Abstract
Strabismus is not a condition in itself but the consequence of an underlying problem. Eye misalignment can be caused by disease, injury, and/or abnormalities in any of the structures and processes involved in visual perception and oculomotor control, from the extraocular muscles and their innervations to the oculomotor and visual processing areas in the brain. A small percentage of all strabismus cases are the consequence of well-described genetic syndromes, acquired insult, or disease affecting the extraocular muscles (EOMs) or their innervations. We will refer to them as strabismus of peripheral origin since their etiology lies in the peripheral nervous system. However, in most strabismus cases, that is comitant, non-restrictive, non-paralytic strabismus, the EOMs and their innervations function properly. These cases are not related to specific syndromes and their precise causes remain poorly understood. They are generally believed to be caused by deficits in the central neural pathways involved in visual perception and oculomotor control. Therefore, we will refer to them as central strabismus. The goal of this narrative review is to discuss the possible causes behind this particular type of eye misalignment and to raise awareness among eyecare professionals about the important role the central nervous system plays in strabismus etiology, and the subsequent implications regarding its treatment. A non-systematic search was conducted using PubMed, Medline, Cochrane, and Google Scholar databases with the keywords “origins,” “causes,” and “etiology” combined with “strabismus.” A snowball approach was also used to find relevant references. In the following article, we will first describe EOM integrity in central strabismus; next, we will address numerous reasons that support the idea of central nervous system (CNS) involvement in the origin of the deviation, followed by listing several possible central causes of the ocular misalignment. Finally, we will discuss the implications CNS etiology has on strabismus treatment.
Keywords: Strabismus, Etiology, Central nervous system, Extraocular muscles
Introduction
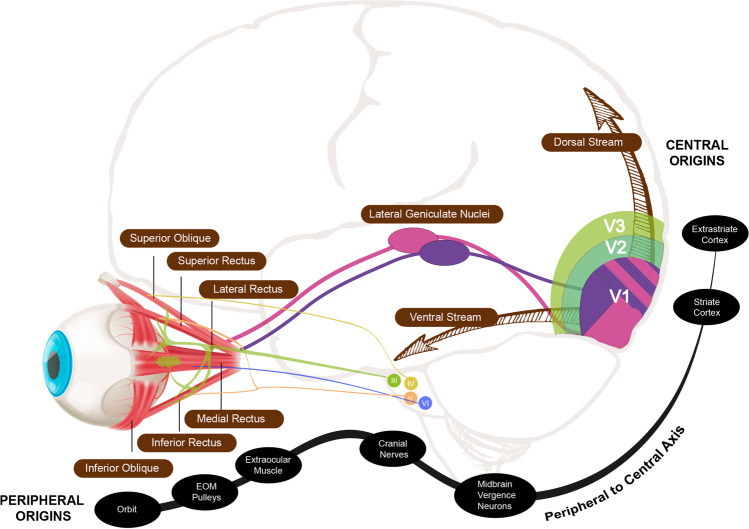
Strabismus is a common disorder that affects from 3 to 6% of the worldwide population [1–4]. The American Academy of Ophthalmology (AAO) defines strabismus as a misalignment of the eyes that may be congenital or acquired [5]. The direction, magnitude, and frequency of the deviation can vary widely between patients. The characteristics of the deviation can also change depending on the position of gaze (incomitance), and the viewing distance, near versus far. In addition, double vision, suppression, or anomalous sensory correspondence might be present, and in 12.5% of cases, the eye turn and amblyopia occur concurrently [6]. Strabismus can present itself in multiple forms, what some authors have called “strabismus polymorphy” [7]. This suggests that the eye turn is a consequence of a vast number of conditions of multiple possible origins, influenced by either genetic or environmental factors, or a combination of both [8–10]. Strabismus is not a single entity nor a condition in itself. The eye misalignment is a manifestation/sign of an underlying problem involving one or multiple components of the visual and oculomotor systems along the peripheral-central axis (Fig. 1), from the extraocular muscles (EOMs) themselves, their pulleys [11] and their innervations, to all brain areas involved in visual perception and oculomotor control: midbrain fusion centres [12], the lateral geniculate nucleus (LGN) and striate and extrastriate areas [13].
Fig. 1.
Peripheral-central axis. It comprises structures of the visual and oculomotor systems, from the eye (periphery) to the brain (center). It includes the orbit, the extraocular muscles (EOMs), their pulleys, the nerves and their nuclei, the midbrain fusion centers, the lateral geniculate nucleus (LGN), and the primary (V1) and secondary visual areas
Strabismus of peripheral origin account for 5–25% of all strabismus cases [1, 4, 7, 14] and are the consequence of either complex well-described genetic syndromes [12, 13] or due to acquired insult to the eye or its innervations. Peripheral strabismus are predominantly incomitant and can be caused by ocular or orbital trauma, craniofacial abnormalities, connective tissue disorders and syndromes, muscular dystrophies, genetic myopathies, and cranial nerve syndromes and palsies [15–18].
On the other hand, the majority of strabismus, 75–95% of all strabismus cases [1, 4, 7, 14], are concomitant, non-restrictive, non-paralytic, or developmental. They are not related to specific syndromes, and their genetic associations remain poorly understood [7, 13, 19–29]. They are generally believed to be caused by deficits in the central neural pathways involved in visual perception and oculomotor control [7, 30–36]. Although several possible mechanisms have been hypothesized, the specific central origins of strabismus remain elusive.
The aim of this study was to review and discuss the latest evidence about the etiology of the most common, and at the same time, the less known, types of ocular deviations: non-restrictive, non-paralytic, and developmental strabismus. For this purpose, the EOM integrity in these cases is described first, addressing the following question “Are there any abnormalities in the EOMs in central strabismus?” Then, numerous reasons that support the idea of central involvement in the origin of the deviation are addressed, and finally, several possible central causes of the ocular misalignment are listed. With this review, we aim to create awareness among eyecare professionals about the important role the central nervous system plays in strabismus etiology, and the subsequent implications regarding its treatment.
The scientific literature on the possible causes of strabismus, in particular regarding the integrity of the EOMs and the structure and function of the CNS, was searched. We used PubMed, Medline, Cochrane, and Google Scholar databases. We did not use restrictions for date nor language of publication; databases were last searched on June 2022. The keywords “origins,” “causes,” and “etiology” were combined with “strabismus.” A snowball approach was also used to track down relevant references.
Extraocular muscle integrity in concomitant, non-paralytic, strabismus
Despite minor differences, gross anatomical, ultra-structural [37], and histological [38] organization of EOMs in concomitant developmental strabismus are similar to that of EOMs without strabismus. High-resolution, surface coil magnetic resonance imaging (MRI) showed normal horizontal rectus muscle path lengths in strabismic patients compared to normal controls [39]. Sizes, paths, structure, and innervation of horizontal rectus EOMs and in connective tissues in the pulley system revealed no significant differences between orthotropic and naturally or artificially strabismic monkeys under histological examination and MRI [40]. On the other hand, high-resolution MRI showed medial rectus muscle to be 39% larger in esotropic patients than in controls [41]. Surprisingly, in the same individuals, lateral rectus muscle cross-sections in esotropia were up to 28% larger but only significantly larger in one plane [41]. Hao et al. 2016 reported similar results: rectus pulleys were found to be displaced differently in subjects with A, V, and Y, pattern exotropia but normal in concomitant exotropia. On the other hand, medial rectus muscle size was found to be significantly reduced in concomitant exotropia compared to normal subjects and individuals with pattern exotropia (P < 0.05) [42]. Other authors reported extensive histological and microscopic abnormalities in strabismic EOMs such as disorganization and atrophy of skeletal muscle fibers, vacuolation and degeneration of myofibrils, accumulation of lipid droplets, and clustering of mitochondria and autophagic processes [43]. Interestingly, all the above-mentioned defects were also seen in the EOMs of a strabismic patient with Down syndrome, a condition both associated with eye misalignment and central nervous system (CNS) defects.
Abnormalities at molecular and gene expression levels in the EOMs appear to be more prominent. Intermediate filament protein distributions were found to be different in EOMs of patients with concomitant exotropia compared to normal subjects [44]. Altick et al. (2012), observed differences in gene expression between strabismic and normal human EOMs in genes associated with signaling, calcium handling, mitochondria function and biogenesis, and energy homeostasis [35]. Moreover, Altick found a decrease in the expression of contractility genes and an increase of extracellular matrix-associated genes. Similar findings of altered gene expression have been reported by other authors. Zhu et al. (2013) found reduced expression of seven myogenesis-related genes in EOMs of patients with concomitant strabismus [45], and Agarwal et al. (2016) reported downregulation of muscle proteins and upregulation of expression of collagens, regulators of collagen synthesis and degradation, connective tissue growth factor (CTGF), and growth factors controlling extracellular matrix (ECM) [46].
These studies suggest that some degree of peripheral muscular abnormality is present in concomitant strabismus. However, it remains unresolved whether the presence of anatomical, histological, and molecular abnormalities in EOM structure are the cause of the ocular deviation, or rather a consequence of altered function, as seen in other muscles [34, 35, 43, 44], for example, in stroke victims where the loss of function leads to abnormalities in skeletal muscle mass and anatomy [47, 48], decrease in fiber length, and change in pennation angle [49]. Mechanical and microstructural changes of skeletal muscle have been reported after changes in function [50], immobilization of skeletal muscles with or without stroke led to atrophy, and deterioration of the mechanical properties of the muscle.
Skeletal muscles, and therefore extraocular muscles [51], have a high degree of adaptability. Muscle fibers contain myofibrils, which are essentially long chains of sarcomeres, the contractile units of skeletal muscle. Skeletal muscles adapt their lengths by addition or subtraction of sarcomeres at the extremes of myofibrils to maintain optimal function. Length adaptation of extraocular muscles can occur in response to muscle position [51], muscle stimulation [52–54], and to facilitate binocular alignment [51, 55]. The cause of abnormal muscle length paths in strabismus could lie well beyond the muscles themselves.
Strabismus of central origin
The idea that concomitant, non-paralytic, developmental strabismus are caused by deficits in the central nervous system is supported by different arguments. The minor abnormalities found in the EOMs (periphery) in these types of strabismus might be a consequence of altered function rather than the cause of the deviation.
First of all, in most strabismus cases, the subject has no limitation of gaze. Patients with esotropia and exotropia can abduct and adduct either eye effortlessly. Moreover, exotropia can be greater at distance than at near [56], known as divergence excess, where there is no muscular impediment to converge. Likewise, in convergence excess, esotropia is greater at near than at distance, the subject being fully capable to diverge [57].
Strabismus is associated with neurodevelopmental and neurologic disorders such as cerebral palsy [58–60], Down’s syndrome [61–63], neurodevelopment delay [61, 63, 64], intellectual disability [65], and white matter damage of immaturity [66]. Greenberg investigated the prevalence and types of esotropia in a Western population and found that 11.4% of esotropias were associated with CNS defects: cerebral palsy, developmental delay, Down syndrome, and seizure disorder [4]. Likewise, approximately 15% of children with exotropia have associated neurologic abnormalities, cerebral palsy, and developmental delay [67]. Acquired brain injury (ABI), which is any type of brain injury occurring after birth, often leads to eye movement and binocular coordination disorders, including strabismus [68–71]. ABI are predominantly caused by stroke, brain tumor, infection, cerebral hypoxia, or after impact or sudden shake to the head. Lesions can occur at the level of the cranial nerves innervating the EOMs (periphery) or in the brainstem and brain areas involved in oculomotor control (center) [72]. The frequency of ocular misalignment in the presence of brain damage is difficult to report since it depends on the nature, extension, and location of the injury. Fowler found that strabismus was present in 28% of patients with stroke, many of them with no obvious signs of brainstem abnormalities [68]. The higher-than-average prevalence of strabismus in the presence of CNS defects indicates that in many cases, the cause of strabismus lies in the brain. Moreover, these studies depict the relationship between strabismus and obvious, well-defined neurological alterations. More subtle, covert neurological deficits could be the cause of strabismus in a much larger proportion of cases.
Smoking during pregnancy increases the risk of children developing strabismus compared to the children of mothers that did not smoke [73–75]. Fetal development of the oculomotor and visual systems could be particularly sensitive to toxic exposure or smoking-induced fetal hypoxia during the second half of pregnancy. Alterations caused by smoking are more likely to be at the level of the CNS than in the EOMs or their innervations, given its associations to thinning of the cerebral cortex [76], and reduced gray matter volumes and densities in specific areas [77]. Exposure to other potentially neurotoxic substances during pregnancy such as alcohol [78, 79] and drugs [80] is also associated with an increased risk of strabismus.
The concept of strabismic control is another important point indicating central origin and central relevance in strabismus. It is widely recognized that strabismus control plays a significant role in the outcomes of EOM surgery, especially in intermittent exotropia [81, 82]. People, whether with strabismus or without, have a certain amount of sensorimotor knowledge related to their eyes and their position in space. In order to grade the amount of control patients have over their deviations, multiple control scores (Table 1) have been developed by different authors [83–86]. They all essentially evaluate strabismic control based on the frequency of the tropic and phoric phase and the quality and speed of the refixation movement after the occlusion of one eye. In addition, some people with strabismus are capable of altering the magnitude of the eye turn, they can do “something” to decrease the deviation, and “something” to increase it even though they are often unable to describe how they do it. In line with strabismus control, in many cases, the deviation worsens when the person is sick, tired, distracted, or absorbed in a highly attention-demanding task. All these unequivocally point to cerebral involvement in eye misalignment pathogenesis [7].
Table 1.
Newcastle control score.
Adapted from Haggerty et al., (2004)[83]
| Home control score | 0 | Squint/monocular eye closure never noticed |
| 1 | Squint/monocular eye closure seen occasionally (< 50% of time child observed) for distance | |
| 2 | Squint/monocular eye closure seen occasionally (> 50% of time child observed) for distance | |
| 3 | Squint/monocular eye closure seen for distance and near fixation | |
| Clinic control near | 0 | Manifest only after cover test and resumes fusion without need for blink or refixation |
| 1 | Blink or refixate to control after CT | |
| 2 | Manifest spontaneously or with any form of fusion disruption without recovery | |
| Clinic control distance | 0 | Manifest only after cover test and resumes fusion without need for blink or refixation |
| 1 | Blink or refixate to control after CT | |
| 2 | Manifest spontaneously or with any form of fusion disruption without recovery |
NCS total = Home + Clinic near + Clinic distance
Strabismus can resolve spontaneously. Infantile esotropia measuring up to 40 PD has been reported to resolve in 46/170 (27%) of patients in the first months of life without treatment [87]. On the other hand, eye misalignment can also worsen over time. Intermittent and variable deviations tend to become constant. Even after successful surgical alignment (less than 10PD from orthotropia), the ocular deviation can reappear. Exotropic drift after an initially successful surgery is a common phenomenon [88–90]. This is another indicator that the cause of the deviation remains untreated and is not related to EOMs structure.
Last but not least, cortical activity changes have been seen after successful treatment in convergence insufficiency, a non-strabismic binocular dysfunction characterized by exodeviation, asthenopia, and in some cases double vision at near [91, 92]. Treatment with vision therapy led to improvement in near point of convergence (NPC), greater positive fusional vergence, reduction in symptoms, and lower near dissociated phoria values. More importantly, improvement in clinical parameters correlated with an increase in functional activity in the frontal areas of the brain, the cerebellum and the brainstem [91, 92].
Central strabismus etiology
Central strabismus can be the consequence of anatomical and/or functional abnormalities found in any of the brain areas and pathways involved in vision and oculomotor control, including the oculomotor and proprioceptive nuclei in the brainstem, the medial reticular formation, the pontine reticular formation, the superior colliculus, the thalamus, the cerebellum, the corpus callosum, and the occipital lobe, and the extraestriate areas involved in visual processing in the parietal and frontal lobes, the parietal eye field, and the frontal and supplementary eye fields [7, 68–71]. Brain abnormalities can either be the consequence of obvious, identifiable lesions such as the ones caused by trauma, stroke, infection, brain tumor, etc., or the consequence of more subtle insult to the brain, undetectable to testing. In the following section, we will provide with examples of brain abnormalities that could be the cause of strabismus. We will focus on studies reporting reduced gray matter volumes, abnormal brain activity, and abnormal connectivity within and between brain regions in subjects with strabismus. By no means, we believe these examples constitute all the possible brain abnormalities that can result in strabismus; we simply intend to illustrate the variety of defects and locations involved in strabismus pathogenesis.
Reduced gray matter volumes and abnormal brain activity
Subjects with strabismus present abnormal brain activity in multiple areas, within the primary and secondary visual cortex, but also beyond the occipital lobe. Ouyang et al. (2017) reported reduced gray matter volumes in strabismic patients in the left cuneus [93]. In the lingual gyrus, corresponding to Brodmann area 19 and site to the secondary visual cortex (V2), higher synchrony of spontaneous neuronal activity was observed in amblyopic-strabismic adults [94] and in concomitant strabismus [95] than in normal controls. Moreover, brain activity in the lingual gyrus has been reported to be higher than average in children with infantile esotropia [96]. Shao et al. (2019) reported higher spontaneous brain activity in right and left middle occipital gyrus in amblyopic-strabismic adults [94]. The middle occipital gyrus also corresponds to the secondary visual cortex and is part of the dorsal visual stream. Along the dorsal stream, Chan et al. (2004) found reduced gray matter volumes in the occipital and parietal lobe in strabismic compared to healthy controls [97]. The dorsal stream processes visual information relevant to the position of objects in space and the visual guidance of action [98].
Yang et al. (2014) found increased brain activity in the bilateral precuneus of subjects with Infantile Esotropia compared to healthy controls [96]. Similar findings have been reported by other authors, who have found increased synchrony of spontaneous neuronal activity in the right precuneus [94]. This structure is located on the medial surface of the superior parietal lobe, anterior to the parietooccipital sulcus. It is associated with a variety of functions including cognition, memory, and emotion. In the visual domain, it is involved in visuo-spatial representations, attention, and in the execution, planning, and imagination of movements [99–101].
In the frontal lobe, Shao et al. (2019) found higher synchrony of spontaneous neuronal activity in the precental gyrus (premotor cortex) of both hemispheres and a reduction in the left inferior frontal gyrus [94]. The premotor cortex plays a role in the control of movement, including eye movements. Ouyang et al. (2017) found the right premotor cortex to have reduced gray matter volumes in strabismic patients [93]. In contrast, Chan et al. (2004) observed greater gray matter volumes in the frontal and supplementary eye fields, in the prefrontal cortex, and in the thalamus and basal ganglia in strabismic adults compared to normal controls [97].
Ouyang et al. (2017) also found lower than normal gray matter volumes in strabismic patients in the left middle temporal pole, the left cerebellum posterior lobe, and the right posterior cingulate cortex [93]. Higher synchrony of spontaneous neuronal activity has also been found in the fusiform gyrus and the cerebellum in concomitant strabismus [95].
On the oculomotor and vestibular systems, abnormal neural activity can also result in strabismus. Altered function anywhere in the proprioceptive extraocular circuitry, especially early during development, can derive in loss of feedback control of eye position and hence loss of binocular vision [102–104]. Eye misalignment can also be a consequence of abnormal activity along the vestibular system and pathways [105, 106].
Abnormal connectivity
Cortico-cortical
Numerous cortico-cortical connections suffer alterations in strabismus. Either connections within a given area, such as in V1 in cats [107] or in pathways connecting distant areas. Yan et al. (2010) found white matter volumes to be reduced along the dorsal visual pathway in adults with concomitant exotropia [108]. Huang, Li, Zhang, et al. (2016) reported increased fractional anisotropy (FA) values in the precuneus and medial frontal gyrus of both hemispheres in patients with concomitant strabismus, suggesting enhanced fiber density, axonal diameter, and myelination [109]. In contrast, the authors found decreased FA values in the left superior temporal gyrus. FA is a marker for white matter microstructural state. Decreased FA values are associated with white matter defects. Ouyang et al. (2017) found significantly reduced white matter volumes in the bilateral middle temporal gyrus, the right precuneus and right premotor cortex in concomitant strabismus patients compared to healthy controls [93]. Zhu et al. (2018) observed abnormal functional connectivity in concomitant exotropia patients between the left primary visual cortex (BA17-V1) and the left lingual gyrus/cerebellum posterior lobe, the right middle occipital gyrus, the left precentral gyrus/postcentral gyrus, and the right inferior parietal lobule/postcentral gyrus; abnormal functional connectivity was also found between the right primary visual cortex and right middle occipital gyrus [110].
Callosal
The corpus callosum plays a role in the development of human binocularity [111, 112]. Ten Tusscher et al. (2018) found abnormal interhemispheric fibers in the corpus callosum connecting right and left primary visual cortical areas in individuals with infantile esotropia (IE) compared to normal controls [113]. Subjects with IE had a higher amount of these fibers, and their hemispheric distribution was asymmetric, with callosal fibers starting from one primary visual cortex being different from the ones arising from the contralateral homologous areas [113]. Abnormal connectivity of the corpus callosum in the primary and secondary visual cortex has been reported in cats with surgically induced strabismus and in Siamese cats with natural esotropia [114]. The latter suggests that abnormal corpus callosum connectivity is not only a consequence of surgically-induced strabismus but a potential factor in strabismus pathogenesis. This is also supported by studies in cats in which the corpus callosum had been sectioned early on life and consequently displayed strabismus [115–117]. In a study of 13 children with corpus callosum agenesis, strabismus was present in 6 (46%) of the children [118]. Corpus callosum maturation is dependent on visual experience: monocular deprivation [119], complete darkness [120, 121], and strabismus [114, 122] result in a reduction of callosal projections, changes in their distribution and detrimental effects of callosal neuron properties. Moreover, spontaneous neural activity even before eye-opening (in absence of visual input) contributes to normal corpus callosum development [123–125].
Dorsal–ventral
It has been hypothesized that a division between the ventral and dorsal streams, as seen in children with Williams syndrome, leads to visual problems and severe visuospatial difficulties. Strabismus is found in a greater proportion of cases of Williams syndrome compared to the normal population [126].
The dorsal stream, involved in processing visuospatial information and planification of visuomotor action [98], has been reported to be particularly compromised in developmental disorders such as Williams syndrome, autism, dyslexia, and in premature infants [126–130]. Atkinson hypothesized that the dorsal stream has specific vulnerability during development [131]. Insult early in development could result in abnormal space representation, altered eye movements, and deficits in visual-directed behaviors such as locomotion, reaching, and grasping, which could be associated to strabismus. Gopal et al. (2020) developed a treatment exercise for amblyopia and strabismus with emphasis on the dorsal stream, both regarding saccadic eye movements and visually guided action such as pointing, and also by improving attention. In their pilot study with 35 subjects with amblyopia, 22 of whom had strabismic amblyopia, stereopsis improved in 34 (97%), and ortophoria was achieved in 15/22 (68%) after 10 one hour sessions [132].
In the retino-geniculo-cortical pathway
Abnormal predominance of crossed retinal ganglion cells at the optic chiasm is sometimes associated with strabismus in humans [36, 133]. An unnaturally high number of crossed RGCs is also found in Siamese cats [134] and in albino rats, rabbits, monkeys [135], and also in humans with albinism [136–139]. All previous cases manifest higher than average percentages of strabismus.
Implications regarding strabismus treatment
The ocular deviation is not a disease in itself but a consequence of an underlying problem ranging from systemic, ocular, and neurological diseases to genetic syndromes and to acquired injury to the structures involved in vision. Lack of understanding of strabismus etiology may prevent treatment from being targeted to the specific causes of the eye misalignment. Optimal medical treatment should be directed to the source. Classical and contemporary standard treatment for strabismus, i.e., EOMs surgery, acts exclusively at a peripheral level. EOM surgery consists of mechanically weakening or strengthening the muscles to correct the eye misalignment. However, in most strabismus cases, there is little or no evidence of abnormalities in the EOMs. In addition, the presence of co-existing CNS abnormalities suggests that the CNS plays a role in strabismus pathogenesis. Not being able to address the concomitant CNS abnormalities in strabismus could be the cause of surgical treatment varying [23] and sometimes unsuccessful results [28, 140–144], often with high recurrence and reoperation rates [145–148], all despite being a common and frequently implemented procedure worldwide [149, 150]. By surgically rearranging EOM position, no steps are taken to enhance control, nor to improve oculomotor and perceptual abilities. If anything, awareness of eye position could be increasingly limited due to the destruction of proprioceptive afferents [151]. Considering that multiple causes, along the periphery-center axis, can be behind the ocular deviation, different treatment strategies tailored to the precise strabismus causes might be needed. Some cases benefiting from surgery, others from patch therapy, glasses prescription, vision therapy, and in some cases, the deviation can resolve spontaneously. Different treatment strategies imply a multidisciplinary approach between ophthalmologists, optometrists, and may be in the future neurologists. Incorporating treatment directed at improving oculomotor control, enhancing fusion, proprioception, interhemispheric connectivity, etc.
Conclusion
Alterations in structures in the oculomotor and visual systems along the peripheral–central axis can result in strabismus. In concomitant, non-restrictive, developmental strabismus (the most common type of strabismus), no significant anatomical and/or functional abnormalities are present at the level of the EOMs. In these cases, the deviation is believed to be caused by alterations in the central neural pathways involved in visual perception and oculomotor control [152]. However, the exact causes remain poorly understood [20–23]. Multiple arguments reinforce the idea that the SNC plays an important role in comitant strabismus pathogenesis: the higher than average presence of strabismus in neurological conditions and diseases; the increased rates of strabismus in children exposed to neurotoxic substances such as tobacco, alcohol, and drugs during pregnancy; the absence of limitations of gaze; the capacity for some exotropes to converge and some esotropes to diverge; the control and awareness that many strabismic patients have over the deviation; the negative effects stress, fever, and tiredness have in strabismus control; and last but not least, the brain activity changes seen after successful treatment of convergence insufficiency with vision therapy. Furthermore, multiple CNS abnormalities co-exist with strabismus. On the one hand, changes in brain activity, brain connectivity, and gray and white area volumes might be direct consequences of the eye misalignment or its adaptations. On the other hand, these very same functional and anatomical alterations could be the initial cause of strabismus. In order to improve strabismus treatment success rates, research regarding the origins of strabismus should be encouraged so that in the future, treatment is tailored to the precise causes of the eye misalignment. Different treatment methods focusing on distinct points of the peripheral-central axis might allow for a more customized approach and yield better results. With some strabismus cases responding better to periphery-acting treatment (surgery), while other cases showing better outcome with treatment acting at CNS level.
Author contribution
All authors contributed to the study conception and design. The first draft of the manuscript was written by Bernat Sunyer-Grau, and all authors commented on previous versions of the manuscript. Lluïsa Quevedo, Manuel Rodríguez-Vallejo, and Marc Argilés critically revised the work. Manuel Rodríguez-Vallejo created the artwork in Fig. 1.
Funding
Open Access funding provided thanks to the CRUE-CSIC agreement with Springer Nature.
Declarations
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Conflict of interest
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Bernat Sunyer-Grau, Email: bernat.sunyer@upc.edu.
Lluïsa Quevedo, Email: luisa.quevedo@upc.edu.
References
- 1.Stidwill D. Epidemiology of strabismus. Ophthalmic Physiol Opt. 1997;17:536–539. doi: 10.1016/s0275-5408(97)00037-9. [DOI] [PubMed] [Google Scholar]
- 2.Ziakas NG, Woodruff G, Smith LK, Thompson JR. A study of hereditary as a risk factor in strabismus. Eye. 2002;16:519–521. doi: 10.1038/sj.eye.6700138. [DOI] [PubMed] [Google Scholar]
- 3.Arora A, Williams B, Arora AK, McNamara R, Yates J, Fielder A. Decreasing strabismus surgery. Br J Ophthalmol. 2005;89:409–412. doi: 10.1136/bjo.2004.053678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Greenberg AE, Mohney BG, Diehl NN, Burke JP. Incidence and types of childhood esotropia. A population-based study Ophthalmology. 2007;114:170–174. doi: 10.1016/j.ophtha.2006.05.072. [DOI] [PubMed] [Google Scholar]
- 5.Dagi LR, Velez FG, Archer SM, Stager Sr DR, Stager Jr D, Capo H (2019) Adult strabismus preferred practice pattern 2019 - American Academy of Ophthalmology. 127:182–298 . 10.1016/j.ophtha.2019.09.023
- 6.Chia A, Dirani M, Chan Y-H, Gazzard G, Au Eong K-G, Selvaraj P, Ling Y, Quah B-L, Young TL, Mitchell P, Varma R, Wong T-Y, Saw S-M. Prevalence of amblyopia and strabismus in young singaporean chinese children. Invest Ophthalmol Vis Sci. 2010;51:3411–3417. doi: 10.1167/IOVS.09-4461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bui Quoc E, Milleret C. Origins of strabismus and loss of binocular vision. Front Integr Neurosci. 2014;8:71. doi: 10.3389/fnint.2014.00071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chew E, Remaley NA, Tamboli A, Zhao J, Podgor MJ, Klebanoff M. Risk factors for esotropia and exotropia. Arch Ophthalmol. 1994;112:1349. doi: 10.1001/archopht.1994.01090220099030. [DOI] [PubMed] [Google Scholar]
- 9.Sanfilippo PG, Hammond CJ, Staffieri SE, Kearns LS, Melissa Liew SH, Barbour JM, Hewitt AW, Ge D, Snieder H, Mackinnon JR, Brown SA, Lorenz B, Spector TD, Martin NG, Wilmer JB, Mackey DA. Heritability of strabismus: genetic influence is specific to eso-deviation and independent of refractive error. Twin Res Hum Genet. 2012;15:624–630. doi: 10.1017/thg.2012.22. [DOI] [PubMed] [Google Scholar]
- 10.Maconachie GDE, Gottlob I, McLean RJ. Risk factors and genetics in common comitant strabismus: a systematic review of the literature. JAMA Ophthalmol. 2013;131:1179–1186. doi: 10.1001/jamaophthalmol.2013.4001. [DOI] [PubMed] [Google Scholar]
- 11.Clark R. The role of extraocular muscle pulleys in incomitant non-paralytic strabismus. Middle East Afr J Ophthalmol. 2015;22:279–285. doi: 10.4103/0974-9233.159698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Engle EC. The genetic basis of complex strabismus. Pediatr Res. 2006;59:343–348. doi: 10.1203/01.pdr.0000200797.91630.08. [DOI] [PubMed] [Google Scholar]
- 13.Ye XC, Pegado V, Patel MS, Wasserman WW. Strabismus genetics across a spectrum of eye misalignment disorders. Clin Genet. 2014;86:103–111. doi: 10.1111/cge.12367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chia A, Roy L, Seenyen L. Comitant horizontal strabismus: an Asian perspective. Br J Ophthalmol. 2007;91:1337–1340. doi: 10.1136/bjo.2007.116905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Velez FG, Thocker N, Britt MT, Rosenbaum AL. Cause of V pattern strabismus in craniosynostosis: a case report. Br J Ophthalmol. 2004;88:1598–1599. doi: 10.1136/bjo.2004.048413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Peragallo JH, Pineles SL, Demer JL. Recent advances clarifying the etiologies of strabismus. J Neuro-Ophthalmology. 2015;35:1. doi: 10.1097/WNO.0000000000000228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Izquierdo NJ, Traboulsi EI, Enger C, Maumenee IH. Strabismus in the Marfan syndrome. Am J Ophthalmol. 1994;117:632–635. doi: 10.1016/S0002-9394(14)70069-8. [DOI] [PubMed] [Google Scholar]
- 18.Gazit Y, Jacob G, Grahame R. Ehlers-Danlos syndrome—hypermobility type: a much neglected multisystemic disorder. Rambam Maimonides Med J. 2016;7:e0034. doi: 10.5041/rmmj.10261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wan MJ, Chiu H, Shah AS, Hunter DG. Long-term surgical outcomes for large-angle infantile esotropia. Am J Ophthalmol. 2018;189:155–159. doi: 10.1016/j.ajo.2017.11.006. [DOI] [PubMed] [Google Scholar]
- 20.Chougule P, Kekunnaya R (2019) Surgical management of intermittent exotropia: do we have an answer for all? BMJ Open Ophthalmol 4. 10.1136/bmjophth-2018-000243 [DOI] [PMC free article] [PubMed]
- 21.Audren F. Intermittent exotropia. J Fr Ophtalmol. 2019;42:1007–1019. doi: 10.1016/J.JFO.2018.12.031. [DOI] [PubMed] [Google Scholar]
- 22.Guidelines for the Management of Strabismus in Childhood (2012) The Royal College of Ophthalmologists 2012. Scientific Department, London. https://www.rcophth.ac.uk/wp-content/uploads/2021/08/2012-SCI-250-Guidelines-for-Management-of-Strabismusin-Childhood-2012.pdf
- 23.Chiu AKC, Din N, Ali N. Standardising reported outcomes of surgery for intermittent exotropia — a systematic literature review. Strabismus. 2014;22:32–36. doi: 10.3109/09273972.2013.877940. [DOI] [PubMed] [Google Scholar]
- 24.Awadein A, Eltanamly RM, Elshazly M. Intermittent exotropia: relation between age and surgical outcome: A change-point analysis. Eye. 2014;28:587–593. doi: 10.1038/eye.2014.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chew FLM, Gesite-De Leon BU, Quah BL. Post-operative strabismus control and motor alignment for basic intermittent exotropia. Int J Ophthalmol. 2016;9:1011–1015. doi: 10.18240/ijo.2016.07.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yang M, Chen J, Shen T, Kang Y, Deng D, Lin X, Wu H, Chen Q, Ye X, Li J, Yan J (2016) Clinical characteristics and surgical outcomes in patients with intermittent exotropia a large sample study in South China. Med (United States) 95. 10.1097/MD.0000000000002590 [DOI] [PMC free article] [PubMed]
- 27.Kimura Y, Kimura T. Comparative study of plication–recession versus resection–recession in unilateral surgery for intermittent exotropia. Jpn J Ophthalmol. 2017;61:286–291. doi: 10.1007/s10384-017-0501-5. [DOI] [PubMed] [Google Scholar]
- 28.Jeon H, Jung J, Choi H. Long-term surgical outcomes of early surgery for intermittent exotropia in children less than 4 years of Aage. Curr Eye Res. 2017;42:1435–1439. doi: 10.1080/02713683.2017.1337154. [DOI] [PubMed] [Google Scholar]
- 29.Magli A, Esposito Veneruso P, Chiariello Vecchio E, Esposito G, Rombetto L. Divergence excess intermittent exotropia: long-term effect of augmented bilateral lateral rectus recession. Semin Ophthalmol. 2018;33:512–516. doi: 10.1080/08820538.2017.1320414. [DOI] [PubMed] [Google Scholar]
- 30.Tychsen L. Can ophthalmologists repair the brain in infantile esotropia? Early surgery, stereopsis, monofixation syndrome, and the legacy of Marshall Parks. J AAPOS. 2005;9:510–521. doi: 10.1016/j.jaapos.2005.06.007. [DOI] [PubMed] [Google Scholar]
- 31.McLoon LK, Christiansen SP. Pharmacological approaches for the treatment of strabismus. Drugs Future. 2005;30:319–327. doi: 10.1358/dof.2005.030.03.891455. [DOI] [Google Scholar]
- 32.Das VE, Mustari MJ. Correlation of cross-axis eye movements and motoneuron activity in non-human primates with “A” pattern strabismus. Investig Ophthalmol Vis Sci. 2007;48:665–674. doi: 10.1167/iovs.06-0249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tychsen L, Richards M, Wong A, Foeller P, Burhkalter A, Narasimhan A, Demer J. Spectrum of infantile esotropia in primates: behavior, brains, and orbits. J AAPOS. 2008;12:375–380. doi: 10.1016/j.jaapos.2007.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lennerstrand G. Strabismus and eye muscle function. Acta Ophthalmol Scand. 2007;85:711–723. doi: 10.1111/j.1600-0420.2007.00853.x. [DOI] [PubMed] [Google Scholar]
- 35.Altick AL, Feng CY, Schlauch K, Alan Johnson L, von Bartheld CS. Differences in gene expression between strabismic and normal human extraocular muscles. Investig Ophthalmol Vis Sci. 2012;53:5168–5177. doi: 10.1167/iovs.12-9785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ten Tusscher MPM. Does dominance of crossing retinal ganglion cells make the eyes cross? the temporal retina in the origin of infantile esotropia — a neuroanatomical and evolutionary analysis. Acta Ophthalmol. 2014;92:e419–e423. doi: 10.1111/aos.12289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Martínez AJ, Biglan AW, Hiles DA. Structural features of extraocular muscles of children with strabismus. Arch Ophthalmol. 1980;98:533–539. doi: 10.1001/archopht.1980.01020030529020. [DOI] [PubMed] [Google Scholar]
- 38.Stager D, McLoon LK, Felius J. Postulating a role for connective tissue elements in inferior oblique muscle overaction. Trans Am Ophthalmol Soc. 2013;111:119–132. [PMC free article] [PubMed] [Google Scholar]
- 39.Rabinowitz R, Demer JL. Muscle path length in horizontal strabismus. J AAPOS. 2014;18:4–9. doi: 10.1016/j.jaapos.2013.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Narasimhan A, Tychsen L, Poukens V, Demer JL. Horizontal rectus muscle anatomy in naturally and artificially strabismic monkeys. Investig Ophthalmol Vis Sci. 2007;48:2576–2588. doi: 10.1167/iovs.06-0662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Schoeff K, Chaudhuri Z, Demer JL. Functional magnetic resonance imaging of horizontal rectus muscles in esotropia. J AAPOS. 2013;17:16–21. doi: 10.1016/j.jaapos.2012.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hao R, Suh SY, Le A, Demer JL. Rectus extraocular muscle size and pulley location in concomitant and pattern exotropia. Ophthalmology. 2016;123:2004–2012. doi: 10.1016/j.ophtha.2016.05.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Al-Falki Y, Al-Shraim M, Alsabaani NA, Eid RA, Radad K. Ultrastructural changes of extraocular muscles in strabismus patients. Ultrastruct Pathol. 2019;43:145–153. doi: 10.1080/01913123.2019.1671927. [DOI] [PubMed] [Google Scholar]
- 44.Shen T, Lin J, Li X, Deng D. Intermediate filaments in the medial rectus muscles in patients with concomitant exotropia. Int Ophthalmol. 2020;40:403–410. doi: 10.1007/s10792-019-01197-3. [DOI] [PubMed] [Google Scholar]
- 45.Zhu Y, Deng D, Long C, Jin G, Zhang Q, Shen H. Abnormal expression of seven myogenesis-related genes in extraocular muscles of patients with concomitant strabismus. Mol Med Rep. 2013;7:217–222. doi: 10.3892/mmr.2012.1149. [DOI] [PubMed] [Google Scholar]
- 46.Agarwal AB, Feng CY, Altick AL, Quilici DR, Wen D, Alan Johnson L, von Bartheld CS. Altered protein composition and gene expression in strabismic human extraocular muscles and tendons. Investig Ophthalmol Vis Sci. 2016;57:5576–5585. doi: 10.1167/iovs.16-20294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.English C, McLennan H, Thoirs K, Coates A, Bernhardt J. Loss of skeletal muscle mass after stroke: a systematic review. Int J Stroke. 2010;5:395–402. doi: 10.1111/j.1747-4949.2010.00467.x. [DOI] [PubMed] [Google Scholar]
- 48.Hunnicutt JL, Gregory CM. Skeletal muscle changes following stroke: a systematic review and comparison to healthy individuals. Top Stroke Rehabil. 2017;24:463–471. doi: 10.1080/10749357.2017.1292720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gray V, Rice CL, Garland SJ. Factors that influence muscle weakness following stroke and their clinical implications: a critical review. Physiother Canada. 2012;64:415–426. doi: 10.3138/ptc.2011-03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Jalal N, Gracies JM, Zidi M. Mechanical and microstructural changes of skeletal muscle following immobilization and/or stroke. Biomech Model Mechanobiol. 2020;19:61–80. doi: 10.1007/s10237-019-01196-4. [DOI] [PubMed] [Google Scholar]
- 51.Scott AB. Change of eye muscle sarcomeres according to eye position. J Pediatr Ophthalmol Strabismus. 1994;31:85–88. doi: 10.3928/0191-3913-19940301-05. [DOI] [PubMed] [Google Scholar]
- 52.Hayat A, Tardieu C, Tabary J, Tabary C. Effects of denervation on the reduction of sarcomere number in cat soleus muscle immobilized in shortened position during seven days. J Physiol. 1978;74:563–567. [PubMed] [Google Scholar]
- 53.Tabary J-C, Tardieu C, Tardieu G, Tabary C. Experimental rapid sarcomere loss with concomitant hypoextensibility. Muscle Nerve. 1981;4:198–203. doi: 10.1002/mus.880040305. [DOI] [PubMed] [Google Scholar]
- 54.Williams PE, Catanese T, Lucey EG, Goldspink G. The importance of stretch and contractile activity in the prevention of connective tissue accumulation in muscle. J Anat. 1988;158:109–10914. [PMC free article] [PubMed] [Google Scholar]
- 55.Guyton DL (2006) The 10th Bielschowsky Lecture. Changes in strabismus over time: the roles of vergence tonus and muscle length adaptation - PubMed. In: Binocul. Vis. Strabismus Q. https://pubmed.ncbi.nlm.nih.gov/16792523/. Accessed 9 Jan 2021 [PubMed]
- 56.Bae GH, Bae SH, Choi DG (2019) Surgical outcomes of intermittent exotropia according to exotropia type based on distance/near differences. PLoS One 14.10.1371/JOURNAL.PONE.0214478 [DOI] [PMC free article] [PubMed]
- 57.Vivian AJ, Lyons CJ, Burke J. Controversy in the management of convergence excess esotropia. Br J Ophthalmol. 2002;86:923–929. doi: 10.1136/BJO.86.8.923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Pennefather PM, Tin W. Ocular abnormalities associated with cerebral palsy after preterm birth. Eye (Lond) 2000;14(Pt 1):78–81. doi: 10.1038/eye.2000.17. [DOI] [PubMed] [Google Scholar]
- 59.Sasmal NK, Maiti P, Mandal R, Das D, Sarkar S, Sarkar P, Biswas MC, Dey AK, Chatterjee S. Ocular manifestations in children with cerebral palsy. J Indian Med Assoc. 2011;109(318):323. [PubMed] [Google Scholar]
- 60.Park MJ, Yoo YJ, Chung CY, Hwang J-M. Ocular findings in patients with spastic type cerebral palsy. BMC Ophthalmol. 2016;16:195. doi: 10.1186/s12886-016-0367-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Pathai S, Cumberland PM, Rahi JS. Prevalence of and early-life influences on childhood strabismus. Arch Pediatr Adolesc Med. 2010;164:250. doi: 10.1001/archpediatrics.2009.297. [DOI] [PubMed] [Google Scholar]
- 62.Yurdakul NS, Ugurlu S, Maden A. Strabismus in Down syndrome. J Pediatr Ophthalmol Strabismus. 2006;43:27–30. doi: 10.3928/01913913-20060101-03. [DOI] [PubMed] [Google Scholar]
- 63.van Splunder J, Stilma JS, Bernsen RM, Evenhuis HM. Prevalence of ocular diagnoses found on screening 1539 adults with intellectual disabilities. Ophthalmology. 2004;111:1457–1463. doi: 10.1016/j.ophtha.2003.12.051. [DOI] [PubMed] [Google Scholar]
- 64.Pennefather PM, Clarke MP, Strong NP, Cottrell DG, Dutton J, Tin W. Risk factors for strabismus in children born before 32 weeks’ gestation. Br J Ophthalmol. 1999;83:514–518. doi: 10.1136/bjo.83.5.514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Alazami AM, Hijazi H, Al-Dosari MS, Shaheen R, Hashem A, Aldahmesh MA, Mohamed JY, Kentab A, Salih MA, Awaji A, Masoodi TA, Alkuraya FS. Mutation in ADAT3, encoding adenosine deaminase acting on transfer RNA, causes intellectual disability and strabismus. J Med Genet. 2013;50:425–430. doi: 10.1136/jmedgenet-2012-101378. [DOI] [PubMed] [Google Scholar]
- 66.Jeon H, Jung J, Kim H, Yeom JA, Choi H. Strabismus in children with white matter damage of immaturity: MRI correlation. Br J Ophthalmol. 2017;101:467–471. doi: 10.1136/bjophthalmol-2016-308769. [DOI] [PubMed] [Google Scholar]
- 67.Govindan M, Mohney BG, Diehl NN, Burke JP. Incidence and types of childhood exotropia: a population-based study. Ophthalmology. 2005;112:104–108. doi: 10.1016/j.ophtha.2004.07.033. [DOI] [PubMed] [Google Scholar]
- 68.Fowler MS, Wade DT, Richardson AJ, Stein JF. Squints and diplopia seen after brain damage. J Neurol. 1996;243:86–90. doi: 10.1007/bf00878537. [DOI] [PubMed] [Google Scholar]
- 69.Ciuffreda KJ, Kapoor N, Rutner D, Suchoff IB, Han ME, Craig S. Occurrence of oculomotor dysfunctions in acquired brain injury: a retrospective analysis. Optometry. 2007;78:155–161. doi: 10.1016/j.optm.2006.11.011. [DOI] [PubMed] [Google Scholar]
- 70.Rowe F, Brand D, Jackson CA, Price A, Walker L, Harrison S, Eccleston C, Scott C, Akerman N, Dodridge C, Howard C, Shipman T, Sperring U, Macdiarmid S, Freeman C. Visual impairment following stroke: do stroke patients require vision assessment? Age Ageing. 2009;38:188–193. doi: 10.1093/ageing/afn230. [DOI] [PubMed] [Google Scholar]
- 71.Rowe FJ, Hanna K, Evans JR, Noonan CP, Garcia-Finana M, Dodridge CS, Howard C, Jarvis KA, Macdiarmid SL, Maan T, North L, Rodgers H (2018) Interventions for eye movement disorders due to acquired brain injury. Cochrane Database Syst Rev 3(3):CD011290. 10.1002/14651858.CD011290.pub2 [DOI] [PMC free article] [PubMed]
- 72.Pierrot-Deseilligny C (2011) Nuclear, internuclear, and supranuclear ocular motor disorders. Handb Clin Neurol. 102:319-31. 10.1016/B978-0-444-52903-9.00018-2 [DOI] [PubMed]
- 73.Cotter SA, Varma R, Tarczy-Hornoch K, McKean-Cowdin R, Lin J, Wen G, Wei J, Borchert M, Azen SP, Torres M, Tielsch JM, Friedman DS, Repka MX, Katz J, Ibironke J, Giordano L, Joint Writing Committee for the Multi-Ethnic Pediatric Eye Disease Study and the Baltimore Pediatric Eye Disease Study Groups Risk factors associated with childhood strabismus: the multi-ethnic pediatric eye disease and Baltimore pediatric eye disease studies. Ophthalmology. 2011;118:2251–61. doi: 10.1016/j.ophtha.2011.06.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Hakim RB, Tielsch JM. Maternal cigarette smoking during pregnancy: a risk factor for childhood strabismus. Arch Ophthalmol. 1992;110:1459–1462. doi: 10.1001/archopht.1992.01080220121033. [DOI] [PubMed] [Google Scholar]
- 75.Pathai S, Cumberland PM, Rahi JS. Prevalence of and early-life influences on childhood strabismus: findings from the millennium cohort study. Arch Pediatr Adolesc Med. 2010;164:250–257. doi: 10.1001/archpediatrics.2009.297. [DOI] [PubMed] [Google Scholar]
- 76.Karama S, Ducharme S, Corley J, Chouinard-Decorte F, Starr JM, Wardlaw JM, Bastin ME, Deary IJ. Cigarette smoking and thinning of the brain’s cortex. Mol Psychiatry. 2015;20:778–785. doi: 10.1038/mp.2014.187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Brody AL, Mandelkern MA, Jarvik ME, Lee GS, Smith EC, Huang JC, Bota RG, Bartzokis G, London ED. Differences between smokers and nonsmokers in regional gray matter volumes and densities. Biol Psychiatry. 2004;55:77–84. doi: 10.1016/S0006-3223(03)00610-3. [DOI] [PubMed] [Google Scholar]
- 78.Strömland K, Dolores Pinazo-Durán M. Ophthalmic involvement in the fetal alcohol syndrome: clinical and animal model studies. Alcohol. 2002;37:2–8. doi: 10.1093/ALCALC/37.1.2. [DOI] [PubMed] [Google Scholar]
- 79.Bruce BB, Biousse V, Dean AL, Newman NJ. Neurologic and ophthalmic manifestations of fetal alcohol syndrome. Rev Neurol Dis. 2009;6:13–20. [PubMed] [Google Scholar]
- 80.Spiteri Cornish K, Hrabovsky M, Scott NW, Myerscough E, Reddy AR. The short- and long-term effects on the visual system of children following exposure to maternal substance misuse in pregnancy. Am J Ophthalmol. 2013;156:190–194. doi: 10.1016/j.ajo.2013.02.004. [DOI] [PubMed] [Google Scholar]
- 81.Buck D, Powell CJ, Rahi J, Cumberland P, Tiffin P, Taylor R, Sloper J, Davis H, Dawson E, Clarke MP (2012) The improving outcomes in intermittent exotropia study: outcomes at 2 years after diagnosis in an observational cohort. BMC Ophthalmol 12. 10.1186/1471-2415-12-1 [DOI] [PMC free article] [PubMed]
- 82.Yulek F, Velez FG, Isenberg SJ, Demer JL, Pineles SL. Binocular summation and control of intermittent exotropia. Strabismus. 2017;25:81–86. doi: 10.1080/09273972.2017.1318929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Haggerty H, Richardson S, Hrisos S, Strong NP, Clarke MP. The Newcastle Control Score: a new method of grading the severity of intermittent distance exotropia. Br J Ophthalmol. 2004;88:233–235. doi: 10.1136/bjo.2003.027615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Wang C, Wang L, Ren M, Wang Q. Far distance control scores for assessing intermittent exotropia. J AAPOS. 2017;21:278–281. doi: 10.1016/j.jaapos.2017.04.007. [DOI] [PubMed] [Google Scholar]
- 85.Mohney BG, Holmes JM (2006) An office-based scale for assessing control in intermittent exotropia. Strabismus 14(3):147–50. 10.1080/09273970600894716 [DOI] [PMC free article] [PubMed]
- 86.Moon Y, Kim H, Kim DH, Lim HT. LACTOSE control scoring helps predict surgical outcomes for childhood intermittent exotropia. Can J Ophthalmol. 2019;54:659–663. doi: 10.1016/j.jcjo.2019.02.017. [DOI] [PubMed] [Google Scholar]
- 87.Beck RW. Spontaneous resolution of early-onset esotropia: Experience of the congenital esotropia observational study. Am J Ophthalmol. 2002;133:109–118. doi: 10.1016/S0002-9394(01)01316-2. [DOI] [PubMed] [Google Scholar]
- 88.Chia A, Seenyen L, Long QB. Surgical experiences with two-muscle surgery for the treatment of intermittent exotropia. J AAPOS. 2006;10:206–211. doi: 10.1016/j.jaapos.2005.11.015. [DOI] [PubMed] [Google Scholar]
- 89.Leow PL, Ko STC, Wu PKW, Chan CWN. Exotropic drift and ocular alignment after surgical correction for intermittent exotropia. J Pediatr Ophthalmol Strabismus. 2010;47:12–16. doi: 10.3928/01913913-20100106-04. [DOI] [PubMed] [Google Scholar]
- 90.Xie F, Zhao K, Zhang W. Comparison of surgical outcomes between bilateral recession and unilateral recession-resection in moderate-angle intermittent exotropia. J AAPOS. 2019;23:79.e1–79.e7. doi: 10.1016/j.jaapos.2018.11.007. [DOI] [PubMed] [Google Scholar]
- 91.Alvarez TL, Vicci VR, Alkan Y, Kim EH, Gohel S, Barrett AM, Chiaravalloti N, Biswal BB (2010) Vision therapy in adults with convergence insufficiency: clinical and functional magnetic resonance imaging measures. Optom Vis Sci 87(12):E985–1002. 10.1097/OPX.0b013e3181fef1aa [DOI] [PMC free article] [PubMed]
- 92.Alvarez TL, Jaswal R, Gohel S, Biswal BB. Functional activity within the frontal eye fields, posterior parietal cortex, and cerebellar vermis significantly correlates to symmetrical vergence peak velocity: an ROI-based, fMRI study of vergence training. Front Integr Neurosci. 2014;8:50. doi: 10.3389/fnint.2014.00050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Ouyang J, Yang L, Huang X, Zhong YL, Hu PH, Zhang Y, Pei CG, Shao Y. The atrophy of white and gray matter volume in patientswith comitant strabismus: Evidence from a voxel-based morphometry study. Mol Med Rep. 2017;16:3276–3282. doi: 10.3892/mmr.2017.7006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Shao Y, Li QH, Li B, Lin Q, Su T, Shi WQ, Zhu PW, Yuan Q, Shu YQ, He Y, Liu WF, Ye L. Altered brain activity in patients with strabismus and amblyopia detected by analysis of regional homogeneity: a resting-state functional magnetic resonance imaging study. Mol Med Rep. 2019;19:4832–4840. doi: 10.3892/mmr.2019.10147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Huang X, Li SH, Zhou FQ, Zhang Y, Zhong YL, Cai FQ, Shao Y, Zeng XJ. Altered intrinsic regional brain spontaneous activity in patients with comitant strabismus: a resting-state functional MRI study. Neuropsychiatr Dis Treat. 2016;12:1303–1308. doi: 10.2147/NDT.S105478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Yang X, Zhang J, Lang L, Gong Q, Liu L. Assessment of cortical dysfunction in infantile esotropia using fMRI. Eur J Ophthalmol. 2014;24:409–416. doi: 10.5301/ejo.5000368. [DOI] [PubMed] [Google Scholar]
- 97.Chan ST, Tang KW, Lam KC, Chan LK, Mendola JD, Kwong KK. Neuroanatomy of adult strabismus: a voxel-based morphometric analysis of magnetic resonance structural scans. Neuroimage. 2004;22:986–994. doi: 10.1016/j.neuroimage.2004.02.021. [DOI] [PubMed] [Google Scholar]
- 98.Goodale MA, Milner AD. Separate visual pathways for perception and action. Trends Neurosci. 1992;15:20–25. doi: 10.1016/0166-2236(92)90344-8. [DOI] [PubMed] [Google Scholar]
- 99.Borsook D, Maleki N, Burstein R. Migraine. In: Neurobiology of brain disorders: biological basis of neurological and psychiatric disorders. Elsevier Inc.; 2015. pp. 693–708. [Google Scholar]
- 100.Cavanna AE, Trimble MR. The precuneus: a review of its functional anatomy and behavioural correlates. Brain. 2006;129:564–583. doi: 10.1093/brain/awl004. [DOI] [PubMed] [Google Scholar]
- 101.Wenderoth N, Debaere F, Sunaert S, Swinnen SP. The role of anterior cingulate cortex and precuneus in the coordination of motor behaviour. Eur J Neurosci. 2005;22:235–246. doi: 10.1111/j.1460-9568.2005.04176.x. [DOI] [PubMed] [Google Scholar]
- 102.Buisseret P. Influence of extraocular muscle proprioception on vision. Physiol Rev. 1995;75:323–338. doi: 10.1152/physrev.1995.75.2.323. [DOI] [PubMed] [Google Scholar]
- 103.Steinbach MJ. Proprioceptive knowledge of eye position. Vision Res. 1987;27:1737–1744. doi: 10.1016/0042-6989(87)90103-9. [DOI] [PubMed] [Google Scholar]
- 104.Weir CR, Knox PC, Dutton GN. Does extraocular muscle proprioception influence oculomotor control? Br J Ophthalmol. 2000;84:1071–1074. doi: 10.1136/BJO.84.9.1071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Brodsky MC, Donahue SP, Vaphiades M, Brandt T. Skew deviation revisited. Surv Ophthalmol. 2006;51:105–128. doi: 10.1016/J.SURVOPHTHAL.2005.12.008. [DOI] [PubMed] [Google Scholar]
- 106.Donahue SP, Itharat P. A-pattern strabismus with overdepression in adduction: a special type of bilateral skew deviation? J AAPOS Off Publ Am Assoc Pediatr Ophthalmol Strabismus. 2010;14:42–46. doi: 10.1016/J.JAAPOS.2009.11.009. [DOI] [PubMed] [Google Scholar]
- 107.Schmidt KF, Löwel S. Strabismus modifies intrinsic and inter-areal connections in cat area 18. Neuroscience. 2008;152:128–137. doi: 10.1016/J.NEUROSCIENCE.2007.08.038. [DOI] [PubMed] [Google Scholar]
- 108.Yan X, Lin X, Wang Q, Zhang Y, Chen Y, Song S, Jiang T (2010) Dorsal visual pathway changes in patients with comitantextropia. PLoS One 5.10.1371/journal.pone.0010931 [DOI] [PMC free article] [PubMed]
- 109.Huang X, Li HJ, Zhang Y, Peng DC, Hu PH, Zhong YL, Zhou FQ, Shao Y. Microstructural changes of the whole brain in patients with comitant strabismus: evidence from a diffusion tensor imaging study. Neuropsychiatr Dis Treat. 2016;12:2007–2014. doi: 10.2147/NDT.S108834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Zhu PW, Huang X, Ye L, Jiang N, Zhong YL, Yuan Q, Zhou FQ, Shao Y. Altered intrinsic functional connectivity of the primary visual cortex in youth patients with comitant exotropia: a resting state fMRI study. Int J Ophthalmol. 2018;11:668–673. doi: 10.18240/ijo.2018.04.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Innocenti GM, Frost DO. Effects of visual experience on the maturation of the efferent system to the corpus callosum. Nature. 1979;280:231–234. doi: 10.1038/280231a0. [DOI] [PubMed] [Google Scholar]
- 112.Pietrasanta M, Restani L, Caleo M (2012) The corpus callosum and the visual cortex: Plasticity is a game for two. Neural Plast 2012:838672. 10.1155/2012/838672 [DOI] [PMC free article] [PubMed]
- 113.Ten Tusscher MPM, Houtman AC, De Mey J, Van Schuerbeek P. Cortical visual connections via the corpus callosum are asymmetrical in human infantile esotropia. Strabismus. 2018;26:22–27. doi: 10.1080/09273972.2017.1418898. [DOI] [PubMed] [Google Scholar]
- 114.Berman NE, Payne BR. Alterations in connections of the corpus callosum following convergent and divergent strabismus. Brain Res. 1983;274:201–212. doi: 10.1016/0006-8993(83)90697-2. [DOI] [PubMed] [Google Scholar]
- 115.Elberger AJ. The role of the corpus callosum in the development of interocular eye alignment and the organization of the visual field in the cat. Exp Brain Res. 1979;36:71–85. doi: 10.1007/BF00238468. [DOI] [PubMed] [Google Scholar]
- 116.Elberger AJ, Hirsch HVB. Divergent strabismus following neonatal callosal section is due to a failure of convergence. Brain Res. 1982;239:275–278. doi: 10.1016/0006-8993(82)90851-4. [DOI] [PubMed] [Google Scholar]
- 117.Payne BR, Berman N, Murphy EH. A quantitative assessment of eye alignment in cats after corpus callosum transection. Exp Brain Res. 1981;43:371–376. doi: 10.1007/BF00238379. [DOI] [PubMed] [Google Scholar]
- 118.Goyal R, Watts P, Hourihan M. Ocular findings in pediatric patients with partial agenesis of the corpus callosum. J Pediatr Ophthalmol Strabismus. 2010;47:236–241. doi: 10.3928/01913913-20090918-06. [DOI] [PubMed] [Google Scholar]
- 119.Watroba L, Buser P, Milleret C. Impairment of binocular vision in the adult cat induces plastic changes in the callosal cortical map. Eur J Neurosci. 2001 doi: 10.1046/j.0953-816X.2001.01720.x. [DOI] [PubMed] [Google Scholar]
- 120.Frost DO, Moy YP. Effects of dark rearing on the development of visual callosal connections. Exp Brain Res. 1989;78:203–213. doi: 10.1007/BF00230700. [DOI] [PubMed] [Google Scholar]
- 121.Lund RD, Mitchell DE. The effects of dark-rearing on visual callosal connections of cats. Brain Res. 1979;167:172–175. doi: 10.1016/0006-8993(79)90273-7. [DOI] [PubMed] [Google Scholar]
- 122.Milleret C. Visual callosal connections and strabismus. Behav Brain Res. 1994;64:85–95. doi: 10.1016/0166-4328(94)90121-X. [DOI] [PubMed] [Google Scholar]
- 123.Mizuno H, Hirano T, Tagawa Y. Evidence for activity-dependent cortical wiring: formation of interhemispheric connections in neonatal mouse visual cortex requires projection neuron activity. J Neurosci. 2007;27:6760–6770. doi: 10.1523/JNEUROSCI.1215-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Innocenti GM, Clarke S, Kraftsik R. Intercharge of callosal and association projections in the developing visual cortex. J Neurosci. 1986;6:1384–1409. doi: 10.1523/jneurosci.06-05-01384.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Tagawa Y, Mizuno H, Hirano T. Activity-dependent development of interhemispheric connections in the visual cortex. Rev Neurosci. 2008;19:19–28. doi: 10.1515/REVNEURO.2008.19.1.19. [DOI] [PubMed] [Google Scholar]
- 126.Atkinson J, Anker S, Braddick O, Nokes L, Mason a, Braddick F, Visual and visuospatial development in young children with Williams syndrome. Dev Med Child Neurol. 2001;43:330–337. doi: 10.1017/S0012162201000615. [DOI] [PubMed] [Google Scholar]
- 127.Spencer J, O’Brien J, Riggs K, Braddick O, Atkinson J, Wattam-Bell J. Motion processing in autism: evidence for a dorsal stream deficiency. NeuroReport. 2000;11:2765–2767. doi: 10.1097/00001756-200008210-00031. [DOI] [PubMed] [Google Scholar]
- 128.Hansen PC, Stein JF, Orde SR, Winter JL, Talcott JB. Are dyslexics’ visual deficits limited to measures of dorsal stream function? NeuroReport. 2001;12:1527–1530. doi: 10.1097/00001756-200105250-00045. [DOI] [PubMed] [Google Scholar]
- 129.Atkinson J, Braddick O. Visual and visuocognitive development in children born very prematurely. Prog Brain Res. 2007;164:123–149. doi: 10.1016/S0079-6123(07)64007-2. [DOI] [PubMed] [Google Scholar]
- 130.Santos A, Duret M, Mancini J, Gire C, Deruelle C. Preterm birth affects dorsal-stream functioning even after age 6. Brain Cogn. 2009;69:490–494. doi: 10.1016/J.BANDC.2008.10.005. [DOI] [PubMed] [Google Scholar]
- 131.Atkinson J, Braddick O. From genes to brain development to phenotypic behavior: “dorsal-stream vulnerability” in relation to spatial cognition, attention, and planning of actions in Williams syndrome (WS) and other developmental disorders. Prog Brain Res. 2011;189:261–283. doi: 10.1016/B978-0-444-53884-0.00029-4. [DOI] [PubMed] [Google Scholar]
- 132.Santhan Gopal K, Jayadev C, Thomas S, Gopal S. Looking beyond occlusion: a novel perspective for amblyopia treatment. Indian J Ophthalmol. 2020;68:2462. doi: 10.4103/IJO.IJO_741_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Creel DJ. Visual and auditory anomalies associated with Albinism. University of Utah Health Sciences Center; 1995. [PubMed] [Google Scholar]
- 134.Montero VM, Guillery RW. Abnormalities of the cortico-geniculate pathway in siamese cats. J Comp Neurol. 1978;179:1–12. doi: 10.1002/CNE.901790102. [DOI] [PubMed] [Google Scholar]
- 135.Guillery R, Hickey T, Kaas J, Felleman D, Debruyn E, Sparks D. Abnormal central visual pathways in the brain of an albino green monkey (Cercopithecus aethiops) J Comp Neurol. 1984;226:165–183. doi: 10.1002/CNE.902260203. [DOI] [PubMed] [Google Scholar]
- 136.Kinnear PE, Jay B, Witkop CJ. Albinism. Surv Ophthalmol. 1985;30:75–101. doi: 10.1016/0039-6257(85)90077-3. [DOI] [PubMed] [Google Scholar]
- 137.St John R, Timney B. Sensitivity deficits consistent with aberrant crossed visual pathways in human albinos. Invest Ophthalmol Vis Sci. 1981;21:873–877. [PubMed] [Google Scholar]
- 138.Witkop CJ, Jay B, Creel D, Guillery RW. Optic and otic neurologic abnormalities in oculocutaneous and ocular albinism. Birth Defects Orig Artic Ser. 1982;18:299–318. [PubMed] [Google Scholar]
- 139.Mcketton L, Kelly KR, Schneider KA. Abnormal lateral geniculate nucleus and optic chiasm in human albinism. J Comp Neurol. 2014;522:2680–2687. doi: 10.1002/CNE.23565. [DOI] [PubMed] [Google Scholar]
- 140.Elliott S, Shafiq A. Interventions for infantile esotropia. In: Elliott S, editor. Cochrane Database of Systematic Reviews. Chichester, UK: John Wiley & Sons Ltd; 2013. p. CD004917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Hatt SR, Gnanaraj L (2013) Interventions for intermittent exotropia. In: Hatt SR (ed) Cochrane Database of Systematic Reviews. John Wiley & Sons, Ltd, Chichester, UK, p CD003737 [DOI] [PubMed]
- 142.Issaho DC, Wang SX, Weakley DR. Intermittent exotropia surgery: results in different age groups. Arq Bras Oftalmol. 2017;80:355–358. doi: 10.5935/0004-2749.20170087. [DOI] [PubMed] [Google Scholar]
- 143.Choi MY, Hwang JM. The long-term result of slanted medial rectus resection in exotropia of the convergence insufficiency type. Eye. 2006;20:1279–1283. doi: 10.1038/sj.eye.6702095. [DOI] [PubMed] [Google Scholar]
- 144.Lee HJ, Kim SJ. Long-term outcomes following resection-recession versus plication-recession in children with intermittent exotropia. Br J Ophthalmol. 2020;104:350–356. doi: 10.1136/bjophthalmol-2018-313711. [DOI] [PubMed] [Google Scholar]
- 145.Leffler CT, Vaziri K, Schwartz SG, Cavuoto KM, McKeown CA, Kishor KS, Janot AC. Rates of reoperation and abnormal binocularity following strabismus surgery in children. Am J Ophthalmol. 2016;162:159–166.e9. doi: 10.1016/j.ajo.2015.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Christensen MR, Pierson K, Leffler CT. Reoperation following strabismus surgery among Medicare beneficiaries: associations with geographic region, academic affiliation, surgeon volume, and adjustable suture technique. Indian J Ophthalmol. 2018;66:1149–1153. doi: 10.4103/ijo.IJO_18_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Kassem A, Xue G, Gandhi NB, Tian J, Guyton DL. Adjustable suture strabismus surgery in infants and children: a 19-year experience. J Am Assoc Pediatr Ophthalmol Strabismus. 2018;22:174–178.e1. doi: 10.1016/j.jaapos.2018.01.013. [DOI] [PubMed] [Google Scholar]
- 148.Jacobs SM, Green-Simms A, Diehl NN, Mohney BG. Long-term follow-up of acquired nonaccommodative esotropia in a population-based cohort. Ophthalmology. 2011;118:1170–1174. doi: 10.1016/j.ophtha.2010.10.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Dombrow M, Engel HM. Rates of strabismus surgery in the United States: Implications for manpower needs in pediatric ophthalmology. J Am Assoc Pediatr Ophthalmol Strabismus. 2007;11:330–335. doi: 10.1016/j.jaapos.2007.05.010. [DOI] [PubMed] [Google Scholar]
- 150.Astle AT, Foulsham T, Foss AJ, McGraw PV. Is the frequency of adult strabismus surgery increasing? Ophthalmic Physiol Opt. 2016;36:487–493. doi: 10.1111/opo.12306. [DOI] [PubMed] [Google Scholar]
- 151.Bruenech JR. Neuroanatomical structures in extraocular muscles and their potential implication in the management of strabismus. Adv Ophthalmol Optom. 2021;6:39–53. doi: 10.1016/J.YAOO.2021.04.004. [DOI] [PubMed] [Google Scholar]
- 152.Schiavi C (2016) Extraocular muscles tension, tonus, and proprioception in infantile strabismus: role of the oculomotor system in the pathogenesis of infantile strabismus—review of the literature. Scientifica (Cairo) 2016. 10.1155/2016/5790981 [DOI] [PMC free article] [PubMed]