Abstract
Aim
The aim of the study was to identify interventions to promote mobility that has an impact on the quality of life of people living in nursing homes and assisted living facilities.
Design
The design of the study was a systematic review.
Methods
The search was performed in September 2021 in the databases PubMed, Epistemonikos and the Cochrane Library for studies published between 2010 and 2021 in the German or English language.
Results
Four studies identified improvements in mobility and quality of life. Nine of the ten included studies showed impacts of the interventions on different mobility variables. Heterogeneous variables and instruments were used to assess quality of life and, in particular, mobility, which made it difficult to compare the results of the studies. Approximately 50% of the identified studies had small sample sizes.
Keywords: assisted living, intervention, mobility, nursing home, quality of life
1. INTRODUCTION
The loss of mobility causes the need for care (Wingenfeld et al., 2020). Factors such as older age and underlying pathologies increase the risk of loss of mobility (Rantakokko et al., 2013). Most nursing home residents experience medical, functional and cognitive impairments and physical inactivity (Powell et al., 2016). People with cognitive dysfunctions are affected by loss of mobility much more frequently than people with little or no existing cognitive dysfunction (Kleina et al., 2012; Sverdrup et al., 2018). Immobility can be seen as a major factor in reduced quality of life and cost‐intensive hospital stays (Groessl et al., 2019; Larsson et al., 2018).
The importance of the issue of mobility loss implies the need for an up‐to‐date overview of effective interventions to promote mobility and increase quality of life.
The aim of this systematic review is to identify interventions that promote mobility and quality of life. The research question is as follows: Which interventions to promote mobility have a positive effect on the quality of life of residents in nursing homes and assisted living facilities?
1.1. Mobility
There are different definitions and understandings of mobility that are used in health and nursing science. In some studies, mobility is operationalized, for example as the ability to walk or more advanced abilities to move (Kleina, 2014). For example, mobility has been defined as physical movement and the ability to control it, including simple gross motor movements as well as complex fine motor movements (Crawford & Harris, 2016). In this context, mobility is understood as a multidimensional construct. Physical, cognitive, emotional and social components are interdependent and manifest as functional mobility (physical and mental disposition) and physical, psychological and social activities (Strupeit & Buss, 2014). The meaning of mobility to individuals is reflected in individual self‐concepts, strategies, goals, needs and motives (ibid.). Based on this definition, mobility impairment is seen as a limitation of independent and targeted physical, psychological, emotional and social mobility (ibid.). Mobility support interventions are understood in this context as conscious actions aimed at changing behaviour, reducing risk or improving a particular outcome (Schillinger, 2010).
1.2. Quality of life
An increasing number of surveys measuring quality of life have been theoretically based on a more resource‐oriented model despite a deficit‐oriented model (Conrad & Riedel‐Heller, 2016). Accordingly, not only health and functionality but also economic and social aspects, as well as subjective perceptions of one's state of health, are included in the concept of quality of life (ibid.). For the present review, the most popular definition of quality of life was chosen: ‘… an individual's perception of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards and concerns. It is a broad concept of how people live, including physical health, psychological state, level of independence, social relationships, and their relationship to salient features of their environment’ (WHO, 1993). La Grow et al. (2013) show that mobility is significantly associated with quality of life. Shafrin et al. (2017) investigated the mobility and quality of life of people aged 50–69 years and proved that better observed mobility is associated with higher self‐reported quality of life.
2. METHODS
2.1. Analysis
The method used to perform the systematic review was based on the ‘CRD's guidance for undertaking reviews in health care’ published by the Centre for Reviews and Dissemination. In this case, we established the background of the review, the research question and the inclusion criteria and described them according to the PICOS elements (CRD, 2009). After the database search, we chose which studies would be included in two stages. In stage 1, the titles and abstracts were screened and compared to the inclusion criteria. In the second stage, the remaining full‐text articles were reviewed to check which of them met the inclusion criteria (Table 1).
TABLE 1.
Inclusion criteria.
| PICOS elements | |
|---|---|
| Population | People aged 55 years and older |
| Nursing homes | |
| Assisted living facilities | |
| Interventions and comparators | interventions to promote mobility |
| interventions for fall prevention | |
| Outcomes | mobility and quality of life |
| Study design | no limitations |
2.2. Eligibility criteria
The inclusion criteria were formulated according to the PICOS elements as follows. All studies examining interventions to promote mobility in inpatient care were included. At the beginning of the review, we found a limited number of studies. To expand the research area, studies with interventions for fall prevention were also included since interventions for fall prevention and mobility promotion have similar foci. Since 7% of the people in assisted living facilities are under 65 years old (AHCA & NCAL, 2022), we added the age group 60–64 years and 55–59 years in our analysis. Studies were included if they focused on a sample of people aged 55 years and older who were living in nursing homes or assisted living facilities. Studies had to include mobility and quality of life as outcome variables to be included. Furthermore, a date of publication from January 2010 to September 2021 and a publication language of English and German were eligibility criteria. We chose the 10 year period because it ensures the analysis of current material and also does justice to a long‐term publication process (Helfer et al., 2015). There were no limitations to the study design or publication type or status.
2.3. Information sources
In September 2021, the databases MEDLINE (via PubMed) and Epistemonikos (Cochrane Database of Systematic Reviews (CDSR), PubMed, EMBASE, CINAHL, PsycINFO, LILACS, Database of Abstracts of Reviews of Effects (DARE), The Campbell Collaboration online library, JBI Database of Systematic Reviews and Implementation Reports and EPPI‐Centre Evidence Library) were searched. Because Epistemonikos searches only titles and abstracts, an additional search on EMBASE (via Cochrane Library) was performed. These databases were selected because they are the most common databases for nursing research.
2.4. Search
To answer our research question, we analysed databases with the following terms: mobility AND interventions AND quality of life. A combination of the individual search terms with the Boolean operator AND was an appropriate strategy for the identification of the relevant literature. The year limitation was set from 2010 to 2021. The first step of the selection of relevant studies was the screening of titles and abstracts. In this step, all studies that did not meet the inclusion criteria or that addressed the mobility of individual body parts rather than treating mobility as a status affecting the whole body (and that thus contradicted our definition of mobility) were excluded. We also excluded studies examining specific populations with regard to a specific disease. In the second step, the articles were screened in a more detailed way. In this step, all studies that did not analyse quality of life as an outcome variable or that did not address the setting or population defined in the inclusion criteria were excluded. Finally, 10 studies were included in the review. Five studies were randomized controlled trials (RCTs), two studies were cluster RCTs, two studies had a pretest–posttest design and one study was a quasi‐experimental longitudinal study.
2.5. Data collection process
The data were collected by two different reviewers independently. To present and summarize the evidence, information on the type of intervention, data collection, population, sample size, setting and measure was extracted. We decided to present the risk of bias in a table, as this is the most convenient format to present this information (Hutton et al., 2015). To assess the quality of the RCTs and the risk of bias, information on the concealment of the allocation sequence, blinding, dropout (loss to follow‐up, defined as less than 20% attrition), characteristics of the participant groups at baseline, the analysis of the participants according to the original groups to which they were assigned and sample size calculation (Liberati et al., 2009) was collected. Aspects that were reported, performed or fulfilled were marked with a ‘+’, aspects that were not reported were indicated with a ‘?’ and aspects that were not fulfilled or not performed were marked with a ‘‐’. To assess the quality of the non‐randomized controlled studies, we used the Mixed Methods Appraisal Tool (MMAT), version 2018 (Hong et al., 2018) (Table 2). The results of the included studies, including the effect size, the confidence interval and the effect of the intervention, are presented.
TABLE 2.
Risk of bias.
| Study | Study design | Concealment of allocation sequence | Blinding | Loss to follow‐up (<20%) | Characteristics of the participant groups at baseline | Participants analysed according to their original groups | Sample size calculation |
|---|---|---|---|---|---|---|---|
|
Álvarez‐Barbosa et al. (2014) |
RCT |
+ |
+ |
+ |
+ |
+ |
− |
|
Lobo et al. (2010) |
RCT |
+ |
−/? |
+ 20% 1 year follow‐up – 15 month follow‐up |
+ |
+ |
− |
|
Quehenberger et al. (2014) |
RCT |
+ |
−/? |
− |
? |
? |
− |
|
Özyemişci‐Taşkiran et al. (2014) |
RCT |
+ |
−/? |
− |
+ |
? |
− |
|
Rezola‐Pardo et al. (2020) |
Single, blind RCT |
+ |
+ |
+ total − multicomponent group |
− |
? |
+ |
|
Hewitt et al. (2018) |
Cluster RCT |
+ |
+ |
+ |
+ |
+ |
+ |
|
Stanmore et al. (2019) |
Cluster RCT |
+ |
+ |
+ |
+ |
+ |
+ |
| + | Reported/fulfilled/performed |
|---|---|
| ? | not reported |
| − | not fulfilled/not performed |
| Study | Study design | Clear research questions | Data collection addresses to research question | Participants representative of target population | Measurements appropriate about the outcome and intervention | Complete outcome data | Confounders accounted for in the design and analysis | Intervention administered as intended |
|---|---|---|---|---|---|---|---|---|
|
Bell et al. (2011) |
Pretest–posttest design |
+ |
+ |
+ |
+ |
+ |
‐ |
+ |
|
Krist et al. (2013) |
Pretest–posttest design |
+ |
+ |
+ |
+ |
‐ |
? |
+ |
|
Mouton et al. (2017) |
Quasi‐experimental longitudinal study |
+ |
+ |
+ |
+ |
+ |
? |
+ |
| + | Yes |
|---|---|
| ? | Cannot tell |
| − | No |
3. RESULTS
3.1. Study selection
The search strategy of the review is shown in Figure 1. Searching with the described search terms led to a result of 7048 records. After the titles and abstracts were screened, 20 articles remained for the full‐text screening. Finally, 10 studies were included in the systematic review. Table 3 gives an overview of the characteristics of the studies.
FIGURE 1.
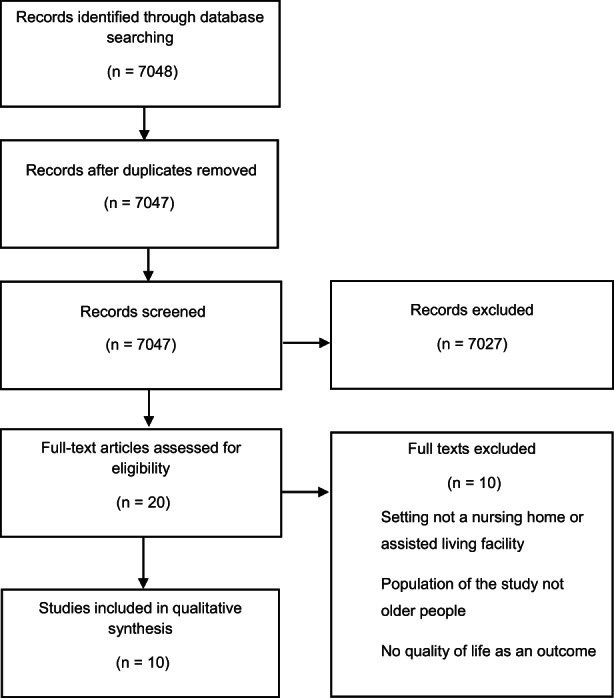
Search strategy.
TABLE 3.
Study characteristics.
| Reference | Intervention | Data collection | Population | Sample size (n) | Setting | Analysis | Measure |
|---|---|---|---|---|---|---|---|
| Álvarez‐Barbosa et al. (2014) | whole‐body vibration (WBV) therapy | baseline 8 weeks (follow‐up) | nursing home residents 80+ | n = 29intervention group n = 15control group n = 14 | nursing home |
Shapiro–Wilk test Mann–Whitney U test chi‐square analysis Wilcoxon test Friedman test |
functional mobility: Timed Up and Go test (TUG) lower limb performance: 30‐s Chair Sit‐to‐Stand test (30‐s CSTS) postural stability: force platform functional dependence: Barthel Index health‐related quality of life: EuroQol (EQ‐5D) |
| Bell et al. (2011) | Nintendo Wii bowling | baseline 8 weeks (completion of intervention) | people aged 65 years and older | n = 21 | assisted living |
Wilcoxon signed‐rank test Repeated‐measures analysis of variance (ANOVA) nonparametric statistical methods |
quality of life: Pleasure subscale of the Control, Autonomy, Self‐Realization and Pleasure‐19 (CASP‐19) social relationship and social support: Social Provisions Scale (SPA) Modified Falls Efficacy Scale (M‐FES) |
| Hewitt et al. (2018) | progressive resistance (sunbeam programme) and balance training | baseline 6 months 12 months (follow‐up Please clarify the meaning of the phrase, “baseline 6 months 12 months” in table 2.") | residents of elder care facilities | n = 221 | elder care facilities |
negative binomial regression linear regression models Hedges' postestimation of Cohen's d |
rate of falls physical performance: short physical performance battery quality of life: 36‐item Short‐Form Health Survey functional mobility: the University of Alabama Life Space Assessment of fear of falling: Falls Efficacy Scale International cognition: Addenbrooke's Cognitive Evaluation – Revisited (ACE) |
| Krist et al. (2013) | progressive resistance training | baseline 8 weeks (follow‐up) | very elder people | n = 15 | nursing home |
Wilcoxon signed‐rank test |
mobility: Elderly Mobility Scale muscle strength: eight repetitions maximum quality of life: 36‐item Short‐Form Health Survey |
| Lobo et al. (2010) | aerobic exercise strength training health education |
Baseline 3 months (follow‐up) 1 year |
institutionalized elder people | n = 185 aerobic exercise n = 49 strength training n = 37 health education n = 52 control group n = 47 | nursing home |
Shapiro–Wilk test one‐way analysis of variance Scheffe's post hoc comparisons multivariate analyses of variance |
quality of life: MOS SF‐36 physical fitness: Functional Fitness Test physical activity: MIT ActiGraph biochemical analysis of blood, blood pressure and bioimpedance |
| Mouton et al. (2017) | exercise intervention with a very large game board | baseline postintervention 3 months (follow‐up) | nursing home residents |
n = 21 intervention group = 10 control group = 11 |
nursing home |
Shapiro–Wilk test one‐way analysis of variance (ANOVA) one‐way ANOVAs with repeated measures Bonferroni correction Kruskal–Wallis test Wilcoxon test chi‐square test mean ± standard deviation median percentiles absolute and relative frequencies |
physical activity: steps/day and energy expenditure/day with ActiGraph cognitive status: Mini‐mental State Examination (MMSE) quality of life: EQ‐5D motivation for physical activity: Behavioural Regulation in Exercise Questionnaire‐2 gait and balance: Tinetti and Short Physical Performance Battery functional mobility: TUG lower limb muscles: muscular isometric strength |
| Özyemişci‐Taşkiran et al. (2014) | Pilates and yoga | Baseline 8 weeks (postintervention) 6 months (follow‐up) | elder people | n = 36intervention group n = 36control group n = 22 | nursing home |
Shapiro–Wilk's test Analysis of variance (ANOVA) Kruskal–Wallis test Tukey or Mann–Whitney U test chi‐square or Fisher's exact tests Wilcoxon or paired T tests |
physical activity level: Turkish version of the International Physical Activity Questionnaire (IPAQ) short‐form cognitive performance: Turkish version of the MMSE health‐related quality of life: Turkish version of Nottingham Health Profile (NHP) multidimensional pain: Geriatric Pain Measure (GPM) |
| Quehenberger et al. (2014) | low‐threshold physical activity intervention | 1 year (follow‐up) | residents of residential elder care | study: n = 222 intervention group n = 104 control group n = 118 follow‐up: n = 68 | residential elder care |
T test chi‐squared test general mixed linear models Friedman tests paired t‐ and Wilcoxon signed‐rank tests |
study: subjective health status: EQ‐5D occupational performance: Canadian Occupational Performance Measure (COPM) functional health: TUG follow‐up: health‐related quality of life: EQ‐5D |
| Rezola‐Pardo et al. (2020) Reference 'ezola‐Pardo et al. 2019' year 2019 has been changed to 2020 to match the reference list. Please check for correctness." | multicomponent exercise vs. walking interventions |
baseline after the 12 week intervention |
nursing home residents |
n = 81 multicomponent group n = 41 walking group n = 40 follow‐up n = 65 |
nursing home |
Shapiro–Wilk test t test chi‐squared test two‐way analysis of variance for repeated measures partial η 2 Cohen's d |
lower limb strength, static balance and usual gait speed: Short physical performance battery physical performance: Senior Fitness Test, Berg Balance Scale (BBS), TUG habitual physical activity: tri‐axial accelerometers global cognitive function: Montreal Cognitive Assessment Test verbal memory: Rey Auditory Verbal Learning Test affective function: Goldberg Anxiety and Depression Scale perceived quality of life: Quality of Life Alzheimer's Disease scale loneliness: de Jong‐Gierveld loneliness scale |
| Stanmore et al. (2019) | strength and balance exergames (active, gamified video‐based exercises) |
BBS, TUG, Fall Risk Assessment Tool (FRAT), Physical Activity Scale for the Elderly (PASE), Addenbrooke's Cognitive Examination III (ACEIII), Short Falls Efficiency Scale‐I (Short FES‐I), 5‐item Geriatric Depression Scale (GDS), health‐related quality of life (HRQoL), EuroQoL (EQ‐5D‐5L): baseline12 week, fall diary: daily self‐report, monthly for 3 months adherence: at each use of the exergames monetary costs: daily self‐report calendar, monthly for 3 months follow‐up phone calls System Usability Scale (SUS) + Technology Assessment Model (TAM):12 weeks (intervention group)12 week follow‐up |
people aged 55 years and older | n = 106 intervention group n = 56 control group n = 50 | assisted living |
case analysis linear regression linear mixed effects modelling Mantel–Haenszel methods |
balance: BBS falls: falls diary adherence: frequency, duration, number of sessions TUG FRAT, including pain VAS and fatigue VAS PASE ACEIII Short FES‐I5‐item GDS HRQoL, EuroQoL EQ‐5D‐5L monetary costs of health care utilization following falls usability and acceptance of exergames (SUS and TAM) |
3.2. Interventions
Two studies investigated the use of progressive resistance training (Hewitt et al., 2018; Krist et al., 2013). Hewitt et al. (2018) studied balance training combined with progressive resistance training with two follow‐ups at 6 and 12 months. Another two studies examined video games as an intervention in assisted living. Bell et al. (2011) used Nintendo Wii Bowling, and Stanmore et al. (2019) investigated strength and balance exergames in assisted living. Álvarez‐Barbosa et al. (2014) evaluated whole‐body vibration therapy in people aged 80 years and older. Lobo et al. (2010) investigated the effect of a combined intervention consisting of aerobic exercise, strength training and health education with two follow‐ups at 3 and 12 months. One study employed exercises with a very large game board in nursing homes (Mouton et al., 2017), and another study investigated the effect of Pilates and yoga in residential aged care (Özyemişci‐Taşkiran et al., 2014). Quehenberger et al. (2014) investigated the effect of a low‐threshold physical activity intervention on mobility and quality of life. One study compared multicomponent exercise including strength and balance exercises to walking programmes in long‐term nursing homes (Rezola‐Pardo et al., 2020).
3.3. Population and setting
Álvarez‐Barbosa et al. (2014) focused on a sample of nursing home residents aged 80 years and older. Mouton et al. (2017), Hewitt et al. (2018), Rezola‐Pardo et al. (2020) and Lobo et al. (2010) examined nursing home residents. Özyemişci‐Taşkiran et al. (2014) included a sample of elder individuals in their study. Bell et al. (2011) examined a sample of people aged 65 years and older, and Stanmore et al. (2019) examined a sample of people aged 55 years and older. Four of the studies had sample sizes ranging from 106 to 222 participants (Hewitt et al., 2018; Lobo et al., 2010; Quehenberger et al., 2014; Stanmore et al., 2019). One study had a sample size of 81 participants (Rezola‐Pardo et al., 2020). The other included studies had sample sizes between 15 and 36 participants (Álvarez‐Barbosa et al., 2014; Bell et al., 2011; Krist et al., 2013; Mouton et al., 2017; Özyemişci‐Taşkiran et al., 2014). Eight of the ten studies were conducted in nursing homes, and two studies were conducted in assisted living facilities.
3.4. Measurements
The authors of the studies use heterogeneous instruments to assess quality of life and mobility. Four of the ten studies assessed health‐related quality of life, and six studies measured quality of life in general. Álvarez‐Barbosa et al. (2014), Mouton et al. (2017), Quehenberger et al. (2014) and Stanmore et al. (2019) used the EuroQol‐5 Dimension Questionnaire (EQ‐5D) to assess health‐related quality of life. Hewitt et al. (2018), Lobo et al. (2010) and Krist et al. (2013) used the 36‐item Short‐Form Health Survey (MOSS SF‐36). One author employed dementia‐specific instruments for the measurement of quality of life, including the Quality of Life Alzheimer's Disease Scale (Rezola‐Pardo et al., 2020). Other authors used different instruments, such as the Turkish version of the Nottingham Health Profile (NHP) (Özyemişci‐Taşkiran et al., 2014) and the Pleasure subscale of the Control, Autonomy, Self‐Realization and Pleasure‐19 (CASP‐19) (Bell et al., 2011). To measure mobility, different instruments and variables, which are shown in Table 3, were used.
3.5. Follow‐up
The follow‐up periods differed between the studies. Three studies performed two follow‐ups at different times: Hewitt et al. (2018) after 6 and 12 months; Lobo et al. (2010) after 3 and 12 months and Özyemişci‐Taşkiran et al. (2014) after 8 weeks and 6 months. Álvarez‐Barbosa et al. (2014), Krist et al. (2013) and Bell et al. (2011) each performed a follow‐up study after 8 weeks. Stanmore et al. (2019) conducted a follow‐up after 12 weeks, Mouton et al. (2017) conducted a follow‐up after 3 months and Quehenberger et al. (2014) performed a follow‐up study 12 months after the intervention. Two studies ended with data collection after the end of the intervention period (Bell et al., 2011; Rezola‐Pardo et al., 2020).
3.6. Risk of bias
The risk of bias and the methodological quality of the studies are summarized in Table 2. All seven RCTs (RCT, cluster RCT) report the concealment of the allocation sequence. Four studies described the blinding process (Álvarez‐Barbosa et al., 2014; Hewitt et al., 2018; Rezola‐Pardo et al., 2020; Stanmore et al., 2019). Five studies described a loss to follow‐up of less than 20% (Álvarez‐Barbosa et al., 2014; Hewitt et al., 2018; Rezola‐Pardo et al., 2020; Stanmore et al., 2019). Lobo et al. (2010) reported a loss to follow‐up of less than 20% after 1 year and 4 months, respectively, and more than 20% after 15 and 12 months respectively. Five of the seven studies described the characteristics of the participant groups at baseline, and four studies stated that the participants were analysed according to the original groups to which they were assigned (Álvarez‐Barbosa et al., 2014; Hewitt et al., 2018; Lobo et al., 2010; Stanmore et al., 2019). Four authors (Hewitt et al., 2018; Krist et al., 2013; Rezola‐Pardo et al., 2020; Stanmore et al., 2019) performed a sample size calculation for the study.
3.7. Analysis
Different analyses were conducted in the studies. Six of the ten studies used the Wilcoxon test to analyse and compare the outcome data between different data collection points and within and between different samples (Álvarez‐Barbosa et al., 2014; Bell et al., 2011; Krist et al., 2013; Mouton et al., 2017; Özyemişci‐Taşkiran et al., 2014; Quehenberger et al., 2014). Five studies used the chi‐square test to analyse the differences between different participant groups (Álvarez‐Barbosa et al., 2014; Mouton et al., 2017; Özyemişci‐Taşkiran et al., 2014; Quehenberger et al., 2014; Rezola‐Pardo et al., 2020). Lobo et al. (2010), Álvarez‐Barbosa et al. (2014), Mouton et al. (2017), Rezola‐Pardo et al. (2020) and Özyemişci‐Taşkiran et al. (2014) used the Shapiro–Wilk test to examine the distribution of data. Lobo et al. (2010), Mouton et al. (2017), Bell et al. (2011), Rezola‐Pardo et al. (2020) and Özyemişci‐Taşkiran et al. (2014) used variance analyses (one‐way or multivariate) to examine the differences in the pre‐ and postintervention groups and the differences between these groups between the different points of data collection. The different tests and methods used in the data analyses of the different studies are shown in Table 3.
3.8. Results of the studies
Table 4 shows the effects of the interventions of the included studies, including the effects of whole‐body vibration (WBV) on performance for the different mobility variables, peak power and number of repetitions, activities of daily living and an increase in health‐related quality of life (Álvarez‐Barbosa et al., 2014). Aerobic and strength training had an effect on physical activity and cardiovascular variables. Strength training increased lower and upper body strength, aerobic endurance and lower and upper body flexibility. Aerobic training improved aerobic endurance, lower‐body strength and agility and affected the body mass index (Lobo et al., 2010). There was no significant effect of aerobic training and strength training on health‐related quality of life (Lobo et al., 2010). A low‐threshold physical activity intervention had no significant effect on health‐related quality of life, but it affected subjective health status and reduced the participants' reported pain and discomfort from baseline to the 1 year follow‐up (Quehenberger et al., 2014). Additionally, Hewitt et al. (2018) showed an effect of progressive resistance and balance training on reducing the rate of falls and increasing physical performance, but there was no effect on quality of life. Krist et al. (2013) examined progressive resistance training and showed an increase in mobility, number of sit‐up repetitions and muscle strength but no effect on quality of life. The use of exergames reduced fear of falling and pain and improved balance but had no effect on quality of life (Stanmore et al., 2019). According to Rezola‐Pardo et al. (2020), there was a significant improvement in different aspects of mobility after the performance of multicomponent training, including strength and balance exercises. Multicomponent and walking exercises also affected quality of life and reduced anxiety (Rezola‐Pardo et al., 2020). Bell et al. (2011) could not prove any effect of using Nintendo Wii Bowling as an intervention for improving mobility and quality of life. Mouton et al. (2017) investigated an exercise intervention using a very large game board and observed an increase in physical activity and energy expenditure. After 3 months, the participants' quality of life and balance gait and ankle strength increased (ibid.). Yoga influenced quality of life, sleep quality, strength and flexibility. After 6 months, none of these effects persisted (Özyemişci‐Taşkiran et al., 2014).
TABLE 4.
Effects of interventions.
| Study | Effect size | Confidence interval | Effect of intervention |
|---|---|---|---|
|
Álvarez‐Barbosa et al. (2014) |
mobility and lower limb performance; TUG (p = <0.001), 30 s‐CSTS (p = 0.006) | 95% |
Increase in performance increases in peak power, number of repetitions |
| HRQoL (EQ‐5D) mobility (p < 0.001), EQ‐5D utility (p < 0.001), EQ‐5DVAS (p = 0.014) | increase in HRQoL | ||
| Barthel Index (p = 0.003) | increase in ADL | ||
| postural stability (p > 0.05) | no significant effect | ||
| Rezola‐Pardo et al. (2020) |
multicomponent group: short physical performance battery (p < 0.01) gait speed test (p < 0.01) chair stand (p < 0.001) arm curl (p < 0.001) Timed up and Go Test (TUG) (p < 0.05) Berg Balance Scale (BBS) (p < 0.05) |
95% |
improvement improvement improvement improvement improvement improvement |
|
walking group: short physical performance battery gait speed test chair stand arm curl TUG BBS |
no significant effect no significant effect no significant effect no significant effect no significant effect no significant effect |
||
|
Both groups Goldberg Anxiety and Depression Scale (p < 0.05) Quality of Life Alzheimer's Disease Scale (p < 0.01) Rey Auditory Verbal Learning Test Montreal Cognitive Assessment test de Jong‐Gierveld loneliness scale |
reduction in anxiety increase in quality of life no significant effect no significant effect no significant effect |
||
|
Lobo et al. (2010) |
aerobic training, strength training (p < 0.05) health education |
95% |
Increase in physical activity (vs. control group and vs. baseline) increase in cardiovascular variables no significant effect |
| aerobic training, strength training, health education HRQoL | no significant effect | ||
| strength training (p < 0.05) | increase in the following: lower body strength (vs. baseline; vs. after intervention), upper body strength (vs. baseline; vs. after intervention), aerobic endurance (vs. control group), lower body flexibility (vs. baseline; vs. after intervention), upper body flexibility (vs. baseline), agility/dynamic balance | ||
| aerobic training (p < 0.05) | improvement in aerobic endurance (vs. baseline, control group), lower body strength (vs. control group, baseline, HE), agility/dynamic balance (vs. control group, HE, baseline, after intervention), BMI (vs. control group HE) | ||
| health education | no significant effect | ||
|
Quehenberger et al. (2014) |
1 year follow‐up |
||
| HRQoL (EQ‐5D) | N/A | no significant effect | |
| p = 0.02 | subjective health status (vs. baseline) | ||
| p = 0.047 | reduction in reported pain and discomfort (baseline to follow‐up) | ||
| p = 0.26 | reported problems with pain and discomfort, no significant effect (intervention period) | ||
|
Hewitt et al. (2018) |
incidence rate ratio = 0.45 | 95% | reduction in the rate of falls |
| p = 0.02 | increase in physical performance | ||
| QoL, cognition | no significant effect | ||
|
Stanmore et al. (2019) |
p = 0.007 | 95% | reduction in fear of falling |
| p = 0.02 | reduction in pain | ||
| p = 0.003 | positive impact on balance | ||
| QoL | no significant effect | ||
|
Krist et al. (2013) |
p = 0.005 | 95% | increase in mobility |
| p = 0,027 | increase in number of sit‐up repetitions | ||
| p < or = 0,008 | increase in muscle strength | ||
| QoL (p = 0,29) | no significant effect | ||
| physical functioning (p = 0.54) | no significant effect | ||
| Bell et al. (2011) | very limited and sporadic in Control, Autonomy, Self‐Realization and Pleasure‐19 (CASP‐19), Social Provisions Scale (SPA), Modified Falls Efficacy Scale (M‐FES) | 95% | no significant effect |
|
Mouton et al. (2017) |
p = 0.04 after intervention, p = 0.03 after 3 months | 95% | increase in physical activity |
| p = 0.01 after intervention, p = 0.02 after 3 months | increase in energy expenditure/day | ||
| p < 0.05 after 3 months | increases in QoL, balance and gait, ankle strength | ||
|
Özyemişci‐Taşkiran et al. (2014) |
p = 0.026 (subcategory QoL) | 95% | decrease in sleep problems (increase in sleep quality) (yoga) |
| p = 0.037 (subcategory QoL) | decrease in emotional reaction (yoga) | ||
| p = 0.017 | increase in hand grip strength (yoga) | ||
| p = 0.019 | increase in sit and reach performance (yoga) | ||
| after 6 months | no persistent effect | ||
Note: The bold term quality of life results refers the bold values in the table. The mobility results are the other values in the table.
3.9. Synthesis of the results
Only three studies showed an increase in quality of life (Mouton et al., 2017; Özyemişci‐Taşkiran et al., 2014; Rezola‐Pardo et al., 2020), and one study showed an increase in health‐related quality of life (Álvarez‐Barbosa et al., 2014). Only the studies by Álvarez‐Barbosa et al. (2014), Lobo et al. (2010), Özyemişci‐Taşkiran et al. (2014), Quehenberger et al. (2014) and Rezola‐Pardo et al. (2020) were RCTs. Mouton et al. (2017) chose a quasi‐experimental design for their study because of the small sample size. Notably, the positive effect on quality of life was measured with only two subscales of the instrument used. Seven studies could not prove an effect of the intervention on mobility and quality of life, while Bell et al. (2011) were able to show such an effect. In this study, a very sporadic effect of Nintendo Wii Bowling in assisted living facilities could be shown. Nine of the included studies showed that an intervention could increase different mobility parameters in nursing homes and among the population of people 55 years and older. For example, whole‐body vibration therapy (Álvarez‐Barbosa et al., 2014), progressive resistance training (Hewitt et al., 2018; Krist et al., 2013), balance training (Hewitt et al., 2018), multicomponent combining strength and balance exercise (Rezola‐Pardo et al., 2020), aerobic exercise and strength training (Lobo et al., 2010), an exercise intervention using a large game board (Mouton et al., 2017), low‐threshold physical activity intervention (Quehenberger et al., 2014) and strength and balance exergames (Stanmore et al., 2019) should be administered. There was also a positive effect of yoga on hand grip strength, sitting and reaching ability and sleep quality. However, the effects were not stable over follow‐up measurements (Özyemişci‐Taşkiran et al., 2014).
4. DISCUSSION
The aim of the study was to identify studies that focused on interventions to improve the mobility and quality of life of residents in nursing homes. We found 10 studies with this aim published from 2010 to 2021. Five of the studies were RCTs and two other studies were cluster RCTs. Our results indicate that multiple interventions had impacts on different mobility variables. Only four studies described an increase in quality of life as an outcome. Among these studies, three had the quality of an RCT.
4.1. Interventions
A large variety of instruments and variables were used to measure the mobility of the populations included in the studies, such as physical activity performance, balance and muscle strength. Only one study used the Barthel index to assess activities of daily living (Álvarez‐Barbosa et al., 2014). Additionally, increased quality of life was measured with six different instruments, which makes it difficult to compare the results.
4.2. Limitations
Our systematic review has limitations. The use of three different databases might have limited the results to the papers listed in these databases. Additionally, the fixed period of 10 years limited the results. Because there were no additional searches in other databases or hand searches, the search results might be incomplete. We used a narrowed search strategy, which involved a risk of relevant studies, for example those excluded because they addressed specific illnesses or specific needs, such as those of people with dementia, not being included. This procedure was necessary because we wanted to focus on the constructs of mobility and quality of life in general and not on an even more specific population than people living in nursing homes.
4.3. Conclusion
The results of our review indicate that there are multiple interventions that have an effect on mobility but mostly no effect on the quality of life of people living in nursing homes or assisted living facilities. The results also show that the outcomes are hardly comparable because of the large variety of instruments and variables used to measure mobility and quality of life. The small sample sizes of some of the studies allowed only low levels of significance of the results.
4.4. Implications for further research
A problematic issue is the variety of measures used in the studies, which makes it difficult to compare the results of the studies. Further studies on the topic of mobility should use validated measurement instruments and frequently used definitions of mobility and should aim to replicate previous studies. Furthermore, most of the included studies had a small number of participants. Further studies should focus on the link between the improvement of mobility and quality of life. Furthermore, the reason why an increase in different mobility variables does not lead to an increase in quality of life must be investigated.
FUNDING INFORMATION
This research did not receive any specific grant from funding agencies in the public, commercial or not‐for‐profit sectors.
CONFLICT OF INTEREST STATEMENT
The authors declare that there are no conflicts of interest.
ETHICAL APPROVAL
This systematic review did not require ethical approval.
ACKNOWLEDGEMENTS
None. Open Access funding enabled and organized by Projekt DEAL.
Bohn, B. , & Strupeit, S. (2023). Interventions to promote mobility and quality of life in nursing homes: A systematic review. Nursing Open, 10, 4172–4184. 10.1002/nop2.1673
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no new data were created or analyzed in this study.
REFERENCES
- AHCA & NCAL . (2022). Facts and Figures. Residents. Retrieved from https://www.ahcancal.org/Assisted‐Living/Facts‐and‐Figures/Pages/default.aspx
- Álvarez‐Barbosa, F. , del Pozo‐Cruz, J. , del Pozo‐Cruz, B. , Alfonso‐Rosa, R. M. , Rogers, M. E. , & Zhang, Y. (2014). Effects of supervised whole body vibration exercise on fall risk factors, functional dependence and health‐related quality of life in nursing home residents aged 80+. Maturitas, 79, 456–463. 10.1016/j.maturitas.2014.09.010 [DOI] [PubMed] [Google Scholar]
- Bell, C. S. , Fain, E. , Daub, J. , Warren, S. H. , Howell, S. H. , Southard, K. S. , Sellers, C. , & Shadoin, H. (2011). Effects of Nintendo Wii on quality of life, social relationships, and confidence to prevent falls. Physical & Occupational Therapy in Geriatrics, 29(3), 213–221. 10.3109/02703181.2011.559307 [DOI] [Google Scholar]
- Centre for Reviews and Dissemination (CRD) . (2009). Systematic reviews. CRD's guidance for undertaking reviews in health care. York Publishing Services. Retrieved from. https://www.york.ac.uk/media/crd/Systematic_Reviews.pdf [Google Scholar]
- Conrad, I. , & Riedel‐Heller, S. G. (2016). Lebensqualität im Alter. In Müller S. V. & Gärtner C. (Eds.), Lebensqualität im Alter. Perspektiven für Menschen mit geistiger Behinderung und psychischen Erkrankungen (pp. 39–51). Springer Fachmedien. [Google Scholar]
- Crawford, A. , & Harris, H. (2016). Caring for adults with impaired physical mobility. Nursing, 46(12), 36–41. 10.1097/01.NURSE.0000504674.19099 [DOI] [PubMed] [Google Scholar]
- Groessl, E. J. , Kaplan, R. M. , Rejeski, W. J. , Katula, J. A. , Glynn, N. W. , King, A. C. , Anton, S. D. , Walkup, M. , Lu, C. J. , Reid, K. , Spring, B. , & Pahor, M. (2019). Physical activity and performance impact long‐term quality of life in older adults at risk for major mobility disability. American Journal of Preventive Medicine, 56(1), 141–146. 10.1016/j.amepre.2018.09.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helfer, B. , Prosser, A. , Samara, M. T. , Geddes, J. R. , Cipriani, A. , Davis, J. M. , Mavridis, D. , Salanti, G. , & Leucht, S. (2015). Recent meta‐analyses neglect previous systematic reviews and meta‐analyses about the same topic: A systematic examination. BMC Medicine, 13, 82. 10.1186/s12916-015-0317-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hewitt, J. , Goodall, S. , Clemson, L. , Henwood, T. , & Refshauge, K. (2018). Progressive resistance and balance training for falls prevention in long‐term residential aged care: A cluster randomized trial of the sunbeam program. Journal of the American Medical Directors Association, 19(4), 361–369. 10.1016/j.jamda.2017.12.014 Reference 'Hewitt et al., 2017' year 2017 has been changed to 2018 to match the text citation. Please check for correctness." [DOI] [PubMed] [Google Scholar]
- Hong, Q. N. , Pluye, P. , Fàbregues, S. , Bartlett, G. , Boardman, F. , Cargo, M. , Dagenais, p. , Gagnon, M.‐P. , Griffiths, F. , Nicolau, B. , O'Cathain, A. , Rousseau, M.‐C. , & Vedel, I. (2018). Mixed methods appraisal tool (MMAT), version 2018. Registration of Copyright, (10), 1148552. [Google Scholar]
- Hutton, B. , Salanti, G. , Caldwell, D. M. , Chaimani, A. , Schmid, C. H. , Cameron, C. , Ioannidis, J. P. A. , Straus, S. , Thorlund, K. , Jansen, J. P. , Mulrow, C. , Catala‐Lopez, F. , Gøtzsche, P. C. , Dickersin, K. , Boutron, I. , Altman, D. G. , & Moher, D. (2015). The PRISMA extension statement for reporting of systematic reviews incorporating network meta‐analyses of health care interventions: Checklist and explanations. Annals of Internal Medicine, 162, 777–784. 10.7326/M14-2385 [DOI] [PubMed] [Google Scholar]
- Kleina, T. (2014). Mobilität und Bewegungsfähigkeit von Nutzern stationärer Langzeitversorgung – Ergebnisse einer Analyse von Studienergebnissen und Versorgungsdaten. Pflege& Gesellschaft, 19(2), 101–186. [Google Scholar]
- Kleina, T. , Brause, M. , Horn, A. , Wingenfeld, K. , & Schaeffer, D. (2012). Qualität und Gesundheit in der stationären Altenhilfe – Eine empirische Bestandsaufnahme. Retrieved from https://www.uni‐bielefeld.de/gesundhw/ag6/downloads/ipw_147.pdf.
- Krist, L. , Dimeo, F. , & Keil, T. (2013). Can progressive resistance training twice a week improve mobility, muscle strength, and quality of life in very elderly nursing‐home residents with impaired mobility? A pilot study. Clinical Interventions in Aging, 8, 443–448. 10.2147/CIA.S42136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- La Grow, S. , Yeung, P. , Towers, A. , Alpass, F. , & Stephens, C. (2013). The impact of mobility on quality of life among older persons. Journal of Aging and Health, 25(5), 723–736. 10.1177/0898264313490198 [DOI] [PubMed] [Google Scholar]
- Larsson, L. , Degens, H. , Li, M. , Salviati, L. , Lee, Y. , Thompson, W. , Kirkland, J. L. , & Sandri, M. (2018). Sarcopenia: Aging‐related loss of muscle mass and function. Physiological Reviews, 99, 427–511. 10.1152/physrev.00061.2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liberati, A. , Altman, D. G. , Tetzlaff, J. , Mulrow, C. , Gøtzsche, P. C. , Ioannidis, J. P. A. , Clarke, M. , Devereaux, P. J. , Kleijnen, J. , & Moher, D. (2009). The PRISMA statement for reporting systematic reviews and meta‐analyses of studies that evaluate health care interventions: Explanation and elaboration. PLOS Medicine, 6(7), 1000100. 10.1371/journal.pmed.1000100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lobo, A. , Carvalho, J. , & Santos, P. (2010). Effects of training and detraining on physical fitness, physical activity patterns, cardiovascular variables, and HRQoL after 3 health‐promotion interventions in institutionalized elders. International Journal of Family Medicine, 2010, 486097. 10.1155/2010/486097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mouton, A. , Gillet, N. , Mouton, F. , Van Kann, D. , Bruyère, O. , Cloes, M. , & Buckinx, F. (2017). Effects of a giant exercising board game intervention on ambulatory physical activity among nursing home residents: A preliminary study. Clinical Interventions in Aging, 12, 847–858. 10.2147/CIA.S134760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Özyemişci‐Taşkiran, Ö. , Cicioglu, I. , Golmoghani‐Zadeh, N. , Demir Atilgan, A. , Bagci, E. , Günay, M. , & Atalay, F. (2014). Do pilates and yoga affect quality of life and pysical performance of elderly living in a nursing home. A prelimitary study. Turkish Journal of Geriatrics‐Turk Geriatri Dergisi, 17(3), 262–271. [Google Scholar]
- Powell, B. , Tazamal, M. , & Buhr, G. (2016). Increasing mobility in the nursing home through implementation of a restorative program. Journal of the American Medical Directors Association, 17(3), B18. 10.1016/j.jamda.2015.12.058 [DOI] [Google Scholar]
- Quehenberger, V. , Cichocki, M. , & Krajic, K. (2014). Sustainable effects of a low‐threshold physical activity intervention on health‐related quality of life in residential aged care. Clinical Interventions in Aging, 9, 1853–1864. 10.2147/CIA.S70359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rantakokko, M. , Mänty, M. , & Rantanen, T. (2013). Mobility decline in old age. Exercise and Sport Sciences Reviews, 41(1), 19–25. 10.1097/JES.0b013e3182556f1e [DOI] [PubMed] [Google Scholar]
- Rezola‐Pardo, C. , Rodriguez‐Larrad, A. , Gomez‐Diaz, J. , Lozano‐Real, G. , Mugica‐Errazquin, I. , Patiño, M. J. , Bidaurrazaga‐Letona, I. , Irazusta, J. , & Gil, S. M. (2020). Comparison between multicomponent exercise and walking interventions in long‐term nursing homes: A randomized controlled trial. Gerontologist, 60(7), 1364–1373. 10.1093/geront/gnz177 [DOI] [PubMed] [Google Scholar]
- Schillinger, D. (2010). An introduction to effectiveness, dissemination and implementation research. In A resource manual for community‐engaged research. University of California San Francisco: Clinical Translational Science Institute Community Engagement Program. [Google Scholar]
- Shafrin, J. , Sullivan, J. , Goldman, D. P. , & Gill, T. M. (2017). The association between observed mobility and quality of life in the near elderly. PLoS One, 12(8), e0182920. 10.1371/journal.pone.0182920 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanmore, E. K. , Mavroeidi, A. , de Jong, L. D. , Skelton, D. A. , Sutton, C. J. , Benedetto, V. , Munford, L. A. , Meekes, W. , Bell, V. , & Todd, C. (2019). The effectiveness and cost‐effectiveness of strength and balance Exergames to reduce falls risk for people aged 55 years and older in UK assisted living facilities: A multi‐Centre, cluster randomised controlled trial. BMC Medicine, 17(49), 49. 10.1186/s12916-019-1278-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strupeit, S. , & Buss, A. (2014). Ein multidimensionales Konstrukt. Definition von Mobilität aus pflegewissenschaftlicher Perspektive. Pflege Zeitschrift, 67(1), 38–40. [PubMed] [Google Scholar]
- Sverdrup, K. , Bergh, S. , Selbæk, G. , Røen, I. , Kirkevold, Ø. , & Tangen, G. G. (2018). Mobility and cognition at admission to the nursing home – A cross‐sectional study. BMC Geriatrics, 18, 30. 10.1186/s12877-018-0724-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wingenfeld, K. , Becker, U. , Beckmann, M. , Berger, B. , Eifert, B. , Freiberger, E. , Horn, A. , Krampen, R. , Kretschmar, D. , Metzelthin, S. , Püttjer, A. , Reuther, S. , Schiff, A. , Skiba, T. , & Schlesselmann, E. (2020). Der Expertenstandard Erhaltung und Förderung der Mobilität in der Pflege 1. Aktualisierung 2020. In: Deutsches Netzwerk für Qualität in der Pflege (DNQP) (2020). Expertenstandard nach § 113a SGB XI „Erhaltung und Förderung der Mobilität in der Pflege. Aktualisierung 2020. Retrieved from https://www.gs‐qsa‐pflege.de/wp‐content/uploads/2020/12/Expertenstandard‐„Erhaltung‐und‐Förderung‐der‐Mobilität‐in‐der‐Pflege“‐Aktualisierung‐2020.pdf
- World Health Organization (WHO) . (1993). Study protocol for the World Health Organization project to develop a quality of life assessment instrument (WHOQOL). Quality of Life Research, 2, 153–159. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no new data were created or analyzed in this study.


