Abstract
Objective
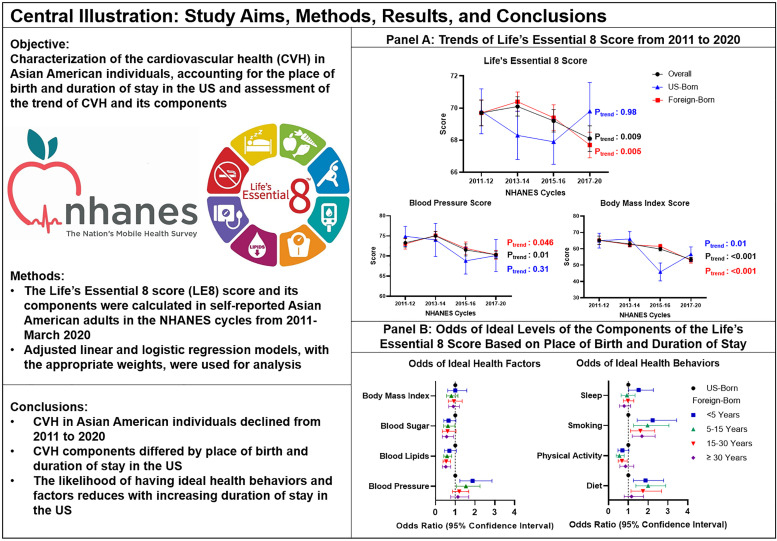
Oversampling of Asian American individuals in the National Health and Nutrition Examination Survey (NHANES) provides a unique opportunity to assess the population-level cardiovascular health (CVH) in the fastest-growing racial group in the US.
Methods
The Life's Essential 8 (LE8) score and its components were calculated in self-reported Asian American individuals ≥20 years of age and free of cardiovascular disease in the NHANES cycles from 2011-March 2020. Multivariable adjusted linear and logistic regression models were used for analysis.
Results
Among 2,059 Asian American individuals, the weighted mean LE8 score was 69.1 (0.4) with US-born [69.0 (0.8)] and foreign-born individuals [69.1 (0.4)] having similar CVH. From 2011 to March 2020, CVH in the overall population [69.7 (0.8) to 68.1 (0.8); Ptrend: 0.009] and foreign-born individuals [69.7 (0.8) to 67.7 (0.8); Ptrend: 0.005] declined. Decreasing trends were noted in the body mass index score irrespective of stratification and in the blood pressure scores in the overall population and foreign-born Asian American individuals. Compared with US-born individuals, the odds of ideal levels of smoking [ORadj:<5 years: 2.23 (95%CI: 1.45–3.44); 5–15 years: 1.97 (95%CI: 1.27–3.05); 15–30 years: 1.61 (95%CI: 1.11–2.34); ≥30 years: 1.69(95%CI:1.20–2.36)] and diet [ORadj: <5 years: 1.87 (95%CI: 1.26–2.79); 5–15 years: 2.00 (95%CI: 1.38–2.89); 15–30 years: 1.74 (95%CI: 1.14–2.68)] were higher in foreign-born individuals. Foreign-born individuals had lower odds of ideal physical activity levels [ORadj: 5–15 years: 0.55 (95%CI: 0.39–0.79); 15–30 years: 0.68 (95%CI: 0.49–0.95)] and ideal cholesterol levels [ORadj: 5–15 years: 0.59 (95%CI: 0.42–0.82); 15–30 years: 0.54 (95%CI :0.38–0.76); ≥30 years: 0.52 (95%CI: 0.38–0.76)].
Conclusion
The CVH in Asian American individuals declined from 2011 to March 2020. The odds of ideal CVH decreased with increasing duration of stay in the US, with foreign-born individuals residing in the US for ≥30 years having ∼28% lower odds of ideal CVH compared with US-born individuals.
Keywords: Asian American, Acculturation, Cardiovascular health, Life's essential 8, Sleep
Central Figure
Study Aims, Methods, Results, and Conclusions
1. Introduction
The Asian American population, currently accounting for about 6% of the US population, has been growing exponentially over the past decade and is projected to increase to about 37 million individuals in 2060 [1,2]. Cardiovascular (CV) disease is the leading cause of mortality in Asian American individuals accounting for about a third of all deaths [3]. However, there is limited contemporary data characterizing CV health (CVH) in Asian American individuals. Additionally, the risk of CV disease and associated cardiometabolic diseases vary between US and foreign-born Asian American individuals [4,5]. Even among foreign-born Asian American individuals, health behaviors and CV risk factors differ with the duration of stay in the US [4,6]. Therefore, an examination of the determinants of CVH in Asian American individuals accounting for the place of birth and duration of stay in the US is needed.
In 2022, the American Heart Association (AHA) introduced the Life's Essential 8 (LE8) score, an updated metric to measure the CVH of an individual [7,8]. The LE8 score improves on the previous tool for CVH measurement, the Life's Simple 7 (LS7) score, by measuring CVH on a scale of 0 to 100 and recognizing sleep as a determinant of CVH [7,8]. About a third of Asian American individuals report poor sleep quality and duration which increases the risk of CV disease directly and indirectly by leading to the dysregulation of other CV risk factors such as hypertension, diabetes, and obesity [3,[9], [10], [11], [12]]. It is unknown how the introduction of sleep as a determinant of CVH will affect the quantification of CVH in Asian American individuals.
This study aimed to characterize the CVH in Asian American individuals, accounting for the place of birth and duration of stay in the US, using the LE8 score and assess the trend of the LE8 score and its components using the National Health and Nutrition Examination Survey (NHANES) data from 2011 to 2020.
2. Methods
The NHANES is a nationwide survey conducted every two years by the National Center for Health Statistics (NCHS) and Center for Disease Control to examine the health and nutritional status of the non-institutionalized US population. The NHANES utilizes a complex multistage probability sampling design to select a sample population representative of the national non-institutionalized civilian US population [8,[13], [14], [15], [16], [17]]. The survey includes a home interview followed by a clinical examination. Written informed consent is taken before the home interview and clinical examination. Information on demographics, diet, sleep, physical activity, smoking, history of medical conditions, and current medication use is collected during the home interview [13]. Participants were invited to a mobile examination center for the clinical examination. During the examination visit, anthropometry, detailed physical examination, blood pressure measurements, and blood draws for laboratory tests were performed for each participant [13].
Since 2011, the NHANES began oversampling Asian American individuals [5,18]. To facilitate this oversampling, the NHANES recruited staff who were fluent in an Asian language and English, provided cultural competency training to its staff, and translated survey materials into select Asian languages [5,18]. However, the questionnaires were not translated due to their complexity [5,18]. Local interpreters were recruited to assist the participants in translating the questionnaires and interpreting their responses [5,18].
This study combined 4 NHANES cycles from 2011 to 2012 to 2017- March 2020. The data collection for the 2019–2020 cycle was discontinued in March 2020 due to the COVID-19 pandemic. Therefore, to generate reliable population-level estimates, the 2019-March 2020 was combined with the 2017–2018 cycle [19]. Individuals aged 20 years and above and self-identifying as non-Hispanic Asian were included in this study. The following exclusion criteria were applied: 1) individuals with missing measurements for the components of the LE8 score; 2) pregnant or breastfeeding females; 3) self-reported prevalent CV disease ("heart attack", stroke, heart failure, angina, and coronary heart disease) [20]. The cohort was stratified by place of birth into US-born Asian American individuals and foreign-born Asian American individuals. Foreign-born Asian American individuals were further sub-stratified by the duration of their stay in the US into <5 years, 5 to 15 years, 15 to 30 years, and ≥30 years.
The LE8 score is a composite of 4 health behaviors and 4 health factors [7]. Health behaviors included smoking, physical activity, diet, and sleep [7]. Health factors included body mass index (BMI), non-HDL cholesterol, blood pressure, and glycosylated hemoglobin (HbA1C) [7]. These components are scored on a scale of 0 to 100. The mean value of the 8 components is calculated to compute the LE8 score. Each component and its scoring scheme have been described in Supplementary Table 1. [7,20]
Blood pressure was measured during the clinical examination visit after resting for 5 min. Blood pressure was measured in the seated position and 3 measurements were taken for each participant. The average of the 3 measurements was used as the systolic and diastolic blood pressures. Data on antihypertensive medication use was retrieved from the home interview questionnaire.
BMI was calculated using the weight (kilograms) and height (meters) measured at the clinical examination visit. The levels of the BMI score were defined using the WHO-recommended guidelines for Asian individuals [7].
Physical activity levels were calculated based on the intensity and duration of recreational physical activity per week reported during the home interview.
Self-reported cigarette smoking status, time since quitting smoking, and use of inhalational nicotine delivery systems such as cigars, pipes, hookahs, and e-cigarettes in the past 5 days were obtained tobacco use questionnaire. The household smokers questionnaire was used to assess exposure to secondhand cigarette smoke at home.
The Dietary Approach to Stop Hypertension (DASH) scores were calculated using data from two 24-hour dietary recalls. The DASH score was calculated using 9 calorie indexed components (saturated fat, total fat, protein, cholesterol, fiber, magnesium, calcium, potassium, and sodium) [21]. In each component, meeting the ideal and intermediate DASH targets were given 1 point and 0.5 points, respectively [21]. The DASH targets have been described in Supplementary Table 2.
Blood samples from the clinical examination visit were used to measure HbA1C levels by high-performance liquid chromatography and cholesterol by enzymatic assay. Non-HDL cholesterol, required for calculating the blood lipids score, was obtained by subtracting the HDL levels from the total cholesterol levels. The current use of lipid-lowering medication, oral hypoglycemic drugs, and insulin was ascertained from the questionnaire completed during the home interview.
Self-reported duration of sleep per day was assessed using the sleep disorders questionnaire.
This study used the following covariates: 1) self-reported sex (male or female); 2) level of education (college degree or higher, some college education, and ≤12 years of education); 3) number of healthcare visits in the past year (4 or more, 1 to 3, or none); 4) insurance status (yes or no); and 5) poverty income ratio [<1.30 (low socioeconomic status), 1.30–3.49 (moderate socioeconomic status), and ≥3.50 (high socioeconomic status)] [8,15].
The LE8 score was used to categorize CVH into poor (<50), intermediate (50–79), and ideal (≥80) [8,22].
To account for combining NHANES cycles from 2011 to 2012 to 2017-March 2020, full sample examination weights in each cycle were adjusted as per the recommendations of the NCHS [13]. SURVEY procedures, incorporating the constructed weights, were used to account for the multistage sampling techniques as recommended by the NHANES statistical analysis guidelines. Categorical variables were summarized as frequency (percentage) using the SURVEYFREQ procedure and continuous variables were summarized as median (interquartile range) using the SURVEYMEANS procedure. The LE8 score and its components were calculated in the overall population and stratified by the birthplace and duration of stay in the US. The direct method of age-standardization was used to generate age-adjusted estimates for the LE8 score and its components [17]. Multivariable adjusted logistic regression models were used to estimate the odds of ideal LE8 and component scores using US-born Asian American individuals as the reference group. Temporal trends of the LE8 score and its components were analyzed using multivariable adjusted linear regression models. Weights provided in each cycle were used for this analysis. All regression models were adjusted for insurance status, age, education level, income, and the number of healthcare visits per year [5,8,14,15]. Statistical analysis was performed on SAS 9.4 (Cary, NC). A two-sided p-value of <0.05 was considered significant.
3. Results
There were a total of 45,462 participants included in the NHANES cycles between 2011 and 2012 to 2017-March 2020. Individuals identifying as races other than non-Hispanic Asian (n = 40,426), below the age of 20 years (n = 1,765), pregnant (n = 38) or breastfeeding (n = 23) females, individuals with a history of CV disease (n = 173), participants who did not undergo the clinical examination (n = 182), those with missing data on place of birth (n = 1), and those with missing components of the LE8 score (n = 795) were excluded (Fig. 1). The final study sample included 2,059 non-Hispanic Asian American individuals, representing 8.9 million non-Hispanic Asian American individuals of the US population. The median age of the population was 40.8 (29.9, 54.2) years and 51.5% were females.
Fig. 1.
Study population flowchart.
In the overall population, the mean LE8 score was 69.1 (0.4). The lowest and highest scoring components were diet [46.1 (0.9)] and sleep [86.5 (0.6)], respectively (Table 1).
Table 1.
Baseline Characteristics and the Life's Essential 8 Scores of Asian American Individuals in the Overall Population and Stratified by Place of Birth in National Health and Nutrition Examination Survey 2011- March 2020.
| Parameter |
Overall [n = 2059 (8,923,302)] |
Foreign Born [n = 1771 (7,596,617)] |
US Born [n = 288 (1,326,685)] |
|||
|---|---|---|---|---|---|---|
| Age* | 40.8 (29.9, 54.2) | 43.0 (32.3, 55.0) | 27.9 (23.2, 38.2) | |||
| Sex | ||||||
| Male | 48.5 (46.5, 50.5) | 48.3 (46.2, 50.4) | 49.8 (43.4, 56.1) | |||
| Female | 51.5 (49.5, 53.5) | 51.7 (49.6, 53.8) | 50.2 (43.9, 56.6) | |||
| Education level | ||||||
| High School or Less | 22.3 (19.1, 25.5) | 23.3 (19.9, 26.8) | 16.5 (11.9, 21.1) | |||
| Some College | 19.9 (17.2, 22.5) | 18.0 (15.3, 20.7) | 30.7 (24.6, 36.9) | |||
| College Graduate | 57.8 (53.4, 62.2) | 58.7 (53.7, 63.6) | 52.7 (45.7, 59.7) | |||
| Insurance Status | ||||||
| Insured | 87.4 (85.2, 89.6) | 87.4 (85.1, 89.7) | 87.3 (81.8, 92.7) | |||
| Uninsured | 12.6 (10.4, 14.8) | 12.6 (10.3, 14.9) | 12.7 (7.3, 18.2) | |||
| Family Poverty Income Ratio | ||||||
| >=3.50 | 47.3 (42.7, 51.9) | 47.2 (42.5, 52.0) | 47.7 (39.3, 56.2) | |||
| 1.30–3.49 | 28.0 (24.0, 31.9) | 27.7 (23.9, 31.6) | 29.3 (19.7, 38.9) | |||
| <1.30 | 24.7 (21.5, 28.0) | 25.0 (21.5, 28.6) | 22.9 (17.7, 28.2) | |||
| Number of Healthcare Visits | ||||||
| None | 20.2 (17.8, 22.6) | 19.8 (17.6, 22.0) | 22.5 (15.9, 29.2) | |||
| 1 to 3 | 57.5 (54.9, 60.2) | 58.4 (55.9, 60.8) | 52.9 (45.1, 60.7) | |||
| >=4 | 22.3 (20.5, 24.0) | 21.9 (19.8, 23.9) | 24.6 (19.1, 30.0) | |||
| Median (IQR) | Mean (SE) | Median (IQR) | Mean (SE) | Median (IQR) | Mean (SE) | |
| Essential 8 Score | 69.4 (59.2, 79.3) | 69.1 (0.4) | 69.1 (58.8, 78.5) | 69.1 (0.4) | 71.7 (61.4, 81.2) | 69.0 (0.8) |
| Physical Activity Score | 67.0 (0.0, 93.6) | 55.2 (1.6) | 59.8 (0.0, 93.3) | 54.0 (1.7) | 89.2 (0.0, 94.9) | 63.4 (2.9) |
| Blood Pressure Score | 79.9 (38.7, 90.0) | 72.2 (0.6) | 77.9 (37.1, 89.8) | 72.3 (0.6) | 82.2 (47.3, 91.1) | 72.8 (1.9) |
| Blood Lipids Score | 55.4 (33.8, 86.4) | 66.7 (0.9) | 53.8 (32.7, 85.2) | 65.8 (0.8) | 81.2 (41.5, 90.6) | 72.1 (2.1) |
| Blood Sugar Score | 67.0 (49.2, 83.5) | 80.2 (0.6) | 65.1 (47.7, 82.5) | 79.4 (0.8) | 74.8 (62.2, 87.4) | 86.0 (1.5) |
| Body Mass Index Score | 38.5 (20.4, 77.5) | 59.3 (0.9) | 38.1 (20.6, 77.0) | 59.3 (1.1) | 41.0 (18.8, 80.3) | 58.0 (2.3) |
| Smoking Score | 86.9 (80.3, 93.4) | 86.4 (0.9) | 87.1 (80.6, 93.5) | 87.2 (1.0) | 85.8 (67.8, 92.9) | 81.6 (1.7) |
| Sleep Score | 92.0 (63.2, 96.0) | 86.5 (0.6) | 91.9 (62.7, 96.0) | 86.5 (0.6) | 92.3 (65.9, 96.1) | 86.7 (1.4) |
| Diet Score | 34.6 (1.4, 62.3) | 46.1 (0.9) | 38.6 (4.8, 63.7) | 48.1 (1.1) | 11.9 (0.0, 49.6) | 31.6 (2.1) |
Median (interquartile range), mean (standard deviation), and frequency (percentage) have been used to describe data.
Median (interquartile range) has been used.
The CVH in the Asian American population decreased across the study period [69.7 (0.8) in 2011–2012 and 68.1 (0.8) in 2017-March 2020; Ptrend: 0.009]. A decline in the blood pressure [73.3 (1.1) in 2011–2012 to 70.3 (0.9); Ptrend: 0.01] and BMI [65.2 (2.5) in 2011–2012 to 53.5 (1.3); Ptrend: <0.001] components of the LE8 score was noted (Table 2) (Fig. 2).
Table 2.
Trends of the life's essential 8 score and its components in the overall population and stratified by place of birth in national health and nutrition examination survey 2011- March 2020.
|
2011–2012 [n = 506 (7,986,329)] |
2013–2014 [n = 444 (8,763,301)] |
2015–2016 [n = 445 (9,497,046)] |
2017–2020 [n = 664 (9,250,321)] |
Ptrend | |
|---|---|---|---|---|---|
| Overall Asian American Individuals | |||||
| Essential 8 Score | 69.7 (0.8) | 70.1 (0.6) | 69.2 (0.7) | 68.1 (0.8) | 0.009 |
| Physical Activity Score | 54.1 (2.3) | 58.0 (3.0) | 50.1 (2.2) | 57.5 (3.1) | 0.90 |
| Blood Pressure Score | 73.3 (1.1) | 75.0 (1.1) | 71.5 (1.5) | 70.3 (0.9) | 0.01 |
| Blood Lipids Score | 67.7 (1.6) | 67.5 (1.8) | 66.8 (1.7) | 65.4 (1.7) | 0.23 |
| Blood Sugar Score | 81.9 (1.3) | 79.7 (1.1) | 79.7 (1.1) | 78.6 (1.0) | 0.13 |
| Body Mass Index Score | 65.2 (2.5) | 63.0 (1.5) | 59.8 (1.1) | 53.5 (1.3) | <0.001 |
| Smoking Score | 84.7 (1.3) | 84.6 (1.6) | 86.7 (1.9) | 88.2 (1.4) | 0.15 |
| Sleep Score | 84.6 (1.3) | 85.5 (0.9) | 88.0 (1.4) | 87.0 (1.0) | 0.19 |
| Diet Score | 45.8 (1.7) | 47.2 (1.2) | 48.4 (1.6) | 44.1 (1.8) | 0.27 |
| US-born Asian American Individuals | |||||
| Essential 8 Score | 69.8 (1.4) | 68.3 (1.5) | 67.9 (1.4) | 69.8 (1.8) | 0.98 |
| Physical Activity Score | 57.6 (4.6) | 58.7 (9.2) | 68.3 (5.3) | 65.7 (4.9) | 0.15 |
| Blood Pressure Score | 74.9 (2.5) | 74.0 (4.1) | 68.8 (3.3) | 70.1 (4.0) | 0.31 |
| Blood Lipids Score | 74.1 (2.5) | 75.0 (4.7) | 69.0 (5.1) | 70.9 (4.8) | 0.23 |
| Blood Sugar Score | 86.5 (1.6) | 85.3 (2.5) | 84.3 (3.8) | 85.1 (1.9) | 0.80 |
| Body Mass Index Score | 65.0 (4.6) | 66.0 (4.6) | 45.8 (5.5) | 56.7 (4.5) | 0.01 |
| Smoking Score | 77.3 (2.3) | 80.2 (4.7) | 80.3 (5.3) | 85.6 (1.9) | 0.06 |
| Sleep Score | 85.0 (2.1) | 82.6 (2.6) | 84.0 (3.4) | 90.4 (1.6) | 0.06 |
| Diet Score | 37.7 (3.7) | 24.5 (3.4) | 42.7 (6.3) | 34.2 (4.3) | 0.98 |
| Foreign-Born Asian American Individuals | |||||
| Essential 8 Score | 69.7 (0.8) | 70.4 (0.6) | 69.4 (0.8) | 67.7 (0.8) | 0.005 |
| Physical Activity Score | 53.4 (2.6) | 57.9 (3.3) | 47.9 (2.4) | 56.0 (3.2) | 0.75 |
| Blood Pressure Score | 73.0 (1.3) | 75.1 (1.0) | 71.9 (1.6) | 70.3 (1.1) | 0.046 |
| Blood Lipids Score | 66.3 (1.8) | 66.2 (1.7) | 66.6 (1.8) | 64.5 (1.5) | 0.44 |
| Blood Sugar Score | 80.9 (1.4) | 78.7 (1.5) | 81.9 (1.1) | 77.4 (1.3) | 0.15 |
| Body Mass Index Score | 65.2 (2.6) | 62.5 (1.5) | 61.5 (1.3) | 52.9 (1.7) | <0.001 |
| Smoking Score | 86.4 (1.8) | 85.4 (2.0) | 87.5 (2.1) | 88.6 (1.6) | 0.50 |
| Sleep Score | 84.5 (1.6) | 86.0 (1.0) | 88.5 (1.5) | 86.3 (1.1) | 0.35 |
| Diet Score | 47.7 (2.0) | 51.1 (1.8) | 49.1 (2.2) | 45.8 (2.2) | 0.25 |
Fig. 2.
Trends of Life's Essential 8 Score and its Components in the Overall Population and Stratified by Place of Birth in the National Health and Nutrition Examination Survey Cycles 2011-March 2020
This figure depicts the trends of the Life's Essential 8 score and its components from 2011-March 2020. The overall population, US-born Asian American individuals, and foreign-born Asian American individuals have been depicted in black, blue, and red, respectively.
After stratification by place of birth, the mean LE8 score was 69.0 (0.8) in US-born participants and 69.1 (0.4) in foreign-born participants (Table 1). A decreasing trend in the BMI score was noted in the US-born [65.0 (4.6) in 2011–2012 to 56.7 (4.5); Ptrend: 0.01] and foreign-born [65.2 (2.6) in 2011–2012 to 52.9 (1.7); Ptrend: <0.001] Asian American individuals. Among foreign-born Asian American individuals, the LE8 score [69.7 (0.8) in 2011–2012 to 67.7(0.8); Ptrend: 0.005] and blood pressure score [73.0 (1.3) in 2011–2012 to 70.3 (1.1); Ptrend: 0.046] decreased between 2011 and 2020 (Table 2) (Fig. 2).
The multivariable-adjusted odds of ideal CVH and components in foreign-born Asian American participants sub-stratified according to the duration of stay in the US (<5 years, 5 to 15 years, 15 to 30 years, and ≥30 years) compared with US-born Asian American individuals are depicted in Table 3. Compared with US-born Asian American individuals, the odds of ideal CVH were similar across the strata of foreign-born Asian American individuals [ORadj: (1.07; 95%CI: 0.69–1.66) with a duration of stay of <5 years; ORadj: 5–15 years (1.07; 95%CI: 0.77–1.49); 15–30 years (ORadj: 0.87; 95%CI: 0.56–1.35); ≥30 years (ORadj: 0.72; 95%CI: 0.49–1.06)]. The odds of ideal diet [ORadj: 1.87 (95%CI: 1.26–2.79) with duration of stay of <5 years; ORadj: 2.00 (95%CI: 1.38–2.89) with duration of stay of 5–15 years; ORadj: 1.74 (95%CI: 1.14–2.68) with duration of stay of 15–30 years; ORadj: 1.19 (0.79–1.77) with duration of stay of ≥30 years] and smoking [ORadj: 2.23 (95%CI: 1.45–3.44) with duration of stay of <5 years; ORadj: 1.97 (95%CI: 1.27–3.05) with duration of stay of 5–15 years; ORadj: 1.61 (95%CI: 1.11–2.34) with duration of stay of 15–30 years; ORadj: 1.69 (95%CI: 1.20–2.36) with duration of stay of ≥30 years] scores were higher across all strata of foreign-born Asian American individuals. Foreign-born Asian American individuals had lower odds of ideal physical activity levels (except those living in the US for <5 years and ≥30 years) [ORadj: 0.55 (95%CI: 0.39–0.79) with duration of stay of 5–15 years; ORadj: 0.68 (95%CI: 0.49–0.95) with duration of stay of 15–30 years] and ideal cholesterol levels (except those living in the US for <5 years) [ORadj: 0.59 (95%CI: 0.42–0.82) with duration of stay of 5–15 years; ORadj: 0.54 (95%CI: 0.38–0.76) with duration of stay of 15–30 years; ORadj: 0.52 (95%CI: 0.35–0.77) with duration of stay of ≥30 years]. The odds of having ideal blood pressure scores were higher in foreign-born Asian Americans residing in the US for <5 years [ORadj: 1.88 (95%CI: 1.23–2.86)] and 5–15 years [ORadj: 1.54 (95%CI: 1.06–2.25)]. Foreign-born Asian American individuals residing in the US for 5–15 years [ORadj: 0.63 (95%CI: 0.41–0.98)] and ≥30 years [ORadj: 0.57 (95%CI: 0.35–0.91)] had lower odds of having ideal HbA1C levels. The odds of ideal sleep duration were lower in foreign-born Asian American individuals living in the US for <5 years [ORadj: 1.52 (95%CI: 1.02–2.27)].
Table 3.
Odds ratio of ideal life's essential 8 score and its components in the overall population and stratified by place of birth and duration of stay in the US in National Health and Nutrition Examination Survey 2011- March 2020.
| Life's Essential 8 Score | Diet | Physical Activity | Blood Pressure | Blood Lipids | Blood Sugar | Body Mass Index | Smoking | Sleep | |
|---|---|---|---|---|---|---|---|---|---|
| US-Born Asian-American Participants | Reference | ||||||||
| Duration of Stay in the US for Foreign-Born Asian American Participants | |||||||||
| <5 Years | 1.07 (0.69–1.66) | 1.87 (1.26–2.79) | 0.70 (0.48–1.03) | 1.88 (1.23–2.86) | 0.70 (0.46–1.06) | 0.66 (0.42–1.03) | 1.00 (0.62–1.59) | 2.23 (1.45–3.44) | 1.52 (1.02–2.27) |
| 5–15 Years | 1.07 (0.77–1.49) | 2.00 (1.38–2.89) | 0.55 (0.39–0.79) | 1.54 (1.06–2.25) | 0.59 (0.42–0.82) | 0.63 (0.41–0.98) | 0.80 (0.56–1.14) | 1.97 (1.27–3.05) | 0.93 (0.64–1.34) |
| 15–30 Years | 0.87 (0.56–1.35) | 1.74 (1.14–2.68) | 0.68 (0.49–0.95) | 1.20 (0.86–1.68) | 0.54 (0.38–0.76) | 0.61 (0.35–1.04) | 0.93 (0.65–1.35) | 1.61 (1.11–2.34) | 0.98 (0.75–1.28) |
| ≥ 30 Years | 0.72 (0.49–1.06) | 1.19 (0.79–1.77) | 0.86 (0.58–1.28) | 1.14 (0.77–1.68) | 0.52 (0.35–0.77) | 0.57 (0.35–0.91) | 0.90 (0.67–1.21) | 1.69 (1.20–2.36) | 0.79 (0.55–1.12) |
Odds ratios (95% confidence interval) of ideal levels (≥80) of the Life's Essential 8 score and its components as the outcome of interest, with non-ideal levels (0–80) as reference, have been presented. US-born Asian-American individuals were taken as the reference population. Foreign-born Asian American individuals were stratified by the duration of stay in the US.
4. Discussion
Among a nationally representative cohort of Asian American individuals, this study noted that the CVH decreased between 2011 and 2020. The decrease in CVH could be attributed to the decline in ideal blood pressure and BMI across the study period. After stratification by place of birth, the mean LE8 score was comparable in US-born Asian American individuals and foreign-born Asian American individuals. Foreign-born Asian American individuals paralleled the trends of the overall Asian American population with a decrease in the overall CVH due to a decline in the ideal blood pressure and BMI scores across the study period. The CVH was stable among US-born Asian American individuals. Only the BMI score displayed a decreasing trend in US-born Asian American individuals. Compared with US-born Asian American individuals, foreign-born Asian American individuals had higher odds of ideal diet and smoking scores but lower odds of ideal physical activity levels, blood lipids, and blood sugar scores. To summarize, the Asian American population had a decline in CVH with notable differences in CVH and its components noted after stratification by place of birth and duration of stay in the US (Central Illustration).
Though the CVH in Asian American individuals did not differ by place of birth, the components of the CVH varied among these subgroups. US-born Asian American individuals had higher scores in the lipids and blood sugar components. Social determinants of health such as education and the yearly number of healthcare visits, may play an essential role in explaining the observed differences in these components by place of birth [23]. Apart from the lack of access to healthcare, other factors such as healthcare literacy and limited proficiency in English may play a role in healthcare-seeking behaviors in Asian American individuals, especially those born outside the US [24]. Limited proficiency in speaking English prevent an individual from seeking healthcare and communicating their ailments [24]. Even with the availability of interpreters, individuals with limited proficiency in English refrain from sharing details of their illnesses [25]. The limited proficiency in English also hampers their ability to improve their healthcare literacy [24]. Additionally, foreign-born Asian American individuals may hold cultural beliefs that prevent them from seeking healthcare and benefitting from preventive health screenings [24]. These factors may lead to the development of distrust in the foreign-born Asian American population toward healthcare providers.
Even though US-born Asian American individuals had higher scores in the abovementioned components compared with foreign-born Asian American individuals, the current study noted that detrimental health behaviors such as smoking and poor diet were more common in US-born Asian American individuals compared with foreign-born Asian American individuals. Furthermore, the likelihood of having ideal levels of diet and smoking habits decreased with increasing duration of stay in the US in foreign-born Asian American individuals. The phenomenon wherein recent immigrants to the US are healthier compared with long-term residents has been termed the healthy immigrant effect [26,27]. The healthy immigrant effect has been attributed to recent immigrants' higher educational attainment and socioeconomic status [26,28]. However, the advantage presented by the healthy immigrant effect has been observed to diminish over time [27]. This gradual decrease in CVH with increasing duration of stay in US highlights the role of acculturation as a determinant of CVH [4,5,[29], [30], [31], [32], [33]]. Acculturation is a phenomenon where immigrants adopt the cultural and social beliefs prevalent in the new country [34]. The role of acculturation has been well established as a predictor of CVH in several immigrant populations in the US [4,5,[29], [30], [31], [32], [33],35]. With increasing duration of residence in the US, foreign-born Asian American individuals gradually adapt their diet to the dietary pattern that is prevalent in the US [29,36]. This change in dietary pattern is associated with increased consumption of processed foods, sugar-sweetened beverages, and red meat [32,36]. Although acculturation mainly leads to deterioration in health behaviors, an improvement in physical activity levels could be attributed to acculturation [29,33,35]. Physical activity levels are independently associated with each component of acculturation (language spoken at home, place of birth, and duration of stay in the US) [37,38]. As acculturation increases with the duration of stay in the US, attitudes towards physical activity may change. This helps overcome cultural barriers to physical exercise such as religious beliefs, lack of social support, lack of awareness of the benefits of physical activity, and lack of time [37,39]. Furthermore, the improvement in physical activity may also be attributed to the improvement in the socioeconomic status and education level with increasing duration of stay in the US [38].
Asian American individuals have been shown to have better CVH compared with the overall US population [6,22]. The higher CVH in Asian American individuals may be attributed to a better diet and a lower prevalence of smoking [6,22]. The remaining six determinants of CVH were similar in the overall US population and Asian American individuals [6,22]. These findings, concurrent with the current study, may help in the identification of potential targets to further improve the CVH in the Asian American population. Additionally, health behaviors, especially diet, in the Asian American population may be used as a reference to enhance the CVH of the US population.
On comparing the trends of the components of the LE8 score, Asian American individuals mirrored the overall population trends [40], [41], [42], [43]. Systolic blood pressure and BMI in the overall US population have been reported to increase over the last decade [43,44]. Asian American individuals, specifically foreign-born Asian American individuals, also displayed similar trends in systolic blood pressure and BMI. Though not statistically significant, HbA1C levels increased and the prevalence of smoking decreased in Asian American individuals, similar to the overall US population [40,45]. A noteworthy finding of the current study is that contrary to the decreasing trends in the serum cholesterol levels in the overall US population, Asian American individuals had a stable blood lipids score during the study period [40,42,46]. The reasons for this difference in the trend of cholesterol levels are unclear. Though an increasing trend in cholesterol screening was noted in other racial and ethnic groups, the trend for cholesterol screening remained stable in Asian American individuals [42]. The decline in cholesterol levels in the overall US population has been attributed to the increased use of statins post the 2013 cholesterol guidelines [16,46]. Lack of awareness, stable cholesterol screening trends, statin prescription patterns, and medication adherence may play a role in the stable blood cholesterol trends in Asian American individuals. Even though South Asian ethnicity has been recognized as a risk-enhancing factor for CV disease and the known efficacy of statins in Asian individuals, there may be a hesitancy in prescribing statins due to an increased risk of statin-related adverse events in Asian individuals [47,48].
The current study builds on the previous literature by examining the trends of CVH in Asian American individuals over a longer period and utilizing the new LE8 score for CVH measurement as endorsed by the AHA. A previous NHANES study analyzing the trend of CVH using the LS7 score in the Asian American population from 2011 to 2016 demonstrated a decrease in the ideal levels of diet, physical activity, and BMI and a stable trend for ideal levels of smoking, blood cholesterol, blood pressure, and blood glucose [5]. The differences in the trends of the CVH components noted in the prior and current study may be attributed to the different tools used to measure CVH. While the LS7 score measures each component using 3 levels (ideal, intermediate, and poor), the LE8 score has at least 5 levels for each component. The additional levels in the LE8 score improve the granularity of measurement and provide a more accurate representation of the CVH component. Apart from these 7 components, the current study noted that the sleep score was above ideal levels across the study period in Asian American individuals. However, prior studies, including a meta-analysis, showed that Asian American individuals have lower sleep quality and duration compared with non-Hispanic White individuals [9,10,49]. Poor sleep in Asian American individuals has been attributed to acculturation stress and socioeconomic factors [49,50]. Furthermore, this study also contributes to limited research examining the “healthy immigrant paradox” among Asian American individuals. A prior examination of the “healthy immigrant paradox” among Asian American individuals showed that foreign-born Asian American individuals had reduced odds of mental disorders or anxiety [51]. However, the health-protective effect of being foreign-born was insignificant after accounting for social determinants of health and psychosocial factors [51]. The present analysis similarly found that being foreign-born was not associated with poorer CVH among Asian American individuals.
The declining CVH in Asian American individuals has several large-scale implications. The proportional mortality for ischemic heart disease and cerebrovascular disease has been reported to be higher in Asian American individuals compared with non-Hispanic White individuals [52,53]. This racial disparity in CV disease burden is expected to widen considering the declining CVH noted in Asian American individuals. Therefore, it is necessary to promote preventive measures to improve CVH aggressively. In an era where individualization of therapy is the norm, a similar ideology must be applied to individualize diagnostic criteria and target levels for treatment. The recognition of individualized BMI cut-offs for Asian American individuals is a step in the right direction [7,54,55]. The current study utilizes these Asian-specific BMI cut-offs which allows a more accurate estimation of CVH in Asian American individuals. Similar efforts are needed to generate specific cut-offs for other determinants of CVH for Asian American individuals. While a comprehensive approach to improving all the determinants of CVH in Asian American individuals is encouraged, special attention must be paid to blood lipid levels. Further research is needed to determine the underlying cause for the lack of improvement in cholesterol levels in Asian American individuals. The current study highlights the need to conduct studies in the Asian American population, such as the MASALA study, to understand the differences in the epidemiology and pathophysiology of CV disease and develop specific treatment recommendations [56].
4.1. Limitations
The current study has several limitations. First, due to the cross-sectional nature of the NHANES, causality cannot be inferred. Furthermore, the trends of CVH could not be measured at an individual level. Third, self-reported race and ethnicity was collected in the NHANES. The self-reported race and ethnicity may not be representative of the genetic ancestry. Importantly, though heterogeneity in the CVH and prevalence of CV diseases have been reported among the Asian subgroups, the data on Asian subgroups is not publically available on the NHANES. Therefore, the current study assessed the CVH in the overall Asian American population. Fifth, data for health behaviors such as diet, exercise, sleep, and smoking were self-reported and are susceptible to recall bias. Finally, though the NHANES oversampled Asian American individuals, the exclusion of individuals due to missing components for the calculation of the LE8 score may increase the variances in the estimates generated.
5. Conclusion
This population-level study showed that CVH in Asian American individuals declined from 2011 to 2020. Though the CVH was similar in foreign-born and US-born Asian American individuals, the components of CVH varied among these groups. The likelihood of having ideal health behaviors and factors reduces with increasing duration of stay in the US. Further research should focus on delineating treatment guidelines, CV risk factor cut-offs, and target levels for treatment specific to the Asian population.
Author contributions
NSS, NP, and PA contributed to the conception, design, acquisition, analysis, interpretation, drafting, and critical revision of the manuscript. GA contributed to the conception, design, acquisition, interpretation, and critical revision of the manuscript. MG contributed to the analysis, interpretation, and drafting of the manuscript. RK, PL, and GP contributed to the design, interpretation, and drafting of the manuscript.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Source of Funding
Dr. Pankaj Arora is supported by the National Heart, Lung, and Blood Institute of the National Institutes of Health (NIH) awards R01HL160982, R01HL163852, R01HL163081, and K23HL146887.
Acknowledgments
None.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.ajpc.2023.100509.
Appendix. Supplementary materials
References
- 1.Vespa J., Armstrong D.M., Medina L. US Department of Commerce, Economics and Statistics Administration; Washington, DC: 2018. Demographic turning points for the United States: population projections for 2020 to 2060. US Census Bureau. [Google Scholar]
- 2.Hoeffel E.M., Rastogi S., Kim M.O., Hasan S. US Department of Commerce, Economics and Statistics Administration, US Census Bureau; 2012. The Asian population: 2010. [Google Scholar]
- 3.Tsao C.W., Aday A.W., Almarzooq Z.I., et al. Heart disease and stroke statistics-2023 update: a report from the american heart association. Circulation. 2023;147:e93–e621. doi: 10.1161/CIR.0000000000001123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Al Rifai M., Kianoush S., Jain V., et al. Association of U.S. birth, duration of residence in the U.S., and atherosclerotic cardiovascular disease risk factors among Asian adults. Prev Med Rep. 2022;29 doi: 10.1016/j.pmedr.2022.101916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kalra R., Patel N., Arora P., Arora G. Cardiovascular health and disease among Asian-Americans (from the national health and nutrition examination survey) Am J Cardiol. 2019;124 doi: 10.1016/j.amjcard.2019.04.026. 270-7. [DOI] [PubMed] [Google Scholar]
- 6.Fang J., Zhang Z., Ayala C., Thompson-Paul A.M., Loustalot F. Cardiovascular health among non-hispanic Asian Americans: NHANES, 2011-2016. J Am Heart Assoc. 2019;8 doi: 10.1161/JAHA.118.011324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lloyd-Jones D.M., Allen N.B., Anderson C.A.M., et al. Life's essential 8: updating and enhancing the American heart association's construct of cardiovascular health: a presidential advisory from the american heart association. Circulation. 2022;146:e18–e43. doi: 10.1161/CIR.0000000000001078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shetty N.S., Parcha V., Patel N., et al. AHA Life's essential 8 and ideal cardiovascular health among young adults. Am J Prev Cardiol. 2023;13 doi: 10.1016/j.ajpc.2022.100452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nandagiri V., Vannemreddy S., Spector A. Sleep disparities in Asian Americans: a comprehensive review. J Clin Sleep Med. 2023;19:393–402. doi: 10.5664/jcsm.10330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Johnson D.A., Jackson C.L., Williams N.J., Alcantara C. Are sleep patterns influenced by race/ethnicity - a marker of relative advantage or disadvantage? Evidence to date. Nat Sci Sleep. 2019;11:79–95. doi: 10.2147/NSS.S169312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lloyd-Jones D.M., Allen N.B., Anderson C.A.M., et al. Life's essential 8: updating and enhancing the American heart association's construct of cardiovascular health: a presidential advisory from the American heart association. Circulation. 2022 doi: 10.1161/CIR.0000000000001078. 101161CIR0000000000001078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.St-Onge M.P., Grandner M.A., Brown D., et al. Sleep duration and quality: impact on lifestyle behaviors and cardiometabolic health: a scientific statement from the American heart association. Circulation. 2016;134 doi: 10.1161/CIR.0000000000000444. e367-e86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zipf G., Chiappa M., Porter K.S., Ostchega Y., Lewis B.G., Dostal J. National health and nutrition examination survey: plan and operations, 1999-2010. Vital Health Stat. 2013;1:1–37. [PubMed] [Google Scholar]
- 14.Parcha V., Patel N., Kalra R., Arora G., Prevalence Arora P. Awareness, treatment, and poor control of hypertension among young American adults: race-stratified analysis of the national health and nutrition examination survey. Mayo Clin Proc. 2020;95 doi: 10.1016/j.mayocp.2020.01.041. 1390-403. [DOI] [PubMed] [Google Scholar]
- 15.Kalra R., Parcha V., Patel N., et al. Increased awareness, inadequate treatment, and poor control of cardiovascular risk factors in American young adults: 2005-2016. Eur J Prev Cardiol. 2021;28 doi: 10.1177/2047487320905190. 304-12. [DOI] [PubMed] [Google Scholar]
- 16.Patel N., Bhargava A., Kalra R., et al. Trends in lipid, lipoproteins, and statin use among U.S. adults: impact of 2013 cholesterol guidelines. J Am Coll Cardiol. 2019;74 doi: 10.1016/j.jacc.2019.09.026. 2525-8. [DOI] [PubMed] [Google Scholar]
- 17.Patel N., Kalra R., Bhargava A., Arora G., Arora P. Ideal cardiovascular health among American Adults after the economic recession of 2008-2009: insights from NHANES. Am J Med. 2019;132 doi: 10.1016/j.amjmed.2019.06.004. 1182-90 e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Paulose-Ram R., Burt V., Broitman L., Ahluwalia N. Overview of Asian American Data Collection, Release, and Analysis: national Health and Nutrition Examination Survey 2011-2018. Am J Public Health. 2017;107 doi: 10.2105/AJPH.2017.303815. 916-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Analytic guidance and brief overview for the 2017-March 2020 pre-pandemic data files. National Center for Health Statistics; 2021.
- 20.Lloyd-Jones D.M., Ning H., Labarthe D., et al. Status of cardiovascular health in us adults and children using the American heart association's new "life's essential 8" metrics: prevalence estimates from the national health and nutrition examination survey (NHANES), 2013-2018. Circulation. 2022 doi: 10.1161/CIRCULATIONAHA.122.060911. [DOI] [PubMed] [Google Scholar]
- 21.Mellen P.B., Gao S.K., Vitolins M.Z., Goff D.C., Jr Deteriorating dietary habits among adults with hypertension: DASH dietary accordance, NHANES 1988-1994 and 1999-2004. Arch Intern Med. 2008;168 doi: 10.1001/archinternmed.2007.119. 308-14. [DOI] [PubMed] [Google Scholar]
- 22.Lloyd-Jones D.M., Ning H., Labarthe D., et al. Status of cardiovascular health in US adults and children using the American heart association's new "life's essential 8" metrics: prevalence estimates from the national health and nutrition examination survey (NHANES), 2013 through 2018. Circulation. 2022;146 doi: 10.1161/CIRCULATIONAHA.122.060911. 822-35. [DOI] [PubMed] [Google Scholar]
- 23.Johnson A.E., Herbert B.M., Stokes N., Brooks M.M., Needham B.L., Magnani J.W. Educational attainment, race, and ethnicity as predictors for ideal cardiovascular health: from the national health and nutrition examination survey. J Am Heart Assoc. 2022;11 doi: 10.1161/JAHA.121.023438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kim W., Keefe R.H. Barriers to healthcare among Asian Americans. Soc Work Public Health. 2010;25 doi: 10.1080/19371910903240704. 286-95. [DOI] [PubMed] [Google Scholar]
- 25.Green A.R., Ngo-Metzger Q., Legedza A.T., Massagli M.P., Phillips R.S., Iezzoni L.I. Interpreter services, language concordance, and health care quality. Experiences of Asian Americans with limited English proficiency. J Gen Intern Med. 2005;20 doi: 10.1111/j.1525-1497.2005.0223.x. 1050-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McDonald J.T., Kennedy S. Insights into the 'healthy immigrant effect': health status and health service use of immigrants to Canada. Soc Sci Med. 2004;59 doi: 10.1016/j.socscimed.2004.02.004. 1613-27. [DOI] [PubMed] [Google Scholar]
- 27.Helgesson M., Johansson B., Nordquist T., Vingard E., Svartengren M. Healthy migrant effect in the Swedish context: a register-based, longitudinal cohort study. BMJ Open. 2019;9 doi: 10.1136/bmjopen-2018-026972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kennedy S., McDonald J.T., Biddle N. The healthy immigrant effect and immigrant selection: evidence from four countries. 2006.
- 29.Li Y., Zhu A., Le A., et al. Association of acculturation with cardiovascular risk factors in Asian-American subgroups. Am J Prev Cardiol. 2023;13 doi: 10.1016/j.ajpc.2022.100437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Goel M.S., McCarthy E.P., Phillips R.S., Wee C.C. Obesity among US immigrant subgroups by duration of residence. JAMA. 2004;292 doi: 10.1001/jama.292.23.2860. 2860-7. [DOI] [PubMed] [Google Scholar]
- 31.Rodriguez F., Echeverria S.E., Pentakota S.R., Amadi C., Hastings K.G., Palaniappan L.P. Comparison of ideal cardiovascular health attainment and acculturation among Asian Americans and Latinos. Ethn Dis. 2019;29 doi: 10.18865/ed.29.2.287. 287-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pachipala K., Shankar V., Rezler Z., et al. Acculturation and associations with ultra-processed food consumption among Asian Americans: NHANES, 2011-2018. J Nutr. 2022;152 doi: 10.1093/jn/nxac082. 1747-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Koya D.L., Egede L.E. Association between length of residence and cardiovascular disease risk factors among an ethnically diverse group of United States immigrants. J Gen Intern Med. 2007;22 doi: 10.1007/s11606-007-0163-y. 841-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Berry J. Cambridge University Press; Cambridge: 2019. Acculturation: a personal journey across cultures (elements in psychology and culture) [Google Scholar]
- 35.Osibogun O., Ogunmoroti O., Mathews L., Okunrintemi V., Tibuakuu M., Michos E.D. Greater acculturation is associated with poorer cardiovascular health in the multi-ethnic study of atherosclerosis. J Am Heart Assoc. 2021;10 doi: 10.1161/JAHA.120.019828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lesser I.A., Gasevic D., Lear S.A. The association between acculturation and dietary patterns of South Asian immigrants. PLoS One. 2014;9:e88495. doi: 10.1371/journal.pone.0088495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhu X., Liu J., Sevoyan M., Pate R.R. Acculturation and leisure-time physical activity among Asian American adults in the United States. Ethn Health. 2022;27 doi: 10.1080/13557858.2021.1979193. 1900-14. [DOI] [PubMed] [Google Scholar]
- 38.Kandula N.R., Lauderdale D.S. Leisure time, non-leisure time, and occupational physical activity in Asian Americans. Ann Epidemiol. 2005;15 doi: 10.1016/j.annepidem.2004.06.006. 257-65. [DOI] [PubMed] [Google Scholar]
- 39.Gerber M., Barker D., Pühse U. Acculturation and physical activity among immigrants: a systematic review. J Public Health. 2012;20 313–41. [Google Scholar]
- 40.He J., Zhu Z., Bundy J.D., Dorans K.S., Chen J., Hamm L.L. Trends in cardiovascular risk factors in US adults by race and ethnicity and socioeconomic status, 1999-2018. JAMA. 2021;326 doi: 10.1001/jama.2021.15187. 1286-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Du Y., Liu B., Sun Y., Snetselaar L.G., Wallace R.B., Bao W. Trends in adherence to the physical activity guidelines for Americans for aerobic activity and time spent on sedentary behavior among US adults, 2007 to 2016. JAMA Netw Open. 2019;2 doi: 10.1001/jamanetworkopen.2019.7597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gao Y., Shah L.M., Ding J., Martin S.S. US trends in cholesterol screening, lipid levels, and lipid-lowering medication use in US adults, 1999 to 2018. J Am Heart Assoc. 2023;12 doi: 10.1161/JAHA.122.028205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Muntner P., Hardy S.T., Fine L.J., et al. Trends in blood pressure control among US adults with hypertension, 1999-2000 to 2017-2018. JAMA. 2020;324 doi: 10.1001/jama.2020.14545. 1190-200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Liu B., Du Y., Wu Y., Snetselaar L.G., Wallace R.B., Bao W. Trends in obesity and adiposity measures by race or ethnicity among adults in the United States 2011-18: population based study. BMJ. 2021;372:n365. doi: 10.1136/bmj.n365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wang L., Li X., Wang Z., et al. Trends in prevalence of diabetes and control of risk factors in diabetes among US adults, 1999-2018. JAMA. 2021;326:1–13. doi: 10.1001/jama.2021.9883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Aggarwal R., Bhatt D.L., Rodriguez F., Yeh R.W., Wadhera R.K. Trends in lipid concentrations and lipid control among US adults, 2007-2018. JAMA. 2022;328 doi: 10.1001/jama.2022.12567. 737-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Volgman A.S., Palaniappan L.S., Aggarwal N.T., et al. Atherosclerotic cardiovascular disease in south Asians in the United States: epidemiology, risk factors, and treatments: a scientific statement from the American heart association. Circulation. 2018;138:e1–e34. doi: 10.1161/CIR.0000000000000580. [DOI] [PubMed] [Google Scholar]
- 48.Newman C.B., Preiss D., Tobert J.A., et al. Statin safety and associated adverse events: a scientific statement from the American Heart association. Arterioscler Thromb Vasc Biol. 2019;39:e38–e81. doi: 10.1161/ATV.0000000000000073. [DOI] [PubMed] [Google Scholar]
- 49.Whinnery J., Jackson N., Rattanaumpawan P., Grandner M.A. Short and long sleep duration associated with race/ethnicity, sociodemographics, and socioeconomic position. Sleep. 2014;37 doi: 10.5665/sleep.3508. 601-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Jackson C.L., Kawachi I., Redline S., Juon H.S., Hu F.B. Asian-White disparities in short sleep duration by industry of employment and occupation in the US: a cross-sectional study. BMC Public Health. 2014;14:552. doi: 10.1186/1471-2458-14-552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.John D.A., de Castro A.B., Martin D.P., Duran B., Takeuchi D.T. Does an immigrant health paradox exist among Asian Americans? Associations of nativity and occupational class with self-rated health and mental disorders. Soc Sci Med. 2012;75 doi: 10.1016/j.socscimed.2012.01.035. 2085-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Shah N.S., Xi K., Kapphahn K.I., et al. Cardiovascular and cerebrovascular disease mortality in Asian American subgroups. Circ Cardiovasc Qual Outcomes. 2022;15 doi: 10.1161/CIRCOUTCOMES.121.008651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Jose P.O., Frank A.T., Kapphahn K.I., et al. Cardiovascular disease mortality in Asian Americans. J Am Coll Cardiol. 2014;64 doi: 10.1016/j.jacc.2014.08.048. 2486-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hsu W.C., Araneta M.R., Kanaya A.M., Chiang J.L., Fujimoto W. BMI cut points to identify at-risk Asian Americans for type 2 diabetes screening. Diabetes Care. 2015;38 doi: 10.2337/dc14-2391. 150-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Consultation WHOE Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363 doi: 10.1016/S0140-6736(03)15268-3. 157-63. [DOI] [PubMed] [Google Scholar]
- 56.Kanaya A.M., Kandula N., Herrington D., et al. Mediators of Atherosclerosis in South Asians Living in America (MASALA) study: objectives, methods, and cohort description. Clin Cardiol. 2013;36 doi: 10.1002/clc.22219. 713-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.