Abstract
Objective:
On October 3-4, 2022, the Memorial Sloan Kettering Cancer Center Supportive Care Service and Department of Psychiatry and Behavioral Sciences hosted the 3rd Annual United States (U.S.) Celebration of World Hospice and Palliative Care Day (WHPCD). The purpose of this article is to reflect on the event within the broader context of the international WHPCD theme: “healing hearts and communities.” We describe lessons learned in anticipation of the fourth annual conference to be held October 3-4, 2023.
Methods:
Description of the third annual event, conference planning team reflection, and attendee evaluation responses.
Results:
The Worldwide Hospice Palliative Care Alliance launched WHPCD in 2005 as an annual unified day of action to celebrate and support hospice and palliative care globally. Since 2020, the conference has attracted an increasing number of attendees from around the world. Two primary aims continue to guide the event: community building and wisdom sharing. 52 interprofessional palliative care experts, advocates, patients, and caregivers provided 13 unique interactive sessions. 458 multidisciplinary registrants from at least 17 countries joined the program. Free registration for colleagues in low- and middle-income countries, students and trainees, and individuals experiencing financial hardship remains a cornerstone of inclusion and equitable access to the event.
Significance of Results:
The U.S. WHPCD Celebration provides a virtual platform that offers opportunities for scientific dissemination and collective reflection on hospice and palliative care delivery amid significant local and global changes in clinical practice, research, policy and advocacy, and population health. We remain committed to ensuring an internationally relevant, culturally diverse, and multidisciplinary agenda that will continue to draw increased participation worldwide during future annual events.
Keywords: palliative care, supportive care, global palliative care, World Hospice and Palliative Care Day, virtual conference
On October 3 and 4, 2022, the Memorial Sloan Kettering (MSK) Cancer Center Supportive Care Service and Department of Psychiatry and Behavioral Sciences co-sponsored the 3rd Annual U.S. Celebration of World Hospice and Palliative Care Day (WHPCD) (MSK, 2022). Building on the promising outcomes of the first two conferences in 2020 and 2021 (Rosa, Pandey et al., 2021; Rosa, Pandey et al., 2022), the 3rd annual conference again used a live virtual format and was condensed over two half-days – one in the morning and the other in the afternoon, to increase global access and participation. The 2022 conference program promoted topics relevant to the Worldwide Hospice Palliative Care Alliance (WHPCA, 2022a) theme—Healing Hearts and Communities (Figure 1). We aim to provide a brief report of the 2022 event to reflect on lessons learned and paths forward as we continue to capture the momentum, maximize the cumulative, ongoing impact of our successive conferences, and prepare for the next annual event that will take place October 3-4, 2023.
Figure 1. Theme and Goal: World Hospice and Palliative Care Day 2022.

Source: Worldwide Hospice Palliative Care Alliance. (2022b). Campaign toolkit: healing hearts and communities. Available at: https://thewhpca.org/world-hospice-and-palliative-care-day/resources-2022/category/campaign-toolkit
*Reprinted with permission from the Worldwide Hospice Palliative Care Alliance.
This year’s conference attracted the highest registrant count to date - a total of 458 individuals from at least 17 different countries, including Armenia, Australia, Bolivia, Canada, Colombia, Germany, Ghana, Kenya, India, Indonesia, Italy, Jamaica, Lebanon, Nigeria, Philippines, United Kingdom, and 15 states across the U.S (Figure 2). The conference course directors and planning committee were comprised of an interdisciplinary team representing nursing (WER, SP), medicine (ASE, AVD), spiritual care (LJA), social work and bioethics (LB), and pharmacy (LAK). Internationally recognized experts in research and academia, policy and advocacy, clinical practice, organizational leadership, education and professional development, and faith communities were invited to celebrate, support, and honor the endeavors of hospice and palliative care workers worldwide. The intentional inclusion of patient and family caregiver participants, as well as a virtual Schwartz Rounds (The Schwartz Center for Compassionate Healthcare, 2023) emphasized the power of humanity, dignity, and compassion, for both care recipients and health professionals.
Figure 2.

Geographic Location of Conference Registrants
2022 World Hospice and Palliative Care Day Theme
The 2022 theme for WHPCD was Healing Hearts and Communities (Figure 1). This theme emerged from the universal experience of grief, the need to heal that is uniting humanity worldwide, and the importance of community-based bereavement support (Figure 3). The more than six million deaths worldwide during the first two years of the COVID-19 pandemic has resulted in tremendous strain on healthcare systems and unprecedented grief and suffering for health workers and caregivers, including the extreme pain of loss for loved ones who could not see dying patients in hospitals and intensive care units due to visitor restrictions (Lynch et al, 2022; McPeake et al, 2023). In addition, numerous armed conflicts, wars, and human-made and natural disasters have occurred around the globe (Rosa, Grant et al., 2022), amplifying unexpected and often traumatic loss for millions of families and caregivers within a broader context of social isolation, displacement and forced migration, and property destruction. See Table 1 for the 2022 WHPCD campaign key messages.
Figure 3. Sub-Themes: World Hospice and Palliative Care Day 2022.
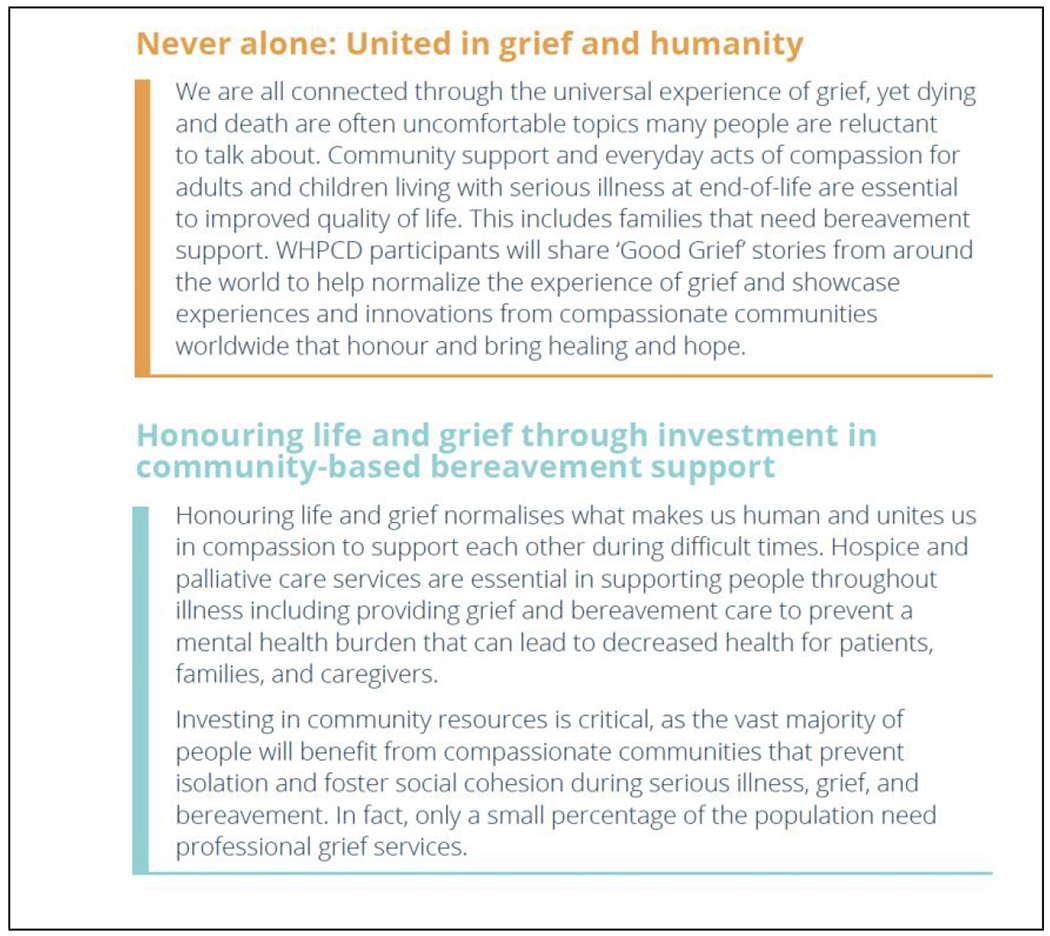
Source: Worldwide Hospice Palliative Care Alliance. (2022b). Campaign toolkit: healing hearts and communities. Available at: https://thewhpca.org/world-hospice-and-palliative-care-day/resources-2022/category/campaign-toolkit
*Reprinted with permission from the Worldwide Hospice Palliative Care Alliance.
Table 1.
Campaign Key Messages: World Hospice and Palliative Care Day 2022.
| • The experience of grief and the need to heal unites humans worldwide. |
| • Global events have resulted in an increased burden of grief among families and healthcare providers. |
| • Fostering a healthy grief experience is essential to resilience, building wellness, and improving health inequities in communities. |
| • Community-based bereavement support is the foundation of a compassionate community. Investment in professional and community services to support grief and healing are critical. |
Source: Worldwide Hospice Palliative Care Alliance. (2022b). Campaign toolkit: healing hearts and communities. Available at: https://thewhpca.org/world-hospice-and-palliative-care-day/resources-2022/category/campaign-toolkit
Reprinted with permission from the Worldwide Hospice Palliative Care Alliance.
Hospice programs – and some palliative care programs - are the only health care delivery services that consistently deliver bereavement follow-up to families and typically offer support and services for one year following the death. Many hospice programs serve not just the families using hospice, but those in the community that are bereaved as well. The WHPCA has called on all governments to develop, fund, and implement national strategies to deliver increased support for bereaved adults and children, particularly for those with complicated grief, such as prolonged grief disorder (Table 2). The pandemic’s disproportionate impact on the world’s poorest and most vulnerable populations has increased the grief burden in countries with the least access to palliative care and other critical social care services.
Table 2.
Key Ask: World Hospice and Palliative Care Day 2022.
| Through this Global Day of Advocacy, we call upon governments, policymakers, and providers to prioritize and implement national strategies for bereaved populations based on a public health approach. | |
|---|---|
| National Strategies for Bereaved Citizens | Compassionate Communities |
| • Primary, secondary, and tertiary education and support ■ Primary education for the public about grief (e.g., national day, media awareness, research sharing) ■ Secondary support for the bereaved (e.g., social support, group support, individual counseling) • Tertiary support for prolonged grief disorder and humanitarian emergencies and disasters |
• Workplace support ■ Flexible bereavement leave policies, education programs for employees • Community engagement and involvement in support for the bereaved • Increased access to hospice and palliative care programs and services |
Source: Worldwide Hospice Palliative Care Alliance. (2022b). Campaign toolkit: healing hearts and communities. Available at: https://thewhpca.org/world-hospice-and-palliative-care-day/resources-2022/category/campaign-toolkit
Reprinted with permission from the Worldwide Hospice Palliative Care Alliance.
A Virtual Coming Together Unifying Collaborators, Countries, and Contexts
As in prior years, the 3rd Annual Event was supported and sponsored by Judith Nelson, MD, JD, Chief of the MSK Supportive Care Service, and, William Breitbart, MD, Chair of the MSK Department of Psychiatry and Behavioral Sciences. The course agenda was carefully curated with consideration of globally relevant topics in the field, areas of growing palliative care research, and ongoing social, ethical, and cultural dilemmas, including the 2022 WHPCA theme. The format remained virtual to increase access to international participants and amplify the voices and priorities of colleagues working in low- and middle-income countries (LMICs),
The event was organized through the MSK Continuing Medical Education program to offer continuing education credits. This year we were expanded continuing education credits to include nursing and psychology credits in addition to the previously available credits for physicians and advanced practice providers. The cost for registration ranged from $50 to $135, depending on discipline. Complimentary registration was made available for all MSK employees and for palliative care professionals residing in LMICs, palliative care students and trainees currently enrolled in a university program or completing a clinical fellowship or residency, and individual experiencing financial strain.
The conference consisted of 13 interactive sessions addressing diverse hospice and palliative care topics delivered by 52 interprofessional experts in palliative care. Topics included person-centered palliative care; cancer pain management and substance use disorder; diversity, equity, inclusion, and cultural humility; advocacy and leadership; resiliency for palliative care workers; research and education; spiritual and existential care; complex communication needs; bereavement and caregiving; and social bioethical considerations (Table 3). Interdisciplinary palliative care scientists and advocates gave five rapid fire talks, which focused on person and family centered hospice and palliative care, bereavement, care of LGBTQ+ patients, dignity, and caregiver-centered interventions. All sessions were recorded, except for the Schwartz Center Rounds session (for confidentiality purposes) and made available to registrants at the end of the conference, in addition to copies of presentation slides prepared by the speakers.
Table 3.
3rd Annual U.S. Celebration of World Hospice and Palliative Care Day Conference Schedule and Session Topics.
| Session Title | Topics Addressed |
|---|---|
| The Platinum Rule: A New Standard in Person-Centered Care | • Annual World Hospice and Palliative Care Day Lectureship: Review of literature on Dignity Conserving Care with pragmatic implications for clinical practice and research pertaining to human-centeredness in palliative care and reflections on The Platinum Rule: treat others as they would like to be treated |
| An Update on Global Serious Health-Related Suffering from The Global Palliative Care and Pain Relief Research Hub | • Research from a hub of international collaborators with findings pertaining to an update of The Lancet Commission on Global Access to Palliative Care and Pain Relief; the need for children’s palliative care worldwide; a regional analysis of palliative care need and access Latin America; a country-level analysis of need and access in Chile |
| The Journey Ahead for Hospice & Palliative Care Teams: Our Collective Suffering and Healing the Wounds | • Breakout session: addressing the welfare of the palliative care workforce, including discussions on trauma-informed care, burnout and moral suffering, the need to develop moral resilience and cultivate meaning-making for health professionals, and strategies to support staff at service, institutional, and system levels |
| Cancer Pain Management and Opioid Use Disorder: How Do We Move Forward? | • Breakout session: focused on emerging science in cancer pain management, opioid misuse, and opioid risk mitigation strategies; identifying next steps in literature to support evidence-based practices and ensure patient and community safety while fulfilling moral obligation to relieve pain |
| Patient-Clinician Conversation | • Interview conducted by palliative care oncologist with a patient working as a palliative care pharmacist undergoing disease-modifying treatment for two cancers |
| Advocacy Corner | • Summary of policy-oriented work led by the Center to Advance Palliative Care in the broader context of local and national advocacy initiatives, U.S. influence on global policy, and need for synergy between clinical, community-based, and decision-making stakeholders |
| Lancet Commission on the Value of Death | • Summary of the Commission report with a focus on implications for clinical stakeholders, hospice and palliative specialists, and community partners to forge a new narrative on the value of death that extends beyond the scope of palliative care; addresses the social determinants of death, dying, and grief; and strives to create a realistic utopia for living and dying |
| Visiting Virtual Schwartz Rounds | • Interdisciplinary discussion on a challenging pediatric oncology case; focused on the emotional and social aspects of patient care and relationship-building, as well as the personal experiences of the physician, nurses, and social workers involved |
| Caregiver-Clinician Conversation | • Exploration of a caregiver’s experience with a spouse’s terminal illness; addressed key roles of mental health, palliative care, and hospice involvement, and takeaways for all interdisciplinary health professionals to consider in the care of patients and their family caregivers |
| Palliative Care for Incarcerated Persons | • Breakout session: program overview of the Humane Prison Hospice Project including viewing of brief documentary, “Prison Terminal: The Last Days of Private Jack Hall”; critical discussion of the need for palliative care improvements and associated barriers among incarcerated people and populations |
| World Perspectives on Medical Aid in Dying | • Breakout session: international views, experiences, and research from interdisciplinary colleagues in Colombia, Kenya, Prague, and the U.S. on ethical, practical, and social considerations related to medical aid in dying |
| Invited Rapid Fire Talks: Person and Family-Centered Hospice and Palliative Care | • “Bereavement Risk-Screening as an Avenue for Bereavement-Conscious Palliative Care”; “Project Respect: LGBTQ+ Experiences with Healthcare Providers for Serious Illness”; “The Patient Dignity Question, Age, and Proximity to Death Among Patients with Cancer”; “Antiracist Approaches to Palliative Care Research”; “Meaning-Focused Interventions for Family Caregivers and Application to Palliative and Hospice Practice” |
| Seeing Ourselves Through Our Patient’s Eyes: Building a Foundation for Diversity, Equity, and Inclusion in Palliative Care and Hospice | • Inaugural Dr. Richard Payne Lecture on Equity, Inclusion, and Belonging in Serious Illness: Innovative discussion on how to forge connection and equity with seriously ill racially marginalized people and communities while considered the historical context of racism and racial inequity, the ongoing social context of racism and racially motivated violence, and the broader reckoning needed in hospice and palliative care |
The opening keynote session was delivered by Harvey Max Chochinov, OC, MD, PhD, FRCPC, FRSC, in which he reviewed his experience in psychiatry and palliative care research. He began by reviewing the role of dignity in the care of seriously ill patients, specifically how clinicians’ empathic response to patients has a profound experience on their lived experience. He explained the importance of dignity conserving care as “the essence of medicine” and listed approaches clinicians can take to affirm personhood. Dr. Chochinov summarized key publications on dignity conserving care, including the development of the Patient Dignity Inventory as a novel method to measure dignity-related distress in palliative care and dignity therapy as a psychotherapeutic intervention for patients near the end-of-life (Chochinov et al., 2011; Chochinov et al., 2012; Schoppee et al., 2022). Conference attendees learned of the development and application of the patient dignity question: “What should I know about you as a person to help me take the best care of you that I can?” Dr. Chochinov proposed a shift to a new standard for person-centered care shifting from the Golden Rule of “do onto others as you would have them do unto you” toward the Platinum Rule “do unto patients as they would want done unto themselves” (Chochinov, 2022). He offers the Platinum Rule as a method to raise the standard of person-centered care, enhance goal concordant care, confront personal biases, and consistently prioritize the patient perspective.
The subsequent session showcased an update on global serious health-related suffering (SHS) from The Global Palliative Care and Pain Relief Research Hub, a group of international and interdisciplinary palliative care specialists and researchers whose aim is to advance the recommendations of the Lancet Commission on Global Access to Palliative Care and Pain Relief (Knaul et al., 2018). First, Felicia Marie Knaul, PhD, shared a broad overview of the imperative to alleviate the burden of SHS from serious illnesses and at the end-of-life. She highlighted the need for universal access to an affordable Essential Package of palliative care, which consists of medications, small inexpensive equipment, and necessary human resources, as a method to alleviate the burden of SHS. She was followed by Professor Julia Downing, RGN, BN, MMedSCi, PhD, who focused on the need to increase access to palliative care for children to address the SHS experienced by the global pediatric population (Coombes et al., 2022; Lohman et al., 2022). She reviewed research methods to prevent underestimation of children’s palliative care need. Data approximations of children’s SHS from 1990 to 2019 and implications for practice were clearly outlined. Recommendations for future research, efforts to advance advocacy, and strategies for palliative specialist service development summarized her talk. She was followed by Renzo Calderon Anyosa, MD, MSc, PhD(c), who presented on SHS in Latin America. He reviewed data from 19 Latin American countries on SHS by year and illness, further characterizing SHS by country income group, and the availability of opioids in distributed opioid morphine-equivalents (DOME). He emphasized the need for policy change and health systems investments toward strengthening existing palliative care delivery and the need to develop PC infrastructure where none exists (De Lima & Pastrana, 2016; Paiva et al., 2022; Pastrana et al., 2022). Pedro Pérez-Cruz, MD, MPH, concluded this session, describing a recent analysis of Chile’s palliative care access gaps in the context of current policies and resources (Pérez-Cruz et al., 2023). Dr. Cruz and his group estimated the current provision of palliative care in Chile compared to the magnitude of SHS among decedents and non-decedents with both cancer and non-cancer conditions, while also estimating the cost of the palliative care Essential Package proposed by the Lancet Commission (Knaul et al., 2018). He concluded with recommendations to increase access to palliative care through clinician training and capacity building, facilitate access to controlled essential palliative medicines (e.g., opioids), and advance needs-based public policy in Chile.
This year, our team offered two breakout sessions throughout the conference. On day one, participants were offered the opportunity to choose from two expert-led sessions, one addressing burn out among the palliative care workforce and another on cancer pain management in the presence of co-morbid opioid use disorder. An expert panel of psychology, social work, spiritual care, and nursing shared insightful presentations on the prevalence of trauma, moral injury, empathic strain, and disconnectedness in palliative care providers and offered approaches to be effective stewards of existing resources with the use of meaning-centered psychotherapy, mindful self-awareness, and additional well-established techniques. In the session on cancer pain management, speakers addressed the impact of restrictive drug policies and opioid stigma on patients with substance use disorder and consensus recommendations on the management approaches for opioid use disorder in the setting of advanced cancer (Jones et al., 2022).
The 2022 program featured deeply personal sessions showcasing the stories of an oncology patient (who is also a palliative care clinical pharmacist) and a bereaved caregiver. These personal narratives provided invaluable insight on suffering, grief of losing a loved one, the benefits of hospice and palliative care for both patients and families, and professional opportunities for enhancing palliative care delivery. The patient session featured Andrew Epstein, MD, FAAHPM, both a medical oncologist and formally trained hospice and palliative medicine specialist, interviewing patient and palliative specialist, Ebtesam “Sammi” Ahmed, PharmD, MS, who shared how her experience as a palliative care pharmacist informed her approach to decision-making while navigating rigorous chemotherapy cycles, surgeries, and discussing her goals and core values with loved ones. She openly shared how this experience helped her learn to advocate for herself so she could receive palliative care and pharmacologic management for distressing symptoms. While initially it was challenging to accept the identity of a person with cancer, Sammi reflected on the significant impact living with cancer has had on her identity as a palliative care clinician. She shared challenges of continuing to work in hospice and palliative care while facing her own mortality as a someone with serious illness. She discussed the importance of creating a space to continue her clinical work while also caring for herself.
Allison Applebaum, PhD, associate attending behavioral scientist in MSK’s Department of Psychiatry and Behavioral Sciences, interviewed her patient of over five years, Claire Mauksch, on day two. Claire shared her experience caring for her husband, Brian, who was diagnosed with colon cancer several weeks before their wedding. His disease progressed over the next few years, including complications of a malignant bowel obstruction, until his eventual death at home with hospice services while Claire was 34 weeks pregnant with their child, Sam. Dr. Applebaum and Claire discussed the challenges of being a caregiver, how they navigated isolation and fear of the future as a young and newly married couple, and the decision to have a child amid the uncertainty of Brian’s illness. Both Claire and Brian received psychosocial care, which profoundly helped their coping, particularly to develop the ability to sit with uncertainty and negative emotions. Claire reflected on missed opportunities in Brian’s care to talk about values, quality of life, prognosis, and end-of-life care planning. She quickly learned the importance of needing to advocate for loved ones while navigating the health care system, which is now a fierce commitment of hers in the care of Sam. She described how her caregiving journey carried over into her grieving process. She emphasized the importance of having enough support and continues to attend a support group for partner loss. She also finds support in social media, especially to find resources as a young widow.
On day two of the conference, an interdisciplinary palliative care team from the Seattle Children’s Hospital provided a thoughtful and emotional discussion of a pediatric patient case for the special Visiting Virtual Schwartz Rounds session. The panel recounted the journey of a young man impressively optimistic and determined throughout the trajectory of the care for his pediatric cancer, from which he ultimately died. One panelist offered how the case challenged her and enriched her experience as a relatively new attending. Other panelists talked about the vulnerability and humility that comes with caring for young adult patients.
The conference also featured a session on hospice and palliative care advocacy led by Brynn Bowman, BA, Chief Executive Officer of the Center to Advance Palliative Care (CAPC), a panel presentation with authors of The Lancet Commission on the Value of Death, and a rapid-fire talk session with five speakers on topics relating to diversity, equity, and inclusion in the delivery of person- and family-centered care. On day one Ms. Bowman reviewed the implications of federal and state-level health policies on palliative care delivery in the U.S. She showcased progress on legislative policy to address disparities in the care of Black patients with serious illness and their families (CAPC, n.d.) and gave an update on the status of the Palliative Care and Hospice Education and Training Act (PCHETA) (PCHETA, 2020). She emphasized the importance of hospice and palliative care workers’ involvement in health care policy as a method of patient advocacy. On day two, commissioners from The Lancet Commission on the Value of Death presented a summary of the report, which proposes greater community involvement alongside health and social care services and increased bereavement support (Sallnow et al., 2022). Libby Sallnow, MBBS, PhD, gave an overview of the report, including a global perspective on how and where people are dying, and the disparities related to over and under-treatment at end-of-life. She shared the commission’s new vision for dying and grieving called “a realistic utopia” and presented five underlying principles to carry this out. Fellow commissioners, Raj Kumar Manu, MD, FRCP, and Sam Guglani, FRCR, contextualized the findings from the report, discussing overt medicalization of death and dying in the modern world. They shared scenarios where modern technology and therapeutics conflict with relationship-building and engaging personhood along with recommendations for health care systems to shift goals and priorities towards alleviation of suffering rather than avoidance of mortality (Sallnow et al., 2022).
Day two also featured a session of five rapid-fire talks from diverse palliative care specialists and researchers focused on the theme of person- and family-centered care. Kailey E. Roberts, PhD, spoke on the development of bereavement-conscious palliative care with the use of bereavement risk screening (Roberts et al., 2021). Natalie McAndrew, PhD, RN, ACNS-BC, CCRN-K, discussed meaning-focused interventions for family caregivers to promote emotional coping and live with uncertainty (Applebaum et al., 2022). Conference attendees learned about Project RESPECT: a study led by Gary L. Stein, JD, MSW, on LGBTQ+ experiences with health care providers and findings that support LGBTQ+ patients and partners to address discriminatory care (Stein et al., 2020). Rachel Hadler, MD, followed with her talk on the results of a study evaluating responses to the Patient Dignity Question (Hadler et al., 2022). Dr. Hadler provided recommendations for future research and was followed by Tamryn F. Gray, PhD, RN, MPH, whose presentation focused on the need for experts in the field to lead and advance palliative care research with an antiracist approach and provided strategies to promote diversity, equity, inclusion, and justice though palliative care research (Sanders et al., 2022).
Kimberly Angelia Curseen, MD, director of outpatient supportive care at Emory Palliative Care Center, delivered the closing keynote in honor of Dr. Richard Payne, former Chief of Palliative Care Services at MSK on the application of principles of diversity, equity, and inclusion in palliative care. Dr. Curseen reviewed the recent societal events that have focused global attention on eradicating systemic racism. She emphasized the importance of understanding medical and personal history to enhance empathy, create honest dialogue, diffuse fears, and build trust. Attendees learned of current anti-racist research on palliative care topics including evidence around disparities in end-of-life care for Black Americans, hospice utilization among patients of color, and ethnic differences in place of death in older hospice enrollees (Marcewicz et al., 2022). Dr. Curseen provided recommendations for health policy, educational tools, and hospice advocacy including Medicaid expansion programs for in-home caregiving. She called on palliative care to serve as a model that can promote social justice principles while actively meeting the needs of our patients and families.
Onward
Participants will have on-demand access to all recorded presentations following the conference to support self-paced learning, ongoing reflection, and practice integration and development. We had a 43% post-conference evaluation response rate (n=132 responses from n=308 e-mail invitations). Disciplines represented included nurses, nurse practitioners, social workers, physicians, physician assistants, chaplains, pharmacists, physical therapists, integrative medicine practitioners, students, and administrative and research personnel working in various clinical and academic settings including medical or acute care units, outpatient clinics, long-term care, inpatient and home hospices, inpatient palliative care units, community-based and home care services, and academic and university settings. Most (81%) identified as a clinician who manages or cares for patients, with 16% managing at least 20 patients weekly. Most respondents rated the overall format of the program and length of the program as good or excellent (97% and 100% respectively). Almost all (98%) responded they would attend this meeting again virtually and 99% rated the overall virtual experience as excellent. All respondents (100%) thought the activity incorporated principles of equity, diversity, and inclusion to the extent possible and 100% reported the conference supported interdisciplinary care practice. 100% of respondents shared they were likely to recommend this course to a colleague.
Participants committed to change in areas of patient and interprofessional communication, patient education, teamwork roles and responsibilities, treatment, quality improvement, diagnosis and screening, safety, and other categories. Some specific examples from comments included: “[I will] make a concentrated effort to learn about patients [from] different culture[s] and their relationship with [the] medical community to provide better care,” “Promote the Platinum Rule to improve patient-provider communication and advance care planning,” “Take more time to listen before interpreting what I think I hear [patients] tell me,” and “Introduce the option and benefit of palliative care [earlier in the disease journey] to help improve their quality of life.” All respondents (100%) reported the content was relevant to practice, with comments ranging from, “The issues discussed were something that I encounter every day in practice,” “I was able to listen to experiences from other colleagues ,” “Discussions of dignity and medical aid in dying [MAiD],” “Lived experiences were displayed,” and, “The concepts of caring for not only a patient but a human with specific needs and characteristics is something I will use in my daily practice with patients.”
Conclusion
Post-conference evaluations highlight the unique contribution of our MSK conference to the hospice and palliative care field with an emphasis on global and multicultural inclusion, interdisciplinary and collaborative practice, social justice, and both art and science (Rosa, Pandey et al., 2021; Rosa, Pandey et al., 2022). The 4th Annual U.S. Celebration of WHPCD will be a two-day virtual event held on October 3-4, 2023. Next year, we will provide access to continuing social work credits in addition to nursing and physician continuing education credits. Given the previous successes of our conferences over these initial three years, we will continue to use a live virtual platform over two half-days, alternating morning and evening times to allow for an international audience. We maintain commitments to ensuring diversity in our planning committee and among invited faculty, as well as equitable program access through continued complimentary registration to those who require it. Through ongoing enhancements in promotion, planning, and dissemination of the program, we expect increased enthusiasm and participation for the 2023 event. In a rapidly changing world and health system, we believe our Annual WHPCD conference will serve as a safe and inclusive space for community building and wisdom sharing for many years to come.
Acknowledgments:
The authors thank all conference speakers who generously donated their time and expertise to create a successful event: Zipporah Ali, MD, MPH, MPC; Allison Applebaum, PhD; Edgar Barens, MFA; Brynn Bowman, MPA; Hailey Bulls, PhD; Rev. Carla Cheatham, MA, MDiv, PhD, TRT; Harvey Max Chochinov, OC, MD, PhD; Maria Cordoba-Nunez, MD, MSc; Kimberly Angelia Curseen, MD; Michele DiTomas, MD, MS; Julia Downing, RGN, BN, MMedSci, PhD; Susan Ehling, MN, ARNP; Tamryn Gray, PhD, RN, MPH; Sam Guglani, BSc, MBBS, MRCP, MA; Rachel Hadler, MD; Susan Hedlund, LCSW, OSW-c; Katie Fitzgerald Jones, PhD, APN, CARN-AP; Felicia Marie Knaul, PhD; Vickie Leff, MSW, LCSW, APHSW-C; Wendy Lichtenthal, PhD; Raj Kumar Mani, MD; Natalie McAndrew, PhD, RN, ACNS-BC; Jessica Merlin, MD, PhD; Ladybird Morgan, RN, MSW; Marvin Mutch; Tania Pastrana, MD, PD; Pedro Perez-Cruz, MD, MPH; Kailey Roberts, PhD; Cynda Hylton Rushton, PhD, RN; Katerina Rusinova, MD, PhD; Zachary Sager, MD; Libby Sallnow, MBBS, PhD; Gary Stein, JD, MSW; Mallory Taylor, MD, MS; Gretchen VonHeeder-Phillips, LICSW; Special thanks to our patient, Ebtesam Ahmed, and family caregiver, Claire Mauksch, who inspired all attendees with their courage, vulnerability, and authenticity. Gratitude to the entire MSK Continuing Medical Education team that designed and managed the event.
Funding:
WER, SP, ASE, LJA, LB, AVD, LAK, WSB, and JEN acknowledge the NIH/NCI Cancer Center Support Grant P30 CA008748.
Footnotes
Conflict of Interest: None.
Contributor Information
William E. Rosa, Department of Psychiatry and Behavioral Sciences, Memorial Sloan Kettering Cancer Center, New York, NY
Shila Pandey, Supportive Care Service, Memorial Sloan Kettering Cancer Center, New York, NY.
Andrew S. Epstein, Department of Medicine, Memorial Sloan Kettering Cancer Center, New York, NY
Stephen R. Connor, Worldwide Hospice Palliative Care Alliance, London, United Kingdom
Laurie J. Andersen, Supportive Care Service, Memorial Sloan Kettering Cancer Center, New York, NY
Liz Blackler, Ethics Committee, Memorial Sloan Kettering Cancer Center, New York, NY.
Anjali V. Desai, Supportive Care Service, Memorial Sloan Kettering, Cancer Center, New York, NY
Lauren Akua Koranteng, Supportive Care Service, Memorial Sloan Kettering, Cancer Center, New York, NY.
William S. Breitbart, Department of Psychiatry and Behavioral Sciences, Memorial Sloan Kettering Cancer Center, New York, NY
Judith E. Nelson, Supportive Care Service, Memorial Sloan Kettering Cancer Center and Weill Cornell Medical College, New York, NY
References
- Applebaum AJ, Sannes T, Mitchell HR, McAndrew NS, Wiener L, Knight JM, Nelson AJ, Gray TF, Fank PM, Lahijani SC, Pozo-Kaderman C, Rueda-Lara M, Miran DM, Landau H, & Amonoo HL (2022). Fit for duty: lessons learned from outpatient and homebound hematopoietic cell transplantation to prepare family caregivers for home-based care. Transplantation and Cellular Therapy, S2666-6367(22), 01841-3. Advance online publication. 10.1016/j.jtct.2022.12.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center to Advance Palliative Care (CAPC). (n.d.). Equitable access to quality palliative care for black patients: A national scan of challenges and opportunities. https://www.capc.org/project-equity-improving-health-equity-for-people-with-serious-illness/equitable-access-to-quality-palliative-care-for-black-patients-a-national-scan-of-challenges-and-opportunities/ [Google Scholar]
- Coombes L, Braybrook D, Roach A, Scott H, Harðardóttir D, Bristowe K, Ellis-Smith C, Bluebond-Langner M, Fraser LK, Downing J, Farsides B, Murtagh FEM, Harding R, & C-POS (2022). Achieving child-centred care for children and young people with life-limiting and life-threatening conditions-a qualitative interview study. European Journal of Pediatrics, 181(10), 3739–3752. 10.1007/s00431-022-04566-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chochinov HM, Kristjanson LJ, Breitbart W, McClement S, Hack TF, Hassard T, & Harlos M (2011). Effect of dignity therapy on distress and end-of-life experience in terminally ill patients: a randomised controlled trial. The Lancet. Oncology, 12(8), 753–762. 10.1016/S1470-2045(11)70153-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chochinov HM, McClement SE, Hack TF, McKeen NA, Rach AM, Gagnon P, Sinclair S, & Taylor-Brown J (2012). The Patient Dignity Inventory: applications in the oncology setting. Journal of Palliative Medicine, 15(9), 998–1005. 10.1089/jpm.2012.0066 [DOI] [PubMed] [Google Scholar]
- Chochinov HM (2022). The Platinum Rule: A new standard for person-centered care. Journal of Palliative Medicine, 25(6), 854–856. 10.1089/jpm.2022.0075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Lima L, & Pastrana T (2016). Evaluation of the effectiveness of workshops on the availability and rational use of opioids in Latin America. Journal of Palliative Medicine, 19(9), 964–971. 10.1089/jpm.2016.0091 [DOI] [PubMed] [Google Scholar]
- Jones KF, Khodyakov D, Arnold R, Bulls H, Dao E, Kapo J, Meier D, Paice J, Liebschutz J, Ritchie C, & Merlin J (2022). Consensus-based guidance on opioid management in individuals with advanced cancer-related pain and opioid misuse or use disorder. JAMA Oncology, 8(8), 1107–1114. 10.1001/jamaoncol.2022.2191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hadler RA, Goldshore M, Rosa WE, & Nelson J (2022). “What do I need to know about you?”: the Patient Dignity Question, age, and proximity to death among patients with cancer. Supportive Care in Cancer, 30(6), 5175–5186. 10.1007/s00520-022-06938-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knaul FM, Farmer PE, Krakauer EL, De Lima L, Bhadelia A, Jiang Kwete X, Arreola-Ornelas H, Gómez-Dantés O, Rodriguez NM, Alleyne G, Connor SR, Hunter DJ, Lohman D, Radbruch L, Del Rocío Sáenz Madrigal M, Atun R, Foley KM, Frenk J, Jamison DT, Rajagopal MR, … Lancet Commission on Palliative Care and Pain Relief Study Group (2018). Alleviating the access abyss in palliative care and pain relief-an imperative of universal health coverage: the Lancet Commission report. Lancet, 391(10128), 1391–1454. doi: 10.1016/S0140-6736(17)32513-8 [DOI] [PubMed] [Google Scholar]
- Lohman D, Cleary J, Connor S, De Lima L, Downing J, Marston J, Morris C, Pardy S, & Pettus K (2022). Advancing global palliative care over two decades: health system integration, access to essential medicines, and pediatrics. Journal of Pain and Symptom Management, 64(1), 58–69. 10.1016/jjpainsymman.2022.03.001 [DOI] [PubMed] [Google Scholar]
- Lynch KA, Green A, Saltz L, Epstein AS, Romano DR, Vera J, & Nelson JE (2022). The Hardest Weeks of My Life: A Qualitative Study of Experiences, Practice Changes, and Emotional Burden of New York City Oncology Physicians During the COVID-19 Surge in 2020. JCO oncology practice, 18(5), e669–e676. 10.1200/OP.21.00585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcewicz L, Kunihiro SK, Curseen KA, Johnson K, & Kavalieratos D (2022). Application of critical race theory in palliative care research: a scoping review. Journal of Pain and Symptom Management, 63(6), e667–e684. 10.1016/jjpainsymman.2022.02.018 [DOI] [PubMed] [Google Scholar]
- McPeake J, Kentish-Barnes N, Banse E, Anderson L, Cuzco C, Azoulay E, Quasim T, Castro P, & Puxty K (2023). Clinician perceptions of the impact of ICU family visiting restrictions during the COVID-19 pandemic: an international investigation. Critical care (London, England), 27(1), 33. 10.1186/s13054-023-04318-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Memorial Sloan Kettering Cancer Center (MSK). (2021). 2nd Annual U.S. Celebration of World Hospice & Palliative Care Day: A Virtual Coming Together. Available at: https://mskcc.cloud-cme.com/course/courseoverview?P=5&EID=28753
- Paiva CE, Bonilla-Sierra P, Tripodoro VA, Rodríguez-Nunez A, De Simone G, Rodriguez LH, de Oliveira Vidal EI, Ríos MR, Crispim DH, Pérez-Cruz P, de Angelis Nascimento MS, Ospina PMR, de Lima L, Pastrana T, Zimmerman C, Hui D, Bruera E, Paiva BSR, & Collaborative Group for the Advancement of Research in Palliative Care in South America (Los PamPAS Group) (2022). How to advance palliative care research in South America? Findings from a delphi study. Journal of Pain and Symptom Management, S0885-3924(22)00998-8. Advance online publication. 10.1016/jjpainsymman.2022.11.020 [DOI] [PubMed] [Google Scholar]
- Palliative Care and Hospice Education and Training Act (PCHETA), H.R. 647, 116th Cong. (2020). https://www.congress.gov/bill/116th-congress/house-bill/647
- Pastrana T, & De Lima L (2022). Palliative care in Latin America: are we making any progress? Assessing development over time using macro indicators. Journal of Pain and Symptom Management, 63(1), 33–41. 10.1016/jjpainsymman.202L07.020 [DOI] [PubMed] [Google Scholar]
- Pérez-Cruz PE, Undurraga E, Arreola-Ornelas H, Corsi O, Jiang Kwete X, Krakauer EL, Rosa WE, & Knaul FN (2023). Bridging gaps to universal palliative care access in Chile: serious health-related suffering and the cost of expanding the package of care services. The Lancet Regional Health Americas, 19, 100425. 10.1016/jlana.2022.100425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts KE, Lichtenthal WG, & Ferrell BR (2021). Being a bereavement-conscious hospice and palliative care clinician. Journal of Hospice and Palliative Nursing, 23(4), 293–295. 10.1097/NJH.0000000000000775 [DOI] [PubMed] [Google Scholar]
- Rosa WE, Grant L, Knaul FM, Marston J, Arreola-Ornelas H, Riga O, Marabyan R, Penkov A, Sallnow L, & Rajagopal MR (2022). The value of alleviating suffering and dignifying death in war and humanitarian crises. Lancet (London, England), 399(10334), 1447–1450. 10.1016/S0140-6736(22)00534-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosa WE, Pandey S, Epstein AS, Connor SR, & Nelson JE (2021). The inaugural United States World Hospice and Palliative Care Day Celebration: A virtual coming together. Palliative & Supportive Care, 19(2), 182–186. doi: 10.1017/S1478951521000237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosa WE, Pandey S, Epstein AS, Connor SR, Andersen LJ, Applebaum AJ, Blackler L, Koranteng LA, Breitbart WS, & Nelson JE (2022). The 2nd annual U.S. celebration of World Hospice and Palliative Care Day: A virtual coming together to support equity in palliative care access. Palliative & Supportive Care, 1–6. Advance online publication. 10.1017/S147895152200013X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanders JJ, Gray TF, Sihlongonyane B, Durieux BN, & Graham L (2022). A framework for anti-racist publication in palliative care: structures, processes, and outcomes. Journal of Pain and Symptom Management, 63(3), e337–e343. 10.1016/jjpainsymman.202L10.001 [DOI] [PubMed] [Google Scholar]
- Sallnow L, Smith R, Ahmedzai SH, Bhadelia A, Chamberlain C, Cong Y, Doble B, Dullie L, Durie R, Finkelstein EA, Guglani S, Hodson M, Husebø BS, Kellehear A, Kitzinger C, Knaul FM, Murray SA, Neuberger J, O’Mahony S, Rajagopal MR, … Lancet Commission on the Value of Death (2022). Report of the Lancet Commission on the Value of Death: bringing death back into life. Lancet, 399(10327), 837–884. 10.1016/S0140-6736(21)02314-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schoppee TM, Scarton L, Bluck S, Yao Y, Keenan G, Samuels V, Fitchett G, Handzo G, Chochinov HM, Emanuel LL, & Wilkie DJ (2022). Dignity therapy intervention fidelity: a cross-sectional descriptive study with older adult outpatients with cancer. BMC Palliative Care, 21(1), 8. 10.1186/s12904-021-00888-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein GL, Berkman C, O’Mahony S, Godfrey D, Javier NM, & Maingi S (2020). Experiences of lesbian, gay, bisexual, and transgender patients and families in hospice and palliative Ccare: perspectives of the palliative care team. Journal of Palliative Medicine, 23(6), 817–824. 10.1089/jpm.2019.0542 [DOI] [PubMed] [Google Scholar]
- The Schwartz Center for Compassionate Healthcare. (2023). Schwartz rounds and membership. Available at: https://www.theschwartzcenter.org/programs/schwartz-rounds/ [Google Scholar]
- Worldwide Hospice Palliative Care Alliance (WHPCA). (2022a). Home. Available at: http://www.thewhpca.org
- Worldwide Hospice Palliative Care Alliance (WHPCA). (2022b). Campaign toolkit: healing hearts and communities. Available at: https://thewhpca.org/world-hospice-and-palliative-care-day/resources-2022/category/campaign-toolkit


