Abstract
It is essential to achieve herd immunity in order to control the COVID-19 pandemic, and this requires a high level of vaccination rate. Despite the importance of vaccination, hesitancy and unwillingness in receiving the COVID-19 vaccine still exists. It is therefore crucial to comprehend the intentions of adults regarding COVID-19 vaccination, which is beneficial for establishing community immunity and an efficient future pandemic response. An online survey was administered to 2722 adults in Vietnam. Cronbach's alpha, exploratory factor analysis (EFA), and confirmatory factor analysis (CFA) were used to test the reliability and validity of the developed scales. Then, structural equational modeling (SEM) was employed to test correlations. This study found that favorable attitudes toward COVID-19 vaccines played the most important role in shaping adults' intention to receive these vaccines, followed by perceived behavioral control, perceived benefits of COVID-19 vaccines, and subjective norms. Concurrently, all three core dimensions of the theory of planned behavior mediated the link between the perceived benefits of COVID-19 vaccines and the intention to receive them. Also, there were significant differences between males and females in the way they formed this intention. The findings of this study offer valuable guidance for practitioners on how to encourage adults to receive COVID-19 vaccinations, as well as how to limit the transmission of the COVID-19 virus.
Keywords: COVID-19 vaccination intention, Perceived benefits of COVID-19 vaccines, Theory of planned behavior
1. Introduction
The emergence of the novel coronavirus disease 2019 (COVID-19) was initially observed in Wuhan city, China, in late 2019, and it rapidly spread to become a global pandemic [[1], [2], [3]]. Confirmed cases and deaths have been reported in over 200 countries worldwide. According to the World Health Organization (WHO)'s report as of May 23, 2023 by that point there had been over 766 million cumulative cases and over 6.9 million deaths globally due to COVID-19 [4]. This pandemic has resulted in significant losses and widespread socioeconomic distress across the globe [5,6].
Since the early phase of the COVID-19 pandemic, a number of measures have been applied and practiced in attempts to restrain and contain the spread of the COVID-19 infection; these include social distancing, hand washing, face-mask wearing, border shutdowns, quarantine, and travel restrictions, among others [[7], [8], [9], [10], [11]]. As part of the ongoing measures to restrict the spread of the COVID-19 pandemic, vaccination played a crucial role in curbing and resolving the COVID-19 pandemic [[12], [13], [14]]. Thus, shortly after the outbreak of the disease was declared, there was an urgent call for COVID-19 vaccine research and development by the WHO [15]. The COVID-19 pandemic has spurred unprecedented efforts in vaccine research [[16], [17], [18]] and development in terms of speed and scale, resulting in the approval of several vaccines by the WHO, such as Moderna, Pfizer/BioNTech, and AstraZeneca [12]. Despite this progress, vaccine hesitancy remained a widespread issue [17,19], with vaccine refusal observed globally, hindering the high vaccination rates necessary to achieve herd immunity [20]. Failure to achieve this level of immunity due to vaccine refusal could impede COVID-19 containment [21]. Therefore, understanding people's intentions regarding COVID-19 vaccination was crucial for a successful vaccination campaign [3,22]. A body of research has been conducted in different countries, such as Hong Kong [22,23], the USA [11], Turkey [24], Canada [15], China [10,25] and many others [26,27]. These studies have explored the problems related to COVID-19 vaccine hesitancy and intentions. However, COVID-19 vaccination intentions and hesitancy have received scant attention in Southeast Asian countries, including Vietnam [12].
The theory of planned behavior (TPB) [28] has been considered to be one of the most influential theories that has been widely implemented to explain human behaviors [29], including behaviors related to COVID-19 vaccination [3,17,22]. Table 1 presented a concise summary of the findings from previous studies which applied the TPB to explain intentions/willingness to receive COVID-19 vaccines. In these studies, perceived benefits, an important dimension of the HBM, were integrated to be one of the most important predictors of intention to receive COVID-19 vaccines [22,[30], [31], [32], [33]], validating for the application of the TPB to explain how perceived benefits of COVID-19 vaccines affect COVID-19 vaccination intentions. In other words, our study aims to adopt the TPB to investigate the role of the perceived benefits of COVID-19 vaccines on attitudes towards COVID-19 vaccination (or attitudes), subjective norms, perceived behavioral control (perceived behavioral control), and COVID-19 vaccination intention among Vietnamese adults.
Table 1.
Empirical contributions on applying the TPB to explain COVID-19 vaccination intention.
| Authors (years) | Sampling and countries | Main influential factors | Remarks/key findings |
|---|---|---|---|
| Li, Lau [22] | 11,141 parents, Hong Kong | Demographics, perceived susceptibility, perceived benefits, perceived barriers, cues to actions, attitudes, subjective norms, perceived behavioral control | higher levels of perceived susceptibility to COVID-19, perceived benefits, positive attitudes, subjective norms and lower levels of perceived barriers increased the level of COVID-19 vaccination intentions |
| Hayashi, Romanowich [34] | 172 adult residents, United States | Demographic variables, attitudes, subjective norms, perceived behavioral control, locus of control, community benefit | Perceived behavioral control, attitude, and perceived community benefit are considered unique predictors |
| Wang, Li [35] | 214 older adults, China | Perceived severity, perceived vulnerability, self-efficacy, response efficacy, response cost, attitudes, subject norms | Self-efficacy, subjective norms, perceived severity, and perceived vulnerability are determined as facilitator while response cost is identified a great obstacle |
| Ong, Prasetyo [32] | 865 young adults, Philippines | Understanding of COVID-19 vaccine, self-efficacy, cues to action, perceived barriers, perceived benefit, perceived side-effects, attitude, perceived behavioral control, subjective norms | Understanding of the COVID-19 vaccines is the strongest predictor, followed by perceived barriers and perceived benefits |
| Shmueli [33] | 398 adults, Israel | Social-demographic variables, health-related variables, HBM variables, and TPB variables | Intention to receive COVID-19 vaccines are sufficiently explained by integrating the variables of the HBM and the TPB |
| Ullah, Lin [36] | 1034 young adults, Pakistan | Perceived infectability, attitude, subjective norms, perceived behavioral control, and fear of COVID-19 | Attitude, subjective norms, perceived behavioral control, and fear of COVID-19 significantly mediate the relationship between perceived infectibility and COVID-19 vaccination intentions |
| Seddig, Maskileyson [37] | 5044 adults, Germany | Fear of COVID-19, skepticism toward doctors and vaccines, COVID-19 conspiracy beliefs, trust variables and demographic variables | Attitude is the best predictor while normative and control beliefs did not predict COVID-19 vaccination intentions. Positive attitudes were bolstered by trust and fear of COVID-19 whilst negative attitudes were linked to acceptance of conspiracy theories and skepticism. |
Vietnam has been identified as a suitable country for collecting data and applying the TPB to investigate how perceived benefits of COVID-19 vaccines can enhance the core components of the TPB and COVID-19 vaccination intention for the following reasons. Firstly, the effectiveness of the 5 K approach (Khẩu trang: mask wearing, Khử khuẩn: disinfection, Khoảng cách: social distancing, Không tụ tập đông người: No gatherings, and Khai báo y tế: health declaration) in controlling the spread of COVID-19 during the first three waves has been demonstrated in this country [12,38]. Secondly, during the time of the study, even though Vietnam was developing its own COVID-19 vaccine (Nanocovax), the majority of the Vietnamese population had only received one dose of a COVID-19 vaccine and they were waiting for international support in order to be vaccinated with their second and third doses of the vaccine [12]. Finally, although some prior studies have investigated the willingness to receive COVID-19 vaccines and the acceptance of vaccination in Southeast Asian countries, the results were mixed and inconsistent, and more importantly, these studies did not explore individuals' COVID-19 vaccination intention in the light of the TPB. For example, Duong and Antriyandarti [38] surveyed 2500 respondents in four countries in Southeast Asia (Vietnam, Indonesia, the Philippines, and Malaysia) to examine the role of vaccine brand on individuals' willingness to be vaccinated against COVID-19 with six COVID-19 vaccines. This research revealed that a higher percentage of respondents express willingness to be vaccinated with Pfizer, Moderna, and AstraZeneca vaccines compared to Sinopharm, Janssen, and Sputnik-V vaccines while the influence of influential factors on the willingness to receive vaccination varies in terms of both magnitude and direction, and this variability was dependent on the specific vaccine brands. Moreover, Duong, Nguyen [39] conducted a qualitative study in Vietnam and reported that people's attitudes toward COVID-19 vaccines were mixed and subject to change. These attitudes were not static and were influenced by individuals' risk-benefit self-assessment of vaccination.
1.1. The roles of the three core components in the TPB
The TPB was widely recognized as a significant theoretical framework that has been effectively utilized to research behavioral intentions [40]. According to this social psychology theory, behavioral intentions were a strong predictor of actual behavior [3,41], particularly in the context of reasoned and goal-directed actions [29]. Additionally, the TPB has demonstrated its effectiveness as a reliable predictor of both intentions and the subsequent behaviors related to receiving COVID-19 vaccines [3,22,[42], [43], [44]]. According to the TPB, intentions most closely predicted actual behaviors while behavioral intentions could be identified as a function of three variables: favorable or unfavorable perception and evaluation of a certain behavior (attitude toward behavior); perceptions of social pressure to carry out or not carry out the behavior (subjective norms); and the perception of the ease or difficulty of carrying out the behavior (perceived behavioral control) [40,45]. Some recent studies have also reported that COVID-19 vaccination intention was positively correlated with attitudes towards COVID-19 vaccination, subjective norms, and perceived behavioral control [3,22]. In the context of Vietnam, it was therefore hypothesized that COVID-19 vaccination intention could be positively driven by favorable attitudes towards COVID-19 vaccination (i.e. receiving a COVID-19 vaccine is attractive to me, receiving a COVID-19 vaccine would bring me great satisfaction), subjective norms (i.e., my friends think that I should have the COVID-19 vaccines, my parents think that I should have the COVID-19 vaccines), and perceived behavioral control (i.e., If I try, I can easily access and receive a COVID-19 vaccine).
H1
COVID-19 vaccination intention is positively interrelated with (a) attitudes towards COVID-19 vaccination; (b) subjective norms; and (c) perceived behavioral control.
Some studies that applied the TPB to explain the intention to conduct different behaviors have indicated that subjective norms can have a significant impact on attitudes toward behaviors, and on perceived behavioral control [46,47]. This was because the opinions and approval of surrounding people could increase our favorable perceptions of performing a certain behavior and how easy or difficult we perceive that it will be to carry out this behavior [40]. Moreover, studies have also found that perceived behavioral control can serve as a predictor of attitude toward behaviors [48,49]. Consequently, as well as testing the effect of the three components of the TPB (subjective norms, attitudes towards COVID-19 vaccination, and perceived behavioral control), this research also examined how subjective norms can increase attitudes towards COVID-19 vaccination and perceived behavioral control, as well as how perceived behavioral control could increase attitudes towards COVID-19 vaccination among Vietnamese adults.
H2
Subjective norms are positively interrelated with (a) attitudes towards COVID-19 vaccination and (b) perceived behavioral control.
H3
Perceived behavioral control is positively interrelated with attitudes towards COVID-19 vaccination.
1.2. The role of the perceived benefits of COVID-19 vaccines
Perceived benefits was a component of the HBM [50], which was a crucial theoretical framework that predicted whether an individual would engage in preventive health behavior such as receiving vaccinations, based on their beliefs. These beliefs included perceived susceptibility to the infection/disease, the perceived severity of becoming ill with this disease or infection, the perceived benefits of the behavior, the perceived barriers to carrying it out, and cues to action. According to the HBM, if a person perceived that adopting a specific health behavior would decrease their susceptibility or the severity of a health risk, they were more likely to adopt it, provided that the benefits outweighed the barriers and that they were prompted by internal or external cues [22,32]. Mir, Parveen [44] argued that the perceived BCV was that being vaccinated decreases the risk of becoming severely infected, which could result in a range of health risks and potentially life-threatening consequences. Among individuals who became infected with COVID-19 after receiving the vaccine, the need for hospitalization and medical care was generally lower than among those who have not been vaccinated [31]. Moreover, vaccinations provided social benefits by reducing the spread of COVID-19, thereby safeguarding society from a pandemic [42,51]. The majority of the respondents in Mir and Parveen's study agreed that having the vaccine was a good option for protecting themselves from COVID-19 infection [44]. Therefore, perceived benefits of COVID-19 vaccines could be determined as a central factor of COVID-19 vaccination intention [31,42,52], and the three core dimensions of the TPB also could act as mediators in the link between perceived benefits of COVID-19 vaccines and COVID-19 vaccination intention. The following hypotheses have been formulated to examine the effects of perceived benefits of COVID-19 vaccines on the attitudes towards COVID-19 vaccination, subjective norms, and perceived behavioral control of Vietnamese adults.
H4
Perceived benefits of COVID-19 vaccines are positive interrelated with (a) attitudes towards COVID-19 vaccination; (b) subjective norms; (c) perceived behavioral control; and (d) COVID-19 vaccination intention.
1.3. The role of gender
Males and females tended to behave in different ways as a result of their different paths in the socialization process, according to Gender Socialization Theory [53]. In a recent study, Dou, Yang [3] highlighted that there were notable variances between males and females in terms of their willingness to receive vaccines, with males being more inclined to have vaccines than females. This research tested the moderation effects of gender on the relationships between the TPB components and COVID-19 vaccination intention. In the context of Vietnam, it was hypothesized that the effects of the antecedents on COVID-19 vaccination intention couldbe different for males and females.
H5
There are differences in the impacts of (a) perceived benefits of COVID-19 vaccines, (b) attitudes towards COVID-19 vaccination, (c) subjective norms, and (d) perceived behavioral control on COVID-19 vaccination intention for males and females.
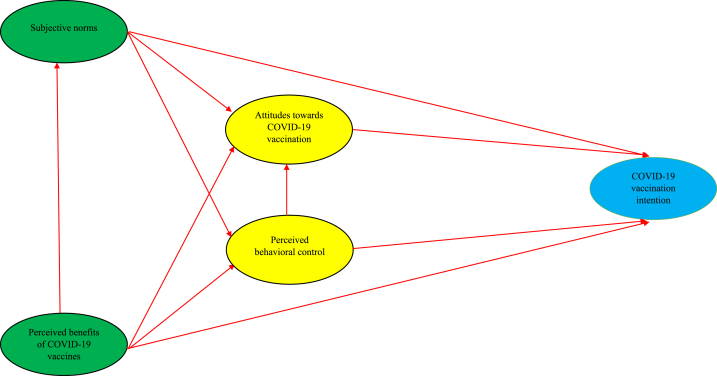
The conceptual framework is illustrated in Fig. 1.
Fig. 1.
Theoretical model.
2. Methods
2.1. Measures
In order to estimate the influences of perceived benefits of COVID-19 vaccines on COVID-19 vaccination intention via the three core components of the TPB, a questionnaire survey was employed in our study to gather the data. All of the measures (scales) used in our study were modified from prior studies. Particularly, the first three-item scale of COVID-19 vaccination intention was taken from the research of Chu and Liu [42], while the remaining items were taken from the research of Mir, Parveen [44], (i.e., “I try to get COVID-19 vaccines”, “My goal is to receive COVID-19 vaccines as soon as possible”). The five-item scale of attitudes towards COVID-19 vaccination (i.e., “Receiving a COVID-19 vaccine implies more advantages than disadvantages to me”) and the five-item scale of perceived behavioral control (i.e., “To receive a COVID-19 vaccine would be easy to me”) was modified from Mir, Parveen [44] and Liñán and Chen [54]. The first two items of the subjective norms scale were adapted from Chu and Liu [42], while the last three items of this scale were modified from Liñán and Chen [54] (i.e., “Most people who are important to me will get vaccinated for COVID-19”). Finally, the seven-item scale of perceived benefits of COVID-19 vaccines was adopted from Chu and Liu [42] and Coe, Elliott [26] (i.e., “COVID-19 vaccines will be effective in preventing COVID-19”, “COVID-19 vaccines are very safe”. All of the observations were scored from 1 to 7, representing “strongly disagree” to “strongly agree”, respectively.
The final section of the questionnaire survey asked for the demographic details of the participants, such as their gender, age, monthly income, and degree of education. As suggested by Lee, Chinna [55], and because the target audience for the survey was Vietnamese adults, all of the questionnaire items were initially translated from English to Vietnamese. Subsequently, to ensure the accuracy of the translation process, two language specialists re-translated the questionnaire items back to English and then compared the two versions.
2.2. Sample and procedure
Our study employed a convenience sampling method and an online-based survey in Vietnam to gather the data between 20 July and October 20, 2021. At that time, Vietnam was going through its fourth significant wave of the COVID-19 pandemic, and various restrictions and social distancing measures were in place [12]. As a result, an online-based survey using Google-Forms was deemed most suitable for collecting data during this period [6]. Our study was conducted in accordance with the Declaration of Helsinki, and it received ethical approval from the Research Ethics Committee of the Faculty of Economics at the College of Economics, Technology and Fisheries, Bac Ninh, Vietnam, and the Department of Research Management, National Economics University, Hanoi, Vietnam, with the reference number of CBQT1.2022.06. Additionally, all of the participants provided informed consent to participate in the survey, with the understanding that their participation was completely voluntary, that they had the option to withdraw from the study at any point they wished, and that the data were intended solely for academic purposes. Furthermore, each participant only had to spend around 15 min completing the questionnaire, and all of their information was kept completely confidential, and any identifying details removed.
Our online survey was distributed directly to personal email addresses and messaging platforms, including Facebook, Zalo, and Viber, to invite potential participants to complete the survey. Ultimately, 2722 individuals completed the questionnaire, resulting in a response rate of 30.2%. The demographic details of the respondents are as follows. Although the majority of the respondents were female (56%), most were aged between 18 and 28 years old, accounting for 60.7% of the total, followed by those aged 29–28 (21.0%), 39–48 (13%), 49–58 (3.8%), and over 59 years old (1.6%). Over half (57.7%) of the respondents reported earning less than 10 million VND per month. In terms of education and marital status, 68.6% of the participants held a bachelor's degree, and 66.3% were single. With regard to vaccine preference, 29.1% of the respondents indicated a preference for the AstraZeneca vaccine, followed by Pfizer (19.5%), Moderna (15.3%), and Sinopharm (6.8%). Finally, 890 respondents reported receiving at least one dose of a COVID-19 vaccine, accounting for 32.7%. In fact, during the time of the study, even though Vietnam was developing its own COVID-19 vaccine (Nanocovax), the majority of the Vietnamese population have still not been vaccinated or only received one-dose of COVID-19 vaccines and were waiting for international support sources in order to be vaccinated with the second and third dose of COVID-19 vaccines [12]. Thus, the concept of “COVID-19 vaccination intention” not only reflects intention to receive the first dose of COVID-19 vaccine, but also shows individuals' intentions to getting vaccinated with the second and third dose of COVID-19 vaccine.
2.3. Analytical approach
In the first step, the reliability and validity of the scales were tested using Cronbach's alpha, exploratory factor analysis (EFA), and confirmatory factor analysis (CFA). The criteria of indices of model fit, standardized regression weight, AVE (Average Variance Extracted) and CR (Composite Reliability) were employed in these analyses, as suggested by some prior studies [[56], [57], [58]]. Additionally, common method bias (CMB) was then used to affirm the absence of a threat to the interpretation of the findings [59]. Next, to examine both direct and indirect associations in the theoretical model, we employed structural equation modeling (SEM) using AMOS 24.0. In this step, we followed the recommendations of Hayes and Matthes [60] to use Gaskin's (2019) plugin with 5000 bootstrapping samples to test the indirect impacts.
3. Results
3.1. Testing normality and scale assessment
All scales showed good internal consistency reliability, with Cronbach's alpha values higher than 0.63 (the lowest value was 0.896) and Corrected Item-Total correlations greater than 0.3 for each observed variable [61] (see Table 2). We conducted an EFA with all the items but found that one item (COVID-19 vaccination intention2 “I actually get vaccinated for COVID-19”) had a factor loading below 0.5 (λCOVID-19 vaccination intention = 0.420). We removed this item and conducted a second EFA, which revealed five factors with a total extracted variance of 73.997%. The KMO value was 0.969, and all items had factor loadings higher than 0.5 [62].
Table 2.
Reliability and discriminant validity of constructs.
| Mean | SD | α | CR | AVE | Bivariate correlations |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | ||||||
| 1. Perceived benefits of COVID-19 vaccines | 5.183 | 1.241 | 0.936 | 0.934 | 0.671 | 0.819 | ||||
| 2. COVID-19 vaccination intention | 4.901 | 1.257 | 0.896 | 0.892 | 0.546 | 0.626** | 0.739 | |||
| 3. Attitudes towards COVID-19 vaccination | 5.195 | 1.323 | 0.933 | 0.930 | 0.726 | 0.714** | 0.698** | 0.852 | ||
| 4. Subjective norms | 5.105 | 1.416 | 0.946 | 0.944 | 0.772 | 0.596** | 0.627** | 0.663** | 0.879 | |
| 5. Perceived behavioral control | 4.657 | 1.374 | 0.914 | 0.914 | 0.681 | 0.527** | 0.625** | 0.587** | 0.556** | 0.825 |
Notes: N = 2722; α: Cronbach's alpha, **p < 0.01.
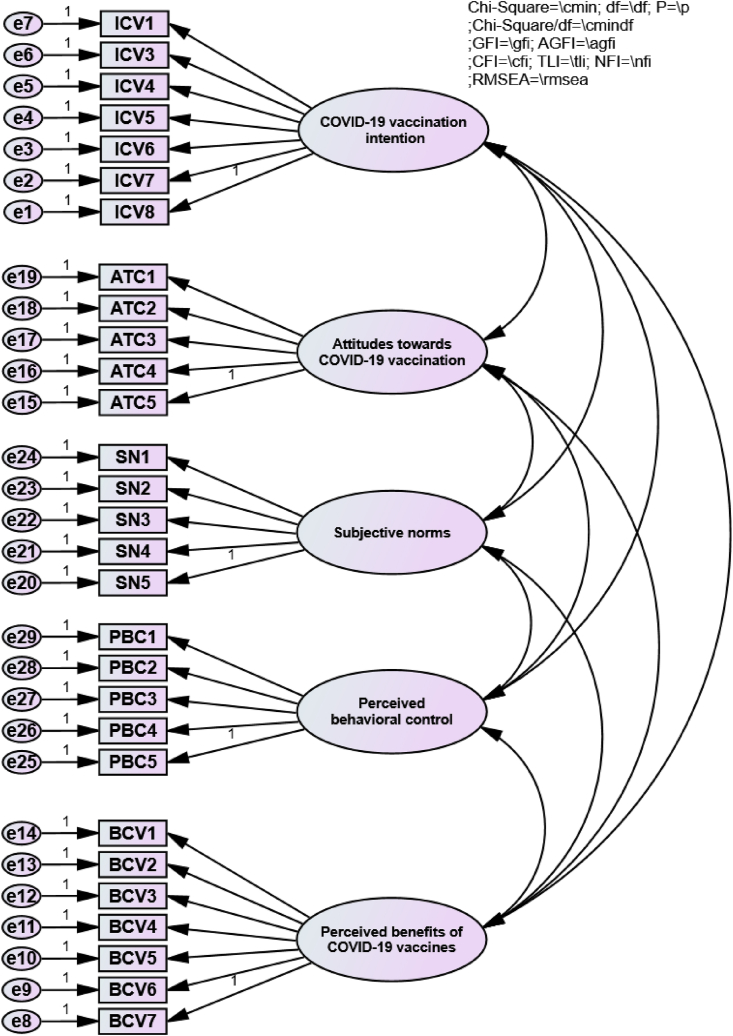
Based on the results of the CFA, the fit indices suggested a good fit between the model and the data (see Fig. 2). The chi-square test was significant (χ2 (355) = 2968.836), but this was often the case with large sample sizes, indicating that other fit indices should be examined. The chi-square/df ratio was 8.363, which is below the recommended threshold of 10, indicating an acceptable fit [63]. The GFI and AGFI indices were both above their respective thresholds of 0.9 and 0.8, indicating a good fit. The CFI, TLI, and NFI indices were all above 0.9, indicating a good fit. Finally, the RMSEA index was 0.052, which was below the recommended threshold of 0.08, indicating a good fit. Table 2 also presented the construct reliability and discriminant validity. The AVE and CR values were also evaluated to test the reliability and validity of the scales. The AVE values were all above 0.5, indicating that each scale accounts for more than 50% of the variance in its respective items [64]. The CR values were all greater than 0.6, indicating high internal consistency reliability [65]. Additionally, the square roots of AVEs were all higher than the inter-construct correlations, indicating good discriminant validity. As a results, all the scales demonstrated their reliability and validity [66].
Fig. 2.
Standardized measurement model for the relationships between observed indicators and the latent variables.
Additionally, as all the participants completed the questionnaires themselves, we used both EFA and CFA analyses to assess whether CMB could affect the interpretation of our results. Initially, we conducted Harman's single-factor test to identify any CMB. The outcome revealed that only 28.63% of the variance was accounted for by the first factor [67]. Moreover, the observed variables of the four constructs were constrained using a single-factor measurement model. However, the results of the single-factor CFA demonstrated that the fitness indices did not meet the desired level of acceptability: χ2 (434) = 23542.781; GFI = 0.524; AGFI = 0.456; CFI = 0.667; TLI = 0.643; NFI = 0.663; RMSEA = 0.140. Consequently, it appeared that CMB did not present a significant issue for the interpretation of our findings [68,69].
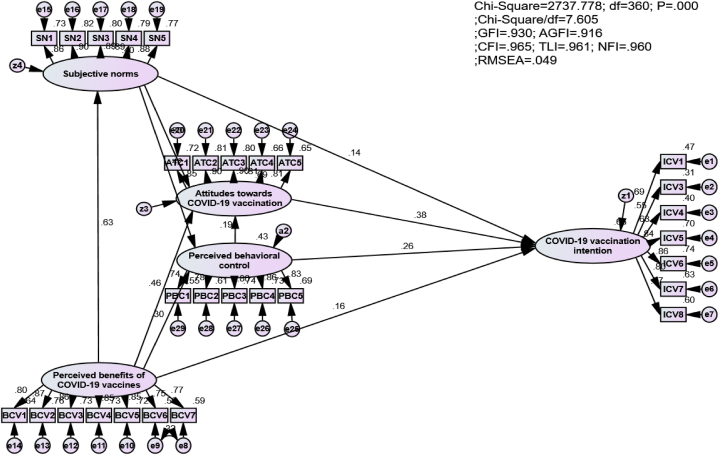
3.2. Structural equation modeling
The results of the SEM analysis indicated that the model achieved a high level of fit (see Fig. 3). To specify, χ2 (360) = 2737.778; Chi-square/df = 7.605; p < 0.01; GFI = 0.930 > 0.9; AGFI = 0.916 > 0.9; CFI = 0.965 > 0.9; TLI = 0.961 > 0.9; and RMSEA = 0.049 < 0.8 [65]. The Square Multiple Correlations (R2) of COVID-19 vaccination intention, attitudes towards COVID-19 vaccination, subjective norms, and perceived behavioral control were 0.665, 0.687, 0.396, and 0.426, respectively. The results of testing the hypotheses were summarized in Table 3. First, the results confirmed that the three core antecedents in the TPB played an important role in shaping COVID-19 vaccination intention. Indeed, COVID-19 vaccination intention was significantly affected by attitudes towards COVID-19 vaccination (H1a: β = 0.344; p-value <0.001), subjective norms (H1b: β = 0.121; p-value <0.001) and perceived behavioral control (H1c: β = 0.215; p-value <0.001). In addition, subjective norms were significantly associated with attitudes towards COVID-19 vaccination (H2a: β = 0.285; p-value <0.001) and perceived behavioral control (H2b: β = 0.427; p-value <0.001) while perceived behavioral control significantly influenced attitudes towards COVID-19 vaccination (H3: β = 0.179; p-value <0.001).
Fig. 3.
Structural equation modeling.
Table 3.
Results of hypothesis testing.
| Hypotheses | Estimate | S.E. | C.R. | P-value | Results | |||
|---|---|---|---|---|---|---|---|---|
| H1a | attitudes towards COVID-19 vaccination | → | COVID-19 vaccination intention | 0.344 | 0.026 | 13.418 | *** | Supported |
| H1b | subjective norms | → | COVID-19 vaccination intention | 0.121 | 0.018 | 6.599 | *** | Supported |
| H1c | perceived behavioral control | → | COVID-19 vaccination intention | 0.215 | 0.017 | 12.359 | *** | Supported |
| H2a | subjective norms | → | attitudes towards COVID-19 vaccination | 0.285 | 0.018 | 15.826 | *** | Supported |
| H2b | subjective norms | → | perceived behavioral control | 0.427 | 0.023 | 18.393 | *** | Supported |
| H3 | perceived behavioral control | → | attitudes towards COVID-19 vaccination | 0.179 | 0.017 | 10.636 | *** | Supported |
| H4a | perceived benefits of COVID-19 vaccines | → | attitudes towards COVID-19 vaccination | 0.498 | 0.022 | 23.123 | *** | Supported |
| H4b | perceived benefits of COVID-19 vaccines | → | subjective norms | 0.723 | 0.024 | 30.739 | *** | Supported |
| H4c | perceived benefits of COVID-19 vaccines | → | perceived behavioral control | 0.346 | 0.026 | 13.085 | *** | Supported |
| H4d | perceived benefits of COVID-19 vaccines | → | COVID-19 vaccination intention | 0.154 | 0.023 | 6.733 | *** | Supported |
Notes: N = 2722, ***p < 0.001.
In terms of the impact of perceived benefits of COVID-19 vaccine, results revealed that these significantly affected attitudes towards COVID-19 vaccination (H4a: β = 0.498; p-value <0.001), subjective norms (H4b: β = 0.723; p-value <0.001), perceived behavioral control (H4c: β = 0.346; p-value <0.001), and COVID-19 vaccination intention (H4d: β = 0.154; p-value <0.001). Besides testing the direct effects, our study adopted Gaskin's (2019) plugin, based on the suggestions of Hayes and Matthes [60], with 5000 bootstrapping samples to test the indirect impacts. The results reported that perceived benefits of COVID-19 vaccines not only had indirect effects on COVID-19 vaccination intention through the three elements of the TPB, including attitudes towards COVID-19 vaccination (β = 0.171; p-value <0.001), subjective norms (β = 0.088; p-value <0.001), and perceived behavioral control (β = 0.074; p-value <0.001), but it also serially and indirectly affected COVID-19 vaccination intention via the serial perceived benefits of COVID-19 vaccines-subjective norms-perceived behavioral control-attitudes towards COVID-19 vaccination-COVID-19 vaccination intention path (β = 0.019; p-value <0.001) (see Table 4).
Table 4.
Results of estimating indirect effects.
| Indirect paths | Estimates | P-value | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| subjective norms | → | perceived behavioral control | → | attitudes towards COVID-19 vaccination | 0.076 | *** | ||||
| subjective norms | → | attitudes towards COVID-19 vaccination | → | COVID-19 vaccination intention | 0.098 | *** | ||||
| subjective norms | → | perceived behavioral control | → | COVID-19 vaccination intention | 0.092 | *** | ||||
| perceived behavioral control | → | attitudes towards COVID-19 vaccination | → | COVID-19 vaccination intention | 0.061 | *** | ||||
| perceived benefits of COVID-19 vaccines | → | subjective norms | → | attitudes towards COVID-19 vaccination | 0.026 | *** | ||||
| perceived benefits of COVID-19 vaccines | → | subjective norms | → | perceived behavioral control | 0.039 | *** | ||||
| perceived benefits of COVID-19 vaccines | → | perceived behavioral control | → | attitudes towards COVID-19 vaccination | 0.062 | *** | ||||
| perceived benefits of COVID-19 vaccines | → | attitudes towards COVID-19 vaccination | → | COVID-19 vaccination intention | 0.171 | *** | ||||
| perceived benefits of COVID-19 vaccines | → | subjective norms | → | COVID-19 vaccination intention | 0.088 | *** | ||||
| perceived benefits of COVID-19 vaccines | → | perceived behavioral control | → | COVID-19 vaccination intention | 0.074 | *** | ||||
| perceived benefits of COVID-19 vaccines | → | subjective norms | → | perceived behavioral control | → | attitudes towards COVID-19 vaccination | 0.055 | *** | ||
| perceived benefits of COVID-19 vaccines | → | subjective norms | → | attitudes towards COVID-19 vaccination | → | COVID-19 vaccination intention | 0.071 | *** | ||
| perceived benefits of COVID-19 vaccines | → | subjective norms | → | perceived behavioral control | → | COVID-19 vaccination intention | 0.066 | *** | ||
| perceived benefits of COVID-19 vaccines | → | subjective norms | → | perceived behavioral control | → | attitudes towards COVID-19 vaccination | → | COVID-19 vaccination intention | 0.019 | *** |
Notes: N = 2722. ***p < 0.001.
Table 5 illustrated the differences in the effects of factors on males and females' COVID-19 vaccination intention. Indeed, while the effects of attitudes towards COVID-19 vaccination (H5a: β = 0.320; p-value <0.001; β = 0.270 p-value <0.001, respectively) and perceived behavioral control (H5c: β = 0.258; p-value <0.001; β = 0.205 p-value <0.001, respectively) on the COVID-19 vaccination intention of females were much higher than on the COVID-19 vaccination intention of males. The impacts of subjective norms (H5b: β = 0.147; p-value <0.001; β = 0183, p-value <0.001, respectively) and the perceived benefits of COVID-19 vaccines (H5d: β = 0.132; p-value <0.001; β = 0.196, p-value <0.001, respectively) on females' COVID-19 vaccination intention were much lower than on males’ COVID-19 vaccination intention.
Table 5.
The differences between males and females in terms of the effects of factors and COVID-19 vaccination intention.
| Hypotheses | Variables |
COVID-19 vaccination intention |
Results | |||
|---|---|---|---|---|---|---|
| Males |
Females |
|||||
| Intercept | 0.599*** | (0.170) | 0.592*** | (0.097) | ||
| H5a | attitudes towards COVID-19 vaccination | 0.270*** | (0.028) | 0.320*** | (0.026) | Supported |
| H5b | subjective norms | 0.183*** | (0.023) | 0.147*** | (0.021) | Supported |
| H5c | perceived behavioral control | 0.205*** | (0.021) | 0.258*** | (0.020) | Supported |
| H5d | perceived benefits of COVID-19 vaccines | 0.196*** | (0.028) | 0.132*** | (0.025) | Supported |
| N (observations) | 1197 | 1525 | ||||
| ΔF | 442.196*** | 547.567*** | ||||
| R2 | 0.597 | 0.590 | ||||
Note: P-values are provided in brackets, ***p < 0.001.
4. Discussion
This study applied the TPB and SEM analyses to predict COVID-19 vaccination intention, and to test the effect of perceived benefits of COVID-19 vaccines on COVID-19 vaccination intention via the three core dimensions of TPB. Using the sample of 2722 adults, our study firstly found that attitudes towards COVID-19 vaccination was the most influential factor with regard to the formation of COVID-19 vaccination intention. This meant that a favorable attitudes towards COVID-19 vaccination is necessary to foster citizens' COVID-19 vaccination intention [10,38]. In other words, to promote citizens' engagement with COVID-19 vaccines, measures to increase positive attitudes towards COVID-19 vaccination should be introduced. Secondly, perceived behavioral control was found to have a strong and positive effect on COVID-19 vaccination intention. This demonstrated that adults' perceived ability and ease of receiving a COVID-19 vaccine significantly contribute to their COVID-19 vaccination intention. At the time of this study, even though the COVID-19 vaccines were not available for over 100 million Vietnamese citizens, many individuals could easily access COVID-19 vaccines as Vietnam received support from the international community thanks to the success of the COVID-19 vaccine diplomacy policy [12,70]. From our participants, 890 of the 2722 adults had already received at least one dose of the vaccine. In addition, subjective norms significantly and positively affected COVID-19 vaccination intention. This aligned with the fact that in a collectivism culture like Vietnam, the decision to conduct a behavior was often influenced by other people. Indeed, opinions/approval from surrounding people (parents, brothers, sisters, friends, and others) were strongly related to individuals' COVID-19 vaccination intention. These findings were in line with the study of Chu, Gupta [43], although this study adopted the TPB to identify individuals' intentions to receive the influenza vaccine. It revealed that all three core dimensions of the TPB were positively associated with these intentions. The findings of our study were different from those of prior studies conducted in Southeast Asia, as well as in Vietnam. For example, while our study applied the TPB to explain how perceived benefits of COVID-19 vaccines could help increase individuals' attitudes towards COVID-19 vaccination, subjective norms, perceived behavioral control, and COVID-19 vaccination intention, prior studies either examined the other drivers of COVID-19 vaccine acceptance with various degrees of pandemic severity [38], or aimed to understand the beliefs and attitudes of South-Asian individuals toward COVID-19 vaccinations [39,71,72]. Particularly, the current study reported the direct and indirect effects of perceived benefits of COVID-19 vaccines on COVID-19 vaccination intention among adults in Vietnam through three core components of the TPB, such as attitudes towards COVID-19 vaccination, subjective norms, perceived behavioral control. However, Chew, Cheong [72] based on the sample of healthcare workers, revealed that a majority of healthcare workers in Asia express willingness to receive COVID-19 vaccination, citing perceived susceptibility to COVID-19, low potential risk of vaccine harm, and pro-socialness as the main driving factors while Hawlader, Rahman [71] revealed that The willingness to receive COVID-19 vaccination among respondents was found to be 65%, 66%, 72%, and 74% for Bangladesh, India, Pakistan, and Nepal, respectively. Significant factors that influenced respondents’ intentions included the perceived destructive impact of COVID-19, positive perception of vaccines, and concerns about possible side effects.
Noticeably, perceived benefits of COVID-19 vaccines have been determined as a key precursor of attitudes towards COVID-19 vaccination, subjective norms, perceived behavioral control, and COVID-19 vaccination intention. Therefore, perceptions related to the effectiveness of COVID-19 vaccines in preventing COVID-19 infections, the benefits of vaccination for the health of others in the community, the safety of COVID-19 vaccines, and the prospect of things going back to normal are crucial factors in individuals’ favorable attitudes towards COVID-19 vaccination and higher COVID-19 vaccination intention [26,42]. Importantly, these results illustrated those attitudes towards COVID-19 vaccination, subjective norms, and perceived behavioral control acted as partial mediators in the link between perceived benefits of COVID-19 vaccines and COVID-19 vaccination intention. In other words, the three core antecedents of the TPB (attitudes towards COVID-19 vaccination, subjective norms, and perceived behavioral control) could transfer the effects of perceived benefits of COVID-19 vaccines on them into COVID-19 vaccination intention. Finally, our results found significant differences in the impacts of attitudes towards COVID-19 vaccination, subjective norms, perceived behavioral control and perceived benefits of COVID-19 vaccines on COVID-19 vaccination intention. For example, males tended to be more influenced by the opinions of other people than females in terms of receiving COVID-19 vaccines.
4.1. Strengths of the current study
Our research offered important strengths. One significant contribution was that it adds to the existing literature on COVID-19 vaccine hesitancy by being one of the first studies conducted in Southeast Asia. Our study shed new light on the intentions to receive the COVID-19 vaccine among adults in this region, thereby expanding our understanding of this important public health issue. Moreover, although prior studies have adopted various theories to explain individuals' COVID-19 vaccination intention, such as the integrative model of behavioral prediction [73] and health behavior theories [42], this study was one of the earliest to employ the TPB [28] to explain adults’ COVID-19 vaccination intention in the context of Vietnam. Our study contributed to our knowledge by illustrating that all three attitudinal antecedents in the TPB make significant contributions to explaining why individuals have COVID-19 vaccination intention. Furthermore, this study was the first to test the mediating roles of the three core dimensions in the TPB (attitudes towards COVID-19 vaccination, subjective norms, and perceived behavioral control) in the link between perceived benefits of COVID-19 vaccines and COVID-19 vaccination intention.
4.2. Policy implications
The results of this research provided practical guidance for policymakers, practitioners, and governments to promote COVID-19 vaccination intentions and behaviors among citizens and to help to control the spread of the COVID-19 pandemic through vaccination. In fact, to foster adults' COVID-19 vaccination intention and vaccination behaviors, practitioners should introduce appropriate measures to promote favorable attitudes towards COVID-19 vaccination as well as to help adults access COVID-19 vaccines more easily to increase their perceived behavioral control. Concurrently, our study showed that the opinions/approval of surrounding people are very important for individuals' decision to have COVID-19 vaccinations. Therefore, suitable communication or marketing measures to increase citizens’ awareness of the benefits of COVID-19 vaccines, for both their own and community health, as well as the safety of COVID-19 vaccines, contribute to forming positive intentions and engagement with COVID-19 vaccines. Lastly, the gender issue should be appropriately addressed as antecedents of COVID-19 vaccination intention impact males and females differently.
5. Limitations
It is important to acknowledge the limitations of our study. Firstly, our sampling method relied on an online survey. Although our sample size was considerable, more than 60% of the sample were aged between 18 and 28 years old as a result of the online nature of the research, while the individuals most vulnerable to the serious side effects of COVID-19 are over the age of 65 [74,75]. Thus, this was also considered to be a limitation of our study. Future studies should employ random sampling methods to improve the representativeness of the research sample as well as to focus on elderly people, who are seriously affected by COVID-19. Secondly, Vietnam had limited access to COVID-19 vaccines during the period of our study, which restricted our ability to explore adults’ intentions to receive the COVID-19 vaccines. Future research should examine the intention-behavior link in individuals' decision to be vaccinated and investigate the factors underlying this decision. Finally, the cross-sectional design was another limitation of our study. Carlson and Morrison [76] argued that the main drawback of a cross-sectional study design was that since the exposure and outcome were evaluated at the same time, there is likely to be no indication of a causal relationship between them. The number of adults who received at least one dose of the COVID-19 vaccine showed the limitation of this research as it reflected their actual behaviors regarding COVID-19 vaccination instead of their behavioral intention. A longitudinal design should be employed in future research to examine the effects of different factors on intentions and behaviors related to receiving COVID-19 vaccines.
6. Conclusion
The TPB has been applied in the current study to estimate the direct and indirect effects of perceived benefits of COVID-19 vaccines on the three core elements of the TPB, through individuals' attitudes towards COVID-19 vaccination, subjective norms, perceived behavioral control, and COVID-19 vaccination intention as well as the gender differences in these relationships. Based on our study's findings, it is clear that attitudes towards COVID-19 vaccination played a critical role in shaping the COVID-19 vaccination intention in adults, followed by perceived behavioral control, perceived benefits of COVID-19 vaccines, and subjective norms. These findings offered valuable insights for practitioners seeking to encourage vaccination uptake and limit the transmission of the COVID-19 pandemic. Furthermore, our study highlighted the significant differences between males and females in how they form the intention to have COVID-19 vaccines. This underscored the importance of tailoring public health campaigns to specific demographic groups to maximize their impact. Overall, our study added to the growing body of research on the TPB and its application to health behavior, specifically related to COVID-19 vaccination uptake among Vietnamese adults. Our findings provided practical recommendations for practitioners seeking to increase vaccination rates and help curb the spread of the COVID-19 pandemic.
Author contribution statement
Huy Nhuong Bui: Conceived and designed the experiments; Performed the experiments; Analyzed and interpreted the data.
Cong Doanh Duong: Performed the experiments; Analyzed and interpreted the data; Wrote the paper.
Van Quang Nguyen; Trung Thanh Le; Trong Nghia Vu; Ngoc Xuan Vu: Contributed reagents, materials, analysis tools or data.
Son Tung Ha: Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data.
Data availability statement
Data will be made available on request.
Declaration of interest's statement
The authors declare no conflict of interest.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgment
This research is funded by National Economics University, Hanoi, Vietnam (ID: 06/HD-CBQT1.2022.06).
References
- 1.Ghosh S. COVID-19, clean energy stock market, interest rate, oil prices, volatility index, geopolitical risk nexus: evidence from quantile regression. J. Econ. Dev. 2022;24(4):329–344. [Google Scholar]
- 2.Botwe B.O., et al. COVID-19 vaccine hesitancy concerns: findings from a Ghana clinical radiography workforce survey. Radiography. 2022;28(2):537–544. doi: 10.1016/j.radi.2021.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dou K., et al. Theory of planned behavior explains males' and females' intention to receive COVID-19 vaccines differently. Hum. Vaccines Immunother. 2022;18(5) doi: 10.1080/21645515.2022.2086393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.WHO . 2023. WHO Coronavirus (COVID-19) Dashboard. in 23 May 2023. [Google Scholar]
- 5.Li J.B., Dou K., Liu Z.H. Profiles of positive changes in life outcomes over the COVID-19 pandemic in Chinese adolescents: the role of resilience and mental health consequence. Child Adolesc. Psychiatr. Ment. Health. 2022;16(1):13. doi: 10.1186/s13034-022-00451-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Duong C.D. The impact of fear and anxiety of Covid-19 on life satisfaction: psychological distress and sleep disturbance as mediators. Pers. Indiv. Differ. 2021;178:1–11. doi: 10.1016/j.paid.2021.110869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Baeza-Rivera M.J., et al. To get vaccinated or not? Social psychological factors associated with vaccination intent for COVID-19. J. Pac. Rim Psychol. 2021;15 [Google Scholar]
- 8.Le T.H., Finch N. Effects of trend inflation on monetary policy and fiscal policy shocks in Vietnam. J. Econ. Dev. 2021;24(2):158–175. [Google Scholar]
- 9.Vasilev A. A business-cycle model with monopolistically competitive firms and Calvo wages: lessons for Bulgaria. J. Econ. Dev. 2022;24(1):80–95. [Google Scholar]
- 10.Wang Z., et al. The willingness of Chinese adults to receive the COVID-19 vaccine and its associated factors at the early stage of the vaccination programme: a network analysis. J. Affect. Disord. 2022;297:301–308. doi: 10.1016/j.jad.2021.10.088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Friedman-Klabanoff D.J., et al. Vaccine-induced seroconversion in participants in the North Carolina COVID-19 community Research Partnership. Vaccine. 2022;40(42):6133–6140. doi: 10.1016/j.vaccine.2022.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nga N.T.V., et al. Perceived barriers and intentions to receive COVID-19 vaccines: psychological distress as a moderator. Vaccines. 2023;11(2) doi: 10.3390/vaccines11020289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hartwig T., Nguyen T.T. Local infrastructure, rural households' resilience capacity and poverty: evidence from panel data for Southeast Asia. J. Econ. Dev. 2022;25(1):2–21. [Google Scholar]
- 14.Yuen M.K., et al. The environment, social and governance (ESG) activities and profitability under COVID-19: evidence from the global banking sector. J. Econ. Dev. 2022;24(4):345–364. [Google Scholar]
- 15.McKinnon B., et al. Social inequalities in COVID-19 vaccine acceptance and uptake for children and adolescents in Montreal, Canada. Vaccine. 2021;39(49):7140–7145. doi: 10.1016/j.vaccine.2021.10.077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kitro A., et al. Acceptance, attitude, and factors affecting the intention to accept COVID-19 vaccine among Thai people and expatriates living in Thailand. Vaccine. 2021;39(52):7554–7561. doi: 10.1016/j.vaccine.2021.11.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Eberhardt J., Ling J. Predicting COVID-19 vaccination intention using protection motivation theory and conspiracy beliefs. Vaccine. 2021;39(42):6269–6275. doi: 10.1016/j.vaccine.2021.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Carlson S.J., et al. Does a major change to a COVID-19 vaccine program alter vaccine intention? A qualitative investigation. Vaccine. 2022;40(4):594–600. doi: 10.1016/j.vaccine.2021.12.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rancher C., et al. Using the 5C model to understand COVID-19 vaccine hesitancy across a National and South Carolina sample. J. Psychiatr. Res. 2023;160:180–186. doi: 10.1016/j.jpsychires.2023.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moini A., et al. COVID-19 vaccine hesitancy among pregnant women and their reported reasons for vaccine refusal - a prospective study in Tehran, Iran. Vaccine. 2023;41(8):1490–1495. doi: 10.1016/j.vaccine.2023.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zolotarova T., et al. Education increases COVID-19 vaccine uptake among people in Canadian federal prisons in a prospective randomized controlled trial: the EDUCATE study. Vaccine. 2023;41(8):1419–1425. doi: 10.1016/j.vaccine.2023.01.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Li J.B., Lau E.Y.H., Chan D.K.C. Why do Hong Kong parents have low intention to vaccinate their children against COVID-19? testing health belief model and theory of planned behavior in a large-scale survey. Vaccine. 2022;40(19):2772–2780. doi: 10.1016/j.vaccine.2022.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lau E.Y.H., Li J.B., King Chung Chan D. Intention to vaccinate young children against COVID-19: a large-scale survey of Hong Kong parents. Hum. Vaccines Immunother. 2022;18(5) doi: 10.1080/21645515.2022.2065838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Turan G.B., et al. The association between coronaphobia and attitude towards COVID-19 Vaccine: a sample in the east of Turkey. Encephale. 2022;48(1):38–42. doi: 10.1016/j.encep.2021.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yuan S., Rui J., Peng X. Trust in scientists on COVID-19 vaccine hesitancy and vaccine intention in China and the US. Int. J. Disaster Risk Reduc. 2023;86 doi: 10.1016/j.ijdrr.2023.103539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Coe A.B., et al. Perceptions and predictors of intention to receive the COVID-19 vaccine. Res. Soc. Adm. Pharm. 2022;18(4):2593–2599. doi: 10.1016/j.sapharm.2021.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mohammed A.H., et al. Parental health beliefs, intention, and strategies about covid-19 vaccine for their children: a cross-sectional analysis from five Arab countries in the Middle East. Vaccine. 2022;40(45):6549–6557. doi: 10.1016/j.vaccine.2022.09.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ajzen I. The theory of planned behavior. Journal of Behavior and Human Decision Process. 1991;50:197–211. [Google Scholar]
- 29.Thi Tuyet Mai N. An investigation into the relationship between materialism and green purchase behavior in Vietnam and Taiwan. J. Econ. Dev. 2019;21(2):247–258. [Google Scholar]
- 30.Mercadante A.R., Law A.V. Will they, or Won't they? Examining patients' vaccine intention for flu and COVID-19 using the Health Belief Model. Res. Soc. Adm. Pharm. 2021;17(9):1596–1605. doi: 10.1016/j.sapharm.2020.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tan C., Liew C.Y. Public Administration and Policy; 2022. Health Belief and Behaviour: an Analysis of the Predictors for Receiving COVID-19 Vaccines in Malaysia. [Google Scholar]
- 32.Ong A.K.S., et al. Determination of factors influencing young adults' intention to have COVID-19 vaccine in the Philippines: an integration of Health Belief Model and the Theory of Planned Behavior. Public Health Pract (Oxf) 2023;5 doi: 10.1016/j.puhip.2023.100359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shmueli L. Predicting intention to receive COVID-19 vaccine among the general population using the health belief model and the theory of planned behavior model. BMC Publ. Health. 2021;21(1):804. doi: 10.1186/s12889-021-10816-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hayashi Y., Romanowich P., Hantula D.A. Predicting intention to take a COVID-19 vaccine in the United States: application and extension of theory of planned behavior. Am. J. Health Promot. 2022;36(4):710–713. doi: 10.1177/08901171211062584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wang J., et al. Applying two behavioral theories to predict the willingness to receive COVID-19 vaccine booster in the elderly: a cross-sectional study. Res. Soc. Adm. Pharm. 2023;19(3):495–501. doi: 10.1016/j.sapharm.2022.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ullah I., et al. Factors affecting Pakistani young adults' intentions to uptake COVID-19 vaccination: an extension of the theory of planned behavior. Brain Behav. 2021;11(11):e2370. doi: 10.1002/brb3.2370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Seddig D., et al. Correlates of COVID-19 vaccination intentions: attitudes, institutional trust, fear, conspiracy beliefs, and vaccine skepticism. Soc. Sci. Med. 2022;302 doi: 10.1016/j.socscimed.2022.114981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Duong A.H., Antriyandarti E. The willingness to get vaccinated against SARS-CoV-2 virus among Southeast Asian countries: does the vaccine brand matter? Appl Res Qual Life. 2022:1–29. doi: 10.1007/s11482-022-10104-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Duong M.C., Nguyen H.T., Duong M. Evaluating COVID-19 vaccine hesitancy: a qualitative study from Vietnam. Diabetes Metabol. Syndr. 2022;16(1) doi: 10.1016/j.dsx.2021.102363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ajzen I. The theory of planned behavior: frequently asked questions. Human Behavior and Emerging Technologies. 2020;2(4):314–324. [Google Scholar]
- 41.Si H., et al. Uncovering people's mask-saving intentions and behaviors in the post-COVID-19 period: evidence from China. Sustain. Cities Soc. 2021;65 doi: 10.1016/j.scs.2020.102626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chu H., Liu S. Integrating health behavior theories to predict American's intention to receive a COVID-19 vaccine. Patient Educ. Counsel. 2021;104(8):1878–1886. doi: 10.1016/j.pec.2021.02.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chu A., Gupta V., Unni E.J. Utilizing the Theory of Planned Behavior to determine the intentions to receive the influenza vaccine during COVID-19: a cross-sectional survey of US adults. Prev Med Rep. 2021;23 doi: 10.1016/j.pmedr.2021.101417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mir H.H., et al. Using structural equation modeling to predict Indian people's attitudes and intentions towards COVID-19 vaccination. Diabetes Metabol. Syndr. 2021;15(3):1017–1022. doi: 10.1016/j.dsx.2021.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ajzen I. The theory of planned behaviour: reactions and reflections. Psychol. Health. 2011;26(9):1113–1127. doi: 10.1080/08870446.2011.613995. [DOI] [PubMed] [Google Scholar]
- 46.Maresch D., et al. The impact of entrepreneurship education on the entrepreneurial intention of students in science and engineering versus business studies university programs. Technol. Forecast. Soc. Change. 2016;104:172–179. [Google Scholar]
- 47.Qi X., Ploeger A. Explaining consumers' intentions towards purchasing green food in Qingdao, China: the amendment and extension of the theory of planned behavior. Appetite. 2019;133:414–422. doi: 10.1016/j.appet.2018.12.004. [DOI] [PubMed] [Google Scholar]
- 48.Tsai K.-H., Chang H.-C., Peng C.-Y. Extending the link between entrepreneurial self-efficacy and intention: a moderated mediation model. Int. Enterpren. Manag. J. 2016;12:445–463. [Google Scholar]
- 49.Duong C.D. Exploring the link between entrepreneurship education and entrepreneurial intentions: the moderating role of educational fields. Educ + Train 64 (7) 2021 869-891. [Google Scholar]
- 50.Rosenstock I.M. Historical origins of health belief model. Health Educ. Behav. 1974;2(4):328–335. [Google Scholar]
- 51.Wong C.Y., et al. Factors influencing COVID-19 vaccination intention among university students: a cross-sectional study in Malaysia. Biosaf Health. 2023;5(1):37–44. doi: 10.1016/j.bsheal.2022.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Luo W., Song S. Perceived benefits and barriers to Chinese COVID-19 vaccine uptake among young adults in China. Front. Public Health. 2022;10 doi: 10.3389/fpubh.2022.825874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Stockard J. In: Handbook of the Sociology of Gender. Chafetz Janet S., editor. Kluwer Academic/Plenum Publishers; New York: 1999. Gender socialization; pp. 215–246. [Google Scholar]
- 54.Liñán F., Chen Y.-W. Development and cross-cultural application of a specific instrument to measure entrepreneurial intentions. Entrep. Theory Pract. 2009;33(3):593–617. [Google Scholar]
- 55.Lee W.L., et al. The forward-backward and dual-panel translation methods are comparable in producing semantic equivalent versions of a heart quality of life questionnaire. Int. J. Nurs. Pract. 2019;25(1) doi: 10.1111/ijn.12715. [DOI] [PubMed] [Google Scholar]
- 56.Duong C.D. “What goes around comes around”: Activating sustainable consumption with curvilinear effects of karma determinants. J. Retailing Consum. Serv. 2023;73:1–14. [Google Scholar]
- 57.Nguyen H.V., et al. Happiness and pro-environmental consumption behaviors. J. Econ. Dev. 2022:1–14. [Google Scholar]
- 58.Duong C.D. A moderated mediation model of perceived barriers, entrepreneurial self-efficacy, intentions, and behaviors: a social cognitive career theory perspective. Oeconomia Copernicana. 2023;14(1):355–388. [Google Scholar]
- 59.Wang L.-X., et al. The association between interparental conflict and problematic internet use among Chinese adolescents: testing a moderated mediation model. Comput. Hum. Behav. 2021:122. [Google Scholar]
- 60.Hayes A.F., Matthes J. Computational procedures for probing interactions in OLS and logistic regression: SPSS and SAS implementations. Behav. Res. Methods. 2009;41(3):924–936. doi: 10.3758/BRM.41.3.924. [DOI] [PubMed] [Google Scholar]
- 61.Sarstedt M., et al. Beyond a tandem analysis of SEM and PROCESS: use of PLS-SEM for mediation analyses! Int. J. Mark. Res. 2020;62(3):288–299. [Google Scholar]
- 62.Hu L.t., Bentler P.M. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct. Equ. Model.: A Multidiscip. J. 1999;6(1):1–55. [Google Scholar]
- 63.Bentler P.M., Speckart G. Models of attitude-behavior relations. Pyschological Review. 1979;86(5):452–464. [Google Scholar]
- 64.Henseler J., Ringle C.M., Sarstedt M. A new criterion for assessing discriminant validity in variance-based structural equation modeling. J. Acad. Market. Sci. 2014;43(1):115–135. [Google Scholar]
- 65.Anderson J.C., Gerbing D.W. Structural equation modeling in practice: a review and recommended two-step approach. Psychol. Bull. 1988;103(3):411–423. [Google Scholar]
- 66.Hair J.F., Howard M.C., Nitzl C. Assessing measurement model quality in PLS-SEM using confirmatory composite analysis. J. Bus. Res. 2020;109:101–110. [Google Scholar]
- 67.Podsakoff P.M., et al. Common method biases in behavioral research: a critical review of the literature and recommended remedies. J. Appl. Psychol. 2003;88(5):879–903. doi: 10.1037/0021-9010.88.5.879. [DOI] [PubMed] [Google Scholar]
- 68.Kock F.B., Assaf Adiyukh, George A. Understanding and managing the threat of common method bias: detection, prevention and control. Tourism Manag. 2021;86 [Google Scholar]
- 69.Duong C.D. Karmic beliefs and social entrepreneurial intentions: a moderated mediation model of environmental complexity and empathy. Journal of Open Innovation: Technology, Market, and Complexity. 2023;9(1) [Google Scholar]
- 70.Dinh Tinh L., Thu Ngan V.T. The COVID-19 pandemic and the emergence of Vietnam as a middle power. J. Curr. Southeast Asian Aff. 2021;41(2):303–325. [Google Scholar]
- 71.Hawlader M.D.H., et al. COVID-19 vaccine acceptance in South Asia: a multi-country study. Int. J. Infect. Dis. 2022;114:1–10. doi: 10.1016/j.ijid.2021.09.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Chew N.W.S., et al. An Asia-Pacific study on healthcare workers' perceptions of, and willingness to receive, the COVID-19 vaccination. Int. J. Infect. Dis. 2021;106:52–60. doi: 10.1016/j.ijid.2021.03.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Chen W.S., et al. Mediating effect of chronic illnesses in the relationship between psychological distress and COVID-19 vaccine acceptance. Asia Pac. J. Publ. Health. 2022;34(1):106–112. doi: 10.1177/10105395211047868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Mueller A.L., McNamara M.S., Sinclair D.A. Why does COVID-19 disproportionately affect older people? Aging. 2020;12(10):9959–9981. doi: 10.18632/aging.103344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Li C., et al. J Am Med Dir Assoc; 2023. Cognitive Decline before and during COVID-19 Pandemic Among Older People with Multimorbidity: A Longitudinal Study. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Carlson M.D., Morrison R.S. Study design, precision, and validity in observational studies. J. Palliat. Med. 2009;12(1):77–82. doi: 10.1089/jpm.2008.9690. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request.