Abstract
Objective
Safety of home fortificants in children is uncertain in areas where infections are common. We tested the hypothesis that provision of lipid-based nutrient supplements (LNS) containing Fe does not increase infectious morbidity in children.
Design
Randomized controlled trial. Infants were randomised to receive 10, 20 or 40 g LNS/d; or no supplement until age 18 months. All LNS contained 6 mg Fe/d. Morbidity outcomes (serious adverse events, non-scheduled visits and guardian-reported morbidity episodes) were compared between control and intervention groups using a non-inferiority margin of 20 %.
Setting
Namwera and Mangochi catchment areas in rural Malawi.
Subjects
Infants aged 6 months (n 1932).
Results
The enrolled 1932 infants contributed 1306 child-years of follow-up. Baseline characteristics were similar across groups. Compared with the control group, the relative risk (95 % CI) of serious adverse events was 0·71 (0·48, 1·07), 0·67 (0·48, 0·95) and 0·91 (0·66, 1·25) in 10, 20 and 40 g LNS/d groups, respectively. The incidence rate ratio (95 % CI) of non-scheduled visits due to malaria was 1·10 (0·88, 1·37), 1·08 (0·89, 1·31) and 1·21 (1·00, 1·46), and of guardian-reported morbidity episodes was 1·04 (0·96, 1·11), 1·03 (0·97, 1·10) and 1·04 (0·97, 1·10), in the respective LNS groups.
Conclusions
Provision of 10 and 20 g LNS/d containing 6 mg Fe/d did not increase morbidity in the children. Provision of 40 g LNS/d did not affect guardian-reported illness episodes but may have increased malaria-related non-scheduled visits.
Keywords: Lipid-based nutrient supplements, Infectious disease morbidity, Iron, Children, Low-income countries
The WHO recommends the use of Fe supplements or home fortificants to improve Fe status and reduce anaemia prevalence among infants and children aged 6–23 months in low-income countries( 1 ). Although home fortificants (such as multiple micronutrient powders (MNP) and small-quantity lipid-based nutrient supplements (LNS)) may have positive effects on children’s micronutrient status, their safety is less well documented, especially in areas where infections are common( 2 ). While some studies suggest that home fortificants are safe( 3 , 4 ) and may reduce morbidity( 5 ), others have reported harmful effects. In Pakistan, provision of MNP with or without Zn as home fortificants was associated with increased risk of diarrhoea and reported chest in-drawing in children( 6 ). Findings from a study in Kenya suggest that Fe fortification modifies the gut microbiome, increasing pathogenic bacteria and causing intestinal inflammation( 7 ). An increased risk of malaria infection and deaths has also been reported in a large trial using Fe and folic acid supplements in Zanzibar, also raising concerns about Fe supplementation in Fe-replete children living in malaria-endemic regions. Excess free Fe circulating in blood may also aid growth of pathogens such as malaria parasites( 8 ).
Currently, there is interest in testing the efficacy and effectiveness of providing LNS as home fortificants to prevent undernutrition and micronutrient deficiencies for programmatic use in vulnerable populations. LNS products are similar to MNP because they contain a range of vitamins and minerals, including Fe. There are concerns about Fe provision to children in areas where malaria is endemic( 9 ). However, there is little evidence regarding the safety of Fe-containing LNS. Safety studies have mainly been reported about MNP, although with conflicting results( 3 , 4 , 6 , 10 ). A few reports on LNS provision for prevention of child undernutrition suggest that it is safe( 11 – 13 ), but the evidence is not conclusive because those studies had either a relatively short duration (i.e. 6 months or less) or insufficient power because of small sample sizes( 14 ).
The iLiNS-DOSE study was a large randomized controlled trial with a primary objective of testing the efficacy of different doses of LNS in promoting linear growth in children in a rural Malawian population. In the main outcome paper, we reported that supplementation with LNS for 1 year did not promote length gain or prevent stunting( 15 ). However, other studies in Ghana( 11 ), Burkina Faso( 16 ) and Malawi( 17 ) reported significant length gain and reduction in stunting associated with LNS. Considering the evidence from these studies, we aimed to assess, as a secondary outcome, the safety of LNS when provided to young children in a malaria-endemic area. In the current analysis, we tested the hypothesis that provision of Fe-containing LNS does not increase infectious disease morbidity when provided to infants and young children for 12 months.
Methods
Study sites and participants
We conducted the study in communities within the catchment areas of Mangochi district hospital and Namwera health centre in the south-eastern part of Malawi. Mangochi district hospital outpatient department serves an estimated population of 100 000 people, whereas Namwera health centre serves a rural population of ~22 000. The hospital catchment area is partly semi-urban, while Namwera is predominantly rural. In this area, the major causes of death among children aged <5 years are malaria (17 %), pneumonia (13 %) and diarrhoeal diseases (11 %)( 18 , 19 ). These diseases are prevalent in the catchment area throughout the year with seasonal fluctuations. The prevalence of HIV is 10·3 % (ages 15–49 years) and an estimated 170 000 children aged 0–14 years are living with HIV/AIDS in Malawi( 20 ).
For a period of 18 months (November 2009 to May 2011), we identified potential participants in the catchment areas through community surveys and invited them to the study clinic for further eligibility assessment. Children who were 5·50 to 6·49 months old, whose guardians had signed informed consent and planned to be available during the whole study period were considered eligible. Exclusion criteria were any severe illness warranting hospital referral, bipedal oedema, Hb<50 g/l, family history of peanut allergy, concurrent participation in another clinical trial and weight-for-height Z-score <−2. We excluded children with weight-for-height Z-score <−2 because these children are at risk of developing severe acute malnutrition. Children with severe acute malnutrition are treated through the national nutritional rehabilitation programmes, therefore were more likely to deviate from our trial protocol. To identify the lowest growth-promoting daily dose and formulation of LNS and to test the hypothesis that milk-free LNS would promote growth equally well as milk-containing LNS, we randomly assigned the children to six groups as follows: milk-containing LNS 10 g/d, 20 g/d and 40 g/d; milk-free LNS 20 g/d and 40 g/d; and a control group which did not receive LNS during the 12-month study period. The nutrient compositions of the five different doses of LNS are reported in Table 1. We used a reduced dose of Fe (6 mg) in the LNS because of safety concerns based on recommendations from the WHO( 9 ). The Zn content (8 mg) was based on the WHO/FAO Recommended Nutrient Intakes for diets with low bioavailability( 21 ). The rationale for selecting specific nutrient levels for LNS is described in detail elsewhere( 22 ).
Table 1.
Nutrient and energy contents of the food supplements used in the present study
| Nutrient | 10 g milk LNS | 20 g milk LNS | 20 g milk-free LNS | 40 g milk LNS | 40 g milk-free LNS |
|---|---|---|---|---|---|
| Daily ration (g) | 10 | 20 | 20 | 40 | 40 |
| Total energy (kJ) | 230 | 490 | 490 | 1008 | 1008 |
| Total energy (kcal) | 55 | 117 | 117 | 241 | 241 |
| Protein (g) | 1·3 | 2·5 | 1·0 | 5·0 | 2·0 |
| Fat (g) | 4·7 | 9·5 | 9·4 | 18·9 | 18·8 |
| Linoleic acid (g) | 2·22 | 4·44 | 4·44 | 8·88 | 8·88 |
| α-Linolenic acid (g) | 0·29 | 0·58 | 0·58 | 1·16 | 1·16 |
| Vitamin A (μg RE) | 400 | 400 | 400 | 400 | 400 |
| Vitamin C (mg) | 30 | 30 | 30 | 30 | 30 |
| Thiamin (mg) | 0·3 | 0·3 | 0·3 | 0·3 | 0·3 |
| Riboflavin (mg) | 0·4 | 0·4 | 0·4 | 0·4 | 0·4 |
| Niacin (mg) | 4 | 4 | 4 | 4 | 4 |
| Folic acid (μg) | 80 | 80 | 80 | 80 | 80 |
| Pantothenic acid (mg) | 1·8 | 1·8 | 1·8 | 1·8 | 1·8 |
| Vitamin B6 (mg) | 0·3 | 0·3 | 0·3 | 0·3 | 0·3 |
| Vitamin B12 (μg) | 0·5 | 0·5 | 0·5 | 0·5 | 0·5 |
| Vitamin D (µg) | 5 | 5 | 5 | 5 | 5 |
| Vitamin E (mg) | 6 | 6 | 6 | 6 | 6 |
| Vitamin K (μg) | 30 | 30 | 30 | 30 | 30 |
| Fe (mg) | 6 | 6 | 6 | 6 | 6 |
| Zn (mg) | 8 | 8 | 8 | 8 | 8 |
| Cu (mg) | 0·34 | 0·34 | 0·34 | 0·34 | 0·34 |
| Ca (mg) | 240 | 240 | 240 | 240 | 240 |
| P (mg) | 208 | 208 | 208 | 208 | 208 |
| K (mg) | 265 | 265 | 265 | 265 | 265 |
| Mg (mg) | 50 | 50 | 50 | 50 | 50 |
| Se (μg) | 20 | 20 | 20 | 20 | 20 |
| Iodine (μg) | 90 | 90 | 90 | 90 | 90 |
| Mn (mg) | 1·2 | 1·2 | 1·2 | 1·2 | 1·2 |
| Phytate (mg) | 28 | 56 | 56 | 112 | 112 |
LNS, lipid-based nutrient supplement; RE, retinol equivalents.
Randomization and masking
The details of the randomization process are described in the main outcome paper( 15 ). Briefly, when the guardian consented to let her infant participate and the infant met all the enrolment criteria, the guardian was asked to choose and open one randomization envelope from a block of six unused envelopes. The envelope contained the participant identification code and supplement code. Randomization into the trial and group allocation was done by a randomizer not participating in the analysis. The investigators involved in data cleaning and analysis were blinded to the group allocation.
Data collection and participant follow-up
Research assistants visited the participants’ homes every week to deliver supplements and collect morbidity data. The data were collected by interviewing the guardians about the child’s health in the previous 7 d using a structured questionnaire. The information was complemented by a picture calendar filled out by the guardians on a daily basis to aid memory of their child’s morbidity status. These were done to minimize problems of recall associated with community morbidity assessments( 23 ). The research assistants collecting morbidity data knew which children were receiving LNS.
We trained health workers to collect data on non-scheduled visits made to health centres when the child was sick, including data for hospitalizations and hospital deaths. For deaths occurring at home, the information was collected by a verbal autopsy method, previously validated in the study area( 24 ). Records of all hospitalizations and deaths were reviewed as serious adverse events (SAE) by a study physician and reported to members of the data and safety monitoring board within 48 h of occurrence.
Anthropometric measurements were taken by research assistants who underwent training and standardization every 6 months. Research assistants who took anthropometric measurements were not aware of group allocation. The details of anthropometric, biochemical and socio-economic measurements and cleaning of anthropometry data are explained in the main outcome paper( 15 ) and in the statistical analysis plans published on the iLiNS website( 25 ).
Ethics
The study was performed according to International Conference of Harmonization–Good Clinical Practice (ICH-GCP) guidelines and the ethical standards of the Helsinki Declaration. The protocol was reviewed and approved by the Institutional Review Boards of the University of Malawi, College of Medicine (IRB reference number P.01/09/722) and the Pirkanmaa Hospital District, Finland (IRB reference number R09130). At least one guardian signed or thumb-printed an informed consent form before enrolment of each participant. The trial was registered at the clinical trials registry (www.clinicaltrials.gov) with the registration ID of NCT00945698. An independent data safety and monitoring board monitored the incidence of suspected SAE during the trial.
Outcomes
We assessed the following morbidity outcomes at the end of the follow-up: SAE, non-scheduled visits, diagnoses made at non-scheduled visits and guardian-reported morbidity symptoms and disease episodes.
SAE were comprised of hospitalizations and deaths, defined according to the US Department of Health and Human Services Office for Human Research Protections( 26 ). Non-scheduled visits were defined as visits made by the participants to any health facility because of illness. At each non-scheduled visit, a diagnosis of malaria, gastroenteritis, acute respiratory infection or other illnesses was made by health workers.
For home visits, diagnoses of gastroenteritis, acute respiratory infection and ‘undefined fever’ were derived from a combination of guardian-reported morbidity symptoms recorded on one or more days.
To ensure that the diagnoses derived from symptoms at home visits were mutually exclusive a diagnosis algorithm was created, whereby any diarrhoea episode (three or more loose stools in 24 h) was categorized as gastroenteritis with or without other symptoms. If diarrhoea was absent but there was presence of any respiratory symptoms (cough, rapid or difficult breathing and nasal discharge) with or without fever, a diagnosis of acute respiratory infection was made. Fever episodes in the absence of diarrhoea and respiratory symptoms, with or without other symptoms, were categorized as ‘undefined fever’. The rest of the symptoms in the absence of diarrhoea, respiratory symptoms and fever were categorized as other illnesses. For all diseases, an episode was defined as the period starting from the day the child had symptoms if preceded by at least two days of either no symptoms or no data. The episode ended on the last day the child had symptoms which was then followed by at least two symptom-free days.
We defined anaemia as Hb<105 g/l based on suggested reference values for infants( 27 ). We defined Fe deficiency as Zn protoporphyrin>70 µmol/mol haem, measured from washed red blood cells( 28 , 29 ).
Sample size calculation
The sample size was calculated based on the primary objective of the main study: to test the hypothesis of non-inferiority of LNS without milk on change in length-for-age Z-score as compared with LNS containing milk. Assuming an sd for the change in length-for-age Z-score of 1·0, a predetermined non-inferiority margin of 0·25 Z-score units and an estimated 15 % attrition rate, a sample size of 320 per group was estimated to provide the trial with 90 % power and 95 % confidence (one-sided test) to discard an inferiority null hypothesis. Morbidity (the outcome for the present paper) was a secondary outcome of the study. We did not calculate a separate sample size or post hoc power for the morbidity outcome. We relied on the confidence interval to determine if the sample size was adequate for each of the morbidity outcomes, as recommended by several scholars( 30 , 31 ).
Data entry and management
The data were double-entered using Microsoft® Access, REDCap™ and TELEform ®. Typographical errors, extreme observations and discrepancies were resolved prior to breaking the randomization code. Analyses were done using the statistical software package Stata version 12·1.
Statistical analysis
Our hypothesis was that the risk of morbidity among children would not be significantly higher in the intervention groups compared with the control group. We used a non-inferiority approach to compare the risk of morbidity between the intervention groups and the control group. We chose a predefined non-inferiority margin of no greater than 20 % increase in morbidity in the intervention groups compared with the control group to conclude that there was no difference in morbidity. We assumed that an increase in morbidity of 20 % or more in the LNS groups relative to the control would be clinically significant, with negative impact on the overall health of the children. There is no agreed definition of non-inferiority in this context, but an increase between 15 % and 20 % in morbidity has previously been considered clinically significant( 3 , 4 , 6 , 8 , 13 ). The non-inferiority approach and the margin of 20 % were predefined in the statistical analysis plan published at the iLiNS website( 25 ) before starting the analysis.
We intended to confirm non-inferiority if the entire 95 % CI (two-sided) for the risk ratio (RR)/incidence rate ratio (IRR) was below the value of 1·20. For each morbidity outcome, we anticipated the following four possible conclusions: (i) if the upper bound of the 95 % CI for the RR/IRR was <1·20, a conclusion of non-inferiority would be made; (ii) if the lower bound of the 95 % CI for the RR/IRR was >1·20, a conclusion of inferiority (suggesting a harmful effect) would be made; (iii) if the upper bound of the 95 % CI for the RR/IRR was <1·00, a conclusion of superiority (suggesting a beneficial effect) would be made; and (iv) If the upper bound of the 95 % CI for the RR/IRR was >1·20 and lower bound was <1·20, the findings would be considered inconclusive for target group inference.
Risks of experiencing an SAE (hospitalization or death) were calculated as numbers of participants experiencing an SAE divided by the total number of participants in each group. We used generalized linear modelling (log-binomial family) to estimate and compare the risks between the intervention groups and the control group, reported as RR (95 % CI). Longitudinal prevalences of common morbidity symptoms were defined as proportions of days when the child had an illness among all days of observation for each child. We compared the longitudinal prevalence for each intervention group with the control group by first log-transforming the data, then performed ordinary least squares regression, and exponentiated the regression coefficients and their 95 % CI. Incidences of non-scheduled visits and guardian-reported disease episodes in each group were calculated as the sum of visits or episodes across individuals divided by total child-years in each group. We used negative binomial regression to compare the incidences between the intervention groups and the control group, reported as IRR (95 % CI).
The primary analysis was done on the intention-to-treat basis. As secondary analysis, the outcomes were fitted in models that included the following covariates at baseline: age, sex, weight-for-length Z-score, weight-for-age Z-score, length-for-age Z-score, Fe status, Hb status, seasonality, maternal education, marital status, household food insecurity (using the Household Food Insecurity Access Scale), household water source and sanitation.
We planned first to compare between the milk and non-milk groups of the same dose, then proceed to collapse the groups if there were no differences between the milk and non-milk groups of the same LNS dose. We outlined this plan in the statistical analysis plan published at our website( 25 ). Although the Fe content was originally the same in all LNS doses, we observed differences in daily intake of LNS between the groups (those given the higher doses of LNS/d consumed a lower proportion)( 32 ), suggesting that the actual daily dose of Fe and other micronutrients also varied among the intervention groups. Therefore we analysed the groups according to the different daily doses of LNS provided.
Results
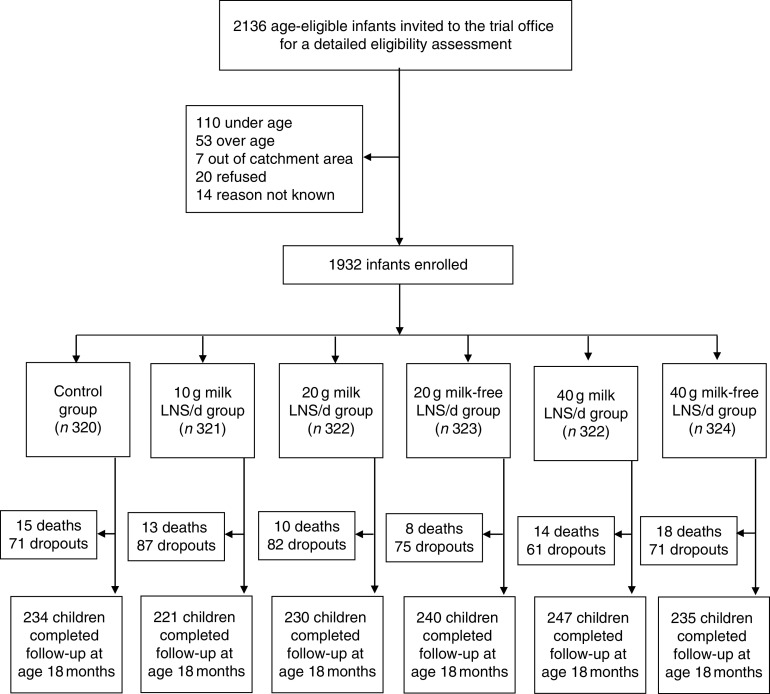
We conducted the iLiNS-DOSE study between November 2009 and May 2012. Out of 2136 infants who came to the study clinic for assessment, 1932 were enrolled and randomized into the six study groups. The group allocation, reasons for exclusion and loss to follow-up are shown in Fig. 1. At baseline, the mean age of the participants was 5·9 (sd 0·3) months and their mean length-for-age Z-score and weight-for-height Z-score were −1·4 (sd 1·1) and +0·3 (sd 1·1), respectively. The proportions of children with stunting, a positive malaria test, severe anaemia (Hb<80 g/l), moderate to severe anaemia (Hb<105 g/l), Fe deficiency (Zn protoporphyrin>70 µmol/mol haem) or Fe-deficiency anaemia were 29·3 %, 16·3 %, 7·9 %, 50·8 %, 66·0 % and 42·0 %, respectively. The reported bed-net utilization by participants was 81·0 %. There were no differences between the groups in the baseline characteristics (Table 2). No episodes of suspected allergy or intolerance of the supplement were recorded during the trial.
Fig. 1.
Participant flow in the present study (LNS, lipid-based nutrient supplement)
Table 2.
Baseline characteristics of the participating rural Malawian infants and young children, iLiNS-DOSE study, November 2009–May 2012
| Control (n 320) | 10 g LNS/d (n 321) | 20 g LNS/d (n 645) | 40 g LNS/d (n 646) | |||||
|---|---|---|---|---|---|---|---|---|
| Variable | n or Mean | % or sd | n or Mean | % or sd | n or Mean | % or sd | n or Mean | % or sd |
| Participants (n, % boys) | 168 | 52·5 | 156 | 48·6 | 331 | 51·3 | 314 | 48·6 |
| Age in months (mean, sd) | 5·9 | 0·3 | 5·9 | 0·3 | 5·9 | 0·3 | 5·9 | 0·3 |
| WAZ (mean, sd) | −0·7 | 1·2 | −0·7 | 1·2 | −0·7 | 1·2 | −0·8 | 1·1 |
| LAZ (mean, sd) | −1·4 | 1·1 | −1·4 | 1·1 | −1·4 | 1·0 | −1·4 | 1·1 |
| WLZ (mean, sd) | 0·3 | 1·2 | 0·3 | 1·1 | 0·3 | 1·1 | 0·2 | 1·1 |
| Hb<105 g/l (n, %) | 145 | 45·6 | 165 | 51·6 | 321 | 50·2 | 343 | 53·8 |
| ZPP>70 µmol/mol haem (n, %) | 208 | 67·5 | 195 | 62·9 | 389 | 63·7 | 423 | 69·1 |
| Malaria RDT-positive (n, %) | 54 | 18·2 | 51 | 17·2 | 92 | 15·5 | 94 | 15·8 |
| Maternal education, completed years (mean, sd) | 4·7 | 3·7 | 4·7 | 3·6 | 4·7 | 3·5 | 4·6 | 3·5 |
| Persons in the household (mean, sd) | 5·5 | 2·3 | 5·4 | 2·4 | 5·4 | 2·4 | 5·5 | 2·2 |
LNS, lipid-based nutrient supplement; WAZ, weight-for-age Z-score; LAZ, length-for-age Z-score; WLZ, weight-for-length Z-score; ZPP, Zn protoporphyrin; RDT, rapid diagnostic test.
The enrolled children contributed a total of 1306 child-years of follow-up, i.e. the mean length of follow-up was 251 (sd 94) d/child. A total of 1534 (79·4 %) children remained in follow-up at 18 months of age and we managed to see 1407 (72·8 %) children on the final home visit. There were no intergroup differences either in the mean length of follow-up (P=0·974) or the proportion of children who remained in the study until its end (P=0·334). We did not see differences in morbidity outcomes between the milk and non-milk groups of the same dose (each P>0·05); therefore we proceeded to collapse the groups. We present all the results by daily ration of LNS (0, 10, 20 or 40 g/d), irrespective of the milk content of the supplement.
We recorded 271 SAE among the study participants. Of these, seventy-eight were deaths (4·0 % of the enrolled participants) and 193 were hospitalizations. Compared with the control group, the 95 % CI for the RR of experiencing an SAE was entirely below 1·20 (suggestive of non-inferiority) in the 10 g LNS/d group, entirely below 1·00 (suggestive of a protective effect) in the 20 g LNS/d group and ranged from 0·66 to 1·25 (inconclusive) in the 40 g LNS/d group. The 95 % CI for the RR of hospitalizations was entirely below 1·20 (suggestive of non-inferiority) in the 10 and 20 g LNS/d groups, and ranged from 0·57 to 1·22 (inconclusive) in the 40 g LNS/d group (Table 3). The 95 % CI for the risk of death was entirely below 1·20 (suggestive of non-inferiority) in the 20 g LNS/d group, and ranged from 0·42 to 1·79 and 0·58 to 1·92 (inconclusive) in the 10 and 40 g LNS/d groups, respectively (Table 3).
Table 3.
Risk of serious adverse events (SAE) by intervention group among rural Malawian infants and young children, iLiNS-DOSE study, November 2009–May 2012
| Results by study group | Comparison between the groups† | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Control (n 320) | 10 g LNS/d (n 321) | 20 g LNS/d (n 645) | 40 g LNS/d (n 646) | 10 g LNS/d v. control | 20 g LNS/d v. control | 40 g LNS/d v. control | ||||||||
| Variable | n | % | n | % | n | % | n | % | RR | 95 % CI | RR | 95 % CI | RR | 95 % CI |
| Total SAE | 57 | – | 39 | – | 77 | – | 98 | – | ||||||
| Children who reported any SAE | 50 | 15·6 | 36 | 11·2 | 68 | 10·5 | 92 | 14·2 | 0·71 | 0·48, 1·07 | 0·67 | 0·48, 0·95* | 0·91 | 0·66, 1·25 |
| Children who were hospitalized | 38 | 11·9 | 25 | 7·8 | 53 | 8·2 | 64 | 9·9 | 0·66 | 0·41, 1·06 | 0·69 | 0·47, 1·03 | 0·83 | 0·57, 1·22 |
| Children who died | 15 | 4·7 | 13 | 4·1 | 18 | 2·8 | 32 | 5·0 | 0·86 | 0·42, 1·79 | 0·60 | 0·30, 1·17 | 1·05 | 0·58, 1·92 |
LNS, lipid-based nutrient supplement; RR, risk ratio.
Statistically significant result.
Groups were compared using generalized linear modelling (log-binomial family).
In total, we recorded 9034 non-scheduled visits to health facilities due to illnesses (5·2 non-scheduled visits/child per year of follow-up). Compared with the control group, the 95 % CI for the IRR of non-scheduled visits was entirely below 1·20 (suggestive of non-inferiority) in the 10 and 20 g LNS/d groups. The incidence was 13 % higher in the 40 g LNS/d group but the lower bound of the 95 % CI for the IRR was <1·20 (inconclusive; Table 4). For non-scheduled visits due to malaria (confirmed by rapid diagnostic test), acute respiratory infection and other illnesses, the incidences were, respectively, 21 %, 14 % and 13 % higher in the 40 g LNS/d group than in the control group, but the comparisons were also inconclusive (Table 4).
Table 4.
Incidence† of non-scheduled visits and clinical diagnoses among rural Malawian infants and young children, iLiNS-DOSE study, November 2009–May 2012
| Results by study group | Comparison between the groups‡ | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Control (follow-up years: 296·7) | 10 g LNS/d (follow-up years: 294·9) | 20 g LNS/d (follow-up years: 595·8) | 40 g LNS/d (follow-up years: 601·9) | 10 g LNS/d v. control | 20 g LNS/d v. control | 40 g LNS/d v. control | ||||||||
| Variable | Total visits | Incidence | Total visits | Incidence | Total visits | Incidence | Total visits | Incidence | IRR | 95 % CI | IRR | 95 % CI | IRR | 95 % CI |
| All non-scheduled visits | 1412 | 4·8 | 1417 | 4·8 | 2988 | 5·0 | 3217 | 5·3 | 1·02 | 0·89, 1·18 | 1·05 | 0·93, 1·19 | 1·13 | 1·00, 1·27* |
| Gastroenteritis | 163 | 0·5 | 159 | 0·5 | 298 | 0·5 | 324 | 0·5 | 0·98 | 0·76, 1·27 | 0·91 | 0·73, 1·14 | 0·98 | 0·79, 1·22 |
| ARI | 454 | 1·5 | 446 | 1·5 | 938 | 1·6 | 1041 | 1·7 | 1·02 | 0·84, 1·22 | 1·04 | 0·88, 1·22 | 1·14 | 0·98, 1·34 |
| Clinical malaria | 185 | 0·6 | 174 | 0·6 | 418 | 0·7 | 409 | 0·7 | 0·94 | 0·74, 1·20 | 1·12 | 0·92, 1·37 | 1·08 | 0·89, 1·33 |
| Confirmed malaria§ | 385 | 1·3 | 418 | 1·4 | 834 | 1·4 | 941 | 1·6 | 1·10 | 0·88, 1·37 | 1·08 | 0·89, 1·31 | 1·21 | 1·00, 1·46* |
| Total malaria | 570 | 1·9 | 592 | 2·0 | 1252 | 2·1 | 1350 | 2·2 | 1·04 | 0·87, 1·25 | 1·09 | 0·93, 1·28 | 1·16 | 1·00, 1·36* |
| Other diseases|| | 274 | 0·9 | 244 | 0·8 | 581 | 1·0 | 627 | 1·0 | 0·89 | 0·71, 1·12 | 1·05 | 0·87, 1·27 | 1·13 | 0·93, 1·36 |
LNS, lipid-based nutrient supplement; IRR, incidence rate ratio; ARI, acute respiratory infection.
Statistically significant results.
Incidence=number of cases/child per year of follow-up.
Groups were compared using negative binomial regression.
Measured by rapid diagnostic test (RDT) for malaria parasites based on histidine-rich protein (HRP-II).
Other diseases=sepsis, measles, anaemia, etc.
The mean longitudinal prevalence of all guardian-reported illness symptoms was 29·1 (sd 19·6) %. Compared with the control group, the 95 % CI for the geometric means ratio of the longitudinal prevalence of all symptoms was entirely below 1·20 (suggestive of non-inferiority) in the 10 g LNS/d and 40 g LNS/d groups and ranged from 0·97 to 1·22 (inconclusive) in the 20 g LNS/d group (Table 5). For most of the individual symptoms, comparisons of the longitudinal prevalences between the LNS groups and the control group were inconclusive (Table 5).
Table 5.
Longitudinal prevalence† of guardian-reported common childhood morbidity symptoms among rural Malawian infants and young children, iLiNS-DOSE study, November 2009–May 2012
| Results by study group | Comparison between the groups‡ | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Control (n 314)§ | 10 g LNS/d (n 315)§ | 20 g LNS/d (n 636)§ | 40 g LNS/d (n 633)§ | 10 g LNS/d v. control | 20 g LNS/d v. control | 40 g LNS/d v. control | ||||||||
| Variable | Geometric mean (%) | sd | Geometric mean (%) | sd | Geometric mean (%) | sd | Geometric mean (%) | sd | GMR | 95 % CI | GMR | 95 % CI | GMR | 95 % CI |
| All symptoms | 21·9 | 2·3 | 22·6 | 2·3 | 23·8 | 2·4 | 22·3 | 2·4 | 1·03 | 0·90, 1·18 | 1·09 | 0·97, 1·22 | 1·02 | 0·91, 1·14 |
| Fever | 6·7 | 2·5 | 6·1 | 2·7 | 6·8 | 2·5 | 6·3 | 2·8 | 0·90 | 0·77, 1·06 | 1·00 | 0·88, 1·15 | 0·93 | 0·81, 1·07 |
| Cough | 9·2 | 2·7 | 9·4 | 2·7 | 10·0 | 2·6 | 9·3 | 2·7 | 1·02 | 0·86, 1·20 | 1·09 | 0·95, 1·25 | 1·01 | 0·88, 1·16 |
| Diarrhoea | 2·8 | 3·0 | 3·1 | 3·4 | 3·1 | 3·1 | 2·7 | 3·2 | 1·13 | 0·92, 1·39 | 1·09 | 0·92, 1·30 | 0·96 | 0·81, 1·14 |
| Nasal discharge | 10·4 | 2·9 | 11·4 | 2·7 | 11·8 | 2·7 | 11·3 | 2·7 | 1·09 | 0·92, 1·30 | 1·14 | 0·98, 1·32 | 1·09 | 0·94, 1·26 |
| Difficult breathing | 2·3 | 3·5 | 2·5 | 3·3 | 2·3 | 3·5 | 2·1 | 3·3 | 1·12 | 0·87, 1·45 | 1·00 | 0·80, 1·27 | 0·94 | 0·75, 1·18 |
| Vomiting | 2·5 | 2·8 | 2·2 | 3·3 | 2·6 | 2·9 | 2·6 | 2·9 | 0·88 | 0·72, 1·07 | 1·04 | 0·89, 1·23 | 1·06 | 0·90, 1·24 |
LNS, lipid-based nutrient supplement; GMR, geometric means ratio.
Longitudinal prevalence = number of days with symptom/total number of days of follow-up.
Groups were compared using ordinary least squares regression.
Excluded thirty-four participants from analysis due to missing data (six in the control group, six in the 10 g LNS/d group, nine in the 20 g LNS/d group and thirteen in the 40 g LNS/d group).
From the guardians’ symptom recalls, we identified 19 690 separate illness episodes among the study participants. We excluded thirty-four children from this analysis because of missing data. The mean incidence of illness episodes was 15·6 (sd 8·8)/child per follow-up year. Compared with the control group, the 95 % CI for the IRR of all illnesses, ‘undefined fever’ and acute respiratory infection episodes were entirely below 1·20 (suggestive of non-inferiority) in all the intervention groups (Table 6).
Table 6.
Incidence† of guardian-reported disease episodes among rural Malawian infants and young children, iLiNS-DOSE study, November 2009–May 2012
| Results by study group | Comparison between the groups‡ | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Control (follow-up years: 220·0) | 10 g LNS/d (follow-up years: 209·7) | 20 g LNS/d (follow-up years: 433·6) | 40 g LNS/d (follow-up years: 443·1) | 10 g LNS/d v. control | 20 g LNS/d v. control | 40 g LNS/d v. control | ||||||||
| Variable | Total episodes | Incidence | Total episodes | Incidence | Total episodes | Incidence | Total episodes | Incidence | IRR | 95 % CI | IRR | 95 % CI | IRR | 95 % CI |
| All diseases | 3215 | 14·7 | 3187 | 15·1 | 6572 | 15·2 | 6716 | 15·1 | 1·04 | 0·96, 1·11 | 1·03 | 0·97, 1·10 | 1·04 | 0·97, 1·10 |
| Gastroenteritis | 408 | 1·8 | 405 | 1·9 | 837 | 1·9 | 761 | 1·7 | 1·07 | 0·89, 1·30 | 1·05 | 0·89, 1·24 | 0·94 | 0·80, 1·12 |
| ARI | 1866 | 8·5 | 1829 | 8·7 | 3794 | 8·8 | 3876 | 8·7 | 1·02 | 0·92, 1·12 | 1·02 | 0·94, 1·11 | 1·02 | 0·94, 1·11 |
| Undefined fever | 345 | 1·6 | 322 | 1·5 | 657 | 1·5 | 687 | 1·6 | 0·97 | 0·81, 1·16 | 0·96 | 0·83, 1·12 | 0·99 | 0·85, 1·16 |
| Other diseases | 596 | 2·7 | 631 | 3·0 | 1284 | 3·0 | 1392 | 3·1 | 1·13 | 0·97, 1·31 | 1·09 | 0·96, 1·24 | 1·16 | 1·02, 1·32 |
LNS, lipid-based nutrient supplement; IRR, incidence rate ratio; ARI, acute respiratory infection.
Incidence=number of episodes/child per year of follow up.
Groups were compared using negative binomial regression.
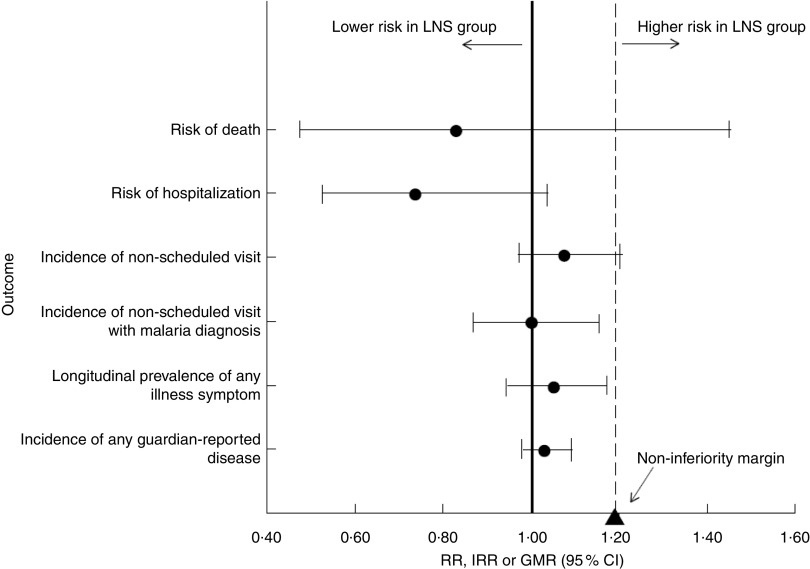
Finally, we combined the intervention groups into one group to compare all participants who received LNS with those who did not. In this comparison, the 95 % CI for all morbidity outcomes were entirely below 1·20 (suggestive of non-inferiority); the 95 % CI for the incidence of non-scheduled visits was just touching the non-inferiority margin of 1·20. The 95 % CI for the risk of death was too wide to draw any conclusions (Fig. 2). Adjusting for baseline anaemia and Fe status did not significantly alter any of the results (data not shown).
Fig. 2.
Plot of selected morbidity outcomes among rural Malawian infants and young children, iLiNS-DOSE study, November 2009–May 2012. All intervention groups receiving lipid-based nutrient supplement (LNS) were pooled together and compared with the control group, with results (●) reported as incidence rate ratios (IRR), relative risks (RR) or geometric means ratios (GMR) with their 95 % CI (represented by horizontal lines). The vertical dashed line represents the margin of non-inferiority. The solid line represents the null effect. None of the point estimates and their 95 % CI fell entirely above the non-inferiority margin (1·20; ▲). We conclude that LNS is does not increase morbidity
Discussion
We tested the hypothesis that long-term supplementation with LNS containing 6 mg Fe would not increase morbidity in children. In a sample of 1932 Malawian infants and young children aged 6–18 months, we found that daily provision of LNS for 1 year was not associated with excess hospitalizations, episodes of common childhood diseases or symptoms when all intervention groups were combined. The incidence of non-scheduled visits was inconclusive. For group comparisons, the 10 and 20 g LNS/d groups had similar outcomes to the control group, except the risk of SAE which was significantly lower in the 20 g LNS/d group. For the 40 g LNS/d group, the comparisons were inconclusive, with increased incidence of non-scheduled visits due to malaria in this LNS group. Our study was not powered to assess mortality outcome.
Our study had several strengths: random allocation of participants; blinding of the investigators involved in data analysis; frequent morbidity data collection; and the year-long follow-up period. Our findings may need to be interpreted with caution since the primary outcome results showed no effect of LNS on growth or stunting( 15 ). However, studies prior to this reported significant length gain and reduction in stunting associated with LNS( 11 , 16 , 17 ). Therefore we believe our results showing that LNS is safe are relevant on a wider scale.
Potential causes of bias were: higher than anticipated attrition (20·4 %); diagnostic malaria tests not done at home visits; and possible differential reporting of illness by guardians who were not blinded. Theoretically, it is also possible that the research assistants may have under-reported morbidity for children in the LNS groups since they were not blinded. However, we had other objective tools for morbidity data collection such as non-scheduled visits reported by clinicians not employed by the study and SAE assessed by the study physician who was blinded to group allocation. All these showed consistent results of no difference in morbidity, except at non-scheduled visits where malaria-related visits were inconclusive in the 40 g LNS/d group. There were no intergroup differences in proportion of children whose data were available and all participants were included in the analysis up to the time of their dropout or death, suggesting that attrition was balanced among the groups. Reimbursement of medical costs could also inflate the non-scheduled visits data. However, Malawi provides a free national health-care system in public health facilities where most of our participants were treated, and we did not reimburse transport for non-scheduled visits. A study in children aged 6–36 months in Chad( 12 ) recorded an incidence of reported disease episodes of 1·17 per child-month (or 14·04 per child-year) which is close to our findings, suggesting that the high disease incidence at home visits was a true observation. Thus, we believe our results are still valid and representative of the target population, suggesting that 10 and 20 g LNS/d did not increase morbidity in our population.
Our findings of no excess morbidity in the 10 and 20 g LNS/d groups are similar to those of a previous study done in Malawi, but in a different area. In that study of 840 children, daily provision of 54 g LNS (containing the same amount of Fe as the LNS used in the present study, 6 mg) did not increase malaria or respiratory morbidity( 13 ). Similar findings have been reported in previous studies that used LNS( 11 , 12 ) or MNP( 3 – 5 ). In our study, although we did not routinely test for malaria during home visits, cases of ‘undefined fever’ could be classified as suspected malaria cases according to the Integrated Management of Childhood Illnesses classification for high-malaria-risk areas( 33 ). In general, Fe-containing home fortificants are assumed to be safer than Fe supplements (such as liquid Fe drops) for children living in areas where infectious diseases are common because home fortificants provide a physiological dose of Fe distributed throughout the day, which potentially avoids the adverse effects associated with Fe given as a bolus dose( 15 ). However, another key mechanism by which Fe may mediate malaria morbidity is by increasing reticulocytosis( 34 ). In unadjusted and preliminary analyses of Hb and Zn protoporphyrin status in this study cohort, LNS provision was associated with improved Fe status and a reduction in the prevalence of Fe deficiency, but no improvement in blood Hb concentration. Thus, the Fe in the LNS improved Fe stores but may not have stimulated reticulocytosis, which might explain the lack of adverse effects on malaria morbidity.
Our findings are different from the reports of the studies in Pakistan( 6 ), Kenya( 7 ), Pemba( 8 ), Zambia( 10 ) and Cote d’Ivoire( 35 ). These studies reported increases in malaria-related hospitalizations and deaths, respiratory infections, diarrhoea and intestinal inflammation associated with Fe supplements or Fe-containing MNP provision in children.
These differences could be due to: (i) the dose of Fe; (ii) prevalence of Fe deficiency in the study population; and (iii) intensive morbidity surveillance.
The dose of Fe used in the above studies was 12·5 mg/d, whereas we used 6 mg/d in our study. We advised that the LNS be eaten on two or more occasions during the day, so as to limit the amount of Fe ingested in a single meal( 22 ). This might have eliminated the detrimental effects of Fe. The high prevalence of Fe deficiency (66 %) in our population may also offer protection to infections aggravated by provision of Fe as suggested by other studies in Africa( 36 , 37 ), although not all( 38 ). In the Ghana and Pemba studies, children with Fe deficiency at baseline were not adversely affected by the intervention( 4 , 8 ). We provided intensive morbidity surveillance and referral for treatment to the national health system which may have improved the overall health of the children, an observation also highlighted in the Ghana and Pemba studies( 4 , 8 ). Thus, it appears that although in some settings provision of Fe may increase the risk of morbidity, this was not the case in our population with a high prevalence of Fe deficiency, using a modest dose of Fe in LNS and providing morbidity surveillance.
The finding that the 40 g LNS/d dose may have been associated with excess malaria-related non-scheduled visits is puzzling, especially given that the 10 and 20 g LNS/d doses were conclusively not associated with increased morbidity. We do not have a clear biological explanation for this because the dose of Fe was intended to be similar in all the LNS groups. Our dietary intake data suggest that children in the 40 g LNS/d group were actually getting less Fe, as the proportion of LNS eaten by children in this group was only about half that of the 10 g LNS/d group( 32 ). In addition, there were no differences in breast milk intake observed between the groups in intention-to-treat analysis( 39 ). Other factors such as modifications of gut microbiota( 7 , 40 ) may be involved in the pathways that link home fortificants and infections, and these require further study.
Conclusion
In conclusion, long-term provision of 10 and 20 g LNS/d containing 6 mg Fe/d did not increase morbidity in infants and young children in a population where Fe deficiency and infectious diseases are both common. Provision of 40 g LNS/d did not affect guardian-reported illness symptoms and episodes but may have increased non-scheduled visits because of malaria. A larger study would be needed to assess the effect of LNS on child mortality.
Acknowledgements
Acknowledgements: The authors thank the study participants, the local communities, the health service staff and their research personnel at the study sites as well as members of the trial’s data safety and monitoring board, the iLiNS extended research team and the iLiNS-Project Steering Committee (http://www.ilins.org) for their contributions in all stages of the study. Financial support: This publication is funded by a grant to the University of California, Davis from the Bill & Melinda Gates Foundation. The findings and conclusions contained within the article are those of the authors and do not necessarily reflect positions or policies of the Bill & Melinda Gates Foundation. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. Conflict of interest: The authors declare no conflict of interest. Authorship: The authors’ responsibilities were as follows: K.M., J.P., K.G.D., S.A.V., Y.B.C., U.A. and P.A. designed the study; J.B., L.A., K.M., J.P., S.A.V., Y.B.C., U.A. and P.A. conducted the study; J.B. analysed data and wrote the paper, with critical input and comments from all other authors; J.B. and P.A. had primary responsibility for final content. All authors read and approved the final manuscript. Ethics of human subject participation: The study was performed according to International Conference of Harmonization–Good Clinical Practice (ICH-GCP) guidelines and the ethical standards of the Helsinki Declaration. The protocol was reviewed and approved by the Institutional Review Boards of the University of Malawi, College of Medicine (IRB reference number P.01/09/722) and the Pirkanmaa Hospital District, Finland (IRB reference number R09130). At least one guardian signed or thumb-printed an informed consent form before enrolment of each participant. The trial was registered at the clinical trials registry (www.clinicaltrials.gov) with the registration ID of NCT00945698. An independent data safety and monitoring board monitored the incidence of suspected SAE during the trial.
References
- 1. World Health Organization (2011) Use of multiple micronutrient powders for home fortification of foods consumed by infants and children 6–23 months of age. http://www.who.int/nutrition/publications/micronutrients/guidelines/guideline_mnp_infants_children/en/ (accessed September 2015). [PubMed]
- 2. De-Regil LM, Suchdev PS, Vist GE et al. (2013) Home fortification of foods with multiple micronutrient powders for health and nutrition in children under two years of age (Review). Evid Based Child Health 8, 112–201. [DOI] [PubMed] [Google Scholar]
- 3. Lemaire M, Islam QS, Shen H et al. (2011) Iron-containing micronutrient powder provided to children with moderate-to-severe malnutrition increases haemoglobin concentrations but not the risk of infectious morbidity: a randomized, double-blind, placebo-controlled, noninferiority safety trial. Am J Clin Nutr 94, 585–593. [DOI] [PubMed] [Google Scholar]
- 4. Zlotkin S, Newton S, Aimone AM et al. (2013) Effect of iron fortification on malaria incidence in infants and young children in Ghana: a randomized trial. JAMA 310, 938–947. [DOI] [PubMed] [Google Scholar]
- 5. Sharieff W, Bhutta Z, Schauer C et al. (2006) Micronutrients (including zinc) reduce diarrhoea in children: the Pakistan Sprinkles Diarrhoea Study. Arch Dis Child 91, 573–579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Soofi S, Cousens S, Iqbal SP et al. (2013) Effect of provision of daily zinc and iron with several micronutrients on growth and morbidity among young children in Pakistan: a cluster-randomized trial. Lancet 382, 29–40. [DOI] [PubMed] [Google Scholar]
- 7. Jaeggi T, Kortman GA, Moretti D et al. (2015) Iron fortification adversely affects the gut microbiome, increases pathogen abundance and induces intestinal inflammation in Kenyan infants. Gut 64, 731–742. [DOI] [PubMed] [Google Scholar]
- 8. Sazawal S, Black RE, Ramsan M et al. (2006) Effects of routine prophylactic supplementation with iron and folic acid on admission to hospital and mortality in preschool children in a high malaria transmission setting: community-based, randomized, placebo-controlled trial. Lancet 367, 133–143. [DOI] [PubMed] [Google Scholar]
- 9. World Health Organization (2007) Conclusions and recommendations of the WHO consultation on prevention and control of iron deficiency in infants and young children in malaria-endemic areas. Food Nutr Bull 28, 4 Suppl., S621–S627. [DOI] [PubMed] [Google Scholar]
- 10. Manno D, Siame J, Larke N et al. (2011) Effect of multiple micronutrient-fortified food on mild morbidity and clinical symptoms in Zambian infants: results from a randomized controlled trial. Eur J Clin Nutr 65, 1163–1166. [DOI] [PubMed] [Google Scholar]
- 11. Adu-Afarwuah S, Lartey A, Brown KH et al. (2007) Randomized comparison of 3 types of micronutrient supplements for home fortification of complementary foods in Ghana: effects on growth and motor development. Am J Clin Nutr 86, 412–420. [DOI] [PubMed] [Google Scholar]
- 12. Huybregts L, Houngbe F, Salpeteur C et al. (2012) The effect of adding ready-to-use supplementary food to a general food distribution on child nutritional status and morbidity: a cluster-randomized controlled trial. PLoS Med 9, e1001313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Mangani C, Ashorn P, Maleta K et al. (2014) Lipid-based nutrient supplements do not affect the risk of malaria or respiratory morbidity in 6- to 18-month-old Malawian children in a randomized controlled trial. J Nutr 144, 1835–1842. [DOI] [PubMed] [Google Scholar]
- 14. Dewey KG, Yang Z & Boy E (2009) Systematic review and meta-analysis of home fortification of complementary foods. Matern Child Nutr 5, 283–321. [Google Scholar]
- 15. Maleta KM, Phuka J, Alho L et al. (2015) Provision of 10–40 g lipid-based nutrient supplements from 6 to 18 months of age does not prevent linear growth faltering in Malawi. J Nutr 145, 1909–1915. [DOI] [PubMed] [Google Scholar]
- 16. Hess SY, Abbeddou S, Jimenez EY et al. (2015) Small-quantity lipid-based nutrient supplements, regardless of their zinc content, increase growth and reduce the prevalence of stunting and wasting in young Burkinabe children: a cluster-randomized trial. PLoS One 10, e0122242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Phuka J, Maleta K, Thakwalakwa C et al. (2008) Complementary feeding with fortified spread and the incidence of severe stunting among 6-to-18 month-old rural Malawians. Arch Pediatr Adolesc Med 162, 619–626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. World Health Organization (2014) African Health Observatory. Malawi. Health Status and Trends: Analytical summary. http://www.aho.afro.who.int/profiles_information/index.php/Malawi:Analytical_summary_-_Health_Status_and_Trends (accessed August 2014).
- 19. National Statistical Office & ICF Macro (2010) Malawi Demographic and Health Survey. Zomba, Malawi and Calverton, MD: NSO and ICF Macro. [Google Scholar]
- 20. Joint United Nations Programme on HIV/AIDS (2014) Malawi: HIV and AIDS estimates. http://www.unaids.org/en/regionscountries/countries/malawi (accessed May 2015). [Google Scholar]
- 21. World Health Organization/Food and Agriculture Organization of the United Nations (2004) Vitamin and Mineral Requirements in Human Nutrition, 2nd ed. Geneva: WHO. [Google Scholar]
- 22. Arimond M, Zeilani M, Jungjohann S et al. (2015) Considerations in developing lipid-based nutrient supplements for prevention of undernutrition: experience from the International Lipid-Based Nutrient Supplements (iLiNS) Project. Matern Child Nutr 11, 31–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Arnold BF, Galiani S, Ram PK et al. (2013) Optimal recall period for caregiver-reported illness in risk factor and intervention studies: a multicountry study. Am J Epidemiol 177, 361–370. [DOI] [PubMed] [Google Scholar]
- 24. Nykanen M, Tamaona W, Cullinan T et al. (1995) Verbal autopsy as a technique to establish causes of infant and child mortality. East Afr Med J 72, 731–734. [PubMed] [Google Scholar]
- 25. iLiNS Project (2015) iLiNS-Dose Statistical Analysis Plan, version 09.0 with appendices 1–9, 2015-02-11. http://www.ilins.org/ilins-project-research/data-analysis/dap (accessed June 2015).
- 26. US Food and Drug Administration (2014) Reporting Serious Problems to FDA. What is a Serious Adverse Event? http://www.fda.gov/safety/medwatch/howtoreport/ucm053087.htm (accessed August 2014).
- 27. Domellof M, Dewey KG, Lonnerdal B et al. (2002) The diagnostic criteria for iron deficiency in infants should be reevaluated. J Nutr 132, 3680–3686. [DOI] [PubMed] [Google Scholar]
- 28. Hastka J, Lasserre JJ, Schwarzbeck A et al. (1992) Washing erythrocytes to remove interferents in measurements of zinc protoporphyrin by front-face hematofluorometry. Clin Chem 38, 2184–2189. [PubMed] [Google Scholar]
- 29. Zimmermann MB, Molinari L, Staubli-Asobayire F et al. (2005) Serum transferrin receptor and zinc protoporphyrin as indicators of iron status in African children. Am J Clin Nutr 81, 615–623. [DOI] [PubMed] [Google Scholar]
- 30. Levine M & Ensom MH (2001) Post hoc power analysis: an idea whose time has passed? Pharmacotherapy 21, 405–409. [DOI] [PubMed] [Google Scholar]
- 31. Feinstein AR & Concato J (1998) The quest for ‘power’: contradictory hypotheses and inflated sample sizes. J Clin Epidemiol 51, 537–545. [DOI] [PubMed] [Google Scholar]
- 32. Hemsworth J, Kumwenda C, Rehman AM et al. (2013) The impact of various doses of lipid based nutrient supplement (LNS) on energy intake of 9 month old Malawian infants. Ann Nutr Metab 63, Suppl. 1, 827. [Google Scholar]
- 33. World Health Organization (2014) Integrated Management of Childhood Illness. Chart Booklet. Geneva: WHO; available at http://www.who.int/maternal_child_adolescent/documents/IMCI_chartbooklet/en/ [Google Scholar]
- 34. Clark MA, Goheen MM, Fulford A et al. (2014) Host iron status and iron supplementation mediate susceptibility to erythrocytic stage Plasmodium falciparum . Nat Commun 5, 4446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Zimmermann MB, Chassard C, Rohner F et al. (2010) The effects of iron fortification on the gut microbiota in African children: a randomized controlled trial in Cote d’Ivoire. Am J Clin Nutr 92, 1406–1415. [DOI] [PubMed] [Google Scholar]
- 36. Jonker FA, Calis JC, van Hensbroek MB et al. (2012) Iron status predicts malaria risk in Malawian preschool children. PLoS One 7, e42670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Nyakeriga AM, Troye-Blomberg M, Dorfman JR et al. (2004) Iron deficiency and malaria among children living on the coast of Kenya. J Infect Dis 190, 439–447. [DOI] [PubMed] [Google Scholar]
- 38. Veenemans J, Milligan P, Prentice AM et al. (2011) Effect of supplementation with zinc and other micronutrients on malaria in Tanzanian children: a randomized trial. PLoS Med 8, e1001125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Kumwenda C, Dewey KG, Hemsworth J et al. (2014) Lipid-based nutrient supplements do not decrease breast milk intake of Malawian infants. Am J Clin Nutr 99, 617–623. [DOI] [PubMed] [Google Scholar]
- 40. Gordon JI, Dewey KG, Mills DA et al. (2012) The human gut microbiota and undernutrition. Sci Transl Med 4, 137. [DOI] [PubMed] [Google Scholar]