Abstract
Frailty, a vulnerability to stressors, has been increasingly woven into the clinical understanding of older people who are unable to respond to the impact of diseases, disability, and age-related decline. While the literature has focused on physical frailty, social frailty has been conceptualized within the domains of social needs (social and emotional support, loneliness), resources (income, food, housing, medical care, etc), social fulfillment (engagement in work and activities), and self-management (cognitive function, mental health, advance planning). This review outlines the assessment of the four domains of social frailty within the structure of clinical visits, particularly annual wellness and advance care planning. Increasing connectivity with the community, health system, and government support is the primary recommended intervention. On a policy level, expanding opportunities to connect socially frail people with resources may help mitigate the vulnerability of physical frailty.
Keywords: frailty, physical frailty, social frailty
INTRODUCTION
Frailty decreases resiliency and reserves, which renders people vulnerable to the stress of disease, disability, or social change. Physical frailty has dominated medical literature for the past 20 years. With prevalence estimates of up to 45% among adults 85 years or older,1 physical frailty increases the risk of low functional status, hospitalization, and mortality.2 Despite its high prevalence, physical frailty is not a normal process of aging, and many have postulated that frailty can be prevented or treated.3
Over the past two decades, physical frailty measurements have emerged: 1) the clinically favorable frailty phenotype and 2) the data-focused frailty index (accumulation of deficits). The phenotype of frailty by Fried et al. (2001) includes five criteria: weight loss, reduced activities, grip strength, gait speed, and exhaustion. Clinically, the objective measurement of the frailty phenotype is possible within the context of an office visit and is billable, starting in 2021, with the R54 ICD-10 code. In contrast, the frailty index presents a model of deficit accumulation.4 With the breadth of comorbidities, disabilities, and age-related decline, each additional deficit results in the patient being less able to rebound from stressors. For example, a patient with many comorbidities, including dementia, is going to be less able to rebound from the stress of acute hospitalization. Frailty indexes incorporate clinical information, such as that from an assessment of function, cognition, depression, physical ability, and comorbidities. For clinicians with access to electronic medical record data, the frailty index can be calculated with fields completed in the course of clinical care.
The social frailty gap
In examining the fundamental definition of frailty – a decrease in resiliency and reserves, clinicians invariably recognize that numerous social factors beyond those contributing to the phenotype of frailty index definitions play a substantial role in patient function. For example, if a person lacks financial resources for food (a socially-anchored process), solely capturing strength loss in the physical frailty phenotype does not account for social factors that may be largely responsible for frailty in nonphysical domain. Thus, there is a gap in the narrow definitions of physical frailty that does not include the broader perspective of social frailty – a gap that has clear ramifications for improving patient care, and even potentially mitigating negative outcomes. Therefore, social frailty should be considered in concert with broader frailty definition. Social frailty has been defined as a progressive loss of resources, activities, or the ability to participate in social activities to fulfill basic social needs.5
Social frailty often manifests with clinical stressors such as the response to a new diagnosis or acute hospitalization, when the system supporting the patient may get overwhelmed or break down. Other symptoms of social frailty include limited social support, a smaller social network, poor living conditions, fewer socially-oriented leisure activities, and risk of losing resources.5 Other features may include unhealthy social behaviors (lack of physical exercise, poor diet, alcohol use, and smoking), social isolation, and loneliness.5 Social frailty is a broad but highly medically relevant construct. Yet, clinical tools for identifying social frailty remain elusive.
The purpose of this article is to describe the intersection of physical frailty and social frailty and utilize existing social frailty literature to describe a framework for building a clinical checklist of social frailty.
The social frailty framework: measurement and integration into care and treatment
Figure 1 highlights the intersection of physical and social frailty. This intersection is influenced by biological, psychological, social, and environmental factors. Prior systematic reviews of social frailty have developed a framework of four social frailty domains5 including 1) social needs; 2) general resources; 3) social fulfillment; and 4) self-management to provide a more comprehensive view of the system supporting people living with frailty. Social needs encompass social and emotional support. General resources include life essentials such as housing, food, water, air, and income. Social fulfillment describes a person’s ability to interact and engage in activities that allow survival and thriving. Self-management is the autonomous component of social frailty that includes self-determination and motivation necessary to achieve equilibrium among the other social frailty domains and potentially avoid physical frailty.
Figure 1.
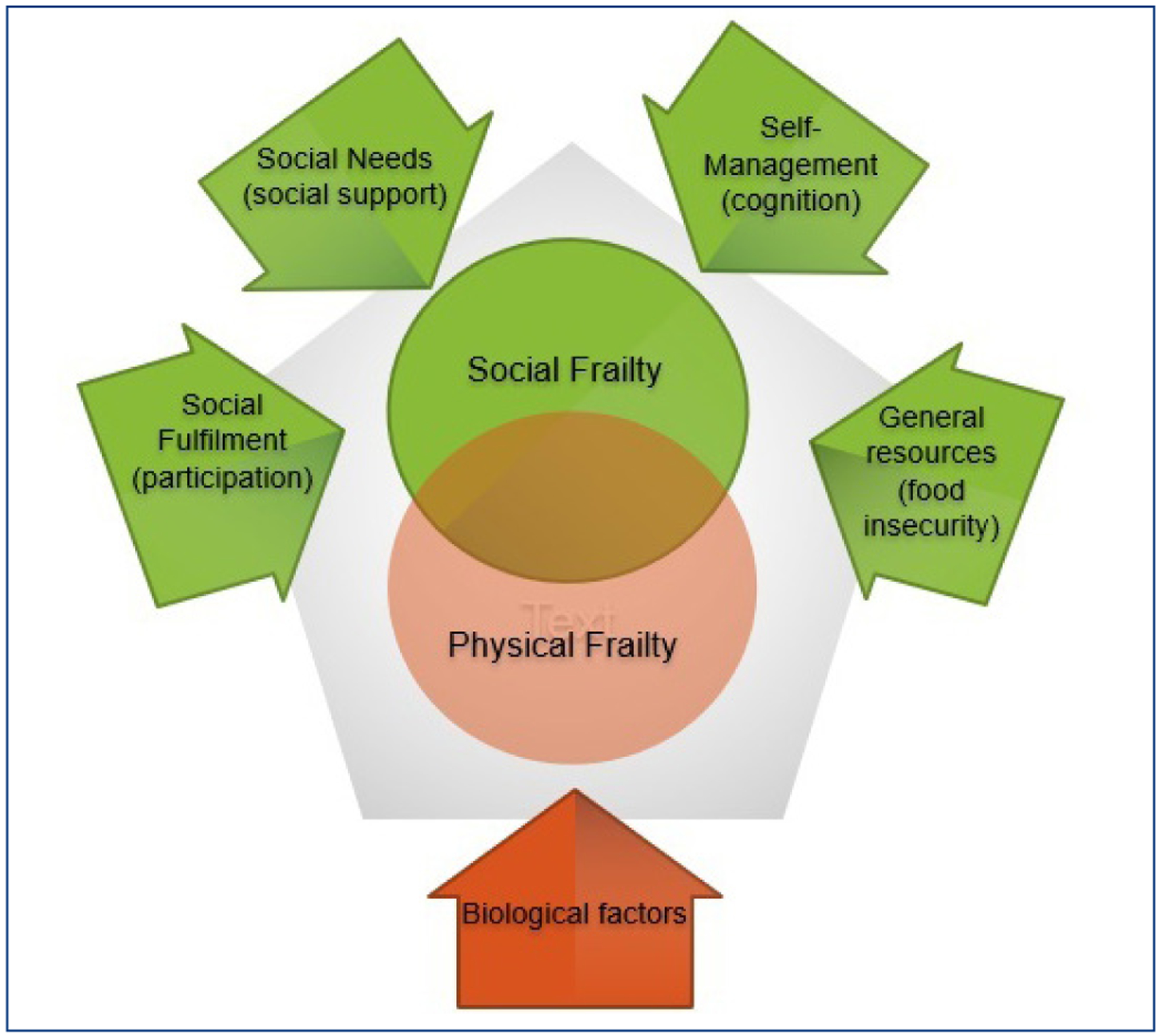
Frailty and social frailty framework
This conceptual framework of social frailty is based on a combination of different theories including: 1) Loneliness Theory,6 which refers to an individuals’ social network and relationships being less satisfactory than expected; 2) The convoy theory of social relations,7 which refers to individuals receiving social support throughout their life by members of their cohort; 3) Self Determination Theory,8 which refers to the status of motivation or autonomy and control, and 4) Social Production Functions Theory,9 which refers to individuals who maximize their psychological and environmental factors or resources for physical and social well-being.
Table 1 describes the relationship between social frailty domains and physical frailty. An analysis conducted by Woo et al. in 2005 found that increasing social support was associated with lower frailty.10 Weight loss from physical frailty phenotype, has been associated with the resource domain of social frailty (occupation, race, gender, and educational level, neighborhood deprivation, and individual socioeconomic status).5,11 The social fulfillment domain highlights that components of frailty such as exhaustion can be associated with depression and slow gait speed leading to reduced social engagement.5,10 Similarly, the self-management domain has a strong relationship with cognitive function and can be associated with weakness, resulting from reduced exercise and poor disease management among people with cognitive impairment.5,11
Table 1.
The relationship between social frailty and physical frailty domains, along with clinical examples.
| Social Frailty Domains | Connection to Physical Frailty Domains | Clinical Example(s) |
|---|---|---|
| Social Needs | Weakness/decreased grip strength | Lack of emotional and social support for daily activities |
| General Resources | Weight loss | Food insecurity results in food vs. housing decision, with housing taking precedence |
| Social Fulfillment | Exhaustion Slow gait speed | Depression leads to reduced social engagement and social participation |
| Self-management | Physical activities | Cognitive impairment results in reduced exercise and disease management leading to further sarcopenia |
Clinical recommendations for integrating frailty and social frailty into treatment
Incorporation of yet another assessment into an already busy clinical practice has potential to benefit patients with physical frailty, but should be accomplished with an eye toward minimizing additional clinical burden. There are components of social frailty that could be built into pre-visit assessments, annual wellness visits, advance care planning, or pre-procedure shared decision making. The purpose would be to facilitate clinical responses when stressors affect the social infrastructure of a patient, rather than simply rote completion of assessment fields. This approach emphasizes that medicine is within the control of the provider.
Table 2 presents a framework for a social frailty checklist with example measures based on a multi-component model of social frailty that includes social isolation, loneliness (social needs), social exercise and participation (social fulfillment), housing, food (resources), behavior, and motivation (self-management). The checklist identifies key elements of social frailty (but is not comprehensive), assessments of the element, and clinical opportunities to complete the assessment. This checklist may assist providers and multidisciplinary teams in coordinating evaluation at the early stages of frailty or addressing frailty in older adults.
Table 2.
Social frailty checklist
| Domain | Element | Assessment | Clinical Assessment Timing |
|---|---|---|---|
| Social Needs | Social Supports | Perceived support when needed12 | Demographic information |
| Loneliness | UCLA loneliness13 | Annual Wellness | |
| General Resources | Food Security | Not able to afford the food in household in the last 12 months14 | Annual Wellness |
| Housing Security | Have any housing problems11 | Annual Wellness | |
| Elder Abuse | Neglect, physical abuse, psychological abuse, financial abuse15 | Annual Wellness | |
| Discrimination | Perceived Discrimination Scale16 | Annual Wellness | |
| Social Fulfillment | Leisure time activities | IADLs17 Internet accessibility |
Introduction to Medicare visit/Annual Wellness |
| Mental Health | PHQ-918 | Annual Wellness | |
| Self-management | Cognitive Function | See AA Cog screening19 | Annual Wellness |
| Care Planning | Physical exercise and Physical Activity Scale for the Elderly (PASE)20 Health care proxy; and instruction directives21 (types of treatment do not want if facing a medical crisis) |
Advance Care Planning |
Clinical research directions
While the physical frailty phenotype has dominated the medical literature, the study of social frailty is less developed.4 The demonstrated association of physical frailty and adverse health outcomes with biological underpinnings strongly suggests that the conceptualizations of physical frailty are appropriate. However, the lack of incorporation of social domains suggests that the overall concept of frailty needs reconsideration. Recent research has systematically examined the association of physical frailty with elements of social frailty domains.11 Additional work is needed to target interventions in social frailty domains using existing infrastructure (e.g., meals on wheels, home, and community-based services, etc.) to determine if modifying social frailty can impact physical frailty. While pharmaceuticals may address biological deficits, larger-scale interventions are necessary to influence social determinants. Fortunately, social support programs could permit or encourage such interventions (e.g., Meals on Wheels, Program of All-Inclusive Care of the Elderly, VA Homeless Programs, State Medicaid home, and community-based services, etc.). Finally, the breadth of social frailty is beyond the ability of a single provider to overcome all aspects. As a result, physicians, providers, researchers, and policymakers should collaborate to find innovations to social frailty that span health systems, social support agencies, and government services.
CONCLUSIONS
Social frailty contributes to reduced resiliency and ability to maintain independence. Using a literature-based conceptual model of social frailty, this manuscript identifies potential opportunities to assess social frailty. Because there is clear overlap between physical and social frailty, integrating a broader and socially-sensitive view of frailty into medical practice may be useful to identify factors that could impact frailty (both physical and social) and maybe amenable to interventions to improve patient outcomes.
Acknowledgments
Dr. LQ was supported in part by grant The National Institutes of Health #1, under grant P2CHD065702, and the National Institutes on Aging #2, the Boston Claude D. Pepper Older Americans Independence Center, under grant P30-AG031679. This work was supported by the VA Health Services Research and Development Center of Innovation in Long Term Services and Supports (CIN 13–419 and C19 20–213), the VA QUERI-Geriatrics and Extended Care Partnered Evaluation Center for Community Nursing Homes (PEC 15–465). The statements and opinions expressed are those of the authors and do not represent the official policy or procedures of the United States Government or the Department of Veterans Affairs.
Footnotes
Financial disclosure
The authors declare that there is no conflict of interest.
Publisher's Disclaimer: Disclaimer
The funding agencies and employers played no role in the content of this paper.
Contributor Information
Lien T. Quach, VA Center of Innovation in Long Term Services, Providence VA Medical Center, Providence, RI; The University of Massachusetts Boston, Department of Gerontology, Boston, MA; Massachusetts Veterans Epidemiology Research and Information Center, VA Boston Healthcare System, Boston, MA..
Jennifer Primack, VA Center of Innovation in Long Term Services, Providence VA Medical Center, Providence, RI; Department of Psychiatry & Human Behavior, Alpert Medical School of Brown University, Providence, RI..
Melanie Bozzay, Department of Psychiatry & Human Behavior, Alpert Medical School of Brown University, Providence, RI; VA RR&D Center for Neurorestoration and Neurotechnology, Providence VA Medical Center, Providence, RI..
Caroline Madrigal, VA Center of Innovation in Long Term Services, Providence VA Medical Center, Providence, RI..
Sebhat Erqou, Department of Medicine, Alpert Medical School of Brown University and Providence VA Medical Center, Providence, RI..
James L. Rudolph, VA Center of Innovation in Long Term Services, Providence VA Medical Center, Providence, RI; Division of Geriatrics and Palliative Medicine, Warren Alpert Medical School of Brown University, Providence, RI; Center for Gerontology and Health Services Research, Brown University School of Public Health, Providence RI..
References
- 1.Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56(3):M146–156. [DOI] [PubMed] [Google Scholar]
- 2.Khandelwal D, Goel A, Kumar U, Gulati V, Narang R, Dey AB. Frailty is associated with longer hospital stay and increased mortality in hospitalized older patients. J Nutr Health Aging. 2012;16(8):732–735. [DOI] [PubMed] [Google Scholar]
- 3.Ahmed N, Mandel R, Fain MJ. Frailty: an emerging geriatric syndrome. Am J Med. 2007;120(9):748–753. [DOI] [PubMed] [Google Scholar]
- 4.Rockwood K, Song X, MacKnight C, et al. A global clinical measure of fitness and frailty in elderly people. Cmaj. 2005; 173(5):489–495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bunt S, Steverink N, Olthof J, van der Schans CP, Hobbelen JSM. Social frailty in older adults: a scoping review. Eur J Ageing. 2017;14(3):323–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dykstra PA. Older adult loneliness: myths and realities. Eur J Ageing. 2009;6(2):91–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Antonucci, Birditt KS, Akiyama H Convoys of social relations: an interdisciplinary approach. In: Bengtson VS, Gans D, Putney NM, & Silverstein M, ed. Handbook of theories of aging. New York: Springer Publishing Company, 2009. [Google Scholar]
- 8.Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol. 2000;55(1):68–78. [DOI] [PubMed] [Google Scholar]
- 9.Ormel J, Lindenberg S, Steverink N, Vonkorff M. Quality of life and social production functions: a framework for understanding health effects. Soc Sci Med. 1997;45(7):1051–1063. [DOI] [PubMed] [Google Scholar]
- 10.Woo J, Goggins W, Sham A, Ho SC. Social determinants of frailty. Gerontology. 2005;51(6):402–408. [DOI] [PubMed] [Google Scholar]
- 11.Bessa B, Ribeiro O, Coelho T. Assessing the social dimension of frailty in old age: A systematic review. Arch Gerontol Geriatr. 2018;78:101–113. [DOI] [PubMed] [Google Scholar]
- 12.Lubben J, Blozik E, Gillmann G, et al. Performance of an abbreviated version of the Lubben Social Network Scale among three European community-dwelling older adult populations. Gerontologist. 2006;46(4):503–513. [DOI] [PubMed] [Google Scholar]
- 13.Hughes ME, Waite LJ, Hawkley LC, Cacioppo JT. A Short Scale for Measuring Loneliness in Large Surveys: Results From Two Population-Based Studies. Res Aging. 2004;26(6):655–672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bishop NJ, Wang K. Food insecurity, comorbidity, and mobility limitations among older U.S. adults: Findings from the Health and Retirement Study and Health Care and Nutrition Study. Prev Med. 2018;114:180–187. [DOI] [PubMed] [Google Scholar]
- 15.Fulmer T Elder abuse and neglect assessment. J Gerontol Nurs. 2003;29(1):8–9. [DOI] [PubMed] [Google Scholar]
- 16.Williams Yu, Jackson Anderson. Perceiced Discrmination Scale. http://sparqtools.org/mobility-measure/perceived-discrimi-nation-scale/. Published 1997. Accessed.
- 17.Graf C The Lawton Instrumental Activities of Daily Living (IADL) Scale. Medsurg Nurs. 2009;18(5):315–316. [PubMed] [Google Scholar]
- 18.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9): 606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Association As. Conitive Assessment Toolkit. https://www.maineddc.org/images/PDFs/Cognitive-Assessment-Toolkit.pdf. Published 2013. Accessed.
- 20.Washburn RA, Smith KW, Jette AM, Janney CA. The Physical Activity Scale for the Elderly (PASE): development and evaluation. J Clin Epidemiol. 1993;46(2):153–162. [DOI] [PubMed] [Google Scholar]
- 21. https://www.nia.nih.gov/health/advance-care-planning-health-care-directives .


