Abstract
Objective:
Lesbian, gay, bisexual, and queer (LGBQ)-affirmative cognitive behavioral therapy (CBT) focused on minority stress processes can address gay and bisexual men’s transdiagnostic mental and behavioral health concerns. Identifying moderators of treatment outcomes may inform the mechanisms of LGBQ-affirmative CBT and subpopulations who may derive particular benefit.
Methods:
Data were from a clinical trial in which gay and bisexual men with mental and behavioral health concerns were randomized to receive ESTEEM (an LGBQ-affirmative transdiagnostic CBT; n=100) or one of two control conditions (n=154): LGBQ-affirmative community mental health treatment or HIV counseling and testing. The pre-registered outcome was a comorbidity index of depression, anxiety, alcohol/drug problems, and HIV-risk-behavior at 8-month follow-up (i.e., 4-months post-intervention). A two-step exploratory machine learning process was employed for 20 theoretically-informed baseline variables identified by study therapists as potential moderators of ESTEEM efficacy. Potential moderators included demographic factors, pre-treatment comorbidities, clinical facilitators, and minority stress factors.
Results:
Racial/ethnic minority identification, namely as Black or Latino, was the only statistically significant moderator of treatment efficacy (B=−3.23 [95% CI: −5.03, −1.64], t[197]=−3.88, p<.001). Racially/ethnically minoritized recipients (d=−0.71, p<.001), but not White/non-Latino recipients (d=0.22, p=0.391), had greater reductions in comorbidity index scores in ESTEEM compared to the control conditions. This moderation was driven by improvements in anxiety and alcohol/drug use problems.
Discussion:
Black and Latino gay and bisexual men experiencing comorbid mental and behavioral health risks might particularly benefit from a minority-stress-focused LGBQ-affirmative CBT. Future research should identify mechanisms for this moderation to inform targeted treatment delivery and dissemination.
Accumulating empirical evidence suggests that lesbian, gay, bisexual, and queer (LGBQ) affirmative cognitive behavioral therapy (CBT) might be a promising treatment approach for gay and bisexual men’s co-occurring mental and behavioral health concerns (Pachankis et al., 2022). In general, LGBQ-affirmative therapies aim to assess and address sexual minority individuals’ distinct experiences with minority stressors and the ways in which those minority stressors can impact psychological functioning (American Psychological Association Task Force on Psychological Practice with Sexual Minority Persons, 2021; Meyer, 2003). Minority stressors refer to the distinct stigma-related challenges faced by minoritized populations, from laws and policies to bullying and family rejection, and the characteristic and stressful psychological adaptations sometimes required to navigate such challenges (Meyer, 2003).
Effective Skills to Empower Effective Men (ESTEEM) is an LGBQ-affirmative transdiagnostic CBT that addresses the minority stress pathways theorized (Hatzenbuehler, 2009) to underlie gay and bisexual men’s disproportionate risk of mental (e.g., depression, anxiety) and behavioral (e.g., HIV-transmission-risk behavior, substance use problems) health concerns (Burton et al., 2019; Pachankis, 2014; Pachankis, 2018; Pachankis et al., 2022b). ESTEEM adapts CBT techniques to address the cognitive, affective, and behavioral stress pathways shown to emerge from minority stress, such as internalized stigma, sexual orientation-based rejection schemas, and social isolation, and to be related to gay and bisexual men’s mental and behavioral health (Hatzenbuehler, 2009). As such, ESTEEM and its adaptations (e.g., Empowering Queer Identities in Psychotherapy for gender-diverse sexual minority women; Pachankis et al., 2020a) represent among the only LGBTQ minority-stress-focused psychotherapies to have been tested in randomized controlled trials and the only known such treatment to have been compared to other active treatments.
Two studies provide evidence for ESTEEM’s potential efficacy in reducing gay and bisexual men’s psychosocial health concerns. In an initial randomized trial, young gay and bisexual men receiving up to 10 sessions of ESTEEM reported significantly greater reductions in depression, alcohol use, sexual compulsivity, and past-90-day condomless sex, and small but significant reductions in some minority stress factors (e.g., internalized homonegativity), compared to a wait-list control (Pachankis et al., 2015). A more recent multi-site trial comparing ESTEEM to an LGBQ-affirmative community mental health treatment and single-session HIV testing and counseling found that ESTEEM was not significantly superior to the control conditions in reducing the primary preregistered outcome of presence of any HIV-transmission-risk behaviors at 8-month follow-up (Pachankis et al., 2022a). Still, there was significantly greater reduction in comorbidity across mental and behavioral health concerns in ESTEEM relative to LGBQ-affirmative community mental health treatment—tracking generally larger, although typically nonsignificant effect sizes in favor of ESTEEM across outcome measures. Further, ESTEEM was superior to HIV testing in improving drug and alcohol use problems after correction for the false discovery rate.
While this empirical evidence increasingly supports the efficacy of ESTEEM (e.g., Pachankis et al., 2015; 2022b), less is known known about factors that might moderate treatment efficacy for this or any minoritized population (Hatzenbuehler & Pachankis, 2021; Millar et al., 2016). This question is particularly important because the impact of within-group heterogeneity on the efficacy of the ESTEEM intervention may mask the potentially stronger effects for ESTEEM among particular subgroups of gay and bisexual men, relative to control interventions. Additionally, establishing empirical guidance for treatment selection among this population can lead to more efficient distribution of therapeutic resources (Lorenzo-Luaces et al., 2017), and may also help some gay and bisexual men achieve unique clinical benefits that they would be less likely to attain in some therapies versus others (Cohen & DeRubeis, 2018).
ESTEEM may be particularly appropriate for some subgroups of young gay and bisexual men for several reasons, related to both its foundations as a transdiagnostic CBT and its focus on ameliorating minority stress. A first set of potential moderators includes differences in individuals’ demographic background and personal history, such as socioeconomic status, trauma history, and racial/ethnic identification, which may reflect important contextual factors and individual differences influencing match to ESTEEM. Among unemployed individuals, CBT has been found to be more effective for treating depression than paroxetine (Fournier et al., 2009) or very brief therapy/treatment as usual (Lorenzo-Luaces et al., 2017), which may be because CBT better helps individuals hone their personal capacities and self-efficacy that may help them achieve employment (Fournier et al., 2015). Moreover, although trauma-focused CBTs are effective for post-traumatic stress disorder, childhood trauma history negatively impacts treatment retention in CBTs relative to psychodynamic therapies for depression and panic disorder (Gibbons et al., 2019; Keefe et al., 2021).
In addition, gay and bisexual men who possess other minoritized identities might be particularly likely to benefit from a minority-stress-focused treatment such as ESTEEM. Racial/ethnic socialization may prepare gay and bisexual men of color to adopt a minority stress conceptualization for understanding their mental and behavioral health (Anderson & Stevenson, 2019), making a minority stress-focused treatment more resonant and thus relatively more effective for them as compared to non-Latino White gay and bisexual men. Broadly speaking, meta-analytic examinations have typically found that culturally adapted psychotherapies for racial/ethnic minority individuals (e.g., including interventions addressing culturally relevant factors and incorporating culturally consonant beliefs about the nature and amelioration of mental illness) yield greater clinical benefits than non-adapted therapies (Benish et al., 2011; Hall et al., 2016). Further, treatment recipient perceptions of greater therapist cultural competence are associated with superior outcomes among racial/ethnic minority individuals (Soto et al., 2018). Yet, whether racial/ethnic minority individuals might benefit more than non-Latino White individuals from a treatment adapted to address the experiences of another minoritized population (e.g., sexual minority individuals) remains unknown.
A second set of potential moderators includes individuals’ comorbidities at baseline. Individuals dealing with multiple comorbid mental and behavioral health problems may respond better to ESTEEM across their presenting problems, given that ESTEEM was adapted from the Unified Protocol, which was developed to address transdiagnostic processes underlying comorbid mental health conditions (Wilamowska et al., 2010). A randomized trial (n = 93) comparing a transdiagnostic behavior therapy to behavioral activation among individuals experiencing depression, anxiety, or both found that individuals with more comorbid mental health problems experienced greater symptom and functioning improvements upon receiving the transdiagnostic therapy (Coyne & Gros, 2022). In addition, depressed individuals with more symptomatically comorbid presentations have better depression outcomes upon receiving CBT as compared to low-intensity interventions or treatment as usual (Lorenzo-Luaces et al., 2017). Suicidality and substance use problems have also both been found to be effectively treated by the Unified Protocol (Cassiello-Robbins et al., 2020), possibly via specifically facilitating improvements in underlying trait neuroticism that contributes to these problems (Sauer-Zavala et al., 2020). Collectively, this prior research suggests that ESTEEM, as a CBT-based treatment targeting minority stress processes and reactions that influence multiple mental and beahvioral health outcomes (Hatzenbuehler, 2009; Meyer, 2003), may be more efficacious among individuals experiencing more (vs. less) comorbidity. Yet, whether ESTEEM could thus be uniquely helpful for gay and bisexual men dealing with multiple behavioral and mental health problems remains unknown.
A third set of potential moderators includes clinical facilitators like social support (Dahlem et al., 1991) or emotion regulation skills (Gratz & Roemer, 2004), both of which represent strengths that an individual may bring into treatment as well as potential areas of growth addressable by an intervention. On the one hand, individuals with relative deficits in domains targeted by ESTEEM, such as social isolation or difficulties with emotion regulation, may have a preferential response to the intervention. On the other hand, CBTs for depression sometimes yield stronger effects when building on an individual’s strengths rather than focusing on areas of deficit (Cheavens et al., 2012; Lemmens et al., 2020; Murphy et al., 2021). Therefore, deficits in these treatment facilitators might be associated with less benefit upon receiving ESTEEM.
A fourth and final set of potential moderators involves minority stress. Specifically, it is possible that ESTEEM is especially efficacious among those particularly affected by challenges related to minority stress. Because ESTEEM entails a structured focus on cognitive, affective, and behavioral minority stress reactions as targets of treatment—with specific modules intended to provide skills to address them—individuals experiencing high (vs. low) degrees of minority stress at baseline may be more likely to benefit from ESTEEM. That is, ESTEEM’s minority stress focus may lead to relatively larger changes among individuals substantively burdened by minority stress, while individuals not endorsing such challenges may experience fewer unique benefits compared to other interventions (for a review of studies examining the relationship between stigma and intervention efficacy, see Hatzenbuehler & Pachankis, 2021). Indeed, evidence from the waitlist control trial of ESTEEM (Miller et al., 2016), as well as a trial of a brief online self-affirmation intervention for sexual minority young adults (Pachankis et al., 2020a), suggests that minority stress experiences moderate the efficacy of these minority-stress-focused interventions, such that those with higher (vs. lower) levels of minority stress exposure will benefit more from ESTEEM. However, it is currently unknown whether minority stress directed toward two or more stigmatized identities held by an individual, such as sexual minority and racial/ethnic minority identities, might moderate treatment efficacy such that gay and bisexual men of color might be particularly likely to benefit from a minority-stress-focused treatment like ESTEEM.
Another reason minority stress factors may moderate treatment outcomes is that ESTEEM’s minority-stress focus may be more congruent with some patients’ beliefs and theories about the causes of their mental and behavioral problems, including attributing that distress to minority stress exposure. These beliefs may also serve as a relevant individual difference for treatment matching. Indeed, common factors psychotherapy and cultural psychological perspectives emphasize that a successful therapy will provide a psychologically and culturally coherent explanation for mental and behavioral health problems and an actionable therapeutic procedure that clearly follows from that explanation (Huey et al., 2014; Laska et al., 2014). Supporting this perspective, one meta-analysis of culturally adapted psychotherapies found specifically that adaptation of a therapy’s explanation of how mental/behavioral problems emerge and are sustained to a target population may statistically mediate the clinical advantage of such approaches over un-adapted treatments (Benish et al., 2011). Consistent with this literature, ESTEEM may resonate particularly with individuals who attribute their mental and behavioral problems to minority stress exposure, which might be particularly likely among individuals who are socialized to make such attributions perhaps as a function of chronic minority stress exposure directed toward one or more aspects of identity.
The current study examined potential moderators of the efficacy of the ESTEEM intervention. As reviewed in the Method section, these moderators were nominated by therapists who delivered ESTEEM as part of a three-arm randomized controlled trial testing the efficacy of ESTEEM. These moderators reflect the four classes reviewed above: sociodemographic and historical variables, clinical comorbidities, clinical facilitators, and minority stress. In the trial, ESTEEM was compared to two existing interventions–LGBQ-affirmative community mental health treatment and single-session HIV counseling and testing–among gay and bisexual men with diagnoses of depression, anxiety, and/or a trauma-related disorder and past-90-day HIV-transmission-risk behavior. The primary contrast of interest in this study of treatment effect heterogeneity was ESTEEM compared to the two comparison treatments to ascertain any specific benefits of ESTEEM relative to two commonly available LGBQ-affirmative interventions as a function of potential moderators of treatment efficacy.
Method
Sample
The parent clinical trial (n = 254) for this moderator investigation is a three-arm, two-site randomized comparison of ESTEEM to LGBQ-affirmative community mental health treatment and single-session HIV counseling and testing (ClinicalTrials.gov registration: NCT02929069).
Inclusion criteria for the parent clinical trial were as follows: (1) age 18–35; (2) identity as a gay or bisexual man; (3) HIV-negative status confirmed through in-office testing; (4) diagnosis of any Diagnostic and Statistical Manual (DSM-5) depressive, anxiety, and/or trauma-/stressor-related disorder using the interview-administered Mini International Neuropsychiatric Interview for DSM-5; (5) HIV-transmission-risk behavior (defined as ≥1 act in past-90-day condomless anal sex with a male partner of unknown status or HIV+ status, unless with a HIV+ primary/main partner with known undetectable viral load); (6) not currently adherent to PrEP (pre-exposure prophylaxis) (defined as taking ≥4 days per week); (7) NYC or Miami residential stability and planned availability for 12 months; and (8) provision of informed consent.
Exclusion criteria included: (1) current active suicidal or homicidal ideation (but not passive suicidal ideation); (2) active untreated mania, psychosis, or gross cognitive impairment; (3) current enrollment in an intervention study; (4) currently receiving ≥1 mental health treatment sessions per month or ≥8 or more CBT sessions within the past year; and (5) HIV-positive status (confirmed through in-office testing). Additional details about the parent clinical trial can be found in the ClinicalTrials.gov registration, the trial’s published protocol paper (Pachankis et al., 2019), and the primary efficacy paper of the study (Pachankis et al., 2022a).
All participants who completed the 8-month or 12-month follow-up assessment were included in the following analyses. The analytic plan for the present moderation analyses was pre-registered (OSF preregistration: H83J4). Any analyses described as exploratory were not included in the preregistered protocol.
Interventions
Participants were randomized by computer program to receive ESTEEM, LGBQ-affirmative community mental health treatment, or single-session HIV counseling and testing using a 2:2:1 randomization scheme, stratified by site. Additional information about the randomization procedure, interventions, and therapy supervision can be found in the primary trial publication and protocol (Pachankis et al., 2019; Pachankis et al., 2022a).
ESTEEM.
ESTEEM is a 10-session intervention adapted for young gay and bisexual men from the Unified Protocol (Barlow et al., 2017), an individually delivered CBT intervention with efficacy for reducing stress-sensitive mental health disorders (e.g., depression, anxiety) by enhancing emotion regulation skills, reducing avoidance patterns, and improving motivation and self-efficacy for behavior change. The Unified Protocol employs modules for motivation enhancement, interoceptive and situational exposure, cognitive restructuring, mindfulness, and self-monitoring techniques (Wilamowska et al., 2010). ESTEEM adapts the Unified Protocol to enhance young gay and bisexual men’s stigma coping by reducing minority stress processes (Burton et al., 2019; Pachankis, 2014; Pachankis, 2018; Pachankis et al., 2022b). For example, modules were adapted to help young gay and bisexual men identify minority stress experiences; track unhealthy reactions to minority stress, focusing on avoidance reactions, like substance use and condomless anal sex; attribute distress to minority stress rather than to personal failure; and assert themselves against minority stress in safe situations. The intervention was delivered by clinical psychologists, advanced clinical psychology doctoral students, and a Masters-level clinician, who were diverse in race/ethnicity, gender identity, and sexual orientation (n=14). Three clinical psychologists supervised ESTEEM delivery through weekly group and individual supervision, including review of session recordings. One of the study clinicians (Craig Rodriguez-Seijas) and one of the supervisors (John Pachankis) were investigators for the present manuscript. Therapists were highly adherent to the protocol, with mean session ratings of 1.89 out of 2.00 across the 139 reviewed sessions based on ratings using a module-specific fidelity checklist. The average ESTEEM participant attended 8.3 sessions (SD = 3.2).
Community Mental Health Treatment (CMHT).
This arm consisted of 10 sessions of LGBQ-affirmative psychotherapy in the community, provided at two established LGBTQ mental health clinics (one at each site) known for LGBTQ-affirmative psychotherapy. These sites delivered the standard of care at their site, which generally included low levels of psychodynamic-interpersonal and/or CBT interventions (Pachankis et al., 2022a), as determined through ratings of recorded therapy sessions using the Comparative Psychotherapy Process Scale (Hilsenroth et al., 2005). LGBQ-affirmative community mental health treatment was selected as an active control reflecting the current standard of care for LGBQ individuals (American Psychological Association Task Force on Psychological Practice with Sexual Minority Persons, 2021), as contrasted with the specific integration of CBT with minority stress principles and techniques provided by ESTEEM. Therapists in this arm were not specifically trained in ESTEEM or CBT and could use any therapy techniques they deemed appropriate for a given patient. The average CMHT patient attended 6 sessions (SD = 4.1).
Single-session HIV Counseling and Testing.
HIV Counseling and Testing (HCT) consisted of HIV/STI testing and counseling lasting approximately 45 minutes within one session, following established guidelines (AIDS Institute, 2017; Kamb et al., 1998; Koblin et al., 2004). A trained counselor at the research site reviewed the purpose, benefits, and risks of HIV/STI testing; provided information about transmission risk and prevention; assessed the participant’s readiness for testing; conducted the testing and reviewed HIV test results; worked with the participant to develop a personalized risk reduction plan; and provided referrals as necessary for sexual or mental health care. Thus, there was little to no discussion of minority stress or co-occurring mental health problems in HCT as compared to ESTEEM. This comparison intervention was therefore included to help inform the added benefits of providing a more comprehensive treatment approach for young sexual minority men experiencing HIV-transmission-risk behavior in the context of other psychosocial health concerns, such as depression or substance use problems. Provision of referrals for follow-up sexual health care (e.g., in the event of a positive STI test result) and mental health care (in the context of a mental health treatment study) is standard and ethical. Six out of 43 (14.0%) HCT participants assessed at 4-months (end of intervention period) reported seeking mental healthcare during the intervention period. Participants were contacted within one week to provide test results for chlamydia and gonorrhea. Participants in the other two treatment arms also received HCT before their first intervention session.
Treatment Comparison.
Per the pre-registered protocol, the two control conditions were combined into one group to compare to ESTEEM. This permitted identification of variables uniquely predicting response to ESTEEM as compared to existing, commonly used interventions for this population.
Outcome Variables
ESTEEM is intended to be a transdiagnostic intervention in that it seeks to reduce the minority stress mechanisms theorized to underlie gay and bisexual men’s disproportionate risk of mental and behavioral health concerns relative to heterosexual men (Hatzenbuehler, 2009; Meyer, 2003). We developed a comorbidity index given the transdiagnostic basis of the ESTEEM intervention (Burton et al., 2019; Pachankis, 2014), which served as the primary pre-registered outcome for this analysis. This comorbidity index was composed of measures of depression, anxiety, alcohol/drug problems, and HIV-transmission-risk behaviors. To calculate an index giving equal weight to each of these component measures (given the range of behavioral health problems represented among participants and that formed inclusion criteria for the study), we first standardized the scales by calculating score quintiles for each measure. The quintiles for each scale were subsequently summed to create the comorbidity index – with values ranging from 0 to 16. This approach of using quintiles has the benefit of handling non-normally distributed outcomes and being comparable across assessment points when summed into an aggregate index of outcomes, as we did here.
All outcome measures were administered at baseline, and 4-month, 8-month, and 12-month follow-up. As the pre-registered outcome timepoint, we used 8-month follow-up outcomes, which occurred approximately 4 months post-intervention and was also designated the primary outcome point of the parent clinical trial. We wanted to choose an assessment point that did not correspond to immediately after completing treatment, per findings in the moderator literature that moderators predicting outcomes at a post-treatment follow-up may be more clinically relevant (e.g., van Bronswijk et al., 2021). We also examined the generalization of attained moderators to the 12-month follow-up (8-month post-intervention) assessment point.
For significant moderators of the comorbidity index, we also decomposed the index into its four component outcomes, as follows:
Hamilton Rating Scale for Depression (HAM-D; Hamilton, 1960).
The HAM-D is a widely used interviewer-based measure for assessing depression symptoms and was administered by trained interviewers masked to treatment condition using a structured interview guide (Williams et al., 2008). Twenty-five raters over the course of the trial established reliability to four taped reference assessments (ICC [2,1] = 0.93) and met biweekly with a clinical supervisor to establish consensus ratings and prevent drift. The HAM-D exhibited adequate internal reliability in this sample (Cronbach’s α = 0.75, 0.81, 0.79, and 0.84 at baseline, 4-month follow-up, 8-month follow-up, and 12-month follow-up assessments, respectively).
Beck Anxiety Inventory (BAI; Beck et al., 1988).
The BAI is a psychometrically reliable and change-sensitive self-report measure of general anxiety symptoms, covering both physical (e.g., heart pounding/racing; faint/lightheadedness) and cognitive (e.g., fear of losing control; nervousness) anxiety symptoms. The BAI exhibited excellent internal reliability in this sample (Cronbach’s α = 0.91, 0.93, 0.93, and 0.93 at baseline, 4-month follow-up, 8-month follow-up, and 12-month follow-up assessments, respectively).
Short Inventory of Problems-Alcohol and Drugs (SIP; Kiluk et al., 2013).
The SIP is a self-report measure assessing the impact of problematic drinking and drug use, including on physical health, interpersonal relationships, self-concept or mood (i.e., intrapersonal), impulsive behaviors, and social responsibilities. The SIP exhibited excellent internal reliability in this sample (Kuder-Richardson-20 = 0.90, 0.91, 0.90, and 0.90 at baseline, 4-month follow-up, 8-month follow-up, and 12-month follow-up assessments, respectively).
Past-90-Day HIV-Transmission-Risk Behavior (Past 90 Days; Carey et al., 2001; Sobell & Sobell, 1992).
Number of condomless anal sex acts in the absence of PrEP or known undetectable viral load of HIV+ partners over the past 90 days was determined using an interviewer-administered timeline follow-back interview. All interviewers were trained to reliability, all interviews were recorded, and 20% were randomly reviewed for quality assurance.
Moderator Variables
With the exception of internalized stigma (Millar et al., 2016), to our knowledge no other moderators of LGBQ-affirmative psychotherapy effects have been explored in previous studies. Prior exploratory moderator research of other treatments has tended to either use all available variables or to select a reduced number of variables based on clinical theory, hypothesized treatment mechanisms, past findings on variables predicting prognosis (i.e., irrespective of specific treatment), or even ease of measurement (Cohen et al., 2020; Keefe et al., 2020; Schwartz et al., 2021).
We aimed to use an innovative approach to selecting variables for examination as potential moderators in this investigation of treatment effect heterogeneity and to integrate research and theory with the perspectives of study researchers and study clinicians. After the clinical trial was completed, we surveyed ESTEEM trial therapists to ascertain their clinically informed hypotheses as to the potential variables that might predict which participants especially benefitted (or not) from ESTEEM compared to the other two conditions. These therapists (n = 9 of 14 total) completed a survey and qualitative assessment asking them to identify those baseline variables that they believed might have moderated the clinical effects of ESTEEM relative to the other treatment conditions, based on their experiences delivering the treatment. Importantly, potential moderators were not generated by the therapists but rather selected a priori at the start of the trial by the study investigators, based on theory and research related to minority stress (Hatzenbuehler, 2009; Meyer, 2003) and on psychotherapy process and outcome research (Crits-Christoph & Connolly Gibbons, 2021); therapists then selected among these variables. Using the survey and qualitative assessment of the study therapists, one author (John Pachankis) selected potential moderators that were repeatedly identified across the therapists. We include further details on this selection in the Online Supplement. We also included the baseline values for the outcome variable (comorbidity index) as a possible moderator, for a total of 20 potential moderating variables, which is consistent with the number of moderators explored in previous investigations (Cohen et al., 2020; Keefe et al., 2020; Schwartz et al., 2021). The included variables, tested as potential moderators, were conceptualized in the following four categories:
Demographic/history variables.
Therapists identified three potential demographic/history variables that might moderate ESTEEM efficacy, including racial/ethnic minority identification, income (reported as an ordinal variable with seven values ranging from <$10,000/year to >$75,000 year), and number of potential PTSD Criterion A trauma exposures as per the self-report Brief Trauma Questionnaire (Schnurr et al., 1999).
Pre-treatment comorbidities.
Therapists identified two comorbidities that they believed may influence response to ESTEEM: greater difficulties with alcohol and drugs as per the self-report Short Inventory of Problems-Alcohol and Drugs (Kiluk et al., 2013) and suicidal ideation on the Suicide Ideation Attributes Scale (van Spijker et al., 2014).
Clinical facilitators.
Therapists identified four clinical facilitators that might moderate ESTEEM efficacy, including: 1) social support, as measured by the 12-item self-report Multidimensional Scale of Perceived Social Support (Dahlem et al., 1991); 2) emotion regulation, as measured by the 36-item Difficulties in Emotional Regulation Scale (Gratz & Roemer, 2004); 3) trait self-concealment, as measured by the 7-item Self-Concealment Scale (Larson & Chastain, 1990); and 4) the extent to which participants attribute their mental health problems to LGBQ-related stress, as measured with a 3-item scale created for this purpose (adapted from Lebowitz & Ahn, 2015).
Minority stress.
Therapists generally believed that participants who reported greater minority stress experiences would have a relatively better response to ESTEEM, given its focus on reducing minority stress processes. These minority stress variables included current parental non-acceptance of the participant’s sexual orientation (Pachankis et al., 2008), constructs measured by six subscales of the LGB Identity Scale (i.e., acceptance concerns; difficult process coming to terms with one’s sexual identity; identity centrality; identity uncertainty; internalized stigma; and concealment motivation; Mohr & Kendra, 2011), stigma salience (Quinn & Chaudoir, 2009), stigma consciousness (Pinel, 1999), and perceived stress from within the gay community (Pachankis et al., 2020b).
Analysis
All analyses were conducted within the R statistical computing environment (R Core Team, 2021).
Missing data.
To impute missing data, we employed a validated random forest imputation methodology producing a single dataset amenable to the variable selection/machine learning methods used in this study to detect moderation (Stekhoven & Bühlmann, 2011). We assumed that missing baseline data were missing at random at worst (Little’s MCAR test χ2 = 56.3, df = 73, p =.926). We also imputed 8-month follow-up outcomes for participants who missed their 8-month assessment using their 12-month follow-up outcomes, if available. Overall, there was a very low level of missing baseline data (average missing = 1.9%). Fifteen participants had a 12-month follow-up but not an 8-month follow-up assessment. The imputation was estimated to be excellent per norms from the method’s developers (normalized root mean square error = 0.01; percentage of false classifications = 8.7%; see Stekhoven & Bühlmann, 2011 for norms). As a check on our imputation, we also ran a complete cases analysis to examine the extent to which the imputation influenced the findings. There were no notable changes to the pattern of results, potentially due to the low level of missing data (results available upon request).
Variable selection.
Random forest model-based recursive partitioning (MoB; Garge, Bobashev, et al., 2013), a type of machine-learning, was employed for variable selection among the possible moderators. This procedure takes a basic parametric model and attempts to detect cut points in variables in which splits into two subgroups lead to significantly different model behavior on either side of the split, forming a tree structure of potential cut-points. For example, this approach could detect whether a parametric model had significantly different beta weights when an individual was over the age of 40 versus under the age of 40.
The extension of this model employs MoB within bootstrapped re-samplings of the dataset across multiple trees to make a “forest.” For each bootstrap, the resulting tree is tested on the out-of-bag sample, which is held out of a given tree construction. A variable’s ability to predict out-of-bag is compared to the ability of randomly permuted data to make the same prediction. Averaging across the trees, variables with a prediction statistic higher than that of the absolute value of the moderator with the most negative predictive value (i.e., in which the permuted data is superior to the real data) are retained (Strobl et al., 2008). We set the algorithm such that at least fifteen participants must be present on each side of a tree split, with an alpha of 0.05 for the split, and 10,000 trees were generated. Following recommended practice for random forest, one third of possible variables (7 out of 20) were randomly allowed to be selected at any given node (i.e., potential split point in a tree). The R package mobForest was employed for this step (Garge, Eggleston, et al., 2013). This procedure partially protects against overfitting by ensuring that any given variable is predictive across bootstrapped replications of the data structure and can predict to groups of participants not used to select the variable (i.e., cross validation).
In this first step, individual variables potentially moderating treatment response were identified. As a second step, these variables were considered in tandem by being subjected to a bootstrapped AIC-based backward selection model (Austin & Tu, 2004) using a linear regression for comparisons, which has demonstrated superior out-of-sample predictions to standard backward selection and is comparable to that of cross-validated models. This model predicted 8-month comorbidity index scores from all main effects of the variables retained from step one and their interactions with treatment condition, covarying for baseline comorbidity index scores. This step considers the robustness of the predictive value of all selected variables considered in tandem in the same model, rather than separately as in the random forest partitioning variable selection. To make it to the final model, a variable had to be retained in the model in at least 60% of 10,000 bootstrapped replicates (Austin & Tu, 2004). The R package bootStepAIC was employed for this step (Rizopoulos, 2009).
This overall variable selection procedure has been employed in several prior treatment moderator investigations (e.g., Cohen et al., 2020; Keefe et al., 2020), including one identifying significant replication of moderation results in a true hold-out sample (Schwartz et al., 2021). We selected this approach in part because variable selection methods entailing cross-validation and backwards variable selection have been found in simulation studies to be superior at reducing false positives, relative to other approaches like LASSO (another machine learning method), forward selection, or methods not entailing testing in hold-out samples (Wester et al., 2022).
Moderator testing.
Among the 20 entered variables, those passing through the previously detailed variable selection process were included together in two-way interactions with treatment condition (ESTEEM vs. CMHT/HCT) in a linear regression predicting the 8-month follow-up comorbidity index score, covarying for baseline comorbidity index score (Vickers & Altman, 2001). A significant interaction indicated that this characteristic at baseline moderated the clinical effects of ESTEEM as compared to LGBQ-affirmative community treatment and HIV testing and counseling on 8-month outcomes.
For significant moderators, we examined whether the moderation effect differed when comparing ESTEEM separately to either LGBQ-affirmative community treatment or HIV testing and counseling. Using the same regression framework, we also examined the generalizability of attained moderators to each of the four component outcomes of the comorbidity index (i.e., HAM-D, BAI, SIP, and number of risky anal sex acts) and to 12-month follow-up outcomes in the comorbidity index. As an additional check of the potential generalizability of our findings, we probed whether treatment site influenced the moderating effects of attained variables, through examining whether there were three-way interactions (p >.10) between the moderator variable, treatment condition, and treatment site. A lack of an interaction suggests that the moderator is acting similarly across sites, providing further evidence for its generalizability.
Results
Descriptive Statistics and Basic Treatment Outcomes
254 participants enrolled in the study (see Table 1 for baseline descriptive statistics, including differences between sites). Participants were predominantly cisgender (92.9%). A majority identified as gay (73.5%); 20.9% identified as bisexual and 5.1% as queer. Participants were allowed to select multiple gender categories, one of which had to be “man” for inclusion. Sixteen participants reported being transgender, genderqueer, or gender non-binary; three were assigned female at birth. Over four-fifths (81.8% of participants enrolled, n = 207) had an 8-month or 12-month follow-up outcome assessment and were included in the moderator analysis.
Table 1.
Baseline characteristics of trial participants, divided by treatment condition (n = 254 at baseline)
| Variable Name | (M/SD) or (# Yes / %) ESTEEM (n=100) | CMHT/HCT (n=154) |
|---|---|---|
|
| ||
|
| ||
| Outcomes | ||
|
| ||
| Comorbidity index (0–16) | 8.4 (3.2) | 8.3 (3.3) |
|
| ||
| Past-90-day HIV-transmission-risk behaviors | 7.8 (10.1) | 7.2 (8.5) |
| Hamilton Rating Scale for Depression | 16.1 (6.3) | 15.5 (6.8) |
| Beck Anxiety Inventory | 21.3 (11.2) | 22.0 (11.8) |
| Short Inventory of Problems-Alcohol and Drugs | 4.9 (4.4) | 4.6 (4.3) |
|
| ||
| Potential Moderators: Demographics and Personal History | ||
| Race | ||
| White | 53 (53.0%) | 88 (57.1%) |
| Black/African-American | 20 (20.0%) | 23 (14.9%) |
| Asian | 5 (5.0%) | 5 (3.2%) |
| American Indian or Alaskan Native | 1 (1.0%) | 0 (0%) |
| Native Hawaiian or Pacific Islander | 0 (0%) | 2 (1.2%) |
| Multiracial | 12 (12.0%) | 26 (16.9%) |
| Other | 9 (9.0%) | 9 (5.8%) |
| Ethnicity (% Latino) | 43 (43.0%) | 65 (42.2%) |
| Income Category (1–7) | 3.6 (1.9) | 3.3 (1.8) |
| Brief Trauma Questionnaire—Number of Categories | 1.5 (1.7) | 1.7 (1.8) |
|
| ||
| Potential Moderators: Pretreatment Comorbidities | ||
|
| ||
| Short Inventory of Problems-Alcohol and Drugs | 4.9 (4.4) | 4.6 (4.3) |
| Suicide Ideation Attributes Scale | 3.4 (7.5) | 4.0 (6.7) |
|
| ||
| Potential Moderators: Clinical Facilitators | ||
|
| ||
| Multidimensional Scale of Perceived Social Support | 4.4 (1.3) | 4.3 (1.5) |
| Difficulties in Emotional Regulation Scale | 95.5 (20.3) | 95.8 (23.8) |
| Self-Concealment Scale | 2.3 (0.8) | 2.2 (0.8) |
|
| ||
| Potential Moderators: Minority Stressors | ||
|
| ||
| Causal Attributions for Symptoms (LGBQ-Related) | 12.3 (5.4) | 12.5 (5.1) |
| Parental Attitudes Toward Son’s Sexual Orientation | 2.6 (1.4) | 2.4 (1.3) |
| LGB Identity Scale | ||
| Acceptance Concerns | 3.4 (1.2) | 3.5 (1.3) |
| Difficult Process | 3.7 (1.3) | 3.6 (1.4) |
| Identity Centrality | 4.1 (1.1) | 4.0 (1.2) |
| Identity Uncertainty | 2.1 (1.2) | 1.9 (1.1) |
| Internalized Homonegativity | 2.3 (1.3) | 2.5 (1.5) |
| Concealment Motivation | 3.7 (1.2) | 3.4 (1.2) |
| Stigma Salience | 4.5 (1.8) | 4.0 (2.0) |
| Stigma Consciousness | 3.6 (0.9) | 3.5 (1.0) |
| Gay Community Stress Scale | 3.9 (0.6) | 3.9 (0.6) |
Note. CMHT = LGBQ-Affirmative Community Mental Health Treatment; ESTEEM = Effective Skills to Empower Effective Men; HCT = HIV Counseling and Testing
Controlling for baseline values in the comorbidity index, participants receiving ESTEEM had lower comorbidity index scores at 8-month follow-up compared to participants randomized to the LGBQ-affirmative community treatment and HIV testing and counseling arms (B = −1.35 [95% CI: −2.16 to −0.53], t[204] = −3.26, p = 0.001, d = −0.46). When examining the treatment effect across component comorbidity index outcomes at the 8-month follow-up, ESTEEM was significantly superior to other treatments at improving alcohol and drug problems (d = −0.39, p = 0.006). However, ESTEEM was not significantly superior at reducing HAM-D depression (d = −0.23, p = 0.095), BAI anxiety outcomes (d = −0.25, p = 0.075), or past-90-day HIV-transmission-risk behavior (d = −0.22, p = 0.112). There was no significant effect of site (F[1,202] = 0.33, p = 0.569) or a site-by-treatment interaction in predicting the 8-month follow-up comorbidity index (F[1,202] = 0.96, p = 0.328).
Variable Selection for Treatment Moderation
As our first variable selection step, we employed a random forest variant of model-based recursive partitioning (Garge et al., 2013). Five variables were retained at this first step based on the fact that they moderated treatment outcomes in held-out data better than randomly permuted values of the dataset: racial/ethnic minority identification, stigma consciousness, alcohol/drug use problems, social support, and parental non-acceptance of the participant’s sexual orientation (see Supplemental Figure 1 for the variable importance plot).
When subjected to the second variable selection step (bootstrapped backward-elimination), only two variables, racial/ethnic identification (99%) and stigma consciousness (71%), were retained as moderators in >60% of bootstrapped replications of the full model (our preregistered inclusion criterion; Austin & Tu, 2004). Thus, the remaining three potential moderators (alcohol/drug use problems, social support, and parental non-acceptance) were removed as interactions from the final moderation model.
Moderation Model
Racial/ethnic minority identification.
Participants’ identification as a racial and/or ethnic minority (i.e., any racial/ethnic minority identity other than non-Latino White) significantly interacted with treatment condition (ESTEEM vs. LGBQ-affirmative community treatment and HIV testing and counseling) to predict 8-month follow-up comorbidity index scores (B = −3.23 [95% CI: −5.03, −1.64], t[197] = −3.88, p < 0.001; see Figure 1 and Table 2). This interaction was similar for ESTEEM as compared separately to both LGBQ-affirmative community treatment (B = −2.74 [95% CI: −4.66, −0.83], t[200] = −2.83, p = 0.005) and HIV testing and counseling (B = −2.81 [95% CI: −5.06, −0.55], t[200] = −2.46, p = 0.015). Probing this interaction found no significant treatment condition differences among non-Latino White participants in 8-month follow-up comorbidity index scores (d = 0.22, p = 0.391). In contrast, among racial and/or ethnic minority participants, receiving ESTEEM relative to LGBQ-affirmative community treatment or HIV testing and counseling was associated with a significantly lower 8-month follow-up comorbidity index score (d = −0.71, p <.001).
Figure 1. Comorbidity index outcomes at 8-month follow-up for ESTEEM versus control treatments for non-Latino White versus racial/ethnic minority participants (n = 207).
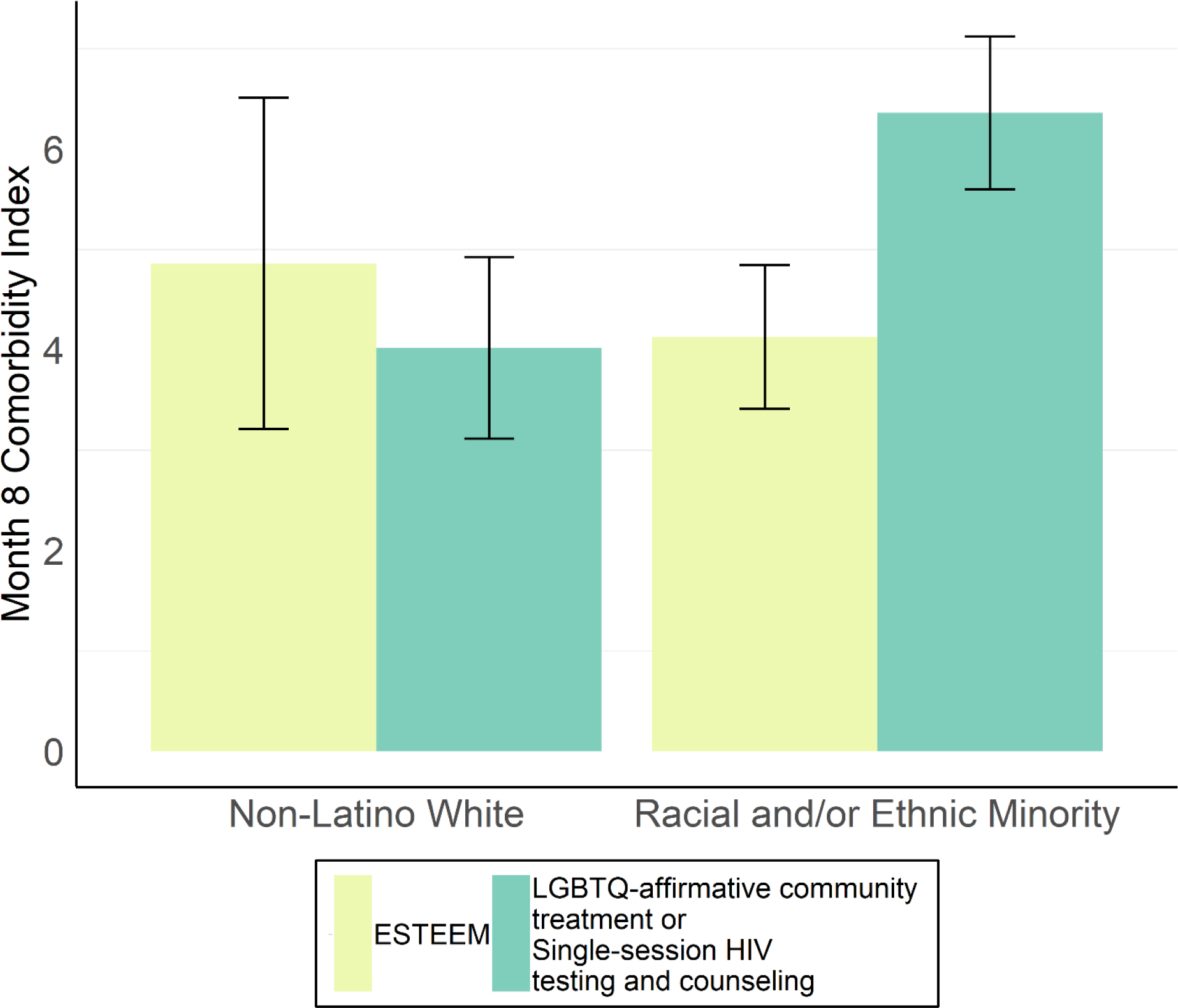
Note. Bars reflect 95% confidence intervals. Displayed values reflect Month 8 scores controlling for Baseline scores. Treatment had no differential effect on 8-month follow-up comorbidity index outcomes for White, non-Latino participants (d = 0.22, p = 0.391), but was associated with a medium-large effect in favor of ESTEEM among racial/ethnic minority participants (d = −0.71, p < 0.001). Among the racial/ethnic minority identifications able to be examined in this sample, this effect was replicable among Black and Latino, but not multiracial, participants.
Table 2.
Baseline characteristics of trial participants, divided by treatment condition (n = 254 at baseline)
| Variable Name | Beta weight (unstandardized) & 95% CI | p-value |
|---|---|---|
| Baseline Comorbidity Index Score | 0.49 [95% CI: 0.37 to 0.61] | <.001 |
| Racial/Ethnic Minority Identification | 2.05 [95% CI: 1.00 to 3.01] | <.001 |
| Stigma Consciousness | 0.36 [95% CI: −0.14, 0.85] | .157 |
| Racial/Ethnic Minority Identification x ESTEEM | −3.23 [95% CI: −5.03, −1.64] | <.001 |
| Stigma Consciousness x ESTEEM | −0.75 [95% CI: −1.58, 0.07] | .073 |
Note. In the context of an interaction, main effects reflect the predictive value of a variable when treatment is CMHT/HCT, while the interaction term reflects the modification of that variable’s beta weight when the treatment is ESTEEM.
In an exploratory (i.e., non-preregistered) linear regression analysis, we examined specific racial minority identifications and Latino identification, in interaction with treatment condition, in predicting 8-month follow-up outcomes. Relative to White participants, Black/African American participants (B = −2.25 [95% CI: −4.46, −0.03], t[189] = −2.00, p = 0.047) had significantly improved outcomes in ESTEEM compared to the other treatments. On the other hand, multiracial participants (i.e., participants who selected this category) did not have significantly different outcomes between treatments (B = −1.56 [95% CI: −3.97, 0.85], t[189] = −1.28, p = 0.204), simultaneously modeling for Latino identification, although the effect was in the same direction as for Black participants. We could not separately explore other racial identifications due to small sample sizes (see Table 1). In addition, identifying as Latino predicted relatively superior outcomes in ESTEEM (B = −2.33 [95% CI: −4.14, −0.52], t[189] = −2.54, p = 0.012), regardless of racial identity.
Stigma consciousness.
Stigma consciousness did not significantly interact with treatment condition to predict 8-month follow-up comorbidity index scores (B = −0.75 [95% CI: −1.58, 0.07], t[197] = −1.81, p = 0.073, interaction r = 0.13; see Table 2). Among participants receiving ESTEEM, there was a nonsignificant, negative relationship between stigma consciousness and 8-month follow-up comorbidity index scores (B = −0.40 [95% CI: −0., 0.85], t[197] = −1.18, p = 0.240, r = −0.13), whereas among participants receiving the comparison interventions, there was a nonsignificant positive relationship between stigma consciousness and 8-month follow-up comorbidity index scores (B = 0.36 [95% CI: −0.14, 0.85], t[197] = 1.42, p = 0.157, r = 0.13).
Site-by-treatment interactions.
Neither racial/ethnic minority identification (F[1,191] = 0.05, p = 0.823) nor stigma consciousness (F[1, 191] = 0.02, p = 0.902) had different moderating influences on treatment outcomes between the two sites.
Generalization of moderators across outcomes
Racial/ethnic minority identification.
Racial/ethnic minority identity remained a significant moderator when predicting 8-month follow-up anxiety symptoms (B = −7.01 [95% CI: −12.91, −1.12], t[197] = −2.35, p = 0.020; d difference for ESTEEM vs. CMHT/HCT for racial/ethnic minority participants = −0.64, d for non-Latino White = 0.13) and alcohol/drug use problems (B = −3.35 [95% CI: −5.11, −1.59], t[197] = −3.75, p<.001; d for racial/ethnic minority participants = −0.70, d for non-Latino White = 0.22). By contrast, racial/ethnic minority identity did not interact with treatment to predict outcomes for depression (B = −1.56 [95% CI: −5.31, 2.19], t[197] = −0.82, p = 0.412; d for racial/ethnic minority patients = −0.31, d for non-Latino White = −0.06) or past-90-day HIV-transmission-risk behavior (B = −2.44 [95% CI: −5.99, 1.10], t[197] = −1.36, p = 0.175; d for racial/ethnic minority participants = −0.43, d for non-Latino White = −0.00), although both nonsignificant interactions were in the same direction as the primary finding. Interactions were similar and in the same direction of effect when restricting analyses to the contrast between participants identifying as Black or Latino versus other participants (anxiety interaction p = 0.040; depression interaction p = 0.437; alcohol/drug use interaction p = 0.002; HIV transmission-risk behaviors p = 0.827).
Stigma consciousness.
Stigma consciousness did not moderate treatment effects for any individual outcome (p range = 0.085–0.811).
Generalization of moderators to 12-month follow-up
At 12-month follow-up, racial/ethnic minority identification still significantly moderated comorbidity index outcomes, such that racial/ethnic minority participants benefited relatively more from ESTEEM compared to the other treatments (B = −2.78 [95% CI: −4.79, −0.78], t[197] = −2.73, p = 0.007; d difference for ESTEEM vs. CMHT/HCT for racial/ethnic minority participants = −0.53, d for non-Latino White = 0.12). However, stigma consciousness was a nonsignificant moderator of treatment effects at this follow-up timepoint (B = −0.07 [95% CI: −1.04, 0.90], t[197] = −0.14, p = 0.893).
Exploration of mediation of race/ethnicity moderation
Given the robustness of the moderating effect of racial/ethnic minority identification and specificity of this finding to Black and Latino men, we conducted further exploratory (i.e., non-preregistered) analyses to examine possible minority stress and psychotherapy process mediators of this moderation effect. From the available variables, we examined rejection sensitivity, internalized stigma, motivation to conceal sexual orientation, reported impact of experiences of sexual-orientation or racial/ethnic-based discrimination, change in attributions for the causes of mental and behavioral health problems, and participant-rated therapeutic alliance. However, we were unable to identify a clear mediator for this moderation finding (see Supplementary Analyses for the full statistical report); that is, differences in amount of change among these variables did not appear to explain why racial/ethnic minority individuals—or specifically Black or Latino individuals—derived more benefits from ESTEEM compared to the other two conditions.
Discussion
ESTEEM represents the first LGBQ-affirmative CBT intervention to have been tested in a randomized controlled trial with gay and bisexual young men experiencing mental and behavioral health concerns (Pachankis et al., 2015; Pachankis et al., 2022a). Whether it might be particularly beneficial among some gay and bisexual men has not been previously explored—despite potential implications for personalized treatment and implementation.
We used a novel approach to identify potential treatment moderators of ESTEEM’s efficacy, namely by surveying the study clinicians for candidate moderators. Results demonstrated that identification as a racial or ethnic minority significantly moderated the efficacy of the ESTEEM intervention. ESTEEM was superior to LGBQ-affirmative community treatment and HIV testing and counseling among participants identifying as racial or ethnic minority—namely, Black/African American and Latino—on a comorbidity outcome measured at the pre-registered 8-month follow-up. No similar superiority for ESTEEM compared to control interventions was observed among non-Latino White participants on this comorbidity outcome. This moderation by race/ethnicity generalized to anxiety symptoms and alcohol/drug use problems, and it persisted at the 12-month follow-up. None of the remaining 19 potential moderators were significant.
Racial and ethnic minority individuals are underrepresented in randomized controlled intervention trials and mental health research (Hartmann et al., 2013; Iwamasa et al., 2002; Nagendra et al., 2020; Perez-Aquino et al., 2020); not infrequently, sample sizes of racial and ethnic minority individuals in randomized controlled trials are too small to permit comparisons of efficacy based on racial and ethnic identity (Santiago & Miranda, 2014). However, the racial/ethnic diversity of participants in the present trial permitted examination of the impact of racial/ethnic identification on the efficacy of the ESTEEM intervention. Contradicting research findings that racial and ethnic minority individuals sometimes experience worse treatment outcomes than their non-Latino White peers (e.g., Eack & Newhill, 2012; Windsor et al., 2015 though see Carpenter et al., 2018 for a null finding among CBTs for anxiety), our results demonstrate that ESTEEM was specifically beneficial for Black and Latino participants in reducing mental and behavioral health comorbidities in this trial.
It is unclear, however, what components of ESTEEM may have driven this moderation, or what treatment mechanisms or therapy processes were especially facilitated by ESTEEM that made it more effective with Black and Latino gay and bisexual men compared to non-Latino White men. While ESTEEM therapists were encouraged to be attentive to the intersections between sexual orientation and race/identity, the manualization of the intervention as delivered in this study focused on sexual orientation minority stress and not explicitly on other forms of minority stress. An exploratory examination of possible mediators of the racial/ethnic minority moderation—focusing on LGBQ minority stress processes (e.g., internalized stigma), change in attributions about the causes of one’s symptoms, and the therapeutic alliance—did not uncover any significant differences in treatment-related changes in these factors according to racial/ethnic identification. However, this study measured predominantly sexual minority stress processes.
It is possible that the methods by which ESTEEM facilitates coping with sexual orientation stigma—such as providing individuals with psychoeducation about stigma-related frameworks (e.g., minority stress), teaching them new stigma coping strategies (e.g., using present-focused awareness to reduce the impact of stigma), and providing structure and motivation to reduce stigma-related stress (e.g., via weekly therapy sessions and home practice assignments)—may have also been relevant to and facilitated coping with race-related stressors (e.g., internalized racism; racial identity management; Williams, 2018) and/or intersectional stressors (e.g., coping with racism in the LGBTQ community or heterosexism in one’s racial/ethnic minority community; racial/sexual identity conflict; Jackson et al., 2021; Jackson et al., 2020). Because measures of these potential mediators were not included in the present trial, future research should further study the race-related and intersectional stressors that might explain racial and ethnic minority individuals’ experience of this and other evidence-based treatments.
Another possibility is that ESTEEM’s focus on the underlying role of minority stress on mental and behavioral health may be especially consonant with the experiences of some racial and ethnic minority individuals. For instance, racial/ethnic socialization refers to the mechanisms through which parents and caregivers transmit information about race and ethnicity to their child. Often included in these socialization processes is education regarding structural inequity and the need to be prepared for facing bias from racial and ethnic majority populations (e.g., Hughes et al., 2006). It is possible that ESTEEM’s explicit focus on interrogating and understanding the ways in which sexual minority stress impacts wellbeing also aligned with earlier racial/ethnic socialization messages transmitted to some racial/ethnic minority participants, thereby permitting easier uptake of the treatment model, and consequently stronger treatment gain. Thus, racial/ethnic minority participants may have been better able to leverage and integrate the minority-stress-focused principles and techniques of ESTEEM within their pre-existing skills for coping with racism and racialized stigma as compared to non-Latino White participants (DiGuiseppi et al., 2021). Although we found that the reported impact of experiences of racial/ethnic discrimination did not explain the treatment effect moderation by racial/ethnic identification, this variable does not fully capture racial/ethnic socialization experiences, which were not assessed in this study.
It might also be the case that by virtue of its explicit focus on minority stress, the ESTEEM intervention permits more open dialogue about the impact of race/ethnicity-related minority stress on Black and Latino participants’ wellbeing than did the control conditions, which did not have a specific focus on minority stress. This explicit focus on minority stress might have produced therapeutic conversations about the broader identity-related factors impacting minoritized participants, as well as case conceptualizations and techniques that addressed broader identity-related stressors beyond just sexual-minority-specific stress (Adames et al., 2018). For example, ESTEEM’s assertiveness module not only counters the ways LGBTQ people learn to be unassertive in an unsafe, anti-LGBTQ world, but also potentially the ways that people of color learn to be unassertive in response to racist stereotypes and interracial hostility (Wilkins et al., 2012). Indeed, the ESTEEM approach to case conceptualization encourages the consideration of the client’s broad sociocultural context and intersecting identities and identity-related stressors (Pachankis et al., 2022b), and a separate open pilot of ESTEEM specifically for racial/ethnic minority gay and bisexual men shows preliminary promise for addressing stress due to anti-sexual minority stigma, racism, and their intersections (Jackson et al., 2022). ESTEEM’s approach may be especially impactful in this population given that structural stigma toward sexual minorities, such as anti-LGBTQ legislation, seems to have a stronger impact on the mental health of Black and Latino sexual minority men than on White sexual minority men (English et al., 2022; English et al., 2021), potentially because they have fewer buffers against the impact of such stigma (e.g., smaller/less supportive LGBTQ social networks; Frost et al., 2016).
Additional quantitative and qualitative research into the treatment experiences of racial/ethnical minority gay and bisexual men who receive ESTEEM may help explain the superior benefit of ESTEEM for Black and Latino compared to non-Latino White gay and bisexual men. Future research that identifies the treatment components and target mechanisms preferentially engaged by ESTEEM among Black and Latino individuals could also lead to further refinements of the treatment model to better serve this population and emphasize the most helpful aspects of ESTEEM during dissemination and implementation. Insights garnered from this research may also lead to more general enhancements of ESTEEM. For instance, if Black and Latino participants benefited more from ESTEEM because they were particularly likely to develop skills for navigating stigma (perhaps because of their greater preparation or other ability to do so), future refinements of the treatment model could emphasize behavioral skills practice—either among those with deficits in this area or among all recipients.
Contrary to our expectations, none of the LGBQ minority stress variables (e.g., internalized stigma) emerged as robust moderators of treatment outcome. On the one hand, these results are unexpected given ESTEEM’s focus on targeting minority stress processes using a CBT approach, and previous research showing that ESTEEM was especially superior to a waitlist control among young gay and bisexual men with higher internalized homonegativity (Millar et al., 2016). However, an LGBQ-affirmative treatment stance characterized all three treatments examined in the present trial, including LGBQ-affirmative community treatment and single-session HIV counseling and testing. This shared identity-affirmative framework may have attenuated possible differences in outcomes specifically attributable to minority stress processes. Future research might find that these factors more strongly moderate the efficacy of ESTEEM compared to other treatments that are not explicitly identity affirming, such as a waitlist control, general community psychotherapy or pharmacotherapy, or non-adapted CBT, as has been documented in studies with other stigmatized groups (e.g., Lee et al., 2019). On the other hand, sexual minority stress is not orthogonal to our moderation finding on race/ethnicity, as racial/ethnic minority participants also reported significantly higher sexual orientation concealment motivation, internalized stigma, stress related to the gay community, negative reactions from parents upon coming out, and tendency to attribute their mental and behavioral problems to sexual minority stress (see Online Supplement). ESTEEM may be uniquely positioned to address these stressors as they specifically co-occur with stressors related to race/ethnicity, a possibility that warrants further inquiry (Jackson et al., 2022).
Limitations
We note several study limitations. Given the sample size of the present study, follow-up analyses to our overall race/ethnicity finding were only able to examine moderation among participants identifying as Black, Latino, multiracial, and non-Latino White, and therefore the attained results may not extend to other racial or ethnic groups. The match of ESTEEM to other minoritized groups (e.g., Asians) is critical for future research. These effects could also differ for Black or Latino men outside the United States who have different experiences of stigmatization. When examining the component parts of the comorbidity index—namely depression, anxiety, alcohol/drug problems, and HIV-transmission risk behavior—anxiety and alcohol/drug problems emerged as the most robustly related to treatment effect moderation by racial/ethnic identity. Less support exists that this moderation effect extends to improvements in depression and HIV-transmission-risk behavior. This trial also did not adequately measure racial/ethnic or intersectional minority stress, and future trials testing LGBQ minority stress-focused treatments should seek to include appropriate measures to assess whether (and how) these treatments address other forms of minority stress. Further, the present study enrolled a relatively specific sample—young gay and bisexual men with mental health symptoms and a heightened risk of contracting HIV—and the present findings might not generalize to other sexual minority populations.
Exploratory moderator analyses rely on several subjective decisions influencing which variables are included in a final model. These decisions regard the methods used to select variables, and how strict to set parameters indicating how well a variable must perform to be retained (Chekroud et al., 2021; Wester et al., 2022)—which often involve considering trade-offs between false positives (i.e., incorrectly identifying prescriptive factors for treatment selection) and false negatives (i.e., missing informative variables). In the case of the present study, our pre-registered selection process incorporating features of cross-validation and bootstrapping (Austin & Tu, 2004; Garge et al., 2013) may have eliminated some moderators with small, but real, effects. This concern is heightened by the sample size of this study, which while perhaps sufficient for the primary trial aims might have produced insufficient power to detect smaller moderator effects (Luedtke et al., 2019). On the other hand, our primary identified moderator—racial/ethnic identification—was associated with a highly statistically significant effect that would have survived a Bonferroni correction (adjusted p threshold < .0025) and was replicated across both sites of the trial, which supports generalization of results.
Conclusion
Young gay and bisexual men identifying as Black or Latino may derive greater, potentially lasting symptom relief from a minority-stress-focused intervention like ESTEEM compared to other LGBQ-affirmative interventions, though the mechanisms underlying this moderating effect await identification in future research.
Supplementary Material
Public Health Significance Statement.
In a trial of LGBQ-affirmative cognitive-behavioral therapy (CBT) for gay and bisexual men with comorbid mental and behavioral health concerns, racial/ethnic identification—namely as Black or Latino—emerged as the most robust moderator of the efficacy of this treatment compared to two control conditions. Results suggest that LGBQ-affirmative CBT might represent a promising approach for Black and Latino gay and bisexual men and highlight the need to understand the mechanisms underlying this effect to inform the development of effective intersectional interventions.
Author’s Note and Acknowledgments
The authors would like to acknowledge the following individuals for their contributions to study implementation, data preparation, intervention delivery, and/or clinical supervision: Oluwaseyi Adeyinka, Christopher Albright, Kriti Behari, Alex Belser, Cal Brisbin, Charles Burton, Xiang (Justin) Cai, Bianca Cersosimo, Kirsty A. Clark, Nitzan Cohen, Adam Eldahan, Denise A. Esserman, Benjamin Fetzner, Emily Finch, Calvin Fitch, Tiffany Glynn, Melvin Hampton, Aaron Heller, Ivan Ivardic, Rebecca Kaplan, Michael Katz, Colin Kimberlin, Jasper Lee, Kaitlin R. Maciejewski, Daniel Mayo, Erin McConocha, Kate McMillen, Noelle Mendez, Meghan Michalski, Faithlynn Morris, Rebecca Pepe, Kobe Pereira, Rachel Perler, Marc Puccinelli, Zachary Rawlings, Jesse Reynolds, Maxwell Richardson, Brooke Rogers, Jasmyn Sanders, Satyanand Satyanarayana, Jillian Scheer, Dominic Schnabel, Ingrid Solano, Rosana Smith-Alvarez, Timothy Sullivan, Tennille Taggart, Arjan van der Star, Elliott Weinstein, Amy Weisman de Mamani, Roxanne Winston.
The authors would like to thank the directors and staff of the Institute for Human Identity (New York City) and Care Resource (Miami) for their contributions to this study. The authors would also like to thank the participants in this study for their many contributions to this research.
This study was funded by the National Institute of Mental Health (R01MH109413); the David R. Kessler, MD ’55 Fund for LGBTQ Mental Health Research at Yale; the Fund for Lesbian and Gay Studies at Yale; and the Yale Clinical and Translational Science Award (UL1TR00183). Skyler D. Jackson’s contributions were supported by a grant from the National Institute of Mental Health (K01MH122316), Audrey Harkness contributions were supported by a grant from the National Institute of Minority Health and Health Disparities (K23MD015690). All data are providable upon request.
Footnotes
Steven A. Safren serves as an Associate Editor of the Journal of Consulting and Clinical Psychology. John E. Pachankis, Skyler D. Jackson, Audrey Harkness, and Steven A. Safren receive royalties from Oxford University Press for books related to LGBTQ-affirmative mental health treatments.
References
- Adames HY, Chavez-Dueñas NY, Sharma S, & La Roche MJ (2018). Intersectionality in psychotherapy: The experiences of an AfroLatinx queer immigrant. Psychotherapy, 55(1), 73–79. 10.1037/pst0000152 [DOI] [PubMed] [Google Scholar]
- Institute AIDS. (2017). HIV testing toolkit: Resources to support routine HIV testing for adults and minors. New York State Department of Health. https://www.health.ny.gov/diseases/aids/providers/testing/docs/testing_toolkit.pdf. [Google Scholar]
- American Psychological Association Task Force on Psychological Practice with Sexual Minority Persons. (2021). APA guidelines for psychological practice with sexual minority persons. American Psychological Association. https://www.apa.org/about/policy/psychological-sexual-minority-persons.pdf [DOI] [PubMed] [Google Scholar]
- Anderson RE, & Stevenson HC (2019). RECASTing racial stress and trauma: Theorizing the healing potential of racial socialization in families. American Psychologist, 74(1), 63–75. 10.1037/amp0000392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Austin PC, & Tu JV (2004). Bootstrap Methods for Developing Predictive Models. The American Statistician, 58(2), 131–137. 10.1198/0003130043277 [DOI] [Google Scholar]
- Barlow DH, Farchione TJ, Bullis JR, Gallagher MW, Murray-Latin H, Sauer-Zavala S, Bentley KH, Thompson-Hollands J, Conklin LR, Boswell JF, Ametaj A, Carl JR, Boettcher HT, & Cassiello-Robbins C (2017). The Unified Protocol for Transdiagnostic Treatment of Emotional Disorders Compared With Diagnosis-Specific Protocols for Anxiety Disorders: A Randomized Clinical Trial. JAMA Psychiatry, 74(9), 875–884. 10.1001/jamapsychiatry.2017.2164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Epstein N, Brown G, & Steer RA (1988). An inventory for measuring clinical anxiety: Psychometric properties. Journal of Consulting and Clinical Psychology, 56(6), 893–897. 10.1037/0022-006X.56.6.893 [DOI] [PubMed] [Google Scholar]
- Carpenter JK, Andrews LA, Witcraft SM, Powers MB, Smits JAJ, & Hofmann SG (2018). Cognitive behavioral therapy for anxiety and related disorders: A meta-analysis of randomized placebo-controlled trials. Depression and Anxiety, 35(6), 502–514. 10.1002/da.22728 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burton CL, Wang K, & Pachankis JE (2019). Psychotherapy for the Spectrum of Sexual Minority Stress: Application and Technique of the ESTEEM Treatment Model. Cognitive and Behavioral Practice, 26(2), 285–299. 10.1016/j.cbpra.2017.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey MP, Carey KB, Maisto SA, Gordon CM, & Weinhardt LS (2001). Assessing sexual risk behaviour with the Timeline Followback (TLFB) approach: continued development and psychometric evaluation with psychiatric outpatients. Int J STD AIDS, 12(6), 365–375. 10.1258/0956462011923309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cassiello-Robbins C, Southward MW, Tirpak JW, & Sauer-Zavala S (2020). A systematic review of Unified Protocol applications with adult populations: Facilitating widespread dissemination via adaptability. Clinical Psychology Review, 78, 101852. 10.1016/j.cpr.2020.101852 [DOI] [PubMed] [Google Scholar]
- Cheavens JS, Strunk DR, Lazarus SA, & Goldstein LA (2012). The compensation and capitalization models: a test of two approaches to individualizing the treatment of depression. Behav Res Ther, 50(11), 699–706. 10.1016/j.brat.2012.08.002 [DOI] [PubMed] [Google Scholar]
- Chekroud AM, Bondar J, Delgadillo J, Doherty G, Wasil A, Fokkema M, Cohen Z, Belgrave D, DeRubeis R, Iniesta R, Dwyer D, & Choi K (2021). The promise of machine learning in predicting treatment outcomes in psychiatry. World Psychiatry, 20(2), 154–170. 10.1002/wps.20882 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen ZD, & DeRubeis RJ (2018). Treatment Selection in Depression. Annual Review of Clinical Psychology, 14(1), 209–236. 10.1146/annurev-clinpsy-050817-084746 [DOI] [PubMed] [Google Scholar]
- Cohen ZD, Kim TT, Van HL, Dekker JJM, & Driessen E (2020). A demonstration of a multi-method variable selection approach for treatment selection: Recommending cognitive–behavioral versus psychodynamic therapy for mild to moderate adult depression. Psychotherapy Research, 30(2), 137–150. 10.1080/10503307.2018.1563312 [DOI] [PubMed] [Google Scholar]
- Coyne AE, & Gros DF (2022). Comorbidity as a moderator of the differential efficacy of transdiagnostic behavior therapy and behavioral activation for affective disorders. Psychotherapy Research, 1–12. 10.1080/10503307.2021.2022236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crits-Christoph P, & Gibbons MBC (2021). Psychotherapy Process-Outcome Research: Advances in Understanding Causal Connections. In Barkham M, Lutz W, & Castonguay LG (Eds.), Bergin and Garfield’s Handbook of Psychotherapy and Behavior Change (7th ed., pp. 263–296). Wiley. [Google Scholar]
- Dahlem NW, Zimet GD, & Walker RR (1991). The Multidimensional Scale of Perceived Social Support: a confirmation study. J Clin Psychol, 47(6), 756–761. [DOI] [PubMed] [Google Scholar]
- DiGuiseppi GT, Davis JP, Srivastava A, Layland EK, Pham D, & Kipke MD (2021). Multiple Minority Stress and Behavioral Health Among Young Black and Latino Sexual Minority Men. LGBT Health. 10.1089/lgbt.2021.0230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eack SM, & Newhill CE (2012). Racial Disparities in Mental Health Outcomes After Psychiatric Hospital Discharge Among Individuals With Severe Mental Illness. Social work research, 36(1), 41–52. 10.1093/swr/svs014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- English D, Boone CA, Carter JA, Talan AJ, Busby DR, Moody RL, Cunningham DJ, Bowleg L, & Rendina HJ (2022). Intersecting Structural Oppression and Suicidality Among Black Sexual Minority Male Adolescents and Emerging Adults. J Res Adolesc, 32(1), 226–243. 10.1111/jora.12726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- English D, Carter JA, Boone CA, Forbes N, Bowleg L, Malebranche DJ, Talan AJ, & Rendina HJ (2021). Intersecting Structural Oppression and Black Sexual Minority Men’s Health. American Journal of Preventive Medicine, 60(6), 781–791. 10.1016/j.amepre.2020.12.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fournier JC, DeRubeis RJ, Amsterdam J, Shelton RC, & Hollon SD (2015). Gains in employment status following antidepressant medication or cognitive therapy for depression. British Journal of Psychiatry, 206(4), 332–338. 10.1192/bjp.bp.113.133694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fournier JC, DeRubeis RJ, Shelton RC, Hollon SD, Amsterdam JD, & Gallop R (2009). Prediction of response to medication and cognitive therapy in the treatment of moderate to severe depression. Journal of Consulting and Clinical Psychology, 77(4), 775–787. 10.1037/a0015401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frost DM, Meyer IH, & Schwartz S (2016). Social support networks among diverse sexual minority populations. The American journal of orthopsychiatry, 86(1), 91–102. 10.1037/ort0000117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garge N, Bobashev G, & Eggleston B (2013). Random forest methodology for model-based recursive partitioning: the mobForest package for R [journal article]. BMC Bioinformatics, 14(1), 125. 10.1186/1471-2105-14-125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garge N, Eggleston B, & Bobashev G (2013). mobForest: Random Forest methodology for model-based recursive partitioning. In (Version 1.2) https://cran.r-project.org/package=mobForest [DOI] [PMC free article] [PubMed]
- Gibbons MBC, Gallop R, Thompson D, Gaines A, Rieger A, & Crits-Christoph P (2019). Predictors of treatment attendance in cognitive and dynamic therapies for major depressive disorder delivered in a community mental health setting. Journal of Consulting and Clinical Psychology, 87(8), 745–755. 10.1037/ccp0000414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gratz KL, & Roemer L (2004). Multidimensional Assessment of Emotion Regulation and Dysregulation: Development, Factor Structure, and Initial Validation of the Difficulties in Emotion Regulation Scale. Journal of Psychopathology and Behavioral Assessment, 26(1), 41–54. 10.1023/B:JOBA.0000007455.08539.94 [DOI] [Google Scholar]
- Hall GCN, Ibaraki AY, Huang ER, Marti CN, & Stice E (2016). A Meta-Analysis of Cultural Adaptations of Psychological Interventions. Behavior Therapy, 47(6), 993–1014. 10.1016/j.beth.2016.09.005 [DOI] [PubMed] [Google Scholar]
- Hamilton M (1960). A rating scale for depression. Journal of Neurology, Neurosurgery & Psychiatry, 23, 56–61. 10.1136/jnnp.23.1.56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartmann WE, Kim ES, Kim JHJ, Nguyen TU, Wendt DC, Nagata DK, & Gone JP (2013). In Search of Cultural Diversity, Revisited: Recent Publication Trends in Cross-Cultural and Ethnic Minority Psychology. Review of General Psychology, 17(3), 243–254. 10.1037/a0032260 [DOI] [Google Scholar]
- Hatzenbuehler ML (2009). How does sexual minority stigma “get under the skin”? A psychological mediation framework. Psychological bulletin, 135(5), 707–730. 10.1037/a0016441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML, & Pachankis JE (2021). Does stigma moderate the efficacy of mental and behavioral health interventions? Examining individual and contextual sources of treatment effect heterogeneity. Current Directions in Psychological Science, 30(6), 476–484. 10.1177/09637214211043884 [DOI] [Google Scholar]
- Hilsenroth MJ, Blagys MD, Ackerman SJ, Bonge DR, & Blais MA (2005). Measuring Psychodynamic-Interpersonal and Cognitive-Behavioral Techniques: Development of the Comparative Psychotherapy Process Scale. Psychotherapy: Theory, Research, Practice, Training, 42(3), 340–356. 10.1037/0033-3204.42.3.340 [DOI] [Google Scholar]
- Huey SJ, Tilley JL, Jones EO, & Smith CA (2014). The Contribution of Cultural Competence to Evidence-Based Care for Ethnically Diverse Populations. Annual Review of Clinical Psychology, 10(1), 305–338. 10.1146/annurev-clinpsy-032813-153729 [DOI] [PubMed] [Google Scholar]
- Hughes D, Rodriguez J, Smith EP, Johnson DJ, Stevenson HC, & Spicer P (2006). Parents’ ethnic-racial socialization practices: A review of research and directions for future study. Developmental Psychology, 42(5), 747–770. 10.1037/0012-1649.42.5.747 [DOI] [PubMed] [Google Scholar]
- Iwamasa GY, Sorocco KH, & Koonce DA (2002). Ethnicity and clinical psychology: a content analysis of the literature. Clin Psychol Rev, 22(6), 931–944. 10.1016/s0272-7358(02)00147-2 [DOI] [PubMed] [Google Scholar]
- Jackson SD, Mohr JJ, & Kindahl AM (2021). Intersectional experiences: A mixed methods experience sampling approach to studying an elusive phenomenon. Journal of Counseling Psychology, 68(3), 299–315. 10.1037/cou0000537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson SD, Mohr JJ, Sarno EL, Kindahl AM, & Jones IL (2020). Intersectional experiences, stigma-related stress, and psychological health among Black LGBQ individuals. J Consult Clin Psychol, 88(5), 416–428. 10.1037/ccp0000489 [DOI] [PubMed] [Google Scholar]
- Jackson SD, Wagner KR, Yepes M, Harvey TD, Higginbottom J, & Pachankis JE (2022). A pilot test of a treatment to address intersectional stigma, mental health, and HIV risk among gay and bisexual men of color. Psychotherapy (Chic), 59(1), 96–112. 10.1037/pst0000417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamb ML, Fishbein M, Douglas J, John M, Rhodes F, Rogers J, Bolan G, Zenilman J, Hoxworth T, Malotte CK, Iatesta M, Kent C, Lentz A, Graziano S, Byers RH, Peterman TA, & Group, f. t. P. R. S. (1998). Efficacy of Risk-Reduction Counseling to Prevent Human Immunodeficiency Virus and Sexually Transmitted DiseasesA Randomized Controlled Trial. JAMA, 280(13), 1161–1167. 10.1001/jama.280.13.1161 [DOI] [PubMed] [Google Scholar]
- Keefe JR, Chambless DL, Barber JP, & Milrod BL (2021). Predictors and moderators of treatment dropout in cognitive-behavioral and psychodynamic therapies for panic disorder. Psychotherapy Research, 31(4), 432–442. 10.1080/10503307.2020.1784487 [DOI] [PubMed] [Google Scholar]
- Keefe JR, Kim TT, DeRubeis RJ, Streiner DL, Links PS, & McMain SF (2020). Treatment selection in borderline personality disorder between dialectical behavior therapy and psychodynamic psychiatric management. Psychological Medicine, 1–9. 10.1017/S0033291720000550 [DOI] [PubMed] [Google Scholar]
- Kiluk BD, Dreifuss JA, Weiss RD, Morgenstern J, & Carroll KM (2013). The Short Inventory of Problems – revised (SIP-R): psychometric properties within a large, diverse sample of substance use disorder treatment seekers. Psychology of addictive behaviors : journal of the Society of Psychologists in Addictive Behaviors, 27(1), 307–314. 10.1037/a0028445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koblin B, Chesney M, & Coates T (2004). Effects of a behavioural intervention to reduce acquisition of HIV infection among men who have sex with men: the EXPLORE randomised controlled study. Lancet, 364(9428), 41–50. 10.1016/s0140-6736(04)16588-4 [DOI] [PubMed] [Google Scholar]
- Larson DG, & Chastain RL (1990). Self-concealment: Conceptualization, measurement, and health implications. Journal of Social and Clinical Psychology, 9(4), 439–455. 10.1521/jscp.1990.9.4.439 [DOI] [Google Scholar]
- Laska KM, Gurman AS, & Wampold BE (2014). Expanding the lens of evidence-based practice in psychotherapy: A common factors perspective. Psychotherapy, 51(4), 467–481. 10.1037/a0034332 [DOI] [PubMed] [Google Scholar]
- Lebowitz MS, & Ahn WK (2015). Emphasizing Malleability in the biology of depression: Durable effects on perceived agency and prognostic pessimism. Behav Res Ther, 71, 125–130. 10.1016/j.brat.2015.06.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lemmens L, van Bronswijk SC, Peeters F, Arntz A, Roefs A, Hollon SD, DeRubeis RJ, & Huibers MJH (2020). Interpersonal Psychotherapy Versus Cognitive Therapy for Depression: How They Work, How Long, and for Whom-Key Findings From an RCT. Am J Psychother, 73(1), 8–14. 10.1176/appi.psychotherapy.20190030 [DOI] [PubMed] [Google Scholar]
- Lorenzo-Luaces L, DeRubeis RJ, van Straten A, & Tiemens B (2017). A prognostic index (PI) as a moderator of outcomes in the treatment of depression: A proof of concept combining multiple variables to inform risk-stratified stepped care models. Journal of Affective Disorders, 213, 78–85. 10.1016/j.jad.2017.02.010 [DOI] [PubMed] [Google Scholar]
- Luedtke A, Sadikova E, & Kessler RC (2019). Sample Size Requirements for Multivariate Models to Predict Between-Patient Differences in Best Treatments of Major Depressive Disorder. Clinical Psychological Science, 7(3), 445–461. 10.1177/2167702618815466 [DOI] [Google Scholar]
- Millar BM, Wang K, & Pachankis JE (2016). The moderating role of internalized homonegativity on the efficacy of LGB-affirmative psychotherapy: Results from a randomized controlled trial with young adult gay and bisexual men. Journal of Consulting and Clinical Psychology, 84(7), 565–570. 10.1037/ccp0000113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohr JJ, & Kendra MS (2011). Revision and extension of a multidimensional measure of sexual minority identity: The Lesbian, Gay, and Bisexual Identity Scale. Journal of Counseling Psychology, 58(2), 234–245. 10.1037/a0022858 [DOI] [PubMed] [Google Scholar]
- Murphy ST, Cooper AA, Hollars SN, & Strunk DR (2021). Who Benefits From a Cognitive vs. Behavioral Approach to Treating Depression? A Pilot Study of Prescriptive Predictors. Behavior Therapy, 52(6), 1433–1448. 10.1016/j.beth.2021.03.012 [DOI] [PubMed] [Google Scholar]
- Nagendra A, Orleans-Pobee M, Spahnn R, Monette M, Sosoo EE, Pinkham AE, & Penn DL (2020). How often do US-based schizophrenia papers published in high-impact psychiatric journals report on race and ethnicity?: A 20-year update of Lewine and Caudle (1999). Journal of Mental Health, 1–8. 10.1080/09638237.2020.1837356 [DOI] [PubMed] [Google Scholar]
- Pachankis JE (2014). Uncovering Clinical Principles and Techniques to Address Minority Stress, Mental Health, and Related Health Risks Among Gay and Bisexual Men. Clin Psychol (New York), 21(4), 313–330. 10.1111/cpsp.12078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pachankis JE (2018). The scientific pursuit of sexual and gender minority mental health treatments: Toward evidence-based affirmative practice. American Psychologist, 73(9), 1207–1219. 10.1037/amp0000357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pachankis JE, McConocha EM, Clark KA, Wang K, Behari K, Fetzner BK, Brisbin CD, Scheer JR, & Lehavot K (2020a). A transdiagnostic minority stress intervention for gender diverse sexual minority women’s depression, anxiety, and unhealthy alcohol use: A randomized controlled trial. Journal of Consulting and Clinical Psychology, 88(7), 613–630. 10.1037/ccp0000508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pachankis JE, Clark KA, Burton CL, Hughto JMW, Bränström R, & Keene DE (2020b). Sex, status, competition, and exclusion: Intraminority stress from within the gay community and gay and bisexual men’s mental health. J Pers Soc Psychol, 119(3), 713–740. 10.1037/pspp0000282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pachankis JE, Goldfried MR, & Ramrattan ME (2008). Extension of the rejection sensitivity construct to the interpersonal functioning of gay men. J Consult Clin Psychol, 76(2), 306–317. 10.1037/0022-006x.76.2.306 [DOI] [PubMed] [Google Scholar]
- Pachankis JE, Harkness A, Maciejewski KR, Behari K, Clark KA, McConocha E, Winston R, Adeyinka O, Reynolds J, Bränström R, Esserman DA, Hatzenbuehler ML, & Safren SA (2022a). LGBQ-affirmative cognitive-behavioral therapy for young gay and bisexual men’s mental and sexual health: A three-arm randomized controlled trial. Journal of Consulting and Clinical Psychology, 90, 459–477. 10.1037/ccp0000724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pachankis JE, Hatzenbuehler ML, Rendina HJ, Safren SA, & Parsons JT (2015). LGB-affirmative cognitive-behavioral therapy for young adult gay and bisexual men: A randomized controlled trial of a transdiagnostic minority stress approach. J Consult Clin Psychol, 83(5), 875–889. 10.1037/ccp0000037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pachankis JE, McConocha EM, Reynolds JS, Winston R, Adeyinka O, Harkness A, Burton CL, Behari K, Sullivan TJ, Eldahan AI, Esserman DA, Hatzenbuehler ML, & Safren SA (2019). Project ESTEEM protocol: a randomized controlled trial of an LGBTQ-affirmative treatment for young adult sexual minority men’s mental and sexual health. BMC Public Health, 19(1), 1086. 10.1186/s12889-019-7346-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pachankis JE, Soulliard ZA, Morris F, & Seager van Dyk I (2022b). A Model for Adapting Evidence-Based Interventions to Be LGBQ-Affirmative: Putting Minority Stress Principles and Case Conceptualization Into Clinical Research and Practice. Cognitive and Behavioral Practice. 10.1016/j.cbpra.2021.11.005 [DOI] [Google Scholar]
- Perez-Aquino P, Bean R, Steffen P, & Banford Witting A (2020). A Content Analysis of Ethnic Minorities in the Professional Discipline of Clinical Psychology Bringham Young University; ]. [Google Scholar]
- Pinel EC (1999). Stigma consciousness: the psychological legacy of social stereotypes. J Pers Soc Psychol, 76(1), 114–128. 10.1037//0022-3514.76.1.114 [DOI] [PubMed] [Google Scholar]
- Quinn DM, & Chaudoir SR (2009). Living with a concealable stigmatized identity: the impact of anticipated stigma, centrality, salience, and cultural stigma on psychological distress and health. J Pers Soc Psychol, 97(4), 634–651. 10.1037/a0015815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team. (2021). R: A language and environment for statistical computing. In (Version 4.0.4) R Foundation for Statistical Computing. https://www.R-project.org/ [Google Scholar]
- Rizopoulos D (2009). bootStepAIC: Bootstrap stepAIC. In (Version 1.2–0) https://cran.r-project.org/web/packages/bootStepAIC/index.html [Google Scholar]
- Sauer-Zavala S, Fournier JC, Jarvi Steele S, Woods BK, Wang M, Farchione TJ, & Barlow DH (2020). Does the unified protocol really change neuroticism? Results from a randomized trial. Psychological Medicine, 51(14), 2378–2387. 10.1017/S0033291720000975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz B, Cohen ZD, Rubel JA, Zimmermann D, Wittmann WW, & Lutz W (2021). Personalized treatment selection in routine care: Integrating machine learning and statistical algorithms to recommend cognitive behavioral or psychodynamic therapy. Psychotherapy Research, 31(1), 33–51. 10.1080/10503307.2020.1769219 [DOI] [PubMed] [Google Scholar]
- Sobell LC, & Sobell MB (1992). Timeline follow-back: A technique for assessing self-reported alcohol consumption. In Measuring alcohol consumption: Psychosocial and biochemical methods. (pp. 41–72). Humana Press. 10.1007/978-1-4612-0357-5_3 [DOI] [Google Scholar]
- Soto A, Smith TB, Griner D, Domenech Rodríguez M, & Bernal G (2018). Cultural adaptations and therapist multicultural competence: Two meta-analytic reviews. Journal of Clinical Psychology, 74(11), 1907–1923. 10.1002/jclp.22679 [DOI] [PubMed] [Google Scholar]
- Stekhoven DJ, & Bühlmann P (2011). MissForest—non-parametric missing value imputation for mixed-type data. Bioinformatics, 28(1), 112–118. 10.1093/bioinformatics/btr597 [DOI] [PubMed] [Google Scholar]
- Strobl C, Boulesteix A-L, Kneib T, Augustin T, & Zeileis A (2008). Conditional variable importance for random forests. BMC Bioinformatics, 9(1), 307. 10.1186/1471-2105-9-307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Spijker BAJ, Batterham PJ, Calear AL, Farrer L, Christensen H, Reynolds J, & Kerkhof AJFM (2014). The Suicidal Ideation Attributes Scale (SIDAS): Community-Based Validation Study of a New Scale for the Measurement of Suicidal Ideation. Suicide and Life-Threatening Behavior, 44(4), 408–419. 10.1111/sltb.12084 [DOI] [PubMed] [Google Scholar]
- van Bronswijk SC, DeRubeis RJ, Lemmens L, Peeters F, Keefe JR, Cohen ZD, & Huibers MJH (2021). Precision medicine for long-term depression outcomes using the Personalized Advantage Index approach: cognitive therapy or interpersonal psychotherapy? Psychol Med, 51(2), 279–289. 10.1017/s0033291719003192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vickers AJ, & Altman DG (2001). Analysing controlled trials with baseline and follow up measurements. BMJ, 323(7321), 1123–1124. 10.1136/bmj.323.7321.1123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wester RA, Rubel J, & Mayer A (2022). Covariate Selection for Estimating Individual Treatment Effects in Psychotherapy Research: A Simulation Study and Empirical Example. Clinical Psychological Science, 21677026211071043. 10.1177/21677026211071043 [DOI] [Google Scholar]
- Wilkins A (2012). “Not Out to Start a Revolution”: Race, Gender, and Emotional Restraint among Black University Men. Journal of Contemporary Ethnography, 41(1), 34–65. 10.1177/0891241611433053 [DOI] [Google Scholar]
- Windsor LC, Jemal A, & Alessi EJ (2015). Cognitive behavioral therapy: A meta-analysis of race and substance use outcomes. Cultural Diversity and Ethnic Minority Psychology, 21(2), 300–313. 10.1037/a0037929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilamowska ZA, Thompson-Hollands J, Fairholme CP, Ellard KK, Farchione TJ, & Barlow DH (2010). Conceptual background, development, and preliminary data from the unified protocol for transdiagnostic treatment of emotional disorders. Depress Anxiety, 27(10), 882–890. 10.1002/da.20735 [DOI] [PubMed] [Google Scholar]
- Williams DR (2018). Stress and the Mental Health of Populations of Color: Advancing Our Understanding of Race-related Stressors. Journal of Health and Social Behavior, 59(4), 466–485. 10.1177/0022146518814251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams JB, Kobak KA, Bech P, Engelhardt N, Evans K, Lipsitz J, Olin J, Pearson J, & Kalali A (2008). The GRID-HAMD: standardization of the Hamilton Depression Rating Scale. Int Clin Psychopharmacol, 23(3), 120–129. 10.1097/YIC.0b013e3282f948f5 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


