Abstract
Objective:
The therapeutic alliance is a dyadic process involving both patient and therapist perspectives. We investigated the effect of patient and therapist agreement on the alliance in cognitive behavioral therapy for depression.
Method:
Patients (N = 191) were drawn from two studies of cognitive behavioral therapy for depression provided over 16 weeks. Alliance data were collected from patients and therapists at the first four sessions. Patients provided symptom data at each session. We used multilevel polynomial regression with response surface analysis to investigate the effect of alliance agreement and disagreement on symptoms.
Results:
The within-person strength of patient and therapist rated alliance (given agreement) predicted lower within-person symptoms. The nature and degree of the discrepancy in patient and therapist alliance scores was not a significant predictor.
Conclusion:
Patients and therapist alliance strength in early sessions (given agreement) predicted greater symptom change. Future research is needed to examine whether specific patient characteristics can be used to identify for whom the alliance plays a more or less important role.
Keywords: alliance, congruence, cognitive behavioral therapy, depression
The relationship of the therapeutic alliance and treatment outcome is among the most frequently studied relationships in psychotherapy process research (Crits-Christoph et al., 2013). Recent meta-analytic findings have supported a small, yet reliable association (Flückiger et al., 2018; Flückiger et al., 2020). This association appears consistent across different measures of the alliance, treatment modalities, patient diagnostic information, clinical settings, and rater perspectives (i.e., patient versus therapist).
Defined broadly, the alliance involves agreement on goals and tasks of psychotherapy as well as the presence of a positive interpersonal bond between patient and therapist (Bordin, 1979). The alliance reflects a dyadic process in which both the patient and the therapist are continuously perceiving and influencing each other’s perspectives (Atzil-Slonim et al., 2015). Given the importance of each person in the relationship, some researchers have advocated for moving away from single observer perspectives on the alliance in favor of examining congruence, or agreement, in the perspectives on the alliance (Rozmarin et al., 2008). The correspondence between patient and therapist views on the alliance may provide more useful information about the alliance than either perspective alone.
Congruence in emotional experiences has been hypothesized to be adaptive for relationships (Anderson & Keltner, 2004). Gonzaga and colleagues (2007) tested this empirically in a sample of couples and found that emotion similarity and emotion convergence was related to relationship quality and relationship satisfaction. Theoretically, congruence in the therapeutic alliance may also be important (Pepinsky & Karst, 1964). Specifically, when the alliance is strong, high congruence suggests the patient and therapist both believe they agree about therapeutic goals and tasks. When the alliance is relatively weak for a therapist-patient dyad, high congruence suggests that both patient and therapist believe they have a strained relationship. The therapist’s recognition of this may enable them to take corrective action. Chen and colleagues (2016) studied deterioration in the therapeutic alliance (commonly called alliance ruptures) and found that therapists’ recognition of alliance ruptures was associated with higher next-session alliance ratings. Unlike more alliance-focused psychotherapies (Safran & Muran, 2000), the therapeutic alliance is not hypothesized to be a primary mechanism of change in cognitive behavioral therapy (CBT). Nonetheless, the alliance is still thought to be important in CBT. A weak alliance may serve as a context in which therapists’ efforts to help patients learn CBT strategies are less likely to meet with success. Thus, it is important to investigate the role of congruence in CBT specifically to learn more about how the therapist and patients’ perspectives on the alliance relate to outcomes in this context.
Prior studies have operationalized congruence by using difference scores and correlation coefficients characterizing the relationship of alliance ratings from each member of a therapeutic dyad (i.e., profile similarity correlations). Some of these studies have found a positive association between alliance congruence and outcomes. For example, Rozmarin et al. (2008) used profile similarity correlations to measure congruence in 22 patient-therapist dyads participating in brief relational therapy. Patients in their sample had heterogeneous diagnoses including mood, anxiety, and personality disorders. Alliance congruence was associated with improvements in therapist and patient ratings of treatment targets, therapist-rated evaluation of patients’ global functioning, and patient’s self-rated interpersonal problems. In another study, Kivlighan (2007) used the absolute value of difference scores to measure congruence in 53 patient-therapist dyads participating in therapy at two counseling centers. He found that agreement about the alliance was related to patient-rated session depth (i.e., ratings of the value and power of a session). Laws et al. (2017) also used a difference score model to measure patient-therapist differences in the alliance in 357 patients randomized to pharmacotherapy plus psychotherapy conditions in a chronic depression trial. They found alliance ratings became more similar over the course of therapy, and higher agreement was related to greater depressive symptom improvements on a pharmacotherapist-assessed measure of symptoms at posttreatment and a patient-reported assessment at the three-month follow-up. Discrepancy in alliance ratings early in psychotherapy did not predict post-treatment depressive symptoms or rate of change in symptoms. More recently, Coyne et al. (2018) characterized alliance convergence using the absolute value of difference scores in 85 individuals with severe generalized anxiety disorder receiving CBT alone or CBT integrated with motivational interviewing. Agreement on the alliance increased over time. Greater agreement on the alliance predicted larger decreases in subsequent worry and distress.
However, the broader literature on the relation of therapist and client perspectives on the alliance with outcome has been mixed. This may be at least in part because of problems with the use of difference scores (Cronbach & Furby, 1970) and profile similarity correlations (Cronbach & Gleser, 1953). These approaches combine data from both informants into a single score, which makes them more difficult to interpret. Further, they are less reliable than the scores that constitute them. To overcome these problems, some recent studies have examined congruence in the alliance by adapting the truth and bias model (West & Kenny, 2011). These studies distinguish congruence and directional discrepancy (Atzil-Slonim et al., 2015; Chen et al., 2018). Papers using this approach have investigated various questions, but studies using the approach to predict outcome have been limited. In one such study, Zilcha-Mano et al. (2017) found that congruence in the alliance predicted symptomatic outcomes one month later.
Using another approach to overcoming these problems, Marmarosh and Kivlighan (2012) drew on the use of polynomial regression and response surface analysis (RSA) used in organizational research (Edwards & Parry, 1993) to study the correspondence between patient and therapist alliance scores and how they relate to outcome. This approach uses a polynomial regression model and the coefficients from this model are then used in a second step to derive values for four parameters of interest. As shown in Figure 1, these parameters are the slope and curvature of the line of congruence and the slope and curvature of the line of incongruence. The line of congruence represents the strength of the alliance given perfect agreement. The line of incongruence represents differing amounts of divergence on the alliance, with higher therapist than client-rated alliance at one end of the line and higher client than therapist-rated alliance at the other end. RSA is used to calculate the model-predicted effect that a range of values of the alliance have on outcome. Thus, rather than characterizing how therapist and client ratings of the alliance are related to outcome directly, the results from these analyses characterize model predictions for how different patterns of therapist and client alliance ratings are related to outcome.
Figure 1. Lines of Congruence and Incongruence.
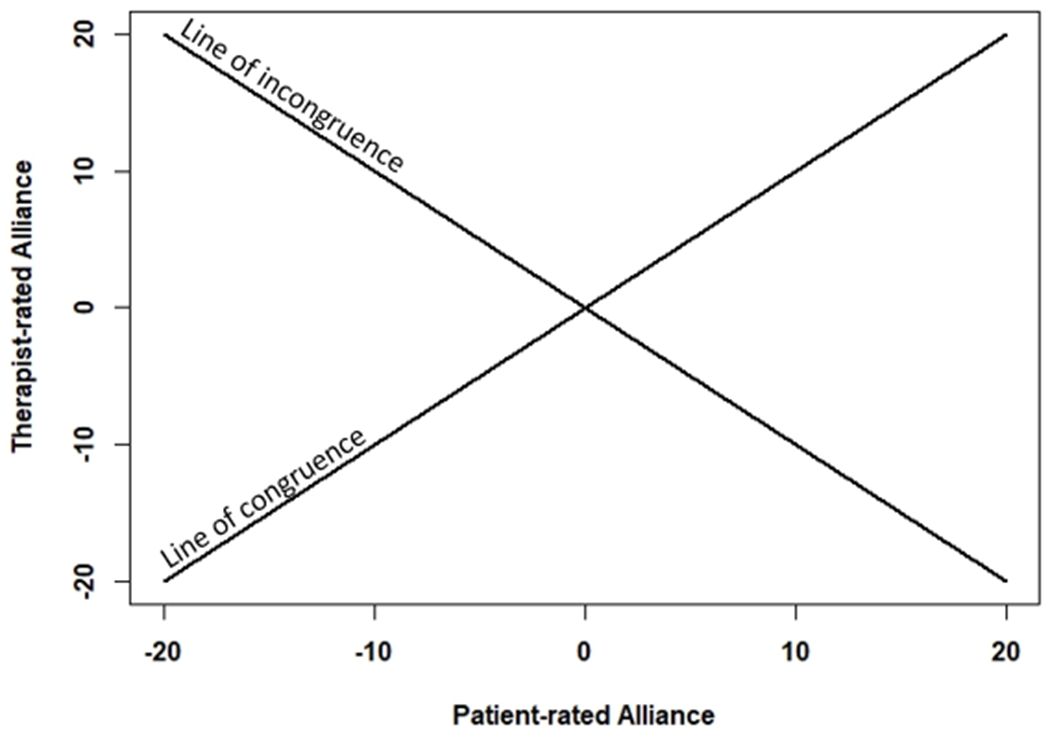
Note. This is a representation of the lines along which the response surface will be plotted. The line of congruence represents the strength of the alliance given perfect agreement. The line of incongruence represents divergence in therapist and client views of the alliance (ranging from the therapist viewing the alliance much more negatively than the client to the client viewing the alliance much more positively than the therapist).
The first parameter indicates how the model predicted effect of the strength of the alliance across therapist and client ratings on symptoms when therapists and clients agree in their alliance ratings. A significant positive value on this parameter is expected, as dyads who view the alliance as strong, who each believe the alliance is strong, are expected to be characterized by clients responding more positively to treatment. Agreement on a strong alliance is thought to be a marker of positive therapeutic activities that lead to symptom improvement. The second parameter indicates whether this relationship is curvilinear. Thus, it indicates whether each unit of agreement on a stronger alliance leads to the same amount of change, or whether the amount of symptom change varies at different levels of alliance strength. The third parameter indicates the effect of the signed degree of disagreement on the alliance. This parameter reflects the predictive value of a variable characterizing the extent to which, on one end, the therapist has higher alliance ratings than the patient, and on the other end, the patient has higher ratings than the therapist. The fourth parameter indicates the curvature of any effect of disagreement on symptoms. For example, in the case of a convex shape, model-predicted symptoms would increase more dramatically as the magnitude of disagreement is greater. These parameters are used to plot a three-dimensional response surface. Rather than depicting the original alliance ratings, the response surface is based on model-predicted values of symptoms at various values of patient and therapist rated alliance.
Only a handful of studies have utilized RSA to examine the effect of alliance congruence on treatment outcome in individual psychotherapy. In the earliest study of the alliance to use this method, Marmarosh and Kivlighan (2012) examined alliance agreement measured at session three in relation to overall symptom change in a sample of 63 therapeutic dyads from a counseling center and community mental health clinic. Their findings showed that the model predicted effect was for a strong alliance predicting lower symptoms when therapist and client agree. Unexpectedly, they also found that a greater discrepancy between alliance ratings predicted greater decreases in symptoms, regardless of the direction of the disagreement. In a related effort, Zilcha-Mano et al. (2017) performed a similar analysis in a sample of 127 therapist-patient dyads from an outpatient clinic. Drawing data from a randomly selected session, they found that the strength of the alliance (using model predictions for when there was agreement between therapist and client) predicted lower symptoms one month later. In their study, neither the degree nor the direction of disagreement was related to subsequent symptoms.
Using a large sample of 580 dyads in a cognitive behavioral outpatient clinic, Rubel et al. (2018) examined the relation between a specific aspect of the alliance, the therapeutic bond, and symptom improvement. Using a session-to-session approach, Rubel et al. found that the strength of the alliance ratings (using model predictions for when there was agreement between therapists and clients) predicted within-person next-session symptom change. They also found that greater disagreement over the bond predicted a decrease in next-session symptoms and patients rating the alliance more positively than therapists predicted less robust symptom improvement. In a sample of 361 dyads from an outpatient training clinic, Jennissen et al. (2020) examined alliance agreement at every fifth session in relation to symptoms five sessions later. Agreement on strong alliances predicted lower subsequent symptoms, but alliance disagreement did not predict subsequent symptoms.
While there appears to be growing support for agreement on strong alliances predicting symptoms, there are several remaining gaps in the literature. All of the studies that have investigated the effect of alliance congruence (broadly defined) on treatment outcome have involved highly heterogenous samples with a wide variety of diagnoses being treated and treatment manuals being used. It is unclear to what extent the heterogeneity within these samples might have contributed to the finding that the strength of the alliance predicts outcome. Samples composed of patients with a common principal diagnosis being treated with a common protocol would help to address this possibility. Second, the effect of discrepant alliance perspectives on therapeutic outcomes remains unclear. Heterogeneity in the samples studied and differences in the time between assessments across studies may have contributed to the mixed findings reported. Although the ideal interval for capturing such effects is unclear, there is reason to believe effects may occur over shorter intervals (Falkenström et al., 2013).
This Study
We use RSA to examine the relation of patient and therapist agreement on the alliance. In line with several other recent alliance-outcome studies using RSA, we will conduct within-person analyses. Any within-person relationship cannot be accounted for by stable between-person confounds (Wang & Maxwell, 2015; Falkenström et al., 2020). We also focused our analysis on patients with major depressive disorder (MDD) participating in a course of CBT (Beck et al., 1979). Patient-rated alliance in such treatments has been found to predict subsequent symptom change (Zilcha-Mano et al., 2016), but studies that have considered patient and therapist-rated alliance together have been quite limited.
Based on prior research, we had two hypotheses. First, we predicted that therapist and patient agreement on a stronger within-person alliance would predict lower within-person next-session depressive symptoms. Second, we predicted that lower levels of disagreement would predict lower levels of within-person symptoms in the subsequent session.
Methods
Participants
Participants were drawn from two prior studies of patients offered a 16-week course of CBT for depression. These studies had very similar inclusion and exclusion criteria. The first sample included 66 patients (see Adler et al., 2015) and the second sample had 125 patients (see Schmidt, Pfeifer, et al., 2019) for a combined total of 191 patients. For each dataset, one additional participant dropped out after their intake and could not be included in analyses. All patients provided informed consent prior to participating in research activities. Inclusion criteria for both samples were current MDD, being at least 18 years of age, and providing informed consent. Exclusion criteria for both samples were: a history of psychosis, bipolar I, a primary diagnosis other than MDD if it necessitated alternative treatment, current suicide or self-harm risk precluding outpatient treatment, substance dependence in the past six months, or clear indication of secondary gain (i.e., court-ordered treatment; no patients were excluded on this basis). The first study also planned to exclude patients with an IQ below 80 (with testing only occurring when clinically indicated), but no patients were excluded on this basis. The second study also excluded patients with a diagnosis of bipolar II. Diagnoses were assessed using the Structured Clinical Interview for the Diagnostic and Statistical Manual of Mental Disorders-IV (First et al., 2002).
In the combined sample, most participants were White (82%), and the next largest groups were African American (8%) and Asian American (7%). The modal patient (39%) completed some college. The majority of participants were female (58%), and the mean age of our sample was 33.5 (SD = 13.3, range = 18 - 70). The most common comorbid disorder was social anxiety disorder (34% of patients), followed by generalized anxiety disorder (28% of patients). The average BDI score at intake was 30.95 (SD = 8.82) which is comparable to other depression studies (e.g., de Graaf et al., 2009; Bruijniks et al., 2020). All participants provided consent and study procedures were approved by an institutional review board at our university.
Therapists and Treatment
Nine graduate students (five men and four women) served as therapists under the supervision of a licensed clinical psychologist (the last author). Treatment was provided according to a manual describing CBT for depression (Beck et al., 1979). In both studies, patients were pseudo-randomly assigned to therapists based on the number of openings in each therapist’s caseload with the additional constraint that a patient’s intake assessor could not serve as that patient’s therapist. Treatment was provided over 16 weeks, with the study protocol calling for twice weekly therapy sessions for the first four weeks and the patient and therapist collaboratively deciding whether and when to switch to weekly sessions after four weeks. For the final four weeks, the protocol called for weekly sessions.
Measures
Depression Severity
Depressive symptoms were assessed with the Beck Depression Inventory-II (BDI-II; Beck et al., 1996), a 21-item self-report measure. Participants completed the measure prior to each session. The BDI-II is a widely used measure with strong psychometric properties (Beck et al., 1996). In this sample, Cronbach’s alpha for the BDI-II ranged from .89-.93 across the sessions we examined.
Working Alliance
To assess the therapeutic alliance, we used the short form of the therapist-rated and client-rated Working Alliance Inventory (WAIT and WAIC respectively; Horvath & Greenberg, 1989; Tracey & Kokotovic, 1989), with each consisting of 12 items evaluated on a 7-point Likert scale (0 = never, 6 = always; reverse scored items were modified so that all items were positively keyed). The WAI shows excellent psychometric properties (Horvath & Greenberg, 1989). In this sample, Cronbach’s alpha across the sessions examined ranged from .94 - .98 for the WAIC and .95 - .96 for the WAIT. Patients and therapists filled out this measure following each of their first four sessions. Because the protocol called for twice weekly sessions, these ratings characterize the first two weeks of treatment.
Analytic Strategy
Response surface analysis (RSA) is a method for assessing the effects of informant congruence on a dependent variable. As described above, this method involves constructing a polynomial regression model, obtaining four parameters of interest from the model, and using these parameters to plot a response surface. We analyzed our data using R 4.0.2 (R Core Team, 2020). We used the two-level RSA approach described by Nestler and colleagues (2019). First, WAIC and WAIT were centered according to the patient-specific mean across both WAIC and WAIT combined (so that each variable is centered according to the same value). The reason for this centering procedure is that, to facilitate comparison of scores relative to the patient-specific means, the variables need to have the same zero point. Variables for WAIC squared, WAIT squared, and their interaction were constructed using these within-person centered variables.
Next, we evaluated a multilevel model with sessions nested within patients. The dependent variable was within-person centered BDI scores at the next session. We utilized four observations of WAIC and WAIT and five observations of BDI, so alliance ratings at each session could be examined as predictors of BDI scores at the next session (e.g., WAI at the end of session four predicted BDI at the start of session five). The polynomial regression contained ten predictors: patient-rated alliance (b1p), therapist-rated alliance (b2p), patient-rated alliance squared (b3p), the product of therapist-rated and patient-rated alliance (b4p), therapist-rated alliance squared (b5p), and each patient’s mean value on each of these predictors. The means of these five predictors are included in the model to ensure the model only estimates within-person variance. The within-person centering method alone did not guarantee this, because the variables were centered according to the aggregate mean of both WAIC and WAIT. The dependent variable was next-session within-person BDI scores. Nestler and colleagues (2019) advise inclusion of a random intercept as well as random effects for coefficients b1p-b5p, though they acknowledge this model will often fail to converge. We evaluated the initial model with all random effects included and intended to remove them as needed for model convergence. Following this approach, our final model included a random intercept and no other random effects. The basic Level 1 model for the symptom rating for session s+1 of patient p is as follows:
Where esp is a Level 1 residual.
The Level 2 equation for the random intercept is :
Where γ00 is the fixed-effects regression coefficient, u0p is a Level 2 residual term, and and are the predictor variables’ group means.
We used the coefficients from this model to obtain four response surface parameters. To obtain these parameters and plot the response surface, we used the RSA package (Schönbrodt & Humberg, 2020) and the code presented in Nestler and colleagues (2019). Parameter a1 represents the slope of the line of congruence (b1p + b2p); if this parameter is significant, it means that the strength of patient and therapist-rated alliance (given agreement between the two) predicts symptoms. Parameter a2, the curvature along the line of congruence (b3p + b4p + b5p), when significant, indicates that the association between alliance congruence and symptoms is quadratic: the strength of the association varies non-linearly as a function of alliance strength. Parameter a3 (b1p-b2p) is the slope of the line of incongruence, and, when significant, it indicates that the effect of disagreement on symptoms depends on the direction of disagreement. Specifically, a significant result would indicate that the effect of disagreement on symptoms depends on whether the patient has a greater alliance than the therapist or whether the therapist has a greater alliance than the patient. Parameter a4 (b3p - b4p + b5p), when significant, means that the line of incongruence is curvilinear, and the degree of patient and therapist disagreement on the alliance predicts symptoms. See Figure 1 for a representation of the line of congruence and the line of incongruence. It is also possible to obtain four response surface parameters from the between-level components of the polynomial regression model (γ01- γ05; Nestler et al., 2019). Therefore, we also evaluated the between-level response surface. We had 6% missing data in both WAIC and WAIT in sessions 1-4 and 8% missing data in BDI in sessions 2-5. Given the low amount of missing data, we opted not to impute missing values.
Results
We started by conducting independent samples t-tests to characterize the differences between patient-reported and therapist-reported working alliance. Table 1 shows the results of these t-tests. As the table shows, patient-rated alliance scores were significantly higher than therapist-rated scores with moderately sized differences across sessions.
Table 1.
Independent Samples t-tests Comparing Client and Therapist Rated Alliance
| Session | Client Rated | Therapist Rated | ||||||
|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | t | df | p | g | |
| Session 1 | 58.16 | 10.28 | 50.54 | 10.77 | 7.00 | 372 | < .001 | .72 |
| Session 2 | 58.52 | 10.56 | 52.27 | 11.08 | 5.51 | 361 | < .001 | .58 |
| Session 3 | 59.16 | 12.50 | 52.76 | 11.57 | 4.95 | 344 | < .001 | .53 |
| Session 4 | 60.36 | 11.09 | 53.16 | 10.80 | 6.14 | 347 | < .001 | .66 |
Next, we evaluated the multilevel model with a random intercept and five random coefficients. As noted earlier, this model did not converge. We examined the variance of the random effects and found it to be close to zero for all five of the random coefficients (with the largest, WAIT squared, having a value of 0.00006). As planned, we removed random effects one by one until the model converged. The final model converged with only a random intercept. As shown in Table 2, within-person patient-rated alliance significantly predicted within-person symptoms. We evaluated this model only as an initial step in calculating the response surface. We used the values from this model to calculate parameters a1-a4 (see Table 3). Only parameter a1 was significant. This parameter was negative, meaning that the within-person strength of patient-rated and therapist-rated alliance (given agreement) predicted lower within-person symptoms.
Table 2.
Two-Level Polynomial Regression Model Predicting Symptoms at the Next Session
| Parameter | Estimate (SE) | t | p |
|---|---|---|---|
| Fixed effects | |||
| Intercept | −0.89 (4.22) | −0.21 | .83 |
| Patient-rated alliance | −0.14 (0.05) | −3.01 | <.01 |
| Therapist-rated alliance | −0.06 (0.04) | −1.61 | .11 |
| Patient-rated alliance^2 | −0.00 (0.00) | −0.73 | .46 |
| Therapist-rated alliance ^2 | 0.00 (0.00) | −0.34 | .73 |
| Patient x therapist-rated alliance | 0.00 (0.00) | 0.96 | .34 |
| Patient-rated alliance mean | 0.02 (0.13) | 0.17 | .87 |
| Therapist-rated alliance mean | 0.03 (0.16) | 0.16 | .87 |
| Patient-rated alliance ^2 mean | 0.00 (0.00) | 0.97 | .33 |
| Therapist-rated alliance^2 mean | 0.00 (0.00) | 0.82 | .41 |
| Patient x therapist-rated alliance mean | −0.00 (0.00) | −1.20 | .23 |
| Error variance | |||
| Residual | 21.98 (4.69) | ||
| Intercept (patient) | 0.00 (0.00) |
Table 3.
Response Surface for Within-level Alliance and Subsequent Symptoms
| Effect | Coefficient | SE | z | p |
|---|---|---|---|---|
| a1 (slope along line of congruence) | −0.20 | 0.05 | −4.20 | <.001 |
| a2 (curvature along line of congruence) | 0.00 | 0.01 | 0.10 | .92 |
| a3 (slope along line of incongruence) | −0.07 | 0.07 | −1.10 | .28 |
| a4 (curvature along line of incongruence) | −0.01 | 0.01 | −1.21 | .23 |
Note. Parameter a1 indicates whether alliance agreement predicts symptoms. Parameter a2 indicates that the strength of the association between agreement and symptoms varies based on whether patients and therapists agree on a stronger or a weaker alliance. Parameter a3 indicates whether the effect of disagreement on symptoms differs between cases where patients rate the alliance as higher and cases where therapists rate the alliance as higher. Parameter a4 indicates whether patient and therapist disagreement on the alliance predicts symptoms.
We then used the values of the RSA parameters to graph the average response surface. In Figure 2, the x-axis contains all possible WAIC scores, WAIT scores are along the y-axis, and symptom scores are along the z-axis. The line of congruence runs from the nearest to the furthest corners of the plot; this line reflects the values at which therapists and patients have the same alliance ratings. As indicated by parameter a1, the line of congruence here had a significant negative slope. This is depicted in the figure; the nearest corner of the plot is higher than the furthest corner such that the surface has a downward tilt. At the nearest corner of the plot, alliance ratings for therapists and patients are at their lowest values. At the furthest corner, shared therapist and patient alliance ratings are at their highest, so the surface is tilted downward to represent the association with decreased within-person depressive symptoms.
Figure 2. Average Response Surface for Patient and Therapist Alliance and Depressive Symptoms.
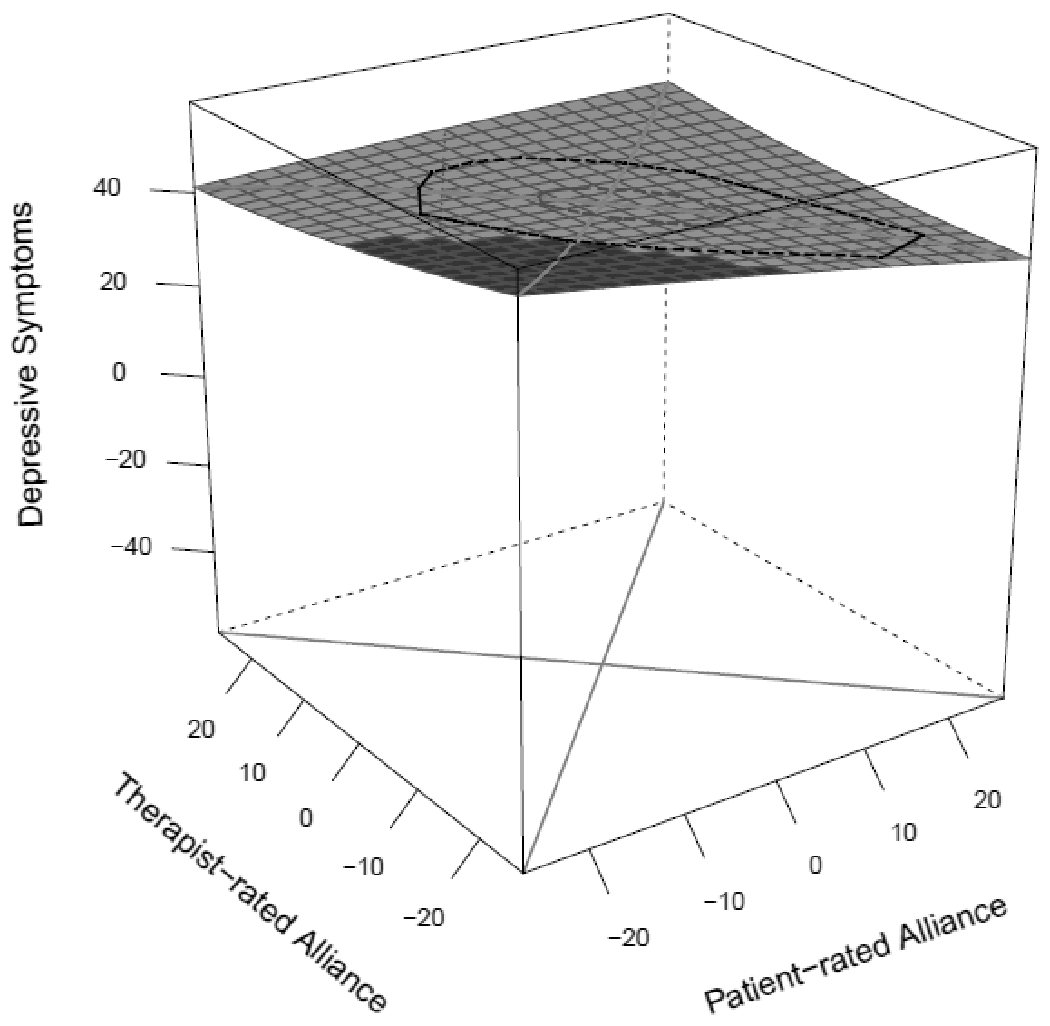
Note. Patient-rated alliance is on the horizontal axis, therapist-rated alliance is on the vertical axis, and depressive symptoms are on the depth axis. The line of congruence runs from the nearest corner to the farther corner and has a significant negative slope. This is represented by the slight downward tilt of the plane (the shaded region indicates values that are closer to the top of the graph). The line of congruence has a slight upward curvature, quantified by the positive value of parameter a2, which was not significantly different than zero. The line of incongruence runs from the left to the right of the figure. Its slope and curvature are quantified by parameters a3 and a4.
In Figure 2, the line of incongruence spans from the left to the right corners of the plot. This line is made up of values at which patient-rated alliance is equal to the negative value of therapist-rated alliance. Points further from the midpoint along this line represent a dyad having greater disagreement about the alliance. Points on the right of the line of incongruence are points at which the patient reported a stronger alliance than that patient’s therapist. As a point is further to the left of the line of incongruence, the more the therapist’s rating is higher than the patient’s rating for a dyad. The curvature and slope of this line, represented by parameters a3 and a4, were slightly negative but not significant. These parameters indicate whether alliance disagreement predicts symptoms and whether the effect of disagreement on symptoms differs when patient-rated versus therapist-rated alliance is higher.
We were primarily interested in within-person relationships because these relationships cannot be confounded by stable between-person variables. In the interest of comprehensiveness, we also calculated the between-person response surface. We estimated parameters a1-a4 and none were significant. We report these results in Table 4.
Table 4.
Response Surface for Between-level Alliance and Subsequent Symptoms
| Effect | Coefficient | SE | z | p |
|---|---|---|---|---|
| a1 (slope along line of congruence) | 0.05 | 0.16 | 0.30 | .77 |
| a2 (curvature along line of congruence) | −0.00 | 0.00 | −0.52 | .60 |
| a3 (slope along line of incongruence) | −0.00 | 0.24 | −0.02 | .99 |
| a4 (curvature along line of incongruence) | −0.00 | 0.00 | −1.03 | .30 |
Discussion
To our knowledge, this was the first study to investigate the patient and therapist perspectives of the alliance and their effects on symptoms using RSA in the context of CBT for depression. Further, our analyses were within-person, which allowed us to analyze the effects of a dyad having more positive or negative alliance scores than are typical for them, rather than simply analyzing overall alliance levels. In line with our first hypothesis, we found that within-person alliance strength (i.e., how positively the alliance is viewed across patients and therapists) predicted lower within-person next-session symptoms. This finding is consistent with past research that examined the effect of alliance congruence on treatment outcome using RSA in other contexts (i.e., Jennissen et al., 2020; Marmarosh & Kivlighan, 2012; Rubel et al., 2018; Zilcha-Mano et al., 2017). This is consistent with the possibility that the most effective work in CBT tends to occur when therapist and patient are both evaluating the alliance more positively than usual. Such consistent positive evaluations suggest that positive therapeutic benefits are likely to follow. In an analysis that used the same dataset as the present study, we modeled the reciprocal effects of alliance and outcome and found small but reliable within-person reciprocal effects (Whelen et al., 2021). Further, we found that the majority of variance (79%) in patient-rated alliance scores was between-person. The remaining 21% of variance consists of error and within-person variance. When within-person variance is relatively limited, detection of within-person effects is more difficult. Therefore, it is noteworthy that we nonetheless detected an effect of alliance strength on symptoms.
Our finding that a shared understanding of a strong alliance predicts outcome is consistent with the possibility that therapists might enhance outcome by fostering a more positive alliance and by working to foster a shared understanding of the alliance. Of course, there are multiple approaches one might take to doing this. For example, this could involve using CBT strategies to demonstrate their benefits to a client. Alternatively, it might involve identifying an alliance rupture and working to repair it. More research is needed to help uncover how therapists can best select strategies for fostering a more positive working alliance and creating a shared understanding of the alliance. We also predicted that lower levels of within-person disagreement on the alliance would predict lower levels of within-person depressive symptoms. However, we did not find support for this hypothesis. Previous findings regarding the impact of such disagreement have been mixed. Zilcha-Mano et al. (2017) and Jennissen et al. (2020) also did not find a significant relationship between alliance disagreement and symptoms. By contrast, Marmarosh and Kivlighan (2012) and Rubel et al. (2018) both found that greater disagreement predicted improved outcomes, and the latter study found that the magnitude of this effect depends on whether the patient or therapist rates the alliance as higher. These differences could be due to differences in the amount of disagreement present, differences in the sample and treatment being provided, or sampling variability.
Another possibility to consider is that disagreement in our sample took the form of patients having alliance scores that are greater than their typical alliance scores much more often than therapists. It may be that when patients have improved ratings, only this form of disagreement is not especially detrimental to outcomes, given that patient-rated improvements in the alliance predicts improved outcomes in this sample. Parameter a3 (the slope along the line of incongruence) was non-significant, thus suggesting that the difference between patient and therapist alliance ratings (e.g., patients having alliance ratings that are more improved than the therapist’s) did not predict outcome; however, therapists having improved ratings may have been uncommon enough that we did not have enough power to detect this effect.
Methodological differences may have also contributed to the inconsistent results across studies. While in this study we opted to use session-to-session data for four sessions, Zilcha-Mano et al. (2017) and Marmarosh and Kivlighan (2012) used alliance ratings at one session to predict subsequent outcome. Jennissen et al. (2020) used ratings much more widely spaced (every five sessions). Predictors of outcomes assessed over different time periods can differ substantially.
Limitations
We note some key limitations. First, our sample was limited to patients who engaged in a course of CBT for depression. Thus, these results may not be generalizable to other samples of patients with varying diagnoses or treated with different treatment modalities. Second, our analyses were limited to the early sessions of treatment. Our analyses were focused on within-person variability in alliance ratings, and it is possible that the amount of variability would have been greater had we sampled the full course of treatment. It is also unclear if our results would hold for the later sessions of treatment. However, two previous alliance studies using RSA examined time as a potential moderator in their analyses. Both failed to find evidence of such moderation (Jennissen et al., 2020; Rubel et al., 2018). Third, our models did not account for variability that could have been attributable to therapist. We did evaluate the amount of variability attributable to therapist in both within- and between-person BDI and found it to be 0.00%. Nonetheless, we had a small number of therapists for such estimates. Future research on therapist effects in larger samples is warranted. Finally, our results were found in the context of a naturalistic study of CBT for depression. Without a manipulation, we cannot establish causality in the relations we investigated.
Conclusions
We investigated the impact of within-person strength of alliance, as rated by therapists and clients, on within-person symptoms in a sample of patients who participated in a course of CBT for depression. Consistent with prior research, within-person agreement on stronger alliances predicted within-person depressive symptoms. This study adds further support to a growing body of evidence which suggests that alliance agreement captures an important construct in the process of change in psychotherapy.
Clinical or Methodological Significance of this Article.
We investigated the within-person relation of patient and therapist agreement on the alliance in predicting depressive symptoms at the next session. Within-person agreement on a strong alliance predicted lower within-person symptoms. Our findings suggest that when taking therapist and patient perspectives into account, positive views, rather than any specific pattern of disagreement, appears most important in predicting outcome.
Funding:
Iony D. Ezawa was supported in part from an NIMH training grant (T32-MH18921) during completion of this work.
Footnotes
Ethical approval: This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by The Ohio State University’s Institutional Review Board.
Informed consent: Informed consent was obtained from all participants.
Competing interests: The authors declare that they have no conflict of interest.
References
- Adler AD, Strunk DR, & Fazio RH (2015). What changes in cognitive therapy for depression? An examination of cognitive therapy skills and maladaptive beliefs. Behavior Therapy, 46, 96–109. 10.1016/j.beth.2014.09.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson C, & Keltner D (2004). The Emotional Convergence Hypothesis: Implications for Individuals, Relationships, and Cultures. In Tiedens LZ & Leach CW (Eds.), The social life of emotions (pp. 144–163). Cambridge University Press. 10.1017/CBO9780511819568.009 [DOI] [Google Scholar]
- Atzil-Slonim D, Bar-Kalifa E, Rafaeli E, Lutz W, Rubel J, Schiefele A-K, & Peri T (2015). Therapeutic bond judgments: Congruence and incongruence. Journal of Consulting and Clinical Psychology, 83, 773– 784. 10.1037/ccp0000015 [DOI] [PubMed] [Google Scholar]
- Beck AT, Rush AJ, Shaw BF, & Emery G (1979). Cognitive therapy of depression. Guilford. [Google Scholar]
- Beck AT, Steer RA, & Brown GK (1996). Beck depression inventory-II. San Antonio, 78, 490–498. [Google Scholar]
- Bordin ES (1979). The generalizability of the psychoanalytic concept of the working alliance. Psychotherapy: Theory, Research & Practice, 16, 252–260. 10.1037/h0085885 [DOI] [Google Scholar]
- Bruijniks SJ, Lemmens LH, Hollon SD, Peeters FP, Cuijpers P, Arntz A, … & Huibers MJ (2020). The effects of once-versus twice-weekly sessions on psychotherapy outcomes in depressed patients. The British Journal of Psychiatry, 216, 222–230. 10.1192/bjp.2019.265 [DOI] [PubMed] [Google Scholar]
- Chen R, Atzil-Slonim D, Bar-Kalifa E, Hasson-Ohayon I, & Refaeli E (2016). Therapists’ recognition of alliance ruptures as a moderator of change in alliance and symptoms. Psychotherapy Research, 28, 560–570. 10.1080/10503307.2016.1227104 [DOI] [PubMed] [Google Scholar]
- Chen R, Rafaeli E, Bar-Kalifa E, Gilboa-Schechtman E, Lutz W, & Atzil-Slonim D (2018). Moderators of congruent alliance between therapists and clients: A realistic accuracy model. Journal of Counseling Psychology, 65, 703–714. 10.1037/cou0000285 [DOI] [PubMed] [Google Scholar]
- Coyne AE, Constantino MJ, Laws HB, Westra HA, & Antony MM (2018). Patient–therapist convergence in alliance ratings as a predictor of outcome in psychotherapy for generalized anxiety disorder. Psychotherapy Research, 28, 969–984. 10.1080/10503307.2017.1303209 [DOI] [PubMed] [Google Scholar]
- Crits-Christoph P, Gibbons MBC, & Mukherjee D (2013). Psychotherapy process-outcome research. In Lambert MJ (Ed.), Bergin and Garfield’s handbook of psychotherapy and behavior change (pp. 298 – 340). Wiley. [Google Scholar]
- Cronbach LJ, & Furby L (1970). How should we measure “change”— or should we? Psychological Bulletin, 74, 68 – 80. 10.1037/h0029382 [DOI] [Google Scholar]
- Cronbach LJ, & Gleser GC (1953). Assessing similarity between profiles. Psychological Bulletin, 50, 456–473. 10.1037/h0057173 [DOI] [PubMed] [Google Scholar]
- de Graaf LE, Huibers MJ, Riper H, Gerhards SA, & Arntz A (2009). Use and acceptability of unsupported online computerized cognitive behavioral therapy for depression and associations with clinical outcome. Journal of Affective Disorders, 116, 227–231. 10.1016/j.jad.2008.12.009 [DOI] [PubMed] [Google Scholar]
- Edwards JR, & Parry ME (1993). On the use of polynomial regression equations as an alternative to difference scores in organizational research. Academy of Management Journal, 36, 1577–1613. 10.2307/256822 [DOI] [Google Scholar]
- Falkenström F, Granström F, & Holmqvist R (2013). Therapeutic alliance predicts symptomatic improvement session by session. Journal of Counseling Psychology, 60, 317–328. 10.1037/a0032258 [DOI] [PubMed] [Google Scholar]
- Falkenström F, Solomonov N, & Rubel J (2020). Using time-lagged panel data analysis to study mechanisms of change in psychotherapy research: Methodological recommendations. Counselling and Psychotherapy Research, 20, 435–441. 10.1002/capr.12293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, & Williams JBW (2002). Structured Clinical Interview for DSM–IV Axis I disorders. New York State Psychiatric Institute. [Google Scholar]
- Flückiger C, Del Re AC, Wampold BE, & Horvath AO (2018). The alliance in adult psychotherapy: A meta-analytic synthesis. Psychotherapy, 55, 316 –340. 10.1037/pst0000172 [DOI] [PubMed] [Google Scholar]
- Flückiger C, Del Re AC, Wlodasch D, Horvath AO, Solomonov N, & Wampold BE (2020). Assessing the alliance–outcome association adjusted for patient characteristics and treatment processes: A meta-analytic summary of direct comparisons. Journal of Counseling Psychology, 67, 706–711. 10.1037/cou0000424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzaga GC, Campos B, & Bradbury T (2007). Similarity, convergence, and relationship satisfaction in dating and married couples. Journal of Personality and Social Psychology, 93, 34–48. 10.1037/0022-3514.93.1.34 [DOI] [PubMed] [Google Scholar]
- Horvath AO, & Greenberg LS (1989). Development and validation of the Working Alliance Inventory. Journal of Counseling Psychology, 36, 223–233. 10.1037/0022-0167.36.2.223 [DOI] [Google Scholar]
- Huibers MJ, Lorenzo-Luaces L, Cuijpers P, & Kazantzis N (2021). On the road to personalized psychotherapy: A research agenda based on cognitive behavior therapy for depression. Frontiers in Psychiatry, 11, 1551. 10.3389/fpsyt.2020.607508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jennissen S, Nikendei C, Ehrenthal JC, Schauenburg H, & Dinger U (2020). Influence of patient and therapist agreement and disagreement about their alliance on symptom severity over the course of treatment: A response surface analysis. Journal of Counseling Psychology, 67, 326–336. 10.1037/cou0000398 [DOI] [PubMed] [Google Scholar]
- Kivlighan DM (2007). Where is the relationship in research on the alliance? Two methods for analyzing dyadic data. Journal of Counseling Psychology, 54, 423–433. 10.1037/0022-0167.54.4.423 [DOI] [Google Scholar]
- Laws HB, Constantino MJ, Sayer AG, Klein DN, Kocsis JH, Manber R, … & Arnow BA (2017). Convergence in patient–therapist therapeutic alliance ratings and its relation to outcome in chronic depression treatment. Psychotherapy Research, 27, 410–424. 10.1080/10503307.2015.1114687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marmarosh CL, & Kivlighan DM Jr. (2012). Relationships among client and counselor agreement about the working alliance, session evaluations, and change in client symptoms using response surface analysis. Journal of Counseling Psychology, 59, 352–367. 10.1037/a0028907 [DOI] [PubMed] [Google Scholar]
- Nestler S, Humberg S, & Schönbrodt FD (2019). Response surface analysis with multilevel data: Illustration for the case of congruence hypotheses. Psychological Methods, 24, 291–308. 10.1037/met0000199 [DOI] [PubMed] [Google Scholar]
- Pepinsky HB, & Karst T (1964). Convergence: A phenomenon in counseling and in psychotherapy. American Psychologist, 19, 333–338. 10.1037/h0044396 [DOI] [Google Scholar]
- R Core Team (2020). R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing. Retrieved from http://www.R-project.org/ [Google Scholar]
- Rozmarin E, Muran J, Safran J, Gorman B, Nagy J, & Winston A (2008). Subjective and intersubjective analyses of the therapeutic alliance in a brief relational therapy. American Journal of Psychotherapy, 62, 313–328. 10.1176/appi.psychotherapy.2008.62.3.313 [DOI] [PubMed] [Google Scholar]
- Rubel JA, Bar-Kalifa E, Atzil-Slonim D, Schmidt S, & Lutz W (2018). Congruence of therapeutic bond perceptions and its relation to treatment outcome: Within- and between-dyad effects. Journal of Consulting and Clinical Psychology, 86, 341–353. 10.1037/ccp0000280 [DOI] [PubMed] [Google Scholar]
- Safran JD, & Muran JC (2000). Negotiating the therapeutic alliance: A relational treatment guide. New York: Guilford Press. [Google Scholar]
- Schmidt ID, Pfeifer BJ, & Strunk DR (2019). Putting the “cognitive” back in cognitive therapy: Sustained cognitive change as a mediator of in-session insights and depressive symptom improvement. Journal of Consulting and Clinical Psychology, 87, 446–456. 10.1037/ccp0000392 [DOI] [PubMed] [Google Scholar]
- Schönbrodt FD & Humberg S (2020). RSA: An R package for response surface analysis (version 0.10.1). Retrieved from https://cran.r-project.org/package=RSA
- Strunk DR, Hollars SN, Adler AD, Goldstein LA, & Braun JD (2014). Assessing patients’ cognitive therapy skills: Initial evaluation of the competencies of cognitive therapy scale. Cognitive Therapy and Research, 38, 559–569. 10.1007/s10608-014-9617-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tracey TJ, & Kokotovic AM (1989). Factor structure of the Working Alliance Inventory. Psychological Assessment: A Journal of Consulting and Clinical Psychology, 1, 207–210. 10.1037/1040-3590.1.3.207 [DOI] [Google Scholar]
- Wang LP, & Maxwell SE (2015). On disaggregating between-person and within-person effects with longitudinal data using multilevel models. Psychological Methods, 20, 63–83. 10.1037/met0000030 [DOI] [PubMed] [Google Scholar]
- West TV, & Kenny DA (2011). The truth and bias model of judgment. Psychological Review, 118, 357–378. 10.1037/a0022936 [DOI] [PubMed] [Google Scholar]
- Whelen ML, Murphy ST, & Strunk DR (2021). Re-evaluating the alliance-outcome relationship in the early sessions of cognitive behavioral therapy of depression. Clinical Psychological Science, 2167702620959352, 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zilcha-Mano S, Muran JC, Hungr C, Eubanks CF, Safran JD, & Winston A (2016). The relationship between alliance and outcome: Analysis of a two-person perspective on alliance and session outcome. Journal of Consulting and Clinical Psychology, 84, 484–496. 10.1037/ccp0000058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zilcha-Mano S, Snyder J, & Silberschatz G (2017). The effect of congruence in patient and therapist alliance on patient’s symptomatic levels. Psychotherapy Research, 27, 371–380. 10.1080/10503307.2015.1126682 [DOI] [PubMed] [Google Scholar]


