Abstract
Purpose:
To evaluate dry eyes in children with vernal kerato-conjunctivitis (VKC) and correlate it with symptoms, clinical findings, and ocular surface analysis (OSA) parameters.
Methods:
Children with clinically diagnosed VKC underwent complete ophthalmological examination, Schirmer’s testing, modified ocular surface disease index (OSDI) scoring, Bonini grading, fluorescein tear-film break-up time (TBUT), VKC – Collaborative Longitudinal Evaluation of Keratoconus (CLEK) scoring, and OSA. Children with a TBUT of < 10 s were defined to have dry eyes. The above-mentioned parameters were compared between dry eye and non-dry eye VKC children.
Results:
The mean age of the 87 children included in the study was 9.1 ± 2.9 years. Dry eyes were seen in 60.9% [95% confidence interval (CI); 51% to 71%]. The mean TBUT was 13.4 ± 3.8 and 5.9 ± 1.9 s in non-dry and dry eye groups, respectively (P < 0.001). The mean value of Schirmer’s test was 25.9 ± 9.8 and 20.8 ± 8.6 mm in the non-dry and dry eye groups, respectively (P = 0.01). The two groups did not differ in their OSDI scores, Bonini grading, and CLEK scores. The OSA parameter of non-invasive break-up time (NIBUT) was 8.3 ± 3.2 s in non-dry eye group and 6.4 ± 2.9 s in dry eye group, P = 0.008. The lower lid Meibomian gland (MG) loss was 7.4% in non-dry eye group and 12.2% in dry eye group, P = 0.028. Other OSA parameters did not differ significantly among the two groups.
Conclusion:
Dry eyes are seen in two-thirds of pediatric VKC. Evaluation of dry eyes should be incorporated in their clinical evaluation. Among OSA parameters, NIBUT and lower lid MG loss are associated with dry eyes in pediatric VKC patients.
Keywords: Ocular surface analyzer, pediatric dry eyes, vernal kerato-conjunctivitis
Vernal kerato-conjunctivitis (VKC) is a chronic allergic conjunctivitis (AC) in children presenting with itching, watering, foreign body sensation, papillary congestion, and corneal involvement. Dry eye disease (DED) is a multi-factorial ocular surface disease characterized by loss of tear-film homeostasis, in which ocular inflammation and damage and neurosensory abnormalities play etiological roles.[1] Traditionally, these two are regarded as different diseases, but dry eye remains an under-diagnosed complication of pediatric VKC patients.[2-5] Children often do not complain of the foreign body sensation and burning associated with dry eyes; thus, the routine clinical tests for dry eye diagnosis are seldom performed.[1,6] Fluorescein tear-film break-up time (TBUT) and Schirmer’s tests are invasive tests for dry eye evaluation and require children’s cooperation. Ocular surface analysis (OSA), being non-invasive, may be used as an alternative tool for dry eye evaluation in pediatric patients. There is scarcity of literature on the prevalence and clinical features of dry eyes in children with VKC.[1,3,7-9] This study aimed to evaluate dry eyes using clinical tests (fluorescein TBUT and Schirmer’s test) and OSA and to correlate with VKC symptom scores and clinical grading.
Methods
The study was a cross-sectional analysis of all VKC children who presented to our tertiary eye center from April 2019 to December 2021. It was approved by the Institutional Review Board (IRB/2019/MAR/17) and was conducted in adherence to the tenets of the Declaration of Helsinki.
The diagnosis of VKC was made based on the typical clinical features described in the literature.[10]
Inclusion criteria:
Children aged 5–15 years with VKC who presented to the out-patient department and cooperated for tests for dry eye.
Parental consent for clinical testing and ocular surface analyzer testing in the children.
Children who were already using medications for VKC were included, and the medications were noted.
Exclusion criteria:
History of any intra-ocular surgery, previous ocular trauma, cranial nerve V or VII injury, chemical injury, or thermal burn in the past.
Any eyelid abnormality except allergic papillae, for example, meibomitis, coloboma, ectropion, and entropion.
Same day instillation of lubricants, anti-allergic, steroids, or any other topical medications.
AC because of foreign bodies such as contact lenses, sutures, prostheses, and cyanoacrylate glue.
The data recorded included patient’s age, gender, duration of allergic symptoms, seasonal variability of the disease, the treatment history (type, frequency, and duration of topical or systemic medications), presence of any systemic allergy, best-corrected visual acuity (BCVA), and refractive error. The modified ocular surface disease index (OSDI) score was adapted from Moon et al.[11] Moon et al. had modified the OSDI score to use it in the pediatric population for assessment of dry eyes because of smartphone use. We replaced two questions in this score to make it suitable for VKC children [Appendix 1]. This modified OSDI score was used to score the symptoms and disease-related difficulties in daily living. The questionnaire was translated in the local language to be self-administered by the patients and their parents.
A protocol was developed for the evaluation of VKC children making sure that none of the tests performed affects the results of another one. First, the details of slit lamp evaluation were noted, specifically the extent and size of the conjunctival papillae in the limbal and upper palpebral conjunctiva (following eversion of upper lid), conjunctival congestion, ropy discharge, scarring, and Horner-Tranta’s dots. Thereafter, the OSA was performed by either of two trained optometrists. All contact procedures were deferred until the OSA was performed. The OSA indices (NIBUT, eye blink, lipid layer morphology, Meibomian gland loss, and tear meniscus height) were recorded.[12] The ocular surface was then stained using 2% sodium fluorescein (Fluorostrip®, Contacare Ophthalmics and Diagnostics, Vadodara, Gujarat, India). A single drop of normal saline was instilled over the fluorostrip. After the strip was completely saturated, excess fluid was shaken away. The strip was then tapped on to the lower tarsal conjunctiva after retracting the lower lid. The patient was then instructed to blink several times without squeezing to distribute the fluorescein. The presence of any positive conjunctival or corneal staining was noted.[13] The corneal fluorescein staining [VKC – Collaborative Longitudinal Evaluation of Keratoconus (VKC-CLEK) grading][14] was used to grade the epithelial damage. The score was considered mild if less than 3, moderate if equal to or more than 3 and less than 6, and severe if more than 6.[14] The Bonini scale was used for clinical classification of VKC.[15]
The tear film stability was measured using the fluorescein TBUT in all cooperative patients.[13] Within 10–30 s of the fluorescein instillation, the patient was asked to stare straight ahead without blinking until told otherwise and seen under the cobalt blue light at 10x slit-lamp magnification. A stopwatch was used to record the time between the last complete blink and the first appearance of growing micelles (dry spots).[13] The procedure was repeated three times for each eye tested, with results reported as the mean value of the three measurements. The fluorescein staining and TBUT tests were completed in one eye before repeating the process in the fellow eye. Schirmer’s test II was then conducted as per the DEWS protocol.[13] In this procedure, one end of the Schirmer’s strip (5 × 35 mm Whatman filter paper no. 41) was inserted over the lower lid margin, midway between the middle and outer third, in an anesthetized closed eye and read at 5 min. The intra-ocular pressure was measured using a non-contact tonometer (Nidek NT-510). Fundoscopy was performed toward the end of examination after dilating the pupils using age-appropriate cycloplegic drops.
Since evaporative loss is the main mechanism of dry eyes in allergic conjunctivitis, dry eye was defined as a TBUT < 10 s.[8,16] The parameters of the clinically worse eye were considered for analysis. The worse eye was determined by a higher Bonini grade. In patients with symmetric Bonini grade in the two eyes, the extent of papillary reaction was considered to determine the worse eye. In the rest of the patients with highly symmetrical involvement, the left eye was considered for analysis. All the patients were divided into two groups based on the TBUT in the worse eye:
Group 1: TBUT ≥10 s (non-dry eye).
Group 2: TBUT <10 sec (dry eye).
The age, gender, modified OSDI score, and various clinical and OSA parameters were compared between the two groups.
We performed TBUT and Schirmer’s testing in 30 children (5–15 years) without any history, symptoms, or signs of allergy or dry eye. These patients were those having well corrected refractive errors as their only ocular diagnosis. These patients served as control to compare the clinical tests of dry eye with the VKC patients.
Statistical analysis
The categorical variables were summarized by their percentages, and Mann–Whitney test was used for their analysis. The continuous variables were reported by their means and standard deviations and analyzed across the groups by Chi-square or Fishers’ exact tests. Receiver operating characteristic (ROC) curves were drawn to assess the diagnostic ability of various OSA parameters to predict dry eye conditions.
Results
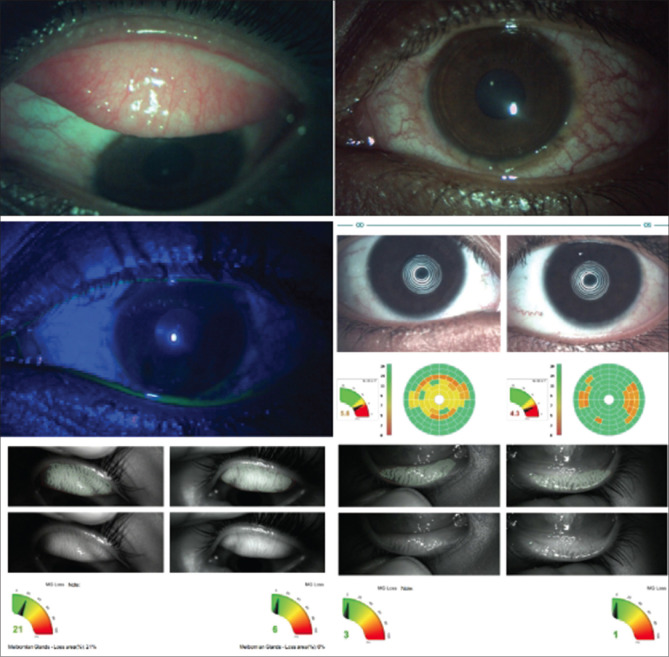
A total of 113 VKC children met the eligibility criteria in the study period. The mean age of patients was 9.27 years. There were 92 males and 21 females. Three children aged 6, 5, and 10 years did not cooperate for the TBUT. The mean TBUT was 8.3 s in RE and 8.9 s in LE in the rest of the 110 patients. Out of 110 patients, 87 patients underwent OSA, and their worse eye was included in the final analysis mentioned henceforth. Table 1 shows the comparison of the clinical tests of dry eye, OSDI scores, and demographic characteristics of 87 children with VKC and the 30 controls. Dry eyes with TBUT of <10 s were seen in 53/87 eyes (60.9%, 95% CI = 51–71%). No dry eye (TBUT ≥10 secs) was seen in the remaining 34 eyes (39.08%). Table 2 shows the demographic characteristics and clinical features of the two groups. Table 3 shows the results of the clinical tests (TBUT, Schirmer’s test, fluorescein staining, Bonini grading, and OSDI scores) and OSA parameters in the two groups. All parameters except for Schirmer’s test, mean NIBUT, and lower lid Meibomian gland loss (LL MG LOSS) showed an insignificant difference between the two groups. Fig. 1 shows the clinical photographs, TBUT, and OSA results of a child with VKC.
Table 1.
Comparison of the demographic characteristics, OSDI scores, and clinical tests of dry eye among VKC children and controls
| Parameter | VKC (n=87) | Control (n=30) | P |
|---|---|---|---|
| Age in years (Mean±SD) | 9.1±2.9 | 11.7±3 | 0.00* |
| Sex (Female: Male) | 5:24 | 14:69 | 0.00$ |
| TBUT in sec (Mean±SD) | 8.8±4.6 | 10.9±5 | 0.04* |
| Schirmer’s II in mm (Mean±SD) | 22.1±9.2 | 21.4±10 | 0.55* |
| OSDI Score (Mean±SD) | 32.7±17.6 | 14.9±11.5 | 0.00* |
*Mann–Whitney, $Chi square test
Table 2.
Comparison of the demographics, symptoms and signs between the non-dry eye and dry eye groups in children with VKC
| Group 1 (non-dry eye) (n=34) | Group II (dry eye) (n=53) | Total | P | |
|---|---|---|---|---|
| Age (years±SD) | 9.1±2.9 | 9.12±2.9 | 9.11±2.94 | 0.92* |
| Sex | ||||
| F | 6 (17.7%) | 9 (17%) | 15 (17.25) | 1.00# |
| M | 28 (82.4%) | 44 (83%) | 72 (82.8%) | |
| Mean duration of symptoms (months) | 25.8±20.9 | 27.7±30.8 | 26.9±27.20 | 0.8* |
| Symptoms | ||||
| Itching | 33 (97.1%) | 53 (100%) | 86 (98%) | 0.89# |
| Redness | 29 (85.3%) | 47 (88.7%) | 76 (87.4%) | 0.73# |
| Burning | 13 (38.2%) | 22 (41.5%) | 35 (40.2%) | 0.84# |
| Discharge | 8 (23.5%) | 14 (26.4%) | 22 (25.3%) | 0.81# |
| Photophobia | 4 (11.8%) | 16 (30.2%) | 20 (22.9%) | 0.07# |
| Type of Allergy | ||||
| Perennial | 14 (42.4%) | 20 (39.2%) | 34 (40.5%) | 0.82# |
| Seasonal | 19 (57.6%) | 31 (60.8%) | 50 (59.5%) | |
| Presence of Atopy | 5 (14.7%) | 8 (15.4%) | 13 (15.1%) | 1.0# |
| Current treatment | 17 (50.0%) | 25 (47.2%) | 42 (48.3%) | 0.83# |
| Topical steroids | 8 (23.5%) | 14 (26.4%) | 22 (25.3%) | 0.81# |
| Antihistamines | 14 (41.2%) | 19 (35.9%) | 33 (37.9%) | 0.66# |
| Lubricants | 13 (38.2%) | 21 (39.6%) | 34 (39.1) | 1.0 # |
| Topical Immunomodulators | 1 (2.9%) | 2 (3.8%) | 3 (3.5%) | 1.0 # |
| Systemic Antiallergics | 1 (2.9%) | 2 (3.8%) | 3 (3.5%) | 1.0 # |
| Visual Acuity | 6/6 | 6/6 | ||
| Conjunctival congestion | 21 (61.8%) | 31 (58.5%) | 52 (59.8%) | 0.82# |
| Lid Papillae[17] | 34 (100%) | 53 (100%) | 87 (100%) | 0.09# |
| Mild (<0.2 mm) | 23 (67.7%) | 36 (67.9) | 59 (67.8) | |
| Moderate (0.3 to 1 mm) | 10 (29.4%) | 9 (16.9%) | 19 (21.8%) | |
| Giant (>1 mm) | 1 (2.9%) | 8 (15.1%) | 9 (10.3%) | |
| Conjunctival scarring | 0 (0.0%) | 2 (3.8%) | 2 (2.4%) | 0.52 # |
| Blepharitis | 3 (9.1%) | 2 (3.8%) | 5 (5.8%) | 0.37# |
| Limbal papillae (clock hrs) | ||||
| <3 | 8 (23.5%) | 14 (26.4%) | 22 (25.3%) | 0.33# |
| 3-6 | 10 (29.4%) | 9 (16.9%) | 19 (21.8%) | |
| 6-9 | 4 (11.8%) | 6 (11.3%) | 10 (11.5%) | |
| >9 | 3 (8.8%) | 13 (24.5%) | 16 (18.4%) | |
| Type of VKC | ||||
| Limbal | 0 | 3 (5.7%) | 3 (3.5%) | 0.23# |
| Palpebral | 16 (47.1%) | 18 (33.9%) | 34 (39.1%) | |
| Mixed | 18 (52.9%) | 32 (60.4%) | 50 (57.5%) |
*Mann–Whitney test, #Fisher’s exact test
Table 3.
Comparison of the clinical parameters and invasive and non-invasive (OSA) tests of dry eye among the non-dry eye and dry eye groups of the children with VKC
| Group 1 (non-dry eye) (n=34) | Group II (dry eye) (n=53) | Total | Statistical test (P) | |
|---|---|---|---|---|
| MEAN TBUT (sec) | 13.4±3.8 | 5.9±1.9 | 8.8±4.6 | 0.00* |
| Schirmer’s (mm) | 25.9±9.8 | 20.8±8.6 | 22.8±9.4 | 0.01* |
| BONINI GRADING | ||||
| 0 | 0 | 1 (1.9%) | 1 (1.9%) | 0.4# |
| 1 | 11 (32.4%) | 11 (20.8%) | 22 (25.3%) | |
| 2A | 6 (17.7%) | 17 (32.1%) | 23 (26.4%) | |
| 2B | 9 (26.5%) | 10 (18.9%) | 19 (21.8%) | |
| 3 | 8 (25.5%) | 14 (26.4%) | 22 (25.3%) | |
| CLEK SCORING | 0.4# | |||
| Mild (0-<3) | 28 (82.4%) | 37 (69.8%) | 65 (74.7%) | |
| Moderate (3-<6) | 6 (17.7%) | 15 (28.3%) | 21 (24.1%) | |
| Severe (6 or more) | 0 | 1 (1.9%) | 1 (1.2%) | |
| MEAN OSDI SCORE | ||||
| OSDI A | 12.3±5.9 | 12.9±6.7 | 12.7±6.4 | 0.6* |
| OSDI B | 4.2±3.8 | 3.6±3.2 | 3.8±3.4 | 0.6* |
| OSDI C | 2.1±2.6 | 2.6±2.9 | 2.4±2.8 | 0.4* |
| TOTAL (% score) | 32.2±14.4 | 33.0±19.6 | 32.7±17.6 | 0.9* |
| OSA PARAMETERS | ||||
| NIBUT | 8.3±3.2 | 6.5±2.9 | 7.2±3.1 | 0.008* |
| UL MG Loss | 16.8±10.9 | 16.3±9.3 | 16.5±9.9 | 0.8* |
| LL MG Loss | 7.4±8.2 | 12.2±11.5 | 10.4±10.6 | 0.05* |
| Blink | 81.6±18.7 | 75.8±20.0 | 77.9±19.6 | 0.3* |
| Tear Meniscus | 0.12±0.04 | 0.12±0.05 | 0.12±0.05 | 0.4* |
| Lipid layer thickness | ||||
| <15 nm | 2 (5.9%) | 6 (11.3%) | 8 (9.2) | 0.2# |
| ~15 nm | 21 (61.8%) | 34 (64.2%) | 55 (63.2%) | |
| ~30 nm | 6 (17.7%) | 12 (22.6%) | 18 (20.7%) | |
| ~30-80 | 1 (2.9%) | 0 | 1 (1.2%) | |
| 80 nm | 4 (11.8%) | 1 (1.9%) | 5 (5.8%) | |
| LIPID LAYER NATURE | ||||
| NONE | 1 (2.9%) | 5 (9.4%) | 6 (6.9%) | 0.2# |
| AMORPHOUS | 4 (11.8) | 1 (1.9%) | 5 (5.8%) | |
| OPEN | 23 (67.7%) | 35 (66%) | 58 (66.7%) | |
| CLOSE | 6 (17.7%) | 12 (22.6%) | 18 (20.7%) |
*Mann–Whitney, #Fisher’s
Figure 1.
The clinical photograph, tear-film break-up time and OSA results of a child with VKC
Fig. 2 shows the ROC for detection of dry eyes with NIBUT and LL MG LOSS. Both NIBUT and LL MG LOSS seemed to have good diagnostic ability to predict dry eye conditions. The area under the ROC curve (AUC) was 0.669 for NIBUT and 0.627 for LL MG LOSS. A cut-off value of 10 s on the NIBUT scale would predict the dry eye condition with 67.8% accuracy [true positive rate (TPR) =90.6%, false positive rate (FPR) =67.6%]. The specificity increases considerably (85.3%) if the cut-off mark is decided based on the maximum value of the Yuden index (cut-off = 5.7 s). Similarly, the best cut-off mark for the LL MG LOSS parameter based on the highest accuracy (63.8%) is 3 with TPR = 77.1% and FPR = 60.0%. Based on the maximum value of the Yuden Index, the best cut-off for the LL MG LOSS parameter is 10% (specificity = 73.7%).
Figure 2.
ROC for detection of dry eyes with NIBUT and LL MG loss
Discussion: VKC is a chronic, bilateral disease which usually affects younger children, significantly affecting their quality of life and productivity.[18,19] According to a report, it is five times more likely to cause non-attendance of school during a 3-month period.[20] It affects males more than females.[9] In our study, the male: female (M: F) ratio was 4.4:1 (92 males and 21 females). There are enough scientific pieces of evidence that dry eye is associated with AC.[2-4,7,8,21] The mechanism of dry eye in AC is still unclear, and several theories have been proposed. First, the conjunctival epithelium and the goblet cells are destroyed by the inflammatory proteins released from the eosinophils, such as major basic protein, eosinophil core protein, epidermal growth factor, interleukin-1 (IL-1) and IL-8, histamine, and platelet-activation factors, resulting in reduction of mucin production and a subsequent decrease of the TBUT.[21,22] Second, the primary mucin glycosaminoglycan sialic acid may be qualitatively altered, compromising the production of hydrophilic surfaces and producing tear film instability.[23]
VKC causes tear film dysfunction, affecting its stability, corneal nerve function, and epithelial cell integrity, which usually persists through its quiescent phases (perineal), causing potential ocular surface damage and resultant dry eye.[23] Reduced TBUT has been reported in the literature in children with AC.[7,23] Our results also demonstrate a short TBUT (mean = 8.8 ± 4.6 s) in pediatric VKC patients as compared to the controls. Villani et al. did a cross-sectional study to evaluate TBUT in 35 active and 35 inactive VKC children < 16 years.[7] They found the mean TBUT to be 6.3 ± 2.6 s and 7.7 ± 2.6 s in active and inactive VKC, respectively, which was reduced when compared to the controls (13.4 ± 2.9 s). A reduced TBUT as compared to controls has been observed in other studies also;[2-4,8] however, they have included children with AC and not VKC per se. Kim et al. found a mean TBUT of 6.4 ± 1.7 s in children aged 6–15 years suffering from AC.[2] Dogru et al. showed unstable tear film in children with allergy (AC, allergic rhinitis and asthma) with a reduced TBUT (5.5 ± 4.4 s) as compared to controls (18.4 ± 2.9 s).[8] In a study from southwest China, Chen et al. found a mean TBUT of 6.5 ± 1.5 s in children with AC,[3] while Akil et al. found a mean TBUT of 11.3 ± 3.4 s from Turkey.[4] All these studies highlight the tear film instability in AC children and the need to include dry eye evaluation in the examination of such children.
To define dry eye, a reference value of <10 s was considered in our study in accordance with the DEWS II criteria. The percentage of children with AC conjunctivitis who have dry eyes varies in the literature from 12% to 97.5%.[3,4] In the current study, 60.9% of VKC children had dry eyes. Chen et al.[3] found dry eye in 97.5% of a sample of 40 children with AC aged 3–6 years using the same reference criteria. Akil et al. found dry eyes in 12% patients with AC.[4] In their study, the dry eyes were diagnosed based on TBUT ≤10 s, tear meniscus height reflex (TMH-R) measurement, and Schirmer’s test.
Chen et al.[3] found statistically significant correlation (r < 0.5) between tear film stability in young children and the duration of AC. Hom et al. in their study showed that the odds of having symptomatically red and dry eye are higher in patients with significant clinical itching.[24] However, we did not find any significant difference in the dry eye and non-dry eye groups in duration of symptoms and complaints of itching.
A greater number and extent of papillae indicate more severe VKC. More severe disease may result in more ocular surface remodeling, thereby causing more severe dry eye.[9] However, we did not find any significant differences in the two groups in the Bonini grading or CLEK scores. Villani et al. in their study showed that inactive VKC patients showed increased photophobia, conjunctival Lissamine Green staining, Schirmer test values, reduced TBUT, and corneal sensitivity compared with control subjects. This signifies that the changes induced in the corneal surface and nerves due to the chronic inflammation may persist despite quiescence.[7] This theory has been supported by in vivo studies by Leonardi et al.[25]
In our study, 48.3% patients were already on treatment with either one or more topical medications (steroid, anti-histaminic, lubricant, and immunomodulators) and systemic anti-allergics also. Despite treatment, 47.2% patients had dry eyes. This highlights the importance of dry eye assessment in patients of VKC irrespective of the treatment provided or disease severity. The mismatch between the signs and symptoms in some patients may be due to an unrecognized underlying dry eye. The presence of dry eye in an apparently inactive VKC may warrant a continuation of anti-inflammatory and lubricating eye drops.
The commonly used tests like TBUT and Schirmer’s, being invasive, are not easy to perform in children and can yield results that differ from the natural properties of the tear. The TBUT relies on subjective timing which may increase the inter-examiner variability. To overcome this, we used stopwatch for calculation of the time. The Schirmer test may cause reflex tearing, resulting in an overestimation of tear volume. To overcome these limitations, several non-invasive devices have been used in adults as well as children for the assessment of dry eye.[26] The ocular surface analyzer is one such non-invasive device which is a quick, accurate, easy-to-use[27] and user-independent way to assess dry eyes[12] and allows detailed structural evaluation tear film and its composition. It is based on the principle of interferometry and infrared meibography.[27] It also helps to identify the type of DED and determine which layers can be treated with a specific treatment, in relation to the type of deficiency.[28]
Recently, Sabu S et al. studied[9] dry eye in 68 VKC and 33 control children using the OSA (OCP SBM Sistemi, Turin, Italy) and found that NIBUT was lower in VKC group than in controls [6.8 ± 1.6 s vs 12.5 ± 0.8 s (P < 0.001)]. Dry eye (defined as OSDI ≥13 and NIBUT <10 s) was seen in 74% patients in their study. The average NIBUT was 7.2 ± 3.1 s in the current study in the VKC patients. Sabu et al. did not perform TBUT in their study and used OSDI as a criterion to determine dry eyes in children.[9] Studies have shown that the symptoms of VKC may not correlate with the signs.[29] This discrepancy is further exaggerated in children as they seldom report their problems accurately.[3,30] The OSDI is a self-reported questionnaire, and its reliability in determining the presence or absence of dry eye is doubtful in children.[30] We chose the OSDI questionnaire for scoring the symptoms from children because it is a widely used survey in dry eye.[11] However, we did not use the results of this survey to classify dry eye in our pediatric patients. Our analysis also failed to show any significant difference in the OSDI scores between the dry eye and non-dry eye groups (classified based on TBUT alone). The OSDI scores did not correlate with the severity of the VKC (Bonini grade) as well.
In the study by Sabu et al., the lipid layer thickness (LLT) was significantly thinner in the VKC group than in the control group and correlated negatively with the severity of the VKC (correlation coefficient = −0.324).[9] However, we did not find any such correlation. Rather, the LL MG loss was higher in the children with dry eye and VKC. Lipid layer interferometry patterns in the VKC group of their study included open patterns in 47.8%, close patterns in 42.7%, and wave patterns in 9.6%. In our study, we found open patterns in 66.7%, close patterns in 20.7%, and amorphous patterns in 5.8%. Further studies are carried out using OSA in children with larger samples.
One of the limitations of our study is that the use of digital devices was not studied as a factor. Excessive digital devices have been shown to predispose to dry eyes in children[11,31] and could have been a confounder in the study. It is difficult to clinically differentiate the mild form of VKC (Bonini grade 1) from simple seasonal allergic conjunctivitis. Thus, we may have included some cases with seasonal allergic conjunctivitis in our VKC cohort.
Conclusion
In conclusion, VKC is a common form of allergic conjunctivitis in pediatric population in this part of the world. Its chronicity may lead to irreversible ocular surface remodeling, leading to several blinding complications. The current study shows that tear film instability and dry eye were common in children with VKC. The symptoms, clinical signs, severity of VKC, and use of topical anti-allergics/steroids did not differ between those with and without dry eye. Among the OSA parameters, the NIBUT and LL MG loss showed an association with dry eye in children with VKC. We recommend that an assessment of dry eye should be performed in all children with VKC. There is a need to understand the effect of treatment of the underlying pathology to reverse or prevent the complications of tear film instability and corneal changes.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We are grateful to Mr. Bhupesh Chandra, B.Optom and Mr. Mukesh Kumar, B.Optom for performing the OSA in the patients included in this study.
Appendix 1
Modifications done in the modified OSDI scoring by Moon et al were as follows:
In Section A: Question no 5 and 9 (asking about the experience of poor vision and fatigue or headache uring the last week) was replaced with symptoms scoring for the presence of itching and discharge respectively.
Modified Ocular Surface Disease Index (OSDI) for children with VKC
1. Have you experienced any of the following during the last week?
| All of the time | Most of the time | Half of the time | Some of the time | None of the time | |
|---|---|---|---|---|---|
| Eyes that are sensitive to light? | 4 | 3 | 2 | 1 | 0 |
| Eyes that feel gritty? | 4 | 3 | 2 | 1 | 0 |
| Painful or sore eyes? | 4 | 3 | 2 | 1 | 0 |
| Blurred vision? | 4 | 3 | 2 | 1 | 0 |
| Itching? | 4 | 3 | 2 | 1 | 0 |
| Dryness? | 4 | 3 | 2 | 1 | 0 |
| Tearing? | 4 | 3 | 2 | 1 | 0 |
| Red eye or injection? | 4 | 3 | 2 | 1 | 0 |
| Discharge? | 4 | 3 | 2 | 1 | 0 |
Subtotal score for answers = (A)
2. Have problems with your eyes limited you in performing any of the following during the last week?
| All of the time | Most of the time | Half of the time | Some of the time | None of the time | N/A | |
|---|---|---|---|---|---|---|
| Reading? | 4 | 3 | 2 | 1 | 0 | N/A |
| Use smartphone? | 4 | 3 | 2 | 1 | 0 | N/A |
| Use computer? | 4 | 3 | 2 | 1 | 0 | N/A |
| Watching television? | 4 | 3 | 2 | 1 | 0 | N/A |
Subtotal score for answers = (B)
3. Have your eyes felt uncomfortable in any of the following situations during the last week?
| All of the time | Most of the time | Half of the time | Some of the time | None of the time | N/A | |
|---|---|---|---|---|---|---|
| Windy condition? | 4 | 3 | 2 | 1 | 0 | N/A |
| Areas with low humidity? | 4 | 3 | 2 | 1 | 0 | N/A |
| Areas that are air conditioned? | 4 | 3 | 2 | 1 | 0 | N/A |
Subtotal score for answers = (C)
Add subtotals A, B, and C to obtain D (D = sum of scores for all questions answered) = (D)
OSDI Score = (D) x 100 / (# of question answered) x 4 = ( )
References
- 1.Craig JP, Nichols KK, Akpek EK, Caffery B, Dua HS, Joo CK, et al. TFOSDEWS II definition and classification report. Ocul Surf. 2017;15:27683. doi: 10.1016/j.jtos.2017.05.008. [DOI] [PubMed] [Google Scholar]
- 2.Kim TH, Moon NJ. Clinical correlations of dry eye syndrome and allergic conjunctivitis in Korean children. J Pediatr Ophthalmol Strabismus. 2013;50:124–7. doi: 10.3928/01913913-20130108-01. [DOI] [PubMed] [Google Scholar]
- 3.Chen L, Pi L, Fang J, Chen X, Ke N, Liu Q. High incidence of dry eye in young children with allergic conjunctivitis in Southwest China. Acta Ophthalmol. 2016;94:e727–30. doi: 10.1111/aos.13093. [DOI] [PubMed] [Google Scholar]
- 4.Akil H, Celik F, Ulas F, Kara IS. Dry eye syndrome and allergic conjunctivitis in the pediatric population. Middle East Afr J Ophthalmol. 2015;22:467–71. doi: 10.4103/0974-9233.167814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Villani E, Rabbiolo G, Nucci P. Ocular allergy as a risk factor for dry eye in adults and children. Curr Opin Allergy Clin Immunol. 2018;18:398–403. doi: 10.1097/ACI.0000000000000471. [DOI] [PubMed] [Google Scholar]
- 6.Alves M, Dias AC, Rocha EM. Dry eye in childhood: Epidemiological and clinical aspects. Ocul Surf. 2008;6:44–51. doi: 10.1016/s1542-0124(12)70104-0. [DOI] [PubMed] [Google Scholar]
- 7.Villani E, Dello Strologo M, Pichi F, Luccarelli SV, De Cillà S, Serafino M, et al. Dry eye in vernal keratoconjunctivitis: A cross-sectional comparative study. Medicine. 2015;94:e1648. doi: 10.1097/MD.0000000000001648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dogru M, Gunay M, Celik G, Aktas A. Evaluation of the tear film instability in children with allergic diseases. Cutan Ocul Toxicol. 2016;35:49–52. doi: 10.3109/15569527.2015.1010727. [DOI] [PubMed] [Google Scholar]
- 9.Sabu S, Gupta N, Raj N, Panigrahi A, Lomi N, Vanathi M, et al. Ocular surface characteristics in pediatric vernal keratoconjunctivitis: A clinico-cytological study. J AAPOS. 2022;26:240.e1–240.e6. doi: 10.1016/j.jaapos.2022.05.015. [DOI] [PubMed] [Google Scholar]
- 10.Leonardi A, Secchi AG. Vernal keratoconjunctivitis. Int Ophthalmol Clin. 2003;43:41–58. doi: 10.1097/00004397-200343010-00007. [DOI] [PubMed] [Google Scholar]
- 11.Moon JH, Kim KW, Moon NJ. Smartphone use is a risk factor for pediatric dry eye disease according to region and age: A case control study. BMC Ophthalmol. 2016;16:188. doi: 10.1186/s12886-016-0364-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Qi Y, Zhang C, Zhao S, Huang Y, Yang R. A novel noninvasive ocular surface analyzer for the assessment of dry eye with Meibomian gland dysfunction. Exp Ther Med. 2017;13:2983–8. doi: 10.3892/etm.2017.4364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Methodologies to diagnose and monitor dry eye disease: Report of the diagnostic methodology subcommittee of the International Dry Eye WorkShop. Ocul Surf. 2007;5:108–152. doi: 10.1016/s1542-0124(12)70083-6. [DOI] [PubMed] [Google Scholar]
- 14.Leonardi A, Lazzarini D, La Gloria Valerio A, Scalora T, Fregona I. Corneal staining patterns in vernal keratoconjunctivitis: the new VKC-CLEK scoring scale. Br J Ophthalmology. 2018;102:1448–1453. doi: 10.1136/bjophthalmol-2017-311171. [DOI] [PubMed] [Google Scholar]
- 15.Bonini S, Sacchetti M, Mantelli F, Lambiase A. Clinical grading of vernal keratoconjunctivitis. Curr Opin Allergy Clin Immunol. 2007;7:4364. doi: 10.1097/ACI.0b013e3282efb726. [DOI] [PubMed] [Google Scholar]
- 16.Wolffsohn JS, Arita R, Chalmers R, Djalilian A, Dogru M, Dumbleton K, et al. TFOS DEWS II diagnostic methodology report. Ocul Surf. 2017;15:539–74. doi: 10.1016/j.jtos.2017.05.001. [DOI] [PubMed] [Google Scholar]
- 17.Kosrirukvongs P, Visitsunthorn N, Vichyanond P, Bunnag C. Allergic conjunctivitis. Asian Pac J Allergy Immunol. 2001;19:237–44. [PubMed] [Google Scholar]
- 18.Vichyanond P, Pacharn P, Pleyer U, Leonardi A. Vernal keratoconjunctivitis: A severe allergic eye disease with remodeling changes. Pediatr Allergy Immunol. 2014;25:314–22. doi: 10.1111/pai.12197. [DOI] [PubMed] [Google Scholar]
- 19.Bielory L, Meltzer EO, Nichols KK, Melton R, Thomas RK, Bartlett JD. An algorithm for the management of allergic conjunctivitis. Allergy Asthma Proc. 2013;34:408–20. doi: 10.2500/aap.2013.34.3695. [DOI] [PubMed] [Google Scholar]
- 20.De Smedt SK, Nkurikiye J, Fonteyne YS, Tuft SJ, Gilbert CE, Kestelyn P. Vernal keratoconjunctivitis in school children in Rwanda: Clinical presentation, impact on school attendance, and access to medical care. Ophthalmology. 2012;119:1766–72. doi: 10.1016/j.ophtha.2012.03.041. [DOI] [PubMed] [Google Scholar]
- 21.Dogru M, Okada N, Asano-Kato N, Tanaka M, Igarashi A, Takano Y, et al. Atopic ocular surface disease: Implications on tear function and ocular surface mucins. Cornea. 2005;24(8 Suppl):S18–23. doi: 10.1097/01.ico.0000178741.14212.53. [DOI] [PubMed] [Google Scholar]
- 22.Pflugfelder SC, Jones D, Ji Z, Afonso A, Monroy D. Altered cytokine balance in the tear fluid and conjunctiva of patients with Sjögren's syndrome keratoconjunctivitis sicca. Curr Eye Res. 1999;19:201–11. doi: 10.1076/ceyr.19.3.201.5309. [DOI] [PubMed] [Google Scholar]
- 23.Toda, Ikuko, Shimazaki, Jun, Tsubota, Kazuo Dry eye with only decreased tear break-up time is sometimes associated with allergic conjunctivitis. Ophthalmology. 1995;102:302–9. doi: 10.1016/s0161-6420(95)31024-x. [DOI] [PubMed] [Google Scholar]
- 24.Hom MM, Nguyen AL, Bielory L. Allergic conjunctivitis and dry eye syndrome. Ann Allergy Asthma Immunol. 2012;108:163–6. doi: 10.1016/j.anai.2012.01.006. [DOI] [PubMed] [Google Scholar]
- 25.Leonardi A, Lazzarini D, Bortolotti M, Piliego F, Midena E, Fregona I. Corneal confocal microscopy in patients with vernal keratoconjunctivitis. Ophthalmology. 2012;119:509–15. doi: 10.1016/j.ophtha.2011.09.018. [DOI] [PubMed] [Google Scholar]
- 26.Bandlitz S, Peter B, Pflugi T, Jaeger K, Anwar A, Bikhu P, et al. Agreement and repeatability of four different devices to measure non-invasive tear breakup time (NIBUT) Cont Lens Anterior Eye. 2020;43:507–11. doi: 10.1016/j.clae.2020.02.018. [DOI] [PubMed] [Google Scholar]
- 27.Sánchez-González MC, Capote-Puente R, García-Romera M-C, De-Hita-Cantalejo C, Bautista-Llamas M-J, Silva-Viguera C, et al. Dry eye disease and tear film assessment through a novel non-invasive ocular surface analyzer: The OSA protocol. Front Med. 2022;9:938484. doi: 10.3389/fmed.2022.938484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.George RM, Mohan P. Ocular surface analyzer. Kerala J Ophthalmol. 2019;31:72–4. [Google Scholar]
- 29.Nichols KK, Nichols JJ, Mitchell GL. The lack of association between signs and symptoms in patients with dry eye disease. Cornea. 2004;23:762–70. doi: 10.1097/01.ico.0000133997.07144.9e. [DOI] [PubMed] [Google Scholar]
- 30.Han SB, Yang HK, Hyon JY, Hwang J. Children with dry eye type conditions may report less severe symptoms than adult patients. Graefes Arch Clin Exp Ophthalmol. 2013;251:791–6. doi: 10.1007/s00417-012-2097-2. [DOI] [PubMed] [Google Scholar]
- 31.Walsh JJ, Barnes JD, Tremblay MS, Chaput JP. Associations between duration and type of electronic screen use and cognition in US children. Comput Human Behav. 2020;108:106312. [Google Scholar]