Abstract
Objective
Exclusive breast-feeding is estimated to reduce infant mortality in low-income countries by up to 13 %. The aim of the present study was to determine the risk factors associated with suboptimal breast-feeding practices in Pakistan.
Design
A cross-sectional study using data extracted from the multistage cluster sample survey of the Pakistan Demographic and Health Survey 2006–2007.
Setting
A nationally representative sample of households.
Subjects
Last-born alive children aged 0–23 months (total weighted sample size 3103).
Results
The prevalences of timely initiation of breast-feeding, bottle-feeding in children aged 0–23 months, exclusive breast-feeding and predominant breast-feeding in infants aged 0–5 months were 27·3 %, 32·1 %, 37·1 % and 18·7 %, respectively. Multivariate analysis indicated that working mothers (OR = 1·48, 95 % CI 1·16, 1·87; P = 0·001) and mothers who delivered by Caesarean section (OR = 1·95, 95 % CI 1·30, 2·90; P = 0·001) had significantly higher odds for no timely initiation of breast-feeding. Mothers from North West Frontier Province were significantly less likely (OR = 0·37, 95 % CI 0·23, 0·59; P < 0·001) not to breast-feed their babies exclusively. Mothers delivered by traditional birth attendants had significantly higher odds to predominantly breast-feed their babies (OR = 1·96, 95 % CI 1·18, 3·24; P = 0·009). The odds of being bottle-fed was significantly higher in infants whose mothers had four or more antenatal clinic visits (OR = 1·93, 95 % CI 1·46, 2·55; P < 0·001) and belonged to the richest wealth quintile (OR = 2·41, 95 % CI 1·62, 3·58; P < 0·001).
Conclusions
The majority of Pakistani mothers have suboptimal breast-feeding practices. To gain the full benefits of breast-feeding for child health and nutrition, there is an urgent need to develop interventions to improve the rates of exclusive breast-feeding.
Keywords: Initiation of breast-feeding, Exclusive breast-feeding, Predominant breast-feeding, Bottle-feeding, Infant feeding practices, Pakistani women
The advantages of exclusive breast-feeding (EBF) and the risks of higher morbidity and mortality associated with suboptimum feeding practices in children are well documented( 1 – 6 ). For this reason, the WHO infant feeding guidelines recommend that newborns should be put to the breast within the first hour of birth (timely initiation of breast-feeding) and infants should be exclusively breast-fed for the first 6 months of life and introduced to nutritionally adequate and safe complementary foods thereafter, with breast-feeding continuing up to 2 years of age to achieve optimal growth, development and health( 7 ). A recent analysis shows that suboptimum breast-feeding, especially non-EBF in the first 6 months of life, results in 1·4 million deaths annually and 10 % of the disease burden in children <5 years of age( 8 ). It is estimated that 10–15 % of deaths in children aged <5 years in-resource poor countries could be prevented through achievement of 90 % coverage with EBF alone( 9 ). Predominant breast-feeding (PBF) is defined as feeding plain water or water-based drinks and fruit juices in addition to breast milk in infants <6 months of age( 10 ). Morbidity is increased significantly in predominantly breast-fed babies, especially from gastroenteritis and respiratory tract infections( 8 , 11 ). Likewise, bottle-feeding has been recognized as detrimental to the health and intellectual development of children( 1 , 12 ).
Pakistan is the sixth most populous country in the world and the second most populated country in the South Asian region. The level of socio-economic development is still low and a quarter of the entire population lives below the poverty line( 13 ). The health profile of Pakistan is characterized by a high population growth rate, high infant and child mortality rates, a high maternal mortality ratio and a high burden of communicable diseases in children( 14 ). Pakistan would gain enormous health and economic benefits by improving infant feeding practices. Identification and recognition of the barriers to EBF in communities is essential for developing effective nutrition education and behaviour change strategies targeting families at heightened risk of suboptimal infant feeding behaviours. The purpose of the present study was to determine the factors associated with non-initiation of timely breast-feeding, non-EBF, PBF and bottle-feeding after controlling for individual-, household- and community-level characteristics.
Methodology
Data source
We analysed data from the 2006–2007 Pakistan Demographic and Health Survey (PDHS), which was carried out by the National Institute of Population Studies and Macro International. The 2006–2007 PDHS used a stratified, multistage cluster sampling strategy with urban and rural samples drawn separately and in proportion to the population of each province. Geographic sampling units were obtained for both urban and rural areas and random household sampling was conducted to select units. A total of 10 023 ever-married women were interviewed with a response rate of 94·5 %. A detailed birth and feeding history for the last 5 years preceding the survey was asked from all of the ever-married women interviewed( 14 ).
The data set was downloaded from the public access website (http://www.measuredhs.com). Afterwards, it was inspected for data quality, completeness of information and comparability of variables required for the present analysis. The required variables from the data set were selected and the files were constructed. We selected last-born children aged <24 months at the time of the survey and living with respondents/mothers. The total weighted number of children aged 0–23 months was 3103.
Measures
The dependent variables in the present study were the timely initiation of breast-feeding (0–23 months) and rates of EBF (<6 months), PBF (<6 months) and bottle-feeding (0–23 months). Indicators were estimated according to the key factors described by the WHO in 2008( 15 ). A household wealth index was constructed from data collected in the household questionnaire, using methods recommended by the World Bank Poverty Network and UNICEF( 16 ), and was divided into five equal categories to classify the households by economic status.
The explanatory variables were classified into three levels, i.e. individual, household and community. The individual level attributes included age, sex, birth weight of the child, mother's age, working status of the mother in the past 12 months, highest education level achieved and marital status at the time of interview. Information on the number of antenatal clinic (ANC) visits, place of delivery, mode of delivery, type of delivery assistance availed, birth order and postnatal contacts (PNC) with a health-care provider was also obtained. Household wealth index was included as a household-level variable. Community-level attributes specific to breast-feeding such as policies and practices that support breast-feeding, implementation of the marketing code for breast milk substitutes and cultural norms regarding breast-feeding were not available in the current DHS data set. Therefore, only the geographical region (province) and residential area (urban and rural) were considered.
Statistical analysis
The EBF indicator was expressed as a dichotomous variable with category 0 for EBF and category 1 for non-EBF; timely initiation of breast-feeding as category 0 for timely initiation and category 1 for no timely initiation; the PBF indicator was expressed as category 0 for non-PBF (EBF or bottle-feeding in infants <6 months separately) and category 1 for PBF; while the bottle-feeding indicator was expressed as category 1 for bottle-feeding and category 0 for not bottle-feeding. These variables were examined against a set of independent variables (individual, household and community characteristics) in order to determine the prevalence of timely initiation of breast-feeding, EBF, PBF and bottle-feeding and factors associated with no timely initiation of breast-feeding, non-EBF, PBF and bottle-feeding. Analyses were performed using the STATA statistical software package version 10 (StataCorp, College Station, TX, USA) with ‘svy’ commands to allow for adjustments for the cluster sampling design used in the surveys when estimating confidence intervals around prevalence estimates. The χ 2 test was used to test the significance of associations.
Associations were examined by univariate analyses (unadjusted OR and 95 % CI) and then by multivariate logistic regression (adjusted OR (AOR) and 95 % CI) analysis. In the univariate analysis, OR and 95 % CI were calculated in order to assess the unadjusted risk of independent variables on feeding practices. Multivariate logistic regression was employed to estimate the OR adjusted for the independent variables. A stepwise backwards elimination approach was used for model construction, retaining those variables with P < 0·05 in the final model.
Results
In the current analysis, 3103 (weighted total) children aged 0–23 months were selected. Table 1 lists the individual-, household- and community-level characteristics of these children. Almost a quarter of the mothers (22·5 %) had worked in the 12 months prior to the survey. Nearly 64 % (63·8 %) of the mothers had no education while just over a third (34·7 %) of the fathers were uneducated. The majority of the mothers (77·6 %) were aged 20–34 years. Both male and female children, and different age categories, were nearly equally represented in the sample. One-third of the mothers (32·5 %) had no ANC visits during the pregnancy. Of the total births, almost two-thirds (61·3 %) were delivered at home and 27·5 % of the deliveries were conducted by untrained personnel. According to the mothers’ perception, 45·1 % of the children were of average size at birth while 34·1 % were of small size. About 70 % (69·8 %) of the children were living in rural areas. Details can be seen in Table 1.
Table 1.
Individual-, household- and community-level characteristics of children aged 0–23 months (n 3103); secondary analysis of data from the Pakistan Demographic and Health Survey (PDHS) 2006–2007
| Characteristic | n | % |
|---|---|---|
| Individual-level factors | ||
| Maternal working status (n 3099) | ||
| Non-working | 2403 | 77·5 |
| Working (past 12 months) | 696 | 22·5 |
| Maternal education | ||
| No education | 1981 | 63·8 |
| Primary | 474 | 15·3 |
| Secondary and above | 648 | 20·9 |
| Father's education (n 3096) | ||
| No education | 1074 | 34·7 |
| Primary | 525 | 17·0 |
| Secondary and above | 1497 | 48·3 |
| Literacy (n 3095) | ||
| Cannot read at all | 1945 | 62·8 |
| Able to read only passage | 1150 | 37·2 |
| Mother's age (years) | ||
| 15–19 | 172 | 5·5 |
| 20–34 | 2409 | 77·6 |
| 35–49 | 522 | 16·8 |
| Marital status | ||
| Currently married | 3081 | 99·3 |
| Formerly married* | 22 | 0·7 |
| Birth order | ||
| First-born | 609 | 19·6 |
| Second- to fourth-born | 1522 | 49·1 |
| Fifth-born or higher | 971 | 31·3 |
| Preceding birth interval (n 3094) | ||
| No previous birth | 609 | 19·7 |
| 0–14 months | 166 | 5·4 |
| 14–24 months | 724 | 23·4 |
| ≥25 months | 1595 | 51·5 |
| Sex of baby | ||
| Male | 1644 | 53·0 |
| Female | 1459 | 47·0 |
| Age of child (months) | ||
| 0–5 | 955 | 30·8 |
| 6–11 | 811 | 26·1 |
| 12–17 | 843 | 27·2 |
| 18–23 | 494 | 15·9 |
| Perceived birth size of baby (n 3100) | ||
| Small | 1056 | 34·1 |
| Average | 1398 | 45·1 |
| Large | 646 | 20·8 |
| Place of delivery (n 3101) | ||
| Home | 1902 | 61·3 |
| Health facility | 1199 | 38·7 |
| Mode of delivery (n 3101) | ||
| Non-Caesarean | 2823 | 91·0 |
| Caesarean section | 278 | 9·0 |
| Type of delivery assistance (n 3074) | ||
| Health professional | 1183 | 38·5 |
| Traditional birth attendant | 1046 | 34·0 |
| Other untrained | 845 | 27·5 |
| Antenatal clinic visits (n 3091) | ||
| None | 1005 | 32·5 |
| 1–3 | 1162 | 37·6 |
| ≥4 | 924 | 29·9 |
| Timing of postnatal check-up (n 1172) | ||
| Day 0–2 | 395 | 33·7 |
| Day 3–6 | 684 | 58·4 |
| Day 7 or later | 72 | 6·2 |
| No check-ups (including missing) | 21 | 1·8 |
| Household level factors | ||
| Household wealth index | ||
| Poorest | 683 | 22·0 |
| Poorer | 670 | 21·6 |
| Middle | 625 | 20·2 |
| Richer | 582 | 18·8 |
| Richest | 543 | 17·5 |
| Community-level factors | ||
| Residence | ||
| Urban | 937 | 30·2 |
| Rural | 2166 | 69·8 |
| Geographical region (province) | ||
| Punjab | 1741 | 56·1 |
| Sindh | 775 | 25·0 |
| North West Frontier | 452 | 14·6 |
| Balochistan | 136 | 4·4 |
Weighted total was 3103 unless stated otherwise within parentheses.
*Divorced, separated and widowed.
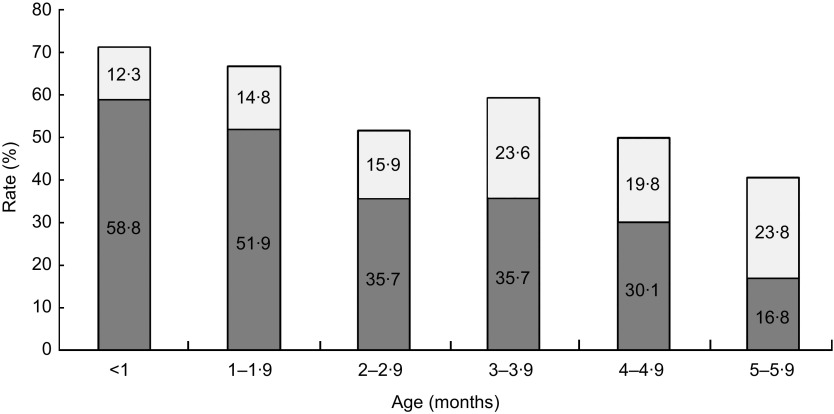
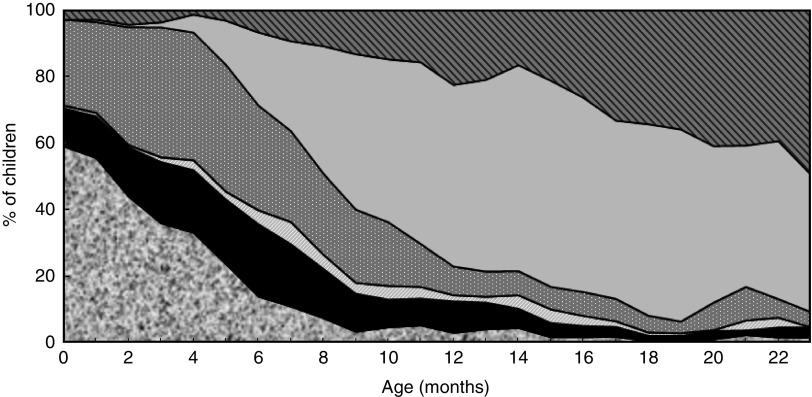
Regardless of being breast-fed or not, 997 (32·1 % (95 % CI 30·0, 34·4) %) infants received food or drink from a bottle with a nipple or teat during the 24 h prior to the interview. Rate of timely initiation of breast-feeding was 27·3 % in children aged 0–23 months. The bottle-feeding rate varied with age; it was 26·8 % in infants aged <6 months, 36·8 % in infants aged 6–11 months and 33·2 % in children 12–23 months of age. The EBF rate in children aged <6 months was 37·1 % (95 % CI 33·4, 40·9) %, while the PBF rate in children <6 months of age was 18·7 % (95 % CI 15·8, 22·1) % (Table 2). Figure 1 indicates that the PBF rate increased consistently as the EBF rate decreased from infants <1 month of age (12·3 % v. 58·8 %) to infants at 5–5·9 months of age (23·8 % v. 16·8 %). Figure 2 shows the distribution of children by breast-feeding status according to child age.
Table 2.
Breast-feeding indicators among children aged 0–23 months (n 3103); secondary analysis of data from the Pakistan Demographic and Health Survey (PDHS) 2006–2007
| Indicator | Sample size (weighted) | n (weighted) | Rate (%) | 95 % CI | |
|---|---|---|---|---|---|
| Timely initiation of breast-feeding (<24 months) | 3103 | 848 | 27·3 | 25·1, 29·7 | |
| Ever breast-fed (<24 months) | 3103 | 3029 | 97·6 | 96·9, 98·2 | |
| Ever breast-fed (<12 months) | 1766 | 1727 | 97·8 | 96·9, 98·4 | |
| Ever breast-fed (12–23 months) | 1337 | 1302 | 97·4 | 96·2, 98·3 | |
| Exclusive breast-feeding (<6 months) | 955 | 354 | 37·1 | 33·4, 40·9 | |
| Exclusive breast-feeding (0–1 month) | 282 | 154 | 54·6 | 47·6, 61·5 | |
| Exclusive breast-feeding (2–3 months) | 355 | 127 | 35·7 | 30·2, 41·6 | |
| Exclusive breast-feeding (4–5 months) | 319 | 74 | 23·1 | 18·4, 28·6 | |
| Exclusive breast-feeding (0–3 months) | 637 | 281 | 44·1 | 39·5, 48·8 | |
| Predominant breast-feeding (<6 months) | 955 | 179 | 18·7 | 15·8, 22·1 | |
| Bottle-feeding (<24 months) | 3103 | 997 | 32·1 | 30·0, 34·4 | |
| Bottle-feeding (<6 months) | 955 | 256 | 26·8 | 23·5, 30·3 | |
| Bottle-feeding (6–11 months) | 811 | 298 | 36·8 | 32·6, 41·1 | |
| Bottle-feeding (12–23 months) | 1337 | 444 | 33·2 | 30·2, 36·3 | |
| Median duration of exclusive breast-feeding (<36 months) (months) | 1·9 | ||||
Fig 1.
Rates of exclusive breast-feeding (
 ) and predominant breast-feeding (
) and predominant breast-feeding (
 ) according to child's age; secondary analysis of data from the Pakistan Demographic and Health Survey (PDHS) 2006–2007
) according to child's age; secondary analysis of data from the Pakistan Demographic and Health Survey (PDHS) 2006–2007
Fig 2.
Distribution of children by breast-feeding (BF) status (
 , exclusive BF;
, exclusive BF;
 , BF+water;
, BF+water;
 , BF+liquids/juice;
, BF+liquids/juice;
 , BF+other milk;
, BF+other milk;
 , BF+complementary foods;
, BF+complementary foods;
 , no BF) according to child's age; secondary analysis of data from the Pakistan Demographic and Health Survey (PDHS) 2006–2007
, no BF) according to child's age; secondary analysis of data from the Pakistan Demographic and Health Survey (PDHS) 2006–2007
The median duration of EBF was 1·9 months. The rates of related breast-feeding indicators among children aged 0–23 months are shown in Table 2.
Univariate analyses
Timely initiation of breast-feeding
Working mothers (20·7 %, P < 0·001), mothers who delivered by Caesarean section (17·0 %, P = 0·001) and those residing in Sindh Province (17·6 %, P < 0·001) had significantly lower rates of timely initiation of breast-feeding (Table 3).
Table 3.
Rates of timely initiation of breast-feeding, bottle-feeding, exclusive breast-feeding and predominant breast-feeding by individual-, household- and community-level characteristics; secondary analysis of data from the Pakistan Demographic and Health Survey (PDHS) 2006–2007
| Timely initiation of breast-feeding (<24 months) | Bottle-feeding (< 24 months) | Exclusive breast-feeding (<6 months) | Predominant breast-feeding (<6 months) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Characteristic | % | 95 % CI | P | % | 95 % CI | P | % | 95 % CI | P | % | 95 % CI | P |
| Individual-level factors | ||||||||||||
| Maternal working status | ||||||||||||
| Non-working | 29·2 | 26·61, 31·83 | <0·001 | 33·6 | 31·30, 36·03 | 0·012 | 39·1 | 34·97, 43·47 | 0·010 | 17·4 | 14·36, 21·02 | 0·058 |
| Working (past 12 months) | 20·7 | 17·36, 24·42 | 27·2 | 23·11, 31·78 | 26·3 | 19·63, 34·32 | 25·5 | 18·76, 33·75 | ||||
| Maternal education | ||||||||||||
| No education | 27·2 | 24·44, 30·24 | 0·922 | 25·3 | 22·84, 27·82 | <0·001 | 37·3 | 32·74, 42·12 | 0·950 | 21·9 | 18·19, 26·07 | 0·016 |
| Primary | 26·7 | 21·94, 32·10 | 39·2 | 34·05, 44·69 | 37·6 | 28·95, 47·13 | 14·4 | 8·93, 22·49 | ||||
| Secondary and above | 28·0 | 24·06, 32·32 | 48·0 | 43·39, 52·69 | 36·0 | 28·29, 44·57 | 11·9 | 7·30, 18·84 | ||||
| Literacy | ||||||||||||
| Cannot read at all | 27·0 | 24·16, 29·94 | 0·828 | 25·3 | 22·88, 27·89 | <0·001 | 36·3 | 31·80, 41·09 | 0·410 | 21·9 | 18·22, 26·15 | 0·010 |
| Able to read only passage | 28·0 | 24·80, 31·34 | 43·7 | 40·28, 47·15 | 38·2 | 32·17, 44·51 | 13·2 | 9·31, 18·44 | ||||
| Mother's age (years) | ||||||||||||
| 15–19 | 29·8 | 22·61, 38·18 | 0·802 | 29·1 | 21·72, 37·72 | 0·754 | 34·5 | 24·34, 46·34 | 0·900 | 22·8 | 13·97, 35·07 | 0·552 |
| 20–34 | 27·3 | 24·79, 29·87 | 32·3 | 29·97, 34·73 | 37·2 | 33·10, 41·57 | 18·8 | 15·59, 22·45 | ||||
| 35–49 | 26·8 | 22·25, 31·89 | 32·4 | 27·70, 37·48 | 37·7 | 28·75, 47·63 | 16·3 | 10·53, 24·23 | ||||
| Marital status | ||||||||||||
| Currently married | 27·3 | 25·09, 29·68 | 0·952 | 32·1 | 30·00, 34·35 | 0·929 | 37·1 | 33·45, 40·93 | 0·440 | 18·7 | 15·78, 22·01 | 0·037 |
| Formerly married* | 26·6 | 10·23, 53·61 | 33·3 | 13·83, 60·77 | 0·0 | 0·0 | ||||||
| Birth order | ||||||||||||
| First-born | 24·9 | 21·00, 29·27 | 0·189 | 35·1 | 30·58, 39·92 | 0·347 | 34·4 | 27·17, 42·49 | 0·050 | 23·2 | 16·97, 30·84 | 0·077 |
| Second- to fourth-born | 26·9 | 24·04, 29·85 | 31·7 | 28·71, 34·86 | 34·3 | 29·45, 39·54 | 19·6 | 15·57, 24·28 | ||||
| Fifth-born or higher | 29·6 | 26·00, 33·43 | 31·0 | 27·51, 34·65 | 44·3 | 37·16, 51·64 | 13·7 | 9·47, 19·50 | ||||
| Preceding birth interval (months) | ||||||||||||
| No previous birth | 24·9 | 21·00, 29·27 | 0·488 | 35·1 | 30·58, 39·92 | 0·169 | 34·4 | 27·17, 42·49 | 0·020 | 23·2 | 16·97, 30·84 | 0·244 |
| 0–14 months | 29·7 | 22·14, 38·55 | 35·8 | 28·50, 43·82 | 22·8 | 12·82, 37·18 | 20·8 | 11·22, 35·22 | ||||
| 14–24 months | 27·0 | 23·14, 31·27 | 33·1 | 28·85, 37·65 | 31·2 | 23·62, 39·86 | 21·2 | 15·10, 29·01 | ||||
| ≥25 months | 28·2 | 25·31, 31·33 | 30·1 | 27·33, 32·98 | 42·1 | 36·94, 47·44 | 18·8 | 12·28, 20·08 | ||||
| Sex of baby | ||||||||||||
| Male | 26·7 | 23·99, 29·66 | 0·497 | 32·8 | 30·03, 35·73 | 0·471 | 38·9 | 34·15, 43·97 | 0·270 | 18·4 | 14·53, 23·06 | 0·829 |
| Female | 28·0 | 25·06, 31·10 | 31·4 | 28·50, 34·42 | 35·0 | 29·91, 40·54 | 19·1 | 15·01, 23·95 | ||||
| Age of child (months) | ||||||||||||
| 0–5 | 25·7 | 22·25, 29·57 | 0·341 | 26·8 | 23·48, 30·33 | 0·001 | 18·7 | 14·80, 22·15 | ||||
| 11–6 | 26·5 | 22·93, 30·46 | 36·8 | 32·57, 41·14 | ||||||||
| 12–17 | 30·0 | 26·38, 33·97 | 34·3 | 30·56, 38·28 | ||||||||
| 18–23 | 27·1 | 22·51, 32·12 | 31·3 | 26·82, 36·06 | ||||||||
| Perceived birth size of baby | ||||||||||||
| Small | 25·9 | 22·57, 29·44 | 0·150 | 31·2 | 27·86, 34·69 | 0·771 | 36·7 | 31·04, 42·73 | 0·800 | 15·6 | 11·40, 20·88 | 0·272 |
| Average | 26·7 | 23·67, 29·87 | 32·6 | 29·64, 35·79 | 38·0 | 32·27, 44·11 | 20·7 | 16·25, 25·90 | ||||
| Large | 31·0 | 25·95, 36·55 | 32·6 | 27·97, 37·49 | 36·1 | 28·09, 44·93 | 20·8 | 14·98, 28·13 | ||||
| Place of delivery | ||||||||||||
| Home | 28·1 | 25·30, 31·01 | 0·464 | 26·2 | 23·70, 28·91 | <0·001 | 37·6 | 32·90, 42·52 | 0·630 | 22·7 | 18·70, 27·37 | 0·002 |
| Health facility | 26·2 | 23·09, 29·52 | 41·6 | 38·11, 45·14 | 36·5 | 30·76, 42·67 | 12·5 | 9·17, 16·89 | ||||
| Mode of delivery | ||||||||||||
| Non-Caesarean | 28·4 | 25·97, 30·85 | 0·001 | 30·6 | 28·44, 32·87 | <0·001 | 37·3 | 33·54, 41·23 | 0·730 | 19·8 | 16·69, 23·36 | 0·002 |
| Caesarean section | 17·0 | 12·34, 22·99 | 47·9 | 40·85, 55·04 | 35·2 | 23·26, 49·29 | 5·4 | 1·92, 14·18 | ||||
| Type of delivery assistance | ||||||||||||
| Health professional | 26·5 | 23·52, 29·76 | 0·745 | 40·4 | 36·77, 44·04 | <0·001 | 37·6 | 31·70, 43·93 | 0·330 | 12·7 | 9·27, 17·19 | 0·002 |
| Traditional birth attendant | 28·1 | 24·61, 31·97 | 30·5 | 27·17, 33·97 | 33·0 | 27·48, 38·97 | 25·5 | 20·27, 31·45 | ||||
| Other | 27·7 | 23·92, 31·81 | 23·1 | 19·76, 26·69 | 41·4 | 34·27, 48·83 | 19·2 | 14·00, 25·83 | ||||
| Antenatal clinic visits | ||||||||||||
| None | 28·4 | 24·86, 32·31 | 0·604 | 21·9 | 18·95, 25·24 | <0·001 | 40·4 | 34·34, 46·81 | 0·270 | 21·8 | 16·65, 27·89 | 0·249 |
| 1–3 | 27·4 | 24·15, 30·81 | 29·4 | 26·39, 32·65 | 37·3 | 31·81, 43·06 | 19·0 | 14·56, 24·29 | ||||
| ≥4 | 25·9 | 22·59, 29·60 | 46·2 | 42·39, 50·12 | 33·4 | 27·02, 40·37 | 15·2 | 10·85, 20·84 | ||||
| Timing of postnatal check-up | ||||||||||||
| Day 0–2 | 26·1 | 21·12, 31·66 | 0·860 | 37·2 | 31·11, 43·67 | <0·001 | 41·8 | 31·50, 52·80 | 0·790 | 13·0 | 7·59, 21·30 | 0·023 |
| Day 3–6 | 27·5 | 23·55, 31·84 | 43·8 | 39·49, 48·20 | 33·8 | 26·77, 41·70 | 11·7 | 7·63, 17·60 | ||||
| Day 7 or later | 21·8 | 12·61, 35·09 | 35·1 | 23·82, 48·34 | 35·3 | 18·12, 57·27 | 13·6 | 4·92, 32·53 | ||||
| Missing/no check-ups | 22·2 | 7·195, 51·28 | 59·0 | 33·83, 80·22 | 30·4 | 6·75, 72·50 | 32·2 | 5·23, 80·28 | ||||
| Household-level factors | ||||||||||||
| Household wealth index | ||||||||||||
| Poorest | 24·1 | 19·80, 29·05 | 0·421 | 18·1 | 14·59, 22·25 | <0·001 | 37·9 | 30·38, 46·07 | 0·130 | 27·6 | 21·04, 35·24 | 0·002 |
| Poorer | 26·9 | 22·42, 31·98 | 27·4 | 23·60, 31·65 | 43·3 | 35·80, 51·02 | 21·6 | 15·94, 28·48 | ||||
| Middle | 28·0 | 23·77, 32·70 | 31·1 | 26·86, 35·76 | 39·3 | 31·16, 48·09 | 11·2 | 6·82, 17·70 | ||||
| Richer | 30·7 | 25·96, 35·86 | 38·4 | 33·85, 43·20 | 34·4 | 26·70, 43·09 | 18·4 | 12·36, 26·53 | ||||
| Richest | 27·4 | 22·49, 32·92 | 50·0 | 45·08, 55·00 | 28·5 | 21·27, 36·92 | 12·6 | 7·774, 19·88 | ||||
| Community-level factors | ||||||||||||
| Residence | ||||||||||||
| Urban | 26·9 | 23·36, 30·78 | 0·807 | 40·5 | 36·61, 44·55 | <0·001 | 35·7 | 29·13, 42·91 | 0·640 | 13·4 | 9·31, 18·89 | 0·022 |
| Rural | 27·5 | 24·70, 30·49 | 28·5 | 26·07, 31·10 | 37·7 | 33·36, 42·27 | 21·1 | 17·47, 25·31 | ||||
| Geographical region (province) | ||||||||||||
| Punjab | 29·0 | 25·77, 32·38 | <0·001 | 38·3 | 35·07, 41·59 | <0·001 | 32·5 | 27·55, 37·88 | 0·001 | 19·7 | 15·46, 24·79 | 0·827 |
| Sindh | 17·6 | 14·43, 21·37 | 26·3 | 22·79, 30·11 | 37·2 | 30·59, 44·23 | 17·5 | 13·09, 22·92 | ||||
| North West Frontier | 34·2 | 28·36, 40·47 | 22·5 | 18·13, 27·57 | 55·2 | 46·39, 63·72 | 18·7 | 12·51, 26·95 | ||||
| Balochistan | 38·8 | 28·21, 50·47 | 19·0 | 14·36, 24·61 | 35·6 | 24·73, 48·14 | 14·1 | 5·42, 32·05 | ||||
*Divorced, separated and widowed.
Exclusive breast-feeding
EBF rates were significantly lower among working mothers (26·3 %, P = 0·010), mothers with a preceding birth interval of <15 months (22·8 %, P = 0·020) and mothers living in Punjab Province (32·5 %, P = 0·001; Table 3).
Bottle-feeding
The bottle-feeding rates were significantly higher among non-working women (33·6 %, P = 0·012) and those who were literate (43·7 %, P < 0·001), especially with secondary and higher education level (48·0 %, P < 0·001). Women who had four or more ANC visits (46·2 %, P < 0·001), delivered at a health facility (41·6 %, P < 0·001), delivered by a health professional (40·4 %, P < 0·001), who underwent a Caesarean section (47·9 %, P < 0·001) and who had no PNC (59·0 %, P < 0·001) had significantly higher bottle-feeding rates. Infants aged 6–11 months (36·8 %, P = 0·001), in the richest household wealth index quintile (50·0 %, P < 0·001), of urban residence (40·5 %, P < 0·001) and residing in Punjab Province (38·3 %, P < 0·001) also had significantly higher bottle-feeding rates (Table 3).
Predominant breast-feeding
PBF rates were significantly higher among mothers who had no education (21·9 %, P = 0·016) compared with those who had primary, secondary or higher education. PBF rates were also higher among women whose deliveries were assisted by traditional birth attendants (25·5 %, P = 0·002). Mothers from rural regions (21·1 %, P = 0·022) and those from the poorest households (27·6 %, P = 0·002) reported significantly higher PBF rates (Table 3).
Multivariate analyses
No timely initiation of breast-feeding
Working mothers (AOR = 1·48, 95 % CI 1·16, 1·87; P = 0·001), mothers who delivered by Caesarean section (AOR = 1·95, 95 % CI 1·30, 2·90; P = 0·001) and those residing in Sindh Province (AOR = 1·88, 95 % CI 1·40, 2·51; P < 0·001) had higher odds for no timely initiation of breast-feeding (Table 4).
Table 4.
Survey logistic modelling for no timely initiation of breast-feeding and bottle-feeding (unadjusted and adjusted odds ratios); secondary analysis of data from the Pakistan Demographic and Health Survey (PDHS) 2006–2007
| No timely initiation of breast-feeding (<24 months) | Bottle-feeding (< 24 months) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Unadjusted | Adjusted | Unadjusted | Adjusted | |||||||||
| Characteristic | OR | 95 % CI | P | OR | 95 % CI | P | OR | 95 % CI | P | OR | 95 % CI | P |
| Individual-level factors | ||||||||||||
| Maternal working status | ||||||||||||
| Non-working | 1·00 | 1·00 | 1·00 | |||||||||
| Working (past 12 months) | 1·58 | 1·25, 1·99 | <0·001 | 1·48 | 1·16, 1·87 | 0·001 | 0·74 | 0·58, 0·93 | 0·011 | |||
| Marital status | ||||||||||||
| Currently married | 1·00 | 1·00 | ||||||||||
| Formerly married* | 1·04 | 0·33, 3·27 | 0·952 | 1·05 | 0·34, 3·28 | 0·929 | ||||||
| Maternal education | ||||||||||||
| No education | 1·00 | 1·00 | ||||||||||
| Primary | 1·03 | 0·77, 1·37 | 0·856 | 1·91 | 1·48, 2·47 | <0·001 | ||||||
| Secondary or above | 0·96 | 0·75, 1·23 | 0·759 | 2·74 | 2·18, 3·44 | <0·001 | ||||||
| Literacy | ||||||||||||
| Cannot read at all | 1·00 | 1·00 | ||||||||||
| Able to read only passage | 0·95 | 0·77, 1·17 | 0·631 | 2·29 | 1·90, 2·77 | <0·001 | ||||||
| Partner's education | ||||||||||||
| No education | 1·00 | 1·00 | 1·00 | |||||||||
| Primary | 0·86 | 0·65, 1·13 | 0·266 | 1·35 | 1·02, 1·77 | 0·033 | 1·31 | 1·00, 1·74 | 0·054 | |||
| Secondary or above | 0·85 | 0·69, 1·04 | 0·120 | 1·71 | 1·38, 2·11 | <0·001 | 1·41 | 1·05, 1·89 | 0·023 | |||
| Mother's age (years) | ||||||||||||
| 15–19 | 1·00 | 1·00 | ||||||||||
| 20–34 | 1·13 | 0·77, 1·67 | 0·455 | 1·16 | 0·78, 1·73 | 0·455 | ||||||
| 35–49 | 1·16 | 0·74, 1·81 | 0·514 | 1·17 | 0·75, 1·82 | 0·490 | ||||||
| Birth order | ||||||||||||
| First-born | 1·00 | 1·00 | ||||||||||
| Second- to fourth-born | 0·90 | 0·71, 1·16 | 0·423 | 0·86 | 0·67, 1·11 | 0·238 | ||||||
| Fifth-born or higher | 0·79 | 0·61, 1·03 | 0·077 | 0·83 | 0·64, 1·07 | 0·152 | ||||||
| Preceding birth interval | ||||||||||||
| No previous birth | 1·00 | 1·00 | ||||||||||
| 0–14 months | 0·79 | 0·50, 1·23 | 0·293 | 1·03 | 0·69, 1·53 | 0·882 | ||||||
| 14–24 months | 0·90 | 0·67, 1·20 | 0·461 | 0·91 | 0·69, 1·22 | 0·538 | ||||||
| ≥25 months | 0·84 | 0·66, 1·07 | 0·163 | 0·80 | 0·62, 1·02 | 0·067 | ||||||
| Sex of baby | ||||||||||||
| Male | 1·00 | 1·00 | ||||||||||
| Female | 0·94 | 0·78, 1·13 | 0·497 | 0·94 | 0·78, 1·12 | 0·471 | ||||||
| Age of child (months) | 0·99 | 0·98, 1·00 | 0·159 | 1·02 | 1·01, 1·03 | 0·005 | 1·02 | 1·01, 1·03 | 0·006 | |||
| Perceived birth size of baby | ||||||||||||
| Average | 1·00 | 1·00 | ||||||||||
| Large | 0·81 | 0·61, 1·07 | 0·143 | 1·00 | 0·78, 1·28 | 0·975 | ||||||
| Small | 1·04 | 0·83, 1·31 | 0·722 | 0·93 | 0·76, 1·15 | 0·518 | ||||||
| Place of delivery | ||||||||||||
| Home | 1·00 | 1·00 | ||||||||||
| Health facility | 1·10 | 0·90, 1·34 | 0·350 | 2·00 | 1·65, 2·44 | <0·001 | ||||||
| Mode of delivery | ||||||||||||
| Non-Caesarean | 1·00 | 1·00 | 1·00 | |||||||||
| Caesarean section | 1·93 | 1·31, 2·84 | 0·001 | 1·95 | 1·30, 2·90 | 0·001 | 2·08 | 1·54, 2·81 | <0·001 | |||
| Type of delivery assistance | ||||||||||||
| Health professional | 1·00 | 1·00 | 1·00 | |||||||||
| Traditional birth attendant | 0·92 | 0·73, 1·16 | 0·486 | 0·65 | 0·52, 0·81 | <0·001 | 1·02 | 0·80, 1·31 | 0·863 | |||
| Other | 0·94 | 0·74, 1·20 | 0·629 | 0·44 | 0·35, 0·56 | <0·001 | 0·76 | 0·58, 0·99 | 0·039 | |||
| Antenatal clinic visits | ||||||||||||
| None | 1·00 | 1·00 | 1·00 | |||||||||
| 1–3 | 1·06 | 0·85, 1·32 | 0·632 | 1·48 | 1·19, 1·85 | <0·001 | 1·21 | 0·95, 1·53 | 0·115 | |||
| ≥4 | 1·13 | 0·89, 1·45 | 0·308 | 3·06 | 2·40, 3·90 | <0·001 | 1·93 | 1·46, 2·55 | <0·001 | |||
| Timing of postnatal check-up | ||||||||||||
| Immediate (hospital birth) | 1·00 | 1·00 | ||||||||||
| Day 0–2 | 0·93 | 0·67, 1·28 | 0·654 | 1·32 | 0·96, 1·81 | 0·091 | ||||||
| Day 3–6 | 1·26 | 0·62, 2·57 | 0·523 | 0·91 | 0·50, 1·67 | 0·771 | ||||||
| Day 7 or later | 1·23 | 0·32, 4·71 | 0·759 | 2·43 | 0·84, 7·04 | 0·101 | ||||||
| Household-level factors | ||||||||||||
| Household wealth index | ||||||||||||
| Poorest | 1·00 | 1·00 | 1·00 | |||||||||
| Poorer | 0·86 | 0·62, 1·21 | 0·386 | 1·71 | 1·25, 2·35 | 0·001 | 1·65 | 1·20, 2·28 | 0·002 | |||
| Middle | 0·82 | 0·59, 1·13 | 0·218 | 2·04 | 1·47, 2·84 | <0·001 | 1·55 | 1·09, 2·22 | 0·015 | |||
| Richer | 0·72 | 0·51, 1·01 | 0·057 | 2·82 | 2·05, 3·88 | <0·001 | 1·78 | 1·26, 2·51 | 0·001 | |||
| Richest | 0·84 | 0·58, 1·22 | 0·359 | 4·53 | 3·26, 6·30 | <0·001 | 2·41 | 1·62, 3·58 | <0·001 | |||
| Community-level factors | ||||||||||||
| Residence | ||||||||||||
| Rural | 1·00 | 1·00 | ||||||||||
| Urban | 1·03 | 0·81, 1·31 | 0·807 | 1·71 | 1·39, 2·10 | <0·001 | ||||||
| Geographical region (province) | ||||||||||||
| Punjab | 1·00 | 1·00 | 1·00 | 1·00 | ||||||||
| Sindh | 1·91 | 1·43, 2·54 | <0·001 | 1·88 | 1·40, 2·51 | <0·001 | 0·58 | 0·46, 0·73 | <0·001 | 0·60 | 0·48, 0·76 | <0·001 |
| North West Frontier | 0·79 | 0·57, 1·08 | 0·133 | 0·86 | 0·62, 1·18 | 0·347 | 0·47 | 0·35, 0·63 | <0·001 | 0·55 | 0·40, 0·75 | <0·001 |
| Balochistan | 0·64 | 0·39, 1·07 | 0·087 | 0·68 | 0·41, 1·14 | 0·143 | 0·38 | 0·26, 0·54 | <0·001 | 0·47 | 0·31, 0·71 | <0·001 |
*Divorced, separated and widowed.
Bottle-feeding
The odds of an infant being bottle-fed was higher when the father's education was secondary or above (AOR = 1·41, 95 % CI 1·05, 1·89; P = 0·023), with increasing age of the child (AOR = 1·02, 95 % CI 1·01, 1·03; P = 0·006) and for women who had four or more ANC visits (AOR = 1·93, 95 % CI 1·46, 2·55; P < 0·001). Compared with mothers from the poorest households, those belonging to the richest households (AOR = 2·41, 95 % CI 1·62, 3·58; P < 0·001) had higher odds of bottle-feeding their babies. Compared with Punjab Province, mothers who lived in other provinces were significantly less likely to bottle-feed their babies (all P < 0·001; Table 4).
Exclusive breast-feeding
Non-EBF was significantly more likely for working mothers (AOR = 1·76, 95 % CI 1·13, 2·75; P = 0·013), infants whose mothers belonged to the highest household wealth index quintile (AOR = 2·31, 95 % CI 1·22, 4·36; P = 0·010) and for mothers who lived in Punjab Province. As expected, increasing age of the infant was associated with significantly more non-EBF (AOR = 1·46, 95 % CI 1·32, 1·62; P < 0·001). Mothers who were able to read a passage of text were less likely not to breast-feed their babies exclusively (AOR = 0·64, 95 % CI 0·43, 0·96; P = 0·029) than mothers who were not able to read at all (Table 5).
Table 5.
Survey logistic modelling for not exclusively breast-feeding and predominant breast-feeding (unadjusted and adjusted odds ratios); secondary analysis of data from the Pakistan Demographic and Health Survey (PDHS) 2006–2007
| Not exclusively breast-feeding (<6 months) | Predominant breast-feeding (<6 months)* | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Unadjusted | Adjusted | Unadjusted | Adjusted | |||||||||
| Characteristic | OR | 95 % CI | P | OR | 95 % CI | P | OR | 95 % CI | P | OR | 95 % CI | P |
| Individual-level factors | ||||||||||||
| Maternal working status | ||||||||||||
| Non-working | 1·00 | 1·00 | 1·00 | |||||||||
| Working (past 12 months) | 1·80 | 1·18, 2·75 | 0·006 | 1·76 | 1·13, 2·57 | 0·013 | 2·17 | 1·27, 3·71 | 0·004 | |||
| Marital status | ||||||||||||
| Currently married | ||||||||||||
| Formerly married† | ||||||||||||
| Maternal education | ||||||||||||
| No education | 1·00 | 1·00 | ||||||||||
| Primary | 1·47 | 0·92, 2·34 | 0·109 | 0·65 | 0·34, 1·22 | 0·187 | ||||||
| Secondary or above | 1·29 | 0·91, 1·83 | 0·152 | 0·56 | 0·30, 1·04 | 0·068 | ||||||
| Literacy | ||||||||||||
| Cannot read at all | 1·00 | 1·00 | 1·00 | 1·00 | ||||||||
| Able to read only passage | 0·92 | 0·67, 1·28 | 0·638 | 0·64 | 0·43, 0·96 | 0·029 | 0·57 | 0·35, 0·92 | 0·024 | 0·58 | 0·35, 0·95 | 0·033 |
| Partner's education | ||||||||||||
| No education | 1·00 | 1·00 | ||||||||||
| Primary | 0·99 | 0·64, 1·53 | 0·955 | 1·58 | 0·87, 2·86 | 0·125 | ||||||
| Secondary or above | 1·06 | 0·70, 1·59 | 0·789 | 1·04 | 0·65, 1·64 | 0·862 | ||||||
| Mother's age (years) | ||||||||||||
| 15–19 | 1·00 | 1·00 | ||||||||||
| 20–34 | 0·89 | 0·53, 1·50 | 0·658 | 0·76 | 0·38, 1·49 | 0·427 | ||||||
| 35–49 | 0·87 | 0·46, 1·66 | 0·674 | 0·65 | 0·27, 1·53 | 0·326 | ||||||
| Birth order | ||||||||||||
| First-born | 1·00 | 1·00 | ||||||||||
| Second- to fourth-born | 1·00 | 0·67, 1·51 | 0·983 | 0·84 | 0·50, 1·41 | 0·524 | ||||||
| Fifth-born or higher | 0·66 | 0·42, 1·04 | 0·070 | 0·46 | 0·24, 0·85 | 0·013 | ||||||
| Preceding birth interval | ||||||||||||
| No previous birth | 1·00 | 1·00 | ||||||||||
| 0–14 months | 1·78 | 0·85, 3·73 | 0·127 | 1·35 | 0·53, 3·42 | 0·522 | ||||||
| 14–24 months | 1·16 | 0·69, 1·94 | 0·572 | 1·01 | 0·53, 1·91 | 0·973 | ||||||
| ≥25 months | 0·72 | 0·48, 1·08 | 0·116 | 0·55 | 0·33, 0·93 | 0·028 | ||||||
| Sex of baby | ||||||||||||
| Male | 1·00 | 1·00 | ||||||||||
| Female | 1·18 | 0·87, 1·60 | 0·276 | 1·15 | 0·74, 1·78 | 0·524 | ||||||
| Age of child (months) | 1·42 | 1·29, 1·57 | <0·001 | 1·46 | 1·32, 1·62 | <0·001 | 1·42 | 1·24, 1·63 | <0·001 | |||
| Perceived birth size of baby | ||||||||||||
| Average | 1·00 | 1·00 | ||||||||||
| Large | 1·09 | 0·70, 1·69 | 0·713 | 1·28 | 0·77, 2·13 | 0·339 | ||||||
| Small | 1·06 | 0·74, 1·52 | 0·758 | 0·35 | 0·74, 2·46 | 0·314 | ||||||
| Place of delivery | ||||||||||||
| Home | 1·00 | 1·00 | ||||||||||
| Health facility | 1·05 | 0·75, 1·46 | 0·784 | 0·56 | 0·35, 0·90 | 0·019 | ||||||
| Mode of delivery | ||||||||||||
| Non-Caesarean | 1·00 | 1·00 | ||||||||||
| Caesarean section | 1·10 | 0·60, 1·99 | 0·763 | 0·28 | 0·08, 0·94 | 0·039 | ||||||
| Type of delivery assistance | ||||||||||||
| Health professional | 1·00 | 1·00 | 1·00 | |||||||||
| Traditional birth attendant | 1·23 | 0·85, 1·78 | 0·282 | 2·28 | 1·39, 3·74 | 0·001 | 1·96 | 1·18, 3·24 | 0·009 | |||
| Other | 0·86 | 0·58, 1·26 | 0·429 | 1·37 | 0·79, 2·38 | 0·255 | 1·33 | 0·75, 2·34 | 0·324 | |||
| Antenatal clinic visits | ||||||||||||
| None | 1·00 | 1·00 | ||||||||||
| 1–3 | 1·14 | 0·82, 1·60 | 0·434 | 0·94 | 0·58, 1·51 | 0·814 | ||||||
| ≥4 | 1·36 | 0·92, 2·00 | 0·128 | 0·84 | 0·48, 1·47 | 0·556 | ||||||
| Timing of postnatal check-up | ||||||||||||
| Immediate (hospital birth) | 1·00 | 1·00 | ||||||||||
| Day 0–2 | 1·40 | 0·80, 2·45 | 0·235 | 1·11 | 0·49, 2·50 | 0·791 | ||||||
| Days 3–6 | 1·32 | 0·50, 3·50 | 0·580 | 1·24 | 0·31, 4·90 | 0·752 | ||||||
| Day 7 or later | 1·64 | 0·26, 9·53 | 0·600 | 3·40 | 0·26, 43·6 | 0·344 | ||||||
| Household-level factors | ||||||||||||
| Household wealth index | ||||||||||||
| Poorest | 1·00 | 1·00 | 1·00 | |||||||||
| Poorer | 0·80 | 0·51, 1·26 | 0·336 | 0·98 | 0·61, 1·58 | 0·943 | 0·68 | 0·39, 1·18 | 0·175 | |||
| Middle | 0·94 | 0·57, 1·55 | 0·817 | 1·07 | 0·62, 1·86 | 0·803 | 0·38 | 0·19, 0·77 | 0·007 | |||
| Richer | 1·16 | 0·71, 1·91 | 0·550 | 1·69 | 0·95, 3·00 | 0·072 | 0·73 | 0·38, 1·38 | 1·389 | |||
| Richest | 1·54 | 0·92, 2·56 | 0·101 | 2·31 | 1·22, 4·36 | 0·010 | 0·61 | 0·29, 1·24 | 1·246 | |||
| Community-level factors | ||||||||||||
| Residence | ||||||||||||
| Rural | 1·00 | 1·00 | ||||||||||
| Urban | 1·09 | 0·76, 1·56 | 0·640 | 1·49 | 0·88, 2·52 | 0·133 | ||||||
| Geographical region (province) | ||||||||||||
| Punjab | 1·00 | 1·00 | 1·00 | 1·00 | ||||||||
| Sindh | 0·81 | 0·56, 1·19 | 0·285 | 0·77 | 0·51, 1·16 | 0·204 | 0·77 | 0·46, 1·28 | 0·324 | 0·78 | 0·47, 1·28 | 0·331 |
| North West Frontier | 0·39 | 0·26, 0·60 | <0·001 | 0·37 | 0·23, 0·59 | <0·001 | 0·55 | 0·30, 1·01 | 0·055 | 0·54 | 0·29, 1·00 | 0·052 |
| Balochistan | 0·87 | 0·49, 1·54 | 0·637 | 0·69 | 0·37, 1·28 | 0·240 | 0·65 | 0·20, 2·12 | 0·480 | 0·58 | 0·17, 1·96 | 0·384 |
*Logistic model based on proportions of predominant (n 179) and exclusive breast-feeding (n 354).
†Divorced, separated and widowed.
Predominant breast-feeding
The practice of PBF was significantly less common in mothers who were literate (AOR = 0·58, 95 % CI 0·35, 0·95; P = 0·033). PBF had a higher odds ratio when the delivery was assisted by a traditional birth attendant (AOR = 1·96, 95 % CI 1·18, 3·24; P = 0·009) as compared with a qualified health professional (Table 5).
When compared with bottle-feeding (only children <6 months of age), working mothers were more significantly likely to predominantly breast-feed their babies (AOR = 2·26, 95 % CI 1·22, 4·18; P = 0·009). On the other hand, significantly lower rates of PBF were reported in mothers who were delivered at a health facility (AOR = 0·47, 95 % CI 0·27, 0·82; P = 0·009) and who delivered by Caesarean section (AOR = 0·19, 95 % CI 0·06, 0·65; P = 0·008).
Discussion
Pakistan has the lowest EBF rate, highest bottle-feeding rate but almost similar PBF compared with other countries in South Asia that have similar socio-economic conditions, such as Sri Lanka( 17 ), Bangladesh( 18 ), India( 19 ) and Nepal( 20 ). These rates of EBF, PBF and bottle-feeding are unacceptable and need improvement if Pakistan is to achieve the goals set out by WHO for optimal infant feeding practices. The present secondary data analysis has identified a number of associations with poor feeding practices which have programmatic implications for child health programmes in Pakistan; the more important ones are examined in the discussion below.
The rates of bottle-feeding were significantly higher among women who belonged to higher socio-economic strata with higher levels of education, reflecting the fact that educational status does not necessarily mean greater awareness of the importance of EBF. This trend could have a trickledown effect as these women potentially are role models to which less privileged women aspire. Also of concern was that those women who had four or more ANC visits, who delivered by health-care professionals and who delivered at health-care facilities had much higher bottle-feeding rates. This shows that women who had better contact with the health-care delivery system were less likely to practise EBF. This trend was seen in Nepal too, where increased antenatal visits had a negative effect on EBF; while in India more ANC visits had a positive effect on EBF( 21 , 22 ). In India women who were delivered at a health-care facility had a lower EBF rate whereas in Sri Lanka increased postnatal contacts with the health system improved the EBF rate( 22 , 23 ). The trend in Pakistan could be due to a lack of training of health-care workers in breast-feeding counselling.
Unfortunately, the attractive marketing strategies of manufacturers of formula milk as substitutes of mother's milk are not in line with the Legislation Ordinance on Breastfeeding issued by Government of Pakistan in 2002( 24 ); this was also shown in a study from Karachi where the majority (P < 0·0001) of doctors supported the idea of receiving gifts, promotional material and donations from the formula milk/feeding bottle manufacturers( 25 ). According to the study in Karachi more than 95 % of mothers considered that breast milk was the best food for their infant, but the practices of urban mothers were quite contradictory to this statement showing a gap between knowledge and practices. According to WHO, Iran was the first among Eastern Mediterranean countries to approve the WHO's international code of marketing on breast milk substitutes, adopt it as national law and implement all aspects of the code( 26 ), which explains the higher EBF and lower bottle-feeding rates in Iran compared with Pakistan. There is need to develop and implement guidelines for all levels of health-care workers on how to counsel mothers about the importance of EBF. The undergraduate medical syllabus in Pakistan needs revision and should include an essential standardized infant and young child feeding (IYCF) training package. It is important to revive the Baby Friendly Hospital Initiative (BFHI) to ensure that all children born in hospitals are put to the breast within the first hour of delivery, the rate of which is low (27·3 %) in Pakistan. All staff providing mother and child health services must also receive training in counselling about young infant feeding and nutrition. A system of close monitoring and evaluation should be put in place for the continuing accreditation of health facilities offering obstetric and child health services. This should also include the institutions operating in the private health sector. Furthermore, EBF rates in Pakistan could also be increased through community health workers (lady health workers)( 27 ) by providing counselling to women during antenatal, natal and postnatal home visits, as the majority of deliveries in Pakistan take place at home. A clinical trial has demonstrated a positive effect of home visiting by registered midwives on improving EBF rate( 28 ).
Achieving increased frequency of EBF requires behaviour change in mothers and other members of the family who influence decision making. Accomplishing behaviour change could be a formidable target, as multiple behaviour changes might be required in mothers who are bottle-feeding or non-EBF. On the other hand, a single behaviour change which aims at convincing ‘at risk’ women not to give water and other non-nutritious liquids may be a feasible achievement. Demographic and Health Survey data from Pakistan show that the profile of mothers who predominantly breast-feed and those who non-exclusively breast-feed are similar, as both are being practised more by illiterate mothers. This finding has programmatic implications. Since the target population for a behaviour change campaign is same it might be easier to develop public health messages which effectively highlight the disadvantages of giving water and water-based liquids before 6 months of age. This would have the potential of significantly increasing the rate of EBF with its attendant benefits. Such changes have been achieved by programmes in Cambodia( 29 , 30 ) where the EBF rates were increased from 11 % to 60 % in five years by targeting mothers practising PBF. Similar programmes in Zambia and Ghana have also produced positive changes in the behaviour of mothers, thereby increasing EBF rates( 31 ).
Another factor having an adverse association with EBF was urban residence as these women were more likely to bottle-feed their babies, a finding which is similar to Sri Lanka( 23 ). In Bangladesh urban mothers did not initiate timely breast-feeding for their infants( 32 ). This paradox could be utilized to the advantage of breast-feeding advocacy programmes, since urban mothers have a much better access to various sources of information that can be used to create awareness regarding the benefits of breast-feeding.
The present secondary analysis also highlighted significantly lower rates of EBF among working mothers. The current legislation in Pakistan for maternity leave and infrastructure to facilitate working women in breast-feeding is not supportive of EBF practices( 24 ). Most workplaces neither have space nor any system of support in place for mothers who want to breast-feed at their place of work. Studies from Iran show that giving a 1 h break daily to mothers for breast-feeding and also facilitating them in the practice have increased the EBF rates( 33 ). National paediatric associations and other similar organizations have an important role as pressure groups to influence parliamentarians to legislate for breast-feeding friendly policies in workplaces. Efforts must be made to ensure there is a breast-feeding friendly environment in both public and private sector workplaces.
The large geographic variation in EBF, with low rates in Punjab Province and high rates in North West Frontier Province, may need further study as the current analysis did not allow us to explore the behavioural, environmental and social factors affecting mothers’ decisions regarding infant feeding practices. Some common factors such as changing lifestyles, aggressive promotion of formula milk, a general unawareness of the importance of breast-feeding and perceived insufficiency of milk could play important roles in contributing towards suboptimal feeding practices. In women delivered through Caesarean section there is a perceived insufficiency of milk contributing towards high bottle-feeding rate, which is a common finding in India, Nepal, Sri Lanka and China where it was the main reason for delayed contact( 21 , 34 – 36 ). This perceived insufficiency was also found to be the most common cause for discontinuing breast-feeding of children in Australia( 37 ).
The main strengths of our study are the nationally representative sample, the comprehensive data on standard infant feeding indicators and the appropriate adjustments for sampling design made in the analysis. However, the major limitation is the 24 h recall method used for estimating EBF rates in the current survey. Although this method is recommended by WHO, there is a concern that it considerably overestimates EBF rates as it excludes children who were given liquids and foods at infrequent intervals( 38 – 43 ). In Sri Lanka the EBF rate was reported as 77·4 % by using ‘24 h recall’ and as 49·1 % by another method of ‘recall since birth’( 44 ). Therefore, it is quite possible that the EBF rates in Pakistan might be even lower than the levels estimated in the current analysis.
Conclusions
The EBF rates in Pakistan are the lowest and the bottle-feeding rates are the highest in South Asia. This should be considered as a wakeup call for child health programmes to focus more on improved infant feeding practices, especially EBF. There is an urgent need to involve all national programmes delivering child health interventions at all levels of health-care infrastructure. There should be enhanced training of health-care providers in infant and young child nutritional counselling. There is a need for breast-feeding friendly laws and their effective implementation to improve the rates of EBF in Pakistan. The advocacy campaigns should focus on all women of childbearing age at all levels of society, with special emphasis on educated, working women from upper socio-economic strata.
Acknowledgements
The study was supported by AusAID through the Public Sector Linkages Program. No author has any conflict of interest on the content of this manuscript. T.H., Y.B.N., N.K. and S.A. designed the study, obtained data sets, guided analysis and wrote the manuscript. T.H., Y.B.N., N.K., D.-S.A. and A.M.K. obtained the literature, checked results and reviewed and revised the manuscript. K.E.A. wrote the results section and interpreted results. K.E.A. and S.A. converted data files, conducted statistical analyses and compiled the results tables. M.J.D. conceptualized the research question, designed and guided the analysis and edited the manuscript. The National Institute of Population Studies of Pakistan carried out the PDHS 2006–2007 for the Health Sector Development Project of the Ministry of Health. A fellowship sponsored by the Australian Leadership Awards (ALA) scheme and a workshop funded by the Public Sector Linkages Program (PSLP) of the AusAID facilitated the data analysis and writing. Dr Upal Senarath, Principal Investigator SAIFRN Sri Lanka Chapter, provided the technical support.
References
- 1. Dewey K, Heinig MJ & Nommsen-Rivers L (1995) Differences in morbidity between breast-fed and formula-fed infants. J Pediatr 126, 696–702. [DOI] [PubMed] [Google Scholar]
- 2. Leung A & Sauve R (2005) Breast is best for babies. J Natl Med Assoc 97, 1010–1019. [PMC free article] [PubMed] [Google Scholar]
- 3. Wright AL, Holberg CJ, Martinez FD et al. (1989) Breast feeding and lower respiratory tract illness in the first year of life. Group Health Medical Associates. BMJ 299, 946–949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bahl R, Frost C, Kirkwood BR et al. (2005) Infant feeding patterns and risks of death and hospitalization in the first half of infancy: multicentre cohort study. Bull World Health Organ 83, 418–426. [PMC free article] [PubMed] [Google Scholar]
- 5. Howie PW, Forsyth JS, Ogston SA et al. (1990) Protective effect of breast feeding against infection. BMJ 300, 11–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Arifeen S, Black RE, Antelman G et al. (2001) Exclusive breastfeeding reduces acute respiratory infection and diarrhea deaths among infants in Dhaka slums. Pediatrics 108, E67. [DOI] [PubMed] [Google Scholar]
- 7. World Health Organization (2002) Infant and Young Child Nutrition; Global Strategy on Infant and Young Child Feeding. Resolution WHA55/15. Geneva: WHO. [Google Scholar]
- 8. Black RE, Allen LH, Bhutta ZA et al. (2008) Maternal and child undernutrition: global and regional exposures and health consequences. Lancet 371, 243–260. [DOI] [PubMed] [Google Scholar]
- 9. Jones G, Steketee RW, Black RE et al. (2003) How many child deaths can we prevent this year? Lancet 362, 65–71. [DOI] [PubMed] [Google Scholar]
- 10. World Health Organization (2002) Infant and Young Child Nutrition; Global Strategy on Infant and Young Child Feeding. Report no. A55/15. Geneva: WHO. [Google Scholar]
- 11. Oddy WH, Sly PD, de Klerk NH et al. (2003) Breast feeding and respiratory morbidity in infancy: a birth cohort study. Arch Dis Child 88, 224–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Temboury MC, Otero A, Polanco I et al. (1994) Influence of breast-feeding on the infant's intellectual development. J Pediatr Gastroenterol Nutr 18, 32–36. [DOI] [PubMed] [Google Scholar]
- 13. Government of Pakistan (2005) Pakistan Economic Survey. Islamabad: Government of Pakistan. [Google Scholar]
- 14. National Institute of Population Studies & Macro International Inc. (2008) Pakistan Demographic and Health Survey 2006–07. Islamabad/Calverton, MD: NIPS/Macro International Inc. [Google Scholar]
- 15. World Health Organization (2008) Indicators for Assessing Infant and Young Child Feeding Practices. Washington, DC: WHO. [Google Scholar]
- 16. Filmer D & Pritchett LH (2001) Estimating wealth effects without expenditure data – or tears: an application to educational enrolments in states of India. Demography 38, 115–132. [DOI] [PubMed] [Google Scholar]
- 17. Department of Census and Statistics Sri Lanka (2000) Sri Lanka Demographic and Health Survey 2000. Colombo: Department of Census and Statistics Sri Lanka. [Google Scholar]
- 18. National Institute of Population Research and Training, Mitra and Associates & ORC Macro (2001) Bangladesh Demographic and Health Survey 2000. Dhaka/Calverton, MD: National Institute of Population Research and Training, Mitra and Associates/ORC Macro. [Google Scholar]
- 19. International Institute for Population Sciences & ORC Macro (2000) National Family Health Survey (NFHS-2), 1998–99, India. Mumbai: IIPS. [Google Scholar]
- 20. Ministry of Health Nepal, New ERA & ORC Macro (2002) Nepal Demographic and Health Survey 2001. Kathmandu/Calverton, MD: Family Health Division, Ministry of Health, New ERA/ORC Macro. [Google Scholar]
- 21. Pandey S, Tiwari K, Senarath U et al. (2010) Determinants of infant and young child feeding practices in Nepal: secondary data analysis of Demographic and Health Survey 2006. Food Nutr Bull 31, 334–351. [DOI] [PubMed] [Google Scholar]
- 22. Patel A, Badhoniya N, Khadse S et al. (2010) Infant and young child feeding indicators and determinants of poor feeding practices in India: secondary data analysis of National Family Health Survey 2005–06. Food Nutr Bull 31, 314–333. [DOI] [PubMed] [Google Scholar]
- 23. Senarath U, Dibley MJ, Godakandage SS et al. (2010) Determinants of infant and young child feeding practices in Sri Lanka: secondary data analysis of Demographic and Health Survey 2000. Food Nutr Bull 31, 352–365. [DOI] [PubMed] [Google Scholar]
- 24. Government of Pakistan (2002) The Protection of Breast Feeding and Child Nutrition Ordinance. The Gazette of Pakistan. http://www.thenetwork.org.pk/Resources/Legislations/PDF/12-8-2011-0-51-50-603-Legislation%20ordinance%20on%20breastfeeding.pdf (accessed May 2011). [Google Scholar]
- 25. Hanif R, Khalil E, Sheikh A et al. (2008) Knowledge about breastfeeding in accordance with the national policy among doctors, paramedics and mothers in baby-friendly hospitals. J Pak Med Assoc 60, 881–886. [PubMed] [Google Scholar]
- 26. World Health Organization (2006) Breast feeding breakthroughs. http:/www.unicef.org/sowc98/panel13.htm (accessed January 2011).
- 27. Nisar YB (2008) Corrections needed to Pakistani programme details. Bull World Health Organ 86, B. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Bashour HN, Kharouf MH, Abdul Salam AA et al. (2008) Effect of postnatal home visits on maternal/infant outcomes in Syria: a randomized controlled trial. Public Health Nurs 25, 115–125. [DOI] [PubMed] [Google Scholar]
- 29. Anonymous (2002) Cambodia 2000: results from the Demographic and Health Survey. Stud Fam Plann 33, 269–273. [DOI] [PubMed] [Google Scholar]
- 30. Islam MM, Khatun M, Peerson JM et al. (2008) Effects of energy density and feeding frequency of complementary foods on total daily energy intakes and consumption of breast milk by healthy breastfed Bangladeshi children. Am J Clin Nutr 88, 84–94. [DOI] [PubMed] [Google Scholar]
- 31. Mangasaryan N (2010) Effective Strategies to Improve Infant and Young Child Feeding. Managua: UNICEF. [Google Scholar]
- 32. Mihrshahi S, Kabir I, Roy SK et al. (2010) Determinants of infant and young child feeding practices in Bangladesh: secondary data analysis of Demographic and Health Survey 2004. Food Nutr Bull 31, 295–313. [DOI] [PubMed] [Google Scholar]
- 33. Zareai M, O'Brien ML & Fallon AB (2007) Creating a breastfeeding culture: a comparison of breastfeeding practises in Australia and Iran. Breastfeed Rev 15, 15–20. [PubMed] [Google Scholar]
- 34. Patel A, Badhoniya N, Khadse S et al. (2010) Infant and young child feeding indicators and determinants of poor feeding practices in India: secondary data analysis of National Family Health Survey 2005–06. Food Nutr Bull 31, 314–333. [DOI] [PubMed] [Google Scholar]
- 35. Senarath U, Siriwardena I, Godakandage SS et al. (2012) Determinants of breastfeeding practices: an analysis of the Sri Lanka Demographic and Health Survey 2006–2007. Matern Child Nutr 8, 315–329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Zhao Y, Niu AM, Xu GF et al. (2003) Early infant feeding practices in Jinan City, Shandong Province, China. Asia Pac J Clin Nutr 12, 104–108. [PubMed] [Google Scholar]
- 37. Australian Bureau of Statistics (2003) Breastfeeding in Australia. http://www.abs.gov.au/ausstats/abs@.nsf/mf/4810.0.55.001 (accessed May 2011).
- 38. Webb K, Marks GC, Lund-Adams M et al. (2001) Towards A National System For Monitoring Breastfeeding in Australia: Recommendations For Population Indicators, Definitions and Next Steps. Canberra: Commonwealth of Australia. [Google Scholar]
- 39. Piwoz EG, Creed de Kanashiro H, Lopez de Romana G et al. (1995) Potential for misclassification of infants’ usual feeding practices using 24-hour dietary assessment methods. J Nutr 125, 57–65. [DOI] [PubMed] [Google Scholar]
- 40. Zohoori N, Popkin BM & Fernandez ME (1993) Breast-feeding patterns in the Philippines: a prospective analysis. J Biosoc Sci 25, 127–138. [DOI] [PubMed] [Google Scholar]
- 41. Aarts C, Kylberg E, Hornell A et al. (2000) How exclusive is exclusive breastfeeding? A comparison of data since birth with current status data. Int J Epidemiol 29, 1041–1046. [DOI] [PubMed] [Google Scholar]
- 42. Ssenyonga R, Muwonge R & Nankya I (2004) Towards a better understanding of exclusive breastfeeding in the era of HIV/AIDS: a study of prevalence and factors associated with exclusive breastfeeding from birth, in Rakai, Uganda. J Trop Pediatr 50, 348–353. [DOI] [PubMed] [Google Scholar]
- 43. Engebretsen IM, Wamani H, Karamagi C et al. (2007) Low adherence to exclusive breastfeeding in Eastern Uganda: a community-based cross-sectional study comparing dietary recall since birth with 24-hour recall. BMC Pediatr 7, 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Agampodi SB, Fernando S & Dharmaratne SD (2009) Comparison of definitions used for exclusive breast feeding – the Labbock's strict definition and the WHO definition as methods of estimating exclusive breastfeeding rates in Sri Lanka. Ceylon Med J 54, 20. [Google Scholar]