Abstract
Introduction
While trends in analgesia have been identified in high-income countries, little research exists regarding analgesia administration in low- and middle-income countries (LMIC). This study evaluates analgesia administration and clinical characteristics among patients seeking emergency injury care at University Teaching Hospital-Kigali in Kigali, Rwanda.
Methods
This retrospective, cross-sectional study utilized a random sample of emergency center (EC) cases accrued between July 2015 and June 2016. Data was extracted from the medical record for patients who had an injury and were ≥ 15 years of age. Injury-related EC visits were identified by presenting complaint or final discharge diagnosis. Sociodemographic information, injury mechanism and type, and analgesic medications ordered and administered were analyzed.
Results
Of the 3,609 random cases, 1,329 met eligibility and were analyzed. The study population was predominantly male (72%) with a median age of 32 years and range between 15 and 81 years. In the studied sample, 728 (54.8%) were treated with analgesia in the EC. In unadjusted logistic regression, only age was not a significant predictor of receiving pain medication and was excluded from the adjusted analysis. In the adjusted model, all predictors remained significant, with being male, having at least one severe injury, and road traffic accident (RTA) as injury mechanism being significant predictors of analgesia administration.
Conclusion
In the study setting of injured patients in Rwanda, being male, involved in RTA or having more than one serious injury was associated with higher odds of receiving pain medication. Approximately half of the patients with traumatic injuries received pain medications, predominantly opioids with no factors predicting whether a patient would receive opioids versus other medications. Further research on implementation of pain guidelines and drug shortages is warranted to improve pain management for injured patients in the LMIC setting.
Keywords: Trauma, Pain management, Analgesia, Rwanda
African relevance
-
•
Pain management in trauma has not been well-evaluated in the Rwandan or African low- and middle-income setting.
-
•
Pain management research is relevant given the global opioid crisis.
-
•
Pain management in trauma is critical for improved patient outcomes.
Introduction
Pain is an “unpleasant sensory and emotional experience associated with actual or potential tissue damage [1].” In United States and Canada, pain represents the main complaint of patients presenting to emergency centers (EC) seeking care, in some studies accounting for 78% of visits [2]. Providing adequate and timely pain management to injured patients is critical for healthcare providers [3].
Traumatic injuries account for 10% of deaths worldwide, more than malaria, HIV and tuberculosis combined [4]. The burden of trauma primarily occurs in low-and middle-income countries (LMICs) with less favorable morbidity and mortality outcomes due to poor infrastructure, inadequate and unwell functional emergency medical services, and lack of primary prevention [5]. Appropriate pain management with analgesic medications for injured patients has been shown to improve patient's outcome, healing, reduce stress, shorten hospital length of stay, lower cost and decrease the risk of chronic pain. Overall patient morbidity and mortality can be substantially reduced with proper pain control [6,7].
Many injured patients worldwide do not receive adequate or timely analgesia for pain relief [8]. The undertreatment of acute pain, oligoanalgesia, is related to geographical factors, lack of resources and inadequate assessment and training for clinicians working in LMIC ECs [9,10]. Even in high income countries (HICs), studies suggest that up to 70% of trauma patients with pain due to acute fractures do not receive analgesia in the EC. Among those who do receive analgesia, approximately 40% do not receive treatment for more than two hours after presentation [8].
Several studies demonstrate disparities in the treatment of pain. Effective administration of analgesia can differ based on many factors, revealing vulnerable groups. Women with isolated extremity injury are less likely to receive analgesia than men in the prehospital setting, and people with higher socioeconomic status are treated with more analgesic medications as compared to those of lower socioeconomic status [11]. Furthermore, children receive less analgesia than adults in healthcare settings [12].
To address oligoanalgesia, the assessment of pain at triage has been implemented in many countries. Time to analgesia and pain score documentation are important clinical indicators utilized in the assessment of EC quality of care and service delivered [13]. The use of triage pain assessment and numeric pain scales have demonstrated a decreased time to analgesia management [14]. The 0–10 Numerical Rating Scale (NRS) is one of the validated commonly used clinical assessment tools for pain [15]. The NRS has been implemented in Africa to improve pain management practices [16,17]. The Rwandan Ministry of Health created pain management guidelines and emphasized the importance of treating and recording pain [18].
In Rwanda and other African LMICs, cultural factors, lack of training, beliefs held by healthcare providers (e.g. that opioids cause addiction), physician shortages and overcrowded EDs are associated with poor pain treatment [19,20]. Additionally, Rwanda has experienced rapid development in roads, transportation (with increasing numbers of motorcycles, cars, and bicycles), and construction since 1994. This development has been associated with an increase in traumatic injuries, which reduce economic capacity at the levels of the individual and family, as well as at the larger national level through treatment costs [21]. Minimal data exists on analgesia administration practices in Rwanda. Given recent developments in emergency care and training programs in Rwanda, it is becoming increasingly important to ensure that pain treatment patterns are understood and improved [22]. In this study, provision of analgesia and clinical characteristics are evaluated among patients presenting for emergency injury care at University Teaching Hospital-Kigali (CHUK); a tertiary university-associated teaching hospital in Rwanda.
Methods
Setting and design
The study was carried out at CHUK, the primary public referral hospital in Kigali, Rwanda. The facility is an urban, tertiary-care institution with approximately 40 EC and 500 inpatient beds with access to specialty services, laboratory medicine and radiologic capabilities. The study site serves approximately 12 million Rwandans as the primary center for all seriously ill patients. CHUK has a dedicated EC with multiple medical and surgical specialists and subspecialists available for consultation.
Cases were identified and data were queried from CHUK records via protocolized methods, as previously described [22]. Using a multipoint composite index generated from a hospital electronic database, all EC cases during each month of the accruement periods (July 2015-June 2016) were identified. Subsequently all cases were coded with a unique identification number and were sampled at random until a sufficient number of records meeting inclusion criteria were identified (range: 135-165 records per month). Protocol-trained personnel abstracted data using a standardized instrument. Data procedures conformed to quality practices for chart review research [23]. Cases without identifiable medical records or lacking EC record documentation for the encounter of interest were excluded. The research was approved by CHUK's Ethics Committee as well as the University of Rwanda IRB.
Patient population
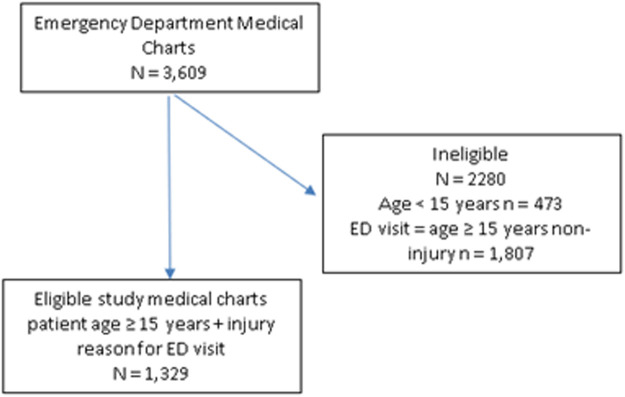
From 3,609 charts reviewed, 1,329 patient records met eligibility criteria and were analyzed. Ineligible charts were cases who presented to the EC with a non-injury complaint but age ≥ 15 (1,807) or were age <15 years (473) (Fig. 1). Adult patients with age ≥ 15 years presenting to the EC with an injury were included in the study. Cases less than 15 years of age are generally treated in a pediatric care area at CHUK unless they are critically ill. Thus, patients under 15 years of age were not included so as not to introduce bias. An injury-related EC visit was identified by the presenting complaint of accident, other traumatic injury, or a final discharge diagnosis of trauma. Patient sociodemographic information, injury mechanism and type, and analgesic medications ordered and administered were extracted from the database for analyses.
Fig. 1.
Flow diagram of study cases.
Data analysis
Data were imported into SAS (Carey N.C.) version 9.4 for analysis. Descriptive statistics analyses were conducted and presented as means with standard deviation or medians with interquartile range (IQR) and frequency. Documented reception of pain medication was the primary outcome variable of interest. Medications considered administered for pain were classified as an opioid (morphine, fentanyl, tramadol and pethidine), ketamine, and non-opioid analgesics (acetylsalicylic acid, paracetamol, and ibuprofen). Injury characteristics were classified by mechanism, type of injury and severity score (number of potentially life-threatening injuries no severe injury, 1,2, or > 2 severe injuries).
The odds of receiving any pain medication associated with patient characteristics (gender and age) and injury characteristics (mechanism, type, and severity) were estimated using logistic regression. The continuous age variable was centered around the median age for ease of interpretation. Given that road traffic accidents (RTAs) represented the most frequent injury mechanism this was reclassified as a binary variable mechanism: RTA or non-RTA. Unadjusted and adjusted odds ratios were reported, the adjusted models included predictors significant at the p < .05 level from the unadjusted models. Additionally, the odds of sedating versus non-sedating medication were evaluated using an adjusted logistic regression model.
Results
Patient characteristics
There were 1,329 patient records included that met the study eligibility criteria. The study population was majority male (n = 955, 72%) with a median age of 32 (IQR: 22,44) and range between 15 to 81 years. Of these patients, 780 (59%) arrived by emergency ambulance services, with the most frequent site of initial prehospital encounter being identified as a district hospital or community health center (n = 468, 35%).
Injury characteristics
The three most frequent causes of the injury across the sample and by gender were RTA (51.8%), fall (21.2%), and fight/stab/cut (11.3%,) (Table 1). RTA was significantly more frequent for males (54.5%) than females (44.6%; p = .001), while fall was significantly more frequent for females than males (30.9% v 17.5%; p < .0001). There was no significant difference between males and females in the frequency of fight, stab, cut injuries (12.3% v 9.8%). Blunt force injury was the only other injury with a significant difference between males and females (5.3% v 1.9%; p < .0001). There were 623 (46.9%) patients admitted after presenting to the ED with an injury.
Table 1.
Injury cause for sample and by gender.
| Injury Mechanism | All (N = 1329) n (%) |
Males (n = 956) n (%) |
Females (n = 373) n (%) |
Statistic |
|---|---|---|---|---|
| RTA | 688 (51.8) | 522 (54.5) | 166 (44.6) | χ2 (1) = 10.4, p = .001 |
| *Blunt force | 58 (4.4) | 51 (5.3) | 7 (1.9) | χ2 (1) = 7.1, p = .01 |
| Burn | 22 (1.7) | 12 (1.3) | 10 (2.7) | NS |
| Fall | 282 (21.2) | 167 (17.5) | 115 (30.9) | χ2 (1) = 28.8, p < .0001 |
| Gunshot | 2 (< 1) | 2 (<1) | 0 | NS |
| Strangulation | 1 (<1) | 1 (< 1) | 0 | NS |
| Animal | 12 (1) | 7 (1) | 5 (1.3) | NS |
| Fight/stab/cut | 150 (11.3) | 117 (12.3) | 33 (8.9) | NS |
| Landmine | 11 (1) | 7 (1) | 4 (1.1) | NS |
Blunt force = non-penetrating injury.
Patient injury type
A total of 2,624 injury types were documented, indicating that many patients had multiple injuries (median = 2, IQR: 1,2) The most common injury was a fracture (n = 546, 41.1% of patients had at least 1 fracture) of these 137 were documented as open (44.0%), closed (32.5%) or unknown (23.5%). The most frequently reported fracture areas were long bone fractures of the lower limb (n = 334, 43.9%) or upper limb (n = 133, 17.5%), the most common injury mechanism associated with fractures was an RTA (n = 311, 57% of fractures). Fractures of the skull were documented for 117 patients (15.4%), additionally, there were 382 head traumas documented that were not associated with a fracture (14.6% of all injury types). Most patients (n = 803, 60.8%) did not have a serious injury, with the remaining patients having one (n = 472, 35.6%) or more than one (n = 45, 3.4%) serious injury. The median injury severity score was 0 (IQR: 0,1).
Pain medications
There was documentation of pain medication ordered for 1,170 patients (88.1%), but pain medication administration (opioids, ketamine, non-opioid analgesics) was documented for 728 patients (54.8% of all patients, 62.2% of those with documented pain medication order). Some patients received administrations of multiple drug types; the total number of medications administered for pain was 1,117 with a median number of one type of drug administered (IQR: 1,2, range 1-5). The most common drug types administered for pain were opioid medications (728 ordered and documented as administered to 611 patients), followed by non-opioid analgesic medications (375 ordered and administered to 340 patients), and ketamine (n=11 ordered and administered to 11 patients) (Table 2).
Table 2.
Medications administered for pain (n=1,117).
| *Analgesic Medication | Frequency (n, %) |
|---|---|
| Opioid | |
| Tramadol | 391 (35.0) |
| Morphine | 238 (21.3) |
| Pethidine | 96 (8.6) |
| Fentanyl | 8 (< 1) |
| Non-opioid | |
| Paracetamol | 214 (19.2) |
| Ibuprofen | 148 (13.2) |
| Acetylsalicylic Acid | 11 (1) |
| Ketamine | 11 (1) |
Multiple medications were administered.
Among patients who received pain medications (n = 728), 103 (14.2%) patients received more than one opioid. Female patients were significantly less likely to receive pain medications compared to males (48.2% v 57.2%, p = .001). Among patients who received pain medications there were no significant differences in the number of females in contrast to males who were administered opioids (82.6% vs. 84.4%, p = .53) or non-opioid analgesics (47.7% vs. 46.1%, p = .61). the median injury score was significantly higher among patients who received opioid medications (median = 1 [IQR,0,1]) versus those who did not (median = 0 [IQR: 0,1]), p < .001. Opioid pain medications were administered to 49.5% of patients with long bone fractures, and 59.8% of patients with a severe injury.
Predictors of analgesic usage
Patient age (median 32 years), injury severity, gender, injury cause (RTA v other) were entered into a series of unadjusted logistic regression analysis to estimate the odds of receiving any pain medication. Only age was not a significant predictor and was excluded from the adjusted analysis (Table 3). In the adjusted model, all predictors remained significant, with being male, having at least one severe injury, and RTA as injury cause were significant predictors of being administered a pain medication.
Table 3.
Unadjusted and adjusted logistic regression model predicting any pain medication.
| Predictor/Referent | Unadjusted odds ratio (95%CI) |
Adjusted odds ratio (95%CI) |
|---|---|---|
| Sex: Female | 1.48 (1.16, 1.88) | 1.73 (1.38, 2.16) |
| Age: median centered = 32 | 1.0 (0.99, 1.01) | |
| Non MVC | 1.82 1.45, 2.24) | 1.73 (1.38, 2.16) |
| Non severe injury | 2.71 (2.52, 3.42) | 2.7 1 (2.14, 3.43) |
Discussion
This study provides insight into EC pain management for injuries in a LMIC setting. Gender was predictive with results indicating that males involved in RTAs, or have at least one severe injury, have higher odds of receiving pain medication. When comparing the mechanism of injury among males and females, males were more likely to be involved in RTAs (the majority of cases in this study). This may introduce confounding factors as RTAs are possibly more likely to have more serious injuries than other mechanisms such as blunt force or falls. Only age was found to not be a predictive factor in the odds of receiving pain medication.
Of the study cohort, 88.1% had pain medications ordered. However only 55.4% of those had medications documented as administered, it is not known why medications were ordered but not administered. Contributing factors may include perceived less serious injury or missing data. Most cases did not have a serious injury; 60.6% had no serious injury, 35.6% had one serious injury and 3.4% had more than one serious injury. This finding may contribute to why 45% of the total cohort did not receive any pain medication.
Providing adequate pain control is a common problem in LMIC ECs [24]. Some point to the importance of developing systems and protocols for doctors and nurses to ensure delivery of pain medications to injured patients [25,26]. Institutions that implement protocol-based pain management provided timely and superior pain relief [27]. Rwanda has developed pain management guidelines based on the WHO's Model Lists of Essential Medications for analgesia including non-opioids and NSAIDS, opioids, anticonvulsants, medications used for mood disorders and general anesthetics [28]. However, in Rwanda and other LMICs, shortages of medicines may affect a practitioner's pain management strategies [29]. Pain medications used in this study reflect what was commonly available at the time patients presented to the EC, however data regarding medications shortages was not available at the time of the study. The commonest medication given for pain was tramadol. Multiple studies suggest alternatives to tramadol for pain control that have a lower risk to benefit ratio as tramadol places the patient at risk for seizures, serotonin syndrome, fatal overdose and addiction. There is growing evidence of abuse of tramadol in African countries [30]. However, some clinicians in Ghana and Nigeria consider tramadol a useful medication because it is considered strong, fast-acting, better tolerated than non-steroidal anti-inflammatories (NSAIDs), less addictive than other opioids and relatively inexpensive [31]. Pethidine, also known as meperidine, has metabolites that can cause toxicity in the elderly and those with renal failure with increased risk of serotonin syndrome [32]. Acetylsalicylic Acid was used for acute pain control in this study, which is consistent Rwanda national guidelines, but differs from aspirin's common use for acute coronary syndromes in ECs of high-income countries [33].
Studies support the analgesic strategies used by EC practitioners in this study (opioid, non-opioids/NSAIDs and ketamine). Despite opioids being WHO Essential Medicines (https://www.who.int/medicines/publications/essentialmedicines/en/) in LMIC settings, opioid access can be limited related to medication costs [34]. Rwanda and other LMICs, have recently begun manufacturing morphine to mitigate supply chain issues as well as cost of procurement (https://apnews.com/article/health-ap-top-news-opioids-rwanda-international-news-4fb083a770cb916348943a2966579bc7). However, at the time of this study, opioids were still being imported and subject to supply-chain issues [35]. If opioids are scarce, research points to alternative strategies. Evidence suggests that a combination of paracetamol and an NSAID may offer superior analgesia compared with either drug alone in acute pain [36]. In renal colic, patients receiving NSAIDs achieve greater reductions in pain scores and are less likely to require further analgesia in the short term than those receiving opioids [37]. Ketamine has been used in clinical interventions for more than 30 years with research showing that intranasal ketamine can have similar analgesic effects to intranasal fentanyl. Due to fewer complications, comparable duration of action, and ease of use, ketamine can be a good choice for controlling pain in children [38]. Subdissociative IV ketamine provides analgesia with apparent safety comparable to that of IV morphine for short-term treatment of acute pain in the EC [39]. Ketamine had low percent use in our study, despite being available, suggesting room to expand its usage in Rwanda. Other alternatives to opioids include regional nerve blocks are a pain management option for orthopedic injuries in LMICs and have been shown to reduce pain and the need for IV opioids [40]. A previous study in Rwanda revealed that regional anesthesia offered improved analgesia with clear advantages including cost and avoidance of sedation [41].
Limitations
Many cases had missing data points such as medication ordered versus administration which may have introduced bias. However, records and data points appeared to be missing at random. Data regarding the amount, delivery, timing, frequency, and pain response to medications was insufficient and thus more studies are warranted to quantify use of analgesics among the injured in the study setting. Further research should include drug shortages impacting analgesic use. Moreover, this research was performed at a single tertiary-care hospital and may not be representative of other institutions or settings with different resources.
Conclusion
In the study setting of injured patients in Rwanda, being male, involved in RTA or having more than one serious injury was associated with higher odds of receiving pain medication. Approximately half of the patients with traumatic injuries received pain medications. The medications used in this study for acute pain were predominantly opioids. There were no factors predicting whether a patient would receive opioids versus other medications. Drug shortages were not known at the time of the study which may have impacted analgesic strategy. Further research on implementation of pain guidelines and drug shortages is warranted to improve pain management for injured patients in the LMIC setting.
Dissemination of results
Results from this study will be shared by the Rwandan first author to his colleagues (emergency medicine physicians) and other staff members (emergency nursing and pharmacy) at CHUK and Ruhengeri Referral Hospital. Results will be shared by email and Whatsapp groups as well as social media platforms.
Author contributions
Authors contributed as follows to the conception or design of the work; the acquisition, analysis or interpretation of data for the work; and drafting the work or revising it critically for important intellectual content: JM contributed 25%, MG 20%, NK 15%, MBH 10%; and BGD, ARA, JPN, AM, JB, and KM 5% each. All authors approved the version to be published and agreed to be accountable for all aspects of the work.
Declaration of Competing Interest
The authors declare no conflicts of interest.
References
- 1.Pain terms: a list with definitions and notes on usage. Recommended by the IASP Subcommittee on Taxonomy. Pain. 1979;6(3):249. [PubMed] [Google Scholar]
- 2.Todd KH, Ducharme J, Choiniere M, et al. Pain in the emergency department: results of the pain and emergency medicine initiative (PEMI) multicenter study. J Pain. 2007;8(6):460–466. doi: 10.1016/j.jpain.2006.12.005. [DOI] [PubMed] [Google Scholar]
- 3.Woolner V, Ahluwalia R, Lum H, Beane K, Avelino J, Chartier LB. Improving timely analgesia administration for musculoskeletal pain in the emergency department. BMJ Open Qual. 2020;9(1) doi: 10.1136/bmjoq-2019-000797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wisborg T, Montshiwa TR, Mock C. Trauma research in low- and middle-income countries is urgently needed to strengthen the chain of survival. Scand J Trauma Resusc Emerg Med. 2011;19:62. doi: 10.1186/1757-7241-19-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization, “Injuries and violence: the facts.” 2010. [Online]. Available: https://www.who.int/violence_injury_prevention/key_facts/VIP_key_facts.pdf?ua=1.
- 6.Ahmad A, Bazargan-Hejazi S, Zadie ZH, Euasobhon P, Ketumarn P, Karbasfrushan A, et al. Pain management in trauma: a review study. J Inj Violence Res. Jul; 8 2016;(2):89–98. doi: 10.5249/jivr.v8i2.707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Castillo RC, Raja SN, Frey KP, et al. Improving pain management and long-term outcomes following high-energy orthopaedic trauma (pain study) [published correction appears in J Orthop Trauma. 2017 Sep;31(9):e308] J Orthop Trauma. 2017;31(Suppl 1):S71–S77. doi: 10.1097/BOT.0000000000000793. [DOI] [PubMed] [Google Scholar]
- 8.Motov SM, Khan AN. Problems and barriers of pain management in the emergency department: are we ever going to get better? J Pain Res. 2008;2:5–11. [PMC free article] [PubMed] [Google Scholar]
- 9.Size M., Soyannwo O.A., Justins D.M. Pain management in developing countries. Anaesthesia. 2007;62:38–43. doi: 10.1111/j.1365-2044.2007.05296.x. [DOI] [PubMed] [Google Scholar]
- 10.Rampanjato RM, Florence M, Patrick NC, Finucane BT. Factors influencing pain management by nurses in emergency departments in Central Africa. Emerg Med J. 2007;24(7):475–476. doi: 10.1136/emj.2006.045815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Michael GE, Sporer KA, Youngblood GM. Women are less likely than men to receive prehospital analgesia for isolated extremity injuries. Am J Emerg Med. 2007;25(8):901–906. doi: 10.1016/j.ajem.2007.02.001. [DOI] [PubMed] [Google Scholar]
- 12.Beyer JE, DeGood DE, Ashley LC, Russell GA. Patterns of postoperative analgesic use with adults and children following cardiac surgery. Pain. 1983;17(1):71–81. doi: 10.1016/0304-3959(83)90129-X. [DOI] [PubMed] [Google Scholar]
- 13.Hatherley C, Jennings N, Cross R. Time to analgesia and pain score documentation best practice standards for the emergency department - a literature review. Australas Emerg Nurs J. 2016;19(1):26–36. doi: 10.1016/j.aenj.2015.11.001. [DOI] [PubMed] [Google Scholar]
- 14.Nelson BP, Cohen D, Lander O, Crawford N, Viccellio AW, Singer AJ. Mandated pain scales improve frequency of ED analgesic administration. Am J Emerg Med. 2004;22(7):582–585. doi: 10.1016/j.ajem.2004.09.003. [DOI] [PubMed] [Google Scholar]
- 15.Ferreira-Valente MA, Pais-Ribeiro JL, Jensen MP. Validity of four pain intensity rating scales. Pain. 2011;152(10):2399–2404. doi: 10.1016/j.pain.2011.07.005. [DOI] [PubMed] [Google Scholar]
- 16.Dilunga G.D., Sawe H.R., Kulola I.B., et al. Pain assessment and management of trauma patients in an emergency department of a tertiary hospital in Tanzania. Saf Health. 2018;4:12. [Google Scholar]
- 17.Andualem AA, Lema GF, Nigatu YA, Ahmed SA. Assessment of Acute Pain Management and Associated Factors among Emergency Surgical Patients in Gondar University Specialized Hospital Emergency Department, Northwest Ethiopia, 2018: Institutional Based Cross-Sectional Study. Pain Res Treat. 2018;2018 doi: 10.1155/2018/5636039. 5636039. Published 2018 Dec 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ministry of Health, Republic of Rwanda. Pain Management Guidelines. PDF file. September 2012. file:///Users/home/Desktop/Rwanda_Pain_Management_Guidelines_15_11_2012.pdf.
- 19.Rampanjato RM, Florence M, Patrick NC, Finucane BT. Factors influencing pain management by nurses in emergency departments in Central Africa. Emerg Med J. Jul 2007;24(7):475–476. doi: 10.1136/emj.2006.045815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nyirigira G, Wilson RA, VanDenKerkhof EG, Goldstein DH, Twagirumugabe T, Mahaffey R, Parlow J, Johnson AP. Barriers and facilitators to postoperative pain management in Rwanda from the perspective of health care providers: a contextualization of the theory of planned behavior. Can J Pain. 2018 Apr 12;2(1):87–102. doi: 10.1080/24740527.2018.1451251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mbanjumucyo G, George N, Kearney A, Karim N, Aluisio AR, Mutabazi Z, Umuhire O, Enumah S, Scott JW, Uwitonze E, Nyinawankusi JD, Byiringiro JC, Kabagema I, Ntakiyiruta G, Jayaraman S, Riviello R, Levine AC. Epidemiology of injuries and outcomes among trauma patients receiving prehospital care at a tertiary teaching hospital in Kigali, Rwanda. Afr J Emerg Med. Dec 2016;6(4):191–197. doi: 10.1016/j.afjem.2016.10.001. Epub 2016 Oct 28. PMID: 30456094; PMCID: PMC6234177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Aluisio AR, Barry MA, Martin KD, Mbanjumucyo G, Mutabazi ZA, Karim N, Moresky RT, D'Arc Nyinawankusi J, Claude Byiringiro J, Levine AC. Impact of emergency medicine training implementation on mortality outcomes in Kigali, Rwanda: An interrupted time-series study. Afr J Emerg Med. Mar 2019;9(1):14–20. doi: 10.1016/j.afjem.2018.10.002. Epub 2018 Oct 13. PMID: 30873346; PMCID: PMC6400013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kaji AH, Schriger D, Green S. Looking through the retrospectoscope: reducing bias in emergency medicine chart review studies. Ann Emerg Med. Sep 2014;64(3):292–298. doi: 10.1016/j.annemergmed.2014.03.025. [DOI] [PubMed] [Google Scholar]
- 24.Haonga BT, Makupa JE, Muhina RI, Nungu KS. Pain management among adult patients with fractures of long bones at Muhimbili Orthopaedic Institute in Dar es Salaam. Tanzania. Tanzan J Health Res. 2011;13(4):107–111. doi: 10.4314/thrb.v13i4.56959. [DOI] [PubMed] [Google Scholar]
- 25.Awolola AM, Campbell L, Ross A. Pain management in patients with long-bone fractures in a district hospital in KwaZulu-Natal, South Africa. Afr J Prim Health Care Fam Med. 2015;7(1):818. doi: 10.4102/phcfm.v7i1.818. Published 2015 Dec 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Patil A, Srinivasarangan M, Ravindra P, Mundada H. Studying protocol-based pain management in the emergency department. J Emerg Trauma Shock. 2017;10(4):180–188. doi: 10.4103/JETS.JETS_83_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fosnocht DE, Swanson ER. Use of a triage pain protocol in the ED. Am J Emerg Med. 2007;25(7):791–793. doi: 10.1016/j.ajem.2006.12.020. [DOI] [PubMed] [Google Scholar]
- 28.Anekar AA, Cascella M. StatPearls [Internet] StatPearls Publishing; Treasure Island (FL): 2022. WHO analgesic ladder. [Updated 2022 Nov 15]https://www.ncbi.nlm.nih.gov/books/NBK554435/ Jan-. Available from: [PubMed] [Google Scholar]
- 29.Shukar S, Zahoor F, Hayat K, Saeed A, Gillani AH, Omer S, Hu S, Babar ZU, Fang Y, Yang C. Drug shortage: causes, impact, and mitigation strategies. Front Pharmacol. 2021 Jul 9;12 doi: 10.3389/fphar.2021.693426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Close BR. Tramadol: does it have a role in emergency medicine? Emerg Med Australas. 2005;17(1):73–83. doi: 10.1111/j.1742-6723.2005.00671.x. [DOI] [PubMed] [Google Scholar]
- 31.Yorke E, Oyebola FO, Otene SA, Klein A. Tramadol: a valuable treatment for pain in Ghana and Nigeria. Curr Med Res Opin. 2019;35(5):777–784. doi: 10.1080/03007995.2019.1585168. [DOI] [PubMed] [Google Scholar]
- 32.Weiner AL. Meperidine as a potential cause of serotonin syndrome in the emergency department. Acad Emerg Med. Feb 1999;6(2):156–158. doi: 10.1111/j.1553-2712.1999.tb01056.x. [DOI] [PubMed] [Google Scholar]
- 33.Redd CH, Diercks DB. Early aspirin use is associated with decreased 30-day mortality in acute coronary syndromes. Ann of Emerg Med. 2004;44(4):S45–S46. [Google Scholar]
- 34.Pastrana T, Wenk R, Radbruch L, Ahmed E, De Lima L. Pain treatment continues to be inaccessible for many patients around the globe: second phase of opioid price watch, a cross-sectional study to monitor the prices of opioids. J Palliat Med. 2017;20(4):378–387. doi: 10.1089/jpm.2016.0414. [DOI] [PubMed] [Google Scholar]
- 35.Bizimana T, Kayumba PC, Heide L. Prices, availability and affordability of medicines in Rwanda. PLoS One. Aug 3 2020;15(8) doi: 10.1371/journal.pone.0236411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ong CK, Seymour RA, Lirk P, Merry AF. Combining paracetamol (acetaminophen) with nonsteroidal antiinflammatory drugs: a qualitative systematic review of analgesic efficacy for acute postoperative pain. Anesth Analg. 2010;110(4):1170–1179. doi: 10.1213/ANE.0b013e3181cf9281. [DOI] [PubMed] [Google Scholar]
- 37.Holdgate A, Pollock T. Systematic review of the relative efficacy of non-steroidal anti-inflammatory drugs and opioids in the treatment of acute renal colic. BMJ. 2004;328(7453):1401. doi: 10.1136/bmj.38119.581991.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Abdolrazaghnejad A, Banaie M, Tavakoli N, Safdari M, Rajabpour-Sanati A. Pain management in the emergency department: a review article on options and methods. Adv J Emerg Med. 2018;2(4) doi: 10.22114/AJEM.v0i0.93. e45. Published 2018 Jun 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Motov S, Mann S, Drapkin J, Butt M, Likourezos A, Yetter E, Brady J, Rothberger N, Gohel A, Flom P, Mai M, Fromm C, Marshall J. Intravenous subdissociative-dose ketamine versus morphine for acute geriatric pain in the Emergency Department: a randomized controlled trial. Am J Emerg Med. Feb 2019;37(2):220–227. doi: 10.1016/j.ajem.2018.05.030. [DOI] [PubMed] [Google Scholar]
- 40.Ritcey B, Pageau P, Woo MY, Perry JJ. Regional nerve blocks for hip and femoral neck fractures in the emergency department: a systematic review. CJEM. 2016;18(1):37–47. doi: 10.1017/cem.2015.75. [DOI] [PubMed] [Google Scholar]
- 41.Ho M, Livingston P, Bould MD, et al. Barriers and facilitators to implementing a regional anesthesia service in a low-income country: a qualitative study. Pan Afr Med J. 2019;32:152. doi: 10.11604/pamj.2019.32.152.17246. [DOI] [PMC free article] [PubMed] [Google Scholar]