Abstract
Objective
This study aimed to explore obstetric care professionals’ experiences with using cardiotocograph (CTG) information and how they employ this tool in their practice.
Design
Qualitative study, involving 30 semi-structured interviews and two focus group sessions. Conventional content analysis was used for data analysis.
Setting
Amsterdam University Medical Centers in the Netherlands.
Participants
In total, 43 care professionals participated. The respondents included obstetricians, residents in obstetrics and gynaecology, junior physicians, clinical midwives and nurses.
Findings
Three main categories were identified that influenced the use of cardiotocography in practice; (1) individual characteristics involving knowledge, experience and personal beliefs; (2) teams involving collaboration in and between shifts and (3) work environment involving equipment, culture and continuing development.
Conclusion
This study underlines the importance of teamwork when working with cardiotocography in practice. There is a particular need to create shared responsibility among team members for cardiotocography interpretation and appropriate management, which should be addressed in educational programmes and regular multidisciplinary meetings, to allow learning from colleagues’ perspectives.
Keywords: QUALITATIVE RESEARCH, Fetal medicine, PERINATOLOGY, Quality in health care, MEDICAL EDUCATION & TRAINING
Strengths and limitations of this study.
A qualitative research approach offers valuable insights in addition to other studies on the use of cardiotocograph (CTG) information in daily practice.
This study included an interprofessional perspective on the use of CTG in practice.
A total of 43 participants is considered to be a sufficient sample for this study approach.
The study was conducted within a single hospital institution with two locations in the Netherlands, and the transferability of the findings to different settings will vary.
Introduction
Monitoring fetal well-being by using a cardiotocograph (CTG) has become a standard practice of intrapartum care.1 CTG records the fetal heart rate (FHR) and uterine contractions to identify signs of intrapartum fetal hypoxia so that a timely intervention, for example, operative delivery, can take place and prenatal asphyxia may be prevented. This tool is heavily dependent on care professionals’ interpretation of its traces.1 2 CTG traces can have ambiguous clinical meanings and considerable interobserver and intraobserver variability has often been demonstrated, even among groups of experts.2 3 Still, 50 years after its introduction, interpretation of the FHR by CTG remains a challenge.
In practice, working with information provided by CTG registrations is complex. CTG monitoring of the fetal and maternal condition not only requires frequent classification of the CTG tracing. Interpretation of this information leading to decision-making involves taking personal needs and circumstances of high-risk women in labour into account by obstetric healthcare providers working in interprofessional teams in dynamic care setting.2 3 Use of (international) interpretation guidelines and training programmes are often recommended to standardise interpretation and improve skills needed for classification of CTG tracings.4–6 The body of literature on classification skills, interventions to improve CTG use and related educational programmes tends to pay particular attention to the individual, without including the social and material context in which CTG is being used.3 5–7
To fully understand how obstetric caregivers, working in the context of dynamic teams and settings, use CTG information in their practice, more emphasis should be placed on the interaction between individuals and their practice context. Therefore, this study aimed to explore obstetric care professionals’ experiences with using CTG information and how they employed this tool in their practice. We have focused specifically on interpretation and interprofessional interactions, as insight in that aspect is deemed necessary to integrate educational interventions or other improvement efforts related to the use of CTG.
Methods
Study design
This qualitative study was based on an interpretivist research paradigm, focusing on understanding perspectives from various care professionals.8 This study combined semi-structured interviews with focus groups sessions. The Consolidated criteria for Reporting Qualitative research criteria were used for reporting qualitative research.9
Setting
This study was conducted in the Netherlands. The Dutch Society of Obstetrics and Gynaecology (NVOG) recommends continuous intrapartum monitoring for women whose babiesare at risk for perinatal asphyxia and to use the modified classification of the International Federation of Obstetrics and Gynaecology (FIGO). This modified FIGO classification involves four categories of CTG classification: normal, suboptimal, abnormal, preterminal.10 Furthermore, the NVOG guideline states that interpretation and classification of the CTG, in the context of medical history and information on current pregnancy, should occur every hour during the first stage of labour and every 15 min during the second stage. If the CTG is classified as suboptimal or abnormal, interpretation has to be more frequent. There is no policy requirement for another clinician to independently review CTGs on a regular basis. However, in practice, both residents, clinical midwives and obstetricians jointly monitor active CTG registrations of women in labour. Clinical information from (ante)natal notes is part of this assessment of the CTG.
In the Netherlands, CTG is used in hospital settings where obstetrical teams take care of women with increased risk of adverse fetal or maternal outcomes. More specialised care for complex and very preterm cases is provided in academic hospitals. Women with lower risks of pathology are cared for by independent primary-care midwives at home and in midwifery practices in the locality. The current study was performed at the Amsterdam University Medical Center (UMC), an academic hospital with two locations in an urban setting. With a total of approximately 2600 childbirths annually, Amsterdam UMC is the largest academic hospital in the Netherlands. CTG monitoring, according to the Dutch guideline, is applied to all women in labour under the care of an obstetrician, since it is a high-risk population. Central fetal monitoring is in use with fetal blood sampling as an additional technique to gain more insight in the fetal condition. Education on FHR monitoring is incorporated at daily handovers and regular meetings for staff.
Participants, sampling and data collection
Participants involved obstetricians, residents in obstetrics and gynaecology, junior physicians working in obstetrics and gynaecology (who are not in a postgraduate training programme), clinical midwives (also called hospital-based midwives) and nurses. For the semi-structured interviews, 30 care professionals were invited (15 care professionals from each location). We expected that we would need less than 30 interviews to reach data sufficiency, which we defined as no substantial additions to the themes that resulted from the interviews. Initial analysis started during data collection. After 20 interviews no new themes were found in the data. At that point, we decided to finish data collection after all 30 interviews were completed.
All semi-structured interviews were conducted by the first author (AR). The interviews focused on care professionals’ experiences with using CTG information in practice as well as the learning process, involving six main topics: attitude towards the use of CTG, interpretation of CTG, decision-making process, consulting with colleagues, learning process and improvement efforts. The interview topics were derived from literature2 3 as well as authors (PB and PWT) with experience in using CTG in daily practice. The interview protocol was pilot tested. Since the interview topic guide barely changed after the pilot, the pilot interview was included in the current research sample. The interview topic guide is given as online supplemental appendix 1. Each interview lasted approximately 60 min. The interviews were conducted between May and October 2018.
bmjopen-2022-068162supp001.pdf (44.2KB, pdf)
Care professionals with different professional backgrounds were approached for two focus group sessions in order to discuss and reflect on findings of the semi-structured interviews. Participation in an interview was no exclusion criterion for participation in the focus group. We included heterogeneous groups of all care professions to explore topics using different perspectives.11 The focus group sessions were facilitated by an independent experienced moderator with the first author (AR) present as an observer. Based on the main results of the semi-structured interviews, participants discussed the interview findings and used that discussion to jointly formulate opportunities for improvement of practical use of CTG. Each focus groups session lasted approximately 90 min. The focus group sessions were conducted in April 2019. All participants in this study were invited by email and gave informed consent for tape-recording the semi-structured interviews and focus group discussions. Within 4 weeks the participants received a summary for verification purposes. None of the participants requested any changes.
Analysis
All recordings of the semi-structured interviews were transcribed verbatim. These qualitative data were analysed using a conventional content analysis approach.12 All interviews were repeatedly read to capture the essence of the data. Relevant text fragments were highlighted and coded. No codes or categories were identified before analysis. An initial coding scheme was created by AR through line-by-line open coding of five interviews (one of each profession). Codes were sorted into categories based on how different codes were related and linked, discussed by all authors.12 For example, care professionals’ experiences on basic information of CTG components (code) as well as guidelines (code) were linked to knowledge (subcategory) as part of the main category ‘Individuals’. Further analysis led to modifications of this coding scheme. After 20 interviews no new codes were generated by the researchers and the final coding scheme was used to analyse the remaining interviews. Data from focus group sessions were not part of the initial content analysis, but were used to further refine the categories and understand how they were related to each other. Analysis was done using Atlas.ti V.8.0 software.
Patient and public involvement
None.
Findings
In this qualitative study, 30 care professionals participated in semi-structured interviews. In addition, 15 care professionals participated in two focus group sessions, of whom two participants were also involved in the interviews (from location A). In total, 43 care professionals were included in this study. Table 1 shows the respondent characteristics. The majority of the respondents were female, representative for the team composition at the hospital.
Table 1.
Respondent characteristics
| Total N (% female) |
Age* | Work experience* (profession) | Work experience* (hospital)† | |
| Obstetricians | 10 (50) | 42 (41–45) | 14 (10–17) | 6 (6–17) |
| Residents in training | 8 (63) | 33 (32–33) | 8 (7–8) | 2 (2–3) |
| Junior physicians | 6 (100) | 29 (28–30) | 4 (3–4) | 2 (1–2) |
| Clinical midwives | 8 (100) | 50 (40–57) | 20 (11–29) | 8 (4–13) |
| Nurses | 11 (100) | 42 (38–51) | 13 (10–25) | 7 (5–18) |
*Median (Q1–Q3), in years.
†Department of Obstetrics and Gynaecology in Amsterdam University Medical Center.
Based on our analysis, we have organised obstetrical care professionals’ experiences with using CTG information and how they employ this tool in their practice in three main categories: (1) individual characteristics, (2) teams, (3) work environment. Figure 1 shows the main categories and the related subcategories.
Figure 1.
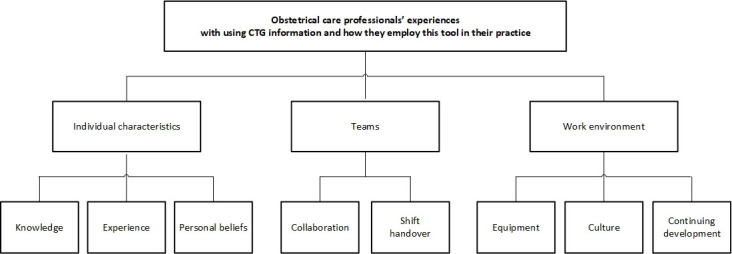
Tree diagram of categories and related subcategories. CTG, cardiotocograph.
Individual characteristics
This category refers to individual characteristics of care professionals. Three characteristics were distinguished: knowledge, experience and personal beliefs.
First, using CTG information in daily practice required knowledge on technical aspects and basic CTG features (baseline, variability, accelerations and decelerations) for classification purposes.
I’ve learned to work with CTG by doing, seeing and being taught. Where to look at? What do you see and why? Basically, knowledge transfer (P2)
Moreover, participants stated that knowledge on physiological mechanisms and clinical context information is necessary for a comprehensive interpretation and adequate management. Participants acknowledged the importance of consensus on the definition of CTG characteristics defined in guidelines, yet struggled to be consistent. Participants recognised that definitions were not always used appropriately which could lead to confusion about a patient’s situation. A common example given by participants was the definition of decelerations, by not specifying the type of deceleration or simple referring to ‘a slight dip’ in the fetal heart rate.
Second, all participants emphasised that the ability to use CTG in clinical context required experience.
CTG is a matter of doing. In theory, there are ways to describe a CTG, good and bad scenario’s. However, in practice there are many variations. (…) And you need exposure to learn about these variations, the outcomes and management. (P1)
Being involved in the interpretation and decision-making process and by questioning or discussing CTG patterns with team members participants developed practical know-how. Participants explained that there was no substitute for practical experience; it helped build confidence in one’s skills and develop intuition by incorporating clinical context information. Moreover, participants mentioned that increasing experience made them more alert for (sudden) pattern changes, enabled a better understanding of appropriate management and a broader range of possible interventions. On the contrary, less experienced participants mentioned that they relied heavily on the assessment of their team members, expressed feelings of insecurity about their own skills and worried about possible diagnostic errors, making them more prone to choose obstetrical interventions (according to them). All participants referred to experience as a dynamic frame of reference, based on pattern recognition. It was often mentioned that experience helped to recognise recurrent scenarios, related to the outcome of childbirth and clinical context. Mentioned drawbacks of this pattern recognition were false reassurance as well as a shift of frame of reference after (several) negative experiences.
Third, participants expressed different personal beliefs about the effectiveness of CTG in adequately monitoring fetal well-being. Some indicated to have faith in the technology, others were reluctant to trust CTG interpretation alone and appreciated additional tests, and few were sceptical of the value of CTG and questioned whether CTG should be used at all. It was suggested by participants that personal beliefs influenced interpretation and decision-making in practice.
And it also has to do with, whether you have a defensive attitude and you want to avoid making a wrong assessment at all costs and, therefore, act on all deviations. Or are you willing to accept variations in nature and to see how something develops without interference? And I believe more in the latter. (P12)
Teams
A much-discussed topic in the interviews and focus groups was the importance of teamwork when using CTG in practice, involving collaboration between different obstetrical team members in and between shifts. Regardless of the level of experience, participants described some degree of uncertainty when interpreting a CTG pattern or determining appropriate management. Therefore, easily approachable team members were highly valued by all care professions to help with and discuss interpretation of CTG patterns.
If I have any doubts about something, I will discuss it. I think you look at it [CTG] with several people, and sometimes I notice something which I will point out to someone and another time someone else does that for me. You have to do it together. (P8)
Participants mentioned various functions of collaboration, a continuum ranging from making an assessment together for learning purposes, looking for confirmation, a second opinion or requesting consultation for an (expected) deteriorating case. In a request for help with (expected) severe and acute cases participants stated that they would involve a more experienced team member and/or supervisor. However, in non-urgent situations most participants indicated that profession was irrelevant and they simply wanted to share their thinking with a team member. Many respondents emphasised that collaboration, in any form, created a sense of shared responsibility.
Sometimes you just need someone to spar with or consult, and I actually think that you often find a solution and that that consultation is sometimes initiated to feel supported or strengthened in a decision. (P19)
According to participants, team composition could have an influence on collaboration which they often illustrated by the difference between day and night shifts. In general, participants referred to day shifts as being more dynamic and crowded as more team members were available for a shared assessment of CTG. Though, some participants stated that more input, distractions and stress were perceived as limitations for practical use of CTG during day shifts. On the contrary, night shifts were relatively more quiet and participants could focus better on CTG traces in a smaller team. However, in this setting, a supervisor was not always physically present and phoning for help with CTG interpretation was perceived as a barrier. In addition, many participants recognised that especially during night shifts there was a risk of ‘tunnel vision’ regarding CTG interpretation.
Care professionals could feel more insecure about CTG interpretation at night and, affected by fatigue and team composition, even postpone a decision for non-urgent interventions until the day shift arrived. Moreover, participants identified shift handovers as important moments for CTG interpretation and decision-making. CTG interpretation by team members of a new shift was described as offering a fresh perspective. Many respondents experienced that this fresh perspective could lead to a different interpretation or policy.
And yet, I don’t know whether its objective or subjective, but still you start a new shift with a more fresh perspective. You are just … well if it is quicker I don’t know (…) but your helicopter view is just wider than if you have been on it for eight hours (P18)
Work environment
This category refers to environmental factors which influenced the use of CTG in practice. First, a prerequisite for working with CTG was functional equipment. Participants found it essential that CTG traces were visible at multiple screens in the labour ward.
Functional equipment is important of course. Well-functioning, complete and visible on screen (P15)
Second, participants referred often to norms and values of the maternity unit. Participants who mentioned their previous workplace were most explicit about difference in cultural aspects as they compared uses of CTG in practice.
Examples of differences in perceived culture were; time to respond to suspicious or abnormal CTG traces and related interventions, frequency of interdisciplinary case reviews based on CTG tracings (eg, during shift handovers) and request for help and speaking up. Participants trusted that their colleagues would speak up on concerns about CTG traces and that team members would accept unsolicited input. Although this was widely supported, many participants were able to recall situations where they struggled to or did not speak up to a supervisor or a more experienced team member.
And that [speak-up] is easy if you have a young colleague, for example a junior physician, but for me it’s something else when it comes to a more experienced colleague (…) a midwife or obstetrician who has been doing this work for much longer than I do, and can cause friction, at least … I find it quite uncomfortable to provide unsolicited input. Because it also gives, a kind of, sign of lack of trust … (P9)
Finally, participants stated that working with CTG implied a continues learning process requiring education. In many interviews and the focus groups sessions it was argued that a basic course should be compulsory, for all who start working with CTG regardless the profession. Subsequently, participants stressed the importance of recurrent training and frequent CTG discussion and reviews with colleagues, preferable in a multidisciplinary setting. This could mean different things, ranging from shared assessments of a CTG trace, explicit attention for interpretation and decision-making based on CTG information during handover as well as specifically planned meetings to discuss case scenarios.
You should organise regular meetings and give colleagues the opportunity, like i said, for example to share cases of their own shifts to learn and learn from each other. (P14).
Discussion
This qualitative study explored obstetric care professionals’ experiences with using CTG information and how they employed this tool in their practice. Based on semi-structured interviews and focus group sessions, three categories were identified; individual characteristics, teams and work environment.
Smith et al performed a systematic review and thematic analysis on professionals’ views of electronic fetal monitoring. Four themes were identified, reassurance, technology, communication/education and midwife by proxy.13 The current study used different methodology, yet some similar results were found. Individual factors were related to views as well as experiences with using CTG information, for example the personal beliefs regarding the technology.13 Moreover, in both studies communication and education were considered as relevant categories. Smith et al13 reported concerns that the technology might hinder effective communication with women in labour. Our study focused on communication between team members and highlighted the importance of collaboration in and between shifts.
Participants emphasised the importance of collaboration considering the need for frequent (interprofessional and intraprofessional) consultations, reassurance as well as establishing shared responsibility for maternal and fetal outcomes. These results relate to the concept of situational awareness and the need to include perceptions of team members in decision-making processes.14 Therefore, comparable to previous findings it is recommended to embed these team factors in educational efforts to improve CTG interpretation and management.5 6 15 16 Our study highlights that use of CTG involves a continuous learning process. Development of individual skills is a prerequisite (regardless of what guideline is in use), however, use of CTG in practice is perceived as a team-based activity which requires regular multidisciplinary meetings to learn from colleagues’ perspectives.
Finally, this study provided insight into vulnerabilities related to use of CTG in practice. For example, care professionals with little CTG experience can feel insecure about their own skills and sometimes perceive a barrier to phone for help. Young et al observed that junior medical staff is a group most frequently involved in suboptimal care.15 Moreover, Ugwumadu et al pointed out in a commentary that ‘often critical decisions are left to trainees or junior staff members, while those who have developed expertise over the years are not even aware that there is a problem’.7 Our results suggested that supervisors and more experienced team members can (and should) work to create a culture that enables a low threshold for collaboration and a safe learning environment. Another finding was the positive impact of ‘a fresh perspective’ at shift handovers. Our participants reported that this is influenced by fatigue, team composition and the availability of resources. This was most apparent comparing day to night shifts, according to many participants. Organisations need to be aware of these issues and further research is necessary on the impact of ‘a fresh perspective’ on patient safety in obstetrics.
Limitations
This study was conducted as a single centre study in one hospital institution, with two locations, in the Netherlands. Therefore, transferability of findings may be limited to settings where composition of the team or workplace environment is structured similarly. The study aimed to be explorative, yielding insight in various factors and their interactions. Findings, however, cannot be used to know what effect changes in one category might have on the other categories.
Conclusions
In conclusion, in this study the use of CTG in practice was perceived as a team-effort rather than an individual task. In practice, individual skills interact with environmental factors and collaboration within multi-professional teams, resulting in CTG interpretation and subsequent decision-making. There is a particular need to create shared responsibility among team members, which should be addressed in educational programmes and regular multidisciplinary meetings to learn from colleagues’ perspectives. Despite its limitations, CTG is still the most commonly used tool worldwide to monitor the condition of the fetus during labour. The findings of this study can contribute to improve how CTG is employed in practice.
Supplementary Material
Acknowledgments
We would like to thank the care professionals who participated in this study.
Footnotes
Contributors: All authors made contributions to the design of this study. AR carried out data collection, performed analyses and drafted the manuscript. PB and PWT made contributions to interpretation of the data and revisions to the manuscript. All authors read and approved the final manuscript. PB is the guarantor.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request. The data that support the findings of this study are not publicly available. Data are available upon reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and this study was deemed exempt from approval by the Medical Ethical Committee of the Amsterdam University Medical Centers on 28 March 2018 (2018.175). The protocol was in accordance with Dutch privacy regulations. Participants gave their informed consent to participate in the interviews and the focus groups.
References
- 1.Alfirevic Z, Devane D, Gyte GM, et al. Continuous Cardiotocography (CTG) as a form of electronic fetal monitoring (EFM) for fetal assessment during labour. Cochrane Database Syst Rev 2017;2:CD006066. 10.1002/14651858.CD006066.pub3 [DOI] [PubMed] [Google Scholar]
- 2.Pinas A, Chandraharan E. Continuous Cardiotocography during labour: analysis, classification and management. Best Pract Res Clin Obstet Gynaecol 2016;30:33–47. 10.1016/j.bpobgyn.2015.03.022 [DOI] [PubMed] [Google Scholar]
- 3.Santo S, Ayres-de-Campos D. Human factors affecting the interpretation of fetal heart rate tracings: an update. Curr Opin Obstet Gynecol 2012;24:84–8. 10.1097/GCO.0b013e3283505b3c [DOI] [PubMed] [Google Scholar]
- 4.Santo S, Ayres-de-Campos D, Costa-Santos C, et al. Da Graça LM for the FM-compare collaboration. agreement and accuracy using the FIGO, ACOG and NICE Cardiotocography interpretation guidelines. Acta Obstet Gynecol Scand 2017;96:166–75. 10.1111/aogs.13064 [DOI] [PubMed] [Google Scholar]
- 5.Pehrson C, Sorensen JL, Amer-Wåhlin I. Evaluation and impact of Cardiotocography training programmes: a systematic review. BJOG 2011;118:926–35. 10.1111/j.1471-0528.2011.03021.x [DOI] [PubMed] [Google Scholar]
- 6.Kelly S, Redmond P, King S, et al. Training in the use of Intrapartum electronic fetal monitoring with Cardiotocography: systematic review and meta-analysis. BJOG 2021;128:1408–19. 10.1111/1471-0528.16619 Available: https://onlinelibrary.wiley.com/toc/14710528/128/9 [DOI] [PubMed] [Google Scholar]
- 7.Ugwumadu A, Steer P, Parer B, et al. Time to Optimise and enforce training in interpretation of Intrapartum Cardiotocograph. BJOG 2016;123:866–9. 10.1111/1471-0528.13846 [DOI] [PubMed] [Google Scholar]
- 8.Bunniss S, Kelly DR. Research paradigms in medical education research. Med Educ 2010;44:358–66. 10.1111/j.1365-2923.2009.03611.x [DOI] [PubMed] [Google Scholar]
- 9.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int J Qual Health Care 2007;19:349–57. 10.1093/intqhc/mzm042 [DOI] [PubMed] [Google Scholar]
- 10.NVOG . Guideline for Intrapartum fetal monitoring [Richtlijn voor intraparum fetale bewaking]. Utrecht 2014. [Google Scholar]
- 11.Gill P, Stewart K, Treasure E, et al. Methods of data collection in qualitative research: interviews and focus groups. Br Dent J 2008;204:291–5. 10.1038/bdj.2008.192 [DOI] [PubMed] [Google Scholar]
- 12.Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res 2005;15:1277–88. 10.1177/1049732305276687 [DOI] [PubMed] [Google Scholar]
- 13.Smith V, Begley CM, Clarke M, et al. Professionals’ views of fetal monitoring during labour: a systematic review and thematic analysis. BMC Pregnancy Childbirth 2012;12:166. 10.1186/1471-2393-12-166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Endsley MR. Toward a theory of situation awareness in dynamic systems. Hum Factors 1995;37:32–64. 10.1518/001872095779049543 [DOI] [Google Scholar]
- 15.Young P, Hamilton R, Hodgett S, et al. Reducing risk by improving standards of Intrapartum fetal care. J R Soc Med 2001;94:226–31. 10.1177/014107680109400507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Miller LA, Miller DA. A collaborative Interdisciplinary approach to electronic fetal monitoring; report of a statewide initiative. J Perinat Neonatal Nurs 2013;27:126–33. 10.1097/JPN.0b013e31828ee7fe [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2022-068162supp001.pdf (44.2KB, pdf)
Data Availability Statement
Data are available upon reasonable request. The data that support the findings of this study are not publicly available. Data are available upon reasonable request.


