Abstract
Introduction
Statin has been reported to reduce cardiovascular events. However, the comparative efficacy of statin with standard therapy on cardiovascular events has not been sufficiently reported in patients on chronic hemodialysis. Thus, this study aimed to compare the effects of pitavastatin and standard therapy on mortality and cardiovascular events in chronic hemodialysis patients with dyslipidemia in Japan.
Methods
Patients on chronic hemodialysis with dyslipidemia were randomized into pitavastatin-administered (pitavastatin group) or dietary therapy as standard therapy (control) group. Primary outcomes are all-cause mortality and myocardial infarction; secondary outcomes are cardiac arrest and fatal myocardial infarction. The composite outcomes included the incidence of coronary intervention, stroke, fracture, and hospitalization due to heart failure and unstable angina. The clinical outcome analyses used a logistic regression model to categorize the variables. A p value of <0.05 was considered statistically significant.
Results
This study included 848 patients (422 in the control group and 426 in the pitavastatin group) from 79 health facilities. The mean age of the patients was 60.1±10.3 years, and the dialysis period was 7.2±7.6 years. The mean observation period was 36.5 months. The low-density lipoprotein cholesterol level was significantly lower than the baseline value in the pitavastatin group after 12 months of trial (79.8±26.1 vs. 107.8±25.5 mg/dL, p < 0.001). Moreover, the total number of deaths was 85, of which 50 occurred in the control group and 35 in the pitavastatin group. In an analysis adjusted for confounding factors due to participant attributes, there was a significant difference between the control group and the pitavastatin group in the primary and composite endpoints (p = 0.007 and p = 0.022, respectively).
Conclusion
Our study has demonstrated that aggressive intervention with pitavastatin is more effective than the standard (dietary) therapy for improving the clinical outcomes in patients with dyslipidemia on chronic hemodialysis.
Keywords: Dyslipidemia, Hemodialysis, Cardiovascular diseases, Mortality, Statins
Introduction
Japanese uremic patients have received high-quality dialysis therapy such as strictly managed high-quality dialyzate, single-use dialysis equipment, and high-performance dialyzer. The standard is dialysis treatment for 4 h or more once or 3 times a week. Hence, the prognosis of patients on chronic hemodialysis in Japan is one of the highest in the world [1]. However, a report by the Japanese Society for Dialysis Therapy (JSDT) indicated that the annual total mortality rate of patients on dialysis was 10.1% in 2019, which is greater than the rate recorded 10 years earlier [2]. In 2006, the annual incidence of myocardial infarction (MI) was reported to be 4.5% in Japan [3]. About 30% of the deaths of chronic dialysis patients were occurred by cardiovascular diseases in 2020 [1]. Cardiovascular events in patients on dialysis are unique to the pathophysiology of renal failure, which may lead to sudden death and congestive heart failure and are different from those in the general population [4, 5]. Arteriosclerosis has also been linked to chronic kidney disease (CKD) [5]. Various results have been shown for the effects of statins in chronic hemodialysis patients with dyslipidemia [6, 7]. In addition to high-quality dialysis treatment, guidance in the management of renal anemia and CKD-mineral bone disorders is provided by JSDT, and comprehensive dialysis care is performed in Japan. Previous studies have indicated that small dense low-density lipoprotein (LDL) in the serum increases due to decreased lipoprotein lipase activity in patients with end-stage kidney disease [8]. Additionally, high serum small dense LDL levels, which were effectively reduced with statins, were found in patients with MI [9, 10]. We speculated that active lipid-lowering using statins would be effective for suppressing cardiac and cerebrovascular events in chronic hemodialysis patients receiving high-quality dialysis therapy, as in healthy people.
Methods
Study Design
DIALYSIS was a randomized, open-label, placebo-controlled, multicenter trial. According to the 2007 report compiled by the Japanese Society of Kidney Dialysis, the annual survival rate of dialysis patients in Japan is reported to be 87.4%, and the incidence of MI in Japan in 2006 is reported to be 4.5% per year [3]. Although these studies differ in the time and method of investigation, the incidence of major events (death and myocardial infarction) in patients undergoing maintenance hemodialysis in this study was set at 10% per year based on these reports. To verify this with a log rank test with a significance level of 5% on both sides and a power of 80% under the conditions of a registration period of 2 years and a follow-up period of 2 years, the expected number of events is 348, and the cumulative dropout rate is 10. In the case of %, 775 cases in one group (1,550 cases in total) were considered appropriate. This study was registered in ClinicalTrials.gov PRS (ID. NCT00846118). However, because the number of registered cases is small and the number of annual events is small after the start of the study, it was judged that reaching the target case was important for this study, and both the registration and the study period were extended. The study was conducted in accordance with the ethical principles of the Declaration of Helsinki, the Good Clinical Practice Guidelines of the International Conference of Harmonization, and local regulatory requirements. This study protocol was reviewed and approved by Juntendo University Hospital Ethics Committee in Juntendo University Hospital, approval number 550. We prepared to recruit patients with chronic hemodialysis including vulnerable patients. Patient enrollment period was from February 1, 2009, to July 31, 2012. All subjects could understand the explanation of participation in the clinical trial and decide to participate by themselves. Eligible patients were assigned a study number. According to the backgrounds (sex, age, and baseline status with respect to coronary heart disease), they were randomly assigned (in a 1:1 ratio) to receive either pitavastatin (Livalo® tablet; Kowa, Tokyo, Japan) at 1–4 mg daily or dietary therapy (control) during the study observation period. During the study period, pamphlets for lipid management prepared by managerial dieticians were distributed periodically to the patients in the control group, and the medical staff provided explanations using the handouts at the time. The baseline assessment was done at once through laboratory evaluation of blood samples at a central laboratory to analyze the levels of lipids, albumin, aspartate aminotransferase, alanine aminotransferase, calcium, inorganic phosphorus, hemoglobin, and high-sensitivity C-reactive protein. Patients were reassessed at the end of the study period.
Eligibility Conditions for the Participants
The inclusion criteria for this study are the following: patients within the age range of 20–75 years with end-stage kidney disease, who were on chronic hemodialysis, and with dyslipidemia (as defined by any of the following parameters: LDL-cholesterol (LDL-C) of >110 mg/dL, a total cholesterol of >180 mg/dL, or receiving cholesterol-lowering treatment). Exclusion criteria are the following: received statin and fibrate therapy within the previous 6 months; enrolled in other trials in which pitavastatin is contraindicated; diagnosed with acute MI within the previous 6 months; underwent cardiovascular revascularization within the previous 6 months; and with familial history of hypercholesterolemia, malignant condition, and/or active liver disease. Additionally, patients were excluded if judged ineligible by the investigators.
Randomization of Patients
A total of 905 patients were screened for this study from February 01, 2009, through July 31, 2012. Only four patients did not meet the inclusion criteria, while four withdrew their consent before grouping. Thus, a total of 897 patients in 79 dialysis centers were randomly assigned to either treatment with pitavastatin (pitavastatin group, 449 patients) at a dose of 1–4 mg daily or dietary therapy (control group, 448 patients).
Clinical Outcomes
The primary outcomes include all-cause mortality and nonfatal MI, whereas fatal MI, arrhythmia, and congestive heart failure (CHF) comprised the secondary outcomes. All MIs, strokes, arrhythmias, and deaths were reviewed and adjudicated by a clinical endpoint committee, whose members were unaware of randomized treatment assignments, to ensure a consistent cardiovascular event diagnosis. Composite outcomes included cardiovascular death, cardiovascular event-free survival (i.e., nonfatal MI, serious arrhythmia, coronary revascularization such as percutaneous coronary intervention and coronary artery bypass grafting), admission for unstable angina and CHF, nonfatal cerebrovascular events, and bone fracture. Additionally, the number of adverse events and the occurrence of side effects were also investigated as safety outcomes. A judgment committee was independently set up, consisting of one cardiologist and one neurologist, to confirm the diagnosis of the cardiac and cerebrovascular events. The observation period for clinical outcomes was from the start date of case enrollment to September 30, 2014.
Statistical Analysis
The results were assessed in an intention-to-treat analysis. The Kaplan-Meier model for censored variables was employed to assess the association between statin use and event occurrences, independent of other predictors. The Cox proportional hazard model was employed to assess the association using variables adjusted for patient background factors that may be associated with or may confound event onset, such as age, gender, dialysis period, presence of hypertension (HT) and diabetes mellitus (DM), smoking habits, and history of ischemic heart disease (IHD) and statin use. All data were shown as mean ± standard deviation. Statistical analysis was performed with paired t test or χ2 test in appropriate data. Time course of LDL-C and triglyceride (TG) was analyzed by one-way ANOVA. A p value of <0.05 was considered statistically significant. All analyses were performed using the Statistical Package for the Social Sciences software (IBM SPSS Statistics, version 28.0.0.0).
Results
Baseline Clinical Profile of Patients
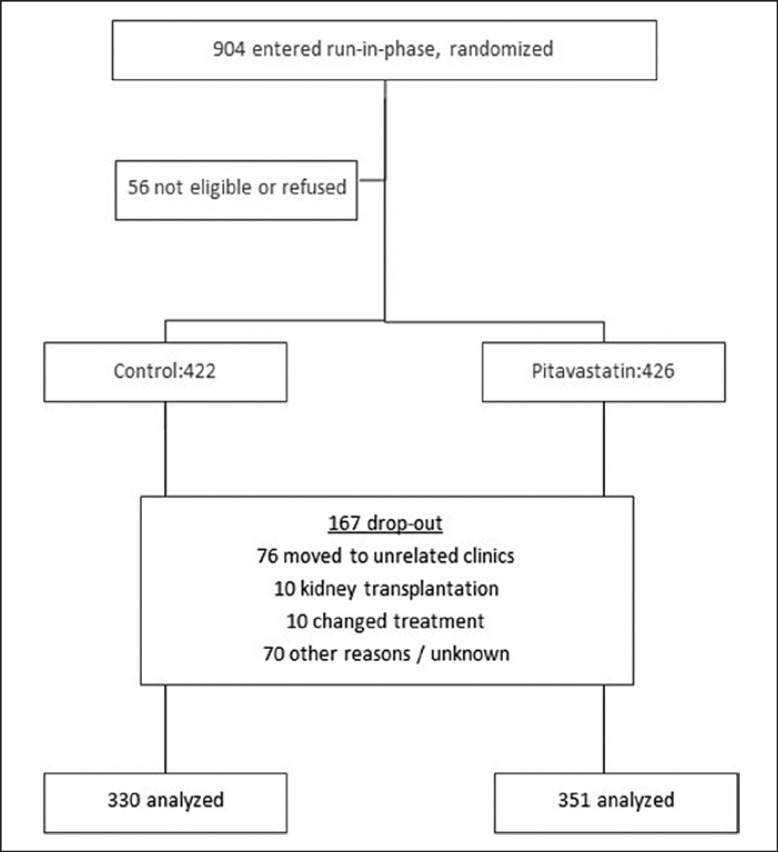
A total of 167 patients, comprising 75 in the pitavastatin group and 72 in the control group, discontinued the protocol before the endpoint. Of which, 76 patients were referred to unrelated clinics, 10 underwent kidney transplantation, 10 changed treatment, and 70 had other reasons (Fig. 1). Of the 904 patients recruited, 848 patients were analyzed for clinical data, and 681 patients were analyzed for the association between statin use and clinical events. Mean age was 60.0±10.3 years, 310 (36.6%) were female, 386 (45.5%) had DM, and 196 (23.1%) had a history of vascular disease (angina, stroke, or peripheral vascular disease). One hundred six patients had IHD, 100 patients had cerebrovascular disease, and 16 patients had both IHD and cerebrovascular disease. Mean baseline non-fasting plasma concentrations were 108.7±26.1 mg/dL for directly measured LDL-C, 43.1±14.9 mg/dL for high-density lipoprotein cholesterol (HDL-C), and 152.7±97.7 mg/dL for TGs (Table 1). Hemodialysis period was 7.3±14.9 years. Seven hundred eighteen (84.7%) had HT. Three hundred eighteen of those (37.5%) used RAS-anti-HT drugs, 91 patients (10.7%) used calcium channel blockers, and 182 patients (21.5%) used diuretics. Erythropoietin was administrated to half of the participants. Antiplatelet drug was used in 39.4% of those patients.
Fig. 1.
Trial protocol.
Table 1.
Characteristics of participants at the initiation of the study
| Control | Pitavastatin | p value | |
|---|---|---|---|
| Age, years | 59.7±11.0 | 61.0±10.8 | ns |
| Gender (female), n | 163 | 173 | ns |
| Duration of HD, years | 8.5±7.3 | 7.4±7.8 | ns |
| Cause of CKD (DM), n | 200 | 207 | ns |
| History of IHD, n | 56 | 57 | ns |
| Body height, cm | 161.2±9.6 | 160.6±9.3 | ns |
| Body weight, kg | 59.7±13.3 | 59.9±13.2 | ns |
| Systolic BP, mm Hg | 148.7±21.1 | 148.7±21.8 | ns |
| Diastolic BP, mm Hg | 78.8±13.2 | 78.9±13.4 | ns |
| Pulse rate, /min | 7.66±12.9 | 76.5±11.8 | ns |
| Comorbidity | |||
| HT, n | 394 | 376 | ns |
| Cerebrovascular events, n | 44 | 65 | ns |
| CHF, n | 26 | 25 | ns |
| Smoking, n | 196 | 202 | ns |
| PAD, n | 11 | 12 | ns |
| Cardiac valve disease, n | 6 | 8 | ns |
| Malignancy, n | 24 | 17 | ns |
| Fracture, n | 7 | 5 | ns |
| Liver diseases, n | 11 | 12 | ns |
| SHPT, n | 37 | 36 | ns |
| Blood data | |||
| Hb, g/dL | 10.7±1.1 | 10.7±1.1 | ns |
| Alb, mg/dL | 3.8±0.3 | 3.8±0.3 | ns |
| LDL-C, mg/dL | 109.0±25.9 | 108.4±26.3 | ns |
| TG, mg/dL | 151.6±98.8 | 153.7±96.7 | ns |
| HDL-C, mg/dL | 43.6±15.6 | 42.6±15.0 | ns |
| Calcium, mg/dL | 8.9±0.7 | 8.9±0.8 | ns |
| Phosphate, mg/dL | 5.6±1.5 | 5.7±1.4 | ns |
| CK, IU/L | 101.9±84.7 | 104.0±71.3 | ns |
| Drug therapy | |||
| ARB/ACE-I, n | 176 (39.5%) | 168 (37.6%) | ns |
| B-blocker, n | 44 (9.9%) | 52 (11.6%) | ns |
| Diuretics, n | 100 (22.4%) | 95 (21.3%) | ns |
| EPA, n | 29 (6.5%) | 25 (5.6%) | ns |
| Erythropoietin, n | 244 (54.7%) | 227 (50.8%) | ns |
| Antiplatelet drugs, n | 179 (40.1%) | 185 (41.4%) | ns |
HD, hemodialysis; CKD, chronic kidney disease; DM, diabetes mellites; IHD, ischemic heart disease; BP, blood pressure; CHD, congestive heart failure; PAD, peripheral arterial disease; SHPT, secondary hyperparathyroidism; Alb, albumin; LDL-C, low-density lipoprotein cholesterol; TG, triglyceride; HDL-C, high-density lipoprotein cholesterol; CK, creatinine kinase; AST, aspartate aminotransferase; ALT, alanine aminotransferase; ARB, angiotensin receptor blocker; ACE-I, angiotensin-converting enzyme blocker; B-blocker, beta blocker; EPA, eicosapentaenoic acid.
Post-Intervention Clinical Parameters
Biological data at 12 months after starting of the pitavastatin intervention are shown in Table 2. The serum LDL-C, TG, and non-HDL-C levels in the pitavastatin group were significantly lower than those in the control group (p < 0.001, p < 0.05, and p < 0.001, respectively), but no significant differences were found in the serum albumin, calcium, inorganic phosphorus, and hemoglobin levels.
Table 2.
Biological data 12 months after the intervention
| Control | Pitavastatin | p value | |
|---|---|---|---|
| Alb, g/dL | 3.8±0.4 | 3.8±0.4 | ns |
| LDL-C, mg/dL | 98.0±26.8 | 79.8±25.4 | <0.001 |
| TG, mg/dL | 144.3±105.5 | 130.2±90.9 | <0.05 |
| HDL-C, mg/dL | 44.3±15.0 | 44.8±15.0 | ns |
| CK, IU/L | 113.7±170.6 | 103.3±69.8 | ns |
| AST, IU/L | 13.4±7.4 | 13.5±6.7 | ns |
| ALT, IU/L | 11.1±7.3 | 11.5±6.4 | ns |
| Ca, mg/dL | 9.0±0.9 | 9.0±0.7 | ns |
| Pi, mg/dL | 5.7±1.3 | 5.8±1.5 | ns |
| Hb, g/dL | 10.6±1.0 | 10.7±1.2 | ns |
Alb, albumin; LDL-C, low-density lipoprotein cholesterol; TG, triglyceride; HDL-C, high-density lipoprotein cholesterol; CK, creatinine kinase; AST, aspartate aminotransferase; ALT, alanine aminotransferase; Ca, calcium; Pi, inorganic phosphorous; Hb, hemoglobin.
Changes in Serum Lipid Profile
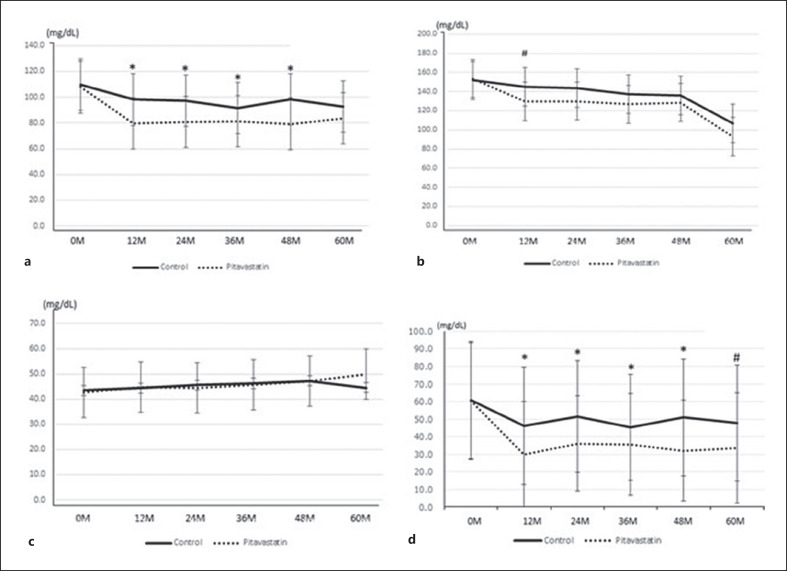
Changes in serum lipids were confirmed in each group after 12, 24, 36, 48, and 60 months and compared between the two groups at the time points (Fig. 2a-d). The levels of LDL-C and non-HDL-C were significantly decreased after the starting observation. The LDL-C in the pitavastatin group was significantly lower than that in the control group from 12 to 48 months (p < 0.05) (Fig. 2a). Additionally, the TG levels in the pitavastatin group were lower than those in the control group during the observation period, but a significant difference (p < 0.05) was observed only at 12 months (Fig. 2b). The levels of TG in sera at 12, 24, and 60 months in the pitavastatin were significantly lower than those at the starting (p < 0.05). No significant changes were found in the HDL-C levels in both groups during the observation period (Fig. 2c). The serial changes in non-HDL-C in both groups tended to be similar to those of LDL-C (Fig. 2d).
Fig. 2.
Changes in serum lipids were confirmed in each group after 12, 24, 36, 48, and 60 months and compared between the two groups at the time points. LDL-C in the pitavastatin group was significantly lower than that in the control group from 12 to 48 months. The levels of LDL-C in the pitavastatin group were significantly lower than those in the control group at 12, 24, 36, 48, and 60 months (*p < 0.001) (a). TG levels in the pitavastatin group were also lower during the observation period, but a significant difference was observed only at 12 months (#p < 0.05) (b). The level of HDL-C was no change in both the two groups during the observation period, and there was no significant difference between the two groups (c). The serial changes of non-HDL-C in both groups tended to be similar to those of LDL-C. The levels of LDL-C in the pitavastatin group were significantly lower than those in the control group at 12, 24, 36, 48, and 60 months (*p < 0.001, #p < 0.05) (d).
Clinical Outcomes
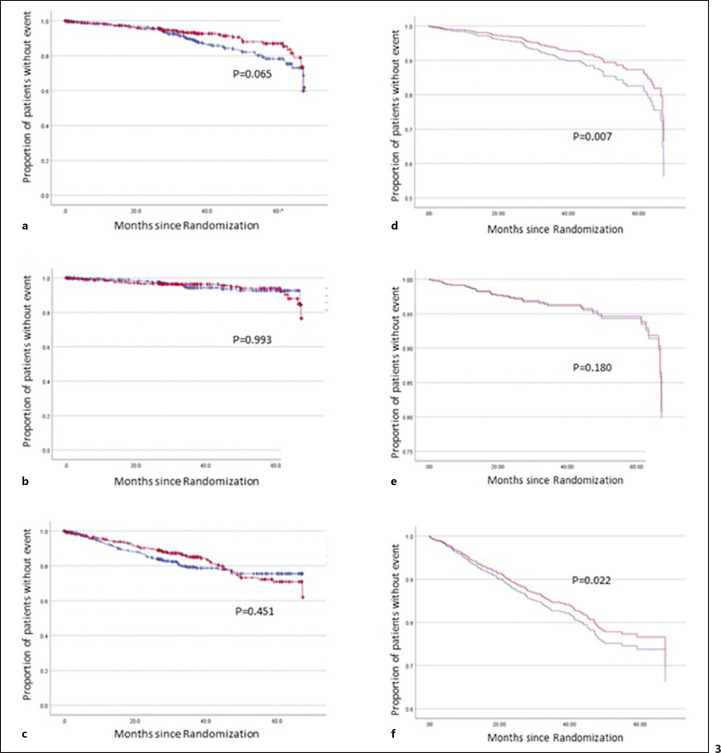
The mean length of the follow-up period was 36.9±17.4 months (maximum of 67.4 months). During the observation, 85 patients died. The adjudicated 33 patients died of cardiovascular causes (Table 3). Among the primary, secondary, and composite endpoints using unadjusted variables, no significant difference was observed between the pitavastatin and the control groups (p = 0.065, p = 0.993, and p = 0.451, respectively) (Fig. 3a-c). Using the adjusted variables about the patients' background information, such as gender and age, the introduction of dialysis due to diabetic nephropathy, dialysis period, complications of HT and DM, smoking, history for IHD and statin use, the primary, secondary, and composite outcome were analyzed between the control and pitavastatin groups, which revealed significant differences in the primary and composite endpoints (p = 0.007 and p = 0.022, respectively) (Fig. 3d-f).
Table 3.
Clinical events during observation
| Control | Pitavastatin | Total | |
|---|---|---|---|
| All cause of death, n | 52 | 38 | 90 |
| Cardiac death, n | 16 | 19 | 35 |
| Acute MI, n | 27 | 20 | 47 |
| Serious arrhythmia, n Admission | 1 | 0 | 1 |
| Unstable angina, n | 11 | 8 | 19 |
| CHF, n | 23 | 17 | 40 |
| Interventions, n | 32 | 29 | 61 |
| Cerebrovascular events, n | 21 | 17 | 38 |
| Fracture, n | 19 | 18 | 37 |
MI, myocardial infarction; CHF, congestive heart failure.
Fig. 3.
Effects of allocation to pitavastatin (red line) versus standard (nutritional therapy, blue line) on clinical outcomes. a Unadjusted Kaplan-Meier curves modeling time to the primary endpoint: all-cause death and new nonfatal myocardial infarction. No significant effect was observed on the primary endpoint between the pitavastatin group and the control group. b Unadjusted Kaplan-Meier curves modeling time to the secondary endpoint: death from cardiovascular causes such as MI, arrhythmia, CHF, and new nonfatal MI. No significant differences were found in the therapeutic effect of pitavastatin and standard (nutritional) therapies on the secondary measures. c Unadjusted Kaplan-Meier curves modeling time to composite endpoint: the secondary endpoint, revascularization (percutaneous coronary intervention and coronary artery bypass grafting), severe arrhythmia, stroke, fracture, or hospitalization due to CHF and unstable angina. No significant effect was observed on the primary endpoint between the pitavastatin group and the control group. d Adjusted Cox proportional hazard curve modeling time to primary endpoint: the occurrence of the primary outcomes was significantly lower in the pitavastatin group than that in the control group (p = 0.007). e Adjusted Cox proportional hazard curve modeling time to secondary endpoint: the occurrence of the secondary outcomes was no significant difference between the pitavastatin and the control groups (p = 0.181). f Adjusted Cox proportional hazard curve modeling time to composite endpoint: the occurrence of the composite outcomes was significantly lower in the pitavastatin group than that in the control group (p = 0.022).
Adverse Events and New Complications during the Observation Period
Neither adverse events nor adverse reactions were reported during the study period. However, secondary hyperparathyroidism, diabetic retinopathy, and hypothyroidism were reported as complications during the study period (Table 4). No significant difference was found between the two groups regarding the onset of these complications.
Table 4.
Complications during the observation period
| Pitavastatin, N (%) | Control, N (%) | |
|---|---|---|
| Secondary hyperparathyroidism | 32 (7.4) | 30(6.2) |
| Diabetic retinopathy | 9 (2.0) | 10 (2.2) |
| Hypothyroidism | 11 (2.5) | 7 (1.6) |
| Atrial fibrillation (chronic/paroxysmal) | 11 (2.5) | 7 (1.6) |
| Cataract | 8 (1.8) | 6 (1.3) |
| Hyperuricemia | 6 (1.3) | 8 (1.8) |
| Colon polyp | 5 (1.1) | 7 (1.6) |
| Bronchial asthma | 6 (1.3) | 6 (1.3) |
| Angina | 5 (1.1) | 7 (1.6) |
| Arteriosclerosis obliterans | 6 (1.3) | 6 (1.3) |
| Multiple kidney cysts | 6 (1.3) | 1 (0.2) |
Conclusion
In the present study, analysis using unadjusted variables did not show a significant difference in clinical outcomes between the control group and the pitavastatin group. However, in an analysis adjusted for confounding factors due to participant attributes, there was a significant difference between the control group and the pitavastatin group in the primary and composite endpoints. Large-scale intervention studies on the effects of statins on cardiovascular events in patients with advanced CKD, such as the AURORA [11] and the 4D [12] studies, have shown that statin intervention was not effective in suppressing cardiovascular events. However, in another study (the SHARP study), the combined intervention of statins and ezetimibe (inhibitor of intestinal cholesterol absorption) significantly suppressed cardiovascular events in the treatment group compared with the control group [13]. In the present study, the LDL-C levels were significantly lower in patients who were treated with pitavastatin compared with those who received standard therapy during the 1-year observation period. This finding was at variance with the SHARP study, in which the baseline and posttreatment LDL-C levels were not significantly different. The low target value of drug intervention is considered one of the factors for suppressing cardiovascular events [13]. Regarding lipid management in patients on dialysis, the target LDL-C value was in response to the report of the “J curve” of life prognosis in a cross-sectional observational study that indicated a poor prognosis in the group showing hypocholesterolemia [14, 15].
During the observation period, pitavastatin suppressed hospitalization for unstable angina, heart failure, cardiac revascularization, and cerebrovascular accidents compared with the standard (nutritional) therapy. Pitavastatin is a novel synthetic lipophilic statin that has several pharmacodynamic and pharmacokinetic properties distinct from those of other statins, which may underlie its potential pleiotropic benefits in reducing cardiovascular risk factors [16]. Large-scale studies, such as the PATROL and the Phase III studies, have compared pitavastatin and other statins, such as atorvastatin, rosuvastatin, and simvastatin, in terms of LDL-C-lowering effect and safety [17, 18]. In both studies, pitavastatin showed the same LDL-C-lowering effect as other drugs, while the tolerability was confirmed on long-term administration [19, 20, 21, 22]. These studies were conducted in patients without impaired renal function. However, a sub-analysis of the LIVES study confirmed pitavastatin as safe and with LDL-C-lowering effect even in patients with impaired renal function [23]. Therefore, the LDL-C-lowering effect of pitavastatin in patients with advanced kidney diseases is not surprising. The Phase III studies of pitavastatin showed that serum HDL-C levels increased after 12 weeks of admission by 2–6% from the baseline value [17].
Recently, the pleiotropic and subclinical effects of several statins, including pitavastatin, have been pointed out [24]. A meta-analysis by Matthew et al. revealed that statin therapy may suppress hospitalization and death from heart failure in patients with IHD [6]. In a cohort study of 4,074 patients on hemodialysis in Taiwan, statins also reduced hospitalization due to unstable angina and ischemic stroke [25]. A retrospective study after 10 years of cardiac revascularization in patients on hemodialysis revealed better outcomes with statin therapy in all-cause mortality, as well as revascularization and readmission due to adverse cardiac events, than the control treatment [26]. The serum LDL-C and non-HDL-C levels in the pitavastatin group were significantly lower than in the control group. In this longitudinal study, the improvement in clinical outcomes in patients on stable hemodialysis is attributed to both the strict control of serum LDL-C and non-HDL-C levels with pitavastatin and the non-lipid effects of statins. In this study, the number of participating patients and the number of events were small, and the evaluation was limited. Therefore, it is necessary to examine a larger number of cases.
The reduction of LDL-C using pitavastatin in chronic hemodialysis patients with dyslipidemia was not effective in improving mortality or suppressing the onset of myocardial infarction. However, it was suggested that continuation of strict management of lipids using statins suppressed mortality and cardiovascular events in the patients with arteriosclerosis risk factors and history of cardiac events.
Statement of Ethics
The study was conducted in accordance with the ethical principles of the Declaration of Helsinki, the Good Clinical Practice Guidelines of the International Conference on Harmonization, and local regulatory requirements. This study protocol was reviewed and approved by Juntendo University Hospital Ethics Committee in Juntendo University Hospital, approval number 550. We prepared to recruit patients with chronic hemodialysis including vulnerable patients. The patients signed voluntarily after being provided with sufficient explanation for participation using written informed consent to participate in the clinical trial. If it was difficult for the individual to understand the research protocol, a family member or legally acceptable person was present at the time of explanation to the individual, and participation could be made with the consenting signature of the legally acceptable person who confirmed the individual's intention. Patient enrollment period was from February 1, 2009, to July 31, 2012. No vulnerable patients participated in the study. All subjects could understand the explanation of participation in the clinical trial and decide to participate by themselves. This study was registered in ClinicalTrials.gov PRS (ID. NCT00846118).
Conflict of Interest Statement
The authors have no conflicts of interest to declare.
Funding Sources
This study was carried out by a research grant from the Japan Kidney Foundation (Chiyoda-Ku, Tokyo, Japan), which manages funds donated by various related companies (no grant number). The Japan Kidney Foundation provided the fund, properly managed expenditures, and monitored research progress.
Author Contributions
Chieko Hamada, MD, PhD (as a data manager and manuscript author), Juntendo University Faculty of Health Sciences and Nursing, 3-7-33 Omiya, Mishima, Shizuoka, 411-8787, Japan, Phone: 81-55-991-3111. Masumi Okuda MD, PhD (as a manager for research and manuscript author), Medical Corporation SHOWAKAI, Shinsen-ikebukuro clinic, Tobu annex-Bldg, 4FL, 1-10-10 Nishiikebukuro Toshima-ku, 171-0021, Tokyo, Japan, Phone: 81-3-5911-1260. Yasuhiko Tomino, MD, PhD (as a general coordinator and manuscript author), Asian Pacific Renal Research Promotion Office, Medical Corporation SHOWAKAI, 3-12-12 Nishi-Shinjuku, Shinjuku, 160-0023, Tokyo, Japan, Phone: 81-3-5304-5655.
Data Availability Statement
All data generated or analyzed during this study are included in this article. Further inquiries can be directed to the corresponding author.
Acknowledgments
We would like to express our deep gratitude to Dr. Tomohito Goda, Dr. Mitsuo Tanimoto, and Dr. Shinji Hagiwara as members of study management; Dr. Kazuo Kitagawa, Dr. Hideki Takayama, and Dr. Tsutomu Yoshikawa as members of event judgment; colleagues of the Department of Nephrology, Juntendo University, who contributed greatly to the data collection; Ms. Fumie Shimazawa and Ms. Hiromi Narushima, who supported the research as the secretaries; and Dr. Kiyoshi Matsuoka who supported to analyze the data. We thank the participants and the staff in the following facilities of the DIALYSIS group for enrolling many cases and for their efforts in collecting clinical data: Bosei Clinic, Saitama, Japan; Saiyu Soka Hospital, Saitama, Japan; Saiyu Clinic, Saitama, Japan; Yuai Clinic, Saitama, Japan; Misato Cyu-o General Hospital, Saitama, Japan; Juntendo Tokyo Koto Geriatric Medical Center, Tokyo, Japan; Juntendo Nerima Hospital, Tokyo, Japan; Shinkoiwa Clinic, Tokyo, Japan; Bosei Tanashi Clinic, Tokyo, Japan; Bosei nishi-shinjuku Clinic, Tokyo, Japan; Bosei Minami-shinjuku Clinic, Tokyo, Japan; Nerima Takanodai Clinic, Tokyo, Japan; Minamisuna Jin Clinic, Tokyo, Japan; Mizue Jin Clinic, Tokyo, Japan; Nishi-ojima Jin Clinic, Tokyo, Japan; Shinkoiwa-Funabori Clinic, Tokyo, Japan; Nerimasakuradai Clinic, Tokyo, Japan; Akihabara Jin Clinic, Tokyo, Japan; Ryogoku Higashiguchi Clinic, Tokyo, Japan; Tsubasa Clinic, Tokyo, Japan; Nisshin Ekimae Clinic, Tokyo, Japan; Tokyo Ayase Jin Clinic, Tokyo, Japan; Koto Hospital, Tokyo, Japan; Monnaka Clinic, Tokyo, Japan; Higashi-Kasai Clinic, Tokyo, Japan; Kitasenju Higashiguchi Clinic, Tokyo, Japan; Shin-minamigyotoku, Chiba, Japan; Motoyahata Jin Clinic, Chiba, Japan; Koza Shibuya Jin Clinic, Kanagawa, Japan; Bosei Hiratsuka Clinic, Kanagawa, Japan; Motoatsugi Medical Clinic, Kanagawa, Japan; Juntendo Shizuoka Hospital, Shizuoka, Japan; Bosei Daiichi Clinic, Shizuoka, Japan; Okachimashi Jin Clinic, Tokyo, Japan; Teikyo University Hospital, Tokyo, Japan; Kawasaki Clinic, Kanagawa, Japan; Yokosuka Clinic, Kanagawa, Japan; Kurihama Clinic, Kanagawa, Japan; Tokai University Oiso Hospital, Kanagawa, Japan; Tobu Nerima Clinic, Tokyo, Japan; Kitasaito Hospital, Hokaido, Japan; Adachi-Iriya-Toneri Clinic, Tokyo, Japan; Kodaira Kitaguchi Clinic, Tokyo, Japan; Higashikurume Clinic, Tokyo, Japan; Kita-Hachioji Clinic, Tokyo, Japan; Tachibana Clinic, Tokyo, Japan; Ikegami General Hospital, Tokyo, Japan; Kurata Hospital, Kanagawa, Japan; Kameido Nephrology Clinic, Tokyo, Japan; Miyamura Clinic, Saitama, Japan; Tokyo-Kita Medical Center, Tokyo, Japan; Akabane Center General Hospital, Tokyo, Japan; Yujin Clinic, Tokyo, Japan; Yujin-Ohizumi-Gakuen Clinic, Tokyo, Japan; Tsuruta Clinic, Tokyo, Japan; Inokuchi Hospital, Tokyo, Japan; Kitami-Higashiyama Clinic, Tokyo, Japan; Horinouchi Clinic, Saitama, Japan; Kakuta Clinic, Saitama, Japan; Kawaguchi-Rokken Clinic, Saitama, Japan; Iwatsuki-Minami Hospital, Saitama, Japan; Nakajima Hospital, Tokyo, Japan; Shonan Kamakura General Hospital, Kanagawa, Japan; Kubojima Clinic, Saitama, Japan; Keiai Clinic, Tokyo, Japan; Akamatsu Dialysis Clinic, Tokyo, Japan; Itabashi-Ishikawa Clinic, Tokyo, Japan; Akatuka-Saiwai Clinic, Tokyo, Japan; Akabane Center General Hospital-Clinic, Tokyo, Japan; Bosei Kannai Clinic, Kanagawa, Japan; Sayama Jin Clinic, Saitama, Japan; Fujidaiichi Clinic, Shizuoka, Japan; Oizumi-Gakuen Clinic, Tokyo, Japan; Seisyokai General Clinic, Saitama, Japan; and Maeda Memorial Musashikosugi Clinic, Kanagawa, Japan.
Funding Statement
This study was carried out by a research grant from the Japan Kidney Foundation (Chiyoda-Ku, Tokyo, Japan), which manages funds donated by various related companies (no grant number). The Japan Kidney Foundation provided the fund, properly managed expenditures, and monitored research progress.
References
- 1.Goodkin DA, Bragg-Gresham JL, Koenig KG, Wolfe RA, Akiba T, Andreucci VE, et al. Association of comorbid conditions and mortality in hemodialysis patients in Europe and the United States the dialysis outcomes and Practice patterns study (DOPPS) J Am Soc Nephrol. 2003;14((12)):3270–3277. doi: 10.1097/01.asn.0000100127.54107.57. [DOI] [PubMed] [Google Scholar]
- 2.The Japanese Society for Dialysis Therapy Aggregation for chronic dialysis patients at the end of 2020. Available from: https://docs.jsdt.or.jp/overview/index.html.
- 3.Iseki K, Shoji T, Nakai S, Watanabe Y, Akiba T, Tsubakihara Y, et al. Higher survival rates of chronic hemodialysis patients on anti-hypertensive drugs. Nephron Clin Pract. 2009;113((3)):c183–c90. doi: 10.1159/000232600. [DOI] [PubMed] [Google Scholar]
- 4.Gregg LP, Hedayati SS. Management of traditional cardiovascular risk factors in CKD what are the data? Am J Kidney Dis. 2018;72((5)):728–744. doi: 10.1053/j.ajkd.2017.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wanner C, Amann K, Shoji T. The heart and vascular system in dialysis. Lancet. 2016;388((10041)):276–284. doi: 10.1016/S0140-6736(16)30508-6. [DOI] [PubMed] [Google Scholar]
- 6.Lee MMY, Sattar N, McMurray JJV, Packard CJ. Statins in the prevention and treatment of heart failure a review of the evidence. Curr Atheroscler Rep. 2019;21((10)):41. doi: 10.1007/s11883-019-0800-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mikolasevic I, Žutelija M, Mavrinac V, Orlic L. Dyslipidemia in patients with chronic kidney disease etiology and management. Int J Nephrol Renovasc Dis. 2017;10:35–45. doi: 10.2147/IJNRD.S101808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nishizawa Y, Shoji T, Tabata T, Inoue T, Morii H. Effects of lipid-lowering drugs on intermediate-density lipoprotein in uremic patients. Kidney Int Suppl. 1999;71:S134–6. doi: 10.1046/j.1523-1755.1999.07133.x. [DOI] [PubMed] [Google Scholar]
- 9.Albers JJ, Slee A, Fleg JL, O'Brien KD, Marcovina SM. Relationship of baseline HDL subclasses, small dense LDL and LDL triglyceride to cardiovascular events in the AIM-HIGH clinical trial. Atherosclerosis. 2016;251:454–459. doi: 10.1016/j.atherosclerosis.2016.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Marrs JC, Saseen JJ. Effects of lipid-lowering therapy on reduction of cardiovascular events in patients with end-stage renal disease requiring hemodialysis. Pharmacotherapy. 2010;30((8)):823–829. doi: 10.1592/phco.30.8.823. [DOI] [PubMed] [Google Scholar]
- 11.Fellström BC, Jardine AG, Schmieder RE, Holdaas H, Bannister K, Beutler J, et al. Rosuvastatin and cardiovascular events in patients undergoing hemodialysis. N Engl J Med. 2009;360((14)):1395–1407. doi: 10.1056/NEJMoa0810177. [DOI] [PubMed] [Google Scholar]
- 12.Wanner C, Krane V, März W, Olschewski M, Mann JFE, Ruf G, et al. Atorvastatin in patients with type 2 diabetes mellitus undergoing hemodialysis. N Engl J Med. 2005;353((3)):238–248. doi: 10.1056/NEJMoa043545. [DOI] [PubMed] [Google Scholar]
- 13.Baigent C, Landray MJ, Reith C, Emberson J, Wheeler DC, Tomson C, et al. The effects of lowering LDL cholesterol with simvastatin plus ezetimibe in patients with chronic kidney disease (Study of Heart and Renal Protection) a randomised placebo-controlled trial. Lancet. 2011;377:2181–2192. doi: 10.1016/S0140-6736(11)60739-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Iseki K, Yamazato M, Tozawa M, Takishita S. Hypocholesterolemia is a significant predictor of death in a cohort of chronic hemodialysis patients. Kidney Int. 2002;61((5)):1887–1893. doi: 10.1046/j.1523-1755.2002.00324.x. [DOI] [PubMed] [Google Scholar]
- 15.Degoulet P, Legrain M, Reach I, Aime F, Devries C, Rojas P, et al. Mortality risk factors in patients treated by chronic hemodialysis. Report of the Diaphane collaborative study. Nephron. 1982;31((2)):103–110. doi: 10.1159/000182627. [DOI] [PubMed] [Google Scholar]
- 16.Davignon J. Pleiotropic effects of pitavastatin. Br J Clin Pharmacol. 2012;73((4)):518–535. doi: 10.1111/j.1365-2125.2011.04139.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Saku K, Zhang B, Noda K. PATROL Trial Investigators. Randomized head-to-head comparison of pitavastatin and rosuvastatin for safety and efficacy (quantity and quality of LDL) the PATROL trial. Circ J. 2011;75((6)):1493–1505. doi: 10.1253/circj.cj-10-1281. [DOI] [PubMed] [Google Scholar]
- 18.Ose L, Budinski D, Hounslow N, Arneson V. Long-term treatment with pitavastatin is effective and well tolerated by patients with primary hypercholesterolemia or combined dyslipidemia. Atherosclerosis. 2010;210((1)):202–208. doi: 10.1016/j.atherosclerosis.2009.12.009. [DOI] [PubMed] [Google Scholar]
- 19.Chapman MJ. Pitavastatin novel effects on lipid parameters. Atheroscler Suppl. 2011;12((3)):277–284. doi: 10.1016/S1567-5688(11)70887-X. [DOI] [PubMed] [Google Scholar]
- 20.da Silva PM. Are all statins the same? Focus on the efficacy and tolerability of pitavastatin. Am J Cardiovasc Drugs. 2011;11((2)):93–107. doi: 10.2165/11591190-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 21.Sasaki J, Ikeda Y, Kuribayashi T, Kajiwara K, Biro S, Yamamoto K, et al. A 52-week parallel-group comparison of the tolerability and effects of pitavastatin and atorvastatin on high-density lipoprotein cholesterol levels and glucose metabolism in Japanese patients with elevated levels of low-density lipoprotein cholesterol and glucose intolerance. Clin Ther. 2008;30((6)):1089–1101. doi: 10.1016/j.clinthera.2008.05.017. [DOI] [PubMed] [Google Scholar]
- 22.Lee SH, Chung N, Kwan J, Kim DI, Kim WH, Kim CJ, et al. Comparison of the efficacy and tolerability of pitavastatin and atorvastatin an 8-week, multicenter, randomized, open-label, dose-titration study in Korean patients with hypercholesterolemia. Clin Ther. 2007;29((11)):2365–2373. doi: 10.1016/j.clinthera.2007.11.002. [DOI] [PubMed] [Google Scholar]
- 23.Kimura K, Shimano H, Yokote K, Urashima M, Teramoto T. Effects of pitavastatin (LIVALO tablet) on the estimated glomerular filtration rate (eGFR) in hypercholesterolemic patients with chronic kidney disease. Sub-analysis of the LIVALO Effectiveness and safety (LIVES) Study. J Atheroscler Thromb. 2010;17((6)):601–609. doi: 10.5551/jat.3764. [DOI] [PubMed] [Google Scholar]
- 24.Balk EM, Lau J, Goudas LC, Jordan HS, Kupelnick B, Kim LU, et al. Effects of statins on nonlipid serum markers associated with cardiovascular disease a systematic review. Ann Intern Med. 2003;139((8)):670–682. doi: 10.7326/0003-4819-139-8-200310210-00011. [DOI] [PubMed] [Google Scholar]
- 25.Huang CC, Chan WL, Chen YC, Chen TJ, Chung CM, Huang PH, et al. The beneficial effects of statins in patients undergoing hemodialysis. Int J Cardiol. 2013;168((4)):4155–4159. doi: 10.1016/j.ijcard.2013.07.115. [DOI] [PubMed] [Google Scholar]
- 26.Hu YN, Luo CY, Tsai MT, Lin TW, Kan CD, Roan JN. Post-coronary artery bypass medications in dialysis patients do we need to change strategies? Thorac Cardiovasc Surg. 2020;68((8)):706–713. doi: 10.1055/s-0039-3400471. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this article. Further inquiries can be directed to the corresponding author.