Abstract
Background:
In countries which lack robust health care systems, congenital conditions such as cleft lip and/or palate deformities are often untreated in certain individuals. Many volunteer organizations have stepped in to fill this gap but certain factors, such as continuity of care, are yet to be studied for these clinics.
Methods:
This is a retrospective cohort study of 167 pediatric patients with cleft lip and/or palate residing in El Salvador treated by a nongovernmental organizations between 2011 and 2020. This data was used in univariate and multivariable models to associate particular patient factors to their likelihood of following up to their annual clinic visits.
Results:
Each 1-year increase in duration of follow-up was associated with a 27% decrease in the odds of attending a visit. In addition, 33.7% of cleft lip and 49.7% of cleft palate/cleft lip and palate patients returned at least once. Males had 36% higher odds of attending a return visit compared with females but this difference was not statistically significant. Time spent travelling to the clinic had no effect on follow-up rates.
Conclusion:
Nongovernmental organizations utilizing a diagonal care model should consider using more strategies to maximize continuity of care by increasing communication with patients and emphasizing the need of following up during clinic visits. Continued and increased collaboration with the local team is also of great importance.
Keywords: Cleft lip and palate, follow-up, international, volunteer
Access to health care can be a true challenge for many patients in low-and-middle-income countries (LMICs) within Latin America. Lack of government-aided financial resource programs and geopolitical conflicts also elevates challenges for providing patient care to the entire community. Some LMICs have programs for national health care coverage; however, the demand for care often overwhelms the health care workforce.1 This ultimately results in patients being deprived of essential care. Some efforts to offset this demand include the establishment of nongovernmental organizations (NGOs) and global health medical trips within Latin American countries.2
The incidence for cleft lip and/or palate (CL/P) deformities in South America is ~1 in 1000.3 In countries with more robust health care systems, almost all children born with a CL/P can receive prompt treatment for this congenital defect. This is not true in countries with more limited resources, and thus patients are often willing to travel far distances to be seen and treated by medical professionals for this defect.1,4 In addition, cleft anomalies are multifaceted disorders that significantly affect multiple basic essential functions including swallowing, hearing, and speech.5,6 Because of this, treatment involves multiple subspecialists and can include various surgeries during the first 18 years of life.5,6 Thus, those delivering comprehensive care for patients with CL/P deformities in countries like El Salvador face many challenges.7,8
This study focuses on a non-profit NGO volunteer medical care organization that provides comprehensive cleft care in several countries with limited medical resources. The NGO, Global Smile Foundation, employs teams of numerous medical specialists from various countries and partners with the local medical hospitals to treat certain more complicated cleft anomalies.9 These teams travel annually to the same location at the same time each year to provide care for new patients with CL/P diagnoses and returning patients, who need follow-up surgeries or routine checkups for their speech and dental needs.10 This NGO partners with a local craniofacial team in San Salvador to treat the more complex cases seen by the local providers. Global Smile Foundation (GSF) focuses on a diagonal care delivery model where short-term treatment teams empower and invest in local infrastructure and care teams.11 It has been estimated that approximately half of the current international surgical organizations use this care model.12
Patient follow-up is essential to the efficacy of any clinic managing this patient population.13–16 Children with CL/P receive their corrective surgeries in the first 2 years of life but require additional medical follow-up until adulthood (eg, for speech, aesthetic, psychosocial, dental, and bone grafting needs).4 Each patient, who has received the surgery, is told to follow up annually to address any issues that arise because of the original cleft diagnosis. The goal of this study is to assess visit patterns in this patient population from their initial surgery to adulthood and to identify potential factors that may impact the likelihood that patients adhere to the annual return visits, especially in the unique setting of a global team care provider.
This study investigates what factors are associated with the return rates of patients, who are asked to return annually, for continued care of their diagnosis of cleft lip and palate. Specifically, this study evaluated whether a patient’s age, sex, specific cleft diagnosis, travel time to the clinic, and duration of follow-up is related to their likelihood of returning to the clinic with each successive year. This NGO is one of many global volunteer organizations that treat CL/P patients, and the knowledge gained from this investigation will hopefully provide insight for centers operating in countries with similar challenges.
METHODS
This is a retrospective cohort study of pediatric patients with CL/P residing in El Salvador treated between 2011 and 2020. After obtaining IRB approval, researchers reviewed patient charts stored in a secure drive owned by GSF. Data was collected on 226 patients seen between 2011 and 2020; information analyzed included: date of initial surgery and visit, dates of subsequent follow up visits, date of birth, cleft diagnosis (cleft lip, cleft palate, cleft lip and palate, other), history of prior surgical intervention independent of GSF, and travel time to the clinic. Twenty-six children were seen for only an initial screening visit and 33 patients had conditions other than CL/P; these 2 groups were excluded from the analysis as they were not operated on and/or would not be asked to return annually to the clinic. Thus, the final study cohort included 167 participants to measure patient’s attendance for annual return visits.
Descriptive statistics were calculated for all patient-level characteristics. Univariate associations between visit attendance and patient characteristics were evaluated using a series of generalized linear mixed models. All models include a fixed effect for the patient characteristics and a random subject effect to account for repeated measures on the same patient over time. We also developed a multivariable model of attendance considering all patient factors with univariate P values <0.2 and interactions between each patient factor with duration of follow-up.17,18 The final model was selected using backward selection retaining all variables significant at P < 0.05. For all models, assumptions were checked graphically, and transformations were considered as needed. All analyses were conducted in SAS v. 9.4 (SAS Institute, Cary, NC).
RESULTS
The study population included 167 subjects. Approximately 70.1% of subjects had both cleft lip and palate, 7.8% had only cleft palate, and 22.2% had only cleft lip. The mean age of participants at the end of the study was 5.7 ± 3.7 years with a follow-up period (total possible follow-up period based on patient age at presentation and study window) of 4.2 ± 1.7 years, and 46.7% of children attended at least one follow-up visit. Patient characteristics are described in Supplemental Table 1 (Supplemental Digital Content 1, http://links.lww.com/SCS/E180).
In univariate models only duration of follow-up was associated with attendance. Specifically, a 1-year increase in duration of follow-up was associated with a 27% decrease in the odds of attending a visit. Patients with CP or CLP had 1.6 times the odds of attending follow-up visits compared to patients with CL, though the association was not significant. There was no association between odds of attending follow-up visits with patient sex, the duration of time it took for patients to travel to the clinic, and whether they had surgery performed by a GSF team.
When examining associations between odds of attending follow-up visits with patient factors over time, there was a significant interaction between duration of follow-up and condition (CP versus CP or CLP). The multivariable model included duration of follow-up, condition, and the interaction between duration of follow-up and condition. Given the interaction between duration of follow-up and condition, these variables should be interpreted together. These results suggest that children with CL are equally likely to attend both early and later follow-up visits, while children with CP/CLP had greater odds of attending earlier visits compared to later visits. Specifically, children with CP/CLP had a 35% decrease in the odds of attending annual follow-up visit with each 1-year increase in duration of follow-up compared with a nonsignificant decrease in children with CL. The univariate and multivariable models of attendance at annual follow-up visits is presented in Supplemental Table 2 (Supplemental Digital Content 2, http://links.lww.com/SCS/E181). Figure 1 shows the probability of patient attendance with each consecutive year.
FIGURE 1.
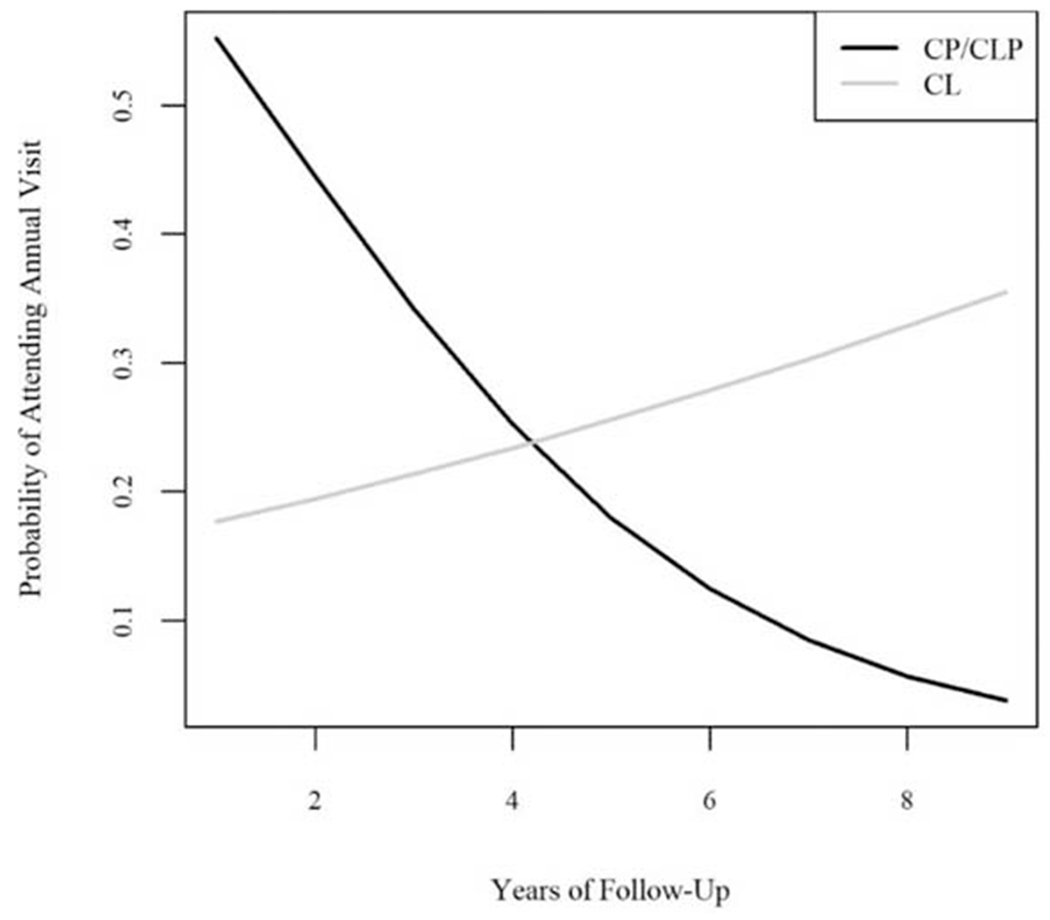
Estimated probability of visit attendance with increasing year of follow-up by condition. CL indicates cleft lip; CL/P cleft lip and/or palate; CP, cleft palate.
DISCUSSION
Patient Characteristics
Interestingly, most patients (85%) had their initial cleft palate or cleft lip surgery performed by GSF. The patient population also had slightly more males (71%). Moreover, 46.7% of the patients followed up with the clinic at least once after their surgery. While this statistic seems low, it should be noted that the patient population is composed of individuals, who already lack access to the existing health care system, for various reasons. In addition, many of these individuals are also seen by the native craniofacial team throughout the year to have more general needs addressed and met.
However, these considerations should not deemphasize the need for studies, such as this one, which seek to improve this metric, for the sake of these patients’ health. While other studies analyzing international NGOs have had some elements of follow-up in their study, none to the knowledge of the authors have measured their follow-up rates and influencing factors.19 Understandably, the team’s presence for a ten-day span annually likely impacts the attendance rate. To overcome this obstacle, the El Salvadorian cleft team, trained by GSF members, follow up on these patients throughout the year and GSF members also see these patients during regular telehealth appointments. These visits were not included as part of this analysis, which is a limitation of this study. The fact that the return rate reached 46.7% for this organization shows that NGOs adopting a care model similar to diagonal care models, if determined, can establish continuity of care.
Follow-Up Rates for CL Versus CP/CLP
These results demonstrate interesting trends in both patients with CL and patients with CL/P. The patients with CL/P would be expected return for annual clinic evaluations because of their greater needs due to palatal involvement. This population can require additional surgeries and/or needs such as speech therapy, speech surgery, and alveolar bone grafting.20–22 However, in this analysis the follow-up rates for patients with CL/P decreased with each consecutive year when compared to the patients with CL (Fig. 1). One possible explanation for this finding is healthcare fatigue. Health care fatigue is a concept that explains how caregivers of patients with more complicated disorders can seek less medical care over time due the social, economic, and medical burden of caring for such individuals. Prior research shows that for those with medical disorders, more debilitating diseases levy higher emotional and psychological tolls on patients.23–25 Since deformities of cleft palate and cleft lip/palate are functionally more impacting than a cleft lip, this may partially explain these findings.
Another possible exacerbating factor for less frequent follow-up is education barriers. Unfortunately, education level of the caregivers was not assessed in this study, but it would be interesting to evaluate in future studies. Helping a caregiver understand the complexity and seriousness of cleft deformities is a challenging task. The more complex a child’s disorder, the higher the risk that a caregiver will be confused about the disorder. From this perspective, it might be easier to understand why some caretakers may not see the utility or the importance of a follow-up appointment. In addition, the adult literacy rate in El Salvador in 2018 was ~90%.26 Thus, educational tools such as hand-outs might not be effective. GSF routinely gives illustrated hand-outs to caregivers; one provides general information about the CL/P disorder and associated surgeries, while the other provides information about follow-up, feeding, and other oral health maintenance. In a survey done in the United Kingdom, caregivers of children with CL/P mentioned desiring more information about their child’s operation, as well as the possible complications and follow-up care, than what they received in their clinic visits.27
Relationship Between Patient Sex and Follow-Up Rates
Our analysis found no difference between sex and patient follow-up rate. This is a surprising statistic considering that other studies have shown females to have a higher rate of cleft surgery complications and a higher propensity for their clefts to be revised, even when controlling for their existing higher complication rate.28 Few studies have focused on the ways in which gender influences healthcare in El Salvador. Reassuringly, the United Nations did find that the country had a more robust reproductive health system than other countries within its same “Human Development Group.” For example, 96% of all births in El Salvador are attended by a skilled health professional compared with their group’s average of 78%. In any case, the fact that the genders did not exhibit statistically different follow-up in this study is an encouraging finding.
Relationship Between Travel Time and Follow-Up Rates
According to our data, distance had no effect on how often children returned to the clinic. At first glance, this result can seem surprising. Fifteen percent of these patients travelled more than 5 and a half hours for their return visit while many patients lived in the city where the clinic was held. Data on how patients traveled to appointments was not collected, but informal conversation with families suggests that both personal cars possessed by a family member or public transportation were used. Regardless, this study showed that distance had no effect on a patient’s likelihood of returning to the clinic.
One study done in Guinea, Madagascar and the Republic of Congo showed that removing the cost of transportation significantly increased patient access to surgical care.29 However, the transportation in El Salvador is quite good when compared with other LMICs. The transportation infrastructure in El Salvador is among the best in South America with the second highest paved and unpaved road density in relation to land area in the continent.30 In one survey of various international companies, the country ranked third in South America for overall road quality.30 Further, El Salvador is also one of the smallest countries in Latin America, and the surgeries in this study were performed in the city, San Salvador, which is located centrally. Consequently, the patients in our study might not be as affected by travel times as patients in other studies simply because travel from anywhere in the country is not quite as difficult.
Moreover, these findings are in line with what studies in other locations with robust transportation have found. In the United Kingdom, one survey of 200 caregivers of children with cleft deformities showed that patients travelled an average distance of 44 miles for their initial surgery and 23 miles for their routine checkups.31 Interestingly, when asked about barriers to their care, the parents largely did not mention distance to be a factor. An even more extreme example is from one study done in North Carolina in which the patients had an average travel distance of 80.2 miles. Over two-thirds of this patient group did not find distance to the clinic to be a problem, with 98% of patients reporting to be either “satisfied” or “very satisfied” with their care.32 Thus, it is certainly possible that in many countries, if transportation quality is above a certain threshold, caregivers simply do not mind travelling long distances to seek treatment of their child’s cleft diagnosis.
Follow-Up Rates and Partnership With the Local Community
In addition, continued emphasis in partnership with and investment in the local community is essential for the follow-up of this patient population. The local craniofacial team in San Salvador sees patients with clefts for follow-up appointments and surgeries throughout the year while GSF sees a small percentage of these patients, who have more complex aspects of their disease. This NGO also trains local providers in the management of some of these more complicated conditions. For example, one of the local surgeons has been trained in Nasoalveolar Molding technique in diagnosis, management, and treatment for children with CL/P through a fellowship program, the GSF Cleft Surgery Training program. As the resident craniofacial team is better trained to manage more complicated patient courses, specific patients can be advised to return to the clinic more frequently for their individual needs and programs like GSF would be needed less often for the care of these individuals.
Follow-Up Rates and Protocol Development
Various protocols have been implemented to solve problems that have arisen for NGOs attempting to deliver complex cleft care internationally. GSF’s emergency response protocol is one example.33 This same NGO utilizes a modified World Health Organization surgery safety checklist.10 GSF and Smile Train have developed quality assurance and anesthetic guidelines to prioritize and ensure patient safety in international surgical endeavors.34–36 In a similar way, protocols can be developed that outline best practices for maximizing follow-up. This protocol could outline the way future appointments are discussed during initial visits, recommend ways for the local providers to maintain continuity with patients throughout the year, and detail what information is given to patients.
CONCLUSION
NGOs face many challenges when attempting to fill the surgical gap in LMICs. Continuity of care poses a significant challenge for many of these organizations. This study has identified cleft diagnosis and time from surgical repair as factors that significantly influence the follow-up of patients in this volunteer surgical clinic in El Salvador. More research needs to be done to understand why the groups with differing cleft diagnoses exhibited distinctly unique follow-up patterns in this setting. Regardless of the underlying reason(s), volunteer surgical clinics in El Salvador that attempt models involving continuity of care should be wary of these influencing factors. Equally noteworthy, this analysis did not find that travel time had any significant impact in this setting. Our findings suggest that in smaller countries with adequate and inexpensive transportation, distance to the clinic may not be as influential of a factor when it comes to patient follow-up. Lastly, 46.7% compliance with follow-up can serve as a point of comparison for this and other NGOs, especially those utilizing a diagonal care model, to use and build upon.
The results of this study reveal the need to further communicate the importance of patients to return to the annually held clinics. In addition, emphasis should be placed on recapturing the patients with CL/P to return for continuing their comprehensive cleft care including speech, dental and orthodontic needs, and psychosocial support with the on-site teams. Most importantly, this study can start the conversation about how this center and others can improve their return rate to be closer to 100%.
Supplementary Material
Footnotes
The authors report no conflicts of interest.
Supplemental Digital Content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website, www.jcraniofacialsurgery.com.
REFERENCES
- 1.Molina G, Funk LM, Rodriguez V, et al. Evaluation of surgical care in El Salvador using the WHO surgical vital statistics. World J Surg 2013;37:1227–1235 [DOI] [PubMed] [Google Scholar]
- 2.Sykes KJ. Short-term medical service trips: a systematic review of the evidence. Am J Public Health 2014;104:e38–e48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Panamonta V, Pradubwong S, Panamonta M, et al. Global birth prevalence of orofacial clefts: a systematic review. J Med Assoc Thai 2015;98(suppl 7):S11–S21 [PubMed] [Google Scholar]
- 4.Farronato G, Kairyte L, Giannini L, et al. How various surgical protocols of the unilateral cleft lip and palate influence the facial growth and possible orthodontic problems? Which is the best timing of lip, palate and alveolus repair? Literature review. Stomatologija 2014;16:53–60 [PubMed] [Google Scholar]
- 5.Chuo CB, Searle Y, Jeremy A, et al. The continuing multidisciplinary needs of adult patients with cleft lip and/or palate. Cleft Palate Craniofac J 2008;45:633–638 [DOI] [PubMed] [Google Scholar]
- 6.Robin NH, Baty H, Franklin J, et al. The multidisciplinary evaluation and management of cleft lip and palate. South Med J 2006;99:1111–1120 [DOI] [PubMed] [Google Scholar]
- 7.Kantar RS, Cammarata MJ, Rifkin WJ, et al. Foundation-based cleft care in developing countries. Plast Reconstr Surg 2019;143:1165–1178 [DOI] [PubMed] [Google Scholar]
- 8.Massenburg BB, Jenny HE, Saluja S, et al. Barriers to cleft lip and palate repair around the world. J Craniofac Surg 2016;27:1741–1745 [DOI] [PubMed] [Google Scholar]
- 9.Chahine EM, Kantar RS, Kassam SN, et al. Sustainable cleft care: a comprehensive model based on the global smile foundation experience. Cleft Palate Craniofac J 2021;58:647–652 [DOI] [PubMed] [Google Scholar]
- 10.Patel KG, Eberlin KR, Vyas RM, et al. Use of safety measures, including the modified world health organization surgical safety checklist, during international outreach cleft missions. Cleft Palate Craniofac J 2014;51:597–604 [DOI] [PubMed] [Google Scholar]
- 11.Patel PB, Hoyler M, Maine R, et al. An opportunity for diagonal development in global surgery: cleft lip and palate care in resource-limited settings. Plast Surg Int 2012;2012:892437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Patel PS, Chung KY, Kasrai L. Innovate global plastic and reconstructive surgery: cleft lip and palate charity database. J Craniofac Surg 2018;29:937–942 [DOI] [PubMed] [Google Scholar]
- 13.Kerfeld CI, Hoffman JM, Ciol MA, et al. Delayed or forgone care and dissatisfaction with care for children with special health care needs: the role of perceived cultural competency of health care providers. Matern Child Health J 2011;15:487–496 [DOI] [PubMed] [Google Scholar]
- 14.Seid M, Sobo EJ, Gelhard LR, et al. Parents’ reports of barriers to care for children with special health care needs: development and validation of the barriers to care questionnaire. Ambul Pediatr 2004;4:323–331 [DOI] [PubMed] [Google Scholar]
- 15.Yu SM, Nyman RM, Kogan MD, et al. Parent’s language of interview and access to care for children with special health care needs. Ambul Pediatr 2004;4:181–187 [DOI] [PubMed] [Google Scholar]
- 16.Yu SM, Singh GK. Household language use and health care access, unmet need, and family impact among CSHCN. Pediatrics 2009;124(suppl 4):S414–S419 [DOI] [PubMed] [Google Scholar]
- 17.Bendel RB, Afifi AA. Comparison of stopping rules in forward “stepwise” regression. J Am Stat Assoc 1977;72:46–53 [Google Scholar]
- 18.Mickey RM, Greenland S. The impact of confounder selection criteria on effect estimation. Am J Epidemiol 1989;129:125–137 [DOI] [PubMed] [Google Scholar]
- 19.de Buys Roessingh AS, Dolci M, Zbinden-Trichet C, et al. Success and failure for children born with facial clefts in Africa: a 15-year follow-up. World J Surg 2012;36:1963–1969 [DOI] [PubMed] [Google Scholar]
- 20.Fisher DM, Sommerlad BC. Cleft lip, cleft palate, and velopharyngeal insufficiency. Plast Reconstr Surg 2011;128:342e–360e [DOI] [PubMed] [Google Scholar]
- 21.Stoll C, Alembik Y, Dott B, et al. Associated malformations in cases with oral clefts. Cleft Palate Craniofac J 2000;37:41–47 [DOI] [PubMed] [Google Scholar]
- 22.Tolarova MM, Cervenka J. Classification and birth prevalence of orofacial clefts. Am J Med Genet 1998;75:126–137 [PubMed] [Google Scholar]
- 23.Heller A, Rafman S, Zvagulis I, et al. Birth defects and psychosocial adjustment. Am J Dis Child 1985;139:257–263 [DOI] [PubMed] [Google Scholar]
- 24.Kapp-Simon KA. Psychological interventions for the adolescent with cleft lip and palate. Cleft Palate Craniofac J 1995;32:104–108 [DOI] [PubMed] [Google Scholar]
- 25.Kapp-Simon KA, Simon DJ, Kristovich S. Self-perception, social skills, adjustment, and inhibition in young adolescents with craniofacial anomalies. Cleft Palate Craniofac J 1992;29:352–356 [DOI] [PubMed] [Google Scholar]
- 26.UNESECO (United Nations Educational Scientific and Cultural Organization). El Salvador Education And Literacy. Available at: http://uis.unesco.org/ Accessed January 23, 2021
- 27.Stock NM, Feragen KB, Rumsey N. Adults’ narratives of growing up with a cleft lip and/or palate: factors associated with psychological adjustment. Cleft Palate Craniofac J 2016;53:222–239 [DOI] [PubMed] [Google Scholar]
- 28.Paganini A, Horfelt C, Mark H. Gender differences in surgical treatment of patients with cleft lip and palate. J Plast Surg Hand Surg 2018;52:106–110 [DOI] [PubMed] [Google Scholar]
- 29.Shrime MG, Hamer M, Mukhopadhyay S, et al. Effect of removing the barrier of transportation costs on surgical utilisation in Guinea, Madagascar and the Republic of Congo. BMJ Glob Health 2017;2(suppl 4):e000434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.ECLAC (Economic Commission for Latin America and the Caribbean). Empalmes de series: aspectos metodológicos y prácticas internacionales. (Evolution of investment in Latin America and the Caribbean: stylized facts, determinants and policy challenges) 2018 [Google Scholar]
- 31.CLAPA (Cleft Lip and Palate Association). Regionalisation of cleft lip and palate services: has it worked? 2007. Available at: https://www.clapa.com/wp-content/uploads/2015/11/Full-report-final.pdf. Accessed May 15, 2020
- 32.Cassell CH, Krohmer A, Mendez DD, et al. Factors associated with distance and time traveled to cleft and craniofacial care. Birth Defects Res A Clin Mol Teratol 2013;97:685–695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Vyas RM, Eberlin KR, Hamdan US. Implementation of an emergency response protocol for overseas surgical outreach initiatives. Plast Reconstr Surg 2013;131:631e–636e [DOI] [PubMed] [Google Scholar]
- 34.Chahine EM, Ramly EP, Marston AP, et al. Quality assurance standards for outreach cleft lip and cleft palate repair programs in low-resource settings. Cleft Palate Craniofac J 2022:10556656221074883. doi: 10.1177/10556656221074883 [DOI] [PubMed] [Google Scholar]
- 35.Kulkarni KR, Patil MR, Shirke AM, et al. Perioperative respiratory complications in cleft lip and palate repairs: an audit of 1000 cases under “Smile Train Project”. Indian J Anaesth 2013;57:562–568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Melhem AM, Ramly EP, Al Abyad OS, et al. Enhanced recovery after cleft lip repair: protocol development and implementation in outreach settings. Cleft Palate Craniofac J 2022:10556656221078744. doi: 10.1177/10556656221078744 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


