Abstract
Ear- and hearing-related conditions pose a significant global health burden, yet public health policy surrounding ear and hearing care (EHC) in low- and middle-income countries is poorly understood. The present study aims to characterize the inclusion of EHC in national health policy by analysing national health policies, strategies and plans in English, French, Spanish, Portuguese and Arabic. Three EHC keywords were searched, including ear*, hear* and deaf*. The terms ‘human immunodeficiency virus/acquired immunodeficiency syndrome (HIV/AIDS)’, ‘tuberculosis’ and ‘malaria’ were included as comparison keywords as these conditions have historically garnered political priority in global health. Of the 194 World Health Organization Member States, there were 100 national policies that met the inclusion criteria of document availability, searchable format, language and absence of an associated national EHC strategy. These documents mentioned EHC keywords significantly less than comparison terms, with mention of hearing in 15 documents, ears in 11 documents and deafness in 3 documents. There was a mention of HIV/AIDS in 92 documents, tuberculosis in 88 documents and malaria in 70 documents. Documents in low- and middle-income countries included significantly fewer mentions of EHC terms than those of high-income countries. We conclude that ear and hearing conditions pose a significant burden of disease but are severely underrepresented in national health policy, especially in low- and middle-income countries.
Keywords: Health policy, otolaryngology, audiology, otology, hearing
Key messages.
Ear and hearing care (EHC) is under-prioritized in national health policy worldwide.
Low- and middle-income countries (LMICs) are particularly vulnerable to the effects of the exclusion of EHC from health policy.
This disparity represents an opportunity for advocacy for the inclusion of EHC in national health policy, especially in LMICs.
Introduction
Hearing loss is estimated to affect >1.5 billion people worldwide. This increasing burden is projected to affect 2.5 billion people, or 1 in 4, by 2050 (Haile et al., 2021). Hearing loss is detrimental to health. It adversely affects educational attainment, employment and physical and mental health (Emmett and Francis, 2015; Graydon et al., 2019). While children are most susceptible to the negative effects of hearing loss, which include restricted language development and academic achievement (Daud et al., 2010; Hall, 2017), adults with hearing loss are more likely to have higher unemployment rates (Chao et al., 2020).
Access to ear and hearing care (EHC) remains a challenge in low- and middle-income countries (LMICs), where 80% of people with moderate or higher levels of hearing loss reside (Haile et al., 2021). Several barriers prevent access to EHC, including workforce and equipment shortages, lack of funding and social stigma attached to hearing loss. In part, these difficulties stem from gaps in government care provision—particularly in LMICs—where public services are more often limited (Waterworth et al., 2022). The 2021 World Report on Hearing recognized that these barriers to service provision can be averted, calling for a ∼20% increase in coverage of EHC services in LMICs by the year 2030 (World Health Organization, 2021).
To adequately address and remediate a problem of this magnitude, it is essential that EHC is integrated into national health systems through policy development (Olusanya et al., 2014). EHC policy can be established as a distinct framework, such as a national EHC strategy, or it can be included within a country’s overarching national health policies, strategies and plans (NHPSPs). These are policy documents developed in collaboration with the World Health Organization (WHO) to provide country-specific frameworks for addressing national priority health issues (World Health Organization, 2023). NHPSPs provide public health strategies, frameworks for analysing health outcomes and impact indicators to guide future policies. Government policy goals in NHPSPs also guide the budget formulation and funding allocation. As healthcare system planners develop healthcare budget cycles, they often engage with NHPSPs to determine which medical issues are prioritized by a given country (O’Neill et al., 2016).
Opportunities to advance national EHC policy are limited in part by a poor understanding of their inclusion within NHPSPs. A 2013 WHO survey identified only 30 countries with national or subnational EHC strategies and 8 countries with other policies for hearing care (World Health Organization, 2013). Therefore, for countries without dedicated EHC plans, it is most probable that ear- and hearing-related policies would be mentioned in NHPSPs. To our knowledge, there are no studies that have examined the inclusion of EHC in NHPSPs. Therefore, the current state of national EHC policy globally is largely unknown.
This study aims to explore the representation of EHC in NHPSPs across countries lacking formal national EHC plans. We hypothesize that EHC will be under-prioritized in the included NHPSPs and that EHC will be disproportionately under-prioritized in LMICs. By characterizing the current state of EHC prioritization in NHPSPs, we expect to identify opportunities to strengthen EHC around the world and avert suffering due to conditions like hearing loss.
Materials and methods
Selection of keywords
A team of otolaryngology-head and neck surgery clinicians and trainees from five continents generated a list of three keywords relevant to EHC (Table 1). This team included EHC providers practicing around the world, researchers involved in international hearing care initiatives and otolaryngology trainees. These keywords were discussed and determined by consensus to be most reflective of and pertinent to the current EHC public health burden. Human immunodeficiency virus/acquired immunodeficiency syndrome (HIV/AIDS), tuberculosis and malaria were included as comparison conditions. These were selected because they are three major threats to health and have been identified by the United Nations Sustainable Development Goals as priorities for public health interventions and funding (United Nations General Assembly, 2015). For NHPSPs that were not in English, keywords were translated by native speakers of Spanish, Portuguese, Arabic and French (Table S1).
Table 1.
Number of ear and hearing care keyword mentions in NHPSPs
| Term | Total mentions, n | Policies with no mentions of term, n (%) | Policies with at least one mention of term, n (%) | Policies with at least five mentions of term, n (%) |
|---|---|---|---|---|
| EHC | ||||
| hear* | 28 | 85 (85) | 15 (15) | 1 (1) |
| ear* | 23 | 89 (89) | 11 (11) | 1 (1) |
| deaf* | 4 | 97 (97) | 3 (3) | 0 (0) |
| Non-EHC | ||||
| HIV | 2682 | 8 (8) | 92 (92) | 73 (73) |
| tuberculosis | 1399 | 12 (12) | 88 (88) | 62 (62) |
| malaria | 922 | 30 (30) | 70 (70) | 47 (47) |
Data collection and data extraction
The most recent NHPSP for each country was obtained through the WHO’s Country Planning Cycle Database (World Health Organization, 2022a). Documents were included if they were written in Arabic, English, French, Spanish and Portuguese. NHPSPs were excluded if they were not searchable by word processing software (most commonly Microsoft Word or Preview). Additionally, NHPSPs were excluded if the authoring country had a standalone national EHC strategy (Figure 1).
Figure 1.
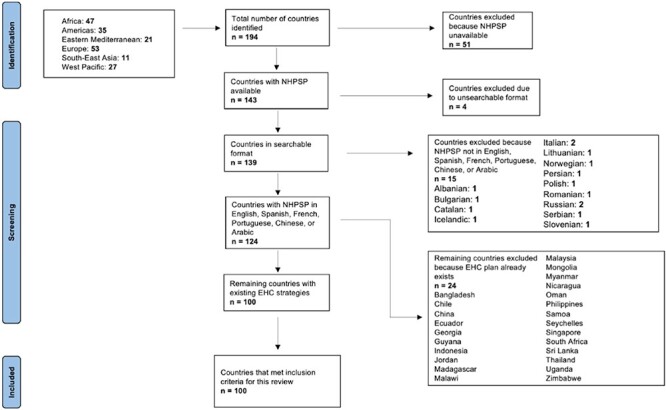
A flow diagram of the inclusion and exclusion of articles
NHPSPs were searched for the three EHC keywords and the three comparison keywords using the word processing software search function. Reviewers attended data collection training sessions that provided standardized instructions before beginning document searches. In each document, reviewers counted the number of sentences that contained each keyword. For example, the sentence ‘Hearing loss is a large problem, with several children reporting diminished hearing’ would count as a single mention of the word ‘hearing’. Only keywords used in the context of otolaryngology were counted. A primary reviewer conducted the initial search and tallied the number of mentions. These counts were then validated independently by a secondary reviewer. Any discrepancies were discussed until a consensus between the two reviewers was reached.
While this metric (number of mentions) does not measure political priority nor the extent of policy implementation, it serves as a means to broadly assess the representation of a topic in policy. This methodology has been adapted from those of prior studies to analyse the representation of medical disciplines (e.g. paediatric surgery) in NHPSPs (Citron et al., 2016; Landrum et al., 2021).
Variable characterization and statistical analysis
Countries, regions and income levels were classified based on WHO regions and World Bank income groups (The World Bank, 2022; World Health Organization, 2022b). We built two multivariable negative binomial regression models assessing mean mentions per EHC keyword (Model 1A) and mean mentions per comparison keyword (Model 1B). In each model, WHO region and World Bank income group were applied as covariates. We also constructed an additional negative binomial regression model (Model 2) assessing mean mentions per keyword with keyword type (EHC vs non-EHC) as the primary independent variable of interest while controlling for WHO region and World Bank income group. Negative binomial regression was employed because the outcome is a count variable with a right-skewed distribution. For Model 2, multilevel regression modelling was initially attempted, given within-subject comparison. However, the intraclass correlation approached 0, and the design effect approached 1. Hence, we reverted back to single-level modelling as described earlier. Statistical significance was assessed as two-tailed, α = 0.05. All analyses were conducted using Stata, Version 17 (StataCorp. 2021, Stata Statistical Software: Release 17, StataCorp LLC, College Station, TX).
Results
Of the 194 WHO Member States, 143 NHPSPs were available and obtained. NHPSPs from 19 countries were excluded for the following reasons: 15 were in a language not within our team’s translation capabilities and 4 were in a format that could not be searched electronically. Of the 124 that remained, 24 countries were excluded because they had existing national standalone EHC strategies. A total of 100 NHPSPs were included in the analysis. An overview of NHPSPs that met inclusion criteria is shown in Figure 1, and further detail is presented in Table S2.
Of the EHC keywords, ‘hear*’ was the most frequent keyword with 28 mentions among 15 (15%) NHPSPs. ‘Ear’ had 23 mentions among 11 (11%) documents, and ‘deaf*’ had 4 mentions among 3 (3%) documents.
In comparison, HIV/AIDS had 2682 mentions among 92 (92%) documents; tuberculosis had 1399 mentions among 88 (88%) documents and malaria had 922 mentions among 70 (70%) documents. Holding WHO region and income group constant, the average mentions per comparison keyword [adjusted mean 16.8, 95% confidence interval (C.I.) 14.7–18.9] was significantly higher than the average mentions per EHC keyword (adjusted mean 0.1, 95% C.I. 0.1–0.3; incidence rate ratio (IRR) 0.01, 95% C.I. 0.01–0.02; Table 2). A summary of the total mentions of EHC and non-EHC terms, as well as the number of policies that mention them, is shown in Figure 2.
Table 2.
Multivariable negative binomial regression for average mentions per keyword
| Negative binomial regression | ||
|---|---|---|
| Outcome: mean mentions per keyword | ||
| IRR [95% C.I.] | P | |
| Keyword | ||
| Comparison | Reference | |
| Ear and hearing care | 0.01 [0.01, 0.02] | <0.001 |
| WHO region | ||
| African region | Reference | |
| Region of the Americas | 0.74 [0.49, 1.14] | 0.17 |
| Eastern Mediterranean region | 0.48 [0.30, 0.79] | <0.001 |
| European region | 0.65 [0.40, 1.04] | 0.08 |
| South-East Asian region | 0.54 [0.27, 1.06] | 0.07 |
| Western Pacific region | 0.54 [0.34, 0.88] | 0.01 |
| World Bank income group | ||
| High-income country | Reference | |
| Upper-middle-income country | 1.54 [1.00, 2.37] | 0.05 |
| Lower-middle-income country | 1.37 [0.88, 2.13] | 0.17 |
| Low-income country | 1.44 [0.83, 2.48] | 0.19 |
Findings that were statistically significant (P < 0.05) are shown in bold.
Figure 2.
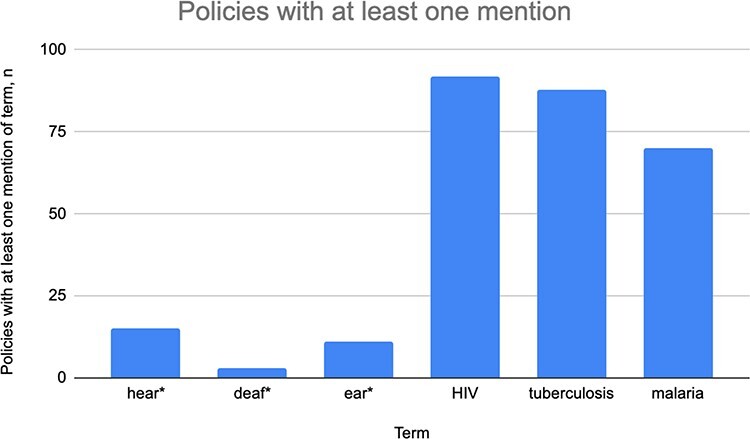
The number of policies mentioning EHC and non-EHC terms at least once
Note: An asterisk after a term denotes that the word can end with any suffix (e.g. ‘hear*’ includes ‘hear’, ‘hears’ and ‘hearing’).
Results from the stratified multivariable analyses by keyword category are presented in Table 3. Mean mentions per EHC keyword did not differ significantly across income groups and WHO regions. Compared with the NHPSPs of countries in the African region, the NHPSPs of countries in the Western Pacific Region (IRR 0.56, 95% C.I. 0.34–0.92), South-East Asian Region (IRR 0.42, 95% C.I. 0.22–0.82) and Eastern Mediterranean Region (IRR 0.51, 95% C.I. 0.31–0.85) had significantly higher mentions per comparison keyword. The NHPSPs of upper-middle-income countries also had higher mentions per EHC keyword than did NHPSPs of high-income countries (IRR 1.61, 95% C.I. 1.03–2.51).
Table 3.
Stratified multivariable negative binomial regression for average mentions per keyword by category
| Negative binomial regression | ||||
|---|---|---|---|---|
| Outcome: mean mentions per EHC keyword | Outcome: mean mentions per comparison keyword | |||
| IRR [95% C.I.] | P | IRR [95% C.I.] | P | |
| WHO region | ||||
| African region | Reference | Reference | ||
| Region of the Americas | 0.48 [0.12, 1.97] | 0.31 | 0.77 [0.50, 1.20] | 0.26 |
| Eastern Mediterranean region | 0.17 [0.01, 2.44] | 0.19 | 0.51 [0.31, 0.85] | 0.01 |
| European region | 0.22 [0.03, 1.84] | 0.16 | 0.69 [0.42, 1.14] | 0.15 |
| South-East Asian region | 2.312 [0.59, 9.12] | 0.23 | 0.42 [0.22, 0.82] | 0.01 |
| Western Pacific region | 0.40 [0.07, 2.22] | 0.29 | 0.56 [0.34, 0.92] | 0.02 |
| World Bank income group | ||||
| High-income country | Reference | Reference | ||
| Upper-middle-income country | 0.67 [0.15, 3.03] | 0.61 | 1.61 [1.03, 2.51] | 0.04 |
| Lower-middle-income country | 0.44 [0.08, 2.31] | 0.33 | 1.47 [0.93, 2.31] | 0.10 |
| Low-income country | 0.15 [0.02 1.46] | 0.10 | 1.68 [0.96, 2.95] | 0.07 |
Findings that were statistically significant (P < 0.05) are shown in bold.
Discussion
Despite hearing loss being the third greatest cause of years lived with disability (Lisan et al., 2022), this study found that EHC keywords were not frequently mentioned in NHPSPs. The most frequently mentioned EHC-related terms were ‘hear*’, which appeared 28 times across 15 policy documents, and ‘ear*’, which appeared 23 times among 11 documents. ‘Deaf*’ appeared only four times among three documents. EHC keywords were infrequently mentioned across all income settings and geographic regions.
The limited literature on national EHC policy aligns with these findings. Although the 1995 World Health Assembly Resolution 48.9 called for WHO Member States to ‘prepare national plans for the prevention and control of major causes of avoidable hearing loss’ (World Health Assembly, 1995), unpublished WHO data from ∼20 years later indicated that only 30 countries had national or subnational EHC strategies. While 83% of respondents from countries lacking a national EHC policy agreed that there was adequate political support to develop such policies, several barriers were reported to limit policy development, including the prioritization of other health issues and a poor general understanding of the national burden of EHC conditions. The authors recommended national and international advocacy to strengthen political support for national EHC policy to overcome these barriers (World Health Organization, 2013).
This study suggests that these barriers persist and contribute to the poor inclusion of EHC in national health policy. Barriers to policy development need to be analysed through stakeholder analysis and qualitative research on political priority, as has been done in global surgery, oral health and other fields (Shiffman and Smith, 2007; Benzian et al., 2011; Shawar et al., 2015). These studies could then identify opportunities to advance priority for national EHC policy at the global, regional and national levels alike.
As members of the EHC field begin to address these knowledge gaps, research must be designed with key stakeholders, including policymakers, funders, civil society organizations and research experts in mind, in order to strategically gather a range of views and opinions. Shiffman and Shawar (2022) describe relevant framing processes; e.g. moralization may be used to garner support from civil society organizations and grassroots advocates by linking EHC with social justice and human rights causes. Another effective framing process is technification, which can be used to motivate experts, such as otolaryngologists, audiologists and researchers by presenting the burden of ear and hearing conditions as solvable problems. As Shiffman and Shawar (2022) point out, the framing of global health issues is often disproportionately influenced by those with power. Moving forward, experts with EHC experience in diverse settings must be included in framing processes. Historically, these stakeholders have been broadly excluded from health policy and systems research, but they often have knowledge that is often not shared by those with more power (Shroff et al., 2017).
Despite the findings of this study, there is renewed enthusiasm for EHC policy in LMICs, with novel tools that can facilitate the policymaking process (Chadha and Stevens, 2013). Wilson et al. (2019) reported that hearing loss is now receiving unprecedented attention, as evidenced by the Lancet Commission on Global Hearing Loss, marking an increase in momentum for EHC in global health policy (Wilson et al., 2019). The World Report on Hearing (World Health Organization, 2021) presents a package of evidence-based interventions for holistic EHC provision that can be delivered through health systems. The interventions are represented by the acronym HEAR: ‘hearing screening and intervention, ear disease prevention and management, access to technologies, and rehabilitation services’ across an individual patient’s lifespan (World Health Organization, 2021). Tordrup et al. (2022) report that scaling up these interventions over 10 years to cover 90% of the global population’s needs would require a USD238.8 billion investment. Per their calculations, this could avert >130 million disability-adjusted life-years worldwide, which corresponds to a monetary value of more than USD1.3 trillion, in addition to productivity benefits of more than USD2 trillion.
Recent successes show that prioritization of EHC by national governments can lead to timely, context-specific national strategies, and the WHO has developed tools to facilitate this. For example, over the past 6 years, the Kenyan and Pakistani governments have developed national EHC policy to address preventable hearing loss (World Health Organization, 2015a,b). As more countries develop EHC policy, resources such as the WHO situational analysis tool and the manual for the planning and monitoring of national strategies will be valuable in approaching policy development in a systematic manner (World Health Organization, 2015a).
This study is subject to some limitations. It is important to note that some nations, such as the UK, are committed to EHC research and care but might not have dedicated EHC documents or NHPSPs. Because such countries were excluded from the present analysis, it is possible that the data here do not represent the most comprehensive depiction of the current EHC landscape. Similarly, several recent efforts have promoted national EHC strategies, so there may be recently developed national EHC strategies that were not included in this analysis. This could result in the inclusion of NHPSPs in the present analysis despite the existence of a standalone national EHC strategy. However, there is no current comprehensive list of signed national EHC strategies to our knowledge. Furthermore, only NHPSPs in English, French, Spanish, Portuguese and Arabic were included. Therefore, this analysis does not characterize trends in EHC keywords across documents in other languages. Finally, the metric used in this study (number of mentions) relies on a predetermined set of keywords. If the NHPSPs that were analysed included other EHC-related terms, this could have resulted in underestimating EHC inclusion. Despite this limitation, this study notes poor overall inclusion of common terms to describe EHC in NHPSPs, which will likely continue to be the case with rarer terms.
Conclusion
There is a poor global representation of EHC in national health policy. This is especially pronounced in national health policies of LMICs, despite a disproportionate burden of ear and hearing conditions. Recent international efforts have incited renewed enthusiasm for the development of national EHC policy, but barriers to these processes remain ill-defined. Further research is necessary to characterize opportunities to advance EHC policy development, and advocacy is urgently needed to support these processes.
Supplementary Material
Acknowledgements
We thank Kee Park, Chitra Chander, Alex Kuo, Shawna Kuo, Fazal Wahid, Touch Sok Davy, Aya Haji Mohamad, Sheng-Po Hao, Nader Zalaquett and Global Otolaryngology-Head and Neck Surgery (OHNS) Initiative.
Contributor Information
Julia Canick, Department of Head and Neck Surgery & Communication Sciences, Duke University Medical Center, Durham, NC 27710, USA.
Beatriz Petrucci, Unified Health System, Ministry of Health, Brasilia, Brazil.
Rolvix Patterson, Department of Head and Neck Surgery & Communication Sciences, Duke University Medical Center, Durham, NC 27710, USA.
James Saunders, Division of Otolaryngology, Dartmouth Hitchcock Medical Center, Lebanon, NH 03766 , USA.
May Htoo Thaw, ORL-HNS Hospital, Mandalay, Myanmar.
Ikeoluwa Omosule, Department of Otorhinolaryngology, University of Abuja Teaching Hospital, Gwagwalada, Abuja, Nigeria.
Alexa Denton, Department of Otolaryngology, Herbert Wertheim College of Medicine, Florida International University, Miami, FL 33199, USA.
Mary Jue Xu, Department of Otolaryngology—Head and Neck Surgery, UCSF, San Francisco , CA 94143, USA.
Shelly Chadha, Department for Management of Noncommunicable Diseases, Disability, Violence and Injury Prevention, World Health Organization, Geneva, Switzerland.
Gabrielle Young, College of Medicine, Medical University of South Carolina, Charleston, SC 29425, USA.
Lyna Siafa, Faculty of Medicine, McGill University, Montreal, QC H3A 0G4, Canada.
Olivier Mortel, Hôpital de l'Université d'état d'Haïti, Port-au-Prince, Haiti.
Alizeh Shamshad, Warren Alpert Medical School of Brown University, Providence, RI 02903, USA.
Ashwin Reddy, Johns Hopkins School of Medicine, Baltimore, MD 21205, USA.
Monet McCalla, Ohio University Heritage College of Osteopathic Medicine, Athens, OH 45701, USA.
Kavita Prasad, Tufts University School of Medicine, Boston, MA 02111, USA.
Hong-Ho Yang, UCLA Medical School, Los Angeles, CA 90095, USA.
Debbie R Pan, Department of Head and Neck Surgery & Communication Sciences, Duke University Medical Center, Durham, NC 27710, USA.
Jaffer Shah, Weill Cornell Medicine, New York, NY 10021, USA.
Emily Smith, Duke Global Health Institute, Durham, NC 27710, USA; Department of Surgery, Duke University, Durham, NC 27710, USA.
Blake Alkire, Department of Otolaryngology—Head and Neck Surgery, Massachusetts Eye and Ear, Boston, MA 02114, USA.
Titus Ibekwe, Department of Otorhinolaryngology, University of Abuja Teaching Hospital, Gwagwalada, Abuja, Nigeria.
Chris Waterworth, Disability Inclusion for Health and Development, Nossal Institute for Global Health, University of Melbourne, Melbourne, VIC, Australia; Audiology and Speech Pathology, University of Melbourne Faculty of Medicine, Dentistry, & Health Sciences, Carlton, VIC, Australia.
Supplementary data
Supplementary data are available at Health Policy and Planning online.
Data availability
The data underlying this article are available in the Duke Research Data Repository. This can be found at DOI https://doi.org/10.7924/r4jw8j211.
Funding
R.P. is supported by the National Institutes of Health (NIH) National Institute on Deafness and Other Communication Disorders (NIDCD) grant [grant number R25DC020172]. This project received no other funding.
Author contributions
J.C., R.P., M.J.X., S.C., E.S. and K.P. participated in the conception or design of the work.
J.C., B.P., M.H.T., I.O., A.D., G.Y., L.S., O.M., A.S., A.R., M.M., D.R.P. and J.S. participated in data collection.
J.C., R.P., M.J.X. and H.-H.Y. participated in the data analysis and interpretation.
J.C., B.P., R.P., M.H.T., M.J.X. and C.W. participated in drafting the article.
J.S., I.O., A.D., S.C., G.Y., L.S., O.M., A.S., A.R., M.M., K.P., H.-H.Y., D.R.P., J.S., E.S., B.A. and T.I. participated in critical revision of the author.
J.C., B.P., R.P., J.S., M.H.T., I.O., A.D., M.J.X., S.C., G.Y., L.S., O.M., A.S., A.R., M.M., H.-H.Y., D.R.P., J.S., E.S., K.P., B.A., T.I. and C.W. provided the final approval of the version to be submitted.
Reflexivity statement
The authors of this study include 14 females and 9 males spanning a wide range of experience and expertise. The authors include 15 otolaryngology trainees, 5 otolaryngology clinicians and 3 health systems researchers, many of whom have significant experience in the study of OHNS care in the global health setting. Included authors represent 7 countries (3 of which are LMICs) and 10 language proficiencies.
Ethical approval
This analysis uses public data without the requirement of ethical approval from an institution.
Conflict of interest
There are no conflicts of interest reported by the authors.
References
- Benzian H, Hobdell M, Holmgren C et al. 2011. Political priority of global oral health: an analysis of reasons for international neglect. International Dental Journal 61: 124–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chadha S, Stevens G. 2013. Editorial: promoting ear and hearing care: the WHO perspective. The Hearing Journal 66: 2. [Google Scholar]
- Chao P, Huang S, Escorpizo R et al. 2020. Effects of hearing disability on the employment status using WHODAS 2.0 in Taiwan. IJERPH 17: 9374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Citron I, Chokotho L, Lavy C. 2016. Prioritisation of surgery in the national health strategic plans of Africa: a systematic review. World Journal of Surgery 40: 779–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daud MKM, Noor RM, Rahman NA, Sidek DS, Mohamad A. 2010. The effect of mild hearing loss on academic performance in primary school children. International Journal of Pediatric Otorhinolaryngology 74: 67–70. [DOI] [PubMed] [Google Scholar]
- Emmett SD, Francis HW. 2015. The socioeconomic impact of hearing loss in U.S. adults. Otology & Neurotology: Official Publication of the American Otological Society, American Neurotology Society [And] European Academy of Otology and Neurotology 36: 545–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graydon K, Waterworth C, Miller H, Gunasekera H. 2019. Global burden of hearing impairment and ear disease. The Journal of Laryngology and Otology 133: 18–25. [DOI] [PubMed] [Google Scholar]
- Haile LM, Kamenov K, Briant PS et al. 2021. Hearing loss prevalence and years lived with disability, 1990–2019: findings from the Global Burden of Disease Study 2019. The Lancet 397: 996–1009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall WC. 2017. What you don’t know can hurt you: the risk of language deprivation by impairing sign language development in deaf children. Maternal and Child Health Journal 21: 961–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landrum K, Cotache-Condor CF, Liu Y et al. 2021. Global and regional overview of the inclusion of paediatric surgery in the national health plans of 124 countries: an ecological study. BMJ Open 11: e045981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lisan Q, Goldberg M, Lahlou G et al. 2022. Prevalence of hearing loss and hearing aid use among adults in France in the CONSTANCES study. JAMA Network Open 5: e2217633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olusanya BO, Neumann KJ, Saunders JE. 2014. The global burden of disabling hearing impairment: a call to action. Bulletin of the World Health Organization 92: 367–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Neill K, Viswanathan K, Celades E, Borma T. 2016. Strategizing National Health in the 21st Century: A Handbook. Copenhagen: World Health Organization Regional Office for Europe. [Google Scholar]
- Shawar YR, Shiffman J, Spiegel DA. 2015. Generation of political priority for global surgery: a qualitative policy analysis. The Lancet Global Health 3: e487–95. [DOI] [PubMed] [Google Scholar]
- Shiffman J, Shawar YR. 2022. Framing and the formation of global health priorities. The Lancet 399: 1977–90. [DOI] [PubMed] [Google Scholar]
- Shiffman J, Smith S. 2007. Generation of political priority for global health initiatives: a framework and case study of maternal mortality. The Lancet 370: 1370–9. [DOI] [PubMed] [Google Scholar]
- Shroff ZC, Javadi D, Gilson L, Kang R, Ghaffar A. 2017. Institutional capacity to generate and use evidence in LMICs: current state and opportunities for HPSR. Health Research Policy and Systems 15: 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tordrup D, Smith R, Kamenov K et al. 2022. Global return on investment and cost-effectiveness of WHO’s HEAR interventions for hearing loss: a modelling study. The Lancet Global Health 10: e52–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United Nations General Assembly . 2015. 70/1: Transforming our world: the 2030 Agenda for Sustainable Development. http://www.un.org/ga/search/view_doc.asp?symbol=A/RES/70/1&Lang=E.
- Waterworth CJ, Marella M, O’Donovan J et al. 2022. Barriers to access to ear and hearing care services in low- and middle- income countries: a scoping review. Global Public Health 17: 1–25. [DOI] [PubMed] [Google Scholar]
- Wilson BS, Tucci DL, O’Donoghue GM, Merson MH, Frankish H. 2019. A Lancet Commission to address the global burden of hearing loss. Lancet (London, England) 393: 2106–8. [DOI] [PubMed] [Google Scholar]
- The World Bank . 2022. World Bank Country and Lending Groups. https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups.
- World Health Assembly . 1995. WHA 48.9: Prevention of hearing impairment. Geneva: World Health Organization. https://apps.who.int/iris/handle/10665/178405. [Google Scholar]
- World Health Organization . 2013. Multi-Country Assessment of National Capacity to Provide Hearing Care. Geneva, Switzerland. https://www.who.int/publications/i/item/9789241506571. [Google Scholar]
- World Health Organization . 2015a. Ear and Hearing Care: Planning and Monitoring of National Strategies: A Manual. Geneva: World Health Organization. [Google Scholar]
- World Health Organization . 2015b. Ear and Hearing Care: Situation Analysis Tool. Geneva: World Health Organization. [Google Scholar]
- World Health Organization . 2021. World Report on Hearing. Geneva: World Health Organization. [Google Scholar]
- World Health Organization . 2022a. Country Planning Cycle Database. https://extranet.who.int/countryplanningcycles/.
- World Health Organization . 2022b. Countries overview. https://www.who.int/countries.
- World Health Organization . 2023. Supporting National Health Policies, Strategies, Plans. https://www.who.int/activities/supporting-national-health-policies-strategies-plans.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article are available in the Duke Research Data Repository. This can be found at DOI https://doi.org/10.7924/r4jw8j211.


