ABSTRACT
BACKGROUND:
Early radiological prediction and diagnosis of perforated acute appendicitis remain controversial. In the current study, it was aimed to examine the predictive value of multidetector computed tomography (MDCT) findings in perforated acute appendicitis.
METHODS:
The patients (n=542) who underwent appendectomy between January 2019 and December 2021 were retrospectively evaluated. The patients were divided into two groups as non-perforated appendicitis and perforated appendicitis. Preoperative abdominal MDCT findings, appendix sphericity index (ASI) scores, and laboratory findings were evaluated.
RESULTS:
The sample consisted of 427 cases in the non-perforated group and 115 cases in the perforated group, with a mean age of 33.88±12.84 years. The mean time until admission was 2.06±1.43 days. Appendicolith, free fluid, wall defect, abscess, free air, and retroperitoneal space (RPS) involvement were all found to be significantly higher in the perforated group (P<0.001). The mean long axis, short axis, and ASI values were found to be higher in the perforated group (P<0.001; P=0.004; and P<0.001, respectively). C-reactive protein (CRP) was found to be significantly higher in the perforated group (P=0.008), but the mean white blood count was found to be similar between the groups (P=0.613). Among MDCT findings, free fluid, wall defect, abscess, high CRP, long axis, and ASI were observed to be predictive values for perforation. According to receiver operating characteristic analysis, ASI had a cut-off value of 1.30, a sensitivity of 80.87%, and a specificity of 93.21%.
CONCLUSION:
MDCT findings, namely, appendicolith, free fluid, wall defect, abscess, free air, and RPS involvement are significant findings for perforated appendicitis. With a high sensitivity and specificity, the ASI appears to be a key predictive parameter for perforated acute appendicitis.
Keywords: Appendix sphericity index, multidedector computed tomography, perforated acute appendicitis
INTRODUCTION
Acute appendicitis is an urgent surgical pathology with a high prevalence, requiring a quick and accurate diagnosis to exclude perforation. With a lifetime risk of 8.6% for men and 6.7% for women, it is one of the most frequent causes of acute abdominal pain in both adults and children.[1] It is often diagnosed based on a patient’s clinical history in conjunction with physical examination and laboratory and radiological imaging. Ultrasound (US) is easily used, non-invasive, cheap, and does not require the administration of contrast material. Multidetector computed tomography (MDCT) is an auxiliary and complementary imaging method to US in the diagnosis of acute appendicitis. It is advised for patients with acute abdominal pain when US results are insufficient, unclear, or normal.[2] However, there are still uncertainties regarding the diagnosis of perforated appendicitis.
Identifying perforated or potential perforation cases at the first admission will solidify the need for early and rapid surgical intervention and reduce morbidity and mortality by preventing life-threatening peritonitis and sepsis. Furthermore, the early prediction of perforation affects the treatment approach. There are some options for perforated appendicitis, such as laparoscopic or open appendectomy and drainage. For non-perforated appendicitis, antibiotic therapy is an alternative to surgery.
Increased appendiceal diameter (>6 mm) and wall thickness (>2 mm), periappendicular inflammation, and calcified appendicolith on MDCT are strong pieces of evidence for acute appendicitis.[3] Perforated appendicitis can be diagnosed with high specificity with the presence of extraluminal free air, abscess, appendiceal wall defect, or extraluminal appendicolith on CT.[4] In addition to these, less specific findings such as periappendiceal phlegmon, ileus, ascites, and appendiceal sphericity index (ASI) are reported in the literature.[5,6] On the other hand, there are also authors who argue that perforation cannot be diagnosed by MDCT alone, unless there is an abscess or extraluminal gas.[7]
The present study aimed to evaluate the importance of sphericity index and other CT findings in predicting perforated appendicitis.
MATERIALS AND METHODS
Retrospective analysis was performed on the patients (n = 542) who underwent open or laparoscopic appendectomy due to acute appendicitis between January 2019 and December 2021. Approval was obtained from the local ethics committee for the study (approval number: 2020–50). All patients with non-perforated or perforated appendicitis over the age of 18 years who underwent surgery were included in the study. Patients who did not have any preoperative MDCT findings, patients who had a negative appendectomy, patients who had elective appendectomy after plastron appendicitis, patients whose appendiceal lumen could not be evaluated by CT, patients with non-contrast CT findings, patients with non-optimal CT image quality, patients with >12 h between CT imaging and surgery, and patients under 18 years of age were excluded from the study.
Two groups of patients were formed: non-perforated and perforated. Age, gender, ASA scores, duration of symptoms (days), clinical diagnosis, pathological diagnosis, and preoperative abdominal MDCT findings were examined. A radiologist with 8 years of experience retrospectively examined each abdominal MDCT image. Without administering oral contrast, CT images were collected using an MDCT scanner (Brilliance 64; Philips Medical Systems, Cleveland, OH). The technical parameters of CT were as follows: beam collimation 0.625 mm; table speed 50.8 mm rotation–1; beam pitch 1.014; rotation time 0.5 s; 140–175 mAs; and voltage 120 kV (peak). After beginning an infusion of 120 mL non-ionic contrast material through the antecubital vein at a rate of 4 mL s-1, the patient underwent a post-contrast scanning of the entire abdomen with a delay of 60–70 s. The axial cross-sectional data were reconstructed with a thickness of 5 mm and a width of 2 mm. The second data set was formatted coronally with a thickness of 3 mm.
In the evaluation of abdominal CT, appendicolith, appendix long and short axis length (mm), sphericity index, wall defect, periappendicular free fluid, abscess, intraabdominal free air, ileus, and retroperitoneal space (RPS) involvement were examined. ASI was measured and recorded as described by Şirik and İnan[6] Sphericity index was calculated according to the long axis/short axis ratio in images on the CT plane perpendicular to the appendix (Fig. 1 and 2).[6] RPS segments were evaluated for signs of inflammation, such as thickening of the fascial plane. The histopathological result was considered the gold standard for the diagnosis of perforation.
Figure 1.
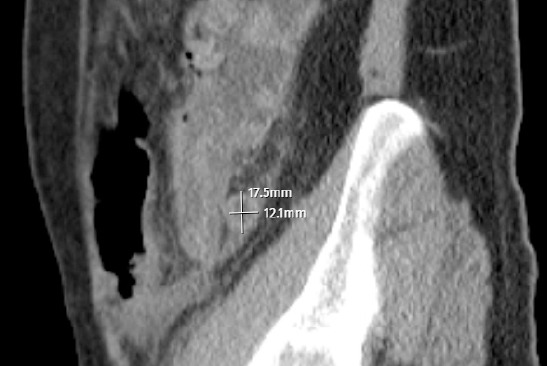
Sagittal-oblique multiplanar reconstruction CT images to calculate the sphericity index in perforated acute appendicitis patients
Figure 2.

Sagittal-oblique multiplanar reconstruction CT images to calculate the sphericity index in perforated acute appendicitis patients
Statistical Analysis
The SPSS software, version 17.0, was used to conduct all statistical analyses. Histogram graphics and the Kolmogorov–Smirnov test were used to examine the conformity of the variables to normal distribution. Descriptive analyses were presented with mean, median, and standard deviation values. The Pearson Chi-squared test was utilized to evaluate categorical variables. For non-normally distributed data, groups of two were compared with the Mann–Whitney-U test. The effects of CT findings, white blood count (WBC), and C-reactive protein (CRP) on perforation were examined using Binary Logistic Regression Analysis. The diagnostic and predictive performance of the same data was assessed using receiver operating characteristic (ROC) curve analysis. A P <0.05 was regarded as statistically significant for all analyses.
RESULTS
In our investigation, 542 patients in total, 427 in the non-perforated group, and 115 in the perforated group, were studied. The overall mean age of the patients was 33.88±12.84 years, with 361 men and 181 women among them (Table 1). The mean wait time for admittance was 2.06±1.43 days. The distribution of ASA scores was similar between the two groups (P=0643).
Table 1.
Distribution of groups, demographic data, and clinical characteristics
| N | % | |
|---|---|---|
| Non-perforated group | 427 | (78.78) |
| Perforated group | 115 | (21.22) |
| Male/female | 361/181 | (66.61/33.39) |
| *Age | 33.88±12.84 | 31.00 |
| *ASA score | 1.21±0.47 | 1.00 |
| *Duration of symptoms | 2.06±1.43 | 2.00 |
| at admission (day) |
n is replaced by mean±SD, and % is replaced by median
There was a significant increase in appendicolith, free fluid, wall defect, abscess, free air, and RPS involvement in the perforated group (Table 2). However, there was no significant difference between the two groups in terms of ileus (P=0.273).
Table 2.
Comparison of MDCT findings and serum WBC and CRP results between groups
| Non-perforated n (%)/ mean±SD | Perforated n (%)/ mean±SD | P | |
|---|---|---|---|
| Appendicolith | 94 (22.0) | 43 (37.4) | 0.001a |
| Free fluid | 100 (23.4) | 74 (64.3) | <0.001a |
| Wall defect | 23 (5.4) | 42 (36.5) | <0.001a |
| Abscess | 6 (1.4) | 17 (14.8) | <0.001a |
| Extraluminal air | 0 | 6 (5.2) | <0.001a |
| Ileus | 22 (5.1) | 9 (7.8) | 0.273a |
| RPS | 56 (13.1) | 52 (45.2) | <0.001a |
| Long axis (mm) | 11.18±2.35 | 14.64±2.35 | <0.001b |
| Short axis (mm) | 9.69±2.07 | 10.19±1.82 | 0.004b |
| Appendix Sphericity index (ASI) | 1.16±0.09 | 1.45±0.17 | <0.001b |
| WBC (103/mm3) | 14.46±4.27 | 14.86±4.56 | 0.613b |
| CRP (mg/dL) | 12.01±30.51 | 17.57±40.85 | 0.008b |
aChi-squared test; bMann-Whitney U test; MDCT: Multidetector computed tomography; RPS: Retroperitoneal space; WBC: White blood count; CRP: C-reactive protein.
The mean long axis, short axis, and ASI scores were found to be higher in the perforated group (Table 2). The mean WBC was similar in both groups (P=0.613), while CRP was considerably higher in the perforated group (P=0.008).
The prognostic impact of appendicolith, free fluid, wall defect, abscess, RPS involvement, CRP, and long axis (mm) on acute appendicitis perforation was investigated using a binary logistic regression analysis. It was observed that free fluid, wall defect, abscess, high CRP, and increased long axis on CT were predictive for perforation. In the case of free fluid, wall defect, and abscess on CT, the probability of perforation increases by 3.4, 4.6, and 5.8 times, respectively. One unit of increase in CRP increases the perforation risk by 1.009 times, and one unit of increase in the long axis (mm) increases it by 1.6 times (Table 3).
Table 3.
Logistic regression analysis of CT findings and CRP
| B | S.E. | Sig. | Exp(B) | 95% CI for EXP (B) | ||
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Appendicolith | 0.009 | 0.319 | 0.976 | 1.009 | 0.541 | 1.885 |
| Free fluid | 1.239 | 0.291 | <0.001 | |||
| 3.452 | 1.953 | 6.101 | ||||
| Wall defect | 1.534 | 0.380 | <0.001 | 4.637 | 2.203 | 9.758 |
| Abscess | 1.761 | 0.675 | 0.009 | 5.816 | 1.549 | 21.834 |
| RPS | 0.505 | 0.325 | 0.120 | 1.657 | 0.877 | 3.131 |
| Long axis (mm) | 0.515 | 0.066 | <0.001 | 1.673 | 1.471 | 1.903 |
| CRP (mg/dL) | 0.009 | 0.004 | 0.023 | 1.009 | 1.001 | 1.017 |
Binary logistic regression; CT: Computed tomography; CRP: C-reactive protein; RPS: Retroperitoneal space.
The predictive effect of ASI on perforation was examined using ROC analysis (Fig. 3). The cut-off value for ASI was found to be 1.30, with a sensitivity of 80.87%, a specificity of 93.21%, a positive predictive value of 76.23%, and a negative predictive value of 94.76% (Table 4). When the cut-off value of 13.15 mm was accepted for the long axis, sensitivity and specificity were calculated as 76.52% and 80.80%, respectively.
Figure 3.
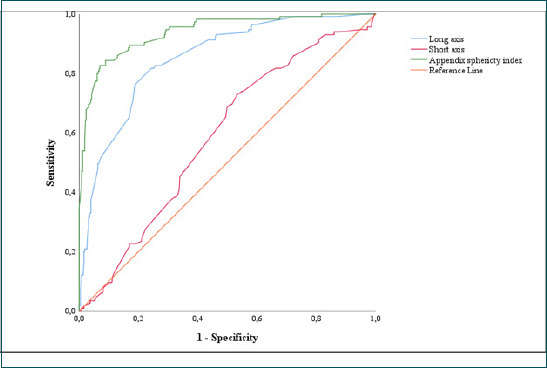
Receiver operating characteristic curves of sphericity index, long-axis length, and short-axis length
Table 4.
ROC analysis of MDCT and laboratory findings
| AUC (%) | P | Cut-off | Sensitivity (%) | Specificity (%) | PPD (%) | NPD (%) | |
|---|---|---|---|---|---|---|---|
| Long axis (mm) | 85.10 | <0.001 | 13.15 | 76.52 | 80.80 | 51.76 | 92.74 |
| Short axis (mm) | 58.60 | 0.004 | 9.35 | 73.04 | 46.60 | 26.92 | 86.52 |
| Appendix Sphericity index (ASI) | 93.90 | <0.001 | 1.30 | 80.87 | 93.21 | 76.23 | 94.76 |
| Appendicolith | 0.001 | 37.39 | 77.99 | 31.39 | 82.22 | ||
| Free fluid | <0.001 | 64.35 | 76.58 | 42.53 | 88.86 | ||
| Wall defect | <0.001 | 36.52 | 94.61 | 64.62 | 84.70 | ||
| Abscess | <0.001 | 14.78 | 98.59 | 73.91 | 81.12 | ||
| Extraluminal air | <0.001 | 5.22 | 100.00 | 100.00 | 79.66 | ||
| Ileus | 0.273 | 7.83 | 94.85 | 29.03 | 79.26 | ||
| RPS | <0.001 | 45.22 | 86.89 | 48.15 | 85.48 | ||
| WBC (103/mm3) | 51.50 | 0.613 | |||||
| CRP (mg/dL) | 58.20 | 0.008 | 1.96 | 67.26 | 25.85 | 47.09 | 83.98 |
ROC analysis: Receiver operating characteristic; MDCT: Multidetector computed tomography; RPS: Retroperitoneal space; WBC: White blood count; CRP: C-reactive protein
DISCUSSION
The most concerning complication of acute appendicitis is perforation. It can result in complications such as generalized purulent peritonitis, intra-abdominal abscess, intestinal obstruction, and sepsis.[8,9] Perforation rates range from 17% to 32% among adults and can lead to a longer hospital stay, antibiotic administration, more serious postoperative complications, and higher costs.[8,10]
Despite laboratory tests and advanced imaging techniques, the misdiagnosis of perforated acute appendicitis is still a common problem (9–20%).[11,12] According to Rao et al., the use of CT significantly reduced the rates of negative laparotomies (from 20% to 7%) and perforations (22–14%).[13] Accurate distinction between perforated vs. non-perforated appendicitis also benefits the selection process for non-surgical management. Therefore, it is very important to detect the presence of perforation in addition to the diagnosis of acute appendicitis in radiological imaging. On the other hand, guidelines do not explicitly recommend how to distinguish between uncomplicated and complicated appendicitis
US is a 75–90% successful imaging method for the diagnosis of acute appendicitis.[6] However, severe appendicitis and inconclusive ultrasonography are related, according to Pelin et al.[14] Echogenic submucosal layering, local fluid in the pericecal region, and decrease in roundness are valuable US findings in suspicion of perforation.[6] Borushok et al. evaluated a decrease in the roundness of the appendix as the ultrasonographic criterion of perforation, with a sensitivity of 59.1% and a specificity of 67.9%.[15] The prognostic significance of long and short axis measures in the differential diagnosis of perforated acute appendicitis, however, was not investigated. According to a recent meta-analysis, CT offers a high specificity, but a low sensitivity for differentiating between perforated and non-perforated appendicitis, including key features include extraluminal free air, periappendicular fluid or an abscess, and appendicolith.[5] Although the sensitivity of CT is far from perfect, it has a high negative predictive value for complicated appendicitis.[16] According to research by Gaskill et al., perforated appendicitis could only be diagnosed with a 68.9% specificity and a low sensitivity of 20.9% in the presence of appendicolitis.[17] Kim et al. found that highest sensitive finding was an appendiceal diameter of ≥11 mm (62.7%) and a focal wall defect had the highest specificity (98.8%) for perforation.[18] In another study involving 48 patients, the presence of mesenteric-pericecal lymph nodes and appendiceal wall defect were reported to be highly sensitive (88.9% and 88.5%, respectively). Although the findings of extraluminal appendicolitis, abscess, and extraluminal air were of the highest specificity (95.2%, 95%, and 95%, respectively).[19] According to Iamwat et al., a moderate-to-severe periappendiceal fat stranding and a mucosal enhancement on a CT scan can both have independent predictive value for complicated appendicitis.[20]
Despite the fact that there are numerous studies on the diagnosis of appendicitis by CT in the literature, few of them have concentrated on the differential diagnosis of perforated versus nonperforated appendicitis. Most studies point to the largest diameter of the appendix. Şirik and İnan evaluated appendix long axis, short axis, and ASI scores in 81 patients and found that long axis and ASI were predictive for perforation.[6] In our study, a larger sample was examined, and it was found that long axis and ASI are two effective parameters in predicting perforated appendicitis. While Şirik and İnan reported a cut-off value of 1.139 for ASI, the cut-off value for ASI was found to be 1.30.[6]
Aydin et al. reported that high leukocyte, neutrophil-to-lymphocyte ratio, CRP, and an appendix diameter of >11 mm indicate complicated acute appendicitis.[21] According to Kim et al., the CRP level had a stronger correlation with CT severity scores than the WBC count did.[22] Similarly, we observed increased CRP to be a predictive factor for perforation, while WBC did not have any statistical significance.
The current study had some advantages over previous research on CT findings in perforated appendicitis. The first is that we included more patients than all other relevant studies in the literature (n=542). Second, as emphasized above, we evaluated short- and long-axis lengths and the appendix sphericity index (ASI) together, and not as a single diameter of the appendix. Third, we also investigated RPS involvement on CT and biochemical acute phase parameters such as WBC and CRP. Moreover, in our study, all CT images were reported by a single, experienced radiologist with a retrospective-blinded evaluation.
The fact that US was not carried out on the patients at the time of admission is one of the study’s shortcomings. The time between CT scan and surgery was a maximum of 12 h for all patients. Still, perforation may develop within 12 h after CT, which may have affected the results of our study.
Conclusion
Appendicolith, free fluid, wall defect, abscess, free air, and RPS involvement on MDCT are significant findings for perforated appendicitis. With its high sensitivity and specificity in the diagnosis of perforated acute appendicitis, the ASI is a crucial predictive parameter.
Footnotes
Ethics Committee Approval: This study was approved by the Sancaktepe Şehit Profesör İlhan Varank Training and Research Hospital Clinical Research Ethics Committee (Date: 16.12.2020, Decision No: 2020-50
Peer-review: Externally peer-reviewed.
Authorship Contributions: Concept: Ö.A.; Design: Ö.A.; Supervision: Ö.A.; Materials: Ö.A.; Data: Ö.A.; Analysis: Ö.A.; Literature search: Ö.A.; Writing: Ö.A.; Critical revision: Ö.A.
Conflict of Interest: None declared.
Financial Disclosure: The authors declared that this study has received no financial support.
REFERENCES
- 1.Jaschinski T, Mosch C, Eikermann M, Neugebauer EA. Laparoscopic versus open appendectomy in patients with suspected appendicitis: A systematic review of meta-analyses of randomised controlled trials. BMC Gastroenterol. 2015;15:48. doi: 10.1186/s12876-015-0277-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Petroianu A. Diagnosis of acute appendicitis. Int J Surg. 2012;10:115–9. doi: 10.1016/j.ijsu.2012.02.006. [DOI] [PubMed] [Google Scholar]
- 3.Karul M, Berliner C, Keller S, Tsui TY, Yamamura J. Imaging of appendicitis in adults. Rofo. 2014;186:551–8. doi: 10.1055/s-0034-1366074. [DOI] [PubMed] [Google Scholar]
- 4.Avanesov M, Wiese NJ, Karul M, Guerreiro H, Keller S, Busch P, et al. Diagnostic prediction of complicated appendicitis by combined clinical and radiological appendicitis severity index (APSI) Eur Radiol. 2018;28:3601–10. doi: 10.1007/s00330-018-5339-9. [DOI] [PubMed] [Google Scholar]
- 5.Kim HY, Park JH, Lee YJ, Lee SS, Jeon JJ, Lee KH. Systematic review and meta-analysis of CT features for differentiating complicated and uncomplicated appendicitis. Radiology. 2018;287:104–15. doi: 10.1148/radiol.2017171260. [DOI] [PubMed] [Google Scholar]
- 6.Şirik M, İnan İ. Contribution of the appendix sphericity index in predicting perforated acute appendicitis. Ulus Travma Acil Cerrahi Derg. 2019;25:123–8. doi: 10.5505/tjtes.2018.29266. [DOI] [PubMed] [Google Scholar]
- 7.Bixby SD, Lucey BC, Soto JA, Theysohn JM, Ozonoff A, Varghese JC. Perforated versus nonperforated acute appendicitis: Accuracy of multidetector CT detection. Radiology. 2006;241:780–6. doi: 10.1148/radiol.2413051896. [DOI] [PubMed] [Google Scholar]
- 8.Mandeville K, Monuteaux M, Pottker T, Bulloch B. Effects of timing to diagnosis and appendectomy in pediatric appendicitis. Pediatr Emerg Care. 2015;31:753–8. doi: 10.1097/PEC.0000000000000596. [DOI] [PubMed] [Google Scholar]
- 9.van den Bogaard VA, Euser SM, van der Ploeg T, de Korte N, Sanders DG, Winter de D, et al. Diagnosing perforated appendicitis in pediatric patients: A new model. J Pediatr Surg. 2016;51:444–8. doi: 10.1016/j.jpedsurg.2015.10.054. [DOI] [PubMed] [Google Scholar]
- 10.Kong V, Aldous C, Handley J, Clarke D. The cost effectiveness of early management of acute appendicitis underlies the importance of curative surgical services to a primary healthcare programme. Ann R Coll Surg Engl. 2013;95:280–4. doi: 10.1308/003588413X13511609958415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tanrıkulu Y, Yılmaz G, Şen Tanrıkulu C, Temi V, Köktürk F, Çağsar M, et al. A prospective clinical study of the effects of the physical features of the appendix on perforation. Ulus Travma Acil Cerrahi Derg. 2015;21:440–5. doi: 10.5505/tjtes.2015.77508. [DOI] [PubMed] [Google Scholar]
- 12.Ekici U, Tatli F, Kanlioz M. Is the appendix length/diameter ratio an early-indicator for the perforation in acute appendicitis? Ann Med Res. 2018;25:390–3. [Google Scholar]
- 13.Rao PM, Rhea JT, Rattner DW, Venus LG, Novelline RA. Introduction of appendiceal CT: Impact on negative appendectomy and appendiceal perforation rates. Ann Surg. 1999;229:344–9. doi: 10.1097/00000658-199903000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pelin M, Paquette B, Revel L, Landecy M, Bouveresse S, Delabrousse E. Acute appendicitis: Factors associated with inconclusive ultrasound study and the need for additional computed tomography. Diagn Interv Imaging. 2018;99:809–14. doi: 10.1016/j.diii.2018.07.004. [DOI] [PubMed] [Google Scholar]
- 15.Borushok KF, Jeffrey RB, Jr, Laing FC, Townsend RR. Sonographic diagnosis of perforation in patients with acute appendicitis. AJR Am J Roentgenol. 1990;154:275–8. doi: 10.2214/ajr.154.2.2105013. [DOI] [PubMed] [Google Scholar]
- 16.Bom WJ, Bolmers MD, Gans SL, Rossem van CC, Geloven van AA, Bossuyt PM, et al. Discriminating complicated from uncomplicated appendicitis by ultrasound imaging, computed tomography or magnetic resonance imaging: Systematic review and meta-analysis of diagnostic accuracy. BJS Open. 2021;5:zraa030. doi: 10.1093/bjsopen/zraa030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gaskill CE, Simianu VV, Carnell J, Hippe DS, Bhargava P, Flum DR, et al. Use of computed tomography to determine perforation in patients with acute appendicitis. Curr Probl Diagn Radiol. 2018;47:6–9. doi: 10.1067/j.cpradiol.2016.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kim MS, Park HW, Park JY, Park HJ, Lee SY, Hong HP, et al. Differentiation of early perforated from nonperforated appendicitis: MDCT findings, MDCT diagnostic performance, and clinical outcome. Abdom Imaging. 2014;39:459–66. doi: 10.1007/s00261-014-0117-x. [DOI] [PubMed] [Google Scholar]
- 19.Suthikeeree W, Lertdomrongdej L, Charoensak A. Diagnostic performance of CT findings in differentiation of perforated from nonperforated appendicitis. J Med Assoc Thai. 2010;93:1422–9. [PubMed] [Google Scholar]
- 20.Iamwat J, Teerasamit W, Apisarnthanarak P, Noppakunsomboon N, Kaewlai R. Predictive ability of CT findings in the differentiation of complicated and uncomplicated appendicitis: A retrospective investigation of 201 patients undergone appendectomy at initial admission. Insights Imaging. 2021;12:143. doi: 10.1186/s13244-021-01086-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Aydin OU, Soylu L, Dandin O, Aydin EU, Karademir S. Laboratory in complicated appendicitis prediction and predictive value of monitoring. Bratisl Lek Listy. 2016;117:697–701. doi: 10.4149/BLL_2016_132. [DOI] [PubMed] [Google Scholar]
- 22.Kim HC, Yang DM, Lee CM, Jin W, Nam DH, Song JY, et al. Acute appendicitis: Relationships between CT-determined severities and serum white blood cell counts and C-reactive protein levels. Br J Radiol. 2011;84:1115–20. doi: 10.1259/bjr/47699219. [DOI] [PMC free article] [PubMed] [Google Scholar]


