Abstract
Background:
For needle arthroscopy with 0° viewing, the visible range of intra-articular structures and the difference between portals remain unknown, as do the risks for neurovascular tissue at each portal.
Purpose:
To clarify the visibility and safety of needle arthroscopy.
Study Design:
Descriptive laboratory study.
Methods:
Ten cadaveric ankle specimens were used. A needle arthroscope with a 1.9-mm diameter was inserted from 4 portals (anteromedial [AM], anterolateral [AL], medial midline [MM], and anterocentral [AC]). Visibility was assessed using a 15-point ankle arthroscopy checklist. In addition, the ankles were dissected to measure the distance between each portal and neurovascular tissues. The visibility of the ankle joint was compared between portals.
Results:
The success rate of visibility in the deltoid ligament and the tip of the medial malleolus was 100% from the AM, MM, and AC portals and 10% from the AL portal, with significant differences between the portals (P < .01). The visibility success rates in the origin of the anterior talofibular ligament and the tip of the lateral malleolus were 20% for the AM portal, 90% for the MM and AC portals, and 100% for the AL portal, with significant differences between the portals (P < .01). All other points of the ankle joint were visualized from all the portals with a 100% success rate. The AC portal was in contact with the anterior neurovascular bundle in 4 of the 10 specimens.
Conclusion:
When needle arthroscopy was performed from the AM or AL portal, the site opposite to the portal in the ankle joint was difficult to visualize. Conversely, most points of the ankle joint could be visualized from the MM and AC portals. Care should be taken when creating an AC portal because of its proximity to the anterior neurovascular bundle.
Clinical Relevance:
The present study provides information regarding which portal should be selected to perform needle arthroscopy in the ankle joint, which will be beneficial for management of ankle injuries.
Keywords: ankle joint, needle arthroscopy, safety, visibility
Anterior ankle arthroscopy is a minimally invasive diagnostic and therapeutic procedure for acute and chronic ankle symptoms. 33 Therefore, it has been used for athletes with sports injuries. Despite improvements in radiographic modalities, diagnostic ankle arthroscopy is more valuable than magnetic resonance imaging (MRI) for detecting osteochondral lesions, syndesmotic injuries, and loose bodies.4,18 Anterior ankle arthroscopy is commonly indicated as a therapeutic procedure for ankle injuries associated with trauma and overuse, including anterior ankle impingement, intra-articular fracture, and osteochondral lesions. 34 In addition, interest in the arthroscopic technique for lateral ankle ligament injury has recently increased. 35 Clinical evidence has suggested reduced morbidity and faster rehabilitation, making this technique more appealing for practicing orthopaedic surgeons than open arthrotomy.4,38 In contrast with these developments, ankle arthroscopy has several downsides, including risks to neurovascular tissue34,37 and cartilage, 37 the need for general or spinal anesthesia and an operating room, and a tendency for unnecessary hospital stays.
Needle arthroscopy began to be developed22,23 in the 1990s, and as technology improved, much attention was given to in-office needle arthroscopy (IONA). IONA is considered to be inherently less invasive than conventional arthroscopy.4,28 Because of this characteristic, IONA is expected to be widely used for athletes with sports injuries in the near future. Although the medical cost usually depends on the medical system of each country, IONA under local anesthesia can cost less than MRI in several countries. 1 Reportedly, IONA can be utilized to diagnose and treat several musculoskeletal disorders, including biceps tenotomy, rotator cuff repair, meniscectomy, meniscal repair, and cheilectomy for hallux rigidus.4,9,11,15,17,24,29,38 Regarding ankle disorders, Dankert et al 7 reported that IONA was valuable in removing loose osseous bodies that could not be identified by MRI. Colasanti et al 4 reported that IONA for anterior ankle impingement resulted in high patient satisfaction.
However, this novel technique presents new concerns. The viewing range of needle arthroscopy differs from that of conventional arthroscopy, with oblique viewing since needle arthroscopy has a 0° angle. In 2020, Stornebrink et al 28 investigated the efficacy and safety of ankle needle arthroscopy, as the safety and efficacy of 2 mm–diameter operative arthroscopy of the ankle were unknown. These authors reported that needle arthroscopy inserted from the anteromedial portal could visualize 96% of the talar and 85% of the tibial surface. However, the visible range of the intra-articular structures, other than articular surfaces, and the differences between portals remain unknown. Moreover, the risk of nerve injury at each portal should be investigated, as this is the most critical and frequent complication of ankle arthroscopy.25,32 Clarifying these concerns will contribute to improving the efficacy and safety of IONA use for athletes with ankle disorders.
In the present study, we aimed to clarify the visualizable range of the ankle joint using needle arthroscopy when performed from several portals and investigate the risk of neurovascular injury. We hypothesized that the viewing range of needle arthroscopy would be different between portals and that a risk of nerve injury per portal would be revealed.
Methods
Specimens
Ethics committee approval was obtained for the present study. Specimens were obtained through the Science Care donation program and donated with consent for use in medical science. A total of 5 specimens with 10 ankles (mean age, 90.2 ± 7.2 years; 2 men and 3 women) were included in the present study. Thiel-embalmed cadavers with whole bodies and bilateral ankles were studied. Specimens with a history of surgery or contractures were excluded. Radiographs were used to confirm the absence of severe arthritis or ankle fractures.
Needle Arthroscopy
All procedures were performed by a single surgeon (Y.Y.) with >15 years of experience in arthroscopic ankle surgery. Each specimen was placed in the supine position. Four standard portals (anteromedial [AM], anterolateral [AL], medial midline [MM], and anterocentral [AC]) were created just medial to the tibialis anterior tendon, just lateral to the peroneus tertius tendon, at the level between the tibialis anterior tendon and the extensor hallucis longus tendon, and at the level between the extensor hallucis longus tendon and the extensor digitorum communis tendon, respectively.2,4,34 After a stab incision, a 1.9 mm–needle arthroscope with 0° viewing (NanoScope; Arthrex) was inserted into the joint. A 0.9% saline solution was used to irrigate the joints. First, the anterior compartment was visualized without joint distraction (Figure 1A). Next, the joint was manually distracted using the bandage distraction technique, 31 and the central part of the joint was observed (Figure 1B). A 2.0-mm shaver (Arthrex) was used to remove any soft tissue—such as synovial hyperplasia or cicatrization—that obstructed the visualization. A previously published 15-point diagnostic checklist of areas to visualize during the examination was used (Figure 2). 19
Figure 1.
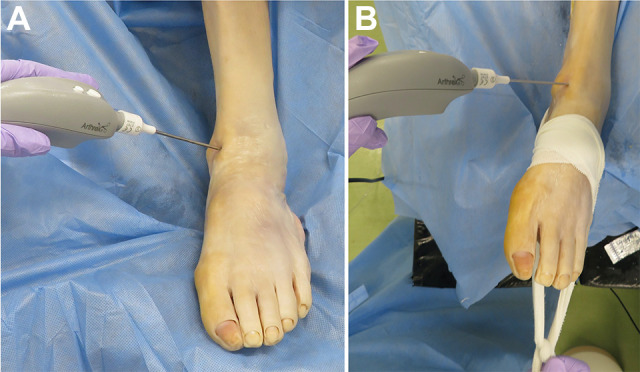
Arthroscopic examination (A) without distraction and (B) with distraction using a bandage.
Figure 2.
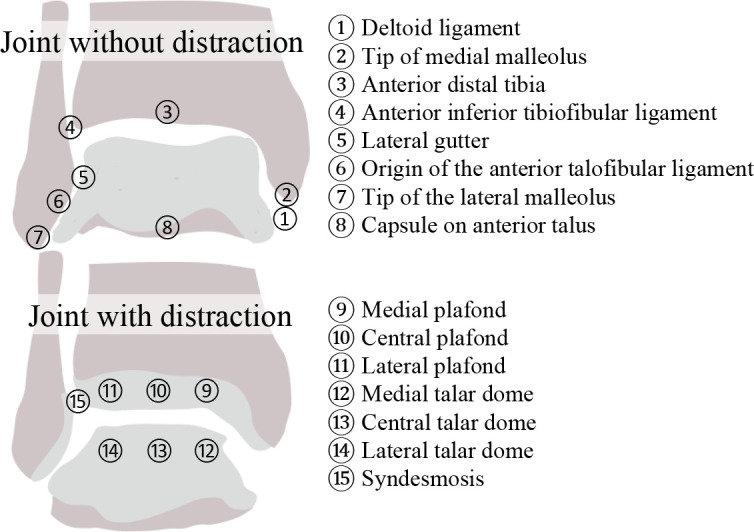
Points to visualize using the arthroscope.
Videos created during the examination were analyzed by another orthopaedic surgeon (J.I.) with 8 years of experience in arthroscopic ankle surgery who was blinded to the findings during the examination. Visualization of each point was assessed using binary variables (yes or no).
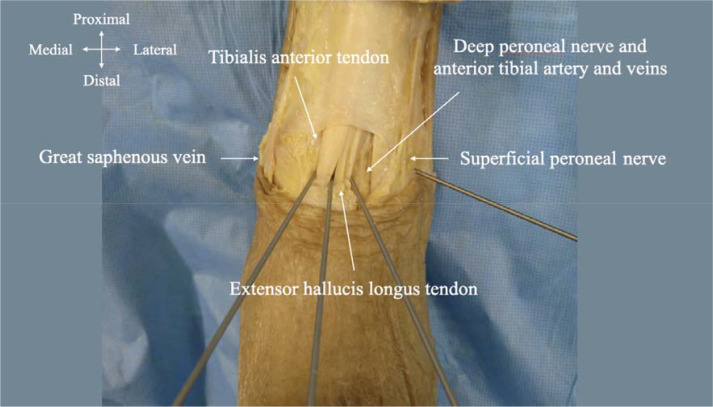
Assessment for Neurovascular Proximity
After the arthroscopic examination, a 1.8 mm–diameter Kirschner wire was introduced at each portal site and inserted into the bone (Figure 3). Each ankle was dissected while taking care to maintain the position of the Kirschner wires to assess the distance between each portal and the important neurovascular tissue. The skin was removed, and the great saphenous vein and the superficial peroneal nerve were identified. The extensor retinaculum was then removed, and the anterior neurovascular bundle (deep peroneal nerve, anterior tibial artery, and veins) was revealed. The distances between each Kirshner wire and the neurovascular structures close to the wires were measured using a digital caliper with a resolution of 0.1 mm (Niigata seiki).
Figure 3.
Dissected left ankle with the 4 portal sites. The distance between a Kirshner wire inserted into each portal and important neurovascular tissue was measured.
Statistical Analysis
Points to be visualized were reported as frequencies with percentages according to the rate of visible numbers, which were compared among the portals using the Fisher exact test. If there was a significant difference among portals, post hoc pairwise comparisons were performed with the Bonferroni correction. The distance between the anterior neurovascular bundle and the portals was compared using the Friedman test. If there were significant differences, post hoc pairwise comparisons were conducted with the Bonferroni correction. Statistical significance was set at P < .05. All statistical analyses were performed using the open-source statistical computing software R package (The R Foundation for Statistical Computing, http://www.r-project.org).
Results
Differences of Visibility Between Portals
Regarding the deltoid ligament and the tip of the medial malleolus, the rate of successful visualization was 100% in the AM, MM, and AC portals and 10% in the AL portal, with a significant difference in visibility between the portals (P < .01). Regarding the origin of the anterior talofibular ligament and the lateral malleolus tip, the rate of successful visualization was significantly different between the portals (AM, 20%; MM, 90%; AC, 90%; and AL, 100%; P < .01).
All other points were confirmed with 100% visibility from every portal. The percentage of points that could be visualized from each portal and the results of the post hoc pairwise comparisons are shown in Table 1.
Table 1.
Percentage of the 15 Points That Could Be Visualized From Each Portal a
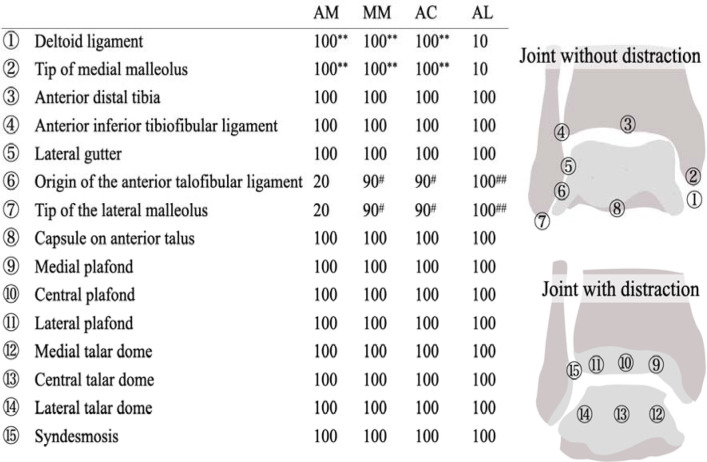
|
a Data are reported as percentage of all ankles. AC, anterocentral; AM, anteromedial; AL, anterolateral; MM, medial midline.
b Significant differences compared with AL (P < .01)
c Significant differences compared with AM (P < .05).
d Significant differences compared with AM using post hoc pairwise comparisons (P < .01).
Assessment for Neurovascular Proximity
The distances between the portals and neurovascular tissues are shown in Table 2. The AM and AL portals were sufficiently far away from the neurovascular tissues traveling nearby. Regarding the anterior neurovascular bundle, the AC portal was significantly closer to the bundle than the AM and MM portals. In 4 patients, the Kirschner wire from the AC portal was in contact with the anterior neurovascular bundle, and this was measured as 0 mm.
Table 2.
Distance Between Portal and Neurovascular Tissue a
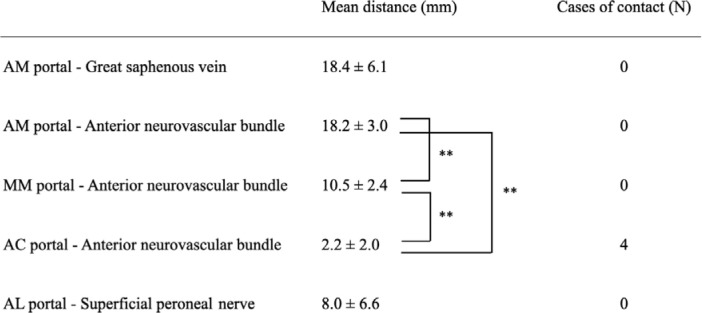
|
a AC, anterocentral; AL, anterolateral; AM, anteromedial; MM, medial midline.
b Significant differences (P < .01) using post hoc pairwise comparisons.
Discussion
In the present study, needle arthroscopy, in which the arthroscope is inserted from both the AC and the MM portals, was able to visualize almost all 15 points in the ankle joint. However, the AL and AM portals had difficulty visualizing the opposite sides of the ankle joint. In addition, the AC portal had a high risk of contact with the anterior neurovascular bundle. To our knowledge, no study has addressed the areas of arthroscopic visualization or addressed the risk of iatrogenic neurovascular tissue injury for each portal in needle arthroscopy. Needle arthroscopy is not a new technology; it has been in use since the 1990s.22,23 However, it did not gain popularity because of the poor quality of the images. Recently, improved image quality has made many clinicians pay greater attention to this modality. The development and advancement of IONA can increase the utilization of this new modality, which has so far been limited to only a few experts. In a recent systematic review, Zhang et al 38 described that “IONA holds potential for cost savings and improved diagnostic accuracy relative to MRI, primarily for intra-articular meniscal, ligamentous, and chondral defects of the knee.” However, they also described how “the current quality and breadth of evidence are significantly lacking, with numerous practical shortcomings. To improve acceptance of IONA, priority should be placed on establishing defined protocols, indications, contraindications, and patient perspectives for the procedure.” The outcomes demonstrated in the present study can become a new body of scientific evidence, which will help physicians who are unfamiliar with IONA to perform diagnostic and therapeutic interventions using needle arthroscopy.
IONA was reported to have more accuracy and lower cost than MRI in the knee and the shoulder.12,21,36 Although the cost of IONA may be higher compared with MRI in several countries because the medical cost usually depends on the medical system of each country, IONA could be superior in detecting the small size of loose bodies or osteochondral defects compared with MRI. 28 Small and Del Gallo 26 reported that the indications for IONA were bony or soft tissue impingement, osteochondral lesions, loose bodies, synovitis, arthrofibrosis, and instability. Labib and Slone 16 reported that needle arthroscopy would be useful to assess the syndesmotic injuries and verify joint reduction. In addition, needle arthroscopy could be used for patients who have undergone osteosynthesis for ankle fracture and had residual pain in their ankle joint since the hardware around the joint would obstruct the image quality of imaging modalities. The flip side of these benefits is that IONA is invasive with potential complications (nerve injuries, wound healing problems, deep vein thrombosis, and septic arthritis). In addition, needle arthroscopy cannot visualize subchondral bone, which means IONA is not good for some disorders, including bone bruises and subchondral cysts. Although further studies about the cost, effectiveness, and safety of IONA are required, we believe that a good indication for using IONA as a diagnostic modality is for patients with ankle pain that cannot be detected by MRI or who cannot undergo MRI due to claustrophobia or metal implantations. Additionally, IONA can be indicated for patients who accept the risk of IONA.
In the present study, the surgeons with sufficient experience in conventional ankle arthroscopy were able to visualize all points of the ankle joint using needle arthroscopy without experience with this technique. The learning curve of conventional arthroscopy has been reported: increasing experience in the procedure decreases the operating time and leads to better clinical outcomes.5,14,20 Meanwhile, there has been no report about the learning curve of needle arthroscopy. To date, IONA has been performed by only a few experts. As the pioneers of this method, Colasanti et al 3 have reported that a disadvantage of IONA might be the learning curve. However, the surgeon involved in the present study was able to confirm all points in the ankle in each specimen, despite lacking experience in needle arthroscopy. In light of the results of the present study, we believe that the visualization of the ankle joint with needle arthroscopy may be uncomplicated for experts familiar with conventional arthroscopic techniques. On the other hand, there are no data regarding physicians unfamiliar with conventional arthroscopic techniques. Considering the decision making about the indications of IONA for ankle disorders and the handling of problems, such as unexpected bleeding, the ideal person to start with IONA is a surgeon with enough experience in ankle arthroscopy. Given the possibility that IONA will be widely used in the future, further studies examining the learning curve are warranted.
The AM and AL portals are the standard portals for anterior ankle arthroscopy, in which 2.7- or 4.0-mm 30° oblique arthroscopy is commonly used. When using conventional arthroscopy with a 30° oblique view, both the deltoid and anterior tibiofibular ligaments can be visualized from the AM portal. 6 However, in the present study, we observed that the anterior tibiofibular ligament was difficult to visualize when the needle arthroscope was inserted through the AM portal. This could be due to the difference in the visible range between the oblique and direct views of each arthroscope. Similarly, when using the needle arthroscope, it was difficult to visualize the deltoid ligament from the AL portal. In contrast to the AM and AL portals, the MM and AC portals could be used to visualize almost all intra-articular sites, except for 1 case in which the origin of the anterior tibiofibular ligament and the tip of the lateral malleolus could not be visualized. When needle arthroscopy is used as a diagnostic modality with only 1 portal created, the MM or AC portal is better for visualization than the AM or AL portal, although the procedures in the present study were performed by an expert with plenty of experience with ankle arthroscopy.
The results of the present study showed that the AC portal had a higher risk of anterior neurovascular injury in IONA. The NanoScope has both a blunt and a sharp obturator. Therefore, the distance between each portal and neurovascular tissues shown in the present study would be referred to especially when a sharp obturator is used. In previous studies, many authors have discouraged the use of the AC portal because of the high risk of anterior neurovascular injury.10,13,32 Feiwell and Frey 10 reported that the mean distance between the AC portal and the anterior neurovascular bundle was 3.3 mm, and the arthroscope was in direct contact with the neurovascular bundle in 22% of cases. Buckingham et al 2 also mentioned that the mean distance was 0.7 mm from the AC portal to the artery and the arthroscope directly touched the artery in 90% of cases. These results were comparable with those of our study, in which the mean distance was 2.2 mm and direct contact occurred in 40% of cases. In contrast, Stotter et al 30 recommended using an AC portal because of its broad visualization and low rate of neurovascular injury in the clinical setting. The present study showed that the MM portal had a longer distance from the neurovascular bundle and almost the same visibility as the AC portal. Therefore, we believe that the MM portal is a better option than the AC portal. In the present study, the portals were created without joint distraction, and the distances between the portals and neurovascular tissues were measured without joint distraction. A previous study has shown that joint distraction can change the distance between the portals and the neurovascular bundle. 8 Therefore, further studies will be needed to reveal the difference in the distances between portals and the neurovascular bundle according to the existence of joint distraction.
Limitations
The present study had several limitations. First, the study consisted of a small sample size of 10 cadaveric ankles. Second, a 21-point assessment, which includes the examination of posterior structures of the ankle joint, 27 was not used in the present study. Third, there was no bleeding since this was a cadaveric study, although intraoperative bleeding might affect the visibility in a clinical setting. Fourth, generalizability is limited since the procedures in the present study were conducted by a single surgeon with vast experience in ankle arthroscopy. Fifth, the age distribution in this cadaveric study was extremely high. In the clinical situation, IONA has been typically used for younger patients.4,9 However, IONA would be indicated for any patients, young or old, as long as their medical status allowed it to be performed in the office instead of an operating room. Sixth, only a 1.9-mm arthroscope with 0° was investigated in the present study; regardless, there are other 1.9-mm arthroscopes with a 25° lens. Additional studies should be conducted with that lens to determine whether it provides better visualization than a 0° arthroscope. Despite these limitations, the present study is valuable, as it provides information regarding which portal should be selected to perform needle arthroscopy in the ankle joint.
Conclusion
With needle arthroscopy, almost all the points in the ankle joint were visualized in both the AC and the MM portals. In contrast, visualization of the opposite sides of the ankle joint was difficult in the AM and AL portals. Care should be taken when creating an AC portal because of its proximity to the anterior neurovascular bundle.
Acknowledgment
The authors sincerely appreciate the support in performing the dissections by Takatoshi Ueki from the Department of Anatomy, Nagoya City University Graduate School of Medical Science.
Footnotes
Final revision submitted January 12, 2023; accepted February 22, 2023.
The authors declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Nagoya City University Graduate School of Medical Science (reference No. 1255).
References
- 1.Amin N, McIntyre L, Carter T, Xerogeanes J, Voigt J. Cost-effectiveness analysis of needle arthroscopy versus magnetic resonance imaging in the diagnosis and treatment of meniscal tears of the knee. Arthroscopy. 2019;35(2):554–562.e13. [DOI] [PubMed] [Google Scholar]
- 2.Buckingham RA, Winson IG, Kelly AJ. An anatomical study of a new portal for ankle arthroscopy. J Bone Joint Surg Br. 1997;79(4):650–652. [DOI] [PubMed] [Google Scholar]
- 3.Colasanti CA, Kaplan DJ, Chen JS, et al. In-office needle arthroscopy for anterior ankle impingement. Arthrosc Tech. 2022;11(3):e327–e331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Colasanti CA, Mercer NP, Garcia JV, Kerkhoffs GMMJ, Kennedy JG. In-office needle arthroscopy for the treatment of anterior ankle impingement yields high patient satisfaction with high rates of return to work and sport. Arthroscopy. 2022;38(4):1302–1311. [DOI] [PubMed] [Google Scholar]
- 5.Cunningham G, Benchouk S, Kherad O, Lädermann A. Comparison of arthroscopic and open Latarjet with a learning curve analysis. Knee Surg Sports Traumatol Arthrosc. 2016;24(2):540–545. [DOI] [PubMed] [Google Scholar]
- 6.Dalmau-Pastor M, Malagelada F, Kerkhoffs GM, Karlsson J, Guelfi M, Vega J. Redefining anterior ankle arthroscopic anatomy: medial and lateral ankle collateral ligaments are visible through dorsiflexion and non-distraction anterior ankle arthroscopy. Knee Surg Sports Traumatol Arthrosc. 2020;28(1):18–23. [DOI] [PubMed] [Google Scholar]
- 7.Dankert JF, Shimozono Y, Williamson ERC, Kennedy JG. Application of nano arthroscopy in the office setting for the removal of an intra-articular loose osseous body not identified by magnetic resonance imaging: a case report. Foot Ankle Surg Tech Rep Cases. 2021;1:100012. [Google Scholar]
- 8.De Leeuw PA, Golanó P, Clavero JA, Van Dijk CN. Anterior ankle arthroscopy, distraction or dorsiflexion? Knee Surg Sports Traumatol Arthrosc. 2010;18(5):594–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.DiBartola AC, Rogers A, Kurzweil P, Knopp MV, Flanigan DC. In-office needle arthroscopy can evaluate meniscus tear repair healing as an alternative to magnetic resonance imaging. Arthrosc Sports Med Rehabil. 2021;3(6):e1755–e1760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Feiwell LA, Frey C. Anatomic study of arthroscopic portal sites of the ankle. Foot Ankle. 1993;14(3):142–147. [DOI] [PubMed] [Google Scholar]
- 11.Gauci MO, Monin B, Rudel A, Blasco L, Bige B, Boileau P. In-office biceps tenotomy with needle arthroscopy: a feasibility study. Arthrosc Tech. 2021;10(5):e1263–e1268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gill TJ, Safran M, Mandelbaum B, Huber B, Gambardella R, Xerogeanes J. A prospective, blinded, multicenter clinical trial to compare the efficacy, accuracy, and safety of in-office diagnostic arthroscopy with magnetic resonance imaging and surgical diagnostic arthroscopy. Arthroscopy. 2018;34:2429–2435. [DOI] [PubMed] [Google Scholar]
- 13.Golanó P, Vega J, Pérez-Carro L, Götzens V.Ankle anatomy for the arthroscopist. Part I: the portals. Foot Ankle Clin. 2006;11(2):253–273. [DOI] [PubMed] [Google Scholar]
- 14.Guttmann D, Graham RD, MacLennan MJ, Lubowitz JH. Arthroscopic rotator cuff repair: the learning curve. Arthroscopy. 2005;21(4):394–400. [DOI] [PubMed] [Google Scholar]
- 15.Kaplan DJ, Chen JS, Colasanti CA, et al. Needle arthroscopy cheilectomy for hallux rigidus in the office setting. Arthrosc Tech. 2022;11(3):e385–e390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Labib SA, Slone HS. Office-based needle arthroscopy for the foot and ankle. Tech Foot Ankle Surg. 2015;14:9–11. [Google Scholar]
- 17.Lavender C, Lycans D, Sina Adil SA, Berdis G. Single-incision rotator cuff repair with a needle arthroscope. Arthrosc Tech. 2020;9(4):e419–e423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Leontaritis N, Hinojosa L, Panchbhavi VK. Arthroscopically detected intra-articular lesions associated with acute ankle fractures. J Bone Joint Surg Am. 2009;91(2):333–339. [DOI] [PubMed] [Google Scholar]
- 19.Martin KD, Patterson D, Phisitkul P, Cameron KL, Femino J, Amendola A. Ankle arthroscopy simulation improves basic skills, anatomic recognition, and proficiency during diagnostic examination of residents in training. Foot Ankle Int. 2015;36(7):827–835. [DOI] [PubMed] [Google Scholar]
- 20.Mattos E, Dinato MC, Pereira Filho MV, Pagnano RG. Endoscopy for the treatment of posterior ankle impact syndrome: learning curve. Foot Ankle Surg. 2021;27(7):755–759. [DOI] [PubMed] [Google Scholar]
- 21.McMillan S, Schwartz M, Jennings B, Faucett S, Owens T, Ford E. In-office diagnostic needle arthroscopy: understanding the potential value for the US healthcare system. Am J Orthop (Belle Mead NJ). 2017;46:252–256. [PubMed] [Google Scholar]
- 22.Meister K, Harris NL, Indelicato PA, Miller G. Comparison of an optical catheter office arthroscope with a standard rigid rod-lens arthroscope in the evaluation of the knee. Am J Sports Med. 1996;24(6):819–823. [DOI] [PubMed] [Google Scholar]
- 23.Patton GW, Zelichowski JE. Office-based ankle arthroscopy. Clin Podiatr Med Surg. 1994;11(3):513–522. [PubMed] [Google Scholar]
- 24.Quinn R, Lang SD, Gilmer BB. Diagnostic needle arthroscopy and partial medial meniscectomy using small bore needle arthroscopy. Arthrosc Tech. 2020;9(5):e645–e650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Simonson DC, Roukis TS. Safety of ankle arthroscopy for the treatment of anterolateral soft-tissue impingement. Arthroscopy. 2014;30(2):256–259. [DOI] [PubMed] [Google Scholar]
- 26.Small NC, Del Gallo WA. Office foot and ankle arthroscopy. In: Guhl JF, Parisien JS, Boynton MD, eds. Foot and Ankle Arthroscopy. Springer; 2005:257–263. [Google Scholar]
- 27.Stetson WB, Ferkel RD. Ankle arthroscopy: I. Technique and complications. J Am Acad Orthop Surg. 1996;4(1):17–23. [DOI] [PubMed] [Google Scholar]
- 28.Stornebrink T, Altink JN, Appelt D, Wijdicks CA, Stufkens SAS, Kerkhoffs GMMJ. Two-millimetre diameter operative arthroscopy of the ankle is safe and effective. Knee Surg Sports Traumatol Arthrosc. 2020;28(10):3080–3086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stornebrink T, van Dijck RAHE, Douven D, Kerkhoffs GMMJ. Needle arthroscopic all-inside repair of meniscal tears under local anesthesia. Arthrosc Tech. 2021;10(9):e2173–e2180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Stotter C, Klestil T, Chemelli A, Naderi V, Nehrer S, Reuter P. Anterocentral portal in ankle arthroscopy. Foot Ankle Int. 2020;41(9):1133–1142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Takao M, Ochi M, Shu N, et al. Bandage distraction technique for ankle arthroscopy. Foot Ankle Int. 1999;20(6):389–391. [DOI] [PubMed] [Google Scholar]
- 32.Takao M, Uchio Y, Shu N, Ochi M. Anatomic bases of ankle arthroscopy: study of superficial and deep peroneal nerves around anterolateral and anterocentral approach. Surg Radiol Anat. 1998;20(5):317–320. [DOI] [PubMed] [Google Scholar]
- 33.Van Dijk CN, Vuurberg G, Amendola A, Lee JW. Anterior ankle arthroscopy: state of the art. J ISAKOS 2016;1:105–115. [Google Scholar]
- 34.Vega J, Dalmau-Pastor M, Malagelada F, Fargues-Polo B, Peña F. Ankle arthroscopy: an update. J Bone Joint Surg Am. 2017;99(16):1395–1407. [DOI] [PubMed] [Google Scholar]
- 35.Vega J, Karlsson J, Kerkhoffs GMMJ, Dalmau-Pastor M. Ankle arthroscopy: the wave that’s coming. Knee Surg Sports Traumatol Arthrosc. 2020;28(1):5–7. [DOI] [PubMed] [Google Scholar]
- 36.Wagner ER, Woodmass JM, Zimmer ZR, et al. Needle diagnostic arthroscopy and magnetic resonance imaging of the shoulder have comparable accuracy with surgical arthroscopy: a prospective clinical trial. Arthroscopy. 2021;37:2090–2098. [DOI] [PubMed] [Google Scholar]
- 37.Yammine K, Assi C. Neurovascular and tendon injuries due to ankle arthroscopy portals: a meta-analysis of interventional cadaveric studies. Surg Radiol Anat. 2018;40(5):489–497. [DOI] [PubMed] [Google Scholar]
- 38.Zhang K, Crum RJ, Samuelsson K, Cadet E, Ayeni OR, de Sa D. In-office needle arthroscopy: a systematic review of indications and clinical utility. Arthroscopy. 2019;35(9):2709–2721. [DOI] [PubMed] [Google Scholar]