnishi, Namekawa and Fukui 2020). A sensitivity analysis substituting the US sex and age pattern of COVID-19 mortality to the pattern prevailing in Brazil, for instance, did produce an “older” distribution than the actual distribution of excess deaths but only reduced the estimated impact on 2020 life expectancy by 3 percent (Heuveline and Tzen 2021). Finally, higher vaccination rates at older ages have also resulted in flatter age patterns in high-income nations over time and should have reduced the difference in the concentration of COVID-19 mortality at older ages between countries.
A different issue might be expected in settings where the number of excess deaths is substantially affected by changes in the number of deaths from other causes. Because COVID-19 deaths are more heavily distributed toward older ages than deaths from most other causes, one excess death due to COVID-19 has less impact on life expectancy than one excess death from another cause. One study estimated that in 2020, COVID-19 deaths accounted for 83 percent of excess deaths but only 73 percent of the years of life lost in the United States, for instance (Chan, Cheng and Martin 2021). The 2019-to-2020 decline in US life expectancy estimated here (1.63 years, see Supplementary File “Life Expectancies”) is indeed smaller than the CDC’s final estimate (1.8 years; Murphy et al. 2021). Conversely, in countries where a ratio of excess to COVID-19 ratio below one could reflect lower than expected mortality from causes other than COVID-19 during the pandemic, the expectation is that the impact of excess deaths would be over-estimated. The 2019-to-2020 decline in life expectancy estimated here for France (0.70 years, see Supplementary File “Life Expectancies”) is indeed larger than the country’s official estimate (0.5 years for females and 0.6 years for males; Papon and Beaumel 2021).
The sensitivity of the results to differences in age and sex patterns of excess mortality appears relatively modest, and in most countries, uncertainty about the total number of excess deaths is by far the main concern. Neither the uncertainty about the scale of excess mortality nor the uncertainty about its distribution by age and sex appear to be substantial enough to invalidate the finding that the global life expectancy declined in 2020 for the first time in 70 years and continued to decline between 2020 and 2021.With 30 percent of the global excess deaths being estimated in Group-III countries, the pandemic impact on the global life expectancy could be substantially smaller than estimated here but not to the point that life expectancy would have continued to increase. The figure of 15.4 million excess deaths at the end of 2021, on which the global life expectancy estimation rests, is 2.8 times the number of global deaths officially attributed to COVID-19 at that point when The Economist (2022) model provided 2.2 to 4.0 as a 95 percent confidence interval for that ratio. At the national level, the result that many countries have experienced a decline in life expectancy since the beginning of the pandemic should also be a robust finding. The exact number is difficult to assess, due less to the uncertainty of the estimates presented here than to the fact that, as of this writing, pandemic life expectancy could not yet be estimated in roughly half of the countries.
When it can be estimated, interpreting these reductions in life expectancy is not entirely straightforward either. The popularity of life expectancy as a summary indicator of mortality conditions results in part from its intuitive interpretation as an average length of life were mortality conditions remain unchanged. The meaning of a change in life expectancy driven by hopefully temporary changes in mortality is less intuitive (Goldstein and Lee 2020; Heuveline 2021a; Modig, Rau and Ahlbom 2020; see the Appendix for further discussion of a possible interpretation of temporary changes in life expectancy). Several alternative measures have been proposed to express how much changing mortality conditions have impacted longevity during the pandemic (Ellege 2020; Goldstein and Lee 2020; Heuveline 2021a; Pifarré i Arolas, Acosta, López Casasnovas et al. 2021; Verdery, Smith-Greenaway, Margolis, and Daw 2020). But life expectancy remains the most available summary indicator of mortality conditions across the world and over time, providing unique opportunities for geographic and historical comparisons. In this respect, pandemic trends in many countries unambiguously signal a mortality impact at a scale rarely observed since 1950 except during famines and violent conflicts.
Conducting these analyses at the national level is largely a data-driven choice. Several analyses have demonstrated important within-country differences both across geographical units (e.g., Castro et al. 2021; Garciá-Guerrero and Beltrán-Sánchez 2021; Heuveline and Tzen 2021) and between racial/ethnic groups (Andrasfay and Goldman 2021). World maps such as Figure 4 would conceal high impacts on subpopulations in relatively better-off countries.
Conclusion
Changes in life expectancy between 2019 and 2020 in America, Europe, and a few other countries have received copious attention. Results presented here confirm several key takeaways from previous analyses such as the large mortality impact of the pandemic (1) in the United States relative to other high-income nations in Western Europe (Aburto et al. 2021; Heuveline 2021b), (2) in Russia relative to the rest of Europe (Islam et al. 2021), and foremost, (3) in some Central and South American nations (Lima et al. 2021).
Using end-of-2021 reports of deaths attributed to COVID-19 and modeling their relationship to excess deaths, preliminary estimates were also presented for changes in life expectancy in 2021. These results suggest a growing gap between, on the one hand, Western European nations and, on the other hand, the United States, where life expectancy continued to decline, and even more so, Russia, where it is expected to decline more in 2021 than in 2020. In Central and South America, the record is more contrasted with countries where life expectancy is expected to recover some of the large declines of 2020 (e.g., Ecuador, Nicaragua), or to continue to decline but substantially less than in 2020 (e.g., Bolivia, Mexico, Peru), and some where the 2021 declines are expected to exceed the 2020 declines (e.g., Brazil, Columbia, Guatemala, Paraguay).
Changes in life expectancies were also estimated for a total of 98 countries including some that had not received as much attention to date. These results highlight a geographical imbalance between the availability and quality of data on excess mortality and the impact of the pandemic. At an early stage in the pandemic, the quantity of data might have been commensurate with the severity of the pandemic. The first wave of the pandemic was well-documented as it affected high-income countries with good statistical systems, foremost in Western Europe and the United States (Kontis et al. 2020; Vestergaard et al. 2020). As these analyses have shown, this is no longer the case. With the notable exception of the United States, the annual change in life expectancy in these wealthy forerunners has never reached the level observed in over half of the countries with the data required for sufficiently reliable estimation. The mortality impact of the pandemic has shifted from West to East in Europe and globally from North to South. As far as current empirical limitations allow them to be quantified, more than 20 percent of global excess deaths to date might have occurred in India, where an understanding of the scale of the pandemic is slowly emerging, and possibly another 30 percent in countries where there is hardly any reliable source to evaluate the local situation. As the results suggest substantial mortality reversals in many parts of Asia, and possibly Africa as well, of a magnitude rarely observed since 1950, the need for better monitoring mortality trends in these countries cannot be overemphasized (Helleringer and Lanza Queiroz 2021).
An attempt to estimate the global life expectancy since the beginning of the pandemic despite these data limitations indicated a 0.92-year decline between 2019 and 2020 and a 0.72 decline between 2020 and 2021. By contrast, the UN (2019) anticipated a 0.18-year gain in global life expectancy between 2019 to 2020. The 2021 global life expectancy would then be two full years below its previously expected level and below its estimated 2013 level. While it is still too early to confidently quantify this decline in global life expectancy, a decline is already beyond doubt, signaling a unique feature of the mortality changes induced by the pandemic. Each year since 1950, years of life lost to mortality reversals in some parts of the world had been more than compensated by years of life gained from declines in other causes of deaths or in other parts of the world. For the first time in at least 70 years, this was not the case in 2020 and will not be the case in 2021 either.
The decline did appear to stabilize at the end of 2021. As has been the case throughout the pandemic, however, the mortality impact was still increasing in some populations while decreasing in others. The seemingly positive trend merely resulted from the fact that at the end of 2021, the increasing impact was mostly observed in comparatively small populations, in archipelagoes in particular. The end-of-2021 trends looked more encouraging than they had in nearly two years, but It would certainly appear unwise at this point to claim that the impact of the pandemic on the global life expectancy has peaked.
Supplementary Material
Acknowledgments
The author benefited from facilities and resources provided by the California Center for Population Research at UCLA (CCPR), which receives core support (P2C-HD041022) from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD). I thank Michael Tzen and Lilian Chen for producing the world map in Figure 4.
Funding information
The author benefited from facilities and resources provided by the California Center for Population Research at UCLA (CCPR), which receives core support (P2C-HD041022) from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD).
Footnotes
Conflict of interest
The author has no conflict of interest.
Ethics statement
The study has no human subjects. All data are publicly available and contain no identifying information.
Patient consent statement
The study was conducted without patient involvement. Patients were not invited to comment on the study design and were not consulted to develop patient-relevant outcomes or interpret the results. Patients were not invited to contribute to the writing or editing of this document for readability or accuracy.
Permission to reproduce material from other sources
All materials from other sources are publicly available.
Data sharing statement
- Demographic data (2019, 2020, and 2021 world population by age and sex and counterfactual life tables by sex) from the United Nations https://population.un.org/wpp/Download/Standard/Interpolated/
- Global and national numbers of COVID-19 deaths from Johns Hopkins University: https://coronavirus.jhu.edu
- US number of COVID-19 deaths by age and sex from the Centers for Disease Control and Prevention (CDC): https://data.cdc.gov/NCHS/Provisional-COVID-19-Death-Counts-by-Sex-Age-and-S/9bhg-hcku
- Excess mortality estimates are from the World Mortality Dataset (WMD) at https://github.com/akarlinsky/world_mortality
- COVID-19 death undercounts are from The Economist at https://www.economist.com/graphic-detail/coronavirus-excess-deaths-estimates
References
- Aburto José Manuel, Schöley Jonas, Kashnitsky Ilya, Zhang Luyin, Rahal Charles, Missov Trifon I, Mills Melinda C, Dowd Jennifer B, and Kashyap Ridhi. 2021. “Quantifying Impacts of COVID-19 Pandemic Through Life-Expectancy Losses: A Population-Level Study of 29 Countries.” International Journal of Epidemiology 51(1): 63–74. 10.1093/ije/dyab207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adam David. 2022. The Pandemic’s True Death Toll: Millions More Than Official Counts, Nature January 18, 2022. https://www.nature.com/articles/d41586-022-00104-8. [DOI] [PubMed] [Google Scholar]
- Ahmad Farida B., and Anderson Robert N. 2021. “The Leading Causes of Death in the US for 2020.” Journal of the American Medical Association 325(18): 1829–1830. 10.1001/jama.2021.5469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrasfay Theresa, and Goldman Noreen. 2021. “Reductions in 2020 US Life Expectancy Due to COVID-19 and the Disproportionate Impact on the Black and Latino Population.” Proceedings of the National Academy of Sciences of the United States of America 118(5): e2014746118. 10.1073/pnas.2014746118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashton Basil, Hill Kenneth, Piazza Alan, and Zeitz Robin. 1984. “Famine in China, 1958–61.” PDR 10(4): 613–645. [Google Scholar]
- Anand Abhishek, Sandefur Justin, and Subramanian Arvind. 2021. “Three New Estimates of India’s All-Cause Excess Mortality During the COVID-19 Pandemic.” Working Paper 589, Center for Global Development. [Google Scholar]
- Arias Elizabeth, Betzaida Tejada-Vera Farida Ahad, and Kochanek Kenneth D. 2021. “Provisional Life Expectancy Estimates for 2020.” Vital Statistics Rapid Release 15. Hyattsville, MD: National Center for Health Statistics. 10.15620/cdc:107201. [DOI] [Google Scholar]
- Beaney Thomas, Clarke Jonathan M., Jain Vageesh, Golestaneh Amelia K., Lyons Gemma, Salman David, and Majeed Azeem. 2020. “Excess Mortality: The Gold Standard in Measuring the Impact of COVID-19 Worldwide?” Journal of the Royal Society of Medicine 113(9): 329–334. 10.1177/0141076820956802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castro Marcia C., Gurzenda Susie, Turra Cassio M., Kim Sun, Andrasfay Thereas, and Goldman Noreen. 2021. “Reduction in Life Expectancy in Brazil After COVID-19.” Nature Medicine 27: 1629–1635. 10.1038/s41591-021-01437-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan Eunice Y. S., Cheng Davy, and Martin Janet. 2021. “Impact of COVID-19 on Excess Mortality, Life Expectancy, and Years of Life Lost in the United States.” PLoS One 16(9): e0256835. 10.1371/journal.pone.0256835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC). 2022. Provisional COVID-19 Death Counts by Sex, Age and State. Accessed January 3, 2022. https://data.cdc.gov/NCHS/Provisional-COVID-19-Death-Counts-by-Sex-Age-and-S/9bhg-hcku.
- Chiang Chin Long. 1969. An Introduction to Stochastic Processes in Biostatistics. New York: Wiley. [Google Scholar]
- Cutler David, Deaton Angus, and Lleras-Muney Adriana. 2006. “The Determinants of Mortality.” Journal of Economic Perspectives 20(3): 97. 10.1257/jep.20.3.97. [DOI] [Google Scholar]
- Demombynes Gabriel, de Walque Damien, Gubbins Paul, Urdinola Beatriz Piedad, and Veillard Jeremy. 2021. “COVID-19 Age-Mortality Curves for 2020 Are Flatter in Developing Countries Using Both Official Death Counts and Excess Deaths.” Working paper 9807, World Bank Group, Policy Research. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Djaafara Bimandra A., Whittaker Charles, Watson Oliver J., Verity Robert, Brazeau Nicholas F., Widyastuti Widyastuti, Oktavia Dwi, Adrian Verry, Salama Ngabila, Bhatia Sangeeta, Nouvellet Pierre, Ellie Sherrard-Smith Thomas S. Churcher, Surendra Henry, Lina Rosa N., Ekawati Lenny L., Lestari Karina D., Andrianto Adhi, Thwaites Guy, Baird J Kevin, Ghani Azra C, Elyazar Iqbal RF, and Walker Patrick G. T. 2021. “Quantifying the Dynamics of COVID-19 Burden and Impact of Interventions in Java, Indonesia.” MedRxiv [Preprint]. 10.1101/2020.10.02.20198663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong Ensheng, Du Hongru, and Gardner Lauren. 2020. “An Interactive Web-Based Dashboard to Track COVID-19 in Real Time.” The Lancet Infectious Diseases 20(5): 533–534. https://www.thelancet.com/journals/laninf/article/PIIS1473-3099(20)30120-1/fulltext. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (The) Economist. 2022. “The Pandemic’s True Death Toll.” Accessed January 3, 2022. https://www.economist.com/graphic-detail/coronavirus-excess-deaths-estimates.
- Ellege Stephen J. 2020. “2.5 Million Person-Years of Life Have Been Lost Due to COVID-19 in the United States.” MedRxiv [Prepint]. 10.1101/2020.10.18.20214783. [DOI] [Google Scholar]
- Garciá-Guerrero Víctor, and Beltrán-Sánchez Hiram. 2021. “Heterogeneity in Excess Mortality and Its Impact on Loss of Life Expectancy due to COVID-19: Evidence from Mexico.” Canadian Studies in Population 48: 165–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerland Patrick, Raftery Adrian E., Ševčíková Hana, Li Nan, Gu Danan, Spoorenberg Thomas, Alkema Leontine, Fosdick Bailey K., Chunn Jennifer, Lalic Nevena, Bay Guiomar, Buettner Thomas, Heilig Gerhard K., and Wilmoth John. 2014. “World Population Stabilization Unlikely this Century.” Science 346(6206): 234–237. 10.1126/science.1257469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldman Noreen, and Lord Graham. 1986. “A New Look at Entropy and the Life Table.” Demography 23(2): 275–282. 10.2307/2061621. [DOI] [PubMed] [Google Scholar]
- Goldstein Joshua R., and Lee Ronald D. 2020. “Demographic Perspectives on the Mortality of COVID-19 and Other Epidemics.” Proceedings of the National Academy of Sciences of the United States of America 117(36): 22035–22041. 10.1073/pnas.2006392117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guilmoto Christophe Z. 2020. “COVID-19 Death Rates by Age and Sex and the Resulting Mortality Vulnerability of Countries and Regions in the World.” MedRxiv [preprint]. 10.1101/2020.05.17.20097410. [DOI] [Google Scholar]
- Guilmoto Christophe Z. 2022. “An alternative estimation of the death toll of the Covid-19 pandemic in India,” PLoS One 17(2): e0263187. 10.1371/journal.pone.0263187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagan John, and Palloni Alberto. 2006. “Death in Darfur.” Science 313(5793): 1578–1579. [DOI] [PubMed] [Google Scholar]
- Helleringer Stephane, and Queiroz Bernardo Lanza. 2021. “Measuring Excess Mortality due to the COVID-19 Pandemic: Progress and Persistent Challenges.” International Journal of Epidemiology 51(1): 85–87. 10.1093/ije/dyab260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heuveline Patrick. 2015. “The Boundaries of Genocide: Quantifying the Uncertainty of the Death Toll During the Pol Pot Regime in Cambodia (1975–1979).” Population Studies 69(2): 201–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heuveline Patrick. 2021a. “The Mean Unfulfilled Lifespan (MUL): A New Indicator of a Disease Impact on the Individual Lifespan.” PLoS One 16(7): e0254925. 10.1371/journal.pone.0254925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heuveline Patrick. 2021b. “The COVID-19 Pandemic Adds Another 200,000 Deaths (50%) to the Annual Toll of Excess Mortality in the United States.” Proceedings of the National Academy of Sciences of the United States of America 118(36): e2107590118. 10.1073/pnas.2107590118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heuveline Patrick, and Tzen Michel. 2021. “Beyond Deaths per Capita: Comparative COVID-19 Mortality Indicators.” British Medical Journal Open 11(3): e042934. 10.1136/bmjopen-2020-042934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ioannidis John P., Axfors Catherine, and Contopoulos-Ioannidis Despina G. 2021. “Second Versus First Wave of COVID-19 Deaths: Shifts in Age Distribution and in Nursing Home Fatalities.” Environmental Research 195: 110856. 10.1016/j.envres.2021.110856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Islam Nazrul, Jdanov Dmitri A., Shkolnikov Vladimir M., Khunti Kamlesh, Kawachi Ichiro, White Martin, Lewington Sarah, and Lacey Ben. 2021. “Effects of Covid-19 Pandemic on Life Expectancy and Premature Mortality in 2020: Time Series Analysis in 37 Countries.” British Medical Journal 375: e066768. 10.1136/bmj-2021-066768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jdanov Dmitri A., Alustiza-Galarza Ainhoa, Shkolnikov Vladimir M., Jasilionis Domantas, Németh László, Leon David A., Boe Carl, and Barbieri Magali. 2021. “The Short-Term Mortality Fluctuations Data Series, Monitoring Mortality Shocks Across Time and Space.” Scientific Data 8: 235. https://www.nature.com/articles/s41597-021-01019-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prabhat Jha, Deshmukh Yashwant, Tumbe Chinmay, Suraweera Wilson, Bhowmick Aditi, Sharma Sankalp, Novosad Paul, Fu Sze Hang, Newcombe Leslie, Gelband Hellen, and Brown Patrick. 2022. “COVID Mortality in India: National Survey Data and Health Facility Deaths.” Science 375(6581): 667–671. 10.1126/science.abm5154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johns Hopkins University (JHU). 2022. Coronavirus Resource Center. Accessed January 3, 2022. https://coronavirus.jhu.edu.
- Ariel Karlinsky, and Kobak Dmitry. 2021. “Tracking Excess Mortality Across Countries During the COVID-19 Pandemic with the World Mortality Dataset.” eLife 10: e69336. 10.7754/eLife.69336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vasilis Kontis, Bennett James E., Rashid Theo, Parks Robbie M., Pearson-Stuttard Johnathan, Guillot Michel, Asaria Perviz, Zhou Bin, Battaglini Marco, Corsetti Gianni, McKee Martin, Cesare Mariachiara Di, Mathers Colin D., and Ezzati Majid. 2020. “Magnitude, Demographics and Dynamics of the Effect of the First Wave of the COVID-19 Pandemic on All-Cause Mortality in 21 Industrialized Countries.” Nature Medicine 26: 1919–1928. 10.1038/s41591-020-1112-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koum Besson Emily S, Norris Andy, Bin Ghouth Abdulla S., Freemantle Terri, Alhaffar Mervat, Vazquez Yolanda, Reeve Chris, Curran Patrick. J., and Checchi Francesco. 2021. “Excess Mortality During the COVID-19 Pandemic: A Geospatial and Statistical Analysis in Aden Governorate, Yemen.” British Medical Journal Global Health 6: e004564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyfitz Nathan. 1977. “What Difference Would It Make if Cancer Were Eradicated? An Examination of the Taeuber Paradox.” Demography 14(4): 411–418. 10.2307/2060587. [DOI] [PubMed] [Google Scholar]
- Lima Everton EC, Vilela Estevão A., Peralta Andrés, Rocha Marília, Queiroz B ernardo L., Gonzaga Marcos R., Piscoya-Díaz Mario, Martinez-Folgar Kevin, García-Guerrero Víctor. M., and Freire Flávio H. M. A. 2021. “Investigating Regional Excess Mortality During 2020 COVID-19 Pandemic in Selected Latin American Countries.” Genus 77: 30. 10.1186/s41118-021-00139-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Modig Karin, Rau Roland, and Ahlbom Anders. 2020. “Life Expectancy: What Does it Measure?” British Medical Journal Open 10(7), e035932. https://bmjopen.bmj.com/content/10/7/e035932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mwananyanda Lawrence, Gill Christopher J., MacLeod William, Kwenda Geoffrey, Pieciak Rachel, Mupila Zachariah, Lapidot Rotem, Mupeta Francis, Forman Leah, Ziko Luunga, Etter Lauren, and Thea Donald. 2021. “Covid-19 Deaths in Africa: Prospective Systematic Postmortem Surveillance Study.” British Medical Journal 372: n334. 10.1136/bmj.n334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy Sherry L., Kochanek Kenneth D., Xu Jiaquan, and Arias Elizabeth. 2021. “Mortality in the United States, 2020.” Data Brief 427, NCHS, Hyattsville, MD: National Center for Health Statistics. https://www.cdc.gov/nchs/products/databriefs/db427.htm [Google Scholar]
- Nepomuceno Marilia R., Klimkin Ilya, Jdanov Dmitri A., Galarza Ainhoa Alustiza, and Shkolnikov Vladimir. 2022. “Sensitivity of Excess Mortality Due to the COVID-19 Pandemic to the Choice of the Mortality Index, Method, Reference Period, and the Time Unit of the Death Series.” Population and Development Review 10.1111/padr.12475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Obermeyer Ziad, Murray Christopher J. L., and Gakidou Emmanuella. 2008. “Fifty Years of Violent War Deaths from Vietnam to Bosnia: Analysis of Data from World Health Survey Programme.” British Medical Journal 336 (7659): 1482–1486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohnishi Akira, Namekawa Yusuke, and Fukui Tokuro. 2020. “Universality in COVID-19 Spread in View of the Gompertz Function.” Progress of Theoretical and Experimental Physics 12: 123J01. 10.1093/ptep/ptaa148. [DOI] [Google Scholar]
- Olshansky S. Jay, Carnes Bruce A., and Désesquelles Aline. 2001. “Prospects for Human Longevity.” Science 291(5508): 1491–1492. 10.1126/science.291.5508.1491 [DOI] [PubMed] [Google Scholar]
- Our World In Data (OWID). 2021. Accessed December 7, 2021. https://ourworldindata.org/excess-mortality-covid.
- O’Driscoll Megan, Santos Gabriel Ribeiro Dos, Wang Lin, Cummings Derek A. T., Azman Andrew S., Paireau Juliette, Fontanet Arnaud, Cauchemez Simon, and Salje Henrik. 2021. “Age-Specific Mortality and Immunity Patterns of SARS-CoV-2.” Nature 590: 140–145. 10.1038/s41586-020-2918-0. [DOI] [PubMed] [Google Scholar]
- Papon Sylvain, and Beaumel Catherine. 2021. “Avec la pandémie de Covid-19, nette baisse de l’ésperance de vie et chute du nombre de mariages.” Insee Première 1834. https://www.insee.fr/fr/statistiques/5012724 [Google Scholar]
- Pifarré i Arolas Héctor, Acosta Enrique, López Casasnovas Guillem, Lo Adeline, Nicodemo Catia, Riffe Tim, and Myrskylä Mikko. 2021. “Global Years of Life Lost to COVID-19.” Nature Scientific Reports 11: 3504. https://www.nature.com/articles/s41598-021-83040-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preston Samuel H., Elo Irma T., Rosenwaike Ira, and Hill Mark. 1996. “African-American Mortality at Older Ages: Results of a Matching Study.” Demography 33(2): 193–209. 10.2307/2061872. [DOI] [PubMed] [Google Scholar]
- Preston Samuel H., Heuveline Patrick, and Guillot Michel. 2001. Demography: Measuring and Modeling Population Processes. Malden, MA: Blackwell. [Google Scholar]
- Schöley J 2021. Robustness and Bias of European Excess Death Estimates in 2020 Under Varying Model Specifications. MedRxiv [Preprint]. 10.1101/2021.06.04.21258353v1. [DOI]
- United Nations. 2019. World Population Prospects 2019, Online Edition. New York: United Nations. https://population.un.org/wpp/Download/Standard/Interpolated/. [Google Scholar]
- United Nations Development Programme (UNDP). 2020. The Human Development Report 2020. New York: UNDP. http://hdr.undp.org/en/2020-report [Google Scholar]
- Verdery Ashton M, Smith-Greenaway Emily, Margolies Rachel, and Daw Jonathan. 2020. “Tracking the Reach of COVID-19 Kin Loss with a Bereavement Multiplier Applied to the United States.” Proceedings of the National Academy of Sciences of the United States of America 117(30): 17695–17701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verwimp Philip. 2004. “Death and Survival During the 1994 Genocide in Rwanda.” Population Studies 58(2): 233–245. [DOI] [PubMed] [Google Scholar]
- Vestergaard Lasse S., Nielsen Jens, Richter Lukas, Schmid Daniela, Bustos Natalia, Braeye Toon, Vestergaard1 Lasse S, Nielsen1 Jens, Richter2 Lukas, Schmid2 Daniela, Bustos3 Natalia, Braeye3 Toon, Denissov Gleb, Veideman Tatjana, Luomala Oskari, Möttönen Teemu, Fouillet Anne, Caserio-Schönemann Céline, an der Heiden Matthias, Uphoff Helmut, Lytras Theodore, Gkolfinopoulou Kassiani, Paldy Anna, Domegan Lisa, O’Donnell Joan, de’ Donato Francesca, Noccioli Fiammetta, Hoffmann Patrick, Velez Telma, England Kathleen, van Asten Liselotte, White Richard A, Tønnessen Ragnhild, da Silva Susana P, Rodrigues Ana P, Larrauri Amparo, Delgado-Sanz Concepción, Farah Ahmed, Galanis Ilias, Junker Christoph, Perisa Damir, Sinnathamby Mary, Andrews Nick, O’Doherty Mark, Marquess Diogo FP, Kennedy Sharon, Olsen Sonja J, Pebody Richard, Krause Tyra G, and Mølbak Kåre. 2020. “Excess All-Cause Mortality During the COVID-19 Pandemic in Europe – Preliminary Pooled Estimates from the EuroMOMO Network, March to April 2020.” ECDC Public Health Emergency Team for COVID-19 26(25): 28. 10.2807/1560-7917.ES.2020.25.26.2001214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson Oliver J., Abdelmagid Nada, Ahmed Aljaile, Elhameed Abd Elhameed Ahmed Abd, Whittaker Charles, Brazeau Nicholas, Hamlet Arran, Walker Patrick, Hay James, Ghani Azra, Checchi Francesco, and Dahab Maysoon. 2020. “Characterising COVID-19 Epidemic Dynamics and Mortality Under-Ascertainment in Khartoum, Sudan.” Report 39, MRC Centre for Global Infectious Disease Analysis, Imperial College London. 10.25561/84283. [DOI] [Google Scholar]
- Watson Oliver J., Alhaffar Mervat, Mehchy Zaki, Whittaker Charles, Akil Zack, Brazeau Nicholas F., Cuomo-Dannenburg G, Hamlet Arran, Thompson Hayley A., Baguelin Marc, FitzJohn Richard G., Knock Edward, Lees John A., Whittles Lilith. K., Mellan Thomas, Winskill Peter, Howard Natasha, Clapham Hannah, Checchi Francesco, Ferguson Neil, Ghani Azra, Beals Emma, and Walker Patrick, Imperial College COVID-19 Response Team, Leveraging community mortality indicators to infer COVID-19 mortality and transmission dynamics in Damascus, Syria. Nat Commun. 2021. “Leveraging Community Mortality Indicators to Infer COVID-19 Mortality and Transmission in Damascus, Syria.” Nature Communications 12: 2394. 10.1038/s41467-021-22474-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


