Abstract
Background
Quality of life is an important concept which is subjective and personal; what is an acceptable quality of life to one may be 'worse than death' to another. The objective of this study was to develop and validate a questionnaire to assess relatives' perceptions and attitudes towards their terminal stage cancer patients' management (information disclosure, treatment choice, hospitalization and support-communication and care) including aspects regarding end-of-life and quality-of-life decisions.
Methods
The final study consisted of 146 relatives of advanced terminal stage cancer patients receiving palliation, attending a Pain Relief and Palliative Care Unit. The questionnaire incorporated 6 multi-item and 7 single-item scales, and was developed following a systematic review of measures appropriate for use in palliative care settings.
Results
Following analysis of the 25-item scale, the questionnaire has been validated as a shortened 21-item scale consisting of 5 multi-item and 5 single-item scales. Factor analysis was based upon information disclosure, hospitalization, and support-communication demonstrating Cronbach's alpha coefficients of 0.66, 0.5 and 0.70 respectively. Average item totals and inter-item scale correlations were between 0.62–0.70, with convergent validity correlations between 0.60–0.86. The questionnaire was well accepted by all subjects with an 8–10 minute completion time.
Conclusion
The shortened 21-item self-assessment questionnaire may provide acceptable and valid assessment of caregiver(s)/Greek cancer patients' relatives perceptions on palliative care.
Background
Quality of life is an important clinical outcome in assessing the efficacy of health care. It is a concept that includes many subjective elements: physical, emotional and social function, attitudes to illness, patients' daily lives-including family interactions, Spitzer, Dobson, et al. [1], Cella and Tulsky [2].
Treatments that are designed to control symptoms are suited for Quality of Life end points. When the goal of treatment is symptom palliation rather than prolongation, the use of Quality of Life as a primary end point of survival can be considered, Winer [3]. As a result of the increased interest in the impact of disease and treatment on the patient's life and functioning, several well-validated questionnaires that measure health-related quality of life (HRQoL) have been developed, some of which formed the foundation for the questionnaire that was used in this study [4][5][6][7].
Cancer is not a disease of an individual but impacts the family system. Families must confront, and attempt to realize the meaning of cancer for the patient, for each family member individually and for the family system as a whole [8]. The diagnosis of cancer confronts both the patient and his/her caregiver(s) with a major life crisis, therefore family therapists now refer to the 'cancer family' and not to the 'cancer personality' [9]. Furthermore, as a life-threatening disease progresses, family members may assume new roles and responsibilities. They are usually supportive or concerned for their terminally ill patients, but they are frequently opposed to the patient's wishes or the recommendations of the treatment team. When the patient is incompetent, conflicts of interest may arise since decision-making is a great responsibility for the family [10]. A relative, who feels guilty or denies the hopelessness of the situation, may press the patient for cure rather than care, or to prolong or discontinue treatment [11].
It is worth noting, that every patient and family has a culture. Cultural aspects of values and behaviors are the key variables, along with life experiences, socio-economic status, and personality differences, that affect the meaning of cancer for both individuals and their families, as well as how they cope with the disease [10][12][13]. Thus, it is important to mention the close bonds found in a Greek family, especially towards severe problems such as cancer [14]. Furthermore, when relatives know the truth and try to keep it from their patients, they are likely to transmit their fears and anxiety through non-verbal ways. The cost of deception is high. For the patient who suspects but still hopes, the state of uncertainty is harder to bear than the certainty of the knowledge [15][16]. This attitude of non-disclosure is not only associated with Greek culture but has also been observed in Japan [17][18][19]. Denying acceptance of the disease, family members even avoid discussing about cancer [20][21].
The objectives of this study were to investigate the attitudes, perceptions and patterns of choice in the management of terminal stage cancer patients with respect to their families through the development of a relatives' patient management questionnaire. Typically HRQoL questionnaires assessing the patients' perceptions and choices are used to determine choice of treatment and palliation, however, with the realization that cancer families are also affected and involved by the disease and its management their perceptions of management choices are becoming important considerations in oncology.
Methods
The study took place in the Pain Relief and Palliative Care Unit, of Areteion Hospital, in University of Athens. The study was carried out between March and September 2000, with hospital ethics committee approval. During this time 400 relatives of advanced cancer patients visited the Unit, from all over Greece. The questionnaire was randomly distributed to 146 Greek relatives who approached the Unit for pain relief and the control of other cancer related symptoms. It was drawn using stratified random sampling, based upon the level of first-degree relatedness, i.e. spouse, child, sibling, parent.
Inclusion criteria were a) first-degree relative, b) mentally capable, c) informed consent.
The relatives were asked to complete the questionnaire in the outpatient unit, and were given brief instructions on how to complete the questionnaire (particularly Question 3). The initial measurement consisted of 25-item questions, composed of 6 multi-item scales, and 7 single item scales. Twelve of the scales were presented into 3 optional statements to be scored "yes", "sometimes", "no", and the relatives were asked to mark the appropriate answer accordingly. Question number 3 consisted of 7 factors and relatives had to mark their choice in a hierarchical order. The questionnaire was designed to be self-assessment and was formulated after a thorough review of the relevant literature, incorporating previously validated questions from other scales and measures appropriate for use in palliative care settings for the assessment of relatives' patient management perceptions and choices [4][5][6][7]. The questionnaire contained 4 sections with different aspects of consultation: information disclosure (Qs, 1, 2, 4, 8); therapy choices (Q 3); support-communication and care (Qs, 5, 6, 7, 9 and 13) and hospitalization (Qs, 10, 11, 12). Patients' medical records provided information about demographics and disease characteristics, specifically: type of cancer, presence of metastasis, and Karnofsky performance. Similar demographic data was obtained from the relatives: age and sex, with stratification based upon degree of relatedness, spouse, child, parent, sibling; educational status, primary, high school and university; residence, rural, village and town. Multivariate analysis was conducted on these stratifications. However, no analysis was conducted for the stratification residence, as only 10 relatives did not reside in the town. Relatives were also timed during the completion of the questionnaire.
Quantitative variables are described by the mean ± standard deviation. Quantitative aspects were analyzed using t-test, one-way and two-way analysis of variance (ANOVA) and categorical variables by Pearson's chi-square, where appropriate. The reliability and validity was assessed by average inter-item and average item totals and Cronbach's alpha. Statistical significance was accepted with p ≤ 0.05.
Results
The patients' survival time was between 4 months to 5 years (median: 2 years) while they were off anti-cancer treatment and under palliative care for symptom control. Socio-demographic and clinical data for patients and relatives are presented in Table 1. In all the questions, except for question number 3, the rate of answers given was 100%, the average time required to complete the questionnaire was 8–10 minutes. Regarding question number 3, 15% of responders did not complete this question.
Table 1.
Socio-demographic characteristics
| Relatives' Age (mean, ± s.d) | Range | ||
| 48 ± 15 | 19–80 | ||
| N | % | ||
| Sex | Male | 39 | 27 |
| Female | 107 | 73 | |
| Education | Primary | 22 | 15 |
| High School | 73 | 50 | |
| University | 51 | 35 | |
| Patients' Sex | Male | 88 | 60 |
| Female | 58 | 40 | |
| Patients' Age (mean, ± s.d) | Range | ||
| 67 ± 12 | 30–98 | ||
| N | % | ||
| Cancer Locations | Lung | 38 | 27 |
| Pancreatic | 18 | 12 | |
| Rectum | 15 | 10 | |
| Bladder | 14 | 10 | |
| Other | 61 | 42 | |
Descriptive statistics for the questionnaire are presented in Table 2, for all questions except question 3. Some points of interest that derive from Table 2 include the following. First, a small percentage (23%) of relatives believe that diagnosis and prognosis should be revealed to the patients, while the majority (56% and 51% respectively) of the participants believe that only "sometimes" they would agree to do so. However, they are of the opinion that the patients should be given information on the possible treatment choices (71%) and the complications or side effects of the treatment (53%). A large percentage (81.5%) would like a health care team to be involved in caring for their patients, and 76% would like physicians from various specialties to co-operate, when this is judged necessary, and 78% of relatives would like the assistance of a social worker. However, only 44% would choose psychological support from specialists, even though 34% answered that they "sometimes" prefer the cooperation with psychologists. Several family members (67%), indicated that they would prefer to inform their patients of the palliative nature of the treatment, but only 44% would discuss with them their fears on death, with 28% "sometimes" choosing to discuss about it and 28% not. Only 30% chose the intensive care unit for a patient in the terminal stage, while 57% preferred the patients to stay at home with the provision of the appropriate care. It is worth mentioning that close communication and support are variables, which are now starting to be considered seriously from the vast majority of the relatives (96%).
Table 2.
Relatives' attitudes towards their patients' quality of life
| Questionnaire items | Percentage (%) of Relatives' | |||||
| Responding 'yes' | n | 'sometimes' | n | 'no' | n | |
| 1) Do you believe that patient should fully be informed | ||||||
| a) for the diagnosis? | 23% | 34 | 56% | 82 | 20.5% | 30 |
| b) for the prognosis of the disease? | 23% | 34 | 51% | 74 | 26% | 38 |
| 2) Do you agree the patient to be informed | ||||||
| a) for the possible treatment choices? | 71% | 104 | 24% | 35 | 5% | 7 |
| b) for the percentage effectiveness? | 51% | 74 | 37% | 54 | 12% | 18 |
| c) for the complications or the side-effects of the treatment? | 53% | 77 | 33% | 48 | 15% | 21 |
| 4) Do you believe that patient should be informed before amputative/disfiguring operations? | 68.5% | 100 | 21% | 31 | 10% | 15 |
| 5) Would you like for the caring and treatment of cancer patients to be involved | ||||||
| a) the health care team? | 81.5% | 119 | 16% | 24 | 2.% | 3 |
| b) physicians from various specialties Cooperating as necessary? | 76% | 111 | 12% | 17 | 12% | 18 |
| 6) Would you like to cooperate with psychological support specialists? | 44% | 64 | 34% | 50 | 22% | 32 |
| 7) Would you like to cooperate with a social worker? | 78% | 114 | 19% | 28 | 3% | 4 |
| 8) In the final stage of the patient would you prefer to inform him/her for the palliative nature of the treatment? | 67% | 98 | 24% | 35 | 9% | 13 |
| 9) Would you like to discuss with the patient his/her fears on death? | 44% | 64 | 28% | 41 | 28% | 41 |
| 10) In order to prolong the life of cancer patient for a few days in the final stage, would you choose the intensive care unit? | 30% | 44 | 1 30% | 44 | 39% | 58 |
| 11) Do you believe that the advanced cancer patient when he/she receives the appropriate care should: | ||||||
| a) be hospitalized | 32% | 47 | 30% | 44 | 38% | 55 |
| b) remain at home | 57% | 83 | 23% | 34 | 20% | 29 |
| 12) According to your opinion, the dying patient should: | ||||||
| a) remain at hospital? | 34% | 50 | 34% | 50 | 31.5* | 46 |
| b) die at home? | 41% | 60 | 29% | 42 | 30% | 44 |
| 13) In order to prolong the life of cancer patient for a few days in the final stage, is communication and support from the relatives and friends important? | 96% | 140 | 4% | 6 | 0 | 0 |
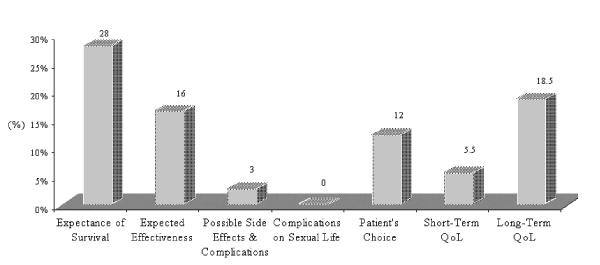
The results of question number 3 "choice of the medical treatment" are presented in Table 3 (the distribution of factors influencing choice of treatment in a hierarchical order), and the percentage first choice for each of the items is depicted in Figure 1. According to the participants, the first choice on the hierarchy is the factor " expectance of survival" (28%), while only an 18.5% chose the factor of "long term quality of life" as first in the hierarchy. The most common second factor is "expected effectiveness" (28%). The "long-term quality of life", depicts third place (19%), while 18.5% chose the factor of "expected effectiveness". The patients' "short-term quality of life" comes forth in the hierarchy (21%), while the factor of "possible complications and side effects" comes fifth (20.5%). The latter, also occupies the sixth place in the hierarchical ranking (23%). As the most common lowest ranked factor was, "consequences in the patients' sexuality" (63%).
Table 3.
Ranking variables of treatment choices
| Expectance of survival | Expected Effectiveness | Complications Side-effects | Consequences in sexuality | Patient's Choice | Short term QoL | Long term QoL | |
| Choices | |||||||
| 1st | 41 (28%) | 24(16%) | 4 (3%) | 0 | 18(12%) | 8 (5.5%) | 27(18.5%) |
| 2nd | 20 (14%) | 41 (28%) | 5 (3%) | 0 | 11(7.5%) | 20(13.5%) | 27(18.5%) |
| 3rd | 20 (14%) | 27(18.5%) | 17(12%) | 0 | 18(12%) | 12 (8%) | 28 (19%) |
| 4th | 23 (16%) | 12 (8%) | 26(18%) | 4 (3%) | 17(11.5%) | 31 (21%) | 11(7.5%) |
| 5th | 5 (3%) | 17(11.5%) | 30 (20.5%) | 2 (1%) | 24(16%) | 28(19%) | 17(11.5%) |
| 6th | 12 (8%) | 2 (1%) | 34 (23%) | 26(18%) | 28(19%) | 14 (9.5%) | 7 (5%) |
| 7th | 3 (2%) | 0 | 6 (4%) | 92 (63%) | 8 (5.5%) | 11 (7.5%) | 4 (3%) |
| missing | 22 (15%) | 22(15%) | 22(15%) | 22 (15%) | 22(15%) | 22(15%) | 22(15%) |
Figure 1.
First choices from each factor in "choice of the medical treatment".
Reliability of the three different aspects of consultation: information disclosure (Qs, 1, 2, 4, 8), support-communication and care (Qs, 5, 6, 7, 9 and 13) and hospitalisation (Qs, 10, 11, 12) (scales) were assessed by average inter-item correlation, average item total correlation and Cronbach's alpha. This initial analysis prompted shortening of the questionnaire via the removal of questions 6 and 13 from the support-communication and care group, and question 12 from the hospitalisation group. This shortening of the questionnaire resulted in improving the average all item total and inter-item correlations to between 0.62–0.70. The internal-consistency reliability coefficients, Cronbach's alpha correlations, for the three scales were: information disclosure (Qs, 1, 2, 4, 8) 0.66, support-communication and care (Qs, 5, 6 and 7) 0.69 and hospitalisation (Qs, 10 and 11) 0.50. Using these shortened scales the construct validity revealed that the items were sensibly related to the domains that contained them (convergent validity correlations between 0.6–0.86) and had no association with items from different domains (discriminate validity). This reappraisal of the questionnaire has resulted in the generation of a 21-item scale consisting of 5 multi-item and 5 single-item scales, which demonstrates acceptable validity in assessing relatives' perceptions and choices for the palliative management of terminal stage cancer patients.
Multivariate analysis of the socio-demographic data was conducted for all remaining scales. For question 3, higher scores were placed on all factors except "patient's long term quality of life" ranked in the order University > High School > Primary (0.001 > p > 0.02, ANOVA). A similar trend, Child > Spouse, was observed for relatedness (as only one relative was a parent and 9 were siblings theses were not included in the analysis) with significance reached in "consequences in patients sexuality", "the patients choice" and "patient's short term quality of life" (p= 0.007, 0.003 and 0.009, respectively; t-test).
With respect to relatedness, statistical significantly more child than spouse favored "yes" to questions 1b) "for the prognosis of the disease", 2b) "for the percentage of effectiveness", 4) "amputative/disfiguring operations" and 5b) "physicians from various specialties" (p = 0.001, 0.036, 0.06 and 0.05 respectively, chi-square). Stratification in relation to the sex of the relative demonstrated significance towards men answering "yes" to Ib) "for the prognosis of the disease", 10) "final stage.... intensive care unit" and 11b) "remain at home" (p = 0.012, 0.016 and 0.048 respectively). For women answering "yes" 2a) "for possible treatment choices" and 4) "amputative/disfiguring operations" (p = 0.037 and 0.010 respectively). As for educational status there was a clearly more pronounced firm "yes" to various questions with higher educational status (University > High school > Primary) for questions 2c) " complications or side-effects of the treatment", 4) "amputative/disfiguring operations", 5a) "the health care team", 5b) "physicians from various specialties", 7) "cooperate with social worker", 8) "inform him/her for the palliative nature of the treatment", 11b) "remain at home" (p = 0.028, 0.001, 0.017, 0.018, 0.024, 0.007 and 0.002 respectively); however the reverse rank order (University < High school < Primary) was observed for 10) "final stage....intensive care unit" and 11a) "be hospitalized" (p = 0.001).
Discussion
Traditionally, studies concerning cancer have focused on the effects of diagnosis, prognosis, treatment or the course of the disease on patients' well-being which refers to psychological as well as social and physical well-being, components referred to as quality of life, Bloom [22], Lewis and Bloom [23], Meyerowitz [24], Penman, Bloom et al [25]. Most clinicians recognize that cancer is painful for patients and their families, but surprisingly there is little research to document this effect. Most of the studies in this area examine the quality of life according to patient assessments, Covinsky, Goldman et al [26].
In this article the assessment and validation of a questionnaire designed to assess terminal stage cancer patient family perceptions and choices in patient management (information disclosure, therapy choices, hospitalization, support-communication and care) including aspects regarding end-of-life and quality-of-life decisions are presented. The goals of palliative treatment are to improve patients' functioning and their quality of life [15], input from relatives may offer additional measures in this respect.
The questionnaire was well accepted by all the relatives that approached the unit. On average, it required 8–10 minutes to complete, and relatives appeared to be pleased that they could have the opportunity to participate in a study examining their patients' quality of life. Following completion of the survey, the reliability and validity of the questionnaire was assessed by average inter-item and average item totals and Cronbach's alpha. Re-appraisal of both the support-communication and care and the hospitalization sections indicated that by shortening the initial 25-item scale to a 21-item scale generated a questionnaire that demonstrates acceptable validity and reliability.
In assessing the benefits of the treatment of a fatal illness, health care professionals need to know about the quality of survival. Withholding the truth from a patient appears common in Greece [27], as reported in other nations Niimi [17], [18][19]; with more information given in the U.S.A and U.K [28][29]. Many studies suggest that most patients would like to be informed about the diagnosis and prognosis of their disease [30], and evidence suggests that there is little benefit in withholding such disclosure [17][18][31]. Frequently, it seems that the caregivers take all the responsibilities or even decide on the patient's behalf, and the suffering person remains in ignorance [32]. This is apparent in the present study, where the percentage of the relatives choosing the disclosure of diagnosis or prognosis to their patients is small (23%, and 23% respectively). However, a large percentage (56%) of the relatives believe that only sometimes the diagnosis should be revealed, while 51% indicated that only sometimes the prognosis should be announced.
Multivariate analysis demonstrated that there was a significant trend (p = 0.001) for children of patients over spouse in disclosure of "prognosis of disease". A similar trend was observed with male relatives over females (p = 0.012). Furthermore, a trend towards a higher educational status also favored this response (however, this was not significant, p = 0.065), and that for patients' with cancer devoid of metastasis there was also a significant trend towards disclose (p = 0.028). This was similarly matched by the response to question 3 "patients long term quality of life", where only in stratification towards patients with cancer (and not metastasis, p = 0.28) was there a significantly greater interest for hierachical importance. In this respect "expectance of survival" (p = 0.008), disclosure "of the prognosis of disease" (p = 0.028) and "the involvement of physicians from various specialties cooperating as necessary" (p = 0.016) all added support to relatives' interest and involvement in the decision making process aimed at cure in non-metastatic patients.
Despite the fact that they confront such a dilemma, they are still fairly certain as to their opinion with other aspects such as their attitudes about informing their patients for the possible treatment choices (71%) and for amputative/disfiguring operations (68.5%). Additionally, 53% of the relatives would choose the patient to be aware of the complications or the side effects of the treatment. Again with these latter two aspects there was a statistically significant trend towards relatives with a higher educational status indicating favorably (p = 0.001 and 0.028 respectively). Still, although in most European countries doctors tend to reveal the truth directly to the patient [27][28][29] without the family's consent, it is still not common practice yet in Greece, possibly as a result of the strong family bonds.
The health care team-patient relationship is a triangle not a dyad, consisting of the health care professionals, the patient and the family. Each part supports the relationship between the other two, and each is affected by what else happens in the triangle [8][33]. Hence, the involvement of health care teams is very important for the care and treatment of the patients. A high percentage (81.5%) of responders indicated "yes", especially the higher educated (p = 0.017), and a high percentage of relatives preferred to cooperate with a social worker (78%, again correlating with the more higher educated (p = 0.024)). The response to the involvement of a psychologist (44%), however, was somewhat contradictory, although only 22% were against it. Cancer affects the family in many ways and it is important for them to have effective co-operation with health care professionals in order to receive care. In the final stage, 67% of family members would prefer to inform patients about the palliative nature of the treatment (p = 0.07 for the higher educated). This is probably due to the fact that the relatives try to preserve the patients' quality of life until their death.
Ongoing open communication between cancer patients and family members is essential, both between each other and with health care professionals. Patients and family members need to feel supported in their expressions. The health care team can help by letting family members know that emotional stress and behavioral changes are not uncommon during illness, that these and other problems can be overcome with patience and support [22]. It is undoubtedly true, that social support can help people to cope with the psychological effects of cancer and help promote physical recovery; when this support is not available or is withheld the patients' situation is aggravated [34]. The aspect that arises from the study is the fact that the vast majority of the caregivers give a special emphasis on communication between patients and the social environment (family, friends), and the support they receive with respect to disclosure of treatment choices, the involvement of health care teams, cooperation with social workers and physicians from various specialties, all of which demonstrated a stronger positive correlation with a higher educational status. Such communication provides support to the family – between health care professionals, patients and relatives – and the means to overcome the dilemma between disclosing information to the patient on prognosis, diagnosis and the treatment choice.
Conclusions
The study argues that more attention needs to be paid to family members of cancer patients, as they are the primary caregivers in order to have more open-communication with their patients, and to be more empathic and realize the welfare of their patients' quality of life. Good family interactions can help cancer patients adjust to diagnosis and treatment. Family relationships appear to be particularly important because the family is involved with the patient during the illness. The dynamics of family interactions can set the stage of social interactions with friends and health care providers. After all, cancer is a family illness and disrupts the relationship between them and the health care team.
Competing interests
None declared
Authors' contributions
All authors participated in the design of the study, conceived of the study, and participated in its design, coordination and statistical analysis. Finally, all authors read and approved the final manuscript.
Pre-publication history
The pre-publication history for this paper can be accessed here:
Contributor Information
Kyriaki Mystakidou, Email: mistakidou@yahoo.com.
Efi Parpa, Email: parpae@hotmail.com.
Eleni Tsilika, Email: eltsilika@yahoo.com.
Ourania Kalaidopoulou, Email: mistakidou@yahoo.com.
Lambros Vlahos, Email: lampvla@aretaieo.uol.gr.
References
- Spitzer WO, Dobson JH, Hall J, et al. Measuring the quality of life of cancer patients. A concise QL-Index for use by physicians. J Chronic Dis, 1981;34:585–597. doi: 10.1016/0021-9681(81)90058-8. [DOI] [PubMed] [Google Scholar]
- Cella D, Tulsky DS. Measuring quality of life today: methodological aspects. Oncology. 1990;4:29–38. [PubMed] [Google Scholar]
- Winer EP. Quality-of-Life research in patients with breast cancer. Cancer. 1994;74:410–415. doi: 10.1002/cncr.2820741328. [DOI] [PubMed] [Google Scholar]
- Krongrad A, Litwin MS, Lai H, Lai S. Dimensions of quality of life in prostate cancer. J Urol. 1998;160:807–810. doi: 10.1097/00005392-199809010-00048. [DOI] [PubMed] [Google Scholar]
- Esper P, Mo F, Chodak , et al. Measuring quality of life in men with prostate cancer using the functional assessment of cancer therapy-prostate instrument. Urology. 1997;50:920–928. doi: 10.1016/S0090-4295(97)00459-7. [DOI] [PubMed] [Google Scholar]
- Aaranson N, Ahmedzai S, Bergman B, et al. The European Organization for research and treatment of cancer QLQ-C30: a Quality-of-Life instrument for use in International clinical trials. J Natl Cancer Inst. 1993;85:365–375. doi: 10.1093/jnci/85.5.365. [DOI] [PubMed] [Google Scholar]
- Grant MM, Rivera ML. Evolution of Quality of Life in Oncology and Oncology Nursing. In: King RC, Hinds SP, editor. In Quality of Life: From Nursing and Patients Perspectives. UK: Jones and Bartlett; 1998. pp. 3–22. [Google Scholar]
- Blanchard GC, Ruckdescel CJ, Albrecht LT. Patient-family communication with physicians. In: Baider L, Cooper LC, De-Nour KA, editor. In Cancer and the Family. UK: John Wiley & Sons; 1996. pp. 369–387. [Google Scholar]
- Weis K, Reiss D. Family reorganization in response to cancer: a developmental perspective. In: Baider L, Cooper LC, De-Nour KA, editor. In Cancer and the Family. UK: John Wiley & Sons; 1996. pp. 3–30. [Google Scholar]
- Gotay CC. Cultural Variation in family adjustment to cancer. In: Baider L, Cooper LC, De-Nour KA, editor. In Cancer and the Family. UK: John Wiley & Sons; 1996. pp. 32–52. [Google Scholar]
- Rothchild E. Family Dynamics in End-of-Life Treatment Decisions. Gen Hosp Psychiatry. 1994;16:251–258. doi: 10.1016/0163-8343(94)90004-3. [DOI] [PubMed] [Google Scholar]
- Germino BB, Mishel MH, Belyea M, Harris L, Ware A, Mohler J. Uncertainty in prostate cancer. Ethnic and family patterns. Cancer Pract. 1998;6:107–113. doi: 10.1046/j.1523-5394.1998.1998006107.x. [DOI] [PubMed] [Google Scholar]
- Juarez G, Ferrell B, Borneman T. Cultural considerations in education for cancer pain management. J Cancer Educ. 1999;14:168–173. doi: 10.1080/08858199909528610. [DOI] [PubMed] [Google Scholar]
- Iconomou G, Viha A, Kalofonos HP, Kardamakis D. Impact of cancer on primary caregivers of patients receiving radiation therapy. Acta Oncol. 2001;40:766–71. doi: 10.1080/02841860152619205. [DOI] [PubMed] [Google Scholar]
- Mystakidou K, Tsilika E, Befon S, et al. Optimizing hospital-based home care for dying cancer patients: a population based study. Palliat Med. 1999;13:385–392. doi: 10.1191/026921699669663451. [DOI] [PubMed] [Google Scholar]
- Aoki Y, Nakagawa K, Hasezawa K, et al. Significance of informed consent and truth-telling for quality of life in terminal cancer patients. Radiat Med. 1997;15:133–135. [PubMed] [Google Scholar]
- Miimi M, Akaza H, Takeshima H, et al. The physical, mental and social impacts of telling prostate cancer patients the true diagnosis. Nippon Hinyokika Gakkai Zasshi. 1997;88:752–761. doi: 10.5980/jpnjurol1989.88.752. [DOI] [PubMed] [Google Scholar]
- Kawakami S, Arai G, Ueda K, et al. Physician's attitudes towards disclosure of cancer diagnosis to elderly patients: a report from Tokyo, Japan. Arch Gerontol Geriatr. 2001;33:29–36. doi: 10.1016/S0167-4943(01)00099-1. [DOI] [PubMed] [Google Scholar]
- Bozcuk H, Erdogan V, Eken C, et al. Does awareness of diagnosis make any difference to quality of life? Determinants of emotional functioning in a group of cancer patients in turkey. Support Care Cancer. 2002;10:51–57. doi: 10.1007/s005200100308. [DOI] [PubMed] [Google Scholar]
- Daikos GK. Informing the cancer patient. Iatriki. 1992;61:263–264. [Google Scholar]
- Tsigourakos D, Velonaki A, Samartzi M, Skourta I. The family as a support mechanism for the cancer patient. Round table discussion. Hellenic Oncology. 1993;29:119–131. [Google Scholar]
- Bloom JR. Social support of the cancer patient and the role of the family. In: Baider L, Cooper LC, De-Nour KA, editor. In Cancer and the Family. UK: John Wiley & Sons; 1996. pp. 54–70. [Google Scholar]
- Lewis FM, Bloom JR. Psychosocial adjustment to breast cancer: a review of selected literature. Int J Psychiatry Med. 1979;9:1978–1. doi: 10.2190/5vkv-hl8n-m9c8-nt7l. [DOI] [PubMed] [Google Scholar]
- Meyerowitz BE. Psychological correlates of breast cancer and its treatments. Psychol Bull. 1980;87:108–131. doi: 10.1037//0033-2909.87.1.108. [DOI] [PubMed] [Google Scholar]
- Penman D, Bloom JR, Fotopolis S, et al. The impact of mastectomy on self-concept and social function: a combined cross-sectional and longitudinal study with comparison groups. Women and Health. 1986;11:101–130. doi: 10.1300/j013v11n03_08. [DOI] [PubMed] [Google Scholar]
- Covinsky KE, Goldman L, Cook EF, et al. The impact of serious illness on patients' families. SUPPORT Investigators. Study to understand prognosis and preferences for outcomes and risks of treatment. JAMA. 1994;272:1839–1844. doi: 10.1001/jama.272.23.1839. [DOI] [PubMed] [Google Scholar]
- Mystakidou K, Liossi C, Vlachos L, Papadimitriou J. Disclosure of diagnostic information to cancer patients in Greece. Palliat Med. 1996;10:195–200. doi: 10.1177/026921639601000303. [DOI] [PubMed] [Google Scholar]
- Buckman R. Talking to patients about cancer. BMJ. 1996;313:699–700. doi: 10.1136/bmj.313.7059.699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simpson M, Buckman R, Stewart M, et al. Doctor-patient communication: the Toronto consensus statement. BMJ. 1991;303:1385–87. doi: 10.1136/bmj.303.6814.1385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meredith C, Symonds P, Webster L, et al. Information needs of cancer patients in west Scotland: cross-sectional survey of patients' views. BMJ. 1996;313:724–726. doi: 10.1136/bmj.313.7059.724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Annunziata MA, Foladore S, Magri MD, et al. Does the information level of cancer patients correlate with quality of life? A prospective study. Tumori. 1998;84:619–623. doi: 10.1177/030089169808400601. [DOI] [PubMed] [Google Scholar]
- Gidopoulou E, Psimouli A. The unspoken truth. In: Kordiolis N, Rigatos G, editor. In The truth and the patient with neoplasm, Hellenic Anticancer Association, Athens; 1990. [Google Scholar]
- Humphrey GB, Littlewood JL, Kamps WA. Physician/patient communication: a model considering the interaction of physicians' therapeutic strategy and patients' coping style. J Cancer Educ. 1992;7:147–152. doi: 10.1080/08858199209528157. [DOI] [PubMed] [Google Scholar]
- Bloom JR, Kang SH, Romano P. Cancer and stress: The effects of social support as a resource. In: Cooper C, Watson M, editor. In Cancer and Stress: Psychological, Biological and Coping Studies. New York: John Wiley; 1990. pp. 95–124. [Google Scholar]