Abstract
Objectives
To better define the spectrum of new-onset post-COVID-19 and post-COVID-19 vaccine inflammatory rheumatic diseases (IRD) from a large multicentric observational study.
Methods
Consecutive cases of IRD encountered during a 12-month period and satisfying one of the following inclusion criteria: (a) onset of the rheumatic manifestations within 4 weeks from SARS-CoV-2 infection or (b) onset of the rheumatic manifestations within 4 weeks from the administration of one of the COVID-19 vaccines ws recruited.
Results
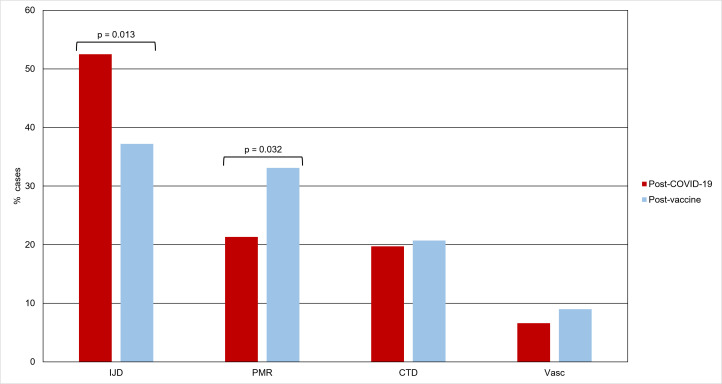
The final analysis cohort comprised 267 patients, of which 122 (45.2%) in the post-COVID-19 and 145 (54.8%) in the postvaccine cohort. Distribution of IRD categories differed between the two cohorts: the post-COVID-19 cohort had a higher percentage of patients classified as having inflammatory joint diseases (IJD, 52.5% vs 37.2%, p=0.013) while the post-vaccine cohort had a higher prevalence of patients classified as polymyalgia rheumatica (PMR, 33.1% vs 21.3%, p=0.032). No differences were detected in the percentage of patients diagnosed with connective tissue diseases (CTD 19.7% vs 20.7%, p=0.837) or vasculitis (6.6% vs 9.0%, p=0.467). Despite the short follow-up period, IJD and PMR patients’ response to first-line therapy was favourable, with both groups achieving a drop in baseline disease activity scores of ~30% and ~70% respectively.
Conclusion
Our article reports the largest cohort published to date of new-onset IRD following SARS-CoV-2 infection or COVID-19 vaccines. Although causality cannot be ascertained, the spectrum of possible clinical manifestations is broad and includes IJD, PMR, CTD and vasculitis.
Keywords: COVID-19, Arthritis, Polymyalgia Rheumatica, Vaccination, Autoimmune Diseases
WHAT IS ALREADY KNOWN ON THIS TOPIC
Since the beginning of the COVID-19 pandemic, isolated cases of inflammatory rheumatic diseases (IRD) with onset after SARS-CoV-2 infection or COVID-19 vaccine administration have been described by several groups. However, the anecdotical nature of the previous reports does not allow to catch the ‘big picture’ of the spectrum of IRD potentially associated with those exposures.
WHAT THIS STUDY ADDS
In this study, we collected a large cohort of IRD developed in close temporal association with SARS-CoV-2 infection or vaccine administration. According to our data, the spectrum of possible presentation is broad and includes inflammatory joint diseases (IJD), polymyalgia rheumatica (PMR), connective tissue diseases (CTD) and vasculitis with IJD prevailing in post-COVID-19 and PMR prevailing in postvaccine patients.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
Our study provides a broad, descriptive analysis of the possible array of IRD associated with SARS-CoV-2 infection and COVID-19 vaccines. This may contribute to strengthen the awareness on similar events—although uncommon—among physicians involved in musculoskeletal care and stimulate further research on this topic.
Introduction
Following the rapid spread of the COVID-19 pandemic, the scientific community demonstrated an unprecedented resilience to tackle an unknown biological threat, obtaining rapid progress in understanding the pathogenesis of the disease1 and the subsequent development of highly specific ‘countermeasures’ such as the novel mRNA vaccines2 and antiviral medications.3 This allowed to scale down the burden of the disease and save tens of millions of lives globally.4 Indeed, most European countries achieved large vaccine coverage and Italy, in particular, attained one of the most successful campaigns with more than 50 million of people (93% of the population >12 years) getting at least one dose.5
Since the beginning, it was evident that the profound interaction between SARS-CoV-2 and the host immune system1 drives the most severe acute manifestations of the disease (eg, acute respiratory distress syndrome and microvascular injury); on the other hand, in the subsequent phases, a long-term immune dysregulation was demonstrated in at least a proportion of patients6 that may bolster prolonged symptoms persisting for months or years after viral clearance.
Postacute COVID-19 syndrome (PACS)7 has now been defined as an extremely heterogeneous condition following COVID-19 and characterised by a multitude of signs and symptoms including complaints of rheumatological interest.8 Musculoskeletal pain, indeed, is reported in almost 10% of individuals infected by SARS-CoV-2 at some time during the first year after the infection8 and, as suggested in a previous study published by our group, most of these patients satisfy the classification criteria for fibromyalgia.9
Concurrently, a growing number of articles described new-onset serological evidence of autoimmunity10 11 or frank inflammatory rheumatic diseases (IRD)—including inflammatory joint diseases (IJD),12 polymyalgia rheumatica (PMR),13 connective tissue diseases (CTD)14 15 and vasculitis16—in close temporal association with SARS-CoV-2 infection. However, this was not surprising as the potential role of infections in triggering rheumatic diseases has been hypothesised since decades on the basis of preclinical studies17 and is clearly recapitulated by reactive arthritis18 or virally induced arthritis (eg, parvovirus B19 or hepatitis C virus (HCV)).19 On the other hand, it was previously speculated that also the exposure to vaccines may elicit autoimmunity.20 The controversial autoimmune/inflammatory syndrome induced by adjuvants (ASIA syndrome),21 in example, is believed to result from the exposure to common vaccine adjuvants. Also in this case, reports of IRD following vaccination with available anti-COVID-19 vaccines appeared in literature since the earliest phases of the vaccine campaign.22–25
On this background, aim of the present study was to contribute to the knowledge on the spectrum of new-onset post-COVID-19 and post-COVID-19 vaccine IRD with a descriptive and comparative analysis from a large multicentric observational study.
Methods
Study design and inclusion/exclusion criteria
The present study was conceived as an observational cohort study. To this purpose, we published a web-based data collection form and invited all members of the Italian COVID-19 and autoimmune systemic diseases (COVID-19 and ASD) collaborative research group26 to submit consecutive cases of IRD or acrosyndrome encountered during routine clinical practice from 1 November 2021 to 31 October 2022 (12 months) and satisfying one of the following inclusion criteria: (a) onset of the rheumatic manifestations within 4 weeks from SARS-CoV-2 infection, demonstrated by RT-PCR and/or antigenic nasopharyngeal swab or (b) onset of the rheumatic manifestations within 4 weeks from the administration of one of the COVID-19 vaccines approved for administration in Italy (BNT162b2—Pfizer/BioNTech), mRNA-1273 (Moderna) during the collection period. Exclusion criteria were predefined as a past history of IRD or acrosyndrome or a diagnosis of PACS or ‘long-COVID’.
The COVID-19 and ASD group is a network of more than 40 physicians with senior experience in the management of patients with IRD, belonging to 11 public academic medical centres, 7 public general hospitals, 3 private academic medical centres and 2 private general hospitals, covering regions from northern to southern Italy and including rheumatologists, clinical immunologists and specialists in internal medicine.
Data were collected anonymously through an online form built using the Google Forms platform. Google Forms is a free and easy to use questionnaire administration tool that has been largely used in medical research.27 Cases submitted by individuals centres were assigned an alphanumeric identifier code, including a centre-specific string and a progressive patient number; before the analysis, records were manually checked for recognising potential duplicate entries (eg, identical demographic data and/or other variables despite different identifier code).
Information gathered included demographic characteristics, past exposure to SARS-CoV-2 infection, vaccine status, clinical features of rheumatological interest, autoantibodies status, erythrocyte sedimentation rate (ESR), C reactive protein (CRP), final diagnosis of the rheumatologist, first-line treatment.
For patients classified as having arthritis, disease activity before and after at least 4 weeks of treatment was recorded using the disease activity score including 28 joints (DAS28).28 For patients classified as having PMR, disease activity before and after at least 4 weeks of treatment was recorded using the PMR activity score (PMR-AS) as previously published.29
The research was conducted in compliance with the Declaration of Helsinki and its latest amendments30 and approved by a central Ethics Committee (Comitato Etico Azienda Sanitaria Locale 1 Avezzano/Sulmona/L’Aquila, L’Aquila, Italy; approval number: 0204194/22). Written informed consent was obtained from all study subjects.
Statistical analysis
Data are expressed as mean±SD, median (25th–75th percentile) or number (percentage) as appropriate. Student’s t test was used to compare differences in normally distributed continuous variables between the two groups; highly skewed variables were ln-transformed before the analysis. Fisher’s exact test was used to compare categorical variables. A p value <0.05 was considered statistically significant. All analyses were performed using the SPSS software V.26.0 (IBM, Armonk, New York).
Results
Clinical features of the overall study population
A total of 270 cases were entered in the database. Three records were excluded because identified as mechanical pain related to osteoarthritis (n=1) or fibromyalgia (n=2). No duplicate records were identified. The final analysis cohort comprised a total of 267 patients, of which 122 (45.2%) patients in the post-COVID-19 (age 54±17 years, 69.7% female subjects) and 145 (54.8%) patients (age 58±16 years, 66.2% female subjects) in the postvaccine cohort. Number of vaccine doses received did not differ between post-COVID-19 and postvaccine patients (2±1 vs 3±1, p=0.123).
In the post-COVID-19 cohort, four (3.3%) patients experienced asymptomatic infection, 104 (85.2%) had mildly symptomatic disease, while 14 (11.5%) had severe disease according to the WHO severity classification.31 Accordingly, 113 patients (92.6%) were treated at home and only 9 (7.4%) were hospitalised; of these, only one required subsequent admission to intensive care unit.
In the postvaccine cohort, most cases occurred after the booster (third) dose (n=66, 45.8%); the remaining were associated with a second dose (n=51, 35.4%), first dose (n=23, 16%) and only three (2.1%) after a fourth dose. In most cases, the specific vaccine associated with IRD onset was the Pfizer/BioNTech BNT162b2 (n=114, 78.6%) followed by Moderna mRNA-1273 (n=24, 16.6%), mirroring the overall distribution of COVID-19 vaccines dispensed in Italy.5 In seven (4.8%) patients, the specific vaccine was unknown. A total of 15 (10.3%) patients reported a history of asymptomatic or mildly symptomatic COVID-19 before the vaccine dose associated with IRD onset.
Mean delay between COVID-19 diagnosis or vaccine administration and rheumatic manifestations development was 14.5±7.8 vs 13.9±8.5 days, respectively (p=0.59).
Distribution of various IRD categories differed between the two cohorts (figure 1): the post-COVID-19 cohort had a higher percentage of patients classified as having IJD (52.5% vs 37.2%, p=0.013), while the postvaccine cohort had a higher prevalence of patients classified as PMR (33.1% vs 21.3%, p=0.032). No differences were detected in the percentage of patients diagnosed with CTD (post-COVID-19: 19.7% vs postvaccine: 20.7%, p=0.837) or vasculitis (post-COVID-19: 6.6% vs postvaccine: 9.0%, p=0.467).
Figure 1.
Relative frequencies of inflammatory rheumatic diseases categories in the two study cohorts. CTD, connective tissue diseases; IJD, inflammatory joint diseases; PMR, polymyalgia rheumatica; Vasc, vasculitis.
Inflammatory joint diseases
The most represented IRD category in both groups was IJD. The range of specific IJD was broad (table 1), with peripheral spondyloarthritis (pSpA), representing the most frequent final diagnosis. Although IJDs were relatively more frequent in post-COVID-19 patients, a significantly higher proportion of patients in the post-vaccine group was diagnosed as having PsA (29.6% vs 12.5%, p=0.021), while no significant differences were observed in other domains, including baseline inflammatory markers, disease activity, follow-up duration and first-line treatment used. The two patients in the post-COVID-19 vaccine cohort classified as having adult-onset Still’s disease (AOSD) were included as part of the IJD subgroup because of a predominantly articular clinical picture. Notably, despite the short follow-up, patients’ response to first-line therapy was favourable, with both groups achieving a 30% drop from baseline in disease activity, as measured by DAS28-CRP.
Table 1.
Comparative analysis of clinical features in inflammatory joint diseases with onset after SARS-CoV-2 infection or COVID-19 vaccine administration
| Post-COVID-19 (n=64) |
Post-vaccine (n=54) |
P value | |
| Age, years | 49±14 | 51±13 | 0.277 |
| Female sex, n (%) | 47 (73.4) | 37 (68.5) | 0.557 |
| N° vaccine doses, n | 2±1 | 3±1 | 0.434 |
| ESR (baseline), mm/h | 32±22 | 36±25 | 0.364 |
| ESR (follow-up), mm/h | 19±12 | 20±14 | 0.689 |
| CRP (baseline), mg/dL | 1.29 (1.00–2.50) | 1.50 (0.56–2.50) | 0.639 |
| CRP (follow-up), mg/dL | 0.53 (0.40–0.90) | 0.50 (0.30–0.80) | 0.456 |
| TJC (baseline), n | 6±4 | 8±6 | 0.081 |
| TJC (follow-up), n | 3±3 | 3±4 | 0.895 |
| SJC (baseline), n | 2 (2–4) | 3 (2–4) | 0.754 |
| SJC (follow-up), n | 0 | 0 | 0.575 |
| DAS28-CRP (baseline), score | 4.3±1.0 | 4.4±1.1 | 0.501 |
| DAS28-CRP (follow-up), score | 3.0±1.0 | 3.1±1.1 | 0.887 |
| Average follow-up, weeks | 8 (6–12) | 8 (7–12) | 0.866 |
| Specific diseases | |||
| pSpA (other than PsA), n (%) | 32 (50.0) | 19 (35.2) | 0.106 |
| HLA-B27 present, n (%) | 8 (25) | 6 (31.6) | 0.748 |
| Enthesitis, n (%) | 4 (12.5) | 1 (5.3) | 0.401 |
| Dactylitis, n (%) | 3 (9.4) | 1 (5.3) | 0.597 |
| RA, n (%) | 19 (29.7) | 14 (25.9) | 0.650 |
| RF positive, n (%) | 11 (57.9) | 10 (71.4) | 0.486 |
| ACPA positive, n (%) | 10 (52.6) | 7 (50.0) | 1.000 |
| PsA, n (%) | 8 (12.5) | 16 (29.6) | 0.021 |
| Enthesitis, n (%) | 3 (37.5) | 8 (50.0) | 0.562 |
| Dactylitis, n (%) | 1 (12.5) | 4 (25.0) | 0.477 |
| AxSpA, n (%) | 5 (7.8) | 3 (5.6) | 0.627 |
| HLA-B27 present, n (%) | 3 (60.0) | 2 (66.7) | 1.000 |
| Enthesitis, n (%) | 1 (20.0) | 0 (0.0) | 0.408 |
| Dactylitis, n (%) | 0 (0.0) | 0 (0.0) | 1.000 |
| AOSD, n (%) | 0 (0.0) | 2 (3.7) | 0.120 |
| Treatment | |||
| Paracetamol, n (%) | 8 (12.5) | 13 (24.1) | 0.101 |
| NSAIDs, n (%) | 30 (46.9) | 22 (40.7) | 0.504 |
| GCs, n (%) | 33 (51.6) | 33 (61.1) | 0.298 |
| Intra-articular GCs, n (%) | 1 (1.6) | 3 (5.6) | 0.232 |
| Colchicine, n (%) | 2 (3.1) | 0 (0.0) | 0.190 |
| MTX, n (%) | 22 (34.4) | 22 (40.7) | 0.476 |
| SSZ, n (%) | 9 (14.1) | 3 (5.6) | 0.128 |
| HCQ, n (%) | 4 (6.3) | 5 (9.3) | 0.540 |
| TNFi, n (%) | 3 (4.7) | 0 (0.0) | 0.107 |
| ANR, n (%) | 0 (0.0) | 1 (1.9) | 0.274 |
ANR, anakinra; AOSD, adult-onset Still’s disease; AxSpA, axial spondyloarthritis; CRP, C reactive protein; DAS28, disease activity score including 28 joints; ESR, erythrocyte sedimentation rate; GCs, glucocorticoids; HCQ, hydroxychloroquine; MTX, methotrexate; NSAIDs, non-steroidal anti-inflammatory drugs; PsA, psoriatic arthritis; pSpA, peripheral spondyloarthritis; RA, rheumatoid arthritis; SJC, swollen joint count; TJC, tender joint count; TNFi, TNF inhibitors.
Polymyalgia rheumatica
PMR was the second most common IRD category (table 2). None of the patients had clinical features reminiscent of concurrent giant cell arteritis (GCA) or required second-level imaging for suspected GCA on the basis of clinical judgement; those patients with prominent symptoms and/or supporting imaging suggestive of GCA with or without associated PMR are reported in the vasculitis subgroup.
Table 2.
Comparative analysis of clinical features in polymyalgia rheumatica with onset after SARS-CoV-2 infection or COVID-19 vaccine administration
| Post-COVID-19 (n=28) |
Post-vaccine (n=46) |
P value | |
| Age, years | 58±20 | 62±17 | 0.632 |
| Female sex, n (%) | 5 (62.5) | 9 (69.2) | 0.751 |
| N° vaccine doses, n | 2±1 | 2±1 | 0.739 |
| ESR (baseline), mm/h | 50±22 | 59±32 | 0.150 |
| ESR (follow-up), mm/h | 22±18 | 22±15 | 0.954 |
| CRP (baseline), mg/dL | 2.15 (1.46–4.10) | 1.99 (1.62–3.09) | 0.630 |
| CRP (follow-up), mg/dL | 0.60 (0.50–1.00) | 0.50 (0.50–0.95) | 0.910 |
| PMR-AS (baseline), score | 28.3 (25.2–33.0) | 24.8 (23.7–27.5) | 0.392 |
| PMR-AS (follow-up), score | 8.44 (5.4–10.0) | 6.43 (4.6–7.0) | 0.268 |
| Average follow-up, weeks | 8±5 | 14±13 | 0.004 |
| Treatment | |||
| Paracetamol, n (%) | 1 (3.6) | 4 (8.7) | 0.666 |
| NSAIDs, n (%) | 2 (7.1) | 7 (15.2) | 0.303 |
| GCs, n (%) | 28 (100.0) | 43 (93.5) | 0.168 |
| MTX, n (%) | 2 (7.1) | 9 (19.6) | 0.145 |
CRP, C reactive protein; ESR, erythrocyte sedimentation rate; GCs, glucocorticoids; MTX, methotrexate; NSAIDs, non-steroidal anti-inflammatory drugs; PMR-AS, polymyalgia rheumatica—activity score.
No significant differences were observed between post-COVID-19 and postvaccine PMR patients, except for a shorter duration of follow-up in the post-COVID-19 patients (8±5 vs 14±13 weeks, p=0.004). Despite this, the patients responded well to first-line therapy, with reductions in PMR-AS of 70% and 74% from baseline, respectively. Of note, six patients in the postvaccine and one in the post-COVID-19 cohort were aged below 50 years (range: 33–48). However, all patients had increased CRP (range: 1.15–5.4 mg/dL) and/or ESR levels (range: 20–110 mm/hour), a clear PMR-like clinical presentation, and steroid responsiveness (overall PMR-AS: baseline 23.5±2.3 vs follow-up 7.7±2.8) and thus were attributed to the PMR subgroup by the treating rheumatologist.
Connective tissue diseases
CTDs were also frequently reported. The range of specific CTD presentation was broad (table 3) and included undifferentiated CTD, systemic sclerosis, idiopathic inflammatory myopathies, amyopathic dermatomyositis, systemic lupus erythematosus, mixed CTD, Sjogren’s syndrome and isolated new-onset acrosyndrome. Notably, when comparing the two cohorts, the only variable reaching statistical significance was the prevalence of acrosyndrome, which was greater in post-COVID-19 group (20.8 vs 3.3%, p=0.02). No information on the follow-up of CTD patients was collected due to the high heterogeneity between outcome measures in such a mixed category of patients.
Table 3.
Comparative analysis of clinical features in connective tissue diseases with onset after SARS-CoV-2 infection or COVID-19 vaccine administration
| Post-COVID-19 (n=24) | Post-vaccine (n=30) | P value | |
| Age, years | 47±18 | 55±19 | 0.134 |
| Female sex, n (%) | 19 (79.2) | 22 (73.3) | 0.618 |
| N° vaccine doses, n (%) | 2±1 | 3±1 | 0.263 |
| ANA positive, n (%) | 21 (87.5) | 28 (93.3) | 0.462 |
| >1:160, n (%) | 12 (57.1) | 16 (57.1) | 1.000 |
| >1:640, n (%) | 3 (14.3) | 5 (17.8) | 1.000 |
| ESR, mm/h | 19±16 | 28±22 | 0.728 |
| CRP, mg/dL | 0.75 (0.30–1.50) | 0.56 (0.20–2.50) | 0.551 |
| Specific diseases | |||
| UCTD, n (%) | 6 (25.0) | 11 (36.7) | 0.359 |
| Anti-SSA positive, n (%) | 0 (0.0) | 3 (27.3) | 0.159 |
| Anti-Scl-70 positive, n (%) | 2 (33.3) | 2 (18.2) | 0.482 |
| SSc, n (%) | 6 (25.0) | 6 (20.0) | 0.661 |
| Anti-Scl-70 positive, n (%) | 2 (33.3) | 2 (33.3) | 1.000 |
| ACA positive, n (%) | 3 (50.0) | 4 (66.7) | 0.558 |
| IIM, n (%) | 4 (16.7) | 6 (20.0) | 0.754 |
| Anti-Mi2 positive, n (%) | 1 (25.0) | 2 (33.3) | 0.778 |
| Anti-Pl7 positive, n (%) | 1 (25.0) | 0 (0.0) | 0.197 |
| Anti-TIF1-γ, n (%) | 0 (0.0) | 2 (33.3) | 0.197 |
| ADM, n (%) | 0 (0.0) | 2 (6.7) | 0.197 |
| Anti-Mi2 positive, n (%) | 0 (0.0) | 1 (50.0) | N/A* |
| Anti-MDA5 positive, n (%) | 0 (0.0) | 1 (50.0) | N/A* |
| SLE, n (%) | 2 (8.3) | 1 (3.3) | 0.425 |
| Anti-ds-DNA positive, n (%) | 1 (50.0) | 1 (100.0) | 0.386 |
| Anti-Sm positive, n (%) | 1 (50.0) | 0 (0.0) | 0.386 |
| MCTD, n (%) | 0 (0.0) | 3 (10.0) | 0.111 |
| Anti-RNP positive, n (%) | 0 (0.0) | 3 (100.0) | N/A* |
| SjS, n (%) | 1 (4.2) | 0 (0.0) | 0.259 |
| SSA positive, n (%) | 1 (100.0) | 0 (0.0) | N/A* |
| Isolated acrosyndrome, n (%) | 5 (20.8) | 1 (3.3) | 0.042 |
| Acrocyanosis, n (%) | 2 (40.0) | 0 (0.0) | 0.439 |
| Raynaud’s phenomenon, n (%) | 3 (60.0) | 1 (100.0) | 0.439 |
| Treatment | |||
| Paracetamol, n (%) | 7 (29.2) | 10 (33.3) | 0.743 |
| NSAIDs, n (%) | 5 (20.8) | 6 (20.0) | 0.940 |
| GCs, n (%) | 9 (37.5) | 17 (56.7) | 0.161 |
| Intra-articular GCs, n (%) | 2 (8.3) | 0 (0.0) | 0.107 |
| Colchicine, n (%) | 0 (0.0) | 3 (10.0) | 0.111 |
| MTX, n (%) | 3 (12.5) | 3 (10.0) | 0.771 |
| HCQ, n (%) | 4 (16.7) | 6 (20.0) | 0.754 |
| AZA, n (%) | 0 (0.0) | 2 (6.7) | 0.197 |
| MMF, n (%) | 1 (4.2) | 1 (3.3) | 0.872 |
| CYC, n (%) | 0 (0.0) | 1 (3.3) | 0.367 |
| IVIg, n (%) | 1 (4.2) | 1 (3.3) | 0.472 |
| CCBs, n (%) | 4 (16.7) | 2 (6.7) | 0.245 |
*Expected number in one category is equal to zero.
ACA, anti-centromere antibodies; ADM, amyopathic dermatomyositis; ANA, antinuclear antibodies; AZA, azathioprine; CCBs, calcium channel blockers; CRP, C reactive protein; CYC, cyclophosphamide; ESR, erythrocyte sedimentation rate; GCs, glucocorticoids; HCQ, hydroxychloroquine; IIM, idiopathic inflammatory myopathy; IVIg, intravenous immunoglobulin; MCTD, mixed connective tissue disease; MMF, mycophenolate mofetil; MTX, methotrexate; N/A, not applicable; NSAIDs, non-steroidal anti-inflammatory drugs; SjS, Sjögren’s syndrome; SLE, systemic lupus erythematosus; SSc, systemic sclerosis; UCTD, undifferentiated connective tissue disease.
Vasculitis
Vasculitis was the least common category in both groups. However, the range of specific presentation was broad (table 4) and included small-vessel vasculitis, large-vessel vasculitis, variable vessel vasculitis and isolated skin vasculitis. No significant differences were found when comparing post-COVID-19 and postvaccine patients. No information on the follow-up of vasculitis patients was collected due to the high heterogeneity between outcome measures in such a mixed category of patients.
Table 4.
Comparative analysis of clinical features in vasculitis with onset after SARS-CoV-2 infection or COVID-19 vaccine administration
| Post-COVID-19 (n=8) |
Post-vaccine (n=13) |
P value | |
| Age, years | 58±20 | 62±17 | 0.632 |
| Female sex, n (%) | 5 (62.5) | 9 (69.2) | 0.751 |
| N° vaccine doses, n | 2±1 | 2±1 | 0.739 |
| ANA positive, n (%) | 2 (25) | 4 (30.8) | 0.776 |
| ESR, mm/h | 42±33 | 67±46 | 0.162 |
| CRP, mg/dL | 3.57±2.80 | 5.48±5.89 | 0.329 |
| Specific diseases | |||
| Large vessel vasculitis, n (%) | 2 (25.0) | 3 (23.1) | 0.920 |
| C-GCA, n (%) | 1 (12.5) | 2 (15.4) | 0.854 |
| LV-GCA, n (%) | 1 (12.5) | 1 (7.7) | 0.716 |
| Small vessel vasculitis, n (%) | 3 (37.5) | 3 (23.1) | 0.477 |
| ANCA positive, n (%) | 2 (66.7) | 1 (33.3) | 0.414 |
| EGPA, n (%) | 2 (66.7) | 2 (66.7) | 1.000 |
| GPA, n (%) | 0 (0.0) | 1 (33.3) | 0.273 |
| MPA, n (%) | 1 (33.3) | 0 (0.0) | 0.273 |
| Variable vessel vasculitis, n (%) | 0 (0.0) | 1 (7.7) | 0.421 |
| BD, n (%) | 0 (0.0) | 1 (7.7) | N/A* |
| Skin vasculitis, n (%) | 3 (37.5) | 6 (46.2) | 0.697 |
| Palpable purpura, n (%) | 2 (66.7) | 6 (100.0) | 0.134 |
| Urticarial vasculitis, n (%) | 1 (33.3) | 0 (0.0) | 0.134 |
| Treatment | |||
| NSAIDs, n (%) | 1 (12.5) | 2 (15.4) | 0.854 |
| GCs, n (%) | 6 (75.0) | 12 (92.3) | 0.271 |
| Colchicine, n (%) | 0 (0.0) | 1 (7.7) | 0.421 |
| MTX, n (%) | 1 (12.5) | 0 (0.0) | 0.191 |
| SSZ, n (%) | 1 (12.5) | 0 (0.0) | 0.191 |
| AZA, n (%) | 2 (25.0) | 1 (7.7) | 0.271 |
| CYC, n (%) | 0 (0.0) | 1 (7.7) | 0.421 |
| ANR, n (%) | 0 (0.0) | 1 (7.7) | 0.421 |
*Expected number in one category is equal to zero.
ANA, antinuclear antibodies; ANCA, antineutrophil cytoplasmic antibodies; ANR, anakinra; AZA, azathioprine; BD, Behçet’s disease; C-GCA, cranial giant cell arteritis; CRP, C reactive protein; CYC, cyclophosphamide; EGPA, eosinophilic granulomatosis with polyangiitis; ESR, erythrocyte sedimentation rate; GCs, glucocorticoids; GPA, granulomatosis with polyangiitis; LV-GCA, large vessel giant cell arteritis; MPA, microscopic polyangiitis; MTX, methotrexate; N/A, not applicable; NSAIDs, non-steroidal anti-inflammatory drugs; SSZ, sulfasalazine.
Discussion
Since the earliest phases of the pandemic, several isolated case reports or small case series reporting the suspicious onset of rheumatic diseases in association with SARS-CoV-2 infection or COVID-19 vaccine administration have been published. Even though the anecdotal nature of those reports did not shed sufficient light on this phenomenon, they represent a stimulating hypothesis-generating basis for encouraging additional research on this topic.
To contribute to the body of knowledge in this field, we systematically collected consecutive cases of IRD onset in close temporal association with COVID-19 or vaccine administration, in order to identify potential differences between the two cohorts and more accurately depict the spectrum of diseases.
According to our results, IRD may occur roughly equivalently both following SARS-CoV-2 infection or COVID-19 vaccination and the range of manifestations is broad, covering different forms of IJD, CTD or vasculitis. However, it is crucial to disclose that temporal association alone does not imply causality and may merely represent a coincidental association, and, thus, no pathophysiological explanation can be extrapolated from ours’ and others’ available data. Furthermore, although we report a similar number of cases in the two cohorts, it must be pointed out that the denominator of the overall population is not known, preventing any epidemiological consideration to be drawn. Anyway, from a merely speculative point of view and according to the Italian Ministry of Health official data, 25 millions of cases of COVID-19 have been registered to date while more than 143 million of doses of COVID-19 vaccines have been administered.5 This implies that the number of individuals potentially susceptible to vaccine-related events is at least fivefold higher than that exposed to SARS-CoV-2 infection. Consequently, the association is anticipated to occur more frequently by coincidence in the postvaccination cohort (ie, no more than the anticipated number of incident cases of the specific IRD in such a heavily immunised population).
Additionally, increase in disease activity following SARS-CoV-2 infection has been reported in a significant portion of patients with pre-existent IRD,32 33 but it is difficult to uncouple the direct role of the virus and/or secondary immune system activation from the consequences of background DMARD treatment disruption. Similarly, vaccine administration has been associated with worsening of disease activity in a minor, but still present, fraction of patients.34 35 In this context, although it is not possible to exclude that a small proportion of patients in our cohort may actually represent a SARS-CoV-2 or vaccine-induced exacerbation of latent or previously undiagnosed IRD, evidence of disease flare-up in previously diagnosed IRD patients may suggest common underling pathophysiological mechanisms, leading to the development of a true, ‘de novo’, immunopathological event.
Despite these limitations, our data provide an interesting overview of the spectrum of the diseases possibly associated with either SARS-CoV-2 infection or COVID-19 vaccine and highlight some potential differences between the two cohorts. Indeed, we found a relatively higher percentage of patient developing IJD after COVID-19, while, on the other hand, a higher percentage of vaccine recipients developed PMR. Conversely, the distribution of other IRD categories did not differ between the two groups.
Viruses are well-known triggers for acute, subacute or chronic arthritis as commonly occur after parvovirus B19, HCV or chikungunya virus infection.36 A previous report from our group25 suggested that the delay between COVID-19 and arthritis onset is associated with the clinical phenotype of arthritis: while an RA-like pattern (polyarthritis mainly involving wrist and hand)—reminiscent of other prototypical viral arthritis—was more common in patients with early onset of rheumatic manifestations after infection (≤2 weeks), a late onset was more frequently associated with oligoarthritis of large joints suggestive of reactive arthritis. Viral infections have been evoked as a potential pathophysiological contributor to a number of other autoimmune diseases with different mechanisms including, but not limited to, molecular mimicry, bystander activation and epitope spreading.37
Similarly to infections, vaccine administration has been associated with the development of autoimmunity.38 The debated ASIA syndrome21 was defined in 2011 by Shoenfeld and collaborators as a condition in which the exposure to an adjuvant (eg, aluminium-based or squalene) leads to an abnormal, autoimmunogenic, immune response. However, it must be pointed out that novel mRNA vaccines do not contain traditional adjuvants because nucleic acids are sufficiently immunogenic to induce an effective immunisation.39
Our findings regarding post-vaccine IRD are in line with available literature, demonstrating that PMR is the most reported IRD after COVID-19 vaccine administration.25 40 41 Similar data were previously reported for influenza vaccine42 43 and supposed to result from an external trigger leading to an aberrant response in the context of a senescent immune system. Similarly to what observed in the post-COVID-19 cohort, however, in the post-vaccine group we reported a number of other ARD belonging to all categories mirroring isolated case reports or small series available in literature.22 44–46 Furthermore, a growing body of evidence support an association between mRNA vaccines and non-rheumatic autoimmune diseases such as myopericarditis,47 48 while adenovirus-based vaccines have been associated with vaccine-induced immune thrombotic thrombocytopenia49 50 and Guillain-Barré syndrome.51 52
Interestingly, when comparing clinical features of IJD between the two cohorts, we observed a higher relative percentage of PsA in the post-vaccine cohort. There are no obvious explanations for this finding although both new-onset psoriasis and psoriasis flares have been reported following COVID-19 vaccination.53 A speculative interpretation may be that the presence of concurrent skin disease (either new-onset or exacerbation of previously unrecognised psoriasis) promoted by vaccine administration, may lead to classify as PsA some patients of the post-vaccine cohort that otherwise would be attributed to the pSpA category. Unfortunately, we did not collect information regarding the cutaneous domain and therefore no sub-analysis can contribute to interpret this finding.
Another interesting finding is the higher prevalence of new-onset acrosyndromes in post-COVID-19 patients. This finding is not unsurprising in the light of the well-described endothelial tropism of SARS-CoV-254; indeed, cutaneous microvascular changes have been described since the beginning of the pandemic as chilblain-like lesions or ‘COVID toes’.55 In a Spanish observational study, acro-ischaemic lesions were observed in 0.6% outpatients and 2.9% hospitalised COVID-19 patients.56 More recently, Sulli et al57 reported that the mean nailfold capillary number per linear millimetre was significantly lower in COVID-19 survivors when compared with primary Raynaud’s phenomenon patients and control individuals.
In conclusion, although the aforementioned limitations, our article reports the largest cohort published to date and supports the hypothesis that new-onset IRD may be triggered by SARS-CoV-2 infection or COVID-19 vaccines and that the spectrum of possible clinical manifestations is broad and includes IJD, PMR, CTD and vasculitis. However, it is highly plausible that the risk conferred by SARS-CoV-2 infection is higher and thus the usefulness and safety of vaccines, in our opinion, are not to be questioned. Larger epidemiological studies are needed to better clarify the causal role of each individual exposure on this association, quantify the true incidence and eventually explore the pathophysiological mechanism linking SARS-CoV-2 infection or vaccination to the development of IRD.
Footnotes
Contributors: FU, CF, PR, FI, AI, RG contributed to the conception and design of the work. FU analysed the data; FU, CF, PR, FI, AI, RG contributed to data interpretation. FU and CF prepared the first draft of the work. All the other authors contributed to data acquisition, revised the draft critically and approved the final version to be published. CF is responsible for the overall content as guarantor.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Data are available upon reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and was approved by Comitato Etico Azienda Sanitaria Locale 1 Avezzano/Sulmona/L’Aquila, L’Aquila, Italy. Participants gave informed consent to participate in the study before taking part.
References
- 1.Lamers MM, Haagmans BL. SARS-Cov-2 pathogenesis. Nat Rev Microbiol 2022;20:270–84. 10.1038/s41579-022-00713-0 [DOI] [PubMed] [Google Scholar]
- 2.Li M, Wang H, Tian L, et al. COVID-19 vaccine development: milestones, lessons and prospects. Sig Transduct Target Ther 2022;7:146. 10.1038/s41392-022-00996-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vangeel L, Chiu W, De Jonghe S, et al. Remdesivir, Molnupiravir and Nirmatrelvir remain active against SARS-Cov-2 Omicron and other variants of concern. Antiviral Research 2022;198:105252. 10.1016/j.antiviral.2022.105252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Watson OJ, Barnsley G, Toor J, et al. Global impact of the first year of COVID-19 vaccination: a mathematical Modelling study. Lancet Infect Dis 2022;22:1293–302. 10.1016/S1473-3099(22)00320-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Italian Ministry of Health . Report Vaccini anti COVID-19; Italian Ministry of health Available: https://www.governo.it/it/cscovid19/report-vaccini/
- 6.Phetsouphanh C, Darley DR, Wilson DB, et al. Immunological dysfunction persists for 8 months following initial mild-to-moderate SARS-Cov-2 infection. Nat Immunol 2022;23:210–6. 10.1038/s41590-021-01113-x [DOI] [PubMed] [Google Scholar]
- 7.Nalbandian A, Sehgal K, Gupta A, et al. Post-acute COVID-19 syndrome. Nat Med 2021;27:601–15. 10.1038/s41591-021-01283-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fernández-de-las-Peñas C, Navarro-Santana M, Plaza-Manzano G, et al. Time course prevalence of post-COVID pain symptoms of musculoskeletal origin in patients who had survived severe acute respiratory syndrome Coronavirus 2 infection: a systematic review and meta-analysis. Pain 2022;163:1220–31. 10.1097/j.pain.0000000000002496 [DOI] [PubMed] [Google Scholar]
- 9.Ursini F, Ciaffi J, Mancarella L, et al. Fibromyalgia: a new facet of the post-COVID-19 syndrome spectrum? results from a web-based survey. RMD Open 2021;7:e001735. 10.1136/rmdopen-2021-001735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rojas M, Rodríguez Y, Acosta-Ampudia Y, et al. Autoimmunity is a hallmark of post-COVID syndrome. J Transl Med 2022;20:129. 10.1186/s12967-022-03328-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gracia-Ramos AE, Martin-Nares E, Hernández-Molina G. New onset of autoimmune diseases following COVID-19 diagnosis. Cells 2021;10:3592. 10.3390/cells10123592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ursini F, Ruscitti P, D’Angelo S, et al. Broad clinical spectrum of SARS-Cov-2-associated inflammatory joint disease in adults: a report of 35 cases from the COVID-19 & autoimmune systemic disease Italian study group. Ann Rheum Dis 2021;80:1498–501. 10.1136/annrheumdis-2021-220606 [DOI] [PubMed] [Google Scholar]
- 13.Metyas S, Chen C, Aung T, et al. Rheumatologic manifestations of post SARS-Cov-2 infection: A case series. CRR 2022;18:346–51. 10.2174/1573397118666220211155716 [DOI] [PubMed] [Google Scholar]
- 14.Shimizu H, Matsumoto H, Sasajima T, et al. New-onset dermatomyositis following COVID-19: A case report. Front Immunol 2022;13:1002329. 10.3389/fimmu.2022.1002329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kazzi B, Fine D, Geetha D, et al. New-onset lupus nephritis associated with COVID-19 infection. Lupus 2022;31:1007–11. 10.1177/09612033221098571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Allez M, Denis B, Bouaziz J-D, et al. COVID-19-related IgA vasculitis. Arthritis Rheumatol 2020;72:1952–3. 10.1002/art.41428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bach J-F. Infections and autoimmune diseases. J Autoimmun 2005;25 Suppl:74–80. 10.1016/j.jaut.2005.09.024 [DOI] [PubMed] [Google Scholar]
- 18.Courcoul A, Brinster A, Decullier E, et al. A Bicentre retrospective study of features and outcomes of patients with reactive arthritis. Joint Bone Spine 2018;85:201–5. 10.1016/j.jbspin.2017.01.013 [DOI] [PubMed] [Google Scholar]
- 19.Vassilopoulos D, Calabrese LH. Virally associated arthritis 2008: clinical, epidemiologic, and pathophysiologic considerations. Arthritis Res Ther 2008;10:215. 10.1186/ar2480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Agmon-Levin N, Paz Z, Israeli E, et al. Vaccines and Autoimmunity. Nat Rev Rheumatol 2009;5:648–52. 10.1038/nrrheum.2009.196 [DOI] [PubMed] [Google Scholar]
- 21.Watad A, Quaresma M, Bragazzi NL, et al. The autoimmune/inflammatory syndrome induced by Adjuvants (ASIA)/Shoenfeld’s syndrome: descriptive analysis of 300 patients from the International ASIA syndrome Registry. Clin Rheumatol 2018;37:483–93. 10.1007/s10067-017-3748-9 [DOI] [PubMed] [Google Scholar]
- 22.Chen Y, Xu Z, Wang P, et al. New-onset autoimmune phenomena post-COVID-19 vaccination. Immunology 2022;165:386–401. 10.1111/imm.13443 [DOI] [PubMed] [Google Scholar]
- 23.Al-Allaf A-W, Neethu M, Al-Allaf Y. A case series and literature review of the Association of COVID-19 vaccination with autoimmune diseases: causality or chance Cureus 2022. 10.7759/cureus.28677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ursini F, Ruscitti P, Raimondo V, et al. Systemic syndromes of Rheumatological interest with onset after COVID-19 vaccine administration: a report of 30 cases. Clin Rheumatol 2022;41:2261–7. 10.1007/s10067-022-06078-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ursini F, Ruscitti P, Raimondo V, et al. Spectrum of short-term inflammatory musculoskeletal manifestations after COVID-19 vaccine administration: a report of 66 cases. Ann Rheum Dis 2022;81:440–1. 10.1136/annrheumdis-2021-221587 [DOI] [PubMed] [Google Scholar]
- 26.Ferri C, Ursini F, Gragnani L, et al. Impaired Immunogenicity to COVID-19 vaccines in autoimmune systemic diseases. high prevalence of non-response in different patients’ subgroups. J Autoimmun 2021;125:102744. 10.1016/j.jaut.2021.102744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rayhan RU, Zheng Y, Uddin E, et al. Administer and collect medical questionnaires with Google documents: a simple, safe, and free system. Appl Med Inform 2013;33:12–21. [PMC free article] [PubMed] [Google Scholar]
- 28.Prevoo ML, van ’t Hof MA, Kuper HH, et al. Modified disease activity scores that include twenty-eight-joint counts. development and validation in a prospective longitudinal study of patients with rheumatoid arthritis. Arthritis Rheum 1995;38:44–8. 10.1002/art.1780380107 [DOI] [PubMed] [Google Scholar]
- 29.Leeb BF, Bird HA. A disease activity score for Polymyalgia Rheumatica. Ann Rheum Dis 2004;63:1279–83. 10.1136/ard.2003.011379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.World Medical Association . World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA 2013;310:2191–4. 10.1001/jama.2013.281053 [DOI] [PubMed] [Google Scholar]
- 31.World Health Organization (WHO) . Living guidance for clinical management of COVID-19. 2021. Available: https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2021-2
- 32.Di Iorio M, Cook CE, Vanni KMM, et al. DMARD disruption, rheumatic disease flare, and prolonged COVID-19 symptom duration after acute COVID-19 among patients with rheumatic disease: A prospective study. Semin Arthritis Rheum 2022;55:152025. 10.1016/j.semarthrit.2022.152025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dharia T, Venkatachalam S, Baker JF, et al. Medication interruptions and subsequent disease flares during the COVID-19 pandemic: A longitudinal Online study of patients with rheumatic disease. Arthritis Care Res (Hoboken) 2022;74:733–40. 10.1002/acr.24837 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Álvaro-Gracia JM, Sanchez-Piedra C, Culqui D, et al. Effects of COVID-19 vaccination on disease activity in patients with rheumatoid arthritis and Psoriatic arthritis on targeted therapy in the COVIDSER study. RMD Open 2023;9:e002936. 10.1136/rmdopen-2022-002936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Machado PM, Lawson-Tovey S, Strangfeld A, et al. Safety of vaccination against SARS-Cov-2 in people with rheumatic and musculoskeletal diseases: results from the EULAR Coronavirus vaccine (COVAX) physician-reported Registry. Ann Rheum Dis 2022;81:695–709. 10.1136/annrheumdis-2021-221490 [DOI] [PubMed] [Google Scholar]
- 36.Marks M, Marks JL. Viral arthritis. Clin Med (Lond) 2016;16:129–34. 10.7861/clinmedicine.16-2-129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Smatti MK, Cyprian FS, Nasrallah GK, et al. Viruses and Autoimmunity: A review on the potential interaction and molecular mechanisms. Viruses 2019;11:762. 10.3390/v11080762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Toussirot É, Bereau M. Vaccination and induction of autoimmune diseases. Inflamm Allergy Drug Targets 2015;14:94–8. 10.2174/1871528114666160105113046 [DOI] [PubMed] [Google Scholar]
- 39.Verbeke R, Hogan MJ, Loré K, et al. Innate immune mechanisms of mRNA vaccines. Immunity 2022;55:1993–2005. 10.1016/j.immuni.2022.10.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mettler C, Jonville-Bera A-P, Grandvuillemin A, et al. Risk of giant cell arteritis and Polymyalgia Rheumatica following COVID-19 vaccination: a global Pharmacovigilance study. Rheumatology (Oxford) 2022;61:865–7. 10.1093/rheumatology/keab756 [DOI] [PubMed] [Google Scholar]
- 41.Ottaviani S, Juge P-A, Forien M, et al. Polymyalgia Rheumatica following COVID-19 vaccination: A case-series of ten patients. Joint Bone Spine 2022;89:105334. 10.1016/j.jbspin.2021.105334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Falsetti P, Conticini E, Acciai C, et al. Polymyalgia Rheumatica following infective triggers or Vaccinations: a different subset of disease Reumatologia 2020;58:76–80. 10.5114/reum.2020.95360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Liozon E, Parreau S, Filloux M, et al. Giant cell arteritis or Polymyalgia Rheumatica after influenza vaccination: A study of 12 patients and a literature review. Autoimmun Rev 2021;20:102732. 10.1016/j.autrev.2020.102732 [DOI] [PubMed] [Google Scholar]
- 44.Chen C-C, Chen C-J. New-onset inflammatory arthritis after COVID-19 vaccination: A systematic review. Int J Rheum Dis 2023;26:267–77. 10.1111/1756-185X.14482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Khanna U, Oprea Y, Mir A, et al. New diagnosis of systemic lupus erythematosus after COVID-19 vaccination: A case report and review of literature. JAAD Case Reports 2022;30:30–4. 10.1016/j.jdcr.2022.09.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Abdelmaksoud A, Wollina U, Temiz SA, et al. SARS-Cov-2 vaccination-induced cutaneous vasculitis: report of two new cases and literature review. Dermatol Ther 2022;35:e15458. 10.1111/dth.15458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ling RR, Ramanathan K, Tan FL, et al. Myopericarditis following COVID-19 vaccination and non-COVID-19 vaccination: a systematic review and meta-analysis. Lancet Respir Med 2022;10:679–88. 10.1016/S2213-2600(22)00059-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Heymans S, Cooper LT. Myocarditis after COVID-19 mRNA vaccination: clinical observations and potential mechanisms. Nat Rev Cardiol 2022;19:75–7. 10.1038/s41569-021-00662-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kelton JG, Arnold DM, Nazy I. Lessons from vaccine-induced immune thrombotic thrombocytopenia. Nat Rev Immunol 2021;21:753–5. 10.1038/s41577-021-00642-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Elberry MH, Abdelgawad HAH, Hamdallah A, et al. A systematic review of vaccine-induced thrombotic thrombocytopenia in individuals who received COVID-19 adenoviral-vector-based vaccines. J Thromb Thrombolysis 2022;53:798–823. 10.1007/s11239-021-02626-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Abolmaali M, Rezania F, Behnagh AK, et al. Guillain-Barré syndrome in association with COVID-19 vaccination: a systematic review. Immunol Res 2022;70:752–64. 10.1007/s12026-022-09316-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hanson KE, Goddard K, Lewis N, et al. Incidence of Guillain-Barré syndrome after COVID-19 vaccination in the vaccine safety Datalink. JAMA Netw Open 2022;5:e228879. 10.1001/jamanetworkopen.2022.8879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wu P-C, Huang I-H, Wang C-W, et al. New Onset and exacerbations of psoriasis following COVID-19 vaccines: A systematic review. Am J Clin Dermatol 2022;23:775–99. 10.1007/s40257-022-00721-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Varga Z, Flammer AJ, Steiger P, et al. Endothelial cell infection and Endotheliitis in COVID-19. Lancet 2020;395:1417–8. 10.1016/S0140-6736(20)30937-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kanitakis J, Lesort C, Danset M, et al. Chilblain-like Acral lesions during the COVID-19 pandemic (‘COVID toes’): histologic, Immunofluorescence, and immunohistochemical study of 17 cases. J Am Acad Dermatol 2020;83:870–5. 10.1016/j.jaad.2020.05.145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Alonso MN, Mata-Forte T, García-León N, et al. Incidence, characteristics, laboratory findings and outcomes in Acro-ischemia in COVID-19 patients. Vasc Health Risk Manag 2020;16:467–78. 10.2147/VHRM.S276530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sulli A, Gotelli E, Bica PF, et al. Detailed Videocapillaroscopic Microvascular changes detectable in adult COVID-19 survivors. Microvasc Res 2022;142:104361. 10.1016/j.mvr.2022.104361 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available upon reasonable request.