Abstract
When treating acute ischemic stroke patients in our daily clinical practice, we strive to achieve recanalization of the occluded blood vessel as fast as possible using pharmacological thrombolysis and mechanical clot removal. However, successful recanalization does not equal successful reperfusion of the ischemic tissue due to mechanisms such as microvascular obstruction. Even if successful reperfusion is achieved, numerous other post-recanalization tissue damage mechanisms may impair patient outcomes, namely blood–brain barrier breakdown, reperfusion injury and excitotoxicity, late secondary changes, and post-infarction local and global brain atrophy. Several cerebroprotectants are currently evaluated as adjunctive treatments to pharmacological thrombolysis and mechanical clot removal, many of which interfere with post-recanalization tissue damage pathways. However, our current lack of knowledge about the prevalence and importance of the various post-recanalization tissue damage mechanisms makes it difficult to reliably identify the most promising cerebroprotectants and to design appropriate clinical trials to evaluate them. Serial human MRI studies with complementary animal studies in higher order primates could provide answers to these critical questions and should be first conducted to allow for adequate cerebroprotection trial design, which could accelerate the translation of cerebroprotective agents from bench to bedside to further improve patient outcomes.
Supplementary Information
The online version contains supplementary material available at 10.1007/s13311-023-01367-3.
Keywords: Stroke, Recanalization, Reperfusion, Pathophysiology, Neuroprotection
Introduction: What Is Acute Ischemic Stroke?
Acute ischemic stroke (AIS) is caused by a blood clot blocking blood flow in a brain artery, and results in ischemia of the downstream brain tissue. The classic theory is that of a central area of irreversibly damaged tissue (“infarct core”), which is surrounded by ischemic tissue that could in theory still be salvaged if reperfusion were to occur quickly (“tissue at risk” or “penumbra”). Recanalization of the occluded artery and, more importantly, reperfusion of the ischemic brain tissue downstream to the occlusion are the goal of both medical and interventional treatments in the setting of AIS. Intravenous thrombolysis (IVT), i.e., dissolving the blood clot through administration of intravenous thrombolytics, was the first approved curative treatment for AIS, but its utility remains limited due to its brief window of efficacy and the extensive list of contraindications. In 2015, endovascular thrombectomy (EVT) in addition to IVT was proven beneficial over and above IVT alone in patients with large vessel occlusions (LVO), the most disabling form of AIS. As a result, outcomes for LVO patients have improved significantly and EVT is now the standard of care for LVO stroke [1], with more and more patients being considered for EVT even outside the guideline recommendations [2]. Despite major advancements in EVT and IVT in recent years, clinical outcomes vary, and approximately half of all AIS patients with LVO do not achieve functional independence. Notably, while we are getting better and better at achieving recanalization (i.e., re-opening of the blood vessel) due to technological innovations in EVT technology and techniques [3] and more effective thrombolytic agents [4], in some patients, outcomes remain poor even when successful recanalization of the occluded blood vessel is achieved.
There are many potential explanations for this apparent discrepancy between technical treatment success and clinical outcomes. On the clinical side, patient factors such as chronic illnesses and co-morbidities and post-stroke complications such as urinary tract infections, pulmonary embolism, post-stroke pneumonia and post-stroke depression, can cause poor outcomes despite technical EVT success [5, 6]. Incomplete reperfusion at the tissue level and numerous other tissue injury pathways constitute additional reasons for patients suffering poor outcomes despite successful recanalization. Our current understanding of the temporal evolution and exact nature of these post-recanalization tissue damage mechanisms, their temporal evolution, imaging correlates, and exact impact on clinical outcomes is limited.
Recanalization vs. Reperfusion: What Is the Difference?
The terms “recanalization” and “reperfusion” are often conflated and erroneously used interchangeably. Recanalization is defined as the re-opening of a blocked vessel, either through pharmacological intravenous thrombolysis (IVT) or by mechanical clot removal (EVT). Recanalization restores blood flow at a macrovascular (arterial) level. The ultimate goal behind recanalization, however, is reperfusion, i.e., re-establishing oxygen and nutrient supply to previously ischemic tissue at the distal capillary and tissue level. The terms recanalization and reperfusion are often used synonymously in clinical practice, but they are not the same. While successful recanalization is virtually always needed for successful reperfusion to occur, its presence does not guarantee reperfusion [7]. Microvascular obstruction describes impaired reperfusion, i.e., persistent occlusion of microscopic vessels (arterioles and capillaries), despite macroscopic recanalization. Microvascular obstruction is one of the main reasons for reperfusion failure despite successful recanalization. While microvascular obstruction has been a well-known poor prognostic marker in myocardial infarction for many years [8], it has been recognized only recently that it is also one of the key drivers in post-recanalization tissue damage in acute ischemic stroke [9]. Microvascular obstruction occurs in up to one-fourth of acute ischemic stroke patients [10] and can occur as a result of persistent microthrombi, endothelial damage, astrocyte swelling, and pericyte constriction [9]. To date, it is not entirely clear which of these mechanisms is the dominant one, or whether there are different dominant mechanisms in different patient subgroups. By imaging reperfusion on a tissue level, microvascular obstruction could be visualized. Therefore, those imaging modalities that are able to visualize true reperfusion, rather than recanalization, as discussed in Table 1, are potentially suitable to assess for microvascular obstruction. Furthermore, some attempts have been made to indirectly image microvascular obstruction by measuring microvascular resistance on transcranial Doppler ultrasonography [9].
Table 1.
Stroke imaging modalities
| Imaging method | Current use in clinical routine | Iodinating radiation | Revascularization vs. reperfusion component | Advantages | Disadvantages | Likelihood of being used for routine post-EVT reperfusion assessment |
|---|---|---|---|---|---|---|
| CT perfusion | Pre-EVT assessment of core and penumbra | + + + | Substantial revascularization component (purely intravascular contrast agent), intravenous injection |
• Widely available • Different parameters • Can be performed on the angio table if hybrid or flat-panel angio suite is available |
• Substantial increase in radiation dose • Post-processing necessary • Prone to motion and technical artifacts |
Very low |
| Multiphase CT angiography | Pre-EVT assessment of collateral circulation (helps to estimate core and penumbra) | + | Substantial revascularization component (purely intravascular contrast agent), intravenous injection |
• Even more widely available • No need for post-processing • Robust against motion and technical artifacts • Can be performed on the angio table if hybrid or flat-panel angio suite is available |
• Slight increase in radiation dose • Less precise (fewer time points) compared to CTP |
Very low |
| Diffusion-weighted MRI and MRP | 24-h post-EVT infarct assessment (in some centers also used for pre-EVT assessment) | None | Primarily reperfusion (DWI: cytotoxic edema, represents severe hypoperfusion/infarction, no contrast agent required; MRP: MR contrast agents can leave the intravascular compartment to some extent, intravenous injection) |
• No substantial recanalization component (as opposed to all other routinely used imaging methods) • Radiation-free • Additional MR sequences can be performed to gain information about other post-recanalization tissue damage mechanisms |
• Less available • Expensive • Contraindications (pacemaker etc.) • Prone to motion artifacts • Patient needs to be transferred from the angio table to the MR scanner |
High |
| DSA perfusion | Not in clinical use yet | None (no additional radiation) | Substantial revascularization component (purely intravascular contrast agent), intra-arterial injection | • Routine intra-arterial injection can be used to generate DSAP maps (no additional steps needed) | • Imaging is obtained on the angio table (no need to transfer the patient) | Unclear |
Different imaging modalities that can potentially be used to measure reperfusion post-recanalization/EVT
CTP CT perfusion, MRP MR perfusion, DSAP digital subtraction angiography perfusion, DWI diffusion-weighted imaging, EVT endovascular treatment
How Is Recanalization Measured?
In patients undergoing IVT, recanalization is not typically assessed in clinical routine although it can in theory be assessed by MRA or CTA. However, it is routinely assessed in patients undergoing EVT, either in addition to IVT or as a standalone treatment. EVT is performed using digital subtraction angiography (DSA), during which the clot is removed with aspiration catheters or stent retrievers. On the final DSA run after clot retrieval, the degree of arterial revascularization in the middle cerebral artery territory (the most common location of vessel occlusions) is evaluated using the expanded Thrombolysis in Cerebral Infarction scale (eTICI; see Fig. 1). Note that there is inconsistency in the literature about what eTICI is supposed to describe—recanalization or reperfusion [11–13]. Others avoid those terms altogether and prefer to use “revascularization” instead [11]. However, since eTICI relies on assessment of arterial and arteriolar vessels after injection of a purely intravascular contrast agent that does not pass the blood–brain barrier, it is probably accurate to say that eTICI, for the most part, represents recanalization, rather than true reperfusion, and this is the terminology that we will use in the following. At the very least, one needs to admit that eTICI is not an accurate reflection of brain reperfusion because it includes a substantial recanalization component. Similar scores are used for the anterior and posterior cerebral artery [14]. The goal of EVT is to achieve eTICI 2c or eTICI 3 recanalization [15], which represent the so-called near-complete or complete recanalization, or 90–99% to 100% opacification of vessels in the affected territory [16]. “Successful recanalization,” another EVT success metric, is defined as eTICI 2b, 2c, or 3, that is > 50% opacification of vessels in the affected territory. Due to improvements in EVT tools and techniques, successful and near-complete recanalization are now achieved in approximately 86% and 46% of LVO patients respectively [17]. As EVT technology continues to evolve, recanalization rates are likely to improve further.
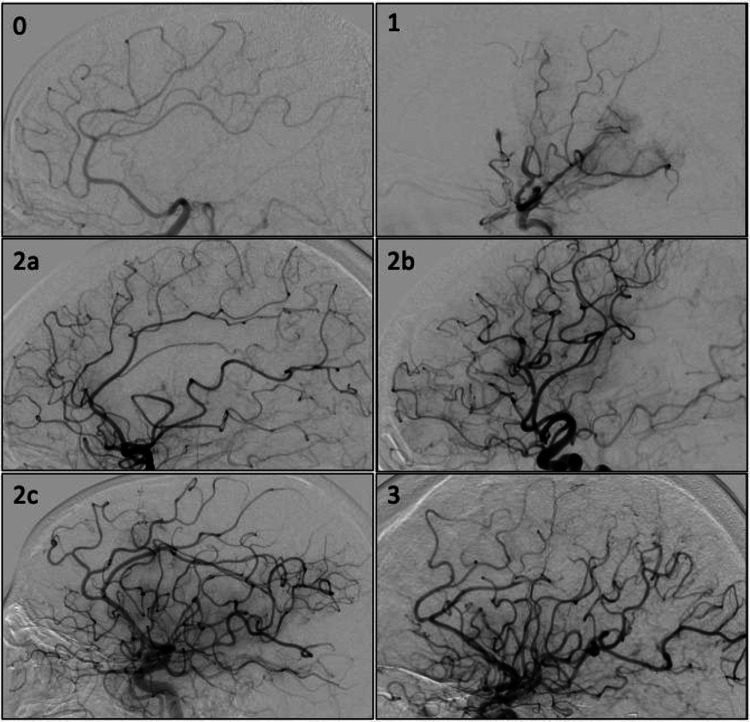
Fig. 1.
Recanalization assessment on digital subtraction angiography using the expanded Thrombolysis in Cerebral Infarction (eTICI) score. The images show lateral intracranial angiograms after intra-arterial contrast injection into the internal carotid artery. eTICI 0—no vessels in the middle cerebral artery territory are opacified. eTICI 1—only very limited opacification of the proximal middle cerebral artery, with no filling of any distal branches is seen. eTICI 2a—normal vascular opacification in < 50% of the middle cerebral artery territory. eTICI 2b—normal vascular opacification in 50–90% of the middle cerebral artery territory. eTICI 2c—normal vascular opacification in 90–99% of the middle cerebral artery territory. eTICI 3—normal vascular opacification in the complete middle cerebral artery territory (100%)
The eTICI score is commonly used to predict patient outcome. However, “technical success” is variably defined, and eTICI assessment is subject to substantial interrater variability [18]. Furthermore, because successful recanalization does not always lead to successful reperfusion, and the latter is needed for tissue survival, clinical outcomes in patients with successful recanalization still vary considerably [19]. Reperfusion is the more meaningful parameter for overall patient outcome compared to recanalization, and the latter has only a moderate association with good outcome [20].
How Is (Re-)Perfusion Measured?
Reperfusion is not routinely measured in clinical practice. The reason is that (a) current imaging methods do not allow us to reliably and accurately assess brain perfusion but rather provide a rough estimate at best and (b) these methods that are used to grossly estimate perfusion are either radiation-intensive, impractical, or both.
CT perfusion
CT perfusion (CTP) is often used at baseline, i.e., prior to EVT, to estimate the size of the infarct core and penumbra, which is used for treatment decision-making by some physicians. The principle of CTP is as follows: After an intravenous injection of iodinated contrast, the brain is scanned continuously over 45–90 s to image contrast flow in arteries, its distribution into the arterioles and capillary bed, and its venous outflow through the venous system [21]. Post-processing algorithms are then used to create color maps that display several parameters, namely cerebral blood flow (CBF), cerebral blood volume (CBV), mean transit time, time-to-peak, and time-to-maximum (Tmax) of the residue function (Fig. 2). CBV and CBF thresholds are then often used to determine the infarct “core” of irreversibly damaged tissue and the penumbra (brain tissue at risk) [22] (see Fig. 2). In theory, many angiography suites are equipped with CT capabilities (“hybrid” or “flat-panel CT” angio suites), so from a technical standpoint, CTP could easily be performed after recanalization/EVT [23]. The 2 key reasons why this is not done are as follows: (1) CTP relies on many assumptions and is based on the dynamic behavior of an intravascular contrast agent, rather than the distribution of oxygen and other nutrients to the brain parenchyma itself [24]. Thus, CTP is probably a reflection of recanalization, rather than true reperfusion, and its accuracy in assessing perfusion is limited. (2) Performing CTP requires a substantial amount of ionizing radiation [21]. It is thus not routinely performed post-recanalization because of concerns about radiation-related risks.
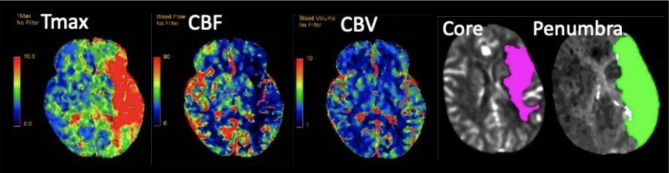
Fig. 2.
CT perfusion obtained before EVT in an acute stroke patient. The 3 color-coded maps on the left show time-to-maximum of the residue function (Tmax), cerebral blood flow (CBF), and cerebral blood volume (CBV). These parameters are often dichotomized and used to generate infarct core and penumbra maps (shown on the right). The maps show a large apparent “perfusion delay” in the left middle cerebral artery territory, suggestive of a proximal occlusion in the left middle cerebral artery territory
Multiphase CT Angiography
Multiphase CT angiography (mCTA) is a faster, less radiation-intensive, and simplified version of CTP, and has the additional advantage of requiring no post-processing [21] (Fig. 3). mCTA is used in many centers as an alternative to CTP in the baseline imaging protocol, i.e., prior to EVT. However, when it comes to measuring reperfusion after recanalization/EVT, similar problems as with CTP occur: just like CTP, mCTA is also based on intravascular contrast distribution and thus primarily measures recanalization rather than true reperfusion. Furthermore, it also adds to the patient’s iodinated radiation dose and is therefore not routinely performed after EVT, although the additional radiation dose is much lower compared to CTP. Lastly, although CTP-like parametric maps can be generated with mCTA as well [25], their accuracy is probably lower since the brain is imaged at fewer time points.
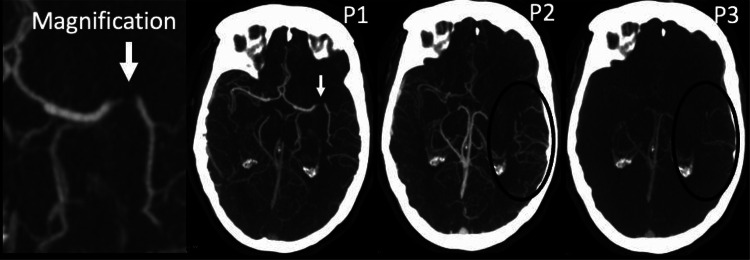
Fig. 3.
Multiphase CT angiography obtained before EVT in an acute stroke patient. The first phase (P1) shows an M1 segment occlusion of the left middle cerebral artery (arrow, magnified image shown on the left). The second (P2) and third (P3) phases show delayed collateral filling and washout (black circles in P2 and P3). As opposed to CT perfusion, in which the brain is imaged 45–90 times, mCTA relies on 3 time points only (P1, arterial phase; P2, peak-venous phase; and P3, late-venous phase)
Magnetic Resonance Imaging
Diffusion-weighted MR imaging (DWI) measures restriction of water molecule movement in tissues, characterizing the extent of cytotoxic edema, which mostly occurs in case of severe hypoperfusion that has already led to, or will invariably lead to, infarction. This translates into a decreased apparent diffusion coefficient (ADC) on imaging (Fig. 4). Although diffusion restriction is usually thought to represent irreversible tissue damage, which may be caused either by lack of reperfusion or by other post-recanalization tissue damage mechanisms, reversal of DWI lesions has been observed in few patients [26]. Availability of MRI is limited, costs are higher compared to CT, and numerous contraindications may prevent the patient from undergoing an MR. Just like CTP, MRI is not routinely performed directly after recanalization mostly due to cost and availability issues, and because it is often hard for acute stroke patients to lie still during the time of MRI acquisition, which is slightly longer compared to CT. MRI is however often used to assess the infarction size and complications such as intracranial hemorrhage at 24 h. Radiation safety is not a concern with MRI, since it is a completely iodinated radiation-free imaging method. Therefore, MRI, particularly DWI-MRI, may be the most promising imaging tool for post-recanalization reperfusion assessment. Furthermore, additional, complementary MRI sequences, such as hemorrhage-sensitive sequences (gradient echo imaging and susceptibility-weighted imaging), can provide additional useful information about post-recanalization tissue damage mechanisms, as described in detail previously by our group [27]. MR perfusion, although rarely used due to MR contraindications in some patients (e.g., pacemakers), as well as longer scan duration, higher cost, and less availability compared to CTP, may reflect brain perfusion more accurately than CT perfusion, because MR contrast media are able to leave the intravascular compartment and enter the brain tissue itself to some extent [28].
Fig. 4.
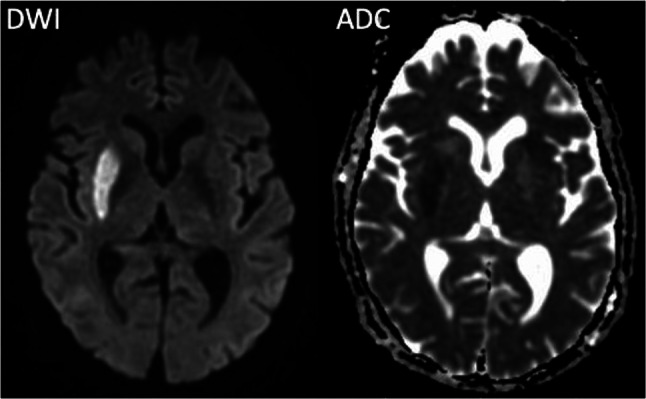
Diffusion-weighted (DWI) MRI and corresponding apparent diffusion coefficient (ADC) maps. Areas with cytotoxic edema, i.e., areas with insufficient tissue perfusion that are infarcted or invariably going to infarct, can be seen as hyperintense signal on DWI with a corresponding decrease (hypointense signal) on the ADC map. The image pair shows a right-sided acute infarct in the lentiform nucleus
Other Novel Techniques
More advanced measures have been proposed to measure perfusion and particularly reperfusion after recanalization/EVT: DSA source images can be used to generate the so-called DSA perfusion (DSAP) to recreate maps of mean transit time, which could routinely be performed on the angio table, after successful EVT [29]. The two main advantages of this type of reperfusion assessment are that (1) it would be based on intra-arterial contrast injections that are performed to assess eTICI anyway, i.e., there are no additional risks, and (2) it would be much more practical compared to CT- or MR-based reperfusion assessment since the patient would not have to be transferred from the angio table to the CT or MR scanner for reperfusion assessment. However, it is not clear yet to which extent these DSA-derived maps represent recanalization vs. reperfusion, and they are not available for clinical routine use yet.
Is Complete Reperfusion the Only Determinant of Post-recanalization Tissue Fate?
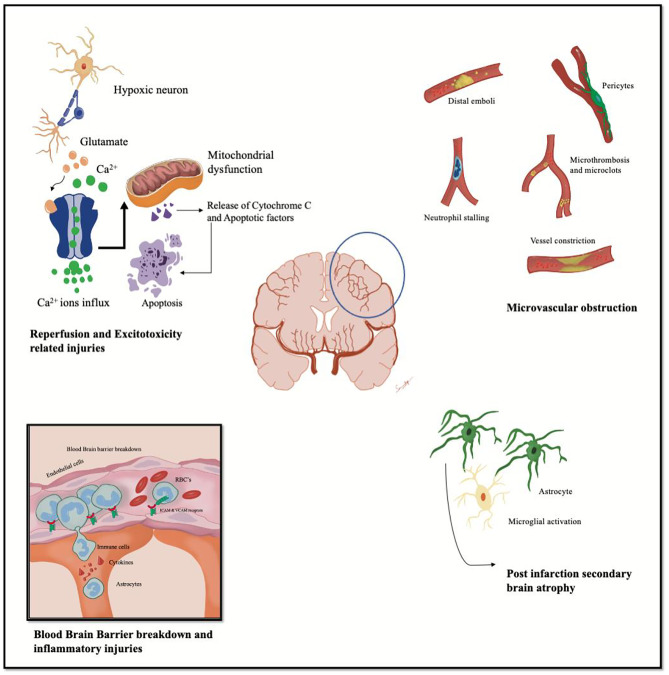
After this extensive discussion on the importance of reperfusion and reperfusion assessment, the question arises whether complete reperfusion is everything that is needed for brain tissue to survive after recanalization. Are there mechanisms that can cause tissue damage even if successful reperfusion has been achieved? [7, 30, 31]. The answer is yes, and the mechanisms that are responsible for sustained tissue damage despite successful reperfusion are shown in Fig. 5 and will be discussed in the following.
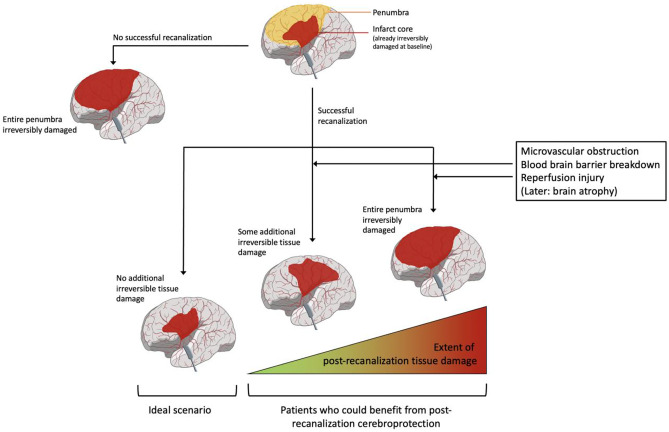
Fig. 5.
Possible outcomes after acute ischemic stroke. In the initial state, the infarct core, i.e., the tissue that is already irreversibly damaged at baseline, is shown in red, and the penumbra (i.e., the tissue at risk that could still be salvaged if recanalization and reperfusion were to occur) is shown in yellow. In case no recanalization, and thus, no reperfusion, is achieved, the entire penumbra will eventually turn into infarct core (left image, “worst-case scenario”). In case successful recanalization is achieved, different scenarios are possible. If successful recanalization translates into successful reperfusion and no other tissue damage mechanisms prevail, no additional irreversible tissue damage will occur over and beyond the infarct core that was already present at baseline (“ideal scenario”). If recanalization results in partial, but not complete reperfusion of the previously ischemic tissue due to some degree of microvascular obstruction, or other, additional tissue damage mechanisms prevail, some additional irreversible tissue damage will occur. In other words, some, but not all, of the penumbral tissue will suffer irreversible damage. If successful recanalization does not result in any reperfusion due to extensive microvascular obstruction, or massive tissue damage is caused by other mechanisms, the entire penumbra will eventually sustain irreversible damage, similar to a scenario in which no recanalization was achieved in the first place. Cases in which successful recanalization does not translate into complete reperfusion, and/or in which additional tissue damage mechanisms prevail, may constitute targets for post-recanalization cerebroprotection therapies, which aim to reduce the post-recanalization tissue damage. Please note that the very rare scenario in which unsuccessful recanalization is followed by complete or near-complete reperfusion is not shown in this diagram
What Are the Imaging Physiological and Cellular Mechanisms of Tissue Damage?
Ischemic tissue damage mechanisms in AIS are complex, non-linear, and discontinuous, involving multiple cell-signaling pathways which differ based on tissue and cell type and the duration of ischemia [27, 32, 33]. Many of these tissue damage mechanisms continue even after recanalization has been achieved, and some, such as reperfusion hemorrhage, occur primarily after recanalization. These mechanisms that contribute to post-recanalization tissue damage in addition to microvascular obstruction/incomplete reperfusion have raised the interest of both basic scientists and clinical researchers. It is however challenging to isolate and evaluate them due to large overlap in their pathophysiology and imaging correlates. Those imaging modalities that seem most capable of accurately reflecting the different mechanisms, such as 18Fluoro-deoxy-glucose positron emission tomography (FDG-PET) or Xenon-CT, are impractical, expensive, radiation-intensive, and therefore not used in clinical routine [34, 35]. Since MRI is radiation-free and available in most hospitals, serial MRI post-recanalization could in theory be performed, and researchers are increasingly trying to find MRI “imaging signatures” of different post-recanalization tissue damage mechanisms [27, 36]. Key post-recanalization tissue damage mechanisms other than incomplete reperfusion/microvascular obstruction and their respective imaging correlates are discussed in the following (see also Figs. 5 and 6) [27].
Fig. 6.
Key contributing mechanisms to post-recanalization tissue damage (in no particular order): (1) incomplete reperfusion/microvascular obstruction, i.e., persistent obstruction on a capillary level (lack of reperfusion) despite recanalization of macroscopic vessels due to microthrombi and endothelial damage; (2) blood–brain barrier breakdown with resulting hemorrhagic complications and inflammatory changes; (3) reperfusion- and excitotoxicity-related injury (for example via calcium influx, mitochondrial dysfunction, and apoptosis through cytochrome C pathways); and (4) secondary changes post-infarction including brain atrophy
Blood–Brain Barrier Breakdown
The blood–brain barrier (BBB) is formed by a neurogliovascular complex that includes tight junctions between endothelial cells, the basal membrane, pericytes, and astrocytes [37]. It constitutes a barrier between the intravascular compartment and the brain tissue itself. BBB disruption in acute ischemic stroke results from lost homeostasis within supporting cells and can cause vasogenic edema and hemorrhagic transformation in the early reversible phase and a hyper-inflammatory response in the late phase. A compromised BBB results in inability to regulate flow appropriately, and the introduction of both high pressure (due to recanalization of the previously occluded vessel) and damaging ischemic metabolites like reactive oxygen and nitrogen species most likely perpetuate the initial damage caused by BBB breakdown. As opposed to other post-recanalization tissue damage mechanisms, BBB disruption is easily recognized on routine imaging, since it results in parenchymal enhancement on contrast-enhanced MRI, and sometimes even contrast-enhanced CT, in the days following AIS as parenchymal enhancement. If hemorrhagic transformation or frank mass hemorrhage occurs as a result, this can be recognized as either petechial or mass-like hemorrhage on non-contrast CT and hemorrhage-sensitive MR sequences [38]. The vasogenic edema that often results from BBB breakdown [39] is also easily visualized as hypodense white matter changes on non-contrast CT, or hyperintense white matter changes in T2 and fluid attenuation inversion recovery MR sequences. Furthermore, arterial spin labeling (ASL) has been proven to be a useful contrast-free method to image BBB permeability in ischemic stroke, both in animal models [40] and humans [41]. As opposed to cytotoxic edema, which mostly represents irreversible infarction and affects both gray and white matter, vasogenic edema is restricted to the white matter only.
Reperfusion Injury and Excitotoxicity-Related Injury
Reperfusion injury is a loose term which most commonly refers to tissue damage that occurs in previously ischemic tissue when oxygen is re-introduced through recanalization. As a consequence, reactive oxygen species (ROS) form. Mitochondria further contribute to ROS formation, creating a state of “oxidative stress,” which leads to peroxidation of cell membranes and subsequent damage of different cell types in the brain tissue. ROS also further accelerate ongoing pro-inflammatory cell signaling pathways, including glutamate-induced excitotoxicity [27, 42]. Owing to the complex, multifactorial mechanisms of reperfusion injury, and the heterogeneity in the use of the term itself, there are no well-established imaging markers for reperfusion injury at the time being. However, it has been suggested that serial MR imaging, and particularly MR perfusion, may provide a framework for better characterizing reperfusion injury [42].
Secondary Changes and Post-infarction Atrophy
Excitotoxicity is not only part of the acute reperfusion injury phase, but it also mediates late (i.e., days to weeks after recanalization) infarct growth and brain atrophy because the initial level of cellular damage and debris initiates a sustained inflammatory response in the days and weeks following the initial ischemic event. Much later, secondary changes occur in brain regions that were connected to the infarcted tissue, but not initially damaged by the infarct itself (Wallerian degeneration). These secondary changes are mediated by astrocytes and microglia, whereby infarction leads to microscopic and eventually also macroscopic tissue loss in adjacent areas connected to the infarct, eventually resulting the formation of dense, non-functional, or dysfunctional gliotic tissue outside the actual infarct [43]. Wallerian degeneration is characterized by an initial increase in signal on T2 and FLAIR MR sequences, followed by subsequent volume loss. Stroke survivors also suffer from accelerated global brain atrophy, particularly in the first few months after the stroke [44]. While Wallerian degeneration is relatively easy to recognize on MRI, global brain atrophy often only results in subtle changes in the early stages, which may only be reliably captured when using automated software solutions that have already been developed as complementary imaging tools for neurocognitive disorders [45] and multiple sclerosis [46].
Can Post-recanalization Tissue Damage Be Prevented, and How?
Numerous cerebroprotectants for human AIS have been investigated, many of which have pleiotropic effects that target both pre- and post-recanalization tissue damage mechanisms, and a few have aimed to primarily prevent post-recanalization tissue damage. However, to date, no post-recanalization cerebroprotectant is approved for use in human AIS. One reason for this is the lack of a robust, conceptual framework for post-recanalization cerebroprotection trials. In order to effectively investigate treatments that specifically target post-recanalization tissue damage, four key questions need to be answered first (see also Table 3):
What is the relative importance of the different post-recanalization tissue damage mechanisms? For example, if hypothetically reperfusion injury were to be very rare, then it may not be worth investing in finding a treatment that prevents it. The same applies if reperfusion injury were to be very common but does not substantially influence patient outcome. We currently know very little about the relative importance of the various post-recanalization tissue damage pathways when compared to each other.
What is the inter-individual variability in the importance of these mechanisms between patients? Some mechanisms may play a more dominant role in certain patients than in others. For example, hyperglycemia is known to destabilize the BBB, so BBB stabilizers may be more effective in patients with diabetes/hyperglycemic patients, since BBB breakdown is likely to be a more dominant tissue damage mechanism in diabetic patients.
What is the appropriate timing of administration for post-recanalization cerebroprotectants? Administration before EVT may be beneficial when it comes to agents that have additional cerebroprotective effects in the pre-recanalization time period. On the other hand, if the half-life of the cerebroprotectant under investigation is short, and its main effects are related to prevention of post-recanalization tissue damage mechanisms, it may be better to wait until after recanalization to achieve the maximum concentration of the cerebroprotectant at the time at which the target tissue damage mechanism occurs. A cerebroprotectant that diminishes late secondary changes and Wallerian degeneration may need to be administered even later and repeatedly over a period of time, days to weeks after the index stroke.
What is an appropriate outcome to measure the efficacy of post-recanalization cerebroprotectants? While clinical outcomes are the most meaningful of all outcome measures, conducting studies with clinical endpoints is time-, cost-, and labor-intensive. Furthermore, post-acute complications such as post-stroke pneumonia, pulmonary embolisms, and other unexpected events introduce noise that may dilute the treatment effect. Imaging outcomes can be obtained immediately after treatment, but while the risk of confounding is lower, the clinical relevance of such imaging surrogate outcomes may be questioned. Therefore, it may be advantageous to use a combination of both imaging surrogate outcomes and clinical outcomes in early phase II/proof-of-principle studies.
Table 3.
Challenges when conducting post-recanalization cerebroprotection trials
| Challenge | Explanation |
|---|---|
| Limited understanding of the prevalence of post-recanalization tissue damage mechanisms | We currently do not know how often the different post-recanalization tissue damage mechanisms occur after AIS and which variables influence their prevalence. We also have a limited understanding about which factors influence their prevalence (e.g., it is roughly known that BBB breakdown occurs more often if the time to recanalization is longer, but it would be desirable to quantify this in greater detail). Cerebroprotection trials should investigate agents that tackle common tissue damage mechanisms, while little, if any, effort should be spent on investigating cerebroprotectants that prevent tissue damage pathways which occur only in rare cases |
| Limited understanding of the importance of post-recanalization tissue damage mechanisms | Some tissue damage mechanisms may have a more detrimental effect on patient outcomes than others. It would be desirable to invest in trials assessing those cerebroprotectants that address the tissue damage mechanisms with the greatest impact on patient outcomes |
| Limited understanding of the inter-individual variability of post-recanalization tissue damage mechanisms | Some tissue damage mechanisms may be more prevalent, or may be more harmful for that matter, in some patients than in others. When assessing a cerebroprotectant in a clinical trial, in order to enhance the treatment effect, only those patients should be included in the trial that are most likely to suffer profoundly from the specific tissue damage mechanism(s) that the cerebroprotection under investigation aims to prevent |
| Uncertainty regarding imaging correlates for certain tissue damage mechanisms | It would be desirable to use imaging criteria for patient enrolment that allow us to choose those patients in which the tissue damage mechanism targeted by the cerebroprotectant under investigation is most prevalent. In order to do so, distinct imaging signatures for certain tissue damage mechanisms need to be established |
| Lack of histology proof for tissue damage mechanisms in humans | Histology proof for tissue damage mechanisms postulated on imaging cannot be obtained in human acute ischemic stroke since whole brain histology cannot be performed. Thus, no reliable radiology-pathology correlation is available for human post-recanalization tissue damage mechanisms |
| Uncertainty regarding the temporal evolution of tissue damage mechanisms | We do not exactly know the temporal evolution of the various tissue damage mechanisms and when they cause the most harm. Thus, there is uncertainty about the appropriate timing of cerebroprotectant administration |
| Problems with differentiating the different cerebroprotective effects in pleiotropic agents | While it is known that some cerebroprotectants, such as Dl-3-n-butylphthalide, have pleiotropic effects, there is currently no reliable way to find out which effect contributes to what degree to the overall effect |
| Uncertainty regarding the appropriate outcome for cerebroprotection studies | There is no consensus on what should be chosen as an outcome measure for cerebroprotection studies. While clinical outcomes are most relevant to patients, using clinical outcomes is prone to treatment effect dilution by post-stroke complications and other unrelated events. Imaging outcomes are more immediate outcome measures but their clinical relevance is not always entirely clear, and thus, their acceptability among clinicians, policymakers, and regulatory bodies is lower |
AIS acute ischemic stroke, BBB blood–brain barrier
Where Are We at and Where Are We Going?
We know that tissue death post-recanalization occurs due to several pathophysiologic pathways in the setting of AIS. Cerebroprotectants are drugs aiming to prevent or diminish tissue damage through these pathways and could in theory improve outcomes in human AIS [17]. Several promising post-recanalization cerebroprotectant candidates have been identified for each of the key tissue damage mechanisms. Many cerebroprotectants seem to have pleiotropic effects and interfere with several, rather than just one, tissue damage pathways, and some aim to prevent tissue damage both before and after recanalization. Exemplary cerebroprotectant candidates with their corresponding target tissue damage mechanisms and imaging signatures are shown in Table 2. Some have already been tested in humans, but to date, no cerebroprotectant is approved as for clinical use as an adjunct to EVT yet. The Stroke Academic Industry Roundtable (STAIR) has recognized cerebroprotection as one of the top priorities in stroke research and provided expert consensus recommendations on phase 2 cerebroprotection studies [47].
Table 2.
Tissue damage mechanisms, imaging correlates, and cerebroprotective candidates
| Tissue damage mechanism category | Detailed tissue damage mechanism | Presumed imaging correlates in humans | Example cerebroprotectant candidate | Current state of things |
|---|---|---|---|---|
| Incomplete reperfusion/microvascular obstruction | Clogging of arterioles and capillaries despite macroscopic recanalization of the occluded arteries due to microthrombi endothelial damage, astrocyte swelling, and pericyte constriction |
• Dynamic susceptibility MR perfusion parameters (prolongation of capillary transit time and increased capillary transit time heterogeneity, mean cerebral rate of metabolic oxygen, mean oxygen extraction fraction [48] • Reduced tissue perfusion may also be seen in CT perfusion maps to some extent |
Intra-arterial alteplase | Efficacy proven in human AIS as an adjunct after successful recanalization in the randomized controlled CHOICE trial [49] |
| Blood–brain barrier breakdown | Extravasation of blood and inflammatory markers from the intravascular into the extravascular space [50] |
• MRI hyperintense acute reperfusion marker (HARM) on post-contrast FLAIR [51] • Hemorrhagic transformation (Heidelberg classification on MRI and CT) [38] • Hemorrhage volume (on MRI and CT) [52] |
Dl-3-n-Butylphthalide [53] (has also other pleiotropic effects) [54, 55] | Improved clinical outcome has been shown in human AIS trials in several studies in the Chinese population [37, 56], and another large randomized trial (BAST) is ongoing (clinicaltrials.gov: NCT03539445). However, none of these trials specifically focuses on the post-recanalization scenario, and it is not clear which tissue damage mechanism (pre- and post-recanalization) is influenced to which extent by Dl-3-n-butylphthalide |
| Reperfusion injury | Post-recanalization tissue damage caused by invasion of reactive oxygen species, pro-inflammatory cytokines, leucocytes, and other cells/molecules into the previously ischemic tissue |
• Problematic because of large overlap of imaging features with other tissue damage mechanisms (BBB breakdown, microvascular obstruction) • (99 m)Tc-duramycin single-photon emission computerized tomography (SPECT), tested in animal models and not used in clinical routine [57] |
Veliparib (third-generation Parthanatos pathway inhibitor) [58] | Currently evaluated within the Stroke Pre-Clinical Assessment (SPAN) network [59]. Successfully evaluated in animal models, safety has been established in human oncology trials, no human AIS trials yet [59, 60] |
| Secondary changes and post-infarction atrophy | Atrophy and gliosis in areas connected with the infarct (Wallerian degeneration) and global loss of brain tissue |
• Wallerian degeneration: T1 hypointense, T2 hyperintense MRI signal changes and later volume loss in the ipsilateral cerebral peduncle and pons [61] • Global brain atrophy: best evaluated by using automated quantification/dedicated software [45, 46] |
No known cerebroprotectant candidate identified at the moment | - |
Key post-recanalization tissue damage mechanisms, presumed imaging correlates, and corresponding cerebroprotectant candidates
AIS acute ischemic stroke, BBB blood–brain barrier, FLAIR fluid attenuation inversion recovery
Hitherto, almost all of the above post-recanalization cerebroprotectant candidates are stuck in the pre-clinical phase, because fundamental questions with regard to the exact prevalence, importance, and inter-variability of the post-recanalization tissue damage mechanisms they are supposed to prevent have not been solved yet. Uncertainty regarding the most appropriate outcome measure and treatment timing constitute additional challenges. How can we choose the most promising cerebroprotectants to prevent post-recanalization tissue damage and design an appropriate clinical trial to prove its efficacy, if we lack the basic knowledge about the prevalence and timing of this particular tissue damage mechanism, its impact on clinical outcomes, and how this differs between patients, etc.? Key challenges and questions with regard to cerebroprotection trial design are outlined in Table 3 and summarized elsewhere in more detail [62]. None of these challenges is however unsurmountable, and many of the questions could be answered through longitudinal, observational prospective imaging studies. For a more detailed discussion on how such a longitudinal imaging study could be designed, we refer to a previous paper by our group [27]. In short, a standardized protocol of serial post-treatment MR imaging or, at the very least, an immediate post-procedure and one delayed time point MRI could provide valuable information regarding the prevalence and timing of post-recanalization tissue damage mechanisms, and a clinical outcome assessment at 24 h and 3 months would complement the study. This combination would also allow us to identify surrogate imaging outcomes with clinical relevance that could be used in future cerebroprotection trials. Complementary radiology-pathology correlation studies in animals, ideally higher order primates, using the same imaging protocol, would allow us to finally obtain histology proof for the various tissue damage imaging signatures. Animal models have successfully been used in AIS research for a long time [63, 64]. As an example, Zivin et al. proved efficacy of intravenous alteplase in a rabbit model in their 1985 landmark paper [65]. Such a hybrid animal-human/radiology-pathology study design would ultimately enable us to design cerebroprotection trials in an informed, thoughtful, and appropriate manner and thereby accelerate the translation of post-recanalization cerebroprotection from bench to bedside to further improve patient outcomes. Indeed, this hybrid design has already successfully been used in some instances, for example in the pre-clinical evaluation of Tat-NR2B9c, whereby a cynomolgus macaque stroke model was used to prove reduced infarct numbers and volumes following Tat-NR2B9c administration [66]. This animal model accurately anticipated the results of a corresponding human trial. It would however be wise to conduct hybrid studies to better understand the evolution of post-recanalization tissue damage first and improve our knowledge about the underlying pathophysiological mechanisms and their imaging correlates before proceeding to therapeutic trials. Otherwise, we continue to conduct cerebroprotection trials in the same haphazard manner and set ourselves up for failure.
Conclusion
Cerebroprotectants hold great potential as adjunctive treatments to further improve patient outcomes by preventing post-recanalization tissue damage. However, our current knowledge about the various post-recanalization tissue damage mechanisms, their prevalence, relative importance, and inter-individual variability is limited, thereby preventing us from accurately and reliably evaluating the efficacy of cerebroprotectants in clinical trials. To answer these fundamental questions, serial MRI is currently the best available imaging modality, as it is radiation-free and provides the most information of all currently used routine imaging methods. Serial MRI studies with complementary animal studies, ideally in higher order primates in order to identify radiology correlates of histological tissue damage patterns through histology-radiology correlation, should be first conducted before further investing into clinical cerebroprotection trials.
Supplementary Information
Below is the link to the electronic supplementary material.
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Declarations
Conflict of Interest
Johanna Ospel: travel grants from Cerenovus and the Norwegian Stroke Organization (not relevant to this work); Mayank Goyal: consultant for Medtronic, Microvention, Stryker, GE Healthcare and Mentice, unrestricted research grants from Microvention (not relevant to this work). Remaining authors: nothing to disclose.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Goyal M, Menon BK, Van Zwam WH, Dippel DWJ, Mitchell PJ, Demchuk AM, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. 2016;387(10029):1723–1731. doi: 10.1016/S0140-6736(16)00163-X. [DOI] [PubMed] [Google Scholar]
- 2.Goyal M, Almekhlafi MA, Cognard C, McTaggart R, Blackham K, Biondi A, et al. Which patients with acute stroke due to proximal occlusion should not be treated with endovascular thrombectomy? Neuroradiology. 2019;61(1):3–8. doi: 10.1007/s00234-018-2117-y. [DOI] [PubMed] [Google Scholar]
- 3.Ospel JM, Volny O, Jayaraman M, McTaggart R, Goyal M. Optimizing fast first pass complete reperfusion in acute ischemic stroke - the BADDASS approach (BAlloon guiDe with large bore Distal Access catheter with dual aspiration with Stent-retriever as Standard approach) Expert Rev Med Devices. 2019;16(11):955–963. doi: 10.1080/17434440.2019.1684263. [DOI] [PubMed] [Google Scholar]
- 4.Menon BK, Buck BH, Singh N, Deschaintre Y, Almekhlafi MA, Coutts SB, et al. Intravenous tenecteplase compared with alteplase for acute ischaemic stroke in Canada (AcT): a pragmatic, multicentre, open-label, registry-linked, randomised, controlled, non-inferiority trial. Lancet. 2022;400(10347):161–169. doi: 10.1016/S0140-6736(22)01054-6. [DOI] [PubMed] [Google Scholar]
- 5.Ganesh A, Menon BK, Assis ZA, Demchuk AM, Al-Ajlan FS, Al-Mekhlafi MA, et al. Discrepancy between post-treatment infarct volume and 90-day outcome in the ESCAPE randomized controlled trial. Int J Stroke. 2021;16(5):593–601. doi: 10.1177/1747493020929943. [DOI] [PubMed] [Google Scholar]
- 6.Lin C, Babiker A, Srdanovic N, Kocherginsky M, Harvey RL. Depressive symptoms after stroke are associated with worse recovery. Int J Psychiatry Med. 2020;55(4):227–238. doi: 10.1177/0091217420905459. [DOI] [PubMed] [Google Scholar]
- 7.Cho TH, Nighoghossian N, Mikkelsen IK, Derex L, Hermier M, Pedraza S, et al. Reperfusion within 6 hours outperforms recanalization in predicting penumbra salvage, lesion growth, final infarct, and clinical outcome. Stroke. 2015;46(6):1582–1589. doi: 10.1161/STROKEAHA.114.007964. [DOI] [PubMed] [Google Scholar]
- 8.Wu KC, Zerhouni EA, Judd RM, Lugo-Olivieri CH, Barouch LA, Schulman SP, et al. Prognostic significance of microvascular obstruction by magnetic resonance imaging in patients with acute myocardial infarction. Circulation. 1998;97(8):765–772. doi: 10.1161/01.CIR.97.8.765. [DOI] [PubMed] [Google Scholar]
- 9.Ng FC, Coulton B, Chambers B, Thijs V. Persistently elevated microvascular resistance postrecanalization. Stroke. 2018;49(10):2512–2515. doi: 10.1161/STROKEAHA.118.021631. [DOI] [PubMed] [Google Scholar]
- 10.Dalkara T, Arsava EM. Can restoring incomplete microcirculatory reperfusion improve stroke outcome after thrombolysis? J Cereb Blood Flow Metab. 2012;32(12):2091–2099. doi: 10.1038/jcbfm.2012.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Goyal M, Fargen KM, Turk AS, Mocco J, Liebeskind DS, Frei D, et al. 2C or not 2C: defining an improved revascularization grading scale and the need for standardization of angiography outcomes in stroke trials. J Neurointerv Surg. 2014;6(2):83. doi: 10.1136/neurintsurg-2013-010665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jayaraman MV, Grossberg JA, Meisel KM, Shaikhouni A, Silver B. The clinical and radiographic importance of distinguishing partial from near-complete reperfusion following intra-arterial stroke therapy. AJNR Am J Neuroradiol. 2013;34(1):135–139. doi: 10.3174/ajnr.A3278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tung EL, McTaggart RA, Baird GL, Yaghi S, Hemendinger M, Dibiasio EL, et al. Rethinking thrombolysis in cerebral infarction 2b: which thrombolysis in cerebral infarction scales best define near complete recanalization in the modern thrombectomy era? Stroke. 2017;48(9):2488–2493. doi: 10.1161/STROKEAHA.117.017182. [DOI] [PubMed] [Google Scholar]
- 14.Ospel JM, Goyal M. A review of endovascular treatment for medium vessel occlusion stroke. J Neurointerv Surg. 2021;13(7):623–630. doi: 10.1136/neurintsurg-2021-017321. [DOI] [PubMed] [Google Scholar]
- 15.Dargazanli C, Fahed R, Blanc R, Gory B, Labreuche J, Duhamel A, et al. Modified thrombolysis in cerebral infarction 2C/thrombolysis in cerebral infarction 3 reperfusion should be the aim of mechanical thrombectomy: insights from the ASTER trial (Contact Aspiration Versus Stent Retriever for Successful Revascularization) Stroke. 2018;49(5):1189–1196. doi: 10.1161/STROKEAHA.118.020700. [DOI] [PubMed] [Google Scholar]
- 16.Liebeskind DS, Bracard S, Guillemin F, Jahan R, Jovin TG, Majoie CB, et al. eTICI reperfusion: defining success in endovascular stroke therapy. J Neurointerv Surg. 2019;11(5):433–438. doi: 10.1136/neurintsurg-2018-014127. [DOI] [PubMed] [Google Scholar]
- 17.Hill MD, Goyal M, Menon BK, Nogueira RG, McTaggart RA, Demchuk AM, et al. Efficacy and safety of nerinetide for the treatment of acute ischaemic stroke (ESCAPE-NA1): a multicentre, double-blind, randomised controlled trial. Lancet. 2020;395(10227):878–887. doi: 10.1016/S0140-6736(20)30258-0. [DOI] [PubMed] [Google Scholar]
- 18.Nielsen M, Waldmann M, Frolich AM, Flottmann F, Hristova E, Bendszus M, et al. Deep learning-based automated thrombolysis in cerebral infarction scoring: a timely proof-of-principle study. Stroke. 2021;52(11):3497–3504. doi: 10.1161/STROKEAHA.120.033807. [DOI] [PubMed] [Google Scholar]
- 19.Liebeskind DS, Bracard S, Guillemin F, Jahan R, Jovin TG, Majoie CB, et al. eTICI reperfusion: defining success in endovascular stroke therapy. J Neurointerv Surg. 2018. [DOI] [PubMed]
- 20.Alaka SA, Menon BK, Brobbey A, Williamson T, Goyal M, Demchuk AM, et al. Functional outcome prediction in ischemic stroke: a comparison of machine learning algorithms and regression models. Front Neurol. 2020;11. [DOI] [PMC free article] [PubMed]
- 21.Menon BK, d’Esterre CD, Qazi EM, Almekhlafi M, Hahn L, Demchuk AM, et al. Multiphase CT angiography: a new tool for the imaging triage of patients with acute ischemic stroke. Radiology. 2015;275(2):510–520. doi: 10.1148/radiol.15142256. [DOI] [PubMed] [Google Scholar]
- 22.Heit JJ, Wintermark M. Perfusion computed tomography for the evaluation of acute ischemic stroke: strengths and pitfalls. Stroke. 2016;47(4):1153–1158. doi: 10.1161/STROKEAHA.116.011873. [DOI] [PubMed] [Google Scholar]
- 23.Struffert T, Deuerling-Zheng Y, Kloska S, Engelhorn T, Strother CM, Kalender WA, et al. Flat detector CT in the evaluation of brain parenchyma, intracranial vasculature, and cerebral blood volume: a pilot study in patients with acute symptoms of cerebral ischemia. AJNR Am J Neuroradiol. 2010;31(8):1462–1469. doi: 10.3174/ajnr.A2083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sheiman RG, Sitek A. CT perfusion imaging: know its assumptions and limitations. Radiology. 2008;246(2):649. doi: 10.1148/radiol.2462070728. [DOI] [PubMed] [Google Scholar]
- 25.Ospel JM, Qiu W, Goyal M. Missed medium-vessel occlusions on CT angiography: make it easier … easily! AJNR Am J Neuroradiol. 2020;41(9):E73–E74. doi: 10.3174/ajnr.A6670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kranz PG, Eastwood JD. Does diffusion-weighted imaging represent the ischemic core? An evidence-based systematic review. AJNR Am J Neuroradiol. 2009;30(6):1206–1212. doi: 10.3174/ajnr.A1547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Goyal M, McTaggart R, Ospel JM, van der Lugt A, Tymianski M, Wiest R, et al. How can imaging in acute ischemic stroke help us to understand tissue fate in the era of endovascular treatment and cerebroprotection? Neuroradiology. 2022;64(9):1697–1707. doi: 10.1007/s00234-022-03001-z. [DOI] [PubMed] [Google Scholar]
- 28.Petrella JR, Provenzale JM. MR perfusion imaging of the brain: techniques and applications. AJR Am J Roentgenol. 2000;175(1):207–219. doi: 10.2214/ajr.175.1.1750207. [DOI] [PubMed] [Google Scholar]
- 29.Kosior JC, Buck B, Wannamaker R, Kate M, Liapounova NA, Rempel JL, et al. Exploring reperfusion following endovascular thrombectomy. Stroke. 2019;50(9):2389–2395. doi: 10.1161/STROKEAHA.119.025537. [DOI] [PubMed] [Google Scholar]
- 30.De Silva DA, Fink JN, Christensen S, Ebinger M, Bladin C, Levi CR, et al. Assessing reperfusion and recanalization as markers of clinical outcomes after intravenous thrombolysis in the echoplanar imaging thrombolytic evaluation trial (EPITHET) Stroke. 2009;40(8):2872–2874. doi: 10.1161/STROKEAHA.108.543595. [DOI] [PubMed] [Google Scholar]
- 31.Tsai JP, Mlynash M, Christensen S, Kemp S, Kim S, Mishra NK, et al. Time from imaging to endovascular reperfusion predicts outcome in acute stroke. Stroke. 2018;49(4):952–957. doi: 10.1161/STROKEAHA.117.018858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cook DJ, Teves L, Tymianski M. Treatment of stroke with a PSD-95 inhibitor in the gyrencephalic primate brain. Nature. 2012;483(7388):213–217. doi: 10.1038/nature10841. [DOI] [PubMed] [Google Scholar]
- 33.Sah RG, Nobakht S, Rajashekar D, Mouches P, Forkert ND, Sitaram A, et al. Temporal evolution and spatial distribution of quantitative T2 MRI following acute ischemia reperfusion injury. Int J Stroke. 2020;15(5):495–506. doi: 10.1177/1747493019895673. [DOI] [PubMed] [Google Scholar]
- 34.Bunevicius A, Yuan H, Lin W. The potential roles of 18F-FDG-PET in management of acute stroke patients. Biomed Res Int. 2013;2013:634598. doi: 10.1155/2013/634598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dani KA, An L, Henning EC, Shen J, Warach S. Multivoxel MR spectroscopy in acute ischemic stroke: comparison to the stroke protocol MRI. Stroke. 2012;43(11):2962–2967. doi: 10.1161/STROKEAHA.112.656058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zille M, Farr TD, Przesdzing I, Müller J, Sommer C, Dirnagl U, et al. Visualizing cell death in experimental focal cerebral ischemia: promises, problems, and perspectives. J Cereb Blood Flow Metab. 2012;32(2):213–231. doi: 10.1038/jcbfm.2011.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nian K, Harding IC, Herman IM, Ebong EE. Blood-brain barrier damage in ischemic stroke and its regulation by endothelial mechanotransduction. Front Physiol. 2020;11:605398. doi: 10.3389/fphys.2020.605398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.von Kummer R, Broderick JP, Campbell BC, Demchuk A, Goyal M, Hill MD, et al. The Heidelberg bleeding classification: classification of bleeding events after ischemic stroke and reperfusion therapy. Stroke. 2015;46(10):2981–2986. doi: 10.1161/STROKEAHA.115.010049. [DOI] [PubMed] [Google Scholar]
- 39.Hoffmann A, Dege T, Kunze R, Ernst AS, Lorenz H, Bohler LI, et al. Early blood-brain barrier disruption in ischemic stroke initiates multifocally around capillaries/venules. Stroke. 2018;49(6):1479–1487. doi: 10.1161/STROKEAHA.118.020927. [DOI] [PubMed] [Google Scholar]
- 40.Tiwari YV, Lu J, Shen Q, Cerqueira B, Duong TQ. Magnetic resonance imaging of blood-brain barrier permeability in ischemic stroke using diffusion-weighted arterial spin labeling in rats. J Cereb Blood Flow Metab. 2017;37(8):2706–2715. doi: 10.1177/0271678X16673385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Niibo T, Ohta H, Miyata S, Ikushima I, Yonenaga K, Takeshima H. Prediction of blood-brain barrier disruption and intracerebral hemorrhagic infarction using arterial spin-labeling magnetic resonance imaging. Stroke. 2017;48(1):117–122. doi: 10.1161/STROKEAHA.116.013923. [DOI] [PubMed] [Google Scholar]
- 42.Nour M, Scalzo F, Liebeskind DS. Ischemia-reperfusion injury in stroke. Interv Neurol. 2013;1(3–4):185–199. doi: 10.1159/000353125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Xu S, Lu J, Shao A, Zhang JH, Zhang J. Glial cells: role of the immune response in ischemic stroke. Front Immunol. 2020;11:294. doi: 10.3389/fimmu.2020.00294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Brodtmann A, Khlif MS, Egorova N, Veldsman M, Bird LJ, Werden E. Dynamic regional brain atrophy rates in the first year after ischemic stroke. Stroke. 2020;51(9):e183–e192. doi: 10.1161/STROKEAHA.120.030256. [DOI] [PubMed] [Google Scholar]
- 45.Gunter JL, Shiung MM, Manduca A, Jack CR., Jr Methodological considerations for measuring rates of brain atrophy. J Magn Reson Imaging. 2003;18(1):16–24. doi: 10.1002/jmri.10325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Smeets D, Ribbens A, Sima DM, Cambron M, Horakova D, Jain S, et al. Reliable measurements of brain atrophy in individual patients with multiple sclerosis. Brain Behav. 2016;6(9):e00518. doi: 10.1002/brb3.518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lyden P, Buchan A, Boltze J, Fisher M, STAIR XI Consortium Top priorities for cerebroprotective studies-a paradigm shift: report from STAIR XI. Stroke. 2021;52(9):3063–3071. doi: 10.1161/STROKEAHA.121.034947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hansen MB, Tietze A, Kalpathy-Cramer J, Gerstner ER, Batchelor TT, Østergaard L, et al. Reliable estimation of microvascular flow patterns in patients with disrupted blood-brain barrier using dynamic susceptibility contrast MRI. J Magn Reson Imaging. 2017;46(2):537–549. doi: 10.1002/jmri.25549. [DOI] [PubMed] [Google Scholar]
- 49.Renu A, Millan M, San Roman L, Blasco J, Marti-Fabregas J, Terceno M, et al. Effect of intra-arterial alteplase vs placebo following successful thrombectomy on functional outcomes in patients with large vessel occlusion acute ischemic stroke: the CHOICE randomized clinical trial. JAMA. 2022;327(9):826–835. doi: 10.1001/jama.2022.1645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Krueger M, Hartig W, Frydrychowicz C, Mueller WC, Reichenbach A, Bechmann I, et al. Stroke-induced blood-brain barrier breakdown along the vascular tree - no preferential affection of arteries in different animal models and in humans. J Cereb Blood Flow Metab. 2017;37(7):2539–2554. doi: 10.1177/0271678X16670922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Choi HY, Lee KM, Kim HG, Kim EJ, Choi WS, Kim BJ, et al. Role of hyperintense acute reperfusion marker for classifying the stroke etiology. Front Neurol. 2017;8:630. doi: 10.3389/fneur.2017.00630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ospel JM, Qiu W, Menon BK, Mayank A, Demchuk A, McTaggart R, et al. Radiologic patterns of intracranial hemorrhage and clinical outcome after endovascular treatment in acute ischemic stroke: results from the ESCAPE-NA1 trial. Radiology. 2021;300(2):402–409. doi: 10.1148/radiol.2021204560. [DOI] [PubMed] [Google Scholar]
- 53.Bi M, Zhang M, Guo D, Bi W, Liu B, Zou Y, et al. N-Butylphthalide alleviates blood-brain barrier impairment in rats exposed to carbon monoxide. Front Pharmacol. 2016;7:394. doi: 10.3389/fphar.2016.00394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Li J, Liu Y, Zhang X, Chen R, Zhang L, Xue J, et al. Dl-3-N-Butylphthalide alleviates the blood-brain barrier permeability of focal cerebral ischemia reperfusion in mice. Neuroscience. 2019;413:99–107. doi: 10.1016/j.neuroscience.2019.06.020. [DOI] [PubMed] [Google Scholar]
- 55.Wang Y, Shen Y, Liu Z, Gu J, Xu C, Qian S, et al. Dl-NBP (Dl-3-N-Butylphthalide) treatment promotes neurological functional recovery accompanied by the upregulation of white matter integrity and HIF-1alpha/VEGF/Notch/Dll4 expression. Front Pharmacol. 2019;10:1595. doi: 10.3389/fphar.2019.01595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Cui LY, Zhu YC, Gao S, Wang JM, Peng B, Ni J, et al. Ninety-day administration of dl-3-n-butylphthalide for acute ischemic stroke: a randomized, double-blind trial. Chin Med J (Engl) 2013;126(18):3405–3410. [PubMed] [Google Scholar]
- 57.Zhang Y, Stevenson GD, Barber C, Furenlid LR, Barrett HH, Woolfenden JM, et al. Imaging of rat cerebral ischemia-reperfusion injury using(99m)Tc-labeled duramycin. Nucl Med Biol. 2013;40(1):80–88. doi: 10.1016/j.nucmedbio.2012.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Koehler RC, Dawson VL, Dawson TM. Targeting parthanatos in ischemic stroke. Front Neurol. 2021;12:662034. doi: 10.3389/fneur.2021.662034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.SPAN. Stroke Pre-Clinical Assessment Network (SPAN) 2022. Available from: https://spannetwork.org/Interventions. Accessed 21 Mar 2023.
- 60.Fisher M, Savitz SI. Pharmacological brain cytoprotection in acute ischaemic stroke - renewed hope in the reperfusion era. Nat Rev Neurol. 2022;18(4):193–202. doi: 10.1038/s41582-021-00605-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Inoue Y, Matsumura Y, Fukuda T, Nemoto Y, Shirahata N, Suzuki T, et al. MR imaging of Wallerian degeneration in the brainstem: temporal relationships. AJNR Am J Neuroradiol. 1990;11(5):897–902. [PMC free article] [PubMed] [Google Scholar]
- 62.Lyden PD. Cerebroprotection for acute ischemic stroke: looking ahead. Stroke. 2021;52(9):3033–3044. doi: 10.1161/STROKEAHA.121.032241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Fluri F, Schuhmann MK, Kleinschnitz C. Animal models of ischemic stroke and their application in clinical research. Drug Des Devel Ther. 2015;9:3445–3454. doi: 10.2147/DDDT.S56071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hermann DM, Popa-Wagner A, Kleinschnitz C, Doeppner TR. Animal models of ischemic stroke and their impact on drug discovery. Expert Opin Drug Discov. 2019;14(3):315–326. doi: 10.1080/17460441.2019.1573984. [DOI] [PubMed] [Google Scholar]
- 65.Zivin JA, Fisher M, DeGirolami U, Hemenway CC, Stashak JA. Tissue plasminogen activator reduces neurological damage after cerebral embolism. Science. 1985;230(4731):1289–1292. doi: 10.1126/science.3934754. [DOI] [PubMed] [Google Scholar]
- 66.Cook DJ, Teves L, Tymianski M. A translational paradigm for the preclinical evaluation of the stroke neuroprotectant Tat-NR2B9c in gyrencephalic nonhuman primates. Sci Transl Med. 2012;4(154):154ra33. doi: 10.1126/scitranslmed.3003824. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.