Abstract
Objective
To document the scale-up of India's Adolescent Girls’ Anaemia Control Programme following a knowledge-centred framework for scaling up nutrition interventions and to identify the critical elements of and lessons learned from a decade of programme experience for the control of anaemia in adolescent girls.
Design
We reviewed all articles, programme and project reports, and baseline and endline assessments published between 1995 and 2012 regarding the control of anaemia through intermittent iron and folic acid supplementation; key programme specialists and managers were interviewed to complete or verify information wherever needed.
Setting
India.
Subjects
Adolescent girls.
Results
The scale-up of India's Adolescent Girls’ Anaemia Control Programme followed a knowledge-centred programme cycle comprising five phases: Evidence, Innovation, Evaluation, Replication and Universalization. By the end of 2011, the programme was being rolled out in thirteen states and was reaching 27·6 million adolescent girls of whom 16·3 million were school-going girls and 11·3 million were out-of-school girls. Building on the critical elements of and lessons learned from the programme, the Government of India launched in 2012 the national Weekly Iron and Folic Acid Supplementation (WIFS) programme to universalize the benefits of anaemia control to the overall population of Indian adolescents.
Conclusions
The Adolescent Girls’ Anaemia Control Programme in India provides a good example of how a knowledge-centred approach can successfully guide the scaling up of public health nutrition interventions and facilitate intersectoral convergence among different government departments and development partners to break the inter-generational cycle of undernutrition and deprivation.
Keywords: India, Adolescent girls, Anaemia, Supplementation, Knowledge
The world is home to 1·2 billion adolescents aged 10–19 years; 240 million (20 %) of the world's adolescents live in India and 115 million (48 %) of Indian adolescents are girls( 1 ). There is global consensus that investing in adolescents, particularly girls, can accelerate the fight against deprivation, inequity and gender discrimination( 2 ). Anaemia is a widespread deprivation among Indian adolescent girls: the latest data available indicate that 56 % of Indian girls aged 15–19 years are anaemic and this figure rises to 69 % among adolescent girls from scheduled tribes( 3 ).
Anaemia during adolescence reduces girls’ learning capacity and physical performance as well as their work capacity and ability to earn income later in life. When anaemic adolescent girls become pregnant – hopefully once they have completed their growth and become adult women – they are exposed to additional risks as anaemia during pregnancy is associated with increased risk of maternal mortality, premature delivery, low birth weight and perinatal mortality; moreover, infants born to anaemic mothers also have a higher risk of anaemia in the first 6 months of life( 4 ).
The consequences of anaemia outlined above are compelling reasons for supporting programmes designed to reduce the prevalence and severity of anaemia. Recent global consensus agrees that in developing countries the provision of weekly Fe + folic acid supplements for the control of anaemia in women should be viewed as one of the most important nutrition interventions and that ‘the critical elements of these programmes must be identified to ensure their successful implementation, improve the iron status of women and reduce the prevalence of anaemia’( 5 ).
The objectives of the current paper were twofold: (i) to document the scale-up of India's Adolescent Girls’ Anaemia Control Programme following a knowledge-centred framework for scaling up nutrition interventions; and (ii) to identify the critical elements of and lessons learned from a decade of intersectoral programme experience among government departments and partners for the control of anaemia in adolescent girls.
Methods
Three sources of information were reviewed comprehensively: (i) all peer-reviewed articles published between 1995 and 2012 regarding the control of anaemia in adolescent girls in India through intermittent Fe + folic acid supplementation – articles were identified through an online search within PubMed (National Academy of Medicine and National Institutes of Health) using as keywords (India)*(anaemia)*(supplementation)*(adolescent girls); (ii) all peer-reviewed articles and publications published on the subject between 1995 and 2012 and referenced in the peer-reviewed articles identified through the PubMed search referred to above; and (iii) all programme and project reports and baseline and endline assessments published between 1995 and 2012 regarding the control of anaemia in adolescent girls in India through intermittent Fe + folic acid supplementation, including interviews with key programme specialists and managers to complete or verify information included in the reports wherever needed.
Findings
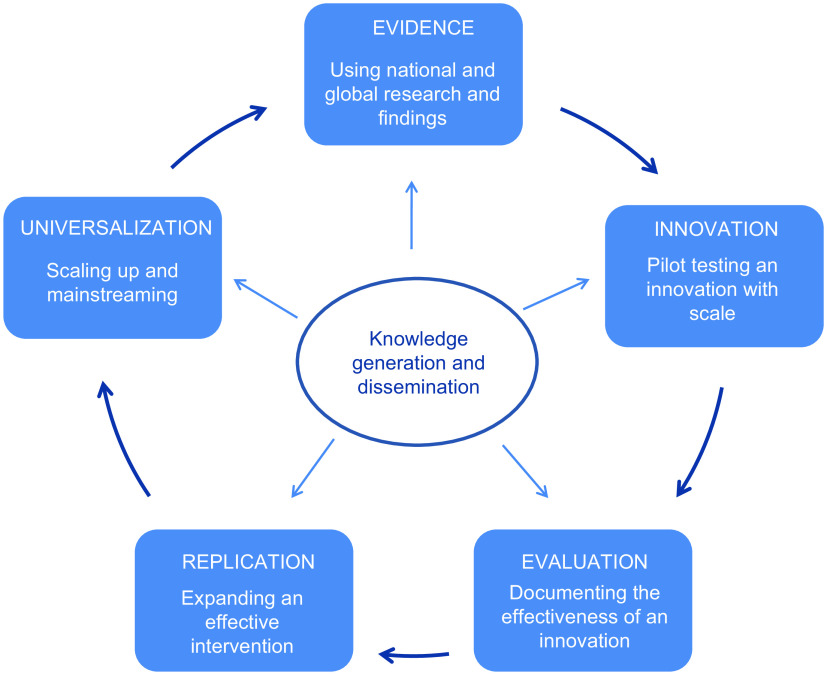
The scale-up of India's Adolescent Girls’ Anaemia Control Programme followed a knowledge-centred programme cycle comprising five chronological phases: Evidence, Innovation, Evaluation, Replication and Universalization (Fig. 1).
Fig. 1.
(colour online) Knowledge-centred programme cycle: from innovation to universalization. Adolescent Girls’ Anaemia Control Programme, India
Evidence phase: using global and national research and findings to design an innovative intervention (1995–2000)
In 1998, India's second National Family Health Survey (NFHS-II) indicated that 56 % of girls aged 15–19 years were anaemic and 20 % of them had moderate-to-severe anaemia( 6 ).
Concurrently, two research trials were being conducted with UNICEF support to assess the effectiveness of weekly Fe + folic acid supplementation in correcting anaemia among Indian adolescent girls in view of global research seeming to indicate that weekly Fe + folic acid supplementation could be a practical, safe and effective strategy for improving nutrition in adolescent girls( 7 ).
A study was carried out in 1996–1999 in north-east Delhi to assess the effectiveness of weekly and daily Fe + folic acid supplementation in correcting anaemia in school-going adolescent girls aged 10–17 years (n 2210) who received supplements over a period of 230 d. The study concluded that weekly administration of Fe + folic acid supplements was a practical and effective strategy to prevent anaemia in school-going adolescent girls( 8 ).
A second study was carried out in 1996–1997 in the urban slums of Mumbai to assess the effectiveness of weekly and daily Fe + folic acid supplementation in correcting anaemia in anaemic school-going adolescent girls aged 10–18 years (n 1748) who received Fe + folic acid supplements over a 25-week period. The study concluded that weekly Fe + folic acid supplementation had a positive impact on reducing the prevalence of anaemia and that this impact was similar to that of daily supplementation( 9 ).
These research findings confirming that weekly Fe + folic acid supplementation was effective in reducing the prevalence of anaemia in adolescent girls added to the emerging global evidence from Africa, Asia and Latin America indicating that the differences in final Hb concentration among daily and weekly treatment groups were small and that under supervised conditions weekly Fe + folic acid supplementation could have a positive impact on the prevalence of anaemia in adolescent girls and be more effective than daily supplementation( 10 ).
In view of the high prevalence of anaemia among adolescent girls and the findings and recommendations emerging from global and national research, the Government of India and State Governments decided to assess the cost and effectiveness of an innovative programme aimed at reducing the prevalence and severity of anaemia in adolescent girls.
It was decided that, in its Innovation phase, the programme would include at least two of the following interventions: (i) weekly Fe + folic acid supplementation comprising 100 mg of elemental Fe and 500 μg of folic acid for the control of Fe deficiency and anaemia; (ii) bi-annual deworming prophylaxis (400 μg of albendazole), 6 months apart, for the control of helminth infestations; and/or (iii) information, counselling and support to adolescent girls on how to improve their diets, prevent anaemia, and minimize the potential undesirable side-effects of Fe + folic acid supplementation and deworming. The pilot programmes would be implemented with technical support by UNICEF using schools as the delivery channel for school-going adolescent girls and anganwadi centres (the village centres of India's Integrated Child Development Services (ICDS) programme) as the delivery platform for out-of-school adolescent girls.
Innovation phase: pilot testing an innovative intervention through existing delivery systems (2000–2005)
The Innovation phase of the programme was launched in 2000–2001 across twenty districts in five states: Andhra Pradesh, Bihar, Gujarat, Rajasthan and Tamil Nadu; in 2001–2002, six additional states – Jharkhand, Madhya Pradesh, Maharashtra, Odisha, Uttar Pradesh and West Bengal – launched the Innovation phase of the programme in twelve districts; finally, between 2002 and 2005, the Innovation phase of the programme took off in twenty districts across the states of Chhattisgarh and Karnataka. The Innovation phase of the programme comprised both school-going and out-of-school adolescent girls in all states except in Andhra Pradesh and Karnataka, where only school-going girls were included.
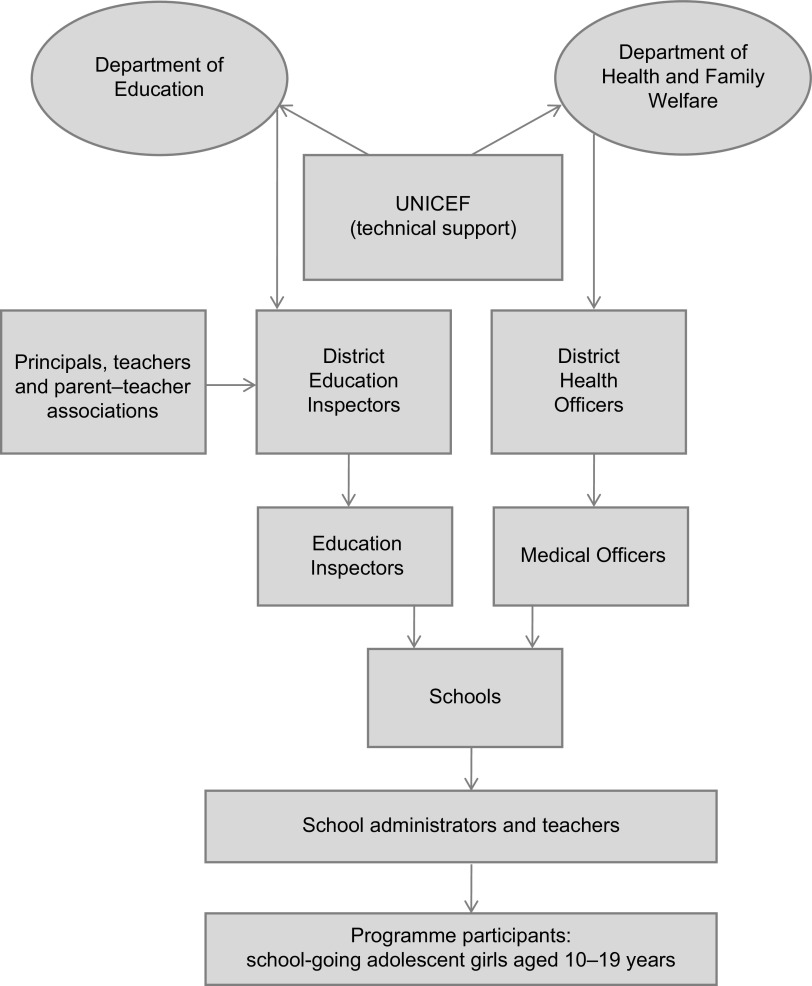
By the end of 2005, the Innovation phase of the programme had been pilot tested in fifty-two districts across thirteen states. Three state departments – Health and Family Welfare, Education, and Women and Child Development – played the lead role in implementing this phase of the programme. The Department of Health and Family Welfare ensured the provision of supplies, specifically of Fe + folic acid supplements and deworming tablets. The Department of Education was the nodal department for implementation of the programme among school-going girls; principals, teachers and parent–teacher associations were involved in the implementation of the programme in the schools, while the District Education Inspectors were responsible for monitoring the effective implementation of the programme and problem-solving in response to constraints in programme delivery. The Department of Women and Child Development was the nodal department for implementation of the programme among out-of-school girls through a community-based girl-to-girl approach that comprised supervised Fe + folic acid supplementation at the anganwadi centres; in each village, the core team responsible for the implementation of the programme comprised the community-based ICDS anganwadi worker and her ICDS Lady Supervisor and Child Development Programme Officer, while the ICDS District Project Officers played a role vis-à-vis anganwadi centres similar to that played by the District Education Inspectors vis-à-vis schools. UNICEF support during the Innovation phase focused on technical support in three main areas: (i) design, planning, implementation, monitoring and documentation of the Innovation phase; (ii) capacity building of teachers, health staff, community workers and supervisors to deliver, supervise and monitor the programme, and counsel adolescent girls and their families; and (iii) design and implementation of programme communication strategies through folk media, mass media, wall writings, posters and booklets and girl-to-girl, girl-to-parent and teacher-to-parent approaches; additionally, UNICEF filled supply gaps to ensure an uninterrupted delivery of Fe + folic acid supplements, deworming tablets, and information, education and communication (IEC) materials. By the end of 2004, some 8·8 million adolescent girls had been reached by the Innovation phase of the programme.
Evaluation phase: documenting the effectiveness of an innovative intervention (2000–2005)
The evaluation of the Innovation phase of the programme aimed to document the cost and effectiveness of the new intervention in reducing the prevalence and severity of anaemia in adolescent girls and to identify the success factors that were critical in scaling up the programme.
Evaluation studies were carried out in six states: Andhra Pradesh, Gujarat, Jharkhand, Madhya Pradesh, Maharashtra and Uttar Pradesh( 11 – 20 ). The evaluation indicated that girls’ adherence to the programme was high; all programme sites reported adherence rates ranging from 88 % to 99 % except in Andhra Pradesh where adherence was 53 % due to intermittent supply stock-outs. When girls’ adherence was low, the main reported reason for it was ‘forgetfulness’ rather than undesirable side-effects.
The proportion of girls who reported undesirable side-effects such as black stools, nausea, giddiness, heartburn and vomiting ranged from 3 % in Andhra Pradesh to 30 % in Jharkhand. The incidence of undesirable effects declined as the implementation of the programme matured; for example, in Gujarat, 30 % of girls reported undesirable effects in the initial stages of the programme while only 14 % did at programme end. However, none of the undesirable effects was serious enough to compel the girls to discontinue taking the supplements.
The proportion of girls who reported beneficial effects from the programme ranged from 31 % in Madhya Pradesh to 100 % in Jharkhand. The benefits most frequently reported by the girls included: ‘feeling healthier’, ‘feeling better’, ‘having more energy’, ‘not feeling sleepy’, ‘feeling less fatigued’, ‘not experiencing breathing problems’, ‘having better physical capacity’, ‘experiencing increased alertness’, ‘having better concentration in school’, ‘having regular menstrual cycles’, ‘experiencing less abdominal pain during menstruation’ and ‘having brighter skin’. These and other perceived benefits have been reported in other Fe + folic acid supplementation programmes for adolescent girls in India, including improved appetite and food intake( 21 , 22 ).
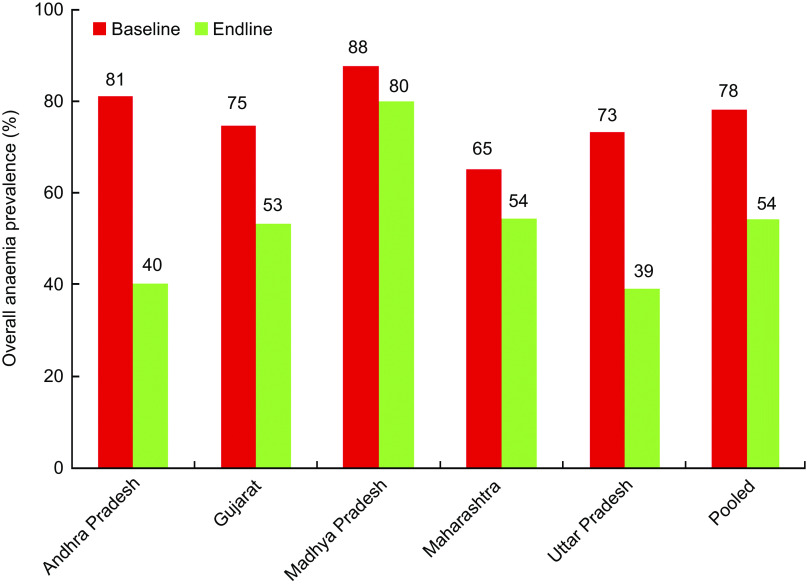
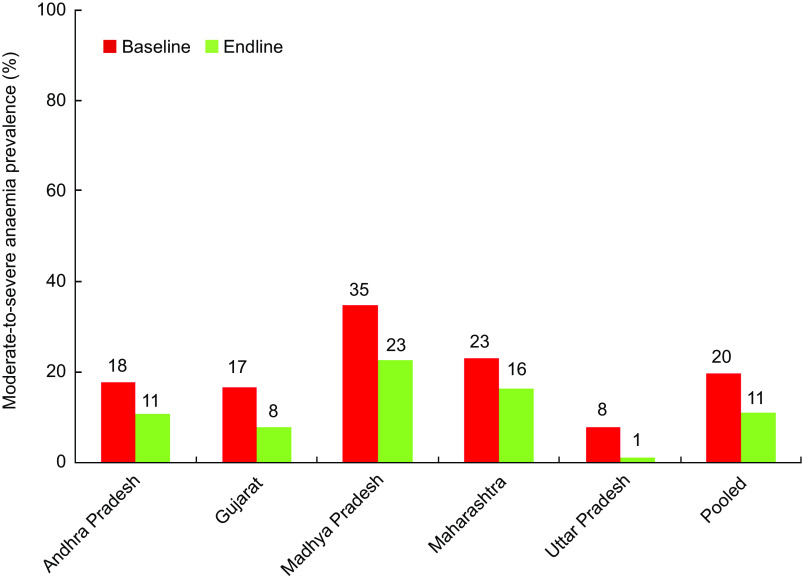
The reported prevalence of anaemia at baseline was high in all programme sites, ranging from 65 % in Maharashtra to 88 % in Madhya Pradesh; no baseline data were available for Jharkhand. The evaluation studies reported a statistically significant (P < 0·001) reduction in the prevalence of anaemia from baseline to endline in intervention groups. Such reduction in the prevalence of anaemia – observed both in school-going and out-of-school girls – ranged from 8 percentage points in Madhya Pradesh (potentially due to the significantly higher prevalence of moderate-to-severe anaemia in this state) to 41 percentage points in Andhra Pradesh, with an average 24 percentage point reduction (30·6 % decrease) after 1 year of programme implementation (Fig. 2). Andhra Pradesh reported a decrease in the prevalence of anaemia of 70 percentage points after 2 years of programme implementation. All programmes reported a significant decrease in the prevalence of moderate-to-severe anaemia (Hb concentration below 99 g/l); this decrease ranged from 6·7 percentage points in Maharashtra to 12·1 percentage points in Madhya Pradesh, with an average 8·4 percentage point reduction (43·1 % decrease) after 1 year of programme implementation (Fig. 3).
Fig. 2.
(colour online) Reduction in the prevalence of overall anaemia (Hb < 120 g/l) in adolescent girls after 1 year of programme implementation. Innovation phase (2000–2005), Adolescent Girls’ Anaemia Control Programme, India
Fig. 3.
(colour online) Reduction in the prevalence of moderate-to-severe anaemia (Hb < 100 g/l) in adolescent girls after 1 year of programme implementation. Innovation phase (2000–2005), Adolescent Girls’ Anaemia Control Programme, India
The evaluations indicated that the additional cost of the programme ranged from $US 0·13 to $US 0·88 per adolescent girl per annum. This variation was largely due to differences in programme components. The average cost per girl per annum was as low as $US 0·13 when the programme included only the procurement and distribution of Fe + folic acid supplements. With the addition of other programme components such as planning, monitoring, training, life-skills education, counselling, supervision, communication and/or additional supplies the programme costs increased, ranging in most programmes from $US 0·30 to $US 0·90 per adolescent girl per annum( 23 ). Once the initial training and monitoring capacity of the programme were in place the additional average cost of the programme was estimated at $US 0·58 per girl per annum( 24 ).
The critical success factor common to all programme sites was girls’ high adherence to the programme, attributable to: (i) the regular supervision of girls’ supplement intake; (ii) the counselling and support given to girls by the health, education and ICDS workers to encourage girls to adhere to the weekly supplementation and bi-annual deworming regime and provide them with timely information and support on how to improve their diets and prevent anaemia; and (iii) the monitoring of programme implementation by programme managers, including effective management of supplies (no stock-outs). Most evaluations reported that the IEC component was at times weak; for example, in Gujarat the evaluation of the communication strategy indicated that the printed materials were read by 87 % of the girls but 56 % of them were not able to recall three of the messages included in the communication materials. Therefore more innovative and effective communication approaches were required( 5 ).
Replication phase: expanding an effective intervention through existing delivery systems (2006–2010)
The encouraging results of the Evaluation phase provided State Governments with a solid evidence base for scaling up what would become India's Adolescent Girls’ Anaemia Control Programme.
The planning, implementation and financing of the Replication phase in the states was carried out in a convergent manner among the departments of Health, Education, and Women and Child Development. As was the case in the Innovation phase, the Department of Education and the Department of Women and Child Development ensured the implementation of the Replication phase of the programme for school-going and out-of-school girls, respectively (Figs 4 and 5); however, in the Replication phase, the Department of Health and Family Welfare strengthened its support to the programme by monitoring the scale-up process in coordination with the two main implementing departments while continuing to ensure the procurement and distribution of supplies through the National Rural Health Mission (NRHM). UNICEF support was limited to the provision of technical support for the finalization of the States’ project implementation plans, comprising state-owned strategies and budgets for scaling up the programme with quality and increasing equity.
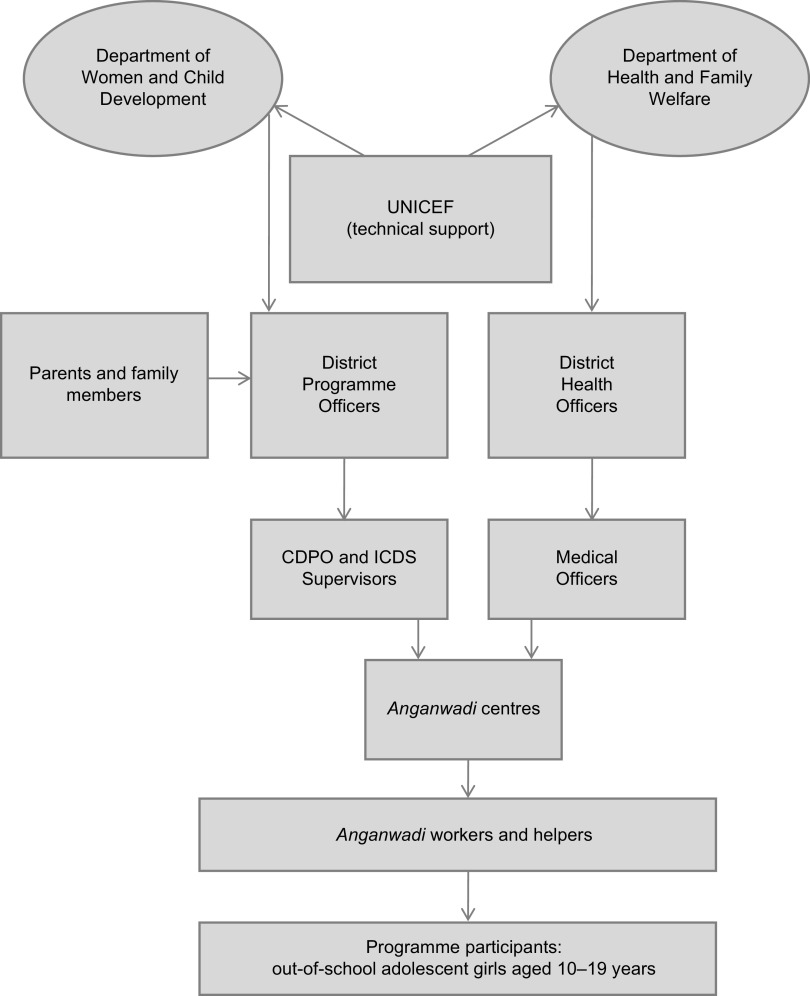
Fig. 4.
Replication phase (2006–2010): key programme implementers of the school-based component of the Adolescent Girls’ Anaemia Control Programme, India
Fig. 5.
Replication phase (2006–2010): key programme implementers of the community-based component of the Adolescent Girls’ Anaemia Control Programme, India (CDPO, Child Development Programme Officers; ICDS, Integrated Child Development Services)
The Replication phase of the programme paid particular attention to the design of IEC strategies to reach adolescent girls, their parents and their communities at large. Some of the strategies that were used to scale up adherence to the programme were: (i) ensure the supervision and recording of weekly Fe + folic acid supplementation in school registers, anganwadi centre registers and girls’ self-reporting cards, as well as the designation of a nodal person at every level, to track and report regularly on girls’ adherence to the programme and the status of supply stocks; (ii) enhance overall awareness about the causes and consequences of anaemia and the benefits of the programme through mass media – particularly radio and television – while dispelling potential misconceptions associated with weekly supplementation; (iii) use community platforms such as the Mother and Child Health and Nutrition Days and the Village Health and Nutrition Days and involve community leaders, community members and community volunteers in IEC and social mobilization in favour of the programme; and (iv) build the capacity of anganwadi workers, female school teachers, parents, community groups and school-going girls in counselling, peer support and programme monitoring.
Between 2006 and 2010, the Adolescent Girls’ Anaemia Control Programme increased its reach and coverage significantly; by the end of 2010, the programme was being implemented state-wide in eleven states with State Government funds. The coverage of the programme doubled as the number of adolescent girls benefiting from the programme increased from 8·8 million by the end of 2005 to 14·5 million by the end of 2010; about 70 % of the girls enrolled in the programme by the end of 2010 were school-going girls while 30 % were out-of-school girls (Table 1).
Table 1.
Replication phase (2006–2010): programme coverage by 31 December 2010, Adolescent Girls’ Anaemia Control Programme, India
| Number of adolescent girls benefiting from the Adolescent Girls’ Anaemia Control Programme | |||
|---|---|---|---|
| State | School-going girls | Out-of-school girls | Total |
| Assam | 162 261 | 0 | 162 261 |
| Bihar | 529 249 | 104 130 | 633 379 |
| Chhattisgarh | 304 005 | 48 900 | 352 905 |
| Jharkhand | 1 946 729 | 150 000 | 2 096 729 |
| Gujarat | 1 118 042 | 506 777 | 1 624 819 |
| Madhya Pradesh | 0 | 104 000 | 104 000 |
| Maharashtra | 1 968 000 | 1 941 885 | 3 909 885 |
| Odisha | 22 013 | 431 441 | 453 454 |
| Rajasthan | 565 514 | 599 083 | 1 164 597 |
| Uttar Pradesh | 1 200 000 | 0 | 1 200 000 |
| West Bengal | 2 271 120 | 564 660 | 2 835 780 |
| Total | 10 086 933 | 4 450 876 | 14 537 809 |
Universalization phase: scaling up and mainstreaming an effective intervention (2011+)
The Innovation and Replication phases of the Adolescent Girls’ Anaemia Control Programme demonstrated that the programme was effective in reducing the prevalence and severity of anaemia among adolescent girls and that it was possible to scale up its reach and coverage with State Government funds using existing delivery platforms. Importantly, the Adolescent Girls’ Anaemia Control Programme contributed to put adolescent girls at the centre of policy formulation and programme design in India.
In 2011, the Government of India lunched the Rajiv Gandhi Scheme for the Empowerment of Adolescent Girls or SABLA (‘enable’ in Hindi) led by the Ministry of Women and Child Development. This flagship programme – implemented in about one-third of India's districts – aims at empowering nearly 20 million out-of-school adolescent girls (11–18 years) by improving their life skills and nutrition and health status. All adolescent girls participating in the programme benefit from an integrated package of services including weekly Fe + folic acid supplementation, bi-annual deworming prophylaxis, nutrition education, a hot cooked meal or a take-home ration, and education and counselling on reproductive and sexual health.
By the end of 2011, the Adolescent Girls’ Anaemia Control Programme was being rolled out state-wide in thirteen states – Assam, Bihar, Chhattisgarh, Jharkhand, Gujarat, Kerala, Madhya Pradesh, Maharashtra, Odisha, Rajasthan, Tamil Nadu, Uttar Pradesh and West Bengal – using schools, anganwadi centres and SABLA as the delivery platforms. The programme was reaching 27·6 million adolescent girls, of whom 16·3 million were school-going girls and 11·3 million were out-of-school girls. This represented almost a doubling (1·9 fold increase) in the number of girls reached by the programme (from 14·5 million to 27·6 million); the number of school-going girls reached increased from 10·1 million to 16·3 million (1·6 fold increase) while the number of out-of-school girls reached increased from 4·4 to 11·3 million (2·6 fold increase) mostly as a result of mainstreaming anaemia control into SABLA, a multi-purpose programme for adolescent girls (Table 2).
Table 2.
Universalization phase (2011+), programme coverage by 31 December 2011, Adolescent Girls’ Anaemia Control Programme, India
| Number of adolescent girls benefiting from the Adolescent Girls’ Anaemia Control Programme | |||
|---|---|---|---|
| State | School-going girls | Out-of-school girls | Total |
| Assam | 247 817 | 632 369 | 880 186 |
| Bihar | 529 249 | 104 130 | 633 379 |
| Chhattisgarh | 552 432 | 125 317 | 677 749 |
| Jharkhand | 1 172 209 | 1 959 584 | 3 131 793 |
| Gujarat | 1 120 789 | 506 777 | 1 627 566 |
| Kerala | 547 898 | 0 | 547 898 |
| Madhya Pradesh | 336 081 | 1 205 626 | 1 541 707 |
| Maharashtra | 1 968 000 | 1 881 820 | 3 849 820 |
| Odisha | 22 013 | 2 199 159 | 2 221 172 |
| Rajasthan | 410 682 | 609 916 | 1 020 598 |
| Tamil Nadu | 2 747 029 | 1 162 464 | 3 909 493 |
| Uttar Pradesh | 1 200 000 | 0 | 1 200 000 |
| West Bengal | 5 424 577 | 914 720 | 6 339 297 |
| Total | 16 278 776 | 11 301 882 | 27 580 658 |
Building on the critical elements of and lessons learned from the Adolescent Girls’ Anaemia Control Programme, the Government of India launched the National Weekly Iron and Folic Acid Supplementation (WIFS) programme in 2012. The objective of the WIFS programme is to universalize the coverage of the Adolescent Girls’ Anaemia Control Programme and expand its benefits to all adolescent girls in India.
Critical elements of and lessons from a decade of programme experience (2000–2012)
The critical elements of and lessons learned from a decade of intersectoral programme experience among government departments and partners for the control of anaemia in adolescent girls can be summarized as follows.
-
1.
The use of global and national evidence as the foundation for advocacy was key to garner political support to pilot test the programme (Innovation phase); the availability and use of data on the effectiveness and cost of the intervention (Evaluation phase) were crucial to garner commitment for the Replication phase of the programme; the evidence on the effectiveness of the programme in reducing the prevalence and severity of anaemia was decisive.
-
2.
The use of existing delivery platforms allowed a large number of adolescent girls to be reached and programme coverage to be expanded rapidly with minimal operating costs, thus increasing the cost-effectiveness of the programme. Existing programme platforms like the school-based education system and the community-based ICDS system provided the initial programme delivery channels; presently, newer opportunities like the SABLA scheme for adolescent girls provide additional mainstreaming opportunities for programme expansion and universalization.
-
3.
The clear definition of roles and responsibilities among the different government sectors both at national and state levels contributed to the successful pilot testing and consolidation of the programme with scale and quality. Each year, state programme implementation plans with appropriate sectoral budget allocations were jointly developed by the departments of Education, Women and Child Development, and Health, contributing to effective programme implementation and monitoring.
-
4.
The involvement of stakeholders at all levels of the programme – including girls, parents, community leaders, teachers, principals, district-level programme managers, state-level policy makers and the media – was essential to ensure programme ownership, uptake, adherence and coverage. Adolescent girls can be very articulate about the benefits of the programme; thus involving girls in ‘girl-to-girl’ information and counselling approaches is effective in reaching out-of-school girls.
-
5.
Timely and quality communication with adolescent girls, their families and communities about the consequences of anaemia, the benefits of the anaemia control programme, and the potential undesirable side-effects of supplementation and deworming and how to mitigate them was essential to ensure girls’ adherence to the programme. Communication strategies focusing on the benefits of the programme for adolescents’ health and school performance seemed to be the most effective.
-
6.
Timely availability of supplies, particularly of Fe + folic acid supplements and deworming tablets, communication and counselling materials, and supervision and monitoring tools in the schools and anganwadi centres contributed to ensure girls’ adherence to the programme and overall programme effectiveness. Adherence rates above 85 % are achievable; however, whenever there was a significant drop in programme coverage it was systematically due to supplement stock-outs. Thus a well-planned procurement and distribution system is essential.
-
7.
A fixed-day approach facilitates girls’ compliance and programme management, including community mobilization, supervision of supplement distribution by teachers, frontline workers and community resource persons, and overall monitoring of programme implementation. Sometimes Wednesday was chosen as the fixed day as religious fasting and festivals seemed to be less common on that day and the potential resistance to supplement intake was expected to be minimal.
-
8.
Simple monitoring tools and aids such as individual self-compliance cards, class registers, and school and anganwadi centre registers with information on each girl facilitates adherence to the programme as it diminishes girls’ ‘forgetfulness’ (most frequently reported cause of low adherence by girls), improves programme implementation and monitoring, and allows for timely corrective action.
-
9.
A package of services for the control of anaemia in adolescent girls, including counselling and support, is better delivered as part of an integrated package of interventions for adolescent girls to keep girls’ motivation and interest. However, it is important to prioritize a limited number of evidence-based interventions and design the programme with a focus on scale.
-
10.
The use of unit cost data can inform programme scale-up. Once the initial training and monitoring capacity of the programme is in place, the additional average cost of the programme in most sites ranges between $US 0·32 and $US 0·36 per girl per annum; the average cost of Fe + folic acid supplements per girl per annum represents about one-third (i.e. $US 0·12) of such additional cost.
Conclusions
The Adolescent Girls’ Anaemia Control Programme in India provides a good example of how a knowledge-based approach can successfully guide the scale-up of evidence-based interventions in public health nutrition; it also illustrates how the control of anaemia in adolescent girls created a platform for intersectoral convergence among different government departments and partners to provide services and support to empower adolescent girls, reduce gender and social inequities, and contribute to break the inter-generational cycle of undernutrition and deprivation in India.
Acknowledgements
Sources of funding: This research received no specific grant from any funding agency in the public, commercial or non-for-profit sectors. Conflict of interest declaration: There are no conflicts to declare. The opinions expressed in this paper are those of the authors and do not necessarily represent an official position of the organizations with which they are affiliated. Ethics: Ethical approval was not required. Authorship responsibilities: V.M.A. designed the study, led the analysis and wrote the manuscript; K.P. and G.S. made substantial conceptual contributions and revisions.
References
- 1. Government of India Census Bureau (2001) Population of States and Union Territories (UTs) of India. http://www.censusindia.gov.in/Census_Data_2001/Projected_Population/Projected_Population.pdf (accessed May 2012).
- 2. UNICEF (2012) Adolescence: An Age of Opportunity. The State of the World's Children, 2011 . New York: UNICEF. [Google Scholar]
- 3. International Institute for Population Sciences (2006) National Family Health Survey (NFHS-3) 2005–2006 . Mumbai and Calverton, MD: International Institute for Population Sciences and ORC Macro. [Google Scholar]
- 4. Lynch AR (2000) The potential impact of iron supplementation during adolescence on iron status in pregnancy. J Nutr 130, 2S Suppl., 448S–451S. [DOI] [PubMed] [Google Scholar]
- 5. World Health Organization (2011) Weekly Iron and Folic Acid Supplementation Programmes for Women of Reproductive Age: An Analysis of Best Programme Practices . Geneva: WHO. [Google Scholar]
- 6. International Institute for Population Sciences (2000) National Family Health Survey (NFHS-2) 1998–1999 . Mumbai and Calverton, MD: International Institute for Population Sciences and ORC Macro. [Google Scholar]
- 7. Tee ES, Kandiah M, Awin N et al. (1999) School-administered weekly iron–folate supplements improve hemoglobin and ferritin concentrations in Malaysian adolescent girls. Am J Clin Nutr 69, 1249–1256. [DOI] [PubMed] [Google Scholar]
- 8. Agarwal KN, Gomber S, Bisht H et al. (2003) Anemia prophylaxis in adolescent school girls by weekly or daily iron–folate supplementation. Indian Pediatr 40, 296–301. [PubMed] [Google Scholar]
- 9. Mehta M (1998) Effectiveness of Daily and Weekly Iron and Folic Acid Supplementation in Anemic Adolescent Girls . Bombay: UNICEF-India. [Google Scholar]
- 10. Beaton GH & McCabe G (1999) Efficacy of Intermittent Iron Supplementation in the Control of Iron Deficiency Anemia in Developing Countries: An Analysis of Experience. Final Report to the Micronutrient Initiative . Ottawa: The Micronutrient Initiative. [Google Scholar]
- 11. Indian Institute of Health and Family Welfare (2008) Prevention and control of anemia in rural adolescent girls through the school system in Andhra Pradesh. In Studies on Adolescent Girls: An Analytical Review , pp. 45–48. New Delhi: National Institute of Public Cooperation and Child Development. [Google Scholar]
- 12. Kotecha P, Patel RZ, Karkar PD et al. (2002) Impact Evaluation of the Adolescent Girls’ Anemia Reduction Programme in the District of Vadodra, Gujarat . Baroda, Gujarat: Government of Gujarat and UNICEF. [Google Scholar]
- 13. Kotecha P, Nirupam S & Karkar P (2009) Adolescent girls’ anaemia control programme, Gujarat, India. Indian J Med Res 130, 584–589. [PubMed] [Google Scholar]
- 14. Seshadri S (2003) Iron Supplementation to Control Anemia in Adolescent Girls: Documentation of the Process and Impact in Ranchi District, Jharkhand . Ranchi, Jharkhand: Department of Education, Government of Jharkhand. [Google Scholar]
- 15. Department of Human Resource Development, Directorate of Social Welfare & Department of Health and Family Welfare (2009) Control of Nutritional Anemia in School Going Adolescent Girls: Experiences in Jharkhand . Ranchi, Jharkhand: Government of Jharkhand and UNICEF. [Google Scholar]
- 16. Indian Institute of Health Management and Research (2002) A Baseline Study on Nutritional Anemia Among Non-School Going Adolescent Girls in Shivpuri District, Madhya Pradesh . Bhopal, Madhya Pradesh: Department of Women and Child Development, Government of Madhya Pradesh. [Google Scholar]
- 17. Sharma K (2002) A Study on Assessing the Impact of Adolescent Anemia Control Project Among Out-of-School Adolescent Girls: A Mid-Term Evaluation in Shivpuri District, Madhya Pradesh . Bhopal, Madhya Pradesh: Department of Women and Child Development, Government of Madhya Pradesh. [Google Scholar]
- 18. Deshmukh PR, Garg BS & Bharambe MS (2008) Effectiveness of weekly supplementation of iron to control anemia among adolescent girls in Nashik, Maharashtra, India. J Health Popul Nutr 26, 74–78. [PMC free article] [PubMed] [Google Scholar]
- 19. Mahatma Gandhi Institute of Medical Sciences (2003) Weekly Iron with Folic Acid Supplementation with Bi-annual Deworming Reduces Significantly the Prevalence of Anemia in Otherwise Unreached Adolescent Girls in Maharashtra, India . Sewagram, Maharashtra: Department of Community Medicine. [Google Scholar]
- 20. Vir SC, Singh N, Nigam AK et al. (2008) Weekly iron and folic acid supplementation with counseling reduces anemia in adolescent girls: a large scale effectiveness study in Uttar Pradesh, India. Food Nutr Bull 29, 186–194. [DOI] [PubMed] [Google Scholar]
- 21. Kanani SJ & Poojara RH (2000) Supplementation with iron and folic acid enhances growth in adolescent Indian girls. J Nutr 130, 2S Suppl., 452S–455S. [DOI] [PubMed] [Google Scholar]
- 22. Dongre AR, Deshmukh PR & Garg BS (2011) Community-led initiative for the control of anemia among children 6 to 35 months of age and unmarried adolescent girls in rural Wardha, India. Food Nutr Bull 32, 315–323. [DOI] [PubMed] [Google Scholar]
- 23. Dwivedi A & Schultink W (2006) Reducing anaemia among Indian adolescent girls through once-weekly supplementation with iron and folic acid. In Adolescence: A Pivotal Stage in the Lifecycle. SCN News issue 31, 19–24. [Google Scholar]
- 24. Dwivedi A (2006) Review of Adolescent Anemia Programs in India . New Delhi: The Micronutrient Initiative. [Google Scholar]