Abstract
Patients with critical limb threatening ischemia often present with complex segmental peripheral arterial chronic total occlusions, which might not be amenable to traditional antegrade revascularization techniques. For these patients, alternative retrograde revascularization techniques could be necessary. In the present report, we describe a novel modified retrograde cannulation technique using a bare back technique that eliminates the need for conventional tibial access sheath placement and, instead, facilitates distal arterial blood sampling, blood pressure monitoring, retrograde administration of contrast agents and vasoactive substances, and a rapid-exchange strategy. This cannulation strategy can serve as part of the armamentarium in the treatment of patients with complex peripheral arterial occlusions.
Keywords: Adductor hiatus, Chronic total occlusion, Endovascular recanalization, Endovascular surgery, Superficial femoral artery
Peripheral arterial disease affects >10 million individuals in the United States and ∼200 million people worldwide.1,2 Among those with peripheral arterial disease, ∼10% develop chronic limb threatening ischemia (CLTI), which is characterized by limb pain at rest, peripheral limb wounds or gangrene, and an increased risk of amputation and death.3 Timely limb revascularization is essential for limb salvage and improving a patient's functional independence.4 Patients with CLTI often present with complex segmental peripheral arterial chronic total occlusions (CTOs), which might not be amenable to traditional antegrade revascularization techniques.5 When confronting such challenging anatomy, a retrograde revascularization strategy could be necessary.5 For this, a distal arterial structure, such as a pedal or distal tibial artery, can be percutaneously cannulated to facilitate the retrograde introduction of an endovascular wire and catheter.5
Traditional percutaneous arterial access sheaths include a dilator, outer catheter shaft, and a communicating side port with a distal Luer lock. The main benefit of traditional sheath placement is maintenance of adequate arterial access during repeated wire and catheter exchanges, and also facilitating arterial blood sampling and flushing. Conversely, placement of an arterial access sheath after initial cannulation with a micropuncture sheath adds a step to the procedure and can risk trauma, dissection, or thrombosis to the cannulation of smaller caliber distal arteries.6 Injury of a distal arterial structure in a patient with CLTI can be consequential, reducing options for distal revascularization and precipitating the risk of major amputation.6 In the present report, we describe an alternative, less-invasive, technique that used no traditional access sheath placement and a “bare-back” microcatheter method during distal retrograde arterial cannulations in patients with CLTI. Uniquely, this technique reduces the distal retrograde arterial cannulation diameter by ≥50% and, therefore, can reduce the risk of traumatic insertions that can potentially occur with traditional distal pedal and tibial arterial access sheaths.
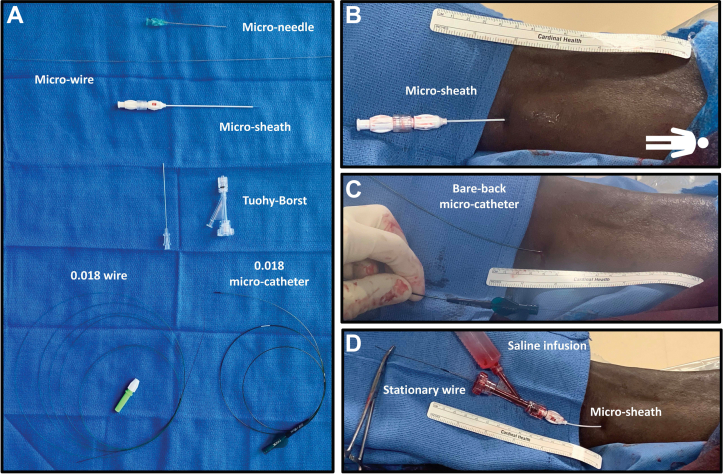
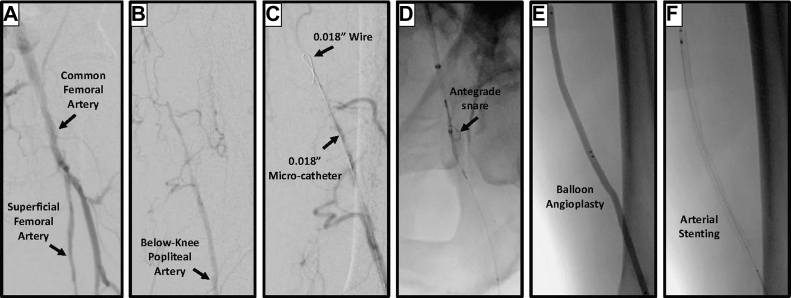
With ultrasound guidance, the anterior or posterior tibial arteries are cannulated using an echogenic micropuncture tapered needle (Micropuncture Access Set; Cook Medical Inc; Fig 1, A). Next, a 0.018-in. nitinol access microwire is advanced in a retrograde fashion into the lumen of the peripheral access artery. The needle is removed, and a 4F hydrophilic micropuncture sheath (outer diameter, 0.85 mm) is placed over the microwire (Fig 1, B). The patient provided written informed consent for the publication of their de-identified representative photographs. After angiographic confirmation of successful cannulation of the distal arterial structure, a 0.018-in. crossing wire (eg, a Command [Abbott] or Asahi [Asahi Intecc]) can be carefully advanced in a retrograde fashion from distally to proximally under fluoroscopic guidance. The micropuncture sheath is then exchanged for a 0.018-in. microcatheter (eg, CXI [Cook Medical Inc], Quick Cross [Philips Healthcare], or Navicross [Terumo Interventional Systems] catheter; Fig 1, C). The microcatheter and 0.018-in. crossing wire can be used in combination to cross CTOs in the proximal arterial system. Once crossing is completed, the wire is externalized from a proximal antegrade arterial access to facilitate endovascular treatment from the antegrade access. The distal access microcatheter is then removed, and the distal arterial access is simply maintained by reinsertion of the original, low-profile 4F micropuncture sheath used during the initial cannulation (Fig 1, D). A Tuohy-Borst Y-connector valve can be strategically placed on the microsheath to maintain wire access. A surgical snap instrument can also be placed on the distal wire to further prevent wire slippage or losing access. The side port of the connector valve readily facilitates access to the arterial blood lumen for distal flushing of intraluminal debris during recanalization procedures such as atherectomy (Fig 1, D). The lumen can also be used for arterial blood sampling for activated clotting time assessments or real-time arterial blood pressure assessments during the revascularization procedure. In a patient with a long-segment CTO, the crossing retrograde wire can be snared to facilitate angioplasty and stenting from an antegrade approach (Fig 2).
Fig 1.
A, Materials needed for modified bare-back micro-retrograde pedal arterial access. From top to bottom: an access kit, including a microsheath, the Tuohy-Borst adapter, and a 0.018-in. wire and catheter. B, Successful vessel cannulation with the 4F microsheath. C, Successful vessel cannulation with a 0.018-in. microcatheter placed over the 0.018-in. crossing wire. D, Successful maintenance of arterial access with 0.018-in. wire and 4F microsheath with attached Tuohy-Borst with flush syringe secured in place.
Fig 2.
A and B, An example patient with complex, long segment chronic total occlusion (CTO) of the superficial femoral artery. C, A 0.018-in. wire and microcatheter were used to cross the CTO. D, The wire was snared from an antegrade access. E and F, The CTO was then treated from the antegrade access with balloon angioplasty and stenting.
Advantages of modified micropuncture retrograde tibial arterial access compared with traditional approaches
The described retrograde access has several advantages. First, the technique allows for safer and less traumatic cannulation and maintenance of distal arterial access in patients with CLTI. Avoiding trauma to the distal arterial outflow is essential for successful revascularization and, ultimately, improved arterial perfusion of the foot and digits. Although placement of a traditional arterial access sheath into the distal arteries is standard, the outer diameter of conventional sheaths ranges from 1.7 mm (for a 4F inner diameter sheath) to 2.7 mm (for a 6F inner diameter sheath). In a small and potentially diseased distal arterial structure, access sheath-associated trauma during insertion can lead to irreparable damage to the outflow artery. This can further complicate ischemia in the compromised limb, decrease the probability of limb salvage, and increase the risk of limb amputation. Our technique allows for distal arterial access with a diameter of no greater than 0.85 mm (for a 4F micropuncture sheath and a 0.018-in. microcatheter), decreasing the risk of distal arterial trauma during cannulation.
Second, traditional arterial access sheaths only allow for blood sampling and monitoring when the side port is unlocked. If the sheath is occlusive in the lumen of the vessel, this will lead to suboptimal flow assessments. Also, infusions through the side port will not readily reach distal arterial outflow. In contrast, our technique uses a Tuohy-Borst Y-connector on a low-profile 4F micropuncture sheath, which allows for nonobstructed arterial blood sampling. Similarly, this type of access provides the option for infusing medications (eg, anticoagulants and vasodilators) to distal arterial structures. Administration of medications can further decrease the risk of intraprocedural arterial thrombosis or vasospasm.
Third, our technique provides a mechanism for retrograde intermittent flushing of the distal arterial outflow through the low-profile micropuncture sheath throughout the procedure. This is especially useful when performing complex recanalization procedures because small microemboli can accumulate in the distal outflow artery. Regular suction and flushing with a heparinized saline solution through the micropuncture sheath or its Tuohy-Borst Y-connector can help mitigate the risk of distal microembolization and preserve arterial outflow patency. The Y-connector can also facilitate administration of contrast administration through the micropuncture sheath to assess lumen patency and flow dynamics. These assessments can help determine when adequate successful revascularization has been achieved. Finally, the Y-connector can facilitate real-time intra-arterial pressure monitoring. This can be especially useful when assessing the hemodynamic effects of an intervention. The ratio between the mean arterial blood pressure recorded in the distal outflow sheath before and after revascularization or compared with the blood pressure recorded more proximally can serve as an index for improvement.
Finally, our described retrograde cannulation technique can also facilitate a rapid-exchange mechanism. Once the wire is externalized from a proximal access site to facilitate intervention from an antegrade fashion, the distal wire tip can be maintained through the hemostatic Tuohy-Borst Y-connector valve and clamped (Fig 1, D). This allows interventionalists to remove interventional tools (eg, balloon and stent catheters) from the antegrade route in a rapid-exchange fashion without conventional “pinch-pull” techniques. This feature simplifies the procedure, eliminates the need to constantly hold the wire in position, and decreases the operative time.
Potential barriers to adoption and implementation
Interventionalists who might not be familiar with this approach could be initially hesitant to implement this into their practice. However, in our experience, this modification of retrograde arterial access is straightforward and does not require any new materials or supplies that are not typically available in endovascular interventional suites. Interventionalists could be initially concerned about the level of hemostasis around the distal cannulation site. However, we have not encountered issues with bleeding around the micropuncture or microcatheter. Even during the bare-back advancement of the catheter and wire, we have not encountered cannulation site bleeding or the formation of hematomas. We believe the system’s low profile (0.85 mm) decreases the arterial puncture and the risk of access site bleeding. This cannulation strategy can serve as a part of the armamentarium in the treatment of patients with complex peripheral arterial occlusions.
Footnotes
Author conflict of interest: M.A.Z. reports equity ownership in Caeli Vascular, Inc, and Inflexion Vascular, LLC, which had no role in this research; consults for Medtronic, Inc, and Cardiovascular Systems, Inc; and received research support from the National Heart, Lung, and Blood Institute, National Institutes of Health (grants R01HL153436, R01HL153262, R01HL150891, and R42HL150963). F.G. and M.L.J. have no conflicts of interest.
The editors and reviewers of this article have no relevant financial relationships to disclose per the Journal policy that requires reviewers to decline review of any manuscript for which they may have a conflict of interest.
References
- 1.Fowkes F., Aboyans V., Fowkes F., McDermott M., Sampson U., Criqui M. Peripheral artery disease: epidemiology and global perspectives. Nat Rev Cardiol. 2017;14:156–170. doi: 10.1038/nrcardio.2016.179. [DOI] [PubMed] [Google Scholar]
- 2.Kullo I., Rooke T. Peripheral artery disease. N Engl J Med. 2016;374:861–871. doi: 10.1056/NEJMcp1507631. [DOI] [PubMed] [Google Scholar]
- 3.Abu Dabrh A., Steffen M., Undavalli C., et al. The natural history of untreated severe or critical limb ischemia. J Vasc Surg. 2015;62:1642–1651.e3. doi: 10.1016/j.jvs.2015.07.065. [DOI] [PubMed] [Google Scholar]
- 4.Conte M., Bradbury A., Kolh P., et al. GVG Writing Group Global vascular guidelines on the management of chronic limb-threatening ischemia. J Vasc Surg. 2019;70:662. doi: 10.1016/j.jvs.2019.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lai S., Fenlon J., Roush B., et al. Analysis of the retrograde tibial artery approach in lower extremity revascularization in an office endovascular center. J Vasc Surg. 2019;70:157–165. doi: 10.1016/j.jvs.2018.10.114. [DOI] [PubMed] [Google Scholar]
- 6.Guilbert C., Elkouri S., Bracco D., et al. Arterial trauma during central venous catheter insertion: case series, review and proposed algorithm. J Vasc Surg. 2008;48:918–925. doi: 10.1016/j.jvs.2008.04.046. discussion: 925. [DOI] [PubMed] [Google Scholar]