Abstract
Older age is reportedly protective against the detrimental psychological impacts of the COVID-19 pandemic, consistent with the theory that reduced future time extension (FTE) leads to prioritization of socioemotional well-being. We investigated whether depression severity and pandemic-related factors (regional severity, threat, social isolation) reduce FTE beyond chronological age and whether these relationships differ between younger and older adults. In May 2020, we recruited 248 adults (younger: 18–43 years, older: 55–80 years) from 13 industrialized nations. Multigroup path analysis found that depression severity was a better predictor of FTE than the reverse association in both age groups, suggesting an affective foreshortening of future time. In both age groups, older age was protective against depression severity, and younger age was associated with heightened vulnerability to the negative impacts of pandemic-related factors. Future research should consider the complex interrelationships between FTE, age, and depression severity and the potential impacts of the broader psychosocial milieu.
Keywords: aging, COVID-19, depression, future thinking, future time perspective, isolation, open data
The COVID-19 pandemic has seen much of the world’s population endure multiple lockdowns in relative social isolation along with the unpredictable threat of the coronavirus. Impacts on mental health have been profound (Holmes et al., 2020). Although older adults have undoubtedly been affected (Lebrasseur et al., 2021; Rodrigues et al., 2022; Rutland-Lawes et al., 2021), some studies report they have coped better than younger adults (Carstensen et al., 2020; Fields et al., 2022; Parlapani et al., 2021; Sun & Sauter, 2021), consistent with findings that emotional well-being improves with age because decreasing future time horizons led to prioritization of socioemotional well-being (socioemotional selectivity theory [SST]; Lang & Carstensen, 2002). The possibility that depression contributes to time horizons in a way that promotes negative well-being is rarely considered in the SST literature. Given numerous anecdotal and scientific reports of distorted time perception during the pandemic (Martinelli et al., 2021; Ogden, 2020, 2021), the current study addressed this important question in an international sample of adults from two phases of the adult life span, early in the COVID-19 pandemic (May 2020).
Temporal horizons are ubiquitous in human experience; our integration of past and future influences our present-moment behavior (Lewin, 1942). Although the experience of psychological time is a fairly stable individual difference (Zimbardo & Boyd, 1999), it also changes dynamically with situational and psychological factors, such as time constraints (Gable & Poole, 2012). It is likely that disruption to short-term time constraints contributed to the perceived slowing of time experienced during the first COVID-19 lockdowns, along with older age, depression, and social dissatisfaction (Ogden, 2020).
The pandemic may have also affected aspects of longer-term future time, such as the perception of one’s remaining time (future time extension [FTE]; Liao & Carstensen, 2018). Although invariably linked to chronological age, salience of one’s mortality (e.g., a life-threatening disease) can elicit a foreshortening of future time that overrides the potentially protective effects of chronological age (Baldensperger et al., 2018; Sullivan-Singh et al., 2015). Although during a pandemic, the threat to life expectancy remains largely hypothetical (unless one is infected), the threat of contracting COVID-19 may nevertheless cause a similar foreshortening of future time. Indeed, Cheung et al. (2003, cited in Fung & Carstensen, 2006) reported this effect during the Hong Kong severe acute respiratory syndrome (SARS) outbreak of 2003. Thus, we expected that during the COVID-19 pandemic, future time horizons would scale with perceived personal threat (e.g., individual risk factors for SARS-CoV-2, being an essential worker) and the severity of the COVID-19 outbreak in one’s locale. Although older adults likely experience a higher degree of threat given most risk factors relate to health status (Carstensen et al., 2020), they may cope better with the potential threat than younger adults, and thus the impacts on FTE may differ across the life span.
FTE can also be affected by less dangerous factors, particularly those emphasizing anticipated social endings (Fredrickson & Carstensen, 1990). Notably, incarceration—which bears some similarities to lockdowns, including reduced social support—is associated with an apparent suspension of time. Studies report that prison inmates with longer sentences are more present oriented and view the future negatively, whereas inmates with social support are more positive about their futures (Carvalho et al., 2018). Social support can also offset the foreshortening effects of terminal illness on FTE (Baldensperger et al., 2018).
Future time horizons have complex associations with mental health; the evidence as to whether shorter or longer time horizons are related to good affective outcomes is mixed and may be related to age. In younger adults, orientation toward both the near and more distant future can predict better outcomes. For instance, focus on shorter-term goals is predictive of lower depressive symptoms and better well-being (Gamble et al., 2021), whereas longer future time horizons contribute to self-continuity and ongoing motivation (Lens et al., 2012) critical for optimal psychological functioning (Chandler & Lalonde, 1998). However, in older adults, shorter FTE is inherently motivational: Anticipation of social endings increases pursuit of meaningful goals and enhances well-being (Lang & Carstensen, 2002). Indeed, substantive literature shows that as FTE decreases in older age, so do negative emotions, whereas positive emotions increase (Carstensen et al., 2000, 2011). This age-related positivity persisted into the first wave of the pandemic (Carstensen et al., 2020; Fields et al., 2022), although these findings may be specific to the United States (see Rutland-Lawes et al., 2021).
Statement of Relevance.
The COVID-19 pandemic has forced people to contend with unprecedented disruptions to everyday life. Unsurprisingly, impacts on mental health have been profound, particularly in younger adults, but other aspects of psychological function have also been affected, such as the perception of time. This research investigated how the perception of future time beyond the pandemic relates to depression severity across two phases of the adult life span. We found that in both younger and older adults, more severe depression was linked to the perception of having less time left, providing evidence that irrespective of age, negative mood states can foreshorten our future time horizons. We found that depression was more severe in younger adults and was heightened by the severity of the pandemic situation, personal threat of COVID-19, and loneliness. This finding further highlights the resilience that comes with older age and the need to support younger adults beyond the COVID-19 pandemic.
Taken together, these results suggest that the relation of future time horizons and affective experience may vary across different phases of the adult life span, although to our knowledge this has not been directly tested. This variance likely reflects, at least in part, movement though life’s changes and transitions, where at times, present- and near-future thinking is more beneficial than focusing on the distant future and vice versa (Lens et al., 2012). Moreover, it may reflect the varying importance of different dimensions of future time perspective (of which FTE is only one; Rohr et al., 2017) at different life phases and across different studies.
In addition to life phase, it is also possible that the relation of FTE and affective outcomes is different for subgroups of the population experiencing mental health conditions. Few studies have directly explored the possibility of the reverse directional relationship, whereby negative emotional states predict lower FTE. There is, however, some evidence suggesting that psychological distress predicts an affective foreshortening of future time—not only following traumatic experiences that disrupt self-continuity (Holman & Grisham, 2020) but also in depression (Coudin & Lima, 2011; Kooij et al., 2018; McKay et al., 2016), in line with impairments of other forms of future thinking (for meta-analyses, see Gamble et al., 2019; Hallford et al., 2018). The pandemic’s disruption of future hopes and plans (e.g., graduations, weddings) has been salient for younger adults (Holman & Grisham, 2020); thus we expect depression-related foreshortenings to be particularly evident in younger adults. Although still undetermined, older adults may likewise experience similar issues resulting from the pandemic’s impact on their important socioemotional goals (e.g., time with family), although whether these effects will be evident over and above age-related decreases in FTE or increases in positivity is an open question.
Together, the findings reviewed here suggest that independently of an expected reduction of FTE with increasing chronological age, pandemic-related factors such as regional severity, threat of a potentially fatal illness, social isolation, and the severity of depression may all act to foreshorten one’s perceived future time horizon. In May 2020, we recruited younger and older adults from 13 industrialized nations across Australasia, Europe, and North America; the international nature of the sample provided variance in real-time pandemic severity statistics, perceived threat, and reported days in isolation (see the Method section). Here, we report path analyses examining the contributions of these pandemic-related factors and chronological age to depressive symptoms and FTE, as well as the directionality of the relationship between depressive symptoms and FTE. Given the possibility that these effects are not uniform across the life span, we constructed a multigroup path analysis that included two demographically matched age groups: younger (18–43 years) and older (55–80 years) adults. Each group’s 25-year age span enabled us to include chronological age in the multigroup path analysis and, critically, to assess whether chronological age effects differed between these two phases of the adult life span.
Open Practices Statement
The data and code from these age-group analyses have been made publicly available at OSF and can be accessed at https://doi.org/10.17605/OSF.IO/3U587. The materials and preregistered study protocol are publicly available at https://doi.org/10.17605/OSF.IO/7X9TQ; note that the specific analyses reported in this article were not preregistered.
Method
Participants
A power analysis was conducted using the findRMSEAsamplesize() function of the semTools package (Jorgensen et al., 2021) to determine the minimum sample size required to achieve a power of .80. When a multigroup path analysis with two groups and 18 degrees of freedom is constructed (parameters based on hypothesized models; Fig. 1), a total sample size of 236 would be required to determine close fit (null root-mean-square error of approximation [RMSEA] = .03; alternative RMSEA = .08). This study used data from 248 participants drawn from the first time point (May 6–25, 2020) of a larger longitudinal study (Thinking Beyond COVID-19; https://doi.org/10.17605/OSF.IO/7X9TQ). English-speaking participants were recruited to participate in the “entry survey” via online advertisements on social media and research participation websites (offering an entry into a prize drawing for a $150 CAD gift card) or via Prolific.co (offering payment at a rate of £5 per hour). General inclusion criteria were an age of 18 years or older and no history of neurological impairments or learning disabilities that could impact performance. Using Prolific’s built-in inclusion/exclusion function, we made the study available only to individuals who met these inclusion criteria. Although this was primarily a convenience sample, we did target recruitment of Prolific participants older than 55 years in line with our study aims, as well as those residing in countries particularly affected early in the pandemic (e.g., United States/Canada, United Kingdom, France, Italy, Spain). To increase the representativeness of our sample, we also targeted recruitment of participants belonging to minority ethnic groups. This project was approved by the Research Ethics Board of Baycrest Health Sciences, and participants provided informed and explicit consent before starting the survey.
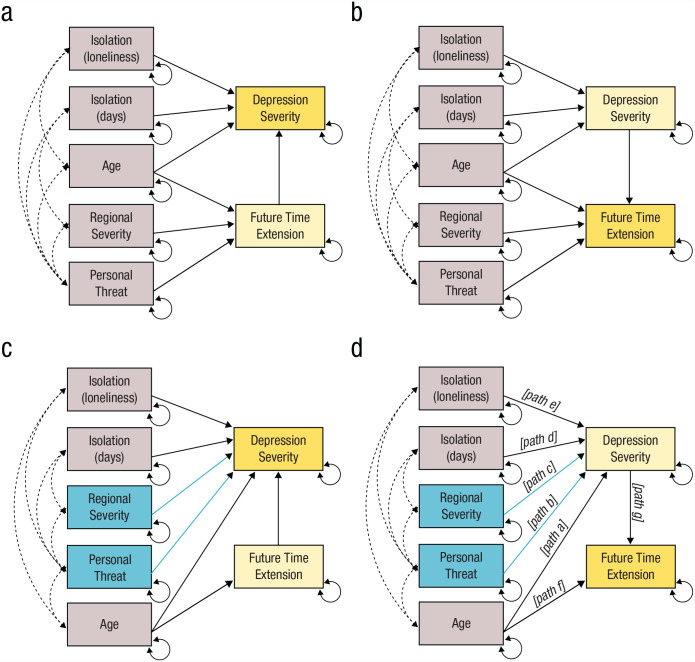
Fig. 1.
Path diagrams of models specified as hypothesized and respecified following optimization. In all models, single-headed arrows represent regression paths and their directionality, dashed double-headed arrows represent correlated error terms, and solid double-headed arrows indicate residual error. Variables on the left-hand side of each model (gray/blue) are exogenous predictors. Variables on the right-hand side are both endogenous and exogenous (light yellow) or fully endogenous (dark yellow). The hypothesized (a) depression-severity model (the Patient Health Questionnaire [PHQ] model) and (b) future time extension (FTE) model included paths from regional severity and personal threat to FTE; chronological age was thought to predict both FTE and depression severity (PHQ), and the two isolation indices were modeled as predictors of depression severity. The PHQ and FTE models were respecified (c and d, respectively) so that regional severity and personal threat predicted depression severity (blue paths). Path labels have been added in (d) for clarity.
Of the 1,060 individuals who consented to the larger study, 327 participants decided to withdraw during the initial open-ended narrative questions 1 and thus did not complete the questionnaires required for this study; thus, these participants were excluded. Of the 733 data sets collected, 53 were excluded for the following reasons: (a) responses on medical history items indicating that they did not meet inclusion criteria (n = 35), (b) being from geographical regions with very low participation rates (n = 9) or from a country employing a herd immunity strategy in May 2020 (n = 1), and (c) data cleaning, where we excluded participants who completed less than 33% of the survey, completed the 30-min survey in less than 10 min, or failed the attention-check item and provided inadequate written responses on other survey questions not reported in this study (n = 8; for more information, see https://doi.org/10.17605/OSF.IO/7X9TQ). The remaining 680 data sets comprised the full sample. Briefly, participants represented 25 countries, 61% were female, ages ranged from 18 to 80 years (M = 36.70, SD = 15.27), and 70% were recruited via online advertising and Prolific.co; for detailed demographics of the full sample, see https://doi.org/10.17605/OSF.IO/7X9TQ.
In the full Thinking Beyond COVID-19 sample, there were 144 participants aged between 55 and 80 years old; 124 had no missing data on any relevant measures and thus comprised the older adult group. We then identified 124 younger adults within a 25-year age span (18–43 years old) with complete data who matched the older adult participants as closely as possible in terms of country of residence and sex (see Table 1 for demographics; for more information on matching, see Section S1 in the Supplemental Material available online).
Table 1.
Demographic Statistics of Younger and Older Adult Groups
| Variable and category | Younger adults (n = 124) |
Older adults (n = 124) |
|---|---|---|
| Recruitment source (n) | ||
| Online advertising | 29 | 31 |
| Prolific.co | 95 | 93 |
| Age (years) | ||
| M | 29.17 | 60.59 |
| SD | 6.42 | 5.42 |
| Range | 18–43 | 55–80 |
| Sex (n) | ||
| Female | 94 | 95 |
| Male | 30 | 29 |
| Countries represented in sample (n) a | 13 | 12 |
| Self-reported ethnicity (n) b | ||
| Arab | 0 | 0 |
| Asian | 19 | 1 |
| Black | 5 | 1 |
| Latin American | 4 | 0 |
| Ma-ori/Pacific Islander | 1 | 0 |
| North American Indigenous | 1 | 0 |
| White | 96 | 122 |
| Other | 5 | 3 |
| Highest level of education (n) | ||
| No schooling | 0 | 0 |
| Primary | 1 | 0 |
| Secondary | 33 | 35 |
| University c | 65 | 63 |
| Graduate or postgraduate | 25 | 26 |
For the breakdown of the subsamples by country of residence, see Table S1 in the Supplemental Material available online. bBecause participants could select more than one ethnicity, the sum of the ethnic group ns is larger than the n for the survey. cThis category included undergraduate or similar program at a tertiary education institution.
Materials
Only measures relevant to addressing the current research questions are described here. These measures were collected as part of a 30-min survey conducted using the Qualtrics platform (the full list of measures collected is available at https://doi.org/10.17605/OSF.IO/7X9TQ).
Demographic and pandemic-related variables
Demographics and medical history
Participants reported their age, sex, ethnicity, country of residence at the time of testing, and highest level of education attained. To confirm that participants met the inclusion criteria of being free of neurological conditions and learning disabilities, we included a medical checklist. Participants responded “yes” or “no” to items including alcohol or drug abuse disorder, dementia, epilepsy, head injury, learning disorder, neurosurgery, psychotic disorder, stroke, or any decline in cognitive function. Participants who endorsed any of these items were subsequently excluded.
COVID-19 risk factors and concern
Participants completed another series of questions about professional and medical factors that, early in the pandemic (May 2020), had been identified as likely increasing one’s risk of contracting COVID-19 and/or the propensity for severe complications. Risk factors were status as an essential worker, cancer (including history of cancer), current smoker or vaper, condition or disease affecting a major organ (heart, lung, liver, or kidneys), diabetes or hyperglycemia, hypertension, and/or immunodeficiency (e.g., HIV/AIDS, leukemia). Participants responded “yes” or “no” (scored 1 and 0, respectively) to each risk factor; total COVID-19 risk was calculated as the sum of all risk factors. Participants indicated their level of concern that COVID-19 would affect them personally on a single item (0 = not at all concerned, 4 = very concerned).
Social isolation and loneliness
Participants reported the number of days they had spent in isolation since COVID-19 was first declared a pandemic on March 11, 2020. They also indicated the number of people living in their household, which was converted to a binary variable (1 = living alone, 0 = living with people). A single item was used to probe feelings of loneliness experienced over the past 2 weeks (0 = not at all, 3 = nearly every day).
Questionnaires
The Patient Health Questionnaire (PHQ; Kroenke et al., 2001) has nine items that measure the frequency with which participants have experienced symptoms of depression over the past 2 weeks; responses are made on a 4-point scale (0 = not at all, 3 = nearly every day). Responses are summed, and higher scores reflect higher severity of depression. Internal consistency of the measure was high (Cronbach’s α = .88, McDonald’s ω = .88).
The Future Time Perspective Scale (Lang & Carstensen, 2002) has 10 items that measure the participant’s perception of the future as being limited in time. Participants rate how true each statement is for them personally (1 = very untrue, 7 = very true). Higher scores represent a more expansive view of the future, whereas lower scores represent feelings of time as limited or constrained. Subscale scores for FTE, future time opportunity (FTO), and future time constraint (FTC) were calculated by averaging the score for items in each subscale (Rohr et al., 2017). In this study, we were interested in FTE specifically. Internal consistency across both the full measure and the FTE subscale was moderate to high (full scale: α = .87, ω = .87; FTE subscale: α = .74, ω = .74).
COVID-19 case data
The weekly COVID-19 cases and deaths, and cumulative cases and deaths (raw and population adjusted), were extracted from the European Centre of Disease Control (2022) COVID-19 case data for each participant based on the week they completed the survey.
Data analysis
Data analyses and descriptive statistics were computed in R (Version 3.6.2, R Core Team, 2019; all code is publicly available at https://doi.org/10.17605/OSF.IO/3U587).
Dimensionality reduction
For use in path analyses, we first created indices from three sets of variables of interest described above: (a) COVID case data statistics (six variables), (b) COVID-19 risk factors and concern (two variables), and (c) social isolation and loneliness (three variables; see Table 2). To this end, we used two multivariate techniques that reduce dimensionality: principal components analysis for continuous data and factor analysis of mixed data (FAMD) for mixed data types. Because these indices are also used in other studies, they were created using the full data set (N = 680), and then loadings for significant latent variables were extracted for participants comprising the older and younger adult subgroups; full methods and results of dimension-reduction analyses are presented in the Supplemental Material (Sections S2 and S3, respectively).
Table 2.
Variables Comprising the Regional-Severity, Personal-Threat, and Isolation Indices
| Index and variable | Younger adults (n = 124) |
Older adults (n = 124) |
|---|---|---|
| Regional severity a | ||
| Weekly COVID-19 cases: range | 2–171,758 | 2–171,758 |
| Weekly COVID-19 deaths: range | 0–11,846 | 0–11,846 |
| Cumulative COVID-19 cases (raw): range | 1,147–1,643,248 | 1,147–1,486,757 |
| Cumulative COVID-19 deaths (raw): range | 21–97,720 | 21–89,562 |
| Cumulative COVID-19 cases (per 100,000): range | 24–496 | 24–621 |
| Cumulative COVID-19 deaths (per 100,000): range | 0–75 | 0–59 |
| Personal threat | ||
| Number of risk factors: M (SD) | 0.41 (0.58) | 0.84 (0.88) |
| Personal-concern rating: M (SD) | 2.12 (1.25) | 2.37 (1.21) |
| Isolation-loneliness index | ||
| Living alone: percentage of sample | 9.68 | 19.35 |
| Loneliness rating: M (SD) | 1.02 (0.93) | 0.52 (0.81) |
| Isolation-days index | ||
| Days in isolation: range | 0–90 | 0–120 |
COVID-19 statistics were extracted from the European Centre for Disease Prevention and Control (2022) COVID-19 statistics for each participant based on the week they completed the study.
Briefly, the regional-severity index comprised loadings on the first principal component that corresponded to shared variance among all COVID-19 case statistics; higher scores indicated greater regional severity of SARS-CoV-2 infection. The personal-threat index comprised loadings on the one resulting principal component, corresponding to shared variance among input variables (total COVID-19 risk and level of concern regarding COVID-19); higher scores indicated greater personal threat. The FAMD on social isolation and loneliness variables yielded two significant latent variables for which higher loadings indicated greater isolation. The first was a generalized isolation factor capturing variance associated with living alone and self-reported feelings of loneliness; loadings on this factor comprised the isolation-loneliness index. The second factor reflected pandemic-specific isolation driven by the number of days spent in isolation since the start of the pandemic; loadings on this factor comprised the isolation-days index.
Path analysis
Model specification and respecification
We began by examining two overidentified multigroup path models based on our hypotheses; the first model predicted depression severity as the outcome variable (the PHQ model; Fig. 1a), and the second model predicted FTE as the outcome variable (the FTE model; Fig. 1b). In both models, chronological age was modeled as a predictor of both PHQ and FTE, the isolation indices (isolation-loneliness and isolation-days) were entered as predictors of PHQ, and the personal-threat and regional-severity indices were modeled as predictors of FTE. Thus, the only difference between the two models was whether FTE was entered as a predictor of PHQ (when depression severity is the outcome variable; model PHQ) or vice versa (when FTE was the outcome variable; model FTE). Because the younger adults and older adults groups were matched by country, we constrained the intercept and variance for the regional-severity index to be equal between groups. All other 38 parameters were freely estimated (18 per group); with our total sample size of 248, the ratio of participants to freely estimated parameters was 6.53:1, exceeding the recommended minimum ratio of 5:1 (Tanaka, 1987) and minimum sample size of 100 (Anderson & Gerbing, 1984) for path analysis.
Path specification was examined and optimized by exploring the modification indices and correlations of residuals. Optimization of the model was considered for paths where the modification index was above 3.84 (Whittaker, 2012) and/or the correlations of residuals was greater than |r| = .10. Modifications were made only where adding the path was consistent with what would be hypothesized on the basis of the literature. By these criteria, in the respecified models for both depressive severity (Fig. 1c) and FTE (Fig. 1d), personal-threat and regional-severity indices were entered as predictors of PHQ rather than FTE.
Model-fit criteria
Multigroup (younger adults vs. older adult) path analyses were performed in R using the lavaan software package (Rosseel, 2012), and a maximum likelihood estimator was used for all analyses. To examine model fit of the hypothesized and respecified models, as well as the final models (i.e., after invariance testing; see below), we computed χ2s to test the null hypothesis that the observed data and predicted model were equal; p values greater than .05 indicate good model fit. In addition, four key indices were used to examine model fit with the following cutoffs for determining good fit: the comparative fit index (CFI; > .90 was acceptable, > .95 indicated good model fit; Hu & Bentler, 1999), standardized root-mean-square residual (SRMR; < .05; Diamantopoulos & Siguaw, 2000), RMSEA (< .06 indicated good model fit; Hu & Bentler, 1999), and the Tucker-Lewis index (TLI; > .90 indicated acceptable model fit, > .95 indicated good model fit; Schumacker & Lomax, 2016).
Comparison between models
The Bayesian information criterion (BIC) was used to make comparisons between pairs of models that were nonnested. Specifically, we compared the two hypothesized models with each other to determine whether the model in which FTE predicted depression severity (the PHQ model; Fig. 1a) or depression severity predicted FTE (the FTE model; Fig. 1b) better fitted the data. We also compared each hypothesized model with its respecified counterpart (i.e., Fig. 1a vs. Fig. 1c, and Fig. 1b vs. Fig. 1d) to determine whether respecification improved model fit. Differences in BIC values were calculated to determine the strength of evidence that one model had superior fit compared with another (models with lower BIC values have superior fit): difference of 0–2 = weak evidence, 2–6 = positive evidence, 6–10 = strong evidence, and > 10 = very strong evidence (Raftery, 1995).
Invariance testing
To examine differences between the younger and older adult age groups, we used systematic invariance testing. First, we examined age-group differences in the overall models with a global test of invariance. A χ2 difference test was used to compare the free model (i.e., where all paths are free to vary by age group) with a fully constrained model (where all paths are constrained to be equal across age groups). After identifying a global difference between age groups, we then independently constrained each of the paths a through f (see Fig. 1d for path labels). Specifically, each of these constrained models was compared with the free model; if an age-group difference for a given path was identified, as indicated by a significant χ2 difference test, the path was allowed to remain freely estimated; if a given path did not differ significantly, suggesting invariance, it was constrained to be equal across groups. We then updated the model on the basis of these results, constraining or freely estimating paths a through f accordingly (this updated model is referred to as the partially constrained model). Finally, we then additionally constrained path g (Fig. 1d) and compared this more restrictive model to the partially constrained model; again, if a significant χ2 difference test indicated group differences, path g was left free to vary, or if nonsignificant, path g was constrained to be equal across groups in the resultant final model.
Mediation analyses
We examined whether factors contributing to an increase in depression severity had an indirect effect on FTE via depression severity. Mediation analyses were conducted on the final model after adjustments were made on the basis of invariance testing. The direct path between each exogenous variable and FTE was modeled so that we could calculate and examine the estimated indirect and total effects of these factors on FTE. Standard error was estimated using 10,000 bootstrapped samples. Significance was determined by examining p values and 95% bootstrapped confidence intervals (CIs; Preacher et al., 2007).
Results
Model fit and respecification
Fit parameters for hypothesized and respecified models are provided in Table 3. The hypothesized PHQ model (Fig. 1a) had poor overall fit on all fit parameters. In contrast, FTE model (Fig. 1b) was found to have acceptable overall fit, albeit with the exception of the TLI. Consistent with these observations, a difference in BIC values of 9.48 between these two models (Fig. 1a vs. 1b) provided strong evidence to favor the FTE model, therefore indicating that the hypothesized model in which depression severity predicted FTE (rather than vice versa) was a significantly better fit for the data. We next examined modification indices for both hypothesized models, which revealed that for the younger adult group, the fit of both models would be improved by including personal threat (PHQ model: index = 9.93, FTE model: index = 10.01) and regional severity (PHQ model: index = 11.49, FTE model: index = 9.74) as predictors of PHQ rather than FTE, as we had hypothesized. Consistent with this interpretation of the modification indices, correlations of the residuals for personal threat/regional severity and PHQ were r > .20 for both hypothesized models (Figs. 1a and 1b), indicating that the unexplained variance of each variable correlated with the unexplained variance of PHQ. Given our expectations that (a) depression severity would foreshorten FTE, (b) isolation indices would predict greater depression severity, and (c) personal threat and regional severity would correlate with isolation indices, we deemed it possible that PHQ could mediate the relationship between personal threat/regional severity and FTE. Thus, paths were modified accordingly (see respecified models in Figs. 1c and 1d).
Table 3.
Model-Fit Parameters
| Fit measure | Hypothesized models | Respecified models | ||
|---|---|---|---|---|
| PHQ | FTE | PHQ | FTE | |
| χ2 | 35.79 | 26.30 | 18.14 | 12.27 |
| p | .008 | .093 | .447 | .833 |
| df | 18 | 18 | 18 | 18 |
| Comparative fit index | .83 | .92 | 1.00 | 1.00 |
| Tucker-Lewis index | .61 | .82 | 1.00 | 1.00 a |
| Standardized root-mean-square residual | .06 | .05 | .05 | .04 |
| Root-mean-square error of approximation (RMSEA) | .09 | .06 | .01 | .00 |
| RMSEA CI | [.04, .13] | [.00, .11] | [.00, .08] | [.00, .05] |
| Bayesian information criterion | 7,103.53 | 7,094.05 | 7,085.88 | 7,080.02 |
| Akaike information criterion | 6,920.84 | 6,911.35 | 6,903.19 | 6,897.32 |
Note: PHQ = Patient Health Questionnaire; FTE = future time extension; CI = confidence interval.
Value > 1 was rounded down.
There was very strong evidence that changing these two paths improved overall model fit relative to hypothesized models (i.e., Fig. 1a vs. Fig. 1c; Fig. 1b vs. Fig. 1d), with BIC differences exceeding 10 (PHQ model: ΔBIC = 17.65; FTE model: ΔBIC = 14.03). Inspection of fit parameters confirmed that, after respecification, both models (Figs. 1c and 1d) now had good overall fit (Table 3). Nevertheless, the BIC scores for the two respecified models (i.e., Figs. 1c and 1d) differed by 5.86, providing positive to strong evidence that the FTE model was still a better fit to the data than the PHQ model (Fig. 1d). Moreover, following respecification, only the FTE model had an upper RMSEA 95% CI that was under the threshold for good model fit. We therefore examined group differences only in the respecified version of the FTE model (henceforth referred to as the final model).
Invariance testing on the final model
To test for age-group differences in the final model (Fig. 1d), we first examined global invariance by constraining all intercepts and regression paths to be equal between groups and compared the result with the unconstrained model. A χ2 difference test revealed a significant difference in fit between the free and constrained models, ∆χ2(13) = 425.88, p < .001, indicating the presence of group inequalities. By independently constraining each of paths a through f (Fig. 1d), we identified age-group inequalities for the paths from regional severity, personal threat, and isolation-loneliness to depression severity (PHQ), indicating that these paths should remain free to vary across groups (Table 4). In contrast, constraining the paths from age to FTE and PHQ, as well as isolation-days to PHQ did not affect overall model fit. Finally, we compared this partially constrained model with a more restrictive model that additionally constrained the path from PHQ to FTE (path g, Fig. 1d). No significant difference was found between these two models, indicating that the effect of PHQ on FTE (i.e., that greater depression severity predicted feelings of a more limited future) was statistically equivalent between the younger adults and older adults groups.
Table 4.
Results of Invariance Testing on the Final Model
| Type of constraint | df | BIC | AIC | χ2 | Δχ2 | Δdf | p |
|---|---|---|---|---|---|---|---|
| Unconstrained | 18 | 7,080.02 | 6,897.32 | 12.27 | |||
| Fully constrained | 31 | 7,430.23 | 7,297.20 | 438.15 | 425.88 | 13 | < .001 |
| Path a (age to PHQ) only | 19 | 7,075.43 | 6,896.24 | 13.19 | 0.92 | 1 | .338 |
| Path b (personal threat to PHQ) only | 19 | 7,080.09 | 6,900.91 | 17.86 | 5.59 | 1 | .018 |
| Path c (regional severity to PHQ) only | 19 | 7,081.21 | 6,902.02 | 18.97 | 6.70 | 1 | .010 |
| Path d (isolation-days to PHQ) only | 19 | 7,075.43 | 6,896.25 | 13.20 | 0.93 | 1 | .336 |
| Path e (isolation-loneliness to PHQ) only | 19 | 7,083.89 | 6,904.70 | 21.65 | 9.38 | 1 | .002 |
| Path f (age to FTE) only | 19 | 7,075.04 | 6,895.86 | 12.81 | 0.53 | 1 | .465 |
| Partially constrained a | 21 | 7,065.87 | 6,893.71 | 14.66 | |||
| Partially constrained + path g (PHQ to FTE) | 22 | 7,060.95 | 6,892.30 | 15.25 | 0.59 | 1 | .442 |
Note: Change values on a given line are relative to the model the line is nested under (e.g., fully constrained vs. unconstrained, path a vs. unconstrained, etc.). The variable “age” refers to chronological age. Significant p values are given in boldface. BIC = Bayesian information criterion; AIC = Akaike information criterion; PHQ = Patient Health Questionnaire; FTE = future time extension.
The partially constrained model allowed the paths from isolation-loneliness to PHQ, regional severity to PHQ, and personal threat to PHQ to vary across age groups while constraining all other paths from the exogenous variables.
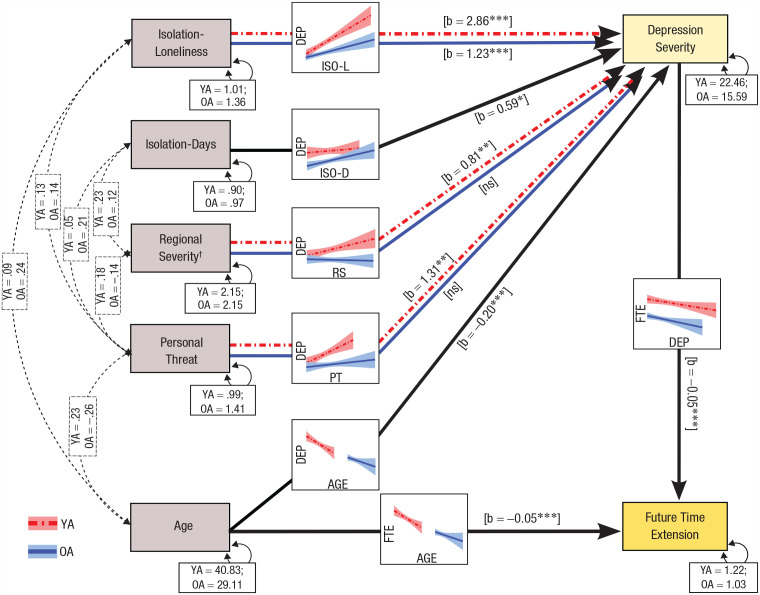
Final model estimation
Overall fit of the final model following invariance testing was good, χ2(22) = 15.25, p = .851; CFI = 1.00; TLI > 1; SRMR = .05; RMSEA < .01, p = .968, 95% CI = [.00, .04]. Path coefficients (see Table 5 and Fig. 2) revealed that, as expected, a 1-year increase in chronological age of both younger and older adults was associated with a 0.05 decrease in FTE (p < .001, 95% CI = [−0.08, −0.03]. As expected, a 1-year increase in chronological age in both groups was associated with a 0.20 decrease in depression severity (p < .001, 95% CI = [−0.29, −0.10]), whereas a 1-unit increase in the isolation-days index was associated with a 0.59 increase in depression severity in both groups (p = .039, 95% CI = [0.03, 1.15]). Although a 1-unit increase in the isolation-loneliness index was associated with an increase of 2.86 in depression-severity scores (p < .001, 95% CI = [2.02, 3.69]) in younger adults, the increase in depression-severity scores was less than half this amount in older adults (1.23; p < .001, 95% CI = [0.63, 1.83]). Moreover, two variables influenced depression severity only in younger adults: (a) A single unit increase in the regional-severity index was associated with a 0.81 increase in depression-severity scores in younger adults (p = .006, 95% CI = [0.23, 1.39]) but not at all in older adults (p = .597, 95% CI = [−0.61, 0.35]), and (b) a single-unit increase in the personal-threat index was associated with an increase of 1.31 in depression severity in younger adults (p = .003, 95% CI = [0.46, 2.16]) but not at all in older adults (p = .755, 95% CI = [−0.50, 0.69]). Irrespective of the age-group differences in terms of predictors of depression severity, an increase in depression severity by 1 point in both younger and older adults (after adjusting for all exogenous predictors) was associated with a 0.05 reduction in their FTE scores (p < .001, 95% CI = [−0.08, −0.03]).
Table 5.
Path Coefficients for the Final Model
| Path and age group | b | z | β | p | 95% CI for b |
|---|---|---|---|---|---|
| Path a (age to PHQ) | |||||
| Younger adults | −0.20 | −4.19 | −0.21 | < .001 | [−0.29, −0.10] |
| Older adults | −0.20 | −4.19 | −0.24 | < .001 | [−0.29, −0.10] |
| Path b (personal threat to PHQ) | |||||
| Younger adults | 1.31 | 3.02 | 0.21 | .003 | [0.46, 2.16] |
| Older adults | 0.10 | 0.31 | 0.03 | .755 | [−0.50, 0.69] |
| Path c (regional severity to PHQ) | |||||
| Younger adults | 0.81 | 2.75 | 0.20 | .006 | [0.23, 1.39] |
| Older adults | −0.13 | −0.53 | −0.04 | .597 | [−0.61, 0.35] |
| Path d (isolation-days to PHQ) | |||||
| Younger adults | 0.59 | 2.07 | 0.09 | .039 | [0.03, 1.15] |
| Older adults | 0.59 | 2.07 | 0.13 | .039 | [0.03, 1.15] |
| Path e (isolation-loneliness to PHQ) | |||||
| Younger adults | 2.86 | 6.70 | 0.47 | < .001 | [2.02, 3.69] |
| Older adults | 1.23 | 4.01 | 0.33 | < .001 | [0.63, 1.83] |
| Path f (age to FTE) | |||||
| Younger adults | −0.05 | −4.63 | −0.29 | < .001 | [−0.08, −0.03] |
| Older adults | −0.05 | −4.63 | −0.27 | < .001 | [−0.08, −0.03] |
| Path g (PHQ to FTE) | |||||
| Younger adults | −0.05 | −4.10 | −0.28 | < .001 | [−0.08, −0.03] |
| Older adults | −0.05 | −4.10 | −0.22 | < .001 | [−0.08, −0.03] |
Note: The variable “age” refers to chronological age. Significant p values are given in boldface. CI = confidence interval; PHQ = Patient Health Questionnaire; FTE = future time extension.
Fig. 2.
Final model predicting future time extension (FTE) from age and depression severity. Modeled covariance (black dashed lines and boxes) and variance (black solid boxes and double-headed arrows) for each variable are presented. Variables on the left-hand side of the figure (gray boxes) were fully exogenous predictors of depression severity (partially endogenous) and/or FTE (fully endogenous). Younger adults (YAs) are represented by dashed red lines, whereas older adults (OAs) are represented by solid blue lines. Asterisks indicate significant paths (*p < .05, **p < .01, ***p < .001). Paths that did not differ between groups are depicted by solid black arrows. For regional severity, the intercept and variance were constrained to be equal between groups. Icon graphs depicting group differences are embedded along each path; the effect of the predictor (x-axis) on the dependent variable (y-axis) for each path is reflected. DEP = depression severity; ISO-L = isolation-loneliness; ISO-D = isolation-days; RS = regional severity; PT = personal threat.
Mediation analysis
In the final model, we additionally sought to examine the possibility that factors predicting greater depression severity in younger and older adults were indirectly influencing FTE. Results of this analysis (see Table S2) revealed significant indirect effects of exogenous predictors on FTE. In younger adults only, a 1-unit increase in regional severity was associated, via depression severity, with a 0.04 decrease in FTE (p = .036, 95% CI = [−0.08, −0.01]), whereas a 1-unit increase in personal threat was indirectly associated with a 0.07 decrease in FTE (p = .036, 95% CI = [−0.14, −0.01]). There was no evidence that either regional severity (p = .111, 95% CI = [−0.04, 0.28]) or personal threat (p = .911, 95% CI = [−0.19, 0.22]) had an independent direct effect on FTE for younger adults. A 1-unit increase in the isolation-loneliness index was associated, via increased depression severity, with a 0.14 reduction in FTE for younger adults (p = .006, 95% CI = [−0.25, −0.05]) and a 0.06 reduction in FTE for older adults (p = .015, 95% CI = [−0.19, −0.02]). There was no evidence that the isolation-loneliness index independently influenced FTE in younger adults (p = .378, 95% CI = [−0.31, 0.12]) or older adults (p = .402, 95% CI = [−0.21, 0.08]). There was no evidence that the isolation-days index was indirectly associated with FTE for either younger or older adults (p = .078, b = −0.03, 95% CI = [−0.07, −0.01]).
Discussion
We investigated the possibility that beyond the effects of chronological age, depression severity and pandemic-related factors—such as regional severity, personal threat of SARS-CoV-2, and social isolation—might independently reduce FTE. We also investigated whether these relationships differ across two phases of the adult life span. We present three key results: (a) Depression severity was a better predictor of FTE than the reverse association, (b) both older chronological age and greater depression severity independently predicted FTE reductions, and (c) the factors contributing to depression severity largely differed between age groups.
Despite substantive evidence for shorter time horizons improving emotional experience and affect regulation (Lang & Carstensen, 2002), our findings add weight to the reverse association: that affective experience predicts FTE. Specifically, in both younger and older adults, depression severity as a predictor of FTE enhanced model fit relative to FTE as a predictor of depression severity. Additionally, chronological age exerted the expected influence on FTE independently of depression severity, such that future time shortened with advancing age. Taken together, these results support the notion of affective foreshortenings of future time (Coudin & Lima, 2011; Holman & Grisham, 2020; Kooij et al., 2018), demonstrating that FTE reductions are not phenomenologically unique to aging. Foreshortenings ahead of chronological age are unlikely to yield the same motivational benefits typically associated with age-related reductions in FTE (cf. SST) and may even be associated with poor psychological outcomes (Cate & John, 2007).
Our results align with evidence suggesting that depression severity is associated with reduced future orientation (McKay et al., 2016; Simon et al., 2022) as well as deficits in imagining the future (Addis et al., 2016; Gamble et al., 2019; Hallford et al., 2018) and goal-oriented future thinking (Gamble et al., 2021). These difficulties projecting the self beyond the present and into the future are a candidate mechanism underlying a foreshortening of future time in depression. Future research is necessary to confirm the mechanistic role of these cognitive changes in reducing FTE in depression. It is also possible that other characteristics of depression, including reduced self-continuity (Chandler & Lalonde, 1998; Melges, 1982), self-efficacy, persistent negative rumination, and a tendency to envision negative future scenarios (MacLeod & Byrne, 1996), contribute to the magnitude of this foreshortening of future time.
Our findings raise important considerations for FTE research. First, the effect of chronological age was linear and consistent between younger and older adults, demonstrating that age gradually influences future time horizons across the adult life span. Thus, some of the motivational benefits associated with decreasing FTE may be evident earlier than typically studied—perhaps as early as 40 when both the awareness of time as limited and the perceived benefits of aging begin to positively affect psychological well-being (Brothers et al., 2016). Thus, the value in longitudinal tracking of changes in FTE and socioemotional functioning cannot be overstated. Second, SST research should consider that older adults with poorer mental health may experience an affective foreshortening of future time in advance of what would be expected by age alone—and potentially with opposite effects on socioemotional motivation. This finding does not rule out potential bidirectional associations between FTE and depression severity, especially given that predicting FTE from depression severity also had acceptable, albeit poorer, overall fit. Nevertheless, the results highlight the complexities of the relationships between FTE, age, and depression severity that should be considered in future research.
Given that FTE is also affected by situational factors (Carvalho et al., 2018; Fredrickson & Carstensen, 1990), we hypothesized that pandemic factors would directly influence FTE. However, we found that for older adults, pandemic factors did not influence FTE directly or even indirectly (via depression severity), perhaps indicating a ceiling effect because time is already limited by older age. In contrast, for younger adults, regional pandemic severity and personal threat indirectly reduced FTE via depression severity, providing partial support for our hypothesis. The mediating indirect pathway of this effect via depression severity dovetails with recent findings linking depression to distorted experiences of time (Ogden, 2020).
Another important finding to emerge was that, consistent with our hypotheses, chronological age was protective against depression, although interestingly, this effect was evident across both age groups: The older adults in both age groups exhibited less severe depression than their younger counterparts. Other researchers also report that age advantages in emotional experience seen in older adults have persisted during the pandemic (Carstensen et al., 2020; Fields et al., 2022), albeit to a reduced degree than in prepandemic times (Sun & Sauter, 2021). Our results extend these findings by demonstrating that age was protective against depression severity during the pandemic for both younger and older adults, above and beyond the detrimental effects of loneliness (in both groups) and pandemic factors (in younger adults).
Older adults generally face poorer outcomes from SARS-CoV-2 (Cohen & Tavares, 2020); although our older sample was relatively healthy—the mean number of risk factors in this sample was less than 1—that number was still double that of younger adults. However, younger adults reported a similar level of personal risk of being affected by COVID-19, again suggestive of poorer emotion regulation than older adults. Unsurprisingly, we found, in younger adults only, that the severity of the pandemic in one’s locale and perceived threat of COVID-19 were associated with depression severity. It may also be that for younger people, the perceived threat from COVID-19 extends beyond physical health. Indeed, pandemic-related disruptions on employment and education (Environics Institute for Survey Research, 2021) as well as loneliness (Wickens et al., 2021) have been felt the greatest by younger adults. Wickens and colleagues contextualized the age difference in loneliness in relation to pandemic-related declines in the quantity (vs. quality) of social interactions that is of higher importance to the young (cf. Nicolaisen & Thorsen, 2017). Our results show that in younger adults, loneliness had more detrimental effects on mental health than in older adults, even though the number of days in isolation was similar between age groups. This is not to say that loneliness does not have negative impacts on older adults; our findings demonstrate that it does significantly increase depression severity, albeit to half the degree as it does in younger adults which likely reflect older adults’ ability to better regulate their emotions (Lang & Carstensen, 2002). Indeed, the protective effects of age were weaker than the detrimental effects of loneliness for both groups. Nevertheless, the impacts of loneliness and isolation beyond depression may be more significant in older adults, given links to cognitive decline and dementia risk (Griffin et al., 2020).
The results of this research highlight that depression severity has a role in reducing the extension of self into the future and that although this relationship was true for both younger and older adults, the factors contributing to depression severity differed across age groups. Critically, our results do not detract from findings supporting SST (i.e., reduced future time perspective with age is associated with a more positive affect); rather, our results add to the wealth of research in this field by suggesting that the association between emotional well-being and FTE is bidirectional. This study is not without limitations, including the sample size, which restricted the number of model parameters and consequently our ability to examine the bidirectional relationship between depression severity and FTE. An important step in examining a bidirectional model would be to identify factors that uniquely influence FTE but not depression severity. Recruiting larger samples and specifically targeting a more diverse range of older adults in future studies will be important to demonstrate the replicability of these findings outside of the COVID-19 context and to facilitate examination of cross-cultural differences using multilevel regression methods. We note that the results reported here using these matched age groups do hold when using our full data set (younger adults < 50 years; older adult ≥ 50 years), which included a small number of middle-age adults (45–55 years old); higher sampling rates in this middle-age group are needed to demonstrate the generalizability of our findings to this group. Despite our efforts to diversify recruitment, our sample predominantly comprised White-identifying individuals from Westernized cultures with secondary or higher education and who were technologically literate with the financial means to access technology; these characteristics should be considered when interpreting these results. However, within this sample, we demonstrated that the reported effects are present after controlling for sex, education, ethnicity, and geographical region (see Section S4 and Tables S3 and S4 in the Supplemental Material). We also matched younger and older participants by sex and country in order to control for these variables in our interpretation of differences between the two age groups. An additional limitation of this study is its cross-sectional nature; an important future directive is to examine these effects longitudinally.
In conclusion, this study provides empirical evidence that, across two phases of the adult life span, both chronological age and mental health are associated with reductions in FTE. Although the effect of depression severity on FTE was similar between younger and older adults, the underlying factors contributing to depression severity differed. Future research should focus on leveraging these individual differences to enhance treatment and support for adults of all ages. This research also supports the conclusion that age advantages for emotional well-being can be reduced when environmental and psychological stressors are present.
Supplemental Material
Supplemental material, sj-docx-1-pss-10.1177_09567976231170560 for Thinking Beyond COVID-19: How Has the Pandemic Impacted Future Time Horizons? by Samuel Fynes-Clinton and Donna Rose Addis in Psychological Science
Acknowledgments
We thank Faryn Starrs, Ziming Cheng, and Audrey Li-Chay-Chung for assistance with data collection.
Narrative data are not reported here; for more information on open-ended narrative questions, see https://doi.org/10.17605/OSF.IO/7X9TQ.
Footnotes
ORCID iD: Samuel Fynes-Clinton  https://orcid.org/0000-0003-2694-7617
https://orcid.org/0000-0003-2694-7617
Supplemental Material: Additional supporting information can be found at http://journals.sagepub.com/doi/suppl/10.1177/09567976231170560
Transparency
Action Editor: Karen Rodrigue
Editor: Patricia J. Bauer
Author Contributions
Samuel Fynes-Clinton: Conceptualization; Data curation; Formal analysis; Investigation; Methodology; Visualization; Writing – original draft; Writing – review & editing.
Donna Rose Addis: Conceptualization; Funding acquisition; Methodology; Project administration; Resources; Supervision; Visualization; Writing – original draft; Writing – review & editing.
The author(s) declared that there were no conflicts of interest with respect to the authorship or the publication of this article.
Funding: This work and the authors were supported by a Canada 150 Research Chair awarded to D. R. Addis.

References
- Addis D. R., Hach S., Tippett L. J. (2016). Do strategic processes contribute to the specificity of future simulation in depression? British Journal of Clinical Psychology, 55, 167–186. 10.1111/bjc.12103 [DOI] [PubMed] [Google Scholar]
- Anderson J. C., Gerbing D. W. (1984). The effect of sampling error on convergence, improper solutions, and goodness-of-fit indices for maximum likelihood confirmatory factor analysis. Psychometrika, 49(2), 155–173. 10.1007/BF02294170 [DOI] [Google Scholar]
- Baldensperger L., Wiedemann A. U., Wessel L., Keilholz U., Knoll N. (2018). Social network, autonomy, and adherence correlates of future time perspective in patients with head and neck cancer. Psycho-Oncology, 27(6), 1545–1552. 10.1002/pon.4690 [DOI] [PubMed] [Google Scholar]
- Brothers A., Gabrian M., Wahl H. W., Diehl M. (2016). Future time perspective and awareness of age-related change: Examining their role in predicting psychological well-being. Psychology and Aging, 31(6), 605–617. 10.1037/pag0000101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carstensen L. L., Pasupathi M., Mayr U., Nesselroade J. R. (2000). Emotional experience in everyday life across the adult life span. Journal of Personality and Social Psychology, 79(4), 644–655. 10.1037/0022-3514.79.4.644 [DOI] [PubMed] [Google Scholar]
- Carstensen L. L., Shavit Y. Z., Barnes J. T. (2020). Age advantages in emotional experience persist even under threat from the COVID-19 pandemic. Psychological Science, 31(11), 1374–1385. 10.1177/0956797620967261 [DOI] [PubMed] [Google Scholar]
- Carstensen L. L., Turan B., Scheibe S., Ram N., Ersner-Hershfield H., Samanez-Larkin G. R., Brooks K. P., Nesselroade J. R. (2011). Emotional experience improves with age: Evidence based on over 10 years of experience sampling. Psychology and Aging, 26(1), 21–33. 10.1037/a0021285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carvalho R. G., Capelo R., Nuñez D. (2018). Perspectives concerning the future when time is suspended: Analysing inmates’ discourse. Time & Society, 27(3), 295–311. 10.1177/0961463X15604533 [DOI] [Google Scholar]
- Cate R. A., John O. P. (2007). Testing models of the structure and development of future time perspective: Maintaining a focus on opportunities in middle age. Psychology and Aging, 22(1), 186–201. 10.1037/0882-7974.22.1.186 [DOI] [PubMed] [Google Scholar]
- Chandler M. J., Lalonde C. (1998). Cultural continuity as a hedge against suicide in Canada’s First Nations. Transcultural Psychiatry, 35, 191–219. 10.1177/136346159803500202 [DOI] [Google Scholar]
- Cheung C. S. S., Cheung T. C. K., Hui N. H. H. (2003, July). Prospect of SARS: How life threatening events change future time perspective and goal pursuit of people in Hong Kong [Paper presentation]. Joint HKU/CUHK/CPU Academic Seminar ‘After SARS: Education and Research Agenda for the Future,’Hong Kong. [Google Scholar]
- Cohen M. A., Tavares J. (2020). Who are the most at-risk older adults in the COVID-19 era? It’s not just those in nursing homes. Journal of Aging and Social Policy, 32(4–5), 380–386. 10.1080/08959420.2020.1764310 [DOI] [PubMed] [Google Scholar]
- Coudin G., Lima M. L. (2011). Being well as time goes by: Future time perspective and well-being. International Journal of Psychology & Psychological Therapy, 11(2), 219–232. [Google Scholar]
- Diamantopoulos A., Siguaw J. (2000). Introducing LISREL. Sage. 10.4135/9781849209359 [DOI] [Google Scholar]
- European Centre for Disease Prevention and Control. (2022, June20). Download historical data (to 20 June 2022) on the weekly number of new reported COVID-19 cases and deaths worldwide [Data set]. https://www.ecdc.europa.eu/en/publications-data/download-historical-data-20-june-2022-weekly-number-new-reported-covid-19-cases
- Environics Institute for Survey Research. (2021). Making up time: The impact of the pandemic on young adults in Canada. https://www.environicsinstitute.org/docs/default-source/default-document-library/report_making-up-time_the-impact-of-the-pandemic-on-young-adults_end292f4ad71b84173b1c6c4da5353acd8.pdf?sfvrsn=672ab506_0
- Fields E. C., Kensinger E. A., Garcia S. M., Ford J. H., Cunningham T. J. (2022). With age comes well-being: Older age associated with lower stress, negative affect, and depression throughout the COVID-19 pandemic. Aging & Mental Health, 26(10), 2071–2079. 10.1080/13607863.2021.2010183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredrickson B. L., Carstensen L. L. (1990). Choosing social partners: How old age and anticipated endings make people more selective. Psychology and Aging, 5(3), 335–347. 10.1037/0882-7974.5.3.335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fung H. H., Carstensen L. L. (2006). Goals change when life’s fragility is primed: Lessons learned from older adults, the September 11 attacks and Sars. Social Cognition, 24(3), 248–278. 10.1521/soco.2006.24.3.248 [DOI] [Google Scholar]
- Gable P. A., Poole B. D. (2012). Time flies when you’re having approach-motivated fun: Effects of motivational intensity on time perception. Psychological Science, 23(8), 879–886. 10.1177/0956797611435817 [DOI] [PubMed] [Google Scholar]
- Gamble B., Moreau D., Tippett L. J., Addis D. R. (2019). Specificity of future thinking in depression: A meta-analysis. Perspectives in Psychological Science, 14, 816–834. 10.1177/1745691619851784 [DOI] [PubMed] [Google Scholar]
- Gamble B., Tippett L. J., Moreau D., Addis D. R. (2021). The futures we want: How goal-directed imagination relates to mental health. Clinical Psychological Science, 9(4), 732–751. 10.1177/2167702620986096 [DOI] [Google Scholar]
- Griffin S. C., Mezuk B., Williams A. B., Perrin P. B., Rybarczyk B. D. (2020). Isolation, not loneliness or cynical hostility, predicts cognitive decline in older Americans. Journal of Aging and Health, 32(1–2), 52–60. 10.1177/0898264318800587 [DOI] [PubMed] [Google Scholar]
- Hallford D. J., Austin D. W., Takano K., Raes F. (2018). Psychopathology and episodic future thinking: A systematic review and meta-analysis of specificity and episodic detail. Behaviour Research and Therapy, 102, 42–51. 10.1016/j.brat.2018.01.003 [DOI] [PubMed] [Google Scholar]
- Holman E. A., Grisham E. L. (2020). When time falls apart: The public health implications of distorted time perception in the age of COVID-19. Psychological Trauma: Theory, Research, Practice, and Policy, 12(Suppl. 1), S63–S65. 10.1037/tra0000756 [DOI] [PubMed] [Google Scholar]
- Holmes E. A., O’Connor R. C., Perry V. H., Tracey I., Wessely S., Arseneault L., Ballard C., Christensen H., Cohen Silver R., Everall I., Ford T., John A., Kabir T., King K., Madan I., Michie S., Przybylski A. K., Shafran R., Sweeney A., . . . Bullmore E. (2020). Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. The Lancet Psychiatry, 7(6), 547–560. 10.1016/S2215-0366(20)30168-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu L., Bentler P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling, 6(1), 1–55. 10.1080/10705519909540118 [DOI] [Google Scholar]
- Jorgensen T. D., Pornprasertmanit S., Schoemann A. M., Rosseel Y. (2021). semTools: Useful tools for structural equation modeling (R Package Version 0.5-5) [Computer software]. https://CRAN.R-project.org/package=semTools
- Kooij D. T. A. M., Kanfer R., Betts M., Rudolph C. W. (2018). Future time perspective: A systematic review and meta-analysis. Journal of Applied Psychology, 103(8), 867–893. 10.1037/apl0000306 [DOI] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R. L., Williams J. B. W. (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16(9), 606–613. 10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lang F. R., Carstensen L. L. (2002). Time counts: Future time perspective, goals, and social relationships. Psychology and Aging, 17(1), 125–139. 10.1037/0882-7974.17.1.125 [DOI] [PubMed] [Google Scholar]
- Lebrasseur A., Fortin-Bédard N., Lettre J., Raymond E., Bussières E.-L., Lapierre N., Faieta J., Vincent C., Duchesne L., Ouellet M.-C., Gagnon E., Tourigny A., Lamontagne M.-È., Routhier F. (2021). Impact of the COVID-19 pandemic on older adults: Rapid review. Journal of Medical Internet Research Aging, 4(2), Article e26474. 10.2196/26474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lens W., Paixão M. P., Herrera D., Grobler A. (2012). Future time perspective as a motivational variable: Content and extension of future goals affect the quantity and quality of motivation: Future time perspective as a motivational variable. Japanese Psychological Research, 54(3), 321–333. 10.1111/j.1468-5884.2012.00520.x [DOI] [Google Scholar]
- Lewin K. (1942). Time perspective and morale. In Watson G. (Ed.), Civilian morale: Second yearbook of the Society for the Psychological Study of Social Issues (pp. 48–70). Houghton Mifflin. 10.1037/13983-004 [DOI] [Google Scholar]
- Liao H.-W., Carstensen L. L. (2018). Future time perspective: Time horizons and beyond. GeroPsych, 31(3), 163–167. 10.1024/1662-9647/a000194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacLeod A. K., Byrne A. (1996). Anxiety, depression, and the anticipation of future positive and negative experiences. Journal of Abnormal Psychology, 105, 286–291. 10.1037//0021-843x.105.2.286 [DOI] [PubMed] [Google Scholar]
- Martinelli N., Gil S., Belletier C., Chevalère J., Dezecache G., Huguet P., Droit-Volet S. (2021). Time and emotion during lockdown and the Covid-19 epidemic: Determinants of our experience of time? Frontiers in Psychology, 11, Article 616169. 10.3389/fpsyg.2020.616169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKay M. T., Cole J. C., Andretta J. R. (2016). Temporal profiles relate meaningfully to anxiety and depression in university undergraduates. Personality and Individual Differences, 101, 106–109. 10.1016/j.paid.2016.05.058 [DOI] [Google Scholar]
- Melges F. (1982). Time and the inner future: A temporal approach to psychiatric disorders. Wiley. [Google Scholar]
- Nicolaisen M., Thorsen K. (2017). What are friends for? Friendships and loneliness over the lifespan—from 18 to 79 years. The International Journal of Aging and Human Development, 84(2), 126–158. 10.1177/0091415016655166 [DOI] [PubMed] [Google Scholar]
- Ogden R. S. (2020). The passage of time during the UK Covid-19 lockdown. PLOS ONE, 15(7), Article e0235871. 10.1371/journal.pone.0235871 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogden R. S. (2021). Distortions to the passage of time during England’s second national lockdown: A role for depression. PLOS ONE, 16(4), Article e0250412. 10.1371/journal.pone.0250412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parlapani E., Holeva V., Nikopoulou V. A., Kaprinis S., Nouskas I., Diakogiannis I. (2021). A review on the COVID-19-related psychological impact on older adults: Vulnerable or not? Aging Clinical and Experimental Research, 33(6), 1729–1743. 10.1007/s40520-021-01873-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher K. J., Rucker D. D., Hayes A. F. (2007). Addressing moderated mediation hypotheses: Theory, methods, and prescriptions. Multivariate Behavioral Research, 42(1), 185–227. 10.1080/00273170701341316 [DOI] [PubMed] [Google Scholar]
- Raftery A. E. (1995). Bayesian model selection in social research. Sociological Methodology, 25, 111–163. 10.2307/271063 [DOI] [Google Scholar]
- R Core Team. (2019). R: A language and environment for statistical computing (Version 3.6.2) [Computer software]. http://www.R-project.org
- Rodrigues N. G., Han C. Q. Y., Su Y., Klainin-Yobas P., Wu X. V. (2022). Psychological impacts and online interventions of social isolation amongst older adults during COVID-19 pandemic: A scoping review. Journal of Advanced Nursing, 78(3), 609–644. 10.1111/jan.15063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rohr M. K., John D. T., Fung H. H., Lang F. R. (2017). A three-component model of future time perspective across adulthood. Psychology and Aging, 32(7), 597–607. 10.1037/pag0000191 [DOI] [PubMed] [Google Scholar]
- Rosseel Y. (2012). lavaan: An R package for structural equation modeling. Journal of Statistical Software, 48(2). 10.18637/jss.v048.i02 [DOI] [Google Scholar]
- Rutland-Lawes J., Wallinheimo A.-S., Evans S. L. (2021). Risk factors for depression during the COVID-19 pandemic: A longitudinal study in middle-aged and older adults. BJPsych Open, 7(5), Article e161. 10.1192/bjo.2021.997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schumacker R. E., Lomax R. G. (2016). A beginner’s guide to structural equation modeling (4th ed.). Routledge. 10.4324/9781315749105 [DOI] [Google Scholar]
- Simon E., Zsidó A. N., Birkás B., Gács B., Csathó Á. (2022). Negative time perspective predicts the self-perceived affective and physical components of pain independently from depression, anxiety, and early life circumstances. Acta Psychologica, 224, Article 103536. 10.1016/j.actpsy.2022.103536 [DOI] [PubMed] [Google Scholar]
- Sullivan-Singh S. J., Stanton A. L., Low C. A. (2015). Living with limited time: Socioemotional selectivity theory in the context of health adversity. Journal of Personality and Social Psychology, 108(6), 900–916. 10.1037/a0039047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun R., Sauter D. (2021). Sustained stress reduces the age advantages in emotional experience of older adults: Commentary on Carstensen et al. (2020). Psychological Science, 32(12), 2035–2041. 10.1177/09567976211052476 [DOI] [PubMed] [Google Scholar]
- Tanaka J. S. (1987). “How big is big enough?” Sample size and goodness of fit in structural equation models with latent variables. Child Development, 58(1), 134–146. 10.2307/1130296 [DOI] [Google Scholar]
- Whittaker T. A. (2012). Using the modification index and standardized expected parameter change for model modification. The Journal of Experimental Education, 80(1), 26–44. 10.1080/00220973.2010.531299 [DOI] [Google Scholar]
- Wickens C. M., McDonald A. J., Elton-Marshall T., Wells S., Nigatu Y. T., Jankowicz D., Hamilton H. A. (2021). Loneliness in the COVID-19 pandemic: Associations with age, gender and their interaction. Journal of Psychiatric Research, 136, 103–108. 10.1016/j.jpsychires.2021.01.047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimbardo P. G., Boyd J. N. (1999). Putting time in perspective: A valid, reliable individual-differences metric. Journal of Personality and Social Psychology, 77(6), 1271–1288. 10.1037/0022-3514.77.6.1271 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-pss-10.1177_09567976231170560 for Thinking Beyond COVID-19: How Has the Pandemic Impacted Future Time Horizons? by Samuel Fynes-Clinton and Donna Rose Addis in Psychological Science