Abstract
Menopausal symptoms are known to affect quality of life and work productivity. This systematic review aimed to describe the range and effectiveness of workplace-based interventions for menopause. MEDLINE, PubMed, Embase, CINAHL, Cochrane Library, Web of Science, PsycINFO, EconLit, and SCOPUS were searched from the inception until April 2022. Quantitative interventional studies evaluating physical/virtual workplace-based interventions aiming to improve well-being, work, and other outcomes, that involved women in menopausal transition, or their line managers/supervisors were eligible for inclusion. Two randomized controlled trials and three uncontrolled trials, comprising 293 women aged 40–60 years and 61, line managers/supervisors, were included in the review. Results were narratively synthesized due to the heterogeneity of interventions and outcomes and we found that only a limited range of interventions have been evaluated for their ability to support women going through menopausal transition in the workplace. Self-help cognitive behavioural therapy (CBT); Raja yoga; and health promotion (involving menopause consultations, work–life coaching and physical training) improved menopausal symptoms significantly. Self-help CBT was associated with a significant improvement in mental resources for work, presenteeism, and work and social adjustment. Awareness programs significantly improved knowledge and attitudes of both employees and line managers/supervisors about menopause. The interventions have mostly been evaluated in small studies with selected populations but have improved menopausal symptoms and work outcomes. A customizable menopause wellbeing intervention package incorporating these evidence-supported interventions should be developed and implemented on a wider scale within organizations alongside robust evaluation of its effectiveness.
Keywords: Climacteric, occupational health, midlife, employee health and wellbeing
Introduction
Menopausal transition is a physiologically and psychosocially challenging period in a woman’s life. Occurring between the ages 45-55 years, transition from reproductive phase to menopause could take 4–8 years and is characterised by irregular or prolonged menstrual cycles and menopausal symptoms. Menopausal symptoms are vasomotor (hot flushes, night sweats), somatic (fatigue, insomnia, body aches, joint pains), psychosocial (poor concentration, forgetfulness, low mood, anxiety, and low confidence), sexual (decreased libido and sexual responsiveness), and urogenital (vaginal dryness and atrophy). They could last up to 5 years into menopause or may even worsen and persist into the latter stages of life.1–3
Menopausal symptoms interfere with day-to-day activities of women including employment.4–6 Poor concentration, tiredness, and poor memory have been reported in around 50% of women aged 45–55 in professional, managerial, and administrative roles. 4 Sleep problems during menopause have been associated with approximately half an hour reduction in work time per week and an annual loss of $2.2 billion of productivity per year. 7 A study on self-perceived ability to perform in the job currently and for the next 2 years, reported that almost one third of female workers in the health sector were concerned about reduced work ability during menopause. 8 Half of employed women at 50 years of age are more likely to retire or work fewer hours per week due to distressing menopausal symptoms. 9
Increased life expectancy has increased the age of retirement of women with the majority remaining in employment during and after menopausal transition. Most women expect their employers to know, communicate and be helpful during menopausal transition and to have workplace policies concerned with their overall wellbeing. They report difficulties working in poorly ventilated workplaces and that provision of cool water and rest facilities will improve their quality of work life.10,11 A review of guidance on menopause at workplaces reports that the available guidelines broadly focus on legislation, policies, information and training, workplace support, and the physical work environment. 12 The European Menopause and Andropause Society (EMAS) recommends health and wellbeing during menopause to be given a higher level of attention at the workplace by creating awareness, alleviating stigma, allowing flexible work schedules, dress codes, and controlling the physical environment. 13
Interventions to enhance the wellbeing of menopausal women include lifestyle modification, complementary and alternative medicines, and hormone replacement therapy. 14 There is a growing interest in potential workplace-based interventions to improve wellbeing and employment outcomes among menopausal women.15–17 These interventions could support women through physical and psychosocial stressors at workplaces and thereby improve the quality of work life. 11 The objective of this systematic review was to describe the range and effectiveness of workplace-based interventions in supporting women during the menopausal transition and to make recommendations for future interventions.
Methods
This review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses: PISMA 2020 statement. 18 The protocol is registered with the International Prospective Register of Systematic Reviews (PROSPERO) under the registration ID CRD42022308412.
Search strategy
Bibliographic databases MEDLINE (via Ovid), PubMed, Embase, CINAHL, Cochrane Library, Web of Science, PsycINFO, EconLit and SCOPUS were searched from inception date until April 2022, without any language restrictions. The search strategy was developed with input from a librarian using the keywords: (menopaus* OR menopausal transition OR climacteric OR middle-aged women OR perimenopaus* OR post-menopaus*) AND (work* OR workforce OR employ* OR workplace* OR occupation*) AND (adapt OR support* OR promote* OR prevent* OR intervention* OR program* OR experiment OR trial). The reference lists of selected papers were searched for any relevant studies.
Inclusion exclusion criteria
Quantitative randomized control trials (RCT), non-RCT, or uncontrolled trials evaluating any workplace-based interventions for women in menopausal transition, or their employers/mangers were eligible. The studies were included if the interventions aimed to improve physical and/or mental wellbeing, work outcomes, or awareness and attitudes among participants. Both physically and virtually conducted interventions were included. Community and clinic-based interventions and pharmacologic interventions such as HRT were excluded.
Outcomes
Primary outcomes related to physical and mental wellbeing, including menopausal symptoms and quality of life. Secondary outcomes related to the job e. g work ability, social support at work, presenteeism/absenteeism, and work stress. A third set of outcomes related to workplace culture such as awareness, attitudes, and behaviours towards menopause at work.
Selection of studies
Titles, abstracts, and full texts were screened for eligibility by two reviewers (CHR and ES) and any disagreements were resolved through discussion with another reviewer (SB). Articles were screened using Rayyan software.
Data extraction
Data were extracted using a data extraction form by two reviewers (CHR and ES) separately and compared for consistency. The extracted data included details on the setting, study population, inclusion/exclusion criteria, number of participants in intervention and control groups, outcomes, and number with each outcome. If a study had more than one publication, the publication with the larger sample or the publication including quantitative data was included. Study authors were contacted if further data was required.
Study quality
As both randomised and non-randomised studies were included, the Downs and Black checklist 19 was used to assess reporting, risk of bias, confounding, external validity, and the power of included studies. Study quality was assessed by two reviewers (CHR and ES) independently and any disagreements were settled by discussion with the third reviewer (SB). To make the scoring of the tool easier, the power sub-scale in the original checklist was interpreted as “reported” or “not” and this score was added to the “reporting” sub-scale. 20
Data synthesis
Due to the heterogeneity of included interventions and outcomes measured between studies, a meta-analysis was inappropriate, and data were narratively synthesized. Studies were grouped by study design and type of outcome measure.
Results
Selection of studies
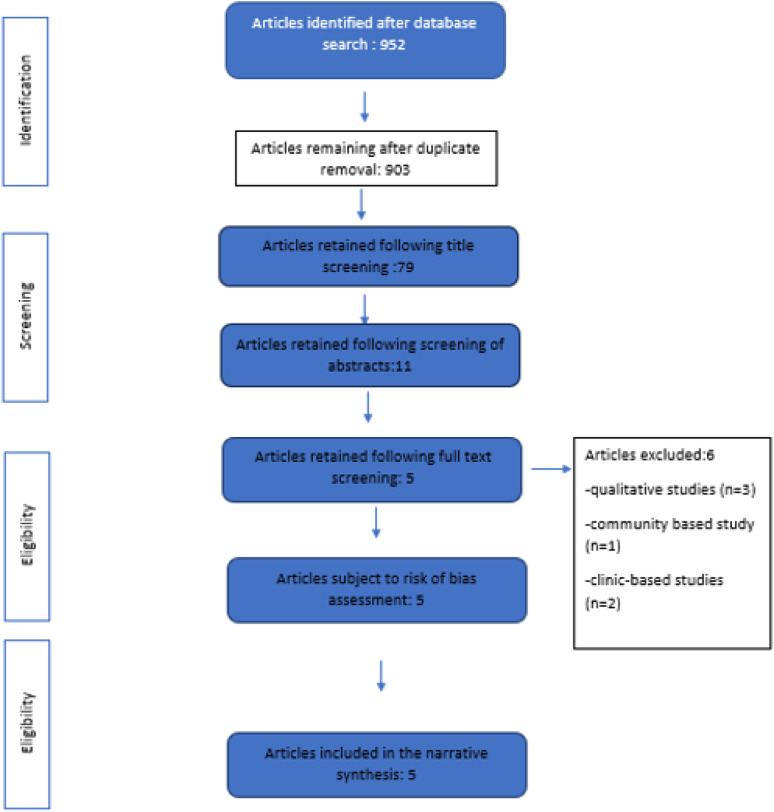
The primary search provided 952 results. Following removal of duplicates and irrelevant titles, 79 articles were retained for abstract screening. Out of them 11 articles were selected for full-text screening. The full text screening excluded six studies because they did not meet the inclusion criteria: three qualitative studies,21–23 a secondary analysis of a larger community-based study, 24 and two clinic-based studies.25,26 The remaining five articles were included in the narrative synthesis. Figure 1 illustrates the study selection process.
Figure 1.
Study selection process and results.
Study characteristics and quality
This review included two RCTs and three uncontrolled intervention studies. The total number of participants included in the review was 354; 293 women in menopausal transition aged between 40 and 60 years and 61 managers/supervisors. All the studies were conducted after 2018. Table 1 describes the characteristics of studies included.
Table 1.
Summary characteristics of the studies (n = 5).
| Author, year | Setting | Population | Intervention | Control |
|---|---|---|---|---|
| Randomised controlled trials | ||||
| 1. Portella et al., 2021 27 | Three centres of the National Institute of Social Security in the city of Sao Paulo, Brazil | Volunteer women clerical workers older than 40 years of age, in the menopausal transition having menopausal symptoms or insomnia | Raja yoga meditation 45 min/day + sleep hygiene guidelines Duration: 8 weeks Allocated/analysed: 24/18 mean age ± SD: (46.7 ± 4.3) |
Sleep hygiene guidelines Allocated/analysed: 23/15 mean age ± SD: (48.6 ± 5.4) |
| 2. Hardy et al., 2018 15 | Eight organizations, from public and private sectors, United Kingdom | Employed postmenopausal women aged 45–60 years having 10 or more problematic hot flushes/night sweats (HFNS) in a week | Self-help cognitive behaviour therapy booklet Duration: 20 weeks allocated/analysed: 60/46 mean age ± SD: (54.0 ± 3.1) |
No treatment Allocated/analysed: 64/60 mean age ± SD (54.1 ± 3.53) |
| Uncontrolled trials | ||||
| 3. Hardy, Griffiths & Hunter 2019 16 | Three large organisations (1 public and 2 private sector) from the UK | Line managers and supervisors (both male and female) | web-based training Duration: 30 min allocated/analysed: 62/61 |
- |
| 4. Gebretatyos et al., 2020 28 | A school in Asmara, Eritrea | Female teachers who were aged from 40 to 60 | Health education session Duration: 3 h allocated/analysed: 99/98 mean age ± SD: 48.97 ± 5.47 |
- |
| 5. Verburgh et al., 2020 29 | Amsterdam Medical Center Netherlands | Female workers aged between 45 and 60 years, working in low-paid jobs | Work life program Duration: Eight sessions of 1 h over 2–4 months allocated/analysed: 70/56 mean age ± SD: (52.6 ± 4.5) |
- |
Table 2 illustrates the quality of the studies assessed according to Downs and Black checklist. 20 The scores ranged from 13–20 out of 27 (mean 15.2) indicating moderate overall quality. Risks of bias was due to poor generalisability because of uncertainty in representativeness of volunteer participants,15,16,27–29 lack of adjustment for confounding factors,16,28,29 lack of blinding or allocation concealment.15,27 Work and social commitments were mentioned by participants as reasons for drop out or discontinuing the interventions.
Table 2.
Summary of the quality of studies using Downs and Black tool a (n = 5).
| Reference | Reporting (maximum 11) | External validity (maximum 3) | Internal validity, bias (maximum 7) | Internal validity, confounding (maximum 6) | Total (maximum 27) |
|---|---|---|---|---|---|
| Portella et al., 2021 27 | 9 | 1 | 2 | 4 | 16 |
| Hardy et al., 2018 15 | 10 | 1 | 4 | 5 | 20 |
| Hardy, Griffiths & Hunter 2019 16 | 8 | 1 | 4 | 0 | 13 |
| Gebretatyos et al., 2020 28 | 7 | 0 | 4 | 2 | 13 |
| Verburgh et al., 2020 29 | 7 | 1 | 4 | 2 | 14 |
aTwenty-seven criteria are used to assess risk of bias. Each criterion is scored as Yes (1), No (0) or unable to determine (0). An overall score is calculated by summation, as well as four sub-scales representing “reporting” (total of 11; includes power criterion), “external validity” (total of 3), “internal validity, bias” (total of 7), and “Internal validity, confounding” (total of 6). Higher scores represent lower risk of bias.19,20
Interventions
Randomized Controlled Trials
Raja yoga meditation by Portella et al., focused on breathing and relaxation. After the introductory session participants were instructed to do the intervention for 45 min daily for 8 weeks at home and were followed up. The drop out rate was 16.6% (n = 4) from intervention and 21.7% (n = 5) in control group. 27 Self-help CBT by Hardy et al., was delivered via a mailed booklet which has been adapted from a previous community-based trial. 30 It included information and exercises about menopause, stress management, and cognitive and behavioural strategies, and was expected to be completed within 20 weeks. Completion rate was 65% (n = 28) at 20 weeks with self-reported use of breathing technique by 79% (n = 33) at least >1 time per week. 15 The booklet was rated as helpful by 88.1% (n = 35) to cope with problems faced at work and life in general by 63%.
Uncontrolled trials
Hardy et al. had recruited line managers/supervisors from three UK organizations for a short online training on menopause which contained videos, role plays, and real-life testimonials on menopause. Participation rate was 22.9% (62 out of 270 invited) and were followed up for 4 weeks. More than 90% found the intervention helpful. 16 In the intervention by Gebretatyos et al., a group of middle-aged school teachers (n = 99) were provided a group discussion-based training on menopause, physical activity, and nutrition by a midwife. The participation rate was 90% (n = 99). 28 The intervention implemented by Verburgh et al., was an adaptation of a pre-existing Work Life Program (WLP)21,29 and had multiple components: menopause consultations, work–life coaching sessions and physical training sessions. Participants consisted of food service assistants, service desk employees, and cleaners at a teaching hospital. Out of the recruited 80% participated until the end of intervention.
Outcomes
Randomized Controlled Trials
Menopausal symptoms
Self-help CBT significantly improved hot flushes and night sweats (p = 0.01), somatic symptoms (p = 0.01), and sleep problems (p = 0.001). 15 Raja Yoga significantly improved menopausal symptoms (p = 0.026) but did not to show a significant impact on insomnia and sleep quality. 27
Work outcomes
Self-help CBT intervention assessed work outcomes and reported significantly improved presenteeism (p = 0.001) (defined as “perceptions of being physically present at their jobs but experiencing decreased productivity and below-normal work quality due to their menopause”) and work and social functioning (p = 0.01) 14 at home, work, and other social situations.
Other outcomes
There was a significant improvement (p = 0.05) in well-being following self-help CBT. 14 The women reported having better awareness, taking better personal care, and improved confidence to talk about menopause following the intervention. Over one third (37%) had talked to their line manager about any menopause related problems by the time program was evaluated.
Uncontrolled trials
WLP 29 significantly reduced menopausal symptoms but did not change work outcomes significantly. The counselling strategy used in the WLP was reported as helpful by women to share their experiences, and to make new life choices. 21 The web-based training by Hady et al., significantly improved the knowledge (p = 0.000), attitudes (p = 0.004), confidence (p = 0.000), and intentions to talking about the menopause at work (p = 0.000). At 4 weeks 49.1% had spoken with someone at work about menopause (pre intervention 47.4%, p > 0.05, n = 57). 15 The health education intervention by Gebretatyos et al., significantly improved the knowledge (p < 0.0001) and attitudes (p = 0.0001) among participants. Table 3 compares the outcomes of all included studies.
Table 3.
Summary of intervention outcomes (n = 5).
| First Author, year | Outcomes | Follow-up (weeks) | Results | p(sig.) group*time | |||||
|---|---|---|---|---|---|---|---|---|---|
| Intervention group | Control group | ||||||||
| Pre | Post* | p(sig.) | Pre | Post* | p(sig.) | ||||
| Randomized controlled trials | |||||||||
| Portella et , 27 2021 | Menopausal symptoms severity 1 | 8 | 23.33 ± 9.11 | 20.06 ± 7.58 | 0.024 | 20.47 ± 10.66 | 19.07 ± 9.06 | 0.363 | 0.026 |
| Insomnia severity 2 | 8 | 13.72 ± 5.92 | 9.72 ± 4.67 | 0.001 | 14.67 ± 5.17 | 12.00 ± 5.23 | 0.005 | 0.278 | |
| Sleep quality 3 | 8 | 8.94 ± 2.99 | 7.67 ± 3.12 | 0.164 | 10.20 ± 2.88 | 8.07 ± 2.73 | 0.016 | 0.492 | |
| Hardy et al., 2018 15 | Severity – hot flushes, night sweats 4 | 20 | 6.25 ± 1.97 | 4.36 ± 2.29 | 6.80 ± 1.90 | 5.8 ± 2.3 | 0.01 | ||
| Frequency – hot flushes, night sweats 5 | 20 | 53.13 ± 34.34 | 34.28 ± 27.62 | 54.28 ± 38.11 | 46.03 ± 37.92 | 0.05 | |||
| Hot flushes, night sweats – behaviour 18 | 20 | 3.34 ± 1.01 | 3.67 ± 0.86 | 3.13 ± 1.19 | 3.13 ± 1.17 | 0.05 | |||
| Hot flush social beliefs 19 | 20 | 2.35 ± 1.67 | 1.55 ± 1.27 | 2.30 ± 1.37 | 2.14 ± 1.39 | 0.001 | |||
| Hot flush coping/control beliefs 19 | 20 | 2.26 ± 1.22 | 1.77 ± 1.23 | 2.45 ± 1.06 | 2.29 ± 1.20 | 0.01 | |||
| Night sweats/sleep beliefs 19 | 20 | 2.08 ± 1.09 | 1.26 ± 0.90 | 2.42 ± 1.33 | 2.08 ± 1.31 | 0.001 | |||
| Sleep problems 6 | 20 | 34.09 ± 25.66 | 48.41 ± 21.72 | 37.78 ± 26.01 | 40.77 ± 30.47 | 0.001 | |||
| Somatic symptoms 6 | 20 | 50.37 ± 23.93 | 58.41 ± 22.47 | 47.67 ± 21.43 | 49.94 ± 20.04 | 0.01 | |||
| well-being 6 | 20 | 71.11 ± 75.79 | 75.79 ± 16.44 | 67.92 ± 19.58 | 67.54 ± 17.3 | 0.01 | |||
| Presenteeism at work 7 | 20 | 20.24 ± 6.34 | 23.21 ± 5.84 | 18.67 ± 6.40 | 18.18 ± 7.18 | 0.001 | |||
| Negative impact 8 | 20 | 2.17 ± 0.73 | 2.09 ± 0.84 | 2.27 ± 2.38 | 2.38 ± 0.69 | 0.05 | |||
| relief 8 | 20 | 2.52 ± 0.82 | 2.70 ± 0.84 | 2.37 ± 0.96 | 2.37 ± 1.00 | 0.024 | |||
| new phase 8 | 20 | 1.72 ± 0.92 | 2.22 ± 0.74 | 1.73 ± 0.87 | 1.89 ± 0.76 | 0.01 | |||
| Control/cure 8 | 20 | 2.11 ± 0.63 | 2.88 ± 0.65 | 1.89 ± 0.76 | 2.10 ± 0.80 | 0.001 | |||
| Work and social adjustment 9 | 20 | 12.74 ± 9.77 | 8.65 ± 8.65 | 12.67 ± 8.44 | 11.81 ± 8.39 | 0.01 | |||
| Sleep quality 3 | 20 | 1.82 ± 0.81 | 1.40 ± 0.77 | 1.85 ± 0.82 | 1.66 ± 0.78 | 0.05 | |||
| Prospective pre-post design | |||||||||
| Hardy, Griffiths and Hunter, 2019 15 | Knowledge on menopause | 4 | 3.32 ± 1.62 | 4.74 ± 1.15 | 0.000 | ||||
| Attitudes | 4 | 3.86 ± 1.82 | 4.56 ± 1.77 | 0.004 | |||||
| Normative belief | 4 | 4.43 ± 0.21 | 4.82 ± 1.52 | 0.061 | |||||
| Confidence | 4 | 3.77 ± 0.24 | 5.10 ± 1.31 | 0.000 | |||||
| Menopause awareness | 4 | 3.84 ± 1.17 | 4.80 ± 1.04 | 0.000 | |||||
| Behavioural intention | 4 | 2.92 ± 0.29 | 3.95 ± 1.98 | 0.000 | |||||
| Gebretatyos et al.,2020 28 | Knowledge on menopause | 12 | 12.3 ± 3.06 | 16.5 ± 2.52 | 0.000 | ||||
| Attitude toward menopause | 12 | 27.9 ± 5.14) | 28.3 ± 5.12) | 0.000 | |||||
| Verburgh et al., 2020 29 | Menopausal symptoms 15 | 16 | 18.0 (12.0) | 13.0 (11.0) | 0.000 | ||||
| Work functioning 14 | 16 | 21.1 (20.0) | 18.6 (16.0) | 0.791 | |||||
| Quality of life; mental 16 | 16 | 48.2 ± 10.37 | 48.7 ± 9.4 | 0.908 | |||||
| Quality of life; physical 16 | 16 | 50.0 (10.0) | 48.8 (15.0) | 0.250 | |||||
| Work ability 17 | 16 | 7.0 (1.0) | 8.0 (1.0) | 0.072 | |||||
Measured by; 1Kupperman menopausal index, 31 2Insomnia severity index, 32 3Pittsburgh sleep questionnaire, 33 4HFNS Rating Scale, 34 19hot flush beliefs scale, 35 18Hot Flush Behaviour Scale, 36 6Women’s Health Questionnaire, 37 Insomnia severity index, 32 7Stanford Presenteeism Scale, 38 8Menopause Representations Questionnaire, 39 9work and social adjustment scale, 40 13Need for recovery after work scale, 41 14Work functioning questionnaire, 42 15Greene Climacteric scale, 43 16Short Form 12, 44 17Work ability Index, 45 * measured at end of follow up period.
Discussion
Principal findings
To the authors’ knowledge, this is the first systematic review exploring the effectiveness of workplace-based interventions for menopause. The interventions for menopause implemented at workplaces were limited in number, heterogenous, and included self-help CBT, Raja yoga, health promotion (including menopause consultations, work–life coaching, and physical training) and awareness programs.15,16,27–29 Menopausal symptoms significantly improved following Raja yoga 27 self-help CBT 15 and health promotion sessions. 29 In addition, self-help CBT reported a significant improvement in presenteeism and work and social adjustment. Awareness programs significantly improved knowledge and attitudes regarding menopause.16,28
Interpretation of results
This review supports self-help CBT as an intervention that can be employed at work settings to alleviate menopausal symptoms and to improve work outcomes. CBT helps to change negative cognitions linked with menopausal symptoms such as fear or embarrassment due to hot flushes. 30 CBT has been reported to reduce the work time impaired by insomnia 25 and is also recommended in NICE guidelines for menopause. Self-help CBT was identified as the only intervention leading to favourable work outcomes during this review.
This review observed the effectiveness of Raja yoga for alleviating menopausal symptoms among working women. Previous mind body therapy interventions of yoga and other breathing based exercises in the community have reported similar improvements in menopausal symptoms and sleep. 46 The WLP promoted a healthier lifestyle through guidance on nutrition, physical activity, and menopausal counselling. Proper nutrition and physical activity are essential for combating increased cardio-metabolic and osteoporosis risk among menopausal women and should be part of any wellbeing strategy for menopause. Menopausal counselling further enabled them to make healthy life choices. 29 The reviewed health education interventions16,28 were short and feasible. They effectively improved knowledge and attitudes relating to menopause highlighting a vacuum of awareness among participants. More robust awareness programs might elicit a significant change in communications on menopause at workplaces. 16
Strengths and limitations of this review
This review does not include a meta-analysis due to the wide heterogeneity observed among included studies. We observed that the study designs, type of workplaces, categories of staff, intervention types, duration, and outcome measures were unique and different for each study. Hence, we attempted to categorise studies by hierarchy of evidence and broad outcome groups during the narrative synthesis. In addition, the strength of evidence generated by this review is limited by the fact that we came across only a few interventions and they were different from each other. More RCT from each intervention type would have enabled to us to present more robust review findings. There is literature suggestive of interventions that are effective in the community setting for menopausal symptoms and functioning of menopausal women. Since the ‘workplace and menopause’ is a topic of current interest it is likely newer interventions will be carried out at workplaces in the future. Given the paucity of published interventions on the topic, we have collated and presented the currently available evidence.
Limitations in the literature and directions for future research
Our review included studies of moderate quality and their interpretations are subject to methodological limitations. Deficiencies noted in the methods were; unadjusted confounding in the uncontrolled studies, lack of blinding, allocation concealment and possible contamination in the RCTs. Outcomes measured using self-administered instruments could be subjective while volunteer participants are likely to be more health-conscious or be more affected by menopausal symptoms. Sample size calculations were also not outlined in most studies while some studies reported poor compliance due to work and other commitments. Further, the interventions were of short durations with the maximum being 5 months. Most studies had presented outcome data at the end of the intervention period and long-term follow-up data were lacking. Only the awareness programs had followed up participants following the intervention. Long term benefits are difficult to be ascertained with interventions limited to a few months and work-related outcomes could take a longer time to show an improvement. Longer duration higher quality RCT might provide stronger evidence as some studies have reported non-significant improvements in work outcomes.21,24,29,32 However, the interventions did not have any in-built mechanisms to ensure long term sustainability which would be necessary to obtain long term benefits in a dynamic workplace setting where there is likely to be a high turnover of employees.
Implications for policy and practice
The EMAS guidelines recommends for employers and organizations to make health and wellbeing during menopause a priority in the workplace with the support of line managers, healthcare workers and employees. 13 Interventions for menopause should be culturally and economically sensitive to ensure sufficient recruitment and compliance. Most women still feel that menopause is a taboo topic at work 22 and this is worsened by racial disparities and male dominance in managerial roles. Employers should consider initiating awareness on menopause at a wider scale as awareness alleviates the stigma and enables discussion and decision-making. Awareness is also likely to improve compliance for further interventions such as CBT and mind body therapy. Menopausal transition should be used as a window of opportunity to promote a healthier lifestyle at the workplace and thereby prevent undesirable health and work outcomes in future. Despite recommendations within existing guidance, this review did not identify any studies concerned with alterations to the physical environments of the workplaces.
The experience of menopause is unique to each woman and different modes of support are likely to be appreciated by different women and their employers. Given the heterogeneity of interventions observed during our review and their varying degrees of effectiveness in improving different outcomes among menopausal women we recommend development and implementation of a customisable multi-component package of interventions at workplaces for menopause incorporating the reviewed evidence. This menopausal wellbeing-oriented intervention package requires to be flexible and culture sensitive. Women, practitioners, and employers should be provided the necessary knowledge and empowered to choose interventions that are most appropriate for them depending on symptom presence or absence, type of employment and workplace requirements. Such a package should ideally include screening for unhealthy lifestyle and non-communicable disease since both are known to worsen the negative impacts of menopausal symptoms.
Conclusions
Self-help CBT, Raja yoga, and support to adopt healthy lifestyles are interventions that were significantly effective in reducing menopausal symptoms and should be considered for inclusion in work-based programmes to support women who are going through the menopause. There is still a vast knowledge and attitude gap to be filled among both menopausal women and their employers regarding menopause and this could be addressed using short duration health education sessions aiming to induce a behaviour change towards menopause at work. Sustainable interventions of longer duration are likely to be of more benefit and should be tested in the future. Overall, CBT, Raja yoga, support to adopt healthy lifestyles, and menopause awareness interventions reviewed in this study were found to improve various aspects of wellbeing among menopausal women and could be used in combination in future and customized to individual women’s or organizations’ needs as appropriate.
Acknowledgements
We would like to acknowledge the support extended by the Aberdeen Center for Women’s Health Research and Department of Public Health of the University of Aberdeen.
Footnotes
Contributorship: Paper conception and design was done by CHR, and SB. Literature search was done by CHR and review, and data extraction were done by CHR and ES. Manuscript and table preparation was done by CHR. Critical review/revision was done by SB, SP and MB.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD
Chithramali Hasanthika Rodrigo https://orcid.org/0000-0002-0524-494X
References
- 1.Sarri G, Davies M, Lumsden MA. Diagnosis and management of menopause: summary of NICE guidance. Bmj 2015; 351: 351. [DOI] [PubMed] [Google Scholar]
- 2.Lumsden MA, Davies M, Sarri G. Diagnosis and management of menopause: the National Institute of Health and Care Excellence (NICE) guideline. JAMA Intern Med 2016; 176(8): 1205–1206. [DOI] [PubMed] [Google Scholar]
- 3.Harlow SD, Gass M, Hall JE, et al. Executive summary of the Stages of Reproductive Aging Workshop+ 10: addressing the unfinished agenda of staging reproductive aging. J Clin Endocrinol Metab 2012; 97(4): 1159–1168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Griffiths A, MacLennan SJ, Hassard J. Menopause and work: An electronic survey of employees’ attitudes in the UK. Maturitas, Maturitas [Internet]. 2013;76(2):155–159. Available from:https://www.sciencedirect.com/science/article/pii/S0378512213002235 [DOI] [PubMed] [Google Scholar]
- 5.Converso D, Viotti S, Sottimano I, et al. The relationship between menopausal symptoms and burnout. A cross-sectional study among nurses. BMC Womens Health 2019; 19(1): 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bariola E, Jack G, Pitts M, et al. Employment conditions and work-related stressors are associated with menopausal symptom reporting among perimenopausal and postmenopausal women. Menopause 2017; 24(3): 247–251. [DOI] [PubMed] [Google Scholar]
- 7.Kagan R, Shiozawa A, Epstein AJ, et al. Impact of sleep disturbances on employment and work productivity among midlife women in the US SWAN database: a brief report. Menopause 2021; 28(10): 1176–1180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pinas I, Botterweg A, Franke H. Exploring workability and conditions to improve work participation among female healthcare workers aged 45-60 years. In: Menopause-The Journal Of The North American Menopause Society; 2019. p. 1457. [Google Scholar]
- 9.Evandrou M, Falkingham J, Qin M, et al. Menopausal transition and change in employment: Evidence from the National Child Development Study. Maturitas 2021; 143: 96–104. [DOI] [PubMed] [Google Scholar]
- 10.Hardy C, Griffiths A, Hunter MS. What do working menopausal women want? A qualitative investigation into women’s perspectives on employer and line manager support. Maturitas 2017;101:37–41. Available from:https://www.sciencedirect.com/science/article/pii/S0378512217304796 [DOI] [PubMed] [Google Scholar]
- 11.Jack G, Riach K, Bariola E, et al. Menopause in the workplace: What employers should be doing. Maturitas 2016; 85: 88–95. [DOI] [PubMed] [Google Scholar]
- 12.Hardy C, Hunter MS, Griffiths A. Menopause and work: an overview of UK guidance. Occup Med (Chic Ill) 2018; 68(9): 580–586. [DOI] [PubMed] [Google Scholar]
- 13.Rees M, Bitzer J, Cano A, et al. Global consensus recommendations on menopause in the workplace: A European Menopause and Andropause Society (EMAS) position statement. 2021:55–62. Available from:https://www.sciencedirect.com/science/article/pii/S0378512221001079 [DOI] [PubMed] [Google Scholar]
- 14.Johnson A, Roberts L, Elkins G. Complementary and alternative medicine for menopause. J Evid Based Integr Med 2019; 24: 2515690X19829380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hardy C, Griffiths A, Norton S, et al. Self-help cognitive behavior therapy for working women with problematic hot flushes and night sweats (MENOS@ Work): a multicenter randomized controlled trial. Menopause 2018; 25(5): 508–519. [DOI] [PubMed] [Google Scholar]
- 16.Hardy C, Griffiths A, Hunter MS. Development and evaluation of online menopause awareness training for line managers in UK organizations. Maturitas 2019; 120: 83–89. [DOI] [PubMed] [Google Scholar]
- 17.Hardy C, Thorne E, Griffiths A, et al. Work outcomes in midlife women: the impact of menopause, work stress and working environment. Womens Midlife Health 2018; 4(1): 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev 2021; 10(1): 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health 1998;52(6):377–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Harris RC, Khan MS, Martin LJ, et al. The effect of surgery on the outcome of treatment for multidrug-resistant tuberculosis: a systematic review and meta-analysis. BMC Infect Dis 2016; 16(1): 1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Verburgh M, Verdonk P, Appelman Y, et al. Workplace health promotion among ethnically diverse women in midlife with a low socioeconomic position. Health Education and Behavior, 2022. 10901981211071030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Targett R, Beck V. Menopause as a well-being strategy: Organizational effectiveness, gendered ageism and racism. Post Reprod Health 2022; 28(1): 23–27. [DOI] [PubMed] [Google Scholar]
- 23.Ariyoshi H. Evaluation of Menopausal Interventions at a Japanese Company. AAOHN Journal 2009; 57(3): 106–111. Available from: DOI: 10.1177/216507990905700305 10.1177/216507990905700305. [DOI] [PubMed] [Google Scholar]
- 24.Rutanen R, Luoto R, Raitanen J, et al. Short- and long-term effects of a physical exercise intervention on work ability and work strain in symptomatic menopausal women. Saf Health Work 2014; 5(4): 186–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kalmbach DA, Cheng P, Arnedt JT, et al. Improving daytime functioning, work performance, and quality of life in postmenopausal women with insomnia: comparing cognitive behavioral therapy for insomnia, sleep restriction therapy, and sleep hygiene education. Journal of Clinical Sleep Medicine 2019; 15(7): 999–1010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Conti DM, Agnelli GM, Chiroque Cruz KJ, et al. Work‐related stress, mood and eating disorders during the menopausal transition. Progr Nutr [Internet, 2020. [Google Scholar]
- 27.Portella CFS, Sorpreso ICE, de Assis A, et al. Meditation as an approach to lessen menopausal symptoms and insomnia in working women undergoing the menopausal transition period: A randomized controlled trial. Adv Integr Med 2021; 8(4): 278–284. [Google Scholar]
- 28.Gebretatyos H, Ghirmai L, Amanuel S, et al. Effect of health education on knowledge and attitude of menopause among middle-age teachers. BMC Womens Health 2020; 20(1): 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Verburgh M, Verdonk P, Appelman Y, et al. “I Get That Spirit in Me”—Mentally Empowering Workplace Health Promotion for Female Workers in Low-Paid Jobs During Menopause and Midlife. Int J Environ Res Public Health 2020; 17(18): 6462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ayers B, Smith M, Hellier J, et al. Effectiveness of group and self-help cognitive behavior therapy in reducing problematic menopausal hot flushes and night sweats (MENOS 2): a randomized controlled trial. Menopause 2012;19, 749, 759(7). Available from:https://journals.lww.com/menopausejournal/Fulltext/2012/07000/Effectiveness_of_group_and_self_help_cognitive.8.aspx [DOI] [PubMed] [Google Scholar]
- 31.Kupperman HS, Blatt MH, Wiesbader H, et al. Comparative clinical evaluation of estrogenic preparations by the menopausal and amenorrheal indices. J Clin Endocrinol Metab 1953; 13: 688–703. [Internet]https://academic.oup.com/jcem/article/13/6/688/2718591 [DOI] [PubMed] [Google Scholar]
- 32.Bastien CH, Vallières A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med 2001; 2(4): 297–307. [DOI] [PubMed] [Google Scholar]
- 33.Backhaus J, Junghanns K, Broocks A, et al. Test–retest reliability and validity of the Pittsburgh Sleep Quality Index in primary insomnia. J Psychosom Res [Internet] 2002; 53(3): 737–740. Available from:https://www.sciencedirect.com/science/article/pii/S0022399902003306 [DOI] [PubMed] [Google Scholar]
- 34.Hunter MS, Gentry‐Maharaj A, Ryan A, et al. Prevalence, frequency and problem rating of hot flushes persist in older postmenopausal women: impact of age, body mass index, hysterectomy, hormone therapy use, lifestyle and mood in a cross‐sectional cohort study of 10 418 British women aged 54–65. BJOG 2012; 119(1): 40–50. [DOI] [PubMed] [Google Scholar]
- 35.Smith MJ, Mann E, Mirza A, et al. Men and women’s perceptions of hot flushes within social situations: are menopausal women’s negative beliefs valid? Maturitas 2011; 69(1): 57–62. [DOI] [PubMed] [Google Scholar]
- 36.Hunter MS, Ayers B, Smith M. The Hot Flush Behavior Scale: a measure of behavioral reactions to menopausal hot flushes and night sweats. Menopause 2011; 18(11): 1178–1183. [DOI] [PubMed] [Google Scholar]
- 37.Girod I, de La Loge C, Keininger D, et al. Development of a revised version of the Women’s Health Questionnaire. Climacteric 2006; 9(1): 4–12. [DOI] [PubMed] [Google Scholar]
- 38.Koopman C, Pelletier KR, Murray JF, et al. Stanford Presenteeism Scale: Health Status and Employee Productivity. J Occup Environ Med [Internet]. 2002;44(1):14–20. Available from:http://www.jstor.org/stable/44995848 [DOI] [PubMed] [Google Scholar]
- 39.Hunter M, O’Dea I. Cognitive appraisal of the menopause: the menopause representations questionnaire (MRQ). Psychol Health Med 2001; 6(1): 65–76. [Google Scholar]
- 40.Mundt JC, Marks IM, Shear MK, et al. The Work and Social Adjustment Scale: a simple measure of impairment in functioning. The British Journal of Psychiatry 2002; 180(5): 461–464. [DOI] [PubMed] [Google Scholar]
- 41.van Veldhoven M, Broersen S. Measurement quality and validity of the “need for recovery scale”. Occup Environ Med 2003; 60(suppl 1): 3i–9i. i3–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Boezeman EJ, Nieuwenhuijsen K, de Bekker-Grob EW, et al. The Relative Importance of the Domains of Work Functioning. J Occup Environ Med 2015; 57(4): 361–366. [DOI] [PubMed] [Google Scholar]
- 43.Greene JG. Constructing a standard climacteric scale. Maturitas 2008; 61(1–2): 78–84. [DOI] [PubMed] [Google Scholar]
- 44.Mols F, Pelle AJ, Kupper N. Normative data of the SF-12 health survey with validation using postmyocardial infarction patients in the Dutch population. Quality of Life Research 2009; 18(4): 403–414. [DOI] [PubMed] [Google Scholar]
- 45.el Fassi M, Bocquet V, Majery N, et al. Work ability assessment in a worker population: comparison and determinants of Work Ability Index and Work Ability score. BMC Public Health 2013; 13(1): 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Innes KE, Selfe TK, Vishnu A. Mind-body therapies for menopausal symptoms: a systematic review. Maturitas 2010; 66(2): 135–149. [DOI] [PMC free article] [PubMed] [Google Scholar]