Abstract
Objective
Strategies are needed to address the shortfall in children's dairy food and Ca intakes. The present review identified interventions targeting an increase in children's dairy food or Ca intakes, and determined characteristics associated with successful intervention.
Design
A systematic literature search identified fourteen intervention studies, published in English, between 1990 and 2010. Studies were evaluated for study population, setting and mode of delivery, dietary targets and outcome measures, measures of intervention intensity, intervention description, the use of behaviour change techniques and intervention effectiveness.
Setting
Interventions targeting an increase in dairy food or Ca intake.
Subjects
Children aged 5–12 years.
Results
Ten of the fourteen studies were considered to be effective. Studies focusing on encouraging intake of dairy foods or Ca alone were all effective, compared with 55 % of studies promoting dairy within the context of a healthy diet. Effective interventions tended to be higher in intensity, provide dairy foods and were delivered across a variety of settings to a range of primary targets. The number of behaviour change techniques used did not differentiate effective and ineffective interventions, but the use of taste exposure and prompting practice appeared to be important for effective intervention.
Conclusions
Interventions that target an increase in children's dairy food or Ca intake could potentially increase children's dairy food intake by about one serving daily. Research conducted outside the USA is needed. The review has identified some promising strategies likely to be part of effective interventions for improving dairy and Ca intakes in countries where children's intake is insufficient.
Keywords: Dairy intake, Children, Intervention
Dairy foods are a major source of nutrients in children's diets and inadequate consumption during childhood has potential health implications later in life. Dairy foods provide a significant amount of total Ca and are an important source of protein, Mg and other essential nutrients( 1 ). Dairy products are unique in that they offer high Ca availability and high Ca content, and Ca provided through dairy has been shown to stimulate bone development and maximise peak bone mass( 2 , 3 ). Sixty per cent of peak bone mass is acquired throughout the pubertal years( 4 ), thus a constant intake of readily available dietary Ca during this intense growth period, among other factors, is essential in strengthening bone and reducing the risk of osteoporosis later in life( 2 , 5 ). Therefore prevention strategies that start with children, to maximise their bone density, are critical to reducing the health-care burden in the future.
Dietary guidelines recommend two to three servings of dairy foods (or about 1000 mg of Ca) daily for children( 6 – 8 ), but shortfalls in intake have been reported in Australian and American children. In Australia, on average, children aged 4–13 years consume fewer than two dairy servings daily( 1 ). The percentage of children meeting their Ca requirement decreases with age( 9 , 10 ). A large cross-sectional data set of American children suggests that as dairy consumption decreases, so does the proportion of children who meet the recommendations for Ca( 10 ). It is evident that without dairy foods, children would find it difficult to achieve adequate Ca intakes.
The majority of research to understand the influences of children's dairy intake or efforts to increase children's dairy have been conducted in the USA. Cross-sectional studies suggest that knowledge of Ca-rich foods and self-efficacy to consume dairy foods are positively associated with milk and Ca intake( 11 , 12 ). Dairy food availability at home( 13 – 15 ), role modelling of eating behaviour, parents’ expectation( 15 ) and provision of milk with meals( 16 ) have also been positively associated with children's dairy consumption. There is also strong evidence that the consumption of both plain and flavoured milk is positively associated with Ca intake( 17 – 20 ). Large population surveys from the USA show that eating a cereal-based breakfast facilitates milk consumption( 21 , 22 ) and has a positive impact on Ca intake over the whole day( 23 , 24 ).
While cross-sectional research is valuable for its insights into associations, the direction of influence is unknown and causality is difficult to determine. Therefore, we aimed to review intervention studies that targeted an increase in children's dairy food intake, to determine which strategies assist children meet their Ca requirements. The review is limited to studies targeting children of primary school age (5–12 years) as intakes are low during this critical window for attaining peak bone mass and it is considered an important stage in the development of food preferences and dietary habits that will continue into adulthood. It is also important to limit the focus to a particular target group as interventions may have different effectiveness in children of different ages. The objectives of the present review are to: (i) identify interventions that focus on children's dairy food or Ca intakes; and (ii) determine the characteristics associated with successful interventions. Using the findings of the review and incorporating current literature on other dietary change interventions including fruits and vegetables, we identify a set of promising strategies that are likely to be the most effective for improving the dairy and Ca intake of children.
Method
Search method for identification of studies
A list of search terms and keywords was developed based on recent and relevant reviews( 25 , 26 ) and refined to reflect a focus on dairy food intake in young children. Search term lists were comprehensive and inclusive (see Supplementary Materials). Terms were combined under the following headings.
-
1.
Study design: e.g. interventions, clinical trials, prospective and comparative studies.
-
2.
Nutrition: e.g. intake, diet, food and beverages.
-
3.
Children: e.g. child, young people and schoolchildren.
-
4.
Dairy intake: e.g. calcium, dairy, milk and cheese.
The main search was conducted by an information specialist in early February 2011 and included the following databases: PubMed, ProQuest, Web of Knowledge, Cochrane databases, PsychINFO and FS Tech Abstracts. Finally, reference lists of identified reviews and articles were searched for additional studies. Unpublished work was not included in the search. However, authors of published protocols that were not accompanied by any published results were contacted to assess whether any results were available. In all cases no further results were available.
Inclusion criteria
Types of studies
Prospective studies of any duration evaluating the effectiveness of an intervention, with or without a comparison group. Interventions that stated an aim to increase or promote dairy food or Ca intake in children (interventions that targeted a switch from regular- to low-fat dairy only, without promoting an increase in dairy intake, were excluded). Interventions delivered directly to young children and/or their parents, through schools or any other settings were included.
Types of participants
Children of primary school age. Primary school in Australia was considered to be children aged 5 to 12 years. If the age range crossed outside this range, then studies were included if the mean age was ≥5 years or ≤12 years. If children's age was described in terms of school years then studies involving ‘primary school’ or ‘elementary school’ were included, thereby excluding studies in pre-school, kindergarten and high schools.
Types of outcomes
Dietary outcomes describing Ca intake, individual dairy food or total dairy intake, reported at an individual or group level.
Exclusion criteria
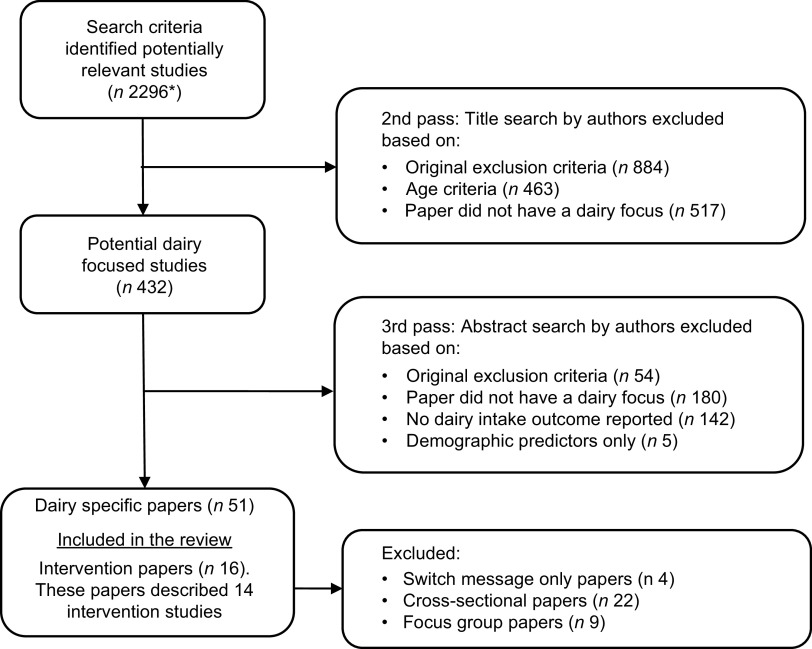
To limit the focus to interventions relevant to the general population, studies that targeted specific subgroups of the population such as clinical populations, individual case studies and children with diabetes or lactose intolerance were excluded. Studies about Ca supplementation, pregnancy, breast-feeding, infants, allergies or complementary medicine were excluded by title search. All animal studies, food science, sensory, metabolic and food processing research was also excluded by title and abstract search (these exclusion search terms are referred to as the ‘exclusion criteria’ in Fig. 1). Studies were limited to those published in English in the last 20 years, to ensure that the findings of the review are relevant to children's current context. Review authors assessed abstracts and full text where necessary against review criteria (Fig. 1). Fourteen intervention studies (described within sixteen papers) were included.
Fig. 1.
Quorum statement flow diagram: interventions focused on children's dairy food or calcium intake (*duplicates were removed by an information specialist prior to this step)
Data extraction and synthesis
Reviewers independently extracted data from papers including details of the study population, setting and mode of delivery, dietary targets and outcome measures, effectiveness, measures of intervention intensity and intervention description (see Supplementary Materials for comprehensive data extraction table). Two reviewers were used to ensure the quality of data entry. Any inconsistencies were resolved by a third reviewer.
Intervention effectiveness
Dietary intake assessment methodology varied from self- or parent-reported intake behaviour to multiple 24 h recalls. Because of heterogeneity in assessment method and outcomes (e.g. Ca, milk consumed, total dairy food intake), meta-analysis was not conducted.
We applied our own criteria whereby a study was considered to be effective when a statistically significant increase (P < 0·05 or better) in a dairy outcome was reported by the authors AND this outcome was measured using an objective method (such as sales data, observed intake) or a robust dietary assessment method (such as FFQ, 24 h recall, weighed records).
The magnitude of increase in Ca or dairy food intake was described, and comparisons made between studies where possible. Intervention effectiveness by study characteristics, intervention intensity and behaviour change techniques were assessed in all interventions.
Intervention intensity
Because of the varied study design and range of intervention settings included in the review, an assessment of intervention requirements or ‘intensity’ was developed to allow for easier comparison between all studies. Two reviewers independently scored the characteristics and resolved discrepancies by discussion. Assessment of intensity was based on four characteristics, guided by a recent review on community-wide interventions for increasing physical activity( 27 , 28 ). A 5-point scale of intensity (1 = low, 2 = low–medium, 3 = medium, 4 = medium–high, 5 = high) was developed to assess each of the following four characteristics, with the exception of ‘reach of the strategies’ (see scale details below and in Table 2).
Table 2.
Summary of intervention requirements and overall intensity ratings
| First author | Duration* | Contact† | Type of contact‡ | Reach§ | Intensity score (out of 20) | Overall intensity rating∥ | Effective¶ (Yes/No ) |
|---|---|---|---|---|---|---|---|
| Caine-Bish( 30 ) | 2 | 4 | 3 | 1 | 10 | lower | Y |
| Koivisto( 44 ) | 3 | 5 | 1 | 1 | 10 | lower | Y |
| Powers ( 40 ) | 2 | 4 | 3 | 1 | 10 | lower | N |
| Condon( 31 ) | 4 | 5 | 1 | 1 | 11 | medium | Y |
| Hovell( 37 ) | 2 | 4 | 4 | 1 | 11 | medium | Y |
| Evans( 43 ) | 3 | 2 | 4 | 3 | 12 | medium | Y |
| Freedman( 34 ) | 1 | 4 | 4 | 3 | 12 | medium | Y |
| Dwyer ( 32 )** | 5 | 5 | 1 | 1 | 12 | medium | N |
| Epstein ( 33 ) | 5 | 2 | 4 | 1 | 12 | medium | N |
| Albala( 42 ) | 3 | 4 | 5 | 1 | 13 | higher | Y |
| Alexy( 45 ) | 4 | 4 | 4 | 1 | 13 | higher | Y |
| Van Horn( 41 )†† | 5 | 3 | 4 | 1 | 13 | higher | Y |
| Muth ( 38 ) | 3 | 4 | 4 | 3 | 14 | higher | N |
| French( 35 ) | 5 | 3 | 4 | 3 | 15 | higher | Y |
Italics: highlights ineffective studies.
*1 = <6 weeks, 2 = 6 to 11 weeks, 3 = 12 weeks to 5 months, 4 = 6 to 12 months, 5 = >12 months.
†1 = annually, 2 = bimonthly to quarterly, 3 = monthly, 4 = weekly, 5 = daily.
‡1 = environmental (intervening at the physical, policy or legislative level), 2 = environmental with a small group/education component, 3 = group, 4 = group with an individual component (goal setting, homework task), 5 = individual (one-on-one personalised contact).
§1 = one setting, 3 = two settings, 5 = three or more settings. No values for 2 and 4 because three was the maximum number of settings used.
IILower = score ≤10, medium = score 11–12, higher = score ≥13.
¶Intervention effectiveness is defined as a statistically significant increase (P < 0·05) in a dairy outcome AND outcome measured using an objective method or robust dietary assessment method.
-
1.
Duration of intervention: described the length of the intervention (scaled relative to interventions included in the review). The longer the intervention, the higher the intensity.
-
2.
Contact with intervention: described the frequency of contact. Where interventions used a multiple frequency of contact points (e.g. weekly for 6 weeks, then monthly for 6 months and then quarterly for 1 year), a sum of the total number of points of contact divided by the duration of the intervention was used to give an average rate of contact.
-
3.
Type of contact or level of contact with the intervention: described the level of personalisation of the intervention. The more personalised the contact, the higher the intensity; from intervening at the environmental level (low: physical, policy or legislative) through to higher intensity individual, one-on-one personalised contact.
-
4.
Reach of the strategies: described the number of settings used to reach the target audience.
Including a description of the cost and a statement of intensity by the authors were also considered for the overall intensity rating. However, due to a lack of consistent reporting on these measures, they were not included.
Studies were scored from 1 to 5 on each of the four intensity criteria and an overall intensity score calculated based on the sum of the four components of intensity (out of a possible 20). Relative to the studies included in the present review, scores greater than 13 were considered as ‘higher’ intensity, 11–12 as ‘medium’ intensity and 10 or less as ‘lower’ intensity.
Behaviour change techniques
Standardised definitions from Abraham and Michie's taxonomy of behaviour change techniques (BCT)( 29 ) were used to define the techniques applied in the intervention (Table 1). A user guide provides definitions to code twenty-six different BCT. A health psychologist coded all interventions using the taxonomy. Techniques were also coded according to whom the BCT was aimed at (child, parent or family). After preliminary coding, an additional four categories were added to the original taxonomy to account for commonly recurring techniques unique to the interventions analysed (see techniques 30–33 in Table 1). ‘Taste exposure’ was used to describe a technique where participants were exposed (once or multiple times) to the foods targeted in the intervention. ‘Provide general nutrition education’ and ‘provide prescriptive diet’ were added to describe BCT originating from nutrition approaches to behaviour change. ‘Provide general nutrition education’ was coded as present when the intervention described a general nutrition education programme. The use of this technique may have occurred independently or in combination with technique 1 or 2. For ‘provide prescriptive diet’, interventions needed to provide participants with clear dietary parameters (e.g. percentage of macronutrients). Finally, a technique described as ‘environmental restructuring’ was added. The authors have used this technique previously( 25 ) to describe intervention attempts to change a child's direct environment to promote behaviour change. For example, this may involve changing a child's daily environment across a variety of settings (e.g. home or school) and include changes in availability of certain foods.
Table 1.
Frequency of intervention characteristics and behaviour change techniques associated with intervention effectiveness*
| Effective interventions (n 10) | Ineffective interventions (n 4) | Total (n 14) | |
|---|---|---|---|
| Specific dairy target of the intervention | |||
| Promote low-fat dairy within the context of a healthy diet | 5 | 4 | 9 |
| Increase milk intake only | 2 | 0 | 2 |
| Increase Ca through increased dairy food intake | 3 | 0 | 3 |
| Intervention intensity | |||
| Lower | 2 | 1 | 3 |
| Medium | 4 | 2 | 6 |
| Higher | 4 | 1 | 5 |
| Behaviour change techniques used† | |||
| 1. Provide general information | 3 | 1 | 4 |
| 2. Provide information consequences | 3 | 2 | 5 |
| 3. Provide information other approval | 2 | 0 | 2 |
| 4. Prompt intention formation | 6 | 2 | 8 |
| 5. Prompt barrier identification | 2 | 1 | 3 |
| 6. General encouragement | 6 | 2 | 8 |
| 7. Set graded tasks | 0 | 2 | 2 |
| 8. Provide instruction | 6 | 2 | 8 |
| 9. Model the behaviour | 5 | 2 | 7 |
| 10. Prompt specific goal setting | 6 | 2 | 8 |
| 11. Prompt review of goals | 2 | 2 | 4 |
| 12. Prompt self-monitoring | 4 | 3 | 7 |
| 13. Provide performance feedback | 0 | 2 | 2 |
| 14. Provide contingent rewards | 1 | 1 | 2 |
| 15. Teach use prompts/cues | 2 | 2 | 4 |
| 16. Agree behavioural contract | 0 | 0 | 0 |
| 17. Prompt practice | 6 | 0 | 6 |
| 18. Use follow-up prompts | 2 | 0 | 2 |
| 19. Opportunities social comparison | 5 | 1 | 6 |
| 20. Plan social support/change | 4 | 1 | 5 |
| 21. Identify role model/advocate | 3 | 1 | 4 |
| 22. Prompt self-talk | 0 | 0 | 0 |
| 23. Relapse prevention | 0 | 0 | 0 |
| 24. Stress management | 0 | 0 | 0 |
| 25. Motivational interviewing | 1 | 0 | 1 |
| 30. Taste exposure | 6 | 0 | 6 |
| 31. General nutrition education | 7 | 3 | 10 |
| 32. Environmental restructuring | 3 | 2 | 5 |
| 33. Prescribed diet | 3 | 2 | 5 |
Bold: techniques that differentiate effective and ineffective studies.
Italics: most commonly used techniques.
Intervention effectiveness is defined as a statistically significant increase (P < 0·05) in a dairy outcome AND outcome measured using an objective method or robust dietary assessment method.
Behaviour change techniques from taxonomy by Abraham and Michie( 29 ).
Results
Intervention studies
Study description
The present review summarises sixteen papers describing fourteen interventions published between years 1990 and 2010, conducted mainly in the USA( 30 – 41 ), one in South America( 42 ) and three in Europe( 43 – 45 ). Children's age spanned from 5 to 12 years, and with the exception of one study that recruited girl scouts only( 35 ), all studies targeted both girls and boys. One intervention targeted overweight and obese children( 45 ), while the others targeted the general or at-risk populations.
Sample size ranged from a small group of children to federally funded school programmes in the USA. Outcome evaluation focused primarily on short-term effects (end of intervention) with only five articles reporting follow-up effects post-intervention( 34 , 36 , 37 , 43 , 44 ).
The intervention techniques were delivered in schools (n 4), the community (n 3), the home (n 2) and within research organisations (n 2). Three studies delivered the intervention across multiple settings. Study designs included randomised controlled trials (n 6), clinical controlled trials (n 4) and uncontrolled trials (n 4; see Supplementary Materials).
Six interventions targeted both dietary and physical activity behaviours( 30 , 33 , 35 , 37 , 38 , 45 ), the other eight focused solely on dietary behaviour. It was common for interventions to target an increase in dairy foods within the context of a healthy diet (n 9). Two studies targeted milk intake only and three targeted an increase in Ca specifically, through an increase in dairy food intake (Table 1). Most interventions targeted children's behaviour (n 11) but three included parent or family behaviours as well. One study focused on parents’ provision of children's lunch( 43 ) and two focused on the family diet as a whole( 33 , 41 ).
Resources provided to the participants as part of the intervention were varied. Some studies provided government-published pamphlets about healthy eating and/or access to specialised equipment for physical activity components of the intervention( 34 , 38 ), others provided children with milk to be consumed as part of the intervention( 31 , 42 , 44 ) or with Ca-rich meals or snacks to be consumed during the intervention sessions( 30 , 35 , 37 ) (see Supplementary Materials).
Dietary assessment methods and outcomes
There was heterogeneity in both measurement and reporting of intake across the studies. Increase in Ca intake (reported in mg, n 4), over the intervention period (10–52 weeks), ranged from 202 to 671 mg. An increase of 200–250 mg (0·7–0·8 servings) was most common; however one intervention reported a 671 mg increase (2·2 servings) over a 16-week period( 42 ). That study was unique in that it promoted an increase in dairy through a swap message. Children were advised to replace sugar-sweetened beverages with low-fat flavoured milk, which was delivered to their homes( 42 ). Two studies that targeted dairy within the context of a healthy diet reported an increase in low-fat dairy foods of about 0·3 servings( 33 , 41 ). Due to the study design and variation in intake, the increase in servings of dairy was significant and sustained over a 3-year period in one study( 41 ), while the other result was not significant( 33 ).
Intervention intensity
Five studies were scored as higher intensity and three as lower intensity, with only five points separating the lowest- from the highest-intensity study (Table 2). Studies which achieved a higher intensity rating scored consistently well across all four measures, with the exception of reach or number of settings targeted. That is, higher intensity interventions were longer in duration, had frequent points of contact, and the contact was of a personalised nature.
Overall, the majority of studies (n 11) targeted only one setting (including all four lower intensity studies). Only two (of five) higher intensity studies( 35 , 38 ) targeted more than one setting, subsequently receiving the highest overall intensity ratings. French and colleagues targeted girl scouts at troop meetings and summer camps, as well as the family through activities at home( 35 ). Muth et al. targeted primarily the school setting through nutrition education sessions, combining this with homework tasks requiring parental involvement( 38 ).
All five higher intensity studies provided a personalised point of contact with intervention participants. This was in the form of either one-on-one individual contact (e.g. nutritionist visits( 36 , 42 )) or group contact with an individual component (e.g. group education with individualised goal setting( 33 , 34 , 37 , 43 )). Intervention duration of the higher intensity studies was at minimum 12–16 weeks( 38 , 42 ), with most intervening for at least 12 months, but some up to 36 months.
None of the lower intensity studies were individualised, instead utilising either group education( 30 , 40 ) or environmental strategies (e.g. provision of milk as part of school lunch programme( 44 )). However, frequency of contact was high in all lower intensity studies, directly contacting participants on either a weekly or a daily basis.
Intervention characteristics and behaviour change techniques
Interventions were delivered by a range of facilitators (from high-school students to paediatricians) in a variety of settings. Four studies used trained intervention facilitators who had no previous nutrition qualification (e.g. librarians)( 34 , 35 , 38 , 44 ).
In six studies, general nutrition education or behavioural nutrition approaches guided intervention design( 30 , 34 , 35 , 37 , 38 , 41 ). Only five studies (of fourteen) made reference to a theoretical approach underlying their intervention; they all referred to Social Cognitive (or Learning) Theory( 34 , 35 , 38 , 40 , 41 ). However, only one study( 34 ) explicitly described how theory was applied in the intervention.
Studies used between one and twenty-one BCT (Table 1). General nutrition education was the most commonly applied BCT (n 10). Other commonly used BCT included prompting intention formation, general encouragement, providing instruction and prompting specific goal setting.
Table 3 further describes the BCT used according to who were the primary targets. Seven studies used BCT targeted at children only( 30 – 32 , 35 , 38 , 40 , 44 ), and two studies focused on children but had a parent or family component( 34 , 45 ). Three studies used BCT predominantly targeted at the family (parent and child together)( 33 , 41 , 43 ), one primarily targeted parents( 37 ) and one used BCT aimed at parents and children equally( 42 ).
Table 3.
Frequency of studies utilising different targets of behaviour change techniques
| Target of technique | |||||
|---|---|---|---|---|---|
| Technique description | Family | Child | Parent | Total | |
| 1. | Provide general information | 1 | 2 | 1 | 4 |
| 2. | Provide information consequences | 2 | 2 | 1 | 5 |
| 3. | Provide information other approval | 1 | 1 | 0 | 2 |
| 4. | Prompt intention formation | 2 | 4 | 2 | 8 |
| 5. | Prompt barrier identification | 2 | 0 | 1 | 3 |
| 6. | General encouragement | 3 | 4 | 1 | 8 |
| 7. | Set graded tasks | 1 | 1 | 0 | 2 |
| 8. | Provide instruction | 1 | 6 | 1 | 8 |
| 9. | Model the behaviour | 1 | 5 | 1 | 7 |
| 10. | Prompt specific goal setting | 2 | 5 | 1 | 8 |
| 11. | Prompt review of goals | 2 | 2 | 0 | 4 |
| 12. | Prompt self-monitoring | 3 | 3 | 1 | 7 |
| 13. | Provide performance feedback | 1 | 1 | 0 | 2 |
| 14. | Provide contingent rewards | 1 | 1 | 0 | 2 |
| 15. | Teach use prompts/cues | 1 | 3 | 0 | 4 |
| 16. | Agree behavioural contract | 0 | 0 | 0 | 0 |
| 17. | Prompt practice | 1 | 5 | 0 | 6 |
| 18. | Use follow-up prompts | 1 | 0 | 1 | 2 |
| 19. | Opportunities social comparison | 0 | 5 | 1 | 6 |
| 20. | Plan social support/change | 5 | 0 | 0 | 5 |
| 21. | Identify role model/advocate | 1 | 0 | 3 | 4 |
| 22. | Prompt self-talk | 0 | 0 | 0 | 0 |
| 23. | Relapse prevention | 0 | 0 | 0 | 0 |
| 24. | Stress management | 0 | 0 | 0 | 0 |
| 25. | Motivational interviewing | 1 | 0 | 0 | 1 |
| 30. | Taste exposure | 0 | 5 | 1 | 6 |
| 31. | General nutrition education | 2 | 5 | 3 | 10 |
| 32. | Environmental restructuring | 1 | 3 | 1 | 5 |
| 33. | Prescribed diet | 2 | 3 | 0 | 5 |
Bold: highlights points of difference between targets.
*Behaviour change techniques from taxonomy by Abraham and Michie( 29 ).
BCT including providing information on the health–behaviour link, modelling the target behaviour, teaching the use of prompts/cues to perform behaviour, promoting practice, providing opportunities for social comparison (i.e. doing activities in groups) and taste exposure were targeted at children more so than parents or the family. Planning for social support was directed more at the family level, while identifying position as a role model for others’ behaviour was aimed at parents. Neither of these two techniques was applied in relation to children's behaviour in any intervention.
Characteristics of effective interventions
Eleven interventions significantly increased children's dairy or Ca intake. One did not use a robust method of intake; therefore according to the definition described, that study was considered ineffective( 40 ). Therefore, 71 % of interventions (n 10) were considered to be effective in increasing children's dairy intake. Studies focused on encouraging dairy foods or Ca intakes alone were all effective, compared with 55 % of studies promoting low-fat dairy foods within the context of a healthy diet (Table 1). The greatest increase in Ca intake was reported in one of the effective interventions (671 mg). Apart from this intervention, the overall ranges in the magnitude of change reported in the effective and ineffective interventions were similar (30–248 mg and 90–210 mg, respectively).
Effectiveness by intervention description
Table 2 shows the intervention intensity by intervention effectiveness. A majority (80 %) of the higher intensity interventions were effective. In comparison, 67 % of lower–medium intensity interventions were effective. Interestingly, the effective lower intensity interventions( 30 , 44 ) all provided dairy foods as part of the programme (see Table 1). One provided dairy as a snack with nutrition education sessions( 30 ), the other focused on an environmental strategy with the provision of milk at school lunch( 44 ). Provision of dairy was common to effective intervention – 60 % of effective studies provided Ca-rich foods, while no ineffective studies provided dairy food to their participants.
Three of the four ineffective studies shared similar intervention characteristics( 32 , 38 , 40 ). These interventions tended to be delivered in schools and all focused on children's dairy food intake within the context of general health behaviours. The ineffective studies directed BCT at children only. In contrast, only one effective intervention was delivered through a school( 31 ) and only three (of ten) effective studies used BCT directed at children only( 30 , 31 , 35 ). The fourth ineffective study( 33 ) was focused primarily on the family and delivered in the home. Interestingly, it was the only intervention to include an active control group (which may have influenced its effectiveness according to the definition used in the present review).
In the review, there were a small number of ineffective studies (four of fourteen) which made it difficult to draw distinct inferences about the potential differences in BCT used between effective and ineffective studies. The number of techniques did not differentiate effective from ineffective studies; ranging from one to twenty-one and from two to twenty for effective and ineffective studies, respectively. Only two BCT seemed to discriminate effective and ineffective studies. These were the use of taste exposure and prompting practice, which were used by 60 % the effective studies but by none of the ineffective studies. Interestingly, none of the effective studies described the use of setting graded tasks for participants or providing feedback on performance, whereas some of the ineffective studies (n 2 for each BCT) detailed the use of these BCT.
There was no clear link between the reference to a theoretical basis and effectiveness. The limited description of how theory was incorporated in those papers mentioning a theoretical underpinning limited the ability to make detailed comparisons according to theory.
The five interventions that aimed to increase dairy alone, i.e. not within the context of a healthy diet, were all effective (Table 1). The intervention intensity of these studies varied (two lower, one medium and two higher). These interventions used a wide range of techniques, delivered across a variety of settings, to a range of primary targets (children, parents and/or the family as a whole). All the dairy-specific interventions used the technique of taste exposure through the provision of dairy foods to participants. Four (of five) used general encouragement, specific goal setting or opportunities for social comparison.
Discussion
The present review identified fourteen interventions that focused on increasing young children's dairy food or Ca intakes. Over 70 % of dairy interventions were classified as effective, supporting the proportion of effective interventions reported in other reviews focusing on changing children's dietary behaviours, such as fruit and vegetable intake( 46 , 47 ). Our review has highlighted an absence of intervention research being published outside the USA. A clear majority of papers included here examined dairy intakes of children in the USA. While there are similarities between the USA and other Westernised cultures, there are unique aspects of American society that require consideration, so it is important to determine the effectiveness of similar interventions published from other countries where children's Ca intake is below recommendations.
All of the interventions identified that aimed to increase dairy or Ca intake alone were effective. In contrast, only half of the interventions that promoted dairy foods as part of a healthy diet were effective. Interventions that focus on one discrete dietary behaviour can use more specialised techniques, like specific goal setting. These interventions may also be more likely to report positive results because all their resources are targeted toward one behaviour and not diluted across several targets. Increasing dairy as a single intervention strategy may have the potential to increase overall energy intake, which should be considered in future interventions. It is also important to recognise that interventions targeting dairy within the context of the whole diet may have other positive dietary impacts (beyond Ca intake), which were not evaluated in the current review.
Despite the fact that interventions varied in their approach, content, intensity and subsequently the magnitude of behaviour change they were able to achieve, our results suggest that an increase of two-thirds to one serving of dairy (20–30 % of recommendations) daily is a possible target for future intervention. This is an important increase in the context of children's total intake. For example, in Australia, children's dairy food intake is about one serving, or about 30 %, short of recommendations( 1 ). Without meta-analysis direct comparisons between the change reported here and other studies targeting different food groups is limited. When considered in the context of dietary recommendations, the magnitude of change in dairy intake reported here is more than that described in interventions targeting children's fruit and vegetable intake, which report increases of 2–14 % of daily recommendations( 47 ). Similarly, an Australian population-level campaign reported an increase of about 11 % of daily recommendations( 48 ). If interventions were to achieve increase in dairy of one serving daily, the potential health impacts for children would be significant. Weaver and colleagues( 49 ) have estimated that increasing children's Ca intake by 500 mg/d (or 38 % of recommendations) would increase peak bone mass by 10 % and delay onset of fractures by 13 years( 5 ).
Providing dairy foods to children in this age group may be a promising way to strengthen the effect size of dairy interventions. This supports previous research that has explored other eating behaviours, such as fruit and vegetable consumption( 47 , 50 ). The provision of food appears to directly influence children's access and availability to these foods, and accessibility and availability are consistent predictors of intake( 50 ). At a population level, this strategy may have policy and infrastructure implications. In the USA, milk is provided to some children in schools as part of national breakfast or lunch programmes( 51 ) and participation in these programmes has been associated with significantly higher intake of Ca( 52 ). It is unclear whether population-level programmes would be as effective in other countries.
When we examined how intensity may be associated with effectiveness, there was no clear association, with some lower, medium and higher intensity interventions considered effective. However, within different levels of intensity different characteristics could be important. For example, effective lower intensity interventions had contact with participants either through group or environmental strategies, targeted only one setting, had high frequency of contact and provided dairy foods to children( 30 , 44 ). When resources are available to invest in intervention, higher intensity interventions can be equally effective in increasing children's dairy food intake.
Effective studies targeted parents or the family as a whole, whereas ineffective studies tended to use BCT directed only at children. The key techniques that appeared to discriminate effective from ineffective studies were the use of taste exposure to dairy foods and prompting practice of the behaviour. Taste is an important factor influencing children's food choices. Taste and taste preferences develop early in life. Milk flavour positively affects children's milk drinking behaviour, although this may be different for boys and girls( 19 ). Taste preferences are amendable to change and repeated exposure has been shown to increase intake of particular foods in children( 53 ). Increasing children's preference is one of the most consistent influences of fruit and vegetable intake( 50 ).
Limited detail in the interventions precluded the evaluation of what taste properties or sensory dimensions children were exposed to. However, one of the most successful interventions reviewed provided sweetened milk to participants. It is unclear how sweet these beverages were and any potential effects that this may have had on taste exposure specific to the flavour of dairy. If taste exposure is to be applied in order to encourage the development of a preference for dairy products, care needs to be taken as to which sensory properties children are exposed to. It is unclear how exposure to plain milk v. flavoured milk may operate to influence preference. The promotion of flavoured milk is likely to result in controversy within the discipline of public health given its potential sugar content. Nevertheless, cross-sectional and focus group research suggests that children who consume plain or flavoured milk have higher dairy intakes( 17 – 20 , 54 ). Furthermore, children like flavoured milk( 15 , 55 – 57 ) and parents think flavoured milk is a good way to increase children's dairy intake( 58 ). Therefore, the potential consequences of exposing children to flavoured milk requires more in-depth evaluation of its relative cost and benefits; as does exploration of dairy foods other than milk where taste exposure may also be relevant. Notwithstanding, our results suggest that increasing access to dairy products, such as milk, in combination with use of the taste exposure technique may be beneficial in increasing intake.
As well as taste exposure, we found effective interventions used prompting practice which is related to taste exposure as it involves rehearsing or repeating behaviour. However, upon closer examination of the interventions using this technique, we found it was not applied specifically to the consumption of dairy as in most cases it was targeted at food preparation or exercise behaviour. Therefore, its association with dairy consumption, per se, is not clear. Previous reviews of general dietary and obesity prevention interventions have also shown prompting practice to be associated with effectiveness( 25 ), so it is possible that this technique has a benefit for dietary behaviour in general, encompassing dairy intake. Coding BCT specific to the behavioural target would be a useful addition to future reviews, but a greater number of studies would be required for this level of comparison. Nevertheless, prompting practice is worth consideration in the development of health intervention, particularly in children, because they are constantly refining and practising life skills as they mature into adulthood.
General nutrition education and providing instruction about how to perform the behaviour were not clearly linked to effectiveness. Cross-sectional literature and other reviews( 3 ) suggest that knowledge of Ca-rich foods is related to intake of dairy foods( 11 ). Therefore, it is interesting that nutrition education was not associated with intervention effectiveness. This may be partly because it was used in most interventions, or it may reflect the quality of the nutrition education provided. Other dietary reviews also suggest there is limited evidence that education alone can positively alter behaviour in children( 46 ), but the additive role of providing knowledge in combination with other effective techniques cannot be determined from the present review. Improving knowledge is an attractive target of intervention because it is a relatively malleable characteristic, and at a population level the knowledge of individuals is most amendable to policy intervention( 46 ). However, the provision of information in an intervention does not mean the acquisition of knowledge. Furthermore, knowledge is ‘required but not sufficient’ for changes in consumers’ food behaviour( 59 ). For other dietary behaviours, such as the intake of fruit and vegetables and potentially for dairy intake as well, there is strong evidence that interventions combining nutrition education with improved availability and some parent involvement are more effective( 46 ).
Our review provided limited direction regarding the best setting to deliver interventions targeting children's dairy consumption. Schools are a logical setting for implementing interventions as they offer frequent contact( 60 ) and are in a unique position to reach large numbers of children( 61 ). However, interventions delivered only within schools tended to be ineffective here, which questions the effectiveness of this setting for dairy interventions. Community- and home-based interventions alone or in combination were largely effective, and these possibly show the most promise as settings for the future.
The home, as an intervention setting, is likely to play an important role in the development of habits in children. Parents, as the nutritional gatekeepers( 62 ), can influence dairy food availability( 13 – 15 , 57 , 63 , 64 ), support and role model favourable behaviours( 11 , 13 , 14 , 16 , 17 , 65 ), which are important to promote dairy intake, particularly in young children. Creating an environment for children where the consumption of dairy foods with meals or as a snack is regular practice appears to be an effective method to increase intake( 12 , 15 , 16 ) – possibly through links with taste exposure but also through habit formation. For example, eating breakfast, as a single dietary behaviour, has a positive impact on dairy intake( 21 – 24 , 66 ). We found that intervention techniques targeted at parents or the family as a whole were related to increases in dairy intake. A recent review of interventions to improve children's diets, in general, also found studies that used direct strategies to engage parents, such as requesting their attendance or participation in sessions, were more likely to report positive outcomes in children than those that relied on parents getting involved indirectly( 67 ). It appears engaging parents in interventions directly through the use of targeted behavioural techniques, or through strategies that require their involvement, shows promise and warrants inclusion into future research and education campaigns.
The present review has identified relevant literature to inform the development of future intervention aiming to increase children's dairy intakes, and in turn Ca intakes. To ensure findings were relevant to children's current context, studies were limited to those published in the last 20 years. A variety of intervention designs from clinical studies to population-level programmes were reviewed. Different measurement methods yield different results( 68 ); hence our results need to be considered within the context of the review. For example, two studies analysed in the review reported an absolute increase in dairy of 0·3 servings and one was significant( 41 ) and the other not( 33 ). In the absence of uniformed reporting or effect size estimates, our definition of effectiveness was based on the significance of results as reported by the authors. While we acknowledge statistical significance is related to the assessment method and sample size, our effectiveness (or not) approach is applied elsewhere( 46 , 67 ). Although a majority of academic communication is published in English, limiting the review to English-language papers may have created a small bias toward American papers. Only published literature was reviewed, which may have also biased the selection to more favourable outcomes and could partially explain the high proportion of successful interventions. This phenomenon is difficult to overcome. Inclusion of grey literature may identify more unsuccessful attempts to increase children's dairy intake not captured in this search, reducing our publication bias and providing more information about characteristics of ineffective intervention.
Only one-third of studies reported follow-up measures; therefore it is unclear what happens to dairy intake after the intervention period, particularly if provision of dairy foods was an integral component of the intervention. Studies of greater length are needed to make it possible to draw conclusions about the longer-term effectiveness of behaviour change and the associated health benefits for children in terms of bone density. For example, to achieve longer-term behaviour change according to social cognitive theory, barriers to dairy intake may need to be overcome. Although identification of barriers has featured in cross-sectional and focus group research, none of the interventions specifically targeting dairy, that we reviewed, utilised this technique. While the provision of dairy overcomes an immediate barrier to intake (availability), longer-term barriers, such as taste and perceived affordability, are also likely to be important. For long-term intervention to succeed intensity cannot remain high without available resources, including dollars. Few studies reported on costs but economic evidence must become part of health behaviour research as this influences the sustainability of the behaviour change.
Conclusions
Interventions that target an increase in children's dairy food or Ca intake could potentially increase children dairy food intake by about one serving daily. The current review has identified some promising strategies likely to be part of effective intervention for improving dairy and Ca intakes in countries where children's intake is insufficient (summarised in Table 4). Research to examine the effectiveness of interventions, conducted outside the USA, is required. The findings from our review can inform future interventions which aim to address the shortfall in children's Ca intake.
Table 4.
Summary of findings: promising strategies and modes of delivery likely to be part of effective intervention for improving children's dairy food and calcium intakes
|
Acknowledgements
This research was co-funded by Dairy Australia and the Commonwealth Scientific Industrial Research Organisation (CSIRO). CSIRO designed and conducted the systematic review, and prepared the manuscript. Dairy Australia reviewed the manuscript and approved it for publication. This review did not require ethics approval. The authors declare no conflicts of interest. All authors were involved in at least two of the following three processes: the development of the selection criteria, data extraction process and writing of results. G.A.H. drafted the manuscript. All authors contributed to the revisions of the manuscript and approved the final manuscript for publication.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S1368980012001322.
click here to view supplementary material
References
- 1. Baird DL, Syrette J, Hendrie GA et al. (2011) Dairy food intake of Australian children and adolescents 2–16 years of age: 2007 Australian National Children's Nutrition and Physical Activity Survey. Public Health Nutr (In the Press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Heaney RP (2009) Dairy and bone health. J Am Coll Nutr 28, Suppl. 1, 82S–90S. [DOI] [PubMed] [Google Scholar]
- 3. Nicklas TA (2003) Calcium intake trends and health consequences from childhood through adulthood. J Am Coll Nutr 22, 340–356. [DOI] [PubMed] [Google Scholar]
- 4. Loud KJ & Gordon CM (2006) Adolescent bone health. Arch Pediatr Adoles Med 160, 1026–1032. [DOI] [PubMed] [Google Scholar]
- 5. Huth PJ, DiRienzo DB & Miller GD (2006) Major scientific advances with dairy foods in nutrition and health. J Dairy Sci 89, 1207–1221. [DOI] [PubMed] [Google Scholar]
- 6. National Health and Medical Research Council (2003) Food for Health. Dietary Guidelines for Australians: A Guide to Healthy Eating. Canberra: Department of Health and Ageing, Australian Government. [Google Scholar]
- 7. Department of Health and Ageing & National Health and Medical Research Council (2006) Nutrient Reference Values for Australia and New Zealand, Including Recommended Dietary Intakes. Canberra: Australian Government. [Google Scholar]
- 8. US Department of Agriculture (not dated) How much food from the Dairy Group is needed daily? http://www.choosemyplate.gov/food-groups/dairy-amount.html (accessed July 2011).
- 9. Commonwealth Scientific Industrial Research Organisation (CSIRO) Preventative Health National Research Flagship & University of South Australia (2008) 2007 Australian National Children's Nutrition and Physical Activity Survey: Main Findings. Canberra: Australian Government, Department of Health and Ageing. [Google Scholar]
- 10. Nicklas TA, O'Neil CE & Fulgoni VL (2009) The role of dairy in meeting the recommendations for shortfall nutrients in the American diet. J Am Coll Nutr 28, Suppl. 1, 73S–81S. [DOI] [PubMed] [Google Scholar]
- 11. Sharma SV, Hoelscher DM, Kelder SH et al. (2009) Psychosocial, environmental and behavioral factors associated with bone health in middle-school girls. Health Educ Res 24, 173–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Thompson VJ, Bachman C, Watson K et al. (2008) Measures of self-efficacy and norms for low-fat milk consumption are reliable and related to beverage consumption among 5th graders at school lunch. Public Health Nutr 11, 421–426. [DOI] [PubMed] [Google Scholar]
- 13. Downs SM, Arnold A, Marshall D et al. (2009) Associations among the food environment, diet quality and weight status in Cree children in Quebec. Public Health Nutr 12, 1504–1511. [DOI] [PubMed] [Google Scholar]
- 14. Sharma SV, Hoelscher DM, Kelder SH et al. (2010) Psychosocial factors influencing calcium intake and bone quality in middle school girls. J Am Diet Assoc 110, 932–936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Vue H & Reicks M (2007) Individual and environmental influences on intake of calcium-rich food and beverages by young Hmong adolescent girls. J Nutr Educ Behav 39, 264–272. [DOI] [PubMed] [Google Scholar]
- 16. Fisher JO, Mitchell DC, Smiciklas-Wright H et al. (2004) Meeting calcium recommendations during middle childhood reflects mother–daughter beverage choices and predicts bone mineral status. Am J Clin Nutr 79, 698–706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Fisher J, Mitchell D Smiciklas-Wright H et al. (2000) Maternal milk consumption predicts the tradeoff between milk and soft drinks in young girls’ diets. J Nutr 131, 246–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Forshee RA, Anderson PA & Storey ML (2006) Changes in calcium intake and association with beverage consumption and demographics: comparing data from CSFII 1994–1996, 1998 and NHANES 1999–2002. J Am Coll Nutr 25, 108–116. [DOI] [PubMed] [Google Scholar]
- 19. Murphy MM, Douglass JS, Johnson RK et al. (2008) Drinking flavored or plain milk is positively associated with nutrient intake and is not associated with adverse effects on weight status in US children and adolescents. J Am Diet Assoc 108, 631–639. [DOI] [PubMed] [Google Scholar]
- 20. Striegel-Moore RH, Thompson D, Affenito SG et al. (2006) Correlates of beverage intake in adolescent girls: the National Heart, Lung, and Blood Institute Growth and Health Study. J Pediatr 148, 183–187. [DOI] [PubMed] [Google Scholar]
- 21. Albertson AM, Thompson D, Franko DL et al. (2008) Consumption of breakfast cereal is associated with positive health outcomes: evidence from the National Heart, Lung, and Blood Institute Growth and Health Study. Nutr Res 28, 744–752. [DOI] [PubMed] [Google Scholar]
- 22. van den Boom A, Serra-Majem L, Ribas L et al. (2006) The contribution of ready-to-eat cereals to daily nutrient intake and breakfast quality in a Mediterranean setting. J Am Coll Nutr 25, 135–143. [DOI] [PubMed] [Google Scholar]
- 23. Affenito SG, Thompson DR, Barton BA et al. (2005) Breakfast consumption by African-American and white adolescent girls correlates positively with calcium and fiber intake and negatively with body mass index. J Am Diet Assoc 105, 938–945. [DOI] [PubMed] [Google Scholar]
- 24. Barton BA, Eldridge AL, Thompson D et al. (2005) The relationship of breakfast and cereal consumption to nutrient intake and body mass index: the National Heart, Lung, and Blood Institute Growth and Health Study. J Am Diet Assoc 105, 1383–1389. [DOI] [PubMed] [Google Scholar]
- 25. Hendrie GA, Brindal E, Corsini N et al. (2012) Combined home and school obesity prevention interventions for children: what behaviour change strategies and intervention characteristics are associated with effectiveness? Health Educ Behav 39, 159–171. [DOI] [PubMed] [Google Scholar]
- 26. Golley RK, Hendrie GA, Slater A et al. (2011) Interventions that involve parents to improve children's (weight-related) nutrition intake and activity patterns – what nutrition and activity targets and behaviour change techniques are associated with intervention effectiveness? Obes Rev 12, 114–130. [DOI] [PubMed] [Google Scholar]
- 27. Francis DP, Baker PRA, Doyle J et al. (2011) Cochrane Update: reviewing interventions delivered to whole communities: learnings and recommendations for application to policy, practice and evidence devlopment. J Public Health 33, 322–325. [DOI] [PubMed] [Google Scholar]
- 28. Baker PRA, Francis DP, Soares J et al. (2011) Community wide interventions for increasing physical activity. Cochrane Database Syst Rev issue 4, CD008366. [DOI] [PubMed] [Google Scholar]
- 29. Abraham C & Michie S (2008) A taxonomy of behavior change techniques used in interventions. Health Psychol 27, 379–387. [DOI] [PubMed] [Google Scholar]
- 30. Caine-Bish N & Lowry Gordon K (2006). Calcium and KIDS: a pilot program developed to increase calcium intakes in third- through sixth-grade children. J Nutr Educ Behav 38, 199–200. [DOI] [PubMed] [Google Scholar]
- 31. Condon EM, Crepinsek MK & Fox MK (2009) School meals: types of foods offered to and consumed by children at lunch and breakfast. J Am Diet Assoc 109, 2 Suppl., S67–S78. [DOI] [PubMed] [Google Scholar]
- 32. Dwyer JT, Hewes LV, Mitchell PD et al. (1996) Improving school breakfasts: effects of the CATCH Eat Smart Program on the nutrient content of school breakfasts. Prev Med 25, 413–422. [DOI] [PubMed] [Google Scholar]
- 33. Epstein LH, Paluch RA, Beecher MD et al. (2008) Increasing healthy eating vs. reducing high energy-dense foods to treat pediatric obesity. Obesity (Silver Spring) 16, 318–326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Freedman MR & Nickell A (2010) Impact of after-school nutrition workshops in a public library setting. J Nutr Educ Behav 42, 192–196. [DOI] [PubMed] [Google Scholar]
- 35. French SA, Story M Fulkerson JA et al. (2005) Increasing weight-bearing physical activity and calcium-rich foods to promote bone mass gains among 9–11 year old girls: outcomes of the Cal-Girls study. Int J Behav Nutr Phys Act 2, 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Friedman LA, Snetselaar L, Stumbo P et al. (2007) Influence of intervention on beverage choices: trends in the Dietary Intervention Study in Children (DISC). J Am Diet Assoc 107, 586–594. [DOI] [PubMed] [Google Scholar]
- 37. Hovell MF, Nichols JF, Irvin VL et al. (2009) Parent/child training to increase preteens’ calcium, physical activity, and bone density: a controlled trial. Am J Health Promot 24, 118–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Muth ND, Chatterjee A, Williams D et al. (2008) Making an IMPACT: effect of a school-based pilot intervention. N C Med J 69, 432–440. [PubMed] [Google Scholar]
- 39. Osganian SK, Ebzery MK, Montgomery DH et al. (1996) Changes in the nutrient content of school lunches: results from the CATCH Eat Smart Food Service Intervention. Prev Med 25, 400–412. [DOI] [PubMed] [Google Scholar]
- 40. Powers AR, Struempler BJ, Guarino A et al. (2005) Effects of a nutrition education program on the dietary behavior and nutrition knowledge of second-grade and third-grade students. J Sch Health 75, 129–133. [PubMed] [Google Scholar]
- 41. Van Horn L, Obarzanek E, Friedman LA et al. (2005) Children's adaptations to a fat-reduced diet: the Dietary Intervention Study in Children (DISC). Pediatrics 115, 1723–1733. [DOI] [PubMed] [Google Scholar]
- 42. Albala C, Ebbeling CB, Cifuentes M et al. (2008) Effects of replacing the habitual consumption of sugar-sweetened beverages with milk in Chilean children. Am J Clin Nutr 88, 605–611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Evans CEL, Greenwood DC, Thomas JD et al. (2010) SMART lunch box intervention to improve the food and nutrient content of children's packed lunches: UK wide cluster randomised controlled trial. J Epidemiol Community Health 64, 970–976. [DOI] [PubMed] [Google Scholar]
- 44. Koivisto UK, Edlund B & Sjoden PO (1994) Exposure to milk or water at preschool lunch for 3 months influences children's choice of elementary school lunch drink 4 months later. Appetite 23, 265–273. [DOI] [PubMed] [Google Scholar]
- 45. Alexy U, Reinehr T, Sichert-Hellert W et al. (2006) Positive changes of dietary habits after an outpatient training program for overweight children. Nutr Res 26, 202–208. [Google Scholar]
- 46. Van Cauwenberghe E, Maes L, Spittales H et al. (2010) Effectiveness of school-based interventions in Europe to promote healthy nutrition in children and adolescents: systematic review of published and ‘grey’ literature. Br J Nutr 103, 781–797. [DOI] [PubMed] [Google Scholar]
- 47. de Sa J & Lock K (2008) Will European agricultural policy for school fruit and vegetables improve public health? A review of school fruit and vegetable programmes. Eur J Public Health 18, 558–568. [DOI] [PubMed] [Google Scholar]
- 48. Pollard CM, Miller MR, Daly AM et al. (2007) Increasing fruit and vegetable consumption: success of the Western Australian Go for 2&5 campaign. Public Health Nutr 11, 314–320. [DOI] [PubMed] [Google Scholar]
- 49. Weaver CM (2010) Why should my teens consume dairy? Presented at International Dairy Federation World Dairy Summit: Nutrition and Health, 5–11 November 2010, Auckland, New Zealand.
- 50. Geller KS & Dzewaltowski DA (2009) Longitudinal and cross-sectional influences on youth fruit and vegetable consumption. Nutr Rev 67, 65–76. [DOI] [PubMed] [Google Scholar]
- 51. Food and Nutrition Service, US Department of Agriculture (2012) National School Breakfast and Lunch Programs. http://www.fns.usda.gov/cnd (accessed July 2012).
- 52. Gordon AR & McKinney P (1995) Sources of nutrients in students’ diets. Am J Clin Nutr 61, 1 Suppl., 232S–240S. [DOI] [PubMed] [Google Scholar]
- 53. Birch LL, Gunder L, Grimm-Thomas K et al. (1998) Infants consumption of a new food enhances acceptance of similar foods. Appetite 30, 283–295. [DOI] [PubMed] [Google Scholar]
- 54. Johnson RK, Frary C & Wang MQ (2002) The nutritional consequences of flavored-milk consumption by school-aged children and adolescents in the United States. J Am Diet Assoc 102, 853–856. [DOI] [PubMed] [Google Scholar]
- 55. Auld G, Boushey CJ, Bock MA et al. (2002) Perspectives on intake of calcium-rich foods among Asian, Hispanic, and white preadolescent and adolescent females. J Nutr Educ Behav 34, 242–251. [DOI] [PubMed] [Google Scholar]
- 56. Connors P, Bednar C & Klammer S (2001) Cafeteria factors that influence milk-drinking behaviors of elementary school children: grounded theory approach. J Nutr Educ 33, 31–36. [DOI] [PubMed] [Google Scholar]
- 57. Novotny R, Ji-Sook H & Biernacke I (1999) Motivators and barriers to consuming calcium-rich foods among Asian adolescents in Hawaii. J Nutr Educ 31, 99–104. [Google Scholar]
- 58. Winzenberg T, Hansen E & Jones G (2008) How do women change osteoporosis preventive behaviours in their children? Eur J Clin Nutr 62, 379–385. [DOI] [PubMed] [Google Scholar]
- 59. Worsley A (2002) Nutrition knowledge amd food consumption: can nutrition knowledge change food behaviour? Asia Pac J Clin Nutr 11, Suppl. 3, S579–S585. [DOI] [PubMed] [Google Scholar]
- 60. Brown T & Summerbell C (2009) Systematic review of school-based interventions that focus on changing dietary intake and physical activity levels to prevent childhood obesity: an update to the obesity guidance produced by the National Institute for Health and Clinical Excellence. Obes Rev 10, 110–141. [DOI] [PubMed] [Google Scholar]
- 61. Peterson KE & Fox MK (2007) Addressing the epidemic of childhood obesity through school-based interventions: what has been done and where do we go from here? J Law Med Ethics 35, Spring issue, 113–130. [DOI] [PubMed] [Google Scholar]
- 62. Wansink B (2006) Nutritional gatekeepers and the 72% solution. J Am Diet Assoc 106, 1324–1327. [DOI] [PubMed] [Google Scholar]
- 63. Edlefsen M, Reicks M, Goldberg D et al. (2008) Strategies of Asian, Hispanic, and non-Hispanic white parents to influence young adolescents’ intake of calcium-rich foods, 2004 and 2005. Prev Chronic Dis 5, A119. [PMC free article] [PubMed] [Google Scholar]
- 64. Olson BH, Chung KR, Reckase M et al. (2009) Parental influences on dairy intake in children, and their role in child calcium-fortified food use. J Nutr Educ Behav 41, 53–57. [DOI] [PubMed] [Google Scholar]
- 65. Gillman MW, Rifas-Shiman SL, Frazier AL et al. (2000) Family dinner and diet quality among older children and adolescents. Arch Fam Med 9, 235–240. [DOI] [PubMed] [Google Scholar]
- 66. Song WO, Chun OK, Kerver J et al. (2006) Ready-to-eat breakfast cereal consumption enhances milk and calcium intake in the US population. J Am Diet Assoc 106, 1783–1789. [DOI] [PubMed] [Google Scholar]
- 67. Hingle MD, O'Connor TM, Dave JM et al. (2010) Parental involvement in interventions to improve child dietary intake: a systematic review. Prev Med 51, 103–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Stevens J, Taber DR, Murray DM et al. (2007) Advances and controversies in the design of obesity prevention trials. Obesity (Silver Spring) 15, 2163–2170. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit https://doi.org/10.1017/S1368980012001322.
click here to view supplementary material