Abstract
Background
The use of robotics in arthroplasty surgery has increased substantially in recent years. The purpose of this study was to objectively identify the 100 most influential studies in the robotic arthroplasty literature and to conduct a bibliometric analysis of these studies to describe their key characteristics.
Methods
The Clarivate Analytics Web of Knowledge database was used to gather data and metrics for robotic arthroplasty research using Boolean queries. The search list was sorted in descending order by the number of citations, and articles were included or excluded based on clinical relevance to robotic arthroplasty.
Results
The top 100 studies were cited a total of 5770 times from 1997 to 2021, with rapid growth in both citation generation and the number of articles published occurring in the past 5 years. The top 100 robotic arthroplasty articles originated from 12 countries, with the United States being responsible for almost half of the top 100. The most common study types were comparative studies (36) followed by case series (20), and the most common levels of evidence were III (23) and IV (33).
Conclusions
Research on robotic arthroplasty is rapidly growing and originates from a wide variety of countries, academic institutions, and with significant industry influence. This article serves as a reference to direct orthopaedic practitioners to the 100 most influential studies in robotic arthroplasty. We hope that these 100 studies and the analysis we provide aid healthcare professionals in efficiently assessing consensus, trends, and needs within the field.
Keywords: Robotic, Arthroplasty, Bibliometric analysis, Citation analysis, Hip arthroplasty, Knee arthroplasty
Introduction
Robotic-assisted orthopaedic surgery has been implemented in the clinical setting for roughly 25 years [1]. In contrast to soft-tissue robotic surgical systems, robotics in orthopaedic surgery has focused on advancing the precision and accuracy of surgical manipulation of hard tissue by correlating preoperative imaging with bony landmarks [[2], [3], [4]]. The implementation of robotics has gained increasing attention, particularly in the field of joint arthroplasty, where semiactive computer navigation combined with haptic and/or visual feedback may allow for improved reproducibility and precision in osteotomy placement, joint alignment, and soft tissue balancing [1,2,5]. Robotic assistance also presents trade-offs of increased intraoperative times and technique complexity with increased accuracy of component position [1,[6], [7], [8]]. However, the evidence is variable as to whether robotic-assisted arthroplasty translates to improvements in clinical outcomes [[9], [10], [11]].
The use of robotics in arthroplasty has increased substantially in prevalence as well as in surgeon and patient interest [10,12]. A recent review of the Nationwide Inpatient Sample demonstrated that robotic and technology-assisted total knee arthroplasties have steadily increased from 1.2% in 2005 to 7.0% in 2014 [10,13]. As the body of literature on robotic arthroplasty continues to expand, developing a comprehensive understanding of the topic becomes increasingly difficult. It is beneficial for orthopaedic residents, fellows, and surgeons to be able to prioritize the most important studies. Fortunately, bibliometric analyses are a well-established tool to elicit common themes and to analyze how the trends of a particular field are evolving [[14], [15], [16]]. Bibliometric analyses synthesize citation impact as well as other research power indicators to identify high-impact articles and their relative effect on a specific field [[16], [17], [18]]. Furthermore, they allow researchers and clinicians to differentiate the areas or topics well-established in the literature from those that may need further investigation and inquiry. Within orthopaedics, bibliometric citation analyses have been conducted on a whole host of topics including elbow surgery, ankle arthroplasty, sports-related concussions, shoulder arthroscopy, total hip arthroplasty, and unicondylar knee arthroplasty [[18], [19], [20], [21], [22], [23], [24]]. In the field of orthopaedic robotics use, a particular citation analysis by Li et al. [4] used bibliometrics to assess the status and trends of robotics used across the entirety of orthopaedic surgery; however, only 72 (32%) of its papers focused on the area of arthroplasty. Therefore, a dedicated bibliometric analysis becomes more relevant as the specialized topic of robotic arthroplasty continues to expand in utilization and prevalence.
The purpose of this study was to objectively identify the 100 most influential studies in the robotic arthroplasty literature and to conduct a bibliometric analysis of these studies to describe their key characteristics. Additionally, the authors hypothesized that the year of publication would influence the number of citations the article was able to accrue.
Material and methods
This study was exempt from institutional review board approval due to the public nature of the data. Data and Metrics were obtained using the Clarivate Analytics Web of Knowledge database using study methods based on similar bibliometric analyses of orthopaedic literature [[25], [26], [27], [28], [29], [30], [31], [32]]. The literature search was performed on May 3rd, 2022 using multiple Boolean queries to capture all iterations of robotic arthroplasty research. The search was conducted with no restrictions on date, language, journal, or country of origin. This original query resulted in 1967 total articles.
The list of articles was then sorted in descending order by the number of citations per article. The titles and abstracts of these articles were reviewed to determine their relevance to robotic arthroplasty and subsequent inclusion in our study. To qualify for selection, the article must present information on surgical indications, descriptions of procedures, surgical outcomes, complications, or an analysis of robotic arthroplasty procedures. Furthermore, the study had to have a clinical focus and involve patient subjects or review articles involving patient subjects. Manuscripts centered on wet lab, cadaveric, and animal studies were excluded. If there was ambiguity regarding whether a study should be included, the full article was examined by 2 independent authors (S.B. and M.L.M.) to make a final decision on inclusion or exclusion. If there was still a question as to whether an article should be included, the senior author (J.S.B.) was consulted.
A total of 389 articles were reviewed before finalizing the 100 most-cited studies that satisfied the inclusion criteria. These 100 studies were then reviewed to extract the following information: total number of citations per article, authors, publication year, country of origin, institution of origin, journal of publication, joint undergoing arthroplasty (shoulder, elbow, hip, knee, or ankle), name or brand of primary robotic device in the study, and any industry funding or affiliation associated with the study. Country of origin and affiliated institution of both the first and last authors were collected. In addition, the reviewer classified articles based on study design (randomized controlled trial, comparative study, case series, review article, descriptive article, cost analysis, or expert opinion) and level of evidence using the guidelines published in The Journal of Bone and Joint Surgery [33]. The level of evidence in a study indicates the relative risk of bias, rather than its quality. Both the study design and level of evidence were determined by a consensus opinion between the first and second authors (S.B. and M.L.M.).
The “comparative study” label was inclusive of prospective cohort studies, retrospective cohort studies, and case-control series. The label “review article” was inclusive of systematic reviews and meta-analyses that analyzed literature present in the field. If an article reviewed the literature without a clear methodology or systematic approach, it was classified with the “expert opinion” label. The “descriptive article” label was reserved for studies that primarily explored a specific robotic arthroplasty device or surgical technique involving a robotic arthroplasty device and minimally involved patient trials or reviews of patient trials. The citation density was calculated for each article by taking the total number of citations per year divided by the number of years since publication [15]. Clinical summaries were obtained for each study through consensus by having 2 reviewers extract the main results and conclusions from each study’s abstract and manuscript.
Results
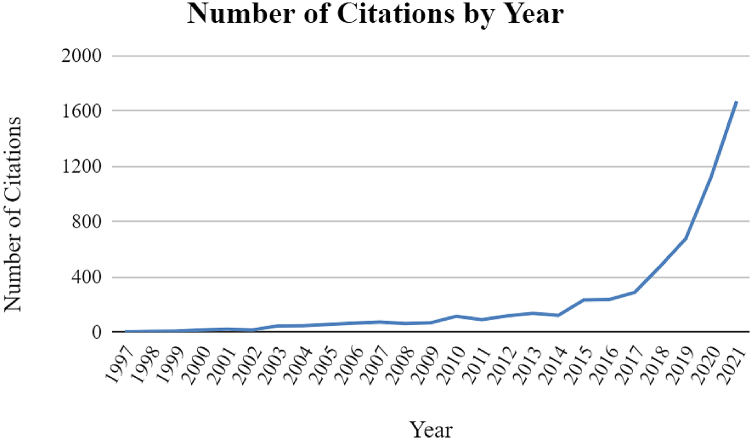
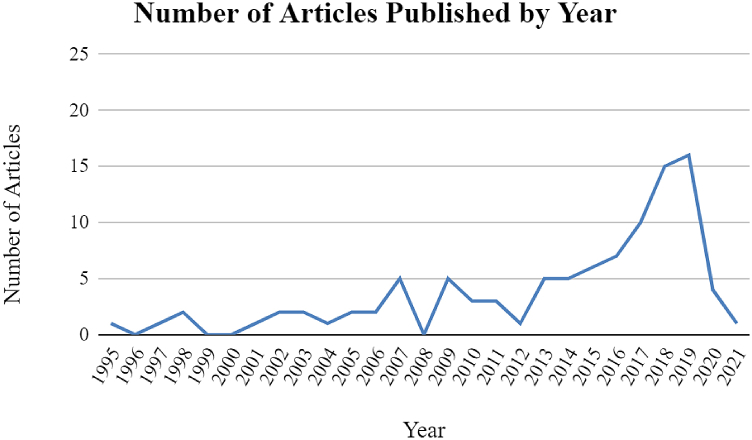
Of the top 100 most-cited papers in robotic arthroplasty, the oldest article was published in 1995, and the most recent article was published in 2021. The greatest number of articles were published in 2019 (16), and the second greatest number of articles were published in 2018 (15). The majority of studies were published after 2015 (59/100). (Fig. 1) The 100 included articles accumulated a total of 6052 citations at the time of analysis. As a whole, the citation density for the 100 robotic arthroplasty studies grew steadily over the past 25 years, with a marked increase observed since 2016. (Fig. 2) A list of the top 100 most-cited papers with their authors, number of citations, citation density, and publication year is presented in Table 1 [Table 1].
Figure 1.
The number of citations accrued by the top 100 most-cited robotic arthroplasty studies over time.
Figure 2.
The number of top 100 most-cited robotic arthroplasty studies published by year.
Table 1.
The top-100 most-cited robotic arthroplasty articles.
| Rank | Article | No. of citations (citation densitya) | Original publication year |
|---|---|---|---|
| 1 | Bargar WL, Bauer A, Börner M. Primary and revision total hip replacement using the Robodoc system. Clin Orthop Relat Res 1998:82–91. https://doi.org/10.1097/00003086-199809000-00011. | 236 (9.83) | 1998 |
| 2 | Cobb J, Henckel J, Gomes P, Harris S, Jakopec M, Rodriguez F, et al. Hands-on robotic unicompartmental knee replacement: a prospective, randomised controlled study of the acrobot system. J Bone Joint Surg Br 2006;88:188–97. https://doi.org/10.1302/0301-620X.88B2.17220. | 205 (12.81) | 2006 |
| 3 | Delp SL, Stulberg SD, Davies B, Picard F, Leitner F. Computer assisted knee replacement. Clin Orthop Relat Res 1998:49–56. https://doi.org/10.1097/00003086-199809000-00007. | 167 (6.96) | 1998 |
| 4 | Jacofsky DJ, Allen M. Robotics in Arthroplasty: A Comprehensive Review. J Arthroplasty 2016;31:2353–63. https://doi.org/10.1016/j.arth.2016.05.026. | 147 (24.50) | 2016 |
| 5 | Bell SW, Anthony I, Jones B, MacLean A, Rowe P, Blyth M. Improved Accuracy of Component Positioning with Robotic-Assisted Unicompartmental Knee Arthroplasty: Data from a Prospective, Randomized Controlled Study. J Bone Joint Surg Am 2016;98:627–35. https://doi.org/10.2106/JBJS.15.00664. | 144 (24.00) | 2016 |
| 6 | Siebert W, Mai S, Kober R, Heeckt PF. Technique and first clinical results of robot-assisted total knee replacement. Knee 2002;9:173–80. https://doi.org/10.1016/s0968-0160(02)00015-7. | 144 (7.20) | 2002 |
| 7 | Song E-K, Seon J-K, Yim J-H, Netravali NA, Bargar WL. Robotic-assisted TKA reduces postoperative alignment outliers and improves gap balance compared to conventional TKA. Clin Orthop Relat Res 2013;471:118–26. https://doi.org/10.1007/s11999-012-2407-3. | 138 (15.33) | 2013 |
| 8 | Honl M, Dierk O, Gauck C, Carrero V, Lampe F, Dries S, et al. Comparison of robotic-assisted and manual implantation of a primary total hip replacement. A prospective study. J Bone Joint Surg Am 2003;85:1470–8. https://doi.org/10.2106/00004623-200308000-00007. | 134 (7.05) | 2003 |
| 9 | Domb BG, El Bitar YF, Sadik AY, Stake CE, Botser IB. Comparison of robotic-assisted and conventional acetabular cup placement in THA: a matched-pair controlled study. Clin Orthop Relat Res 2014;472:329–36. https://doi.org/10.1007/s11999-013-3253-7. | 127 (15.88) | 2014 |
| 10 | Lonner JH, John TK, Conditt MA. Robotic arm-assisted UKA improves tibial component alignment: a pilot study. Clin Orthop Relat Res 2010;468:141–6. https://doi.org/10.1007/s11999-009-0977-5. | 124 (10.33) | 2010 |
| 11 | Jakopec M, Harris SJ, Rodriguez y Baena F, Gomes P, Cobb J, Davies BL. The first clinical application of a “hands-on” robotic knee surgery system. Comput Aided Surg 2001;6:329–39. https://doi.org/10.1002/igs.10023. | 118 (5.62) | 2001 |
| 12 | Song E-K, Seon J-K, Park S-J, Jung WB, Park H-W, Lee GW. Simultaneous bilateral total knee arthroplasty with robotic and conventional techniques: a prospective, randomized study. Knee Surg Sports Traumatol Arthrosc 2011;19:1069–76. https://doi.org/10.1007/s00167-011-1400-9. | 112 (10.18) | 2011 |
| 13 | Lang JE, Mannava S, Floyd AJ, Goddard MS, Smith BP, Mofidi A, et al. Robotic systems in orthopaedic surgery. J Bone Joint Surg Br 2011;93:1296–9. https://doi.org/10.1302/0301-620X.93B10.27418. | 106 (9.64) | 2011 |
| 14 | Park SE, Lee CT. Comparison of robotic-assisted and conventional manual implantation of a primary total knee arthroplasty. J Arthroplasty 2007;22:1054–9. https://doi.org/10.1016/j.arth.2007.05.036. | 106 (7.07) | 2007 |
| 15 | Kayani B, Konan S, Tahmassebi J, Pietrzak JRT, Haddad FS. Robotic-arm assisted total knee arthroplasty is associated with improved early functional recovery and reduced time to hospital discharge compared with conventional jig-based total knee arthroplasty: a prospective cohort study. Bone Joint J 2018;100-B:930–7. https://doi.org/10.1302/0301-620X.100B7.BJJ-2017-1449.R1. | 104 (26.00) | 2018 |
| 16 | Liow MHL, Xia Z, Wong MK, Tay KJ, Yeo SJ, Chin PL. Robot-assisted total knee arthroplasty accurately restores the joint line and mechanical axis. A prospective randomised study. J Arthroplasty 2014;29:2373–7. https://doi.org/10.1016/j.arth.2013.12.010. | 98 (12.25) | 2014 |
| 17 | Pearle AD, O’Loughlin PF, Kendoff DO. Robot-assisted unicompartmental knee arthroplasty. J Arthroplasty 2010;25:230–7. https://doi.org/10.1016/j.arth.2008.09.024. | 98 (8.17) | 2010 |
| 18 | Bellemans J, Vandenneucker H, Vanlauwe J. Robot-assisted total knee arthroplasty. Clin Orthop Relat Res 2007;464:111–6. https://doi.org/10.1097/BLO.0b013e318126c0c0. | 92 (6.13) | 2007 |
| 19 | Schulz AP, Seide K, Queitsch C, von Haugwitz A, Meiners J, Kienast B, et al. Results of total hip replacement using the Robodoc surgical assistant system: clinical outcome and evaluation of complications for 97 procedures. Int J Med Robot 2007;3:301–6. https://doi.org/10.1002/rcs.161. | 91 (6.07) | 2007 |
| 20 | Jakopec M, Rodriguez y Baena F, Harris SJ, Gomes P, Cobb J, Davies BL. The hands-on orthopaedic robot “acrobot”: Early clinical trials of total knee replacement surgery. IEEE Transactions on Robotics and Automation 2003;19:902–11. https://doi.org/10.1109/TRA.2003.817510. | 90 (4.74) | 2003 |
| 21 | Dunbar NJ, Roche MW, Park BH, Branch SH, Conditt MA, Banks SA. Accuracy of dynamic tactile-guided unicompartmental knee arthroplasty. J Arthroplasty 2012;27:803-808.e1. https://doi.org/10.1016/j.arth.2011.09.021. | 86 (8.60) | 2012 |
| 22 | Sugano N. Computer-assisted orthopaedic surgery and robotic surgery in total hip arthroplasty. Clin Orthop Surg 2013;5:1–9. https://doi.org/10.4055/cios.2013.5.1.1. | 79 (8.78) | 2013 |
| 23 | Pearle AD, van der List JP, Lee L, Coon TM, Borus TA, Roche MW. Survivorship and patient satisfaction of robotic-assisted medial unicompartmental knee arthroplasty at a minimum 2-year follow-up. Knee 2017;24:419–28. https://doi.org/10.1016/j.knee.2016.12.001. | 78 (15.60) | 2017 |
| 24 | Kayani B, Konan S, Huq SS, Tahmassebi J, Haddad FS. Robotic-arm assisted total knee arthroplasty has a learning curve of seven cases for integration into the surgical workflow but no learning curve effect for accuracy of implant positioning. Knee Surg Sports Traumatol Arthrosc 2019;27:1132–41. https://doi.org/10.1007/s00167-018-5138-5. | 72 (24.00) | 2019 |
| 25 | Blyth MJG, Anthony I, Rowe P, Banger MS, MacLean A, Jones B. Robotic arm-assisted versus conventional unicompartmental knee arthroplasty: Exploratory secondary analysis of a randomised controlled trial. Bone Joint Res 2017;6:631–9. https://doi.org/10.1302/2046-3758.611.BJR-2017-0060.R1. | 72 (14.40) | 2017 |
| 26 | Marchand RC, Sodhi N, Khlopas A, Sultan AA, Harwin SF, Malkani AL, et al. Patient Satisfaction Outcomes after Robotic Arm-Assisted Total Knee Arthroplasty: A Short-Term Evaluation. J Knee Surg 2017;30:849–53. https://doi.org/10.1055/s-0037-1607450. | 71 (14.20) | 2017 |
| 27 | Moschetti WE, Konopka JF, Rubash HE, Genuario JW. Can Robot-Assisted Unicompartmental Knee Arthroplasty Be Cost-Effective? A Markov Decision Analysis. J Arthroplasty 2016;31:759–65. https://doi.org/10.1016/j.arth.2015.10.018. | 71 (11.83) | 2016 |
| 28 | Nakamura N, Sugano N, Nishii T, Kakimoto A, Miki H. A comparison between robotic-assisted and manual implantation of cementless total hip arthroplasty. Clin Orthop Relat Res 2010;468:1072–81. https://doi.org/10.1007/s11999-009-1158-2. | 69 (5.75) | 2010 |
| 29 | Batailler C, White N, Ranaldi FM, Neyret P, Servien E, Lustig S. Improved implant position and lower revision rate with robotic-assisted unicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 2019;27:1232–40. https://doi.org/10.1007/s00167-018-5081-5. | 68 (22.67) | 2019 |
| 30 | Plate JF, Mofidi A, Mannava S, Smith BP, Lang JE, Poehling GG, et al. Achieving accurate ligament balancing using robotic-assisted unicompartmental knee arthroplasty. Adv Orthop 2013;2013:837167. https://doi.org/10.1155/2013/837167. | 67 (7.44) | 2013 |
| 31 | Sodhi N, Khlopas A, Piuzzi NS, Sultan AA, Marchand RC, Malkani AL, et al. The Learning Curve Associated with Robotic Total Knee Arthroplasty. J Knee Surg 2018;31:17–21. | 66 (16.50) | 2018 |
| 32 | Kayani B, Konan S, Pietrzak JRT, Haddad FS. Iatrogenic Bone and Soft Tissue Trauma in Robotic-Arm Assisted Total Knee Arthroplasty Compared With Conventional Jig-Based Total Knee Arthroplasty: A Prospective Cohort Study and Validation of a New Classification System. J Arthroplasty 2018;33:2496–501. https://doi.org/10.1016/j.arth.2018.03.042. | 65 (16.25) | 2018 |
| 33 | Liow MHL, Goh GS-H, Wong MK, Chin PL, Tay DK-J, Yeo S-J. Robotic-assisted total knee arthroplasty may lead to improvement in quality-of-life measures: a 2-year follow-up of a prospective randomized trial. Knee Surg Sports Traumatol Arthrosc 2017;25:2942–51. https://doi.org/10.1007/s00167-016-4076-3. | 65 (13.00) | 2017 |
| 34 | Kayani B, Konan S, Pietrzak JRT, Huq SS, Tahmassebi J, Haddad FS. The learning curve associated with robotic-arm assisted unicompartmental knee arthroplasty: a prospective cohort study. Bone Joint J 2018;100-B:1033–42. https://doi.org/10.1302/0301-620X.100B8.BJJ-2018-0040.R1. | 64 (16.00) | 2018 |
| 35 | Kayani B, Konan S, Tahmassebi J, Rowan FE, Haddad FS. An assessment of early functional rehabilitation and hospital discharge in conventional vs robotic-arm assisted unicompartmental knee arthroplasty: a prospective cohort study. Bone Joint J 2019;101-B:24–33. https://doi.org/10.1302/0301-620X.101B1.BJJ-2018-0564.R2. | 61 (20.33) | 2019 |
| 36 | Domb BG, Redmond JM, Louis SS, Alden KJ, Daley RJ, LaReau JM, et al. Accuracy of Component Positioning in 1980 Total Hip Arthroplasties: A Comparative Analysis by Surgical Technique and Mode of Guidance. J Arthroplasty 2015;30:2208–18. https://doi.org/10.1016/j.arth.2015.06.059. | 60 (8.57) | 2015 |
| 37 | Gilmour A, MacLean AD, Rowe PJ, Banger MS, Donnelly I, Jones BG, et al. Robotic-Arm-Assisted vs Conventional Unicompartmental Knee Arthroplasty. The 2-Year Clinical Outcomes of a Randomized Controlled Trial. J Arthroplasty 2018;33:S109–15. https://doi.org/10.1016/j.arth.2018.02.050. | 59 (14.75) | 2018 |
| 38 | Kazanzides P, Mittelstadt BD, Musits BL, Bargar WL, Zuhars JF, Williamson B, et al. An integrated system for cementless hip replacement. IEEE Engineering in Medicine and Biology Magazine 1995;14:307–13. https://doi.org/10.1109/51.391772. | 57 (2.11) | 1995 |
| 39 | Herry Y, Batailler C, Lording T, Servien E, Neyret P, Lustig S. Improved joint-line restitution in unicompartmental knee arthroplasty using a robotic-assisted surgical technique. Int Orthop 2017;41:2265–71. https://doi.org/10.1007/s00264-017-3633-9. | 55 (11.00) | 2017 |
| 40 | Nishihara S, Sugano N, Nishii T, Miki H, Nakamura N, Yoshikawa H. Comparison between hand rasping and robotic milling for stem implantation in cementless total hip arthroplasty. J Arthroplasty 2006;21:957–66. https://doi.org/10.1016/j.arth.2006.01.001. | 52 (3.25) | 2006 |
| 41 | Decking J, Theis C, Achenbach T, Roth E, Nafe B, Eckardt A. Robotic total knee arthroplasty: the accuracy of CT-based component placement. Acta Orthop Scand 2004;75:573–9. https://doi.org/10.1080/00016470410001448. | 50 (2.78) | 2004 |
| 42 | Yang HY, Seon JK, Shin YJ, Lim HA, Song EK. Robotic Total Knee Arthroplasty with a Cruciate-Retaining Implant: A 10-Year Follow-up Study. Clin Orthop Surg 2017;9:169–76. https://doi.org/10.4055/cios.2017.9.2.169. | 48 (9.60) | 2017 |
| 43 | llgen RL, Bukowski BR, Abiola R, Anderson P, Chughtai M, Khlopas A, et al. Robotic-Assisted Total Hip Arthroplasty: Outcomes at Minimum Two-Year Follow-Up. Surg Technol Int 2017;30:365–72. | 47 (9.40) | 2017 |
| 44 | Plate JF, Augart MA, Seyler TM, Bracey DN, Hoggard A, Akbar M, et al. Obesity has no effect on outcomes following unicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 2017;25:645–51. https://doi.org/10.1007/s00167-015-3597-5. | 47 (9.40) | 2017 |
| 45 | Swank ML, Alkire M, Conditt M, Lonner JH. Technology and cost-effectiveness in knee arthroplasty: computer navigation and robotics. Am J Orthop (Belle Mead NJ) 2009;38:32–6. | 47 (3.62) | 2009 |
| 46 | Hansen DC, Kusuma SK, Palmer RM, Harris KB. Robotic guidance does not improve component position or short-term outcome in medial unicompartmental knee arthroplasty. J Arthroplasty 2014;29:1784–9. https://doi.org/10.1016/j.arth.2014.04.012. | 46 (5.75) | 2014 |
| 47 | Kayani B, Konan S, Ayuob A, Onochie E, Al-Jabri T, Haddad FS. Robotic technology in total knee arthroplasty: a systematic review. EFORT Open Rev 2019;4:611–7. https://doi.org/10.1302/2058-5241.4.190022. | 45 (15.00) | 2019 |
| 48 | Kleeblad LJ, Borus TA, Coon TM, Dounchis J, Nguyen JT, Pearle AD. Midterm Survivorship and Patient Satisfaction of Robotic-Arm-Assisted Medial Unicompartmental Knee Arthroplasty: A Multicenter Study. J Arthroplasty 2018;33:1719–26. https://doi.org/10.1016/j.arth.2018.01.036. | 45 (11.25) | 2018 |
| 49 | Kamara E, Robinson J, Bas MA, Rodriguez JA, Hepinstall MS. Adoption of Robotic vs Fluoroscopic Guidance in Total Hip Arthroplasty: Is Acetabular Positioning Improved in the Learning Curve? J Arthroplasty 2017;32:125–30. https://doi.org/10.1016/j.arth.2016.06.039. | 45 (9.00) | 2017 |
| 50 | Nodzo SR, Chang C-C, Carroll KM, Barlow BT, Banks SA, Padgett DE, et al. Intraoperative placement of total hip arthroplasty components with robotic-arm assisted technology correlates with postoperative implant position: a CT-based study. Bone Joint J 2018;100-B:1303–9. https://doi.org/10.1302/0301-620X.100B10-BJJ-2018-0201.R1. | 44 (11.00) | 2018 |
| 51 | Chun YS, Kim KI, Cho YJ, Kim YH, Yoo MC, Rhyu KH. Causes and patterns of aborting a robot-assisted arthroplasty. J Arthroplasty 2011;26:621–5. https://doi.org/10.1016/j.arth.2010.05.017. | 44 (4.00) | 2011 |
| 52 | Kim Y-H, Yoon S-H, Park J-W. Does Robotic-assisted TKA Result in Better Outcome Scores or Long-Term Survivorship Than Conventional TKA? A Randomized, Controlled Trial. Clin Orthop Relat Res 2020;478:266–75. https://doi.org/10.1097/CORR.0000000000000916. | 43 (21.50) | 2020 |
| 53 | Redmond JM, Gupta A, Hammarstedt JE, Petrakos AE, Finch NA, Domb BG. The learning curve associated with robotic-assisted total hip arthroplasty. J Arthroplasty 2015;30:50–4. https://doi.org/10.1016/j.arth.2014.08.003. | 43 (6.14) | 2015 |
| 54 | Roche M, O’Loughlin PF, Kendoff D, Musahl V, Pearle AD. Robotic arm-assisted unicompartmental knee arthroplasty: preoperative planning and surgical technique. Am J Orthop (Belle Mead NJ) 2009;38:10–5. | 42 (3.23) | 2009 |
| 55 | Marchand RC, Sodhi N, Khlopas A, Sultan AA, Higuera CA, Stearns KL, et al. Coronal Correction for Severe Deformity Using Robotic-Assisted Total Knee Arthroplasty. J Knee Surg 2018;31:2–5. https://doi.org/10.1055/s-0037-1608840. | 41 (10.25) | 2018 |
| 56 | Jeon S-W, Kim K-I, Song SJ. Robot-Assisted Total Knee Arthroplasty Does Not Improve Long-Term Clinical and Radiologic Outcomes. J Arthroplasty 2019;34:1656–61. https://doi.org/10.1016/j.arth.2019.04.007. | 40 (13.33) | 2019 |
| 57 | Cho K-J, Seon J-K, Jang W-Y, Park C-G, Song E-K. Robotic vs conventional primary total knee arthroplasty: clinical and radiological long-term results with a minimum follow-up of 10 years. Int Orthop 2019;43:1345–54. https://doi.org/10.1007/s00264-018-4231-1. | 40 (13.33) | 2019 |
| 58 | Dretakis K, Igoumenou VG. Outcomes of robotic-arm-assisted medial unicompartmental knee arthroplasty: minimum 3-year follow-up. Eur J Orthop Surg Traumatol 2019;29:1305–11. https://doi.org/10.1007/s00590-019-02424-4. | 40 (3.07) | 2009 |
| 59 | Börner M, Bauer A, Lahmer A. Computer-guided robot-assisted hip endoprosthesis. Orthopade 1997;26:251–7. https://doi.org/10.1007/s001320050092. | 40 (1.6) | 1997 |
| 60 | Boylan M, Suchman K, Vigdorchik J, Slover J, Bosco J. Technology-Assisted Hip and Knee Arthroplasties: An Analysis of Utilization Trends. J Arthroplasty 2018;33:1019–23. https://doi.org/10.1016/j.arth.2017.11.033. | 38 (9.50) | 2018 |
| 61 | Liow MHL, Chin PL, Tay KJD, Chia SL, Lo NN, Yeo SJ. Early experiences with robot-assisted total knee arthroplasty using the DigiMatch ROBODOC surgical system. Singapore Med J 2014;55:529–34. https://doi.org/10.11622/smedj.2014136. | 38 (4.75) | 2014 |
| 62 | Lonner JH. Indications for unicompartmental knee arthroplasty and rationale for robotic arm-assisted technology. Am J Orthop (Belle Mead NJ) 2009;38:3–6. | 38 (2.92) | 2009 |
| 63 | Pearle AD, Kendoff D, Stueber V, Musahl V, Repicci JA. Perioperative management of unicompartmental knee arthroplasty using the MAKO robotic arm system (MAKOplasty). Am J Orthop (Belle Mead NJ) 2009;38:16–9. | 38 (2.92) | 2009 |
| 64 | Thienpont E, Fennema P, Price A. Can technology improve alignment during knee arthroplasty. Knee 2013;20 Suppl 1:S21-28. https://doi.org/10.1016/S0968-0160(13)70005-X. | 37 (4.11) | 2013 |
| 65 | Kanawade V, Dorr LD, Banks SA, Zhang Z, Wan Z. Precision of robotic guided instrumentation for acetabular component positioning. J Arthroplasty 2015;30:392–7. https://doi.org/10.1016/j.arth.2014.10.021. | 36 (5.14) | 2015 |
| 66 | Banerjee S, Cherian JJ, Elmallah RK, Jauregui JJ, Pierce TP, Mont MA. Robotic-assisted knee arthroplasty. Expert Rev Med Devices 2015;12:727–35. https://doi.org/10.1586/17434440.2015.1086264. | 36 (5.14) | 2015 |
| 67 | Hananouchi T, Sugano N, Nishii T, Nakamura N, Miki H, Kakimoto A, et al. Effect of robotic milling on periprosthetic bone remodeling. J Orthop Res 2007;25:1062–9. https://doi.org/10.1002/jor.20376. | 36 (2.40) | 2007 |
| 68 | Marchand RC, Sodhi N, Anis HK, Ehiorobo J, Newman JM, Taylor K, et al. One-Year Patient Outcomes for Robotic-Arm-Assisted vs Manual Total Knee Arthroplasty. J Knee Surg 2019;32:1063–8. https://doi.org/10.1055/s-0039-1683977. | 35 (11.67) | 2019 |
| 69 | Cool CL, Jacofsky DJ, Seeger KA, Sodhi N, Mont MA. A 90-day episode-of-care cost analysis of robotic-arm assisted total knee arthroplasty. J Comp Eff Res 2019;8:327–36. https://doi.org/10.2217/cer-2018-0136. | 35 (11.67) | 2019 |
| 70 | Khlopas A, Sodhi N, Sultan AA, Chughtai M, Molloy RM, Mont MA. Robotic Arm-Assisted Total Knee Arthroplasty. J Arthroplasty 2018;33:2002–6. https://doi.org/10.1016/j.arth.2018.01.060. | 35 (8.75) | 2018 |
| 71 | Mofidi A, Plate JF, Lu B, Conditt MA, Lang JE, Poehling GG, et al. Assessment of accuracy of robotically assisted unicompartmental arthroplasty. Knee Surg Sports Traumatol Arthrosc 2014;22:1918–25. https://doi.org/10.1007/s00167-014-2969-6. | 35 (4.37) | 2014 |
| 72 | Davies BL, Rodriguez y Baena FM, Barrett ARW, Gomes MPSF, Harris SJ, Jakopec M, et al. Robotic control in knee joint replacement surgery. Proc Inst Mech Eng H 2007;221:71–80. https://doi.org/10.1243/09544119JEIM250. | 35 (2.33) | 2007 |
| 73 | Canetti R, Batailler C, Bankhead C, Neyret P, Servien E, Lustig S. Faster return to sport after robotic-assisted lateral unicompartmental knee arthroplasty: a comparative study. Arch Orthop Trauma Surg 2018;138:1765–71. https://doi.org/10.1007/s00402-018-3042-6. | 34 (8.50) | 2018 |
| 74 | Antonios JK, Korber S, Sivasundaram L, Mayfield C, Kang HP, Oakes DA, et al. Trends in computer navigation and robotic assistance for total knee arthroplasty in the United States: an analysis of patient and hospital factors. Arthroplasty Today 2019;5:88–95. https://doi.org/10.1016/j.artd.2019.01.002. | 33 (11.00) | 2019 |
| 75 | van der List JP, Chawla H, Joskowicz L, Pearle AD. Current state of computer navigation and robotics in unicompartmental and total knee arthroplasty: a systematic review with meta-analysis. Knee Surg Sports Traumatol Arthrosc 2016;24:3482–95. https://doi.org/10.1007/s00167-016-4305-9. | 33 (5.50) | 2016 |
| 76 | Rodriguez F, Harris S, Jakopec M, Barrett A, Gomes P, Henckel J, et al. Robotic clinical trials of uni-condylar arthroplasty. The International Journal of Medical Robotics and Computer Assisted Surgery 2005;1:20–8. https://doi.org/10.1002/rcs.52. | 33 (1.94) | 2005 |
| 77 | Bukowski BR, Anderson P, Khlopas A, Chughtai M, Mont MA, Illgen RL. Improved Functional Outcomes with Robotic Compared with Manual Total Hip Arthroplasty. Surg Technol Int 2016;29:303–8. | 32 (5.33) | 2016 |
| 78 | Clement ND, Deehan DJ, Patton JT. Robot-assisted unicompartmental knee arthroplasty for patients with isolated medial compartment osteoarthritis is cost-effective: a Markov decision analysis. Bone Joint J 2019;101-B:1063–70. https://doi.org/10.1302/0301-620X.101B9.BJJ-2018-1658.R1. | 31 (10.33) | 2019 |
| 79 | Robinson PG, Clement ND, Hamilton D, Blyth MJG, Haddad FS, Patton JT. A systematic review of robotic-assisted unicompartmental knee arthroplasty: prosthesis design and type should be reported. Bone Joint J 2019;101-B:838–47. https://doi.org/10.1302/0301-620X.101B7.BJJ-2018-1317.R1. | 31 (10.33) | 2019 |
| 80 | Lonner JH, Fillingham YA. Pros and Cons: A Balanced View of Robotics in Knee Arthroplasty. J Arthroplasty 2018;33:2007–13. https://doi.org/10.1016/j.arth.2018.03.056. | 31 (7.75) | 2018 |
| 81 | Bargar WL, Parise CA, Hankins A, Marlen NA, Campanelli V, Netravali NA. Fourteen Year Follow-Up of Randomized Clinical Trials of Active Robotic-Assisted Total Hip Arthroplasty. J Arthroplasty 2018;33:810–4. https://doi.org/10.1016/j.arth.2017.09.066. | 31 (7.75) | 2018 |
| 82 | Netravali NA, Shen F, Park Y, Bargar WL. A perspective on robotic assistance for knee arthroplasty. Adv Orthop 2013;2013:970703. https://doi.org/10.1155/2013/970703. | 31 (3.44) | 2013 |
| 83 | Siebel T, Käfer W. Clinical outcome following robotic assisted versus conventional total hip arthroplasty: a controlled and prospective study of seventy-one patients. Z Orthop Ihre Grenzgeb 2005;143:391–8. https://doi.org/10.1055/s-2005-836776. | 31 (1.82) | 2005 |
| 84 | Bach CM, Winter P, Nogler M, Göbel G, Wimmer C, Ogon M. No functional impairment after Robodoc total hip arthroplasty. Acta Orthopaedica Scandinavica 2002;73:386–91. https://doi.org/10.1080/00016470216316. | 31 (1.55) | 2002 |
| 85 | Sultan AA, Piuzzi N, Khlopas A, Chughtai M, Sodhi N, Mont MA. Utilization of robotic-arm assisted total knee arthroplasty for soft tissue protection. Expert Rev Med Devices 2017;14:925–7. https://doi.org/10.1080/17434440.2017.1392237. | 30 (6.00) | 2017 |
| 86 | Elson L, Dounchis J, Illgen R, Marchand RC, Padgett DE, Bragdon CR, et al. Precision of acetabular cup placement in robotic integrated total hip arthroplasty. Hip Int 2015;25:531–6. https://doi.org/10.5301/hipint.5000289. | 30 (4.29) | 2015 |
| 87 | Marchand RC, Sodhi N, Bhowmik-Stoker M, Scholl L, Condrey C, Khlopas A, et al. Does the Robotic Arm and Preoperative CT Planning Help with 3D Intraoperative Total Knee Arthroplasty Planning? J Knee Surg 2019;32:742–9. https://doi.org/10.1055/s-0038-1668122. | 29 (9.67) | 2019 |
| 88 | Kayani B, Konan S, Thakrar RR, Huq SS, Haddad FS. Assuring the long-term total joint arthroplasty: a triad of variables. Bone Joint J 2019;101-B:11–8. https://doi.org/10.1302/0301-620X.101B1.BJJ-2018-0377.R1. | 29 (9.67) | 2019 |
| 89 | Chen X, Xiong J, Wang P, Zhu S, Qi W, Peng H, et al. Robotic-assisted compared with conventional total hip arthroplasty: systematic review and meta-analysis. Postgrad Med J 2018;94:335–41. https://doi.org/10.1136/postgradmedj-2017-135352. | 29 (7.25) | 2018 |
| 90 | Ren Y, Cao S, Wu J, Weng X, Feng B. Efficacy and reliability of active robotic-assisted total knee arthroplasty compared with conventional total knee arthroplasty: a systematic review and meta-analysis. Postgrad Med J 2019;95:125–33. https://doi.org/10.1136/postgradmedj-2018-136190. | 28 (9.33) | 2019 |
| 91 | Tsai T-Y, Dimitriou D, Li J-S, Kwon Y-M. Does haptic robot-assisted total hip arthroplasty better restore native acetabular and femoral anatomy? Int J Med Robot 2016;12:288–95. https://doi.org/10.1002/rcs.1663. | 28 (4.67) | 2016 |
| 92 | MacCallum KP, Danoff JR, Geller JA. Tibial baseplate positioning in robotic-assisted and conventional unicompartmental knee arthroplasty. Eur J Orthop Surg Traumatol 2016;26:93–8. https://doi.org/10.1007/s00590-015-1708-0. | 28 (4.67) | 2016 |
| 93 | Gupta A, Redmond JM, Hammarstedt JE, Petrakos AE, Vemula SP, Domb BG. Does Robotic-Assisted Computer Navigation Affect Acetabular Cup Positioning in Total Hip Arthroplasty in the Obese Patient? A Comparison Study. J Arthroplasty 2015;30:2204–7. https://doi.org/10.1016/j.arth.2015.06.062. | 28 (4.00) | 2015 |
| 94 | St Mart J-P, de Steiger RN, Cuthbert A, Donnelly W. The 3-year survivorship of robotically assisted vs non-robotically assisted unicompartmental knee arthroplasty. Bone Joint J 2020;102-B:319–28. https://doi.org/10.1302/0301-620X.102B3.BJJ-2019-0713.R1. | 27 (13.50) | 2020 |
| 95 | Burger JA, Kleeblad LJ, Laas N, Pearle AD. Mid-term survivorship and patient-reported outcomes of robotic-arm assisted partial knee arthroplasty. Bone Joint J 2020;102-B:108–16. https://doi.org/10.1302/0301-620X.102B1.BJJ-2019-0510.R1. | 27 (13.50) | 2020 |
| 96 | Sires JD, Craik JD, Wilson CJ. Accuracy of Bone Resection in MAKO Total Knee Robotic-Assisted Surgery. J Knee Surg 2021;34:745–8. https://doi.org/10.1055/s-0039-1700570. | 26 (26.00) | 2021 |
| 97 | Khlopas A, Sodhi N, Hozack WJ, Chen AF, Mahoney OM, Kinsey T, et al. Patient-Reported Functional and Satisfaction Outcomes after Robotic-Arm-Assisted Total Knee Arthroplasty: Early Results of a Prospective Multicenter Investigation. J Knee Surg 2020;33:685–90. https://doi.org/10.1055/s-0039-1684014. | 26 (13.00) | 2020 |
| 98 | Kayani B, Konan S, Ayuob A, Ayyad S, Haddad FS. The current role of robotics in total hip arthroplasty. EFORT Open Rev 2019;4:618–25. https://doi.org/10.1302/2058-5241.4.180088. | 26 (8.67) | 2019 |
| 99 | Karunaratne S, Duan M, Pappas E, Fritsch B, Boyle R, Gupta S, et al. The effectiveness of robotic hip and knee arthroplasty on patient-reported outcomes: A systematic review and meta-analysis. Int Orthop 2019;43:1283–95. https://doi.org/10.1007/s00264-018-4140-3. | 26 (8.67) | 2019 |
| 100 | Perets I, Walsh JP, Close MR, Mu BH, Yuen LC, Domb BG. Robot-assisted total hip arthroplasty: Clinical outcomes and complication rate. Int J Med Robot 2018;14:e1912. https://doi.org/10.1002/rcs.1912. | 26 (6.50) | 2018 |
Number of citations per year since publication.
The mean and median numbers of citations per article were 60.5 and 44.0, respectively. The top 3 articles by citation density had densities of 26.0, 26.0, and 24.5 [1,34,35]. The bottom 3 citation densities were 1.5, 1.6, and 1.8 [[36], [37], [38]]. The oldest published study was published in 1995 and ranked 38 out of 100 articles with 57 citations and a citation density of 2.1 [39].
The top 3 authors by number of published articles in the top 100 were Mont, Haddad, and Kayani with 11, 8, and 8 articles, respectively. The top 3 authors by total number of citations were Davies, Haddad, and Kayani with 481, 466, and 466, respectively. There were a total of 10 authors with 4 or more studies included in this list of the top 100 most-cited articles in robotic arthroplasty [Table 2].
Table 2.
The most represented first and last authors among the top 100 robotic arthroplasty articles.
| Author name | Number of first author publications | Number of last author publications | Number of articles included | Total number of citations | Average citations per publication |
|---|---|---|---|---|---|
| Mont, Michael A. | 0 | 11 | 11 | 451 | 41.0 |
| Haddad, Fares S. | 0 | 8 | 8 | 466 | 58.3 |
| Kayani, Babar | 8 | 0 | 8 | 466 | 58.3 |
| Pearle, Andrew D. | 3 | 4 | 7 | 361 | 51.6 |
| Davies, Brian L. | 1 | 4 | 5 | 481 | 96.2 |
| Domb, Benjamin G. | 2 | 3 | 5 | 284 | 56.8 |
| Bargar, William L. | 2 | 2 | 4 | 436 | 109.0 |
| Song, Eun-Kyoo | 2 | 2 | 4 | 338 | 84.5 |
| Lonner, Jess H. | 3 | 1 | 4 | 240 | 60.0 |
| Marchand, Robert C. | 4 | 0 | 4 | 176 | 44.0 |
All authors with 4 or more first/last author publications included.
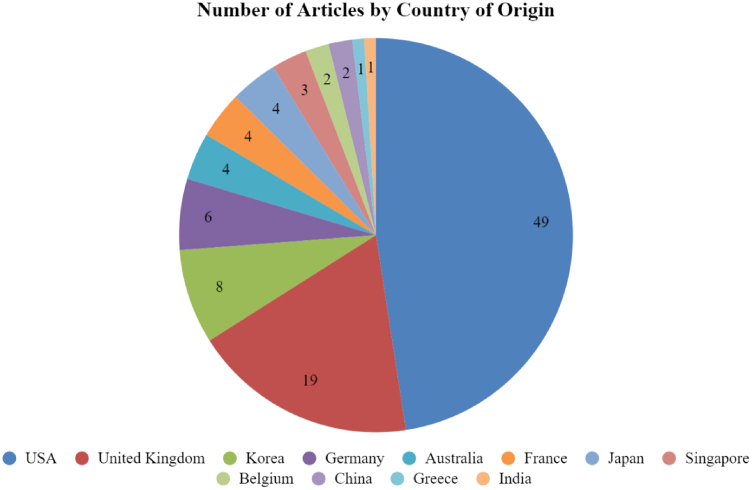
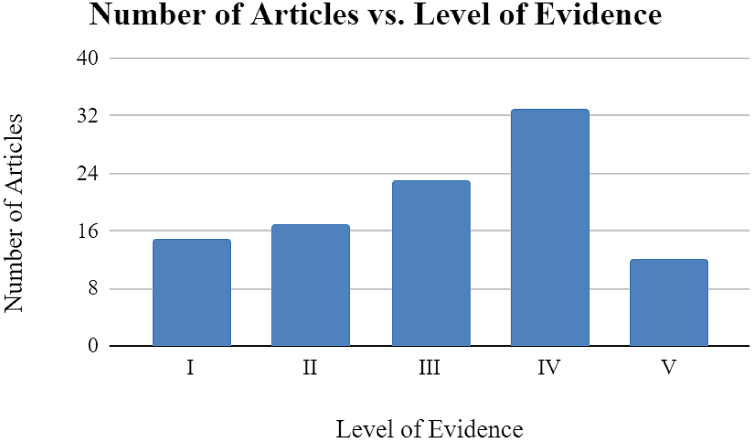
The included articles were published in 29 journals in the United States and internationally. The Journal of Arthroplasty, Journal of Bone and Joint Surgery, and Clinical Orthopaedics and Related Research published the greatest number of robotic arthroplasty studies with 22, 14, and 8 articles, respectively [Table 3]. These articles originated from 12 different countries, with the United States (49), United Kingdom (19), and Korea (8) having published the most articles (Fig. 3). A total of 14 different institutions produced 3 or more articles in the top 100, with University College London (8), Hospital for Special Surgery (7), and Cleveland Clinic (6) producing the most [Table 4]. The most common study types were comparative studies (36), followed by case series (20), and randomized controlled trials (15) [Table 5]. The most common level of evidence was type IV (33), followed by type III (23), and type II (17) (Fig. 4).
Table 3.
The top 100 most-cited robotic arthroplasty journals of origin.
| Journal name | Number of articles |
|---|---|
| Journal of Arthroplasty | 22 |
| Journal of Bone and Joint Surgery | 14 |
| Clinical Orthopaedics and Related Research | 8 |
| Journal of Knee Surgery | 7 |
| Knee Surgery, Sports Traumatology, Arthroscopy | 7 |
| American Journal of Orthopedics | 5 |
| International Journal of Medical Robotics and Computer Assisted Surgery | 4 |
| International Orthopaedics | 3 |
| Knee | 3 |
All journals with 3 or more articles included.
Figure 3.
The number of the top 100 most-cited robotic arthroplasty studies originating from each country.
Table 4.
The top 100 most-cited robotic arthroplasty institutions of origin.
| Institution name | Number of articles |
|---|---|
| University College London | 8 |
| Hospital for Special Surgery | 7 |
| Cleveland Clinic | 6 |
| American Hip Institute | 5 |
| Imperial College London | 5 |
| Chonnam National University | 4 |
| University of California, Davis School of Medicine | 4 |
| Lenox Hill Hospital | 4 |
| Osaka University Medical School | 4 |
| Ortho Rhode Island | 4 |
| Croix-Rousse Hospital | 3 |
| Glasgow Royal Infirmary | 3 |
| Singapore General Hospital | 3 |
| Wake Forest School of Medicine | 3 |
All institutions with greater than 3 articles included.
Table 5.
The top-100 most-cited robotic arthroplasty articles by study type.
| Type of study | Number of articles |
|---|---|
| Randomized controlled trial | 15 |
| Comparative study | 36 |
| Case series | 20 |
| Review article | 11 |
| Cost analysis | 4 |
| Descriptive article | 3 |
| Expert opinion | 11 |
Figure 4.
Categorization of the top 100 most-cited robotic arthroplasty studies by level of evidence.
Of the 100 studies, 98 focused on a specific joint. Of these 98 focused studies, distribution of focus was as follows: 68 knee (69.4%), 27 hip (27.5%), and 3 both hip and knee (3.1%). None of the top 100 articles focused on shoulder, elbow, or ankle arthroplasty. Within the 68 articles focused on the knee joint, 38 centered on total knee arthroplasty (55.9%), 28 explored unicompartmental knee arthroplasty (41.2%), and 2 examined both total knee arthroplasty and unicompartmental knee arthroplasty (2.9%). In addition, 68 of the 100 articles utilized or examined a specific robotic device. The distribution of robotic device name or brand is as follows: 38 studies involved MAKO (55.9%), 20 studies involved ROBODOC (29.4%), 4 studies involved ACROBOT (5.9%), 3 studies involved CASPAR (4.4%), and 3 studies involved NAVIO (4.4%) [Table 6]. Eighty-nine of the 100 studies included information relating to funding or affiliation for the studies, revealing that 64 of the 89 (71.9%) studies were associated with and/or funded by industry.
Table 6.
The top-100 most-cited robotic arthroplasty articles by robot name/brand.
| Robot name/brand | Number of articles |
|---|---|
| ACROBOT | 4 |
| CASPAR | 3 |
| MAKO | 38 |
| NAVIO | 3 |
| ROBODOC | 20 |
The top 100 studies presented a variety of results and clinical findings [Table 7]. Most commonly, 37 studies found an improvement in radiographic outcomes and accuracy using robotic arthroplasty procedures when compared to conventional manual techniques, while 17 studies found an improvement in clinical outcomes when compared to conventional manual techniques. However, 19 studies found no difference in outcomes across robotic and conventional manual techniques, and 6 studies found worse outcomes with robotic techniques when compared to conventional manual techniques. Studies exploring the operating time, cost-effectiveness, and learning curve of the procedure also demonstrated mixed findings.
Table 7.
Clinical summaries of the top-100 most-cited robotic arthroplasty articles.
| Rank | Article citation | Summary |
|---|---|---|
| 1 | Bargar WL, Bauer A, Börner M. Primary and revision total hip replacement using the Robodoc system. Clin Orthop Relat Res 1998:82–91. https://doi.org/10.1097/00003086-199809000-00011. |
|
| 2 | Cobb J, Henckel J, Gomes P, Harris S, Jakopec M, Rodriguez F, et al. Hands-on robotic unicompartmental knee replacement: a prospective, randomised controlled study of the acrobot system. J Bone Joint Surg Br 2006;88:188–97. https://doi.org/10.1302/0301-620X.88B2.17220. |
|
| 3 | Delp SL, Stulberg SD, Davies B, Picard F, Leitner F. Computer assisted knee replacement. Clin Orthop Relat Res 1998:49–56. https://doi.org/10.1097/00003086-199809000-00007. |
|
| 4 | Jacofsky DJ, Allen M. Robotics in Arthroplasty: A Comprehensive Review. J Arthroplasty 2016;31:2353–63. https://doi.org/10.1016/j.arth.2016.05.026. |
|
| 5 | Bell SW, Anthony I, Jones B, MacLean A, Rowe P, Blyth M. Improved Accuracy of Component Positioning with Robotic-Assisted Unicompartmental Knee Arthroplasty: Data from a Prospective, Randomized Controlled Study. J Bone Joint Surg Am 2016;98:627–35. https://doi.org/10.2106/JBJS.15.00664. |
|
| 6 | Siebert W, Mai S, Kober R, Heeckt PF. Technique and first clinical results of robot-assisted total knee replacement. Knee 2002;9:173–80. https://doi.org/10.1016/s0968-0160(02)00015-7. |
|
| 7 | Song E-K, Seon J-K, Yim J-H, Netravali NA, Bargar WL. Robotic-assisted TKA reduces postoperative alignment outliers and improves gap balance compared to conventional TKA. Clin Orthop Relat Res 2013;471:118–26. https://doi.org/10.1007/s11999-012-2407-3. |
|
| 8 | Honl M, Dierk O, Gauck C, Carrero V, Lampe F, Dries S, et al. Comparison of robotic-assisted and manual implantation of a primary total hip replacement. A prospective study. J Bone Joint Surg Am 2003;85:1470–8. https://doi.org/10.2106/00004623-200308000-00007. |
|
| 9 | Domb BG, El Bitar YF, Sadik AY, Stake CE, Botser IB. Comparison of robotic-assisted and conventional acetabular cup placement in THA: a matched-pair controlled study. Clin Orthop Relat Res 2014;472:329–36. https://doi.org/10.1007/s11999-013-3253-7. |
|
| 10 | Lonner JH, John TK, Conditt MA. Robotic arm-assisted UKA improves tibial component alignment: a pilot study. Clin Orthop Relat Res 2010;468:141–6. https://doi.org/10.1007/s11999-009-0977-5. |
|
| 11 | Jakopec M, Harris SJ, Rodriguez y Baena F, Gomes P, Cobb J, Davies BL. The first clinical application of a “hands-on” robotic knee surgery system. Comput Aided Surg 2001;6:329–39. https://doi.org/10.1002/igs.10023. |
|
| 12 | Song E-K, Seon J-K, Park S-J, Jung WB, Park H-W, Lee GW. Simultaneous bilateral total knee arthroplasty with robotic and conventional techniques: a prospective, randomized study. Knee Surg Sports Traumatol Arthrosc 2011;19:1069–76. https://doi.org/10.1007/s00167-011-1400-9. |
|
| 13 | Lang JE, Mannava S, Floyd AJ, Goddard MS, Smith BP, Mofidi A, et al. Robotic systems in orthopaedic surgery. J Bone Joint Surg Br 2011;93:1296–9. https://doi.org/10.1302/0301-620X.93B10.27418. |
|
| 14 | Park SE, Lee CT. Comparison of robotic-assisted and conventional manual implantation of a primary total knee arthroplasty. J Arthroplasty 2007;22:1054–9. https://doi.org/10.1016/j.arth.2007.05.036. |
|
| 15 | Kayani B, Konan S, Tahmassebi J, Pietrzak JRT, Haddad FS. Robotic-arm assisted total knee arthroplasty is associated with improved early functional recovery and reduced time to hospital discharge compared with conventional jig-based total knee arthroplasty: a prospective cohort study. Bone Joint J 2018;100-B:930–7. https://doi.org/10.1302/0301-620X.100B7.BJJ-2017-1449.R1. |
|
| 16 | Liow MHL, Xia Z, Wong MK, Tay KJ, Yeo SJ, Chin PL. Robot-assisted total knee arthroplasty accurately restores the joint line and mechanical axis. A prospective randomised study. J Arthroplasty 2014;29:2373–7. https://doi.org/10.1016/j.arth.2013.12.010. |
|
| 17 | Pearle AD, O’Loughlin PF, Kendoff DO. Robot-assisted unicompartmental knee arthroplasty. J Arthroplasty 2010;25:230–7. https://doi.org/10.1016/j.arth.2008.09.024. |
|
| 18 | Bellemans J, Vandenneucker H, Vanlauwe J. Robot-assisted total knee arthroplasty. Clin Orthop Relat Res 2007;464:111–6. https://doi.org/10.1097/BLO.0b013e318126c0c0. |
|
| 19 | Schulz AP, Seide K, Queitsch C, von Haugwitz A, Meiners J, Kienast B, et al. Results of total hip replacement using the Robodoc surgical assistant system: clinical outcome and evaluation of complications for 97 procedures. Int J Med Robot 2007;3:301–6. https://doi.org/10.1002/rcs.161. |
|
| 20 | Jakopec M, Rodriguez y Baena F, Harris SJ, Gomes P, Cobb J, Davies BL. The hands-on orthopaedic robot “acrobot”: Early clinical trials of total knee replacement surgery. IEEE Transactions on Robotics and Automation 2003;19:902–11. https://doi.org/10.1109/TRA.2003.817510. |
|
| 21 | Dunbar NJ, Roche MW, Park BH, Branch SH, Conditt MA, Banks SA. Accuracy of dynamic tactile-guided unicompartmental knee arthroplasty. J Arthroplasty 2012;27:803-808.e1. https://doi.org/10.1016/j.arth.2011.09.021. |
|
| 22 | Sugano N. Computer-assisted orthopaedic surgery and robotic surgery in total hip arthroplasty. Clin Orthop Surg 2013;5:1–9. https://doi.org/10.4055/cios.2013.5.1.1. |
|
| 23 | Pearle AD, van der List JP, Lee L, Coon TM, Borus TA, Roche MW. Survivorship and patient satisfaction of robotic-assisted medial unicompartmental knee arthroplasty at a minimum 2-year follow-up. Knee 2017;24:419–28. https://doi.org/10.1016/j.knee.2016.12.001. |
|
| 24 | Kayani B, Konan S, Huq SS, Tahmassebi J, Haddad FS. Robotic-arm assisted total knee arthroplasty has a learning curve of seven cases for integration into the surgical workflow but no learning curve effect for accuracy of implant positioning. Knee Surg Sports Traumatol Arthrosc 2019;27:1132–41. https://doi.org/10.1007/s00167-018-5138-5. |
|
| 25 | Blyth MJG, Anthony I, Rowe P, Banger MS, MacLean A, Jones B. Robotic arm-assisted versus conventional unicompartmental knee arthroplasty: Exploratory secondary analysis of a randomised controlled trial. Bone Joint Res 2017;6:631–9. https://doi.org/10.1302/2046-3758.611.BJR-2017-0060.R1. |
|
| 26 | Marchand RC, Sodhi N, Khlopas A, Sultan AA, Harwin SF, Malkani AL, et al. Patient Satisfaction Outcomes after Robotic Arm-Assisted Total Knee Arthroplasty: A Short-Term Evaluation. J Knee Surg 2017;30:849–53. https://doi.org/10.1055/s-0037-1607450. |
|
| 27 | Moschetti WE, Konopka JF, Rubash HE, Genuario JW. Can Robot-Assisted Unicompartmental Knee Arthroplasty Be Cost-Effective? A Markov Decision Analysis. J Arthroplasty 2016;31:759–65. https://doi.org/10.1016/j.arth.2015.10.018. |
|
| 28 | Nakamura N, Sugano N, Nishii T, Kakimoto A, Miki H. A comparison between robotic-assisted and manual implantation of cementless total hip arthroplasty. Clin Orthop Relat Res 2010;468:1072–81. https://doi.org/10.1007/s11999-009-1158-2. |
|
| 29 | Batailler C, White N, Ranaldi FM, Neyret P, Servien E, Lustig S. Improved implant position and lower revision rate with robotic-assisted unicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 2019;27:1232–40. https://doi.org/10.1007/s00167-018-5081-5. |
|
| 30 | Plate JF, Mofidi A, Mannava S, Smith BP, Lang JE, Poehling GG, et al. Achieving accurate ligament balancing using robotic-assisted unicompartmental knee arthroplasty. Adv Orthop 2013;2013:837167. https://doi.org/10.1155/2013/837167. |
|
| 31 | Sodhi N, Khlopas A, Piuzzi NS, Sultan AA, Marchand RC, Malkani AL, et al. The Learning Curve Associated with Robotic Total Knee Arthroplasty. J Knee Surg 2018;31:17–21. |
|
| 32 | Kayani B, Konan S, Pietrzak JRT, Haddad FS. Iatrogenic Bone and Soft Tissue Trauma in Robotic-Arm Assisted Total Knee Arthroplasty Compared With Conventional Jig-Based Total Knee Arthroplasty: A Prospective Cohort Study and Validation of a New Classification System. J Arthroplasty 2018;33:2496–501. https://doi.org/10.1016/j.arth.2018.03.042. |
|
| 33 | Liow MHL, Goh GS-H, Wong MK, Chin PL, Tay DK-J, Yeo S-J. Robotic-assisted total knee arthroplasty may lead to improvement in quality-of-life measures: a 2-year follow-up of a prospective randomized trial. Knee Surg Sports Traumatol Arthrosc 2017;25:2942–51. https://doi.org/10.1007/s00167-016-4076-3. |
|
| 34 | Kayani B, Konan S, Pietrzak JRT, Huq SS, Tahmassebi J, Haddad FS. The learning curve associated with robotic-arm assisted unicompartmental knee arthroplasty: a prospective cohort study. Bone Joint J 2018;100-B:1033–42. https://doi.org/10.1302/0301-620X.100B8.BJJ-2018-0040.R1. |
|
| 35 | Kayani B, Konan S, Tahmassebi J, Rowan FE, Haddad FS. An assessment of early functional rehabilitation and hospital discharge in conventional versus robotic-arm assisted unicompartmental knee arthroplasty: a prospective cohort study. Bone Joint J 2019;101-B:24–33. https://doi.org/10.1302/0301-620X.101B1.BJJ-2018-0564.R2. |
|
| 36 | Domb BG, Redmond JM, Louis SS, Alden KJ, Daley RJ, LaReau JM, et al. Accuracy of Component Positioning in 1980 Total Hip Arthroplasties: A Comparative Analysis by Surgical Technique and Mode of Guidance. J Arthroplasty 2015;30:2208–18. https://doi.org/10.1016/j.arth.2015.06.059. |
|
| 37 | Gilmour A, MacLean AD, Rowe PJ, Banger MS, Donnelly I, Jones BG, et al. Robotic-Arm-Assisted vs Conventional Unicompartmental Knee Arthroplasty. The 2-Year Clinical Outcomes of a Randomized Controlled Trial. J Arthroplasty 2018;33:S109–15. https://doi.org/10.1016/j.arth.2018.02.050. |
|
| 38 | Kazanzides P, Mittelstadt BD, Musits BL, Bargar WL, Zuhars JF, Williamson B, et al. An integrated system for cementless hip replacement. IEEE Engineering in Medicine and Biology Magazine 1995;14:307–13. https://doi.org/10.1109/51.391772. |
|
| 39 | Herry Y, Batailler C, Lording T, Servien E, Neyret P, Lustig S. Improved joint-line restitution in unicompartmental knee arthroplasty using a robotic-assisted surgical technique. Int Orthop 2017;41:2265–71. https://doi.org/10.1007/s00264-017-3633-9. |
|
| 40 | Nishihara S, Sugano N, Nishii T, Miki H, Nakamura N, Yoshikawa H. Comparison between hand rasping and robotic milling for stem implantation in cementless total hip arthroplasty. J Arthroplasty 2006;21:957–66. https://doi.org/10.1016/j.arth.2006.01.001. |
|
| 41 | Decking J, Theis C, Achenbach T, Roth E, Nafe B, Eckardt A. Robotic total knee arthroplasty: the accuracy of CT-based component placement. Acta Orthop Scand 2004;75:573–9. https://doi.org/10.1080/00016470410001448. |
|
| 42 | Yang HY, Seon JK, Shin YJ, Lim HA, Song EK. Robotic Total Knee Arthroplasty with a Cruciate-Retaining Implant: A 10-Year Follow-up Study. Clin Orthop Surg 2017;9:169–76. https://doi.org/10.4055/cios.2017.9.2.169. |
|
| 43 | llgen RL, Bukowski BR, Abiola R, Anderson P, Chughtai M, Khlopas A, et al. Robotic-Assisted Total Hip Arthroplasty: Outcomes at Minimum Two-Year Follow-Up. Surg Technol Int 2017;30:365–72. |
|
| 44 | Plate JF, Augart MA, Seyler TM, Bracey DN, Hoggard A, Akbar M, et al. Obesity has no effect on outcomes following unicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 2017;25:645–51. https://doi.org/10.1007/s00167-015-3597-5. |
|
| 45 | Swank ML, Alkire M, Conditt M, Lonner JH. Technology and cost-effectiveness in knee arthroplasty: computer navigation and robotics. Am J Orthop (Belle Mead NJ) 2009;38:32–6. |
|
| 46 | Hansen DC, Kusuma SK, Palmer RM, Harris KB. Robotic guidance does not improve component position or short-term outcome in medial unicompartmental knee arthroplasty. J Arthroplasty 2014;29:1784–9. https://doi.org/10.1016/j.arth.2014.04.012. |
|
| 47 | Kayani B, Konan S, Ayuob A, Onochie E, Al-Jabri T, Haddad FS. Robotic technology in total knee arthroplasty: a systematic review. EFORT Open Rev 2019;4:611–7. https://doi.org/10.1302/2058-5241.4.190022. |
|
| 48 | Kleeblad LJ, Borus TA, Coon TM, Dounchis J, Nguyen JT, Pearle AD. Midterm Survivorship and Patient Satisfaction of Robotic-Arm-Assisted Medial Unicompartmental Knee Arthroplasty: A Multicenter Study. J Arthroplasty 2018;33:1719–26. https://doi.org/10.1016/j.arth.2018.01.036. |
|
| 49 | Kamara E, Robinson J, Bas MA, Rodriguez JA, Hepinstall MS. Adoption of Robotic vs Fluoroscopic Guidance in Total Hip Arthroplasty: Is Acetabular Positioning Improved in the Learning Curve? J Arthroplasty 2017;32:125–30. https://doi.org/10.1016/j.arth.2016.06.039. |
|
| 50 | Nodzo SR, Chang C-C, Carroll KM, Barlow BT, Banks SA, Padgett DE, et al. Intraoperative placement of total hip arthroplasty components with robotic-arm assisted technology correlates with postoperative implant position: a CT-based study. Bone Joint J 2018;100-B:1303–9. https://doi.org/10.1302/0301-620X.100B10-BJJ-2018-0201.R1. |
|
| 51 | Chun YS, Kim KI, Cho YJ, Kim YH, Yoo MC, Rhyu KH. Causes and patterns of aborting a robot-assisted arthroplasty. J Arthroplasty 2011;26:621–5. https://doi.org/10.1016/j.arth.2010.05.017. |
|
| 52 | Kim Y-H, Yoon S-H, Park J-W. Does Robotic-assisted TKA Result in Better Outcome Scores or Long-Term Survivorship Than Conventional TKA? A Randomized, Controlled Trial. Clin Orthop Relat Res 2020;478:266–75. https://doi.org/10.1097/CORR.0000000000000916. |
|
| 53 | Redmond JM, Gupta A, Hammarstedt JE, Petrakos AE, Finch NA, Domb BG. The learning curve associated with robotic-assisted total hip arthroplasty. J Arthroplasty 2015;30:50–4. https://doi.org/10.1016/j.arth.2014.08.003. |
|
| 54 | Roche M, O’Loughlin PF, Kendoff D, Musahl V, Pearle AD. Robotic arm-assisted unicompartmental knee arthroplasty: preoperative planning and surgical technique. Am J Orthop (Belle Mead NJ) 2009;38:10–5. |
|
| 55 | Marchand RC, Sodhi N, Khlopas A, Sultan AA, Higuera CA, Stearns KL, et al. Coronal Correction for Severe Deformity Using Robotic-Assisted Total Knee Arthroplasty. J Knee Surg 2018;31:2–5. https://doi.org/10.1055/s-0037-1608840. |
|
| 56 | Jeon S-W, Kim K-I, Song SJ. Robot-Assisted Total Knee Arthroplasty Does Not Improve Long-Term Clinical and Radiologic Outcomes. J Arthroplasty 2019;34:1656–61. https://doi.org/10.1016/j.arth.2019.04.007. |
|
| 57 | Cho K-J, Seon J-K, Jang W-Y, Park C-G, Song E-K. Robotic versus conventional primary total knee arthroplasty: clinical and radiological long-term results with a minimum follow-up of 10 years. Int Orthop 2019;43:1345–54. https://doi.org/10.1007/s00264-018-4231-1. |
|
| 58 | Dretakis K, Igoumenou VG. Outcomes of robotic-arm-assisted medial unicompartmental knee arthroplasty: minimum 3-year follow-up. Eur J Orthop Surg Traumatol 2019;29:1305–11. https://doi.org/10.1007/s00590-019-02424-4. |
|
| 59 | Börner M, Bauer A, Lahmer A. Computer-guided robot-assisted hip endoprosthesis. Orthopade 1997;26:251–7. https://doi.org/10.1007/s001320050092. |
|
| 60 | Boylan M, Suchman K, Vigdorchik J, Slover J, Bosco J. Technology-Assisted Hip and Knee Arthroplasties: An Analysis of Utilization Trends. J Arthroplasty 2018;33:1019–23. https://doi.org/10.1016/j.arth.2017.11.033. |
|
| 61 | Liow MHL, Chin PL, Tay KJD, Chia SL, Lo NN, Yeo SJ. Early experiences with robot-assisted total knee arthroplasty using the DigiMatch ROBODOC surgical system. Singapore Med J 2014;55:529–34. https://doi.org/10.11622/smedj.2014136. |
|
| 62 | Lonner JH. Indications for unicompartmental knee arthroplasty and rationale for robotic arm-assisted technology. Am J Orthop (Belle Mead NJ) 2009;38:3–6. |
|
| 63 | Pearle AD, Kendoff D, Stueber V, Musahl V, Repicci JA. Perioperative management of unicompartmental knee arthroplasty using the MAKO robotic arm system (MAKOplasty). Am J Orthop (Belle Mead NJ) 2009;38:16–9. |
|
| 64 | Thienpont E, Fennema P, Price A. Can technology improve alignment during knee arthroplasty. Knee 2013;20 Suppl 1:S21-28. https://doi.org/10.1016/S0968-0160(13)70005-X. |
|
| 65 | Kanawade V, Dorr LD, Banks SA, Zhang Z, Wan Z. Precision of robotic guided instrumentation for acetabular component positioning. J Arthroplasty 2015;30:392–7. https://doi.org/10.1016/j.arth.2014.10.021. |
|
| 66 | Banerjee S, Cherian JJ, Elmallah RK, Jauregui JJ, Pierce TP, Mont MA. Robotic-assisted knee arthroplasty. Expert Rev Med Devices 2015;12:727–35. https://doi.org/10.1586/17434440.2015.1086264. |
|
| 67 | Hananouchi T, Sugano N, Nishii T, Nakamura N, Miki H, Kakimoto A, et al. Effect of robotic milling on periprosthetic bone remodeling. J Orthop Res 2007;25:1062–9. https://doi.org/10.1002/jor.20376. |
|
| 68 | Marchand RC, Sodhi N, Anis HK, Ehiorobo J, Newman JM, Taylor K, et al. One-Year Patient Outcomes for Robotic-Arm-Assisted versus Manual Total Knee Arthroplasty. J Knee Surg 2019;32:1063–8. https://doi.org/10.1055/s-0039-1683977. |
|
| 69 | Cool CL, Jacofsky DJ, Seeger KA, Sodhi N, Mont MA. A 90-day episode-of-care cost analysis of robotic-arm assisted total knee arthroplasty. J Comp Eff Res 2019;8:327–36. https://doi.org/10.2217/cer-2018-0136. |
|
| 70 | Khlopas A, Sodhi N, Sultan AA, Chughtai M, Molloy RM, Mont MA. Robotic Arm-Assisted Total Knee Arthroplasty. J Arthroplasty 2018;33:2002–6. https://doi.org/10.1016/j.arth.2018.01.060. |
|
| 71 | Mofidi A, Plate JF, Lu B, Conditt MA, Lang JE, Poehling GG, et al. Assessment of accuracy of robotically assisted unicompartmental arthroplasty. Knee Surg Sports Traumatol Arthrosc 2014;22:1918–25. https://doi.org/10.1007/s00167-014-2969-6. |
|
| 72 | Davies BL, Rodriguez y Baena FM, Barrett ARW, Gomes MPSF, Harris SJ, Jakopec M, et al. Robotic control in knee joint replacement surgery. Proc Inst Mech Eng H 2007;221:71–80. https://doi.org/10.1243/09544119JEIM250. |
|
| 73 | Canetti R, Batailler C, Bankhead C, Neyret P, Servien E, Lustig S. Faster return to sport after robotic-assisted lateral unicompartmental knee arthroplasty: a comparative study. Arch Orthop Trauma Surg 2018;138:1765–71. https://doi.org/10.1007/s00402-018-3042-6. |
|
| 74 | Antonios JK, Korber S, Sivasundaram L, Mayfield C, Kang HP, Oakes DA, et al. Trends in computer navigation and robotic assistance for total knee arthroplasty in the United States: an analysis of patient and hospital factors. Arthroplasty Today 2019;5:88–95. https://doi.org/10.1016/j.artd.2019.01.002. |
|
| 75 | van der List JP, Chawla H, Joskowicz L, Pearle AD. Current state of computer navigation and robotics in unicompartmental and total knee arthroplasty: a systematic review with meta-analysis. Knee Surg Sports Traumatol Arthrosc 2016;24:3482–95. https://doi.org/10.1007/s00167-016-4305-9. |
|
| 76 | Rodriguez F, Harris S, Jakopec M, Barrett A, Gomes P, Henckel J, et al. Robotic clinical trials of uni-condylar arthroplasty. The International Journal of Medical Robotics and Computer Assisted Surgery 2005;1:20–8. https://doi.org/10.1002/rcs.52. |
|
| 77 | Bukowski BR, Anderson P, Khlopas A, Chughtai M, Mont MA, Illgen RL. Improved Functional Outcomes with Robotic Compared with Manual Total Hip Arthroplasty. Surg Technol Int 2016;29:303–8. |
|
| 78 | Clement ND, Deehan DJ, Patton JT. Robot-assisted unicompartmental knee arthroplasty for patients with isolated medial compartment osteoarthritis is cost-effective: a Markov decision analysis. Bone Joint J 2019;101-B:1063–70. https://doi.org/10.1302/0301-620X.101B9.BJJ-2018-1658.R1. |
|
| 79 | Robinson PG, Clement ND, Hamilton D, Blyth MJG, Haddad FS, Patton JT. A systematic review of robotic-assisted unicompartmental knee arthroplasty: prosthesis design and type should be reported. Bone Joint J 2019;101-B:838–47. https://doi.org/10.1302/0301-620X.101B7.BJJ-2018-1317.R1. |
|
| 80 | Lonner JH, Fillingham YA. Pros and Cons: A Balanced View of Robotics in Knee Arthroplasty. J Arthroplasty 2018;33:2007–13. https://doi.org/10.1016/j.arth.2018.03.056. |
|
| 81 | Bargar WL, Parise CA, Hankins A, Marlen NA, Campanelli V, Netravali NA. Fourteen Year Follow-Up of Randomized Clinical Trials of Active Robotic-Assisted Total Hip Arthroplasty. J Arthroplasty 2018;33:810–4. https://doi.org/10.1016/j.arth.2017.09.066. |
|
| 82 | Netravali NA, Shen F, Park Y, Bargar WL. A perspective on robotic assistance for knee arthroplasty. Adv Orthop 2013;2013:970703. https://doi.org/10.1155/2013/970703. |
|
| 83 | Siebel T, Käfer W. Clinical outcome following robotic assisted versus conventional total hip arthroplasty: a controlled and prospective study of seventy-one patients. Z Orthop Ihre Grenzgeb 2005;143:391–8. https://doi.org/10.1055/s-2005-836776. |
|
| 84 | Bach CM, Winter P, Nogler M, Göbel G, Wimmer C, Ogon M. No functional impairment after Robodoc total hip arthroplasty. Acta Orthopaedica Scandinavica 2002;73:386–91. https://doi.org/10.1080/00016470216316. |
|
| 85 | Sultan AA, Piuzzi N, Khlopas A, Chughtai M, Sodhi N, Mont MA. Utilization of robotic-arm assisted total knee arthroplasty for soft tissue protection. Expert Rev Med Devices 2017;14:925–7. https://doi.org/10.1080/17434440.2017.1392237. |
|
| 86 | Elson L, Dounchis J, Illgen R, Marchand RC, Padgett DE, Bragdon CR, et al. Precision of acetabular cup placement in robotic integrated total hip arthroplasty. Hip Int 2015;25:531–6. https://doi.org/10.5301/hipint.5000289. |
|
| 87 | Marchand RC, Sodhi N, Bhowmik-Stoker M, Scholl L, Condrey C, Khlopas A, et al. Does the Robotic Arm and Preoperative CT Planning Help with 3D Intraoperative Total Knee Arthroplasty Planning? J Knee Surg 2019;32:742–9. https://doi.org/10.1055/s-0038-1668122. |
|
| 88 | Kayani B, Konan S, Thakrar RR, Huq SS, Haddad FS. Assuring the long-term total joint arthroplasty: a triad of variables. Bone Joint J 2019;101-B:11–8. https://doi.org/10.1302/0301-620X.101B1.BJJ-2018-0377.R1. |
|
| 89 | Chen X, Xiong J, Wang P, Zhu S, Qi W, Peng H, et al. Robotic-assisted compared with conventional total hip arthroplasty: systematic review and meta-analysis. Postgrad Med J 2018;94:335–41. https://doi.org/10.1136/postgradmedj-2017-135352. |
|
| 90 | Ren Y, Cao S, Wu J, Weng X, Feng B. Efficacy and reliability of active robotic-assisted total knee arthroplasty compared with conventional total knee arthroplasty: a systematic review and meta-analysis. Postgrad Med J 2019;95:125–33. https://doi.org/10.1136/postgradmedj-2018-136190. |
|
| 91 | Tsai T-Y, Dimitriou D, Li J-S, Kwon Y-M. Does haptic robot-assisted total hip arthroplasty better restore native acetabular and femoral anatomy? Int J Med Robot 2016;12:288–95. https://doi.org/10.1002/rcs.1663. |
|
| 92 | MacCallum KP, Danoff JR, Geller JA. Tibial baseplate positioning in robotic-assisted and conventional unicompartmental knee arthroplasty. Eur J Orthop Surg Traumatol 2016;26:93–8. https://doi.org/10.1007/s00590-015-1708-0. |
|
| 93 | Gupta A, Redmond JM, Hammarstedt JE, Petrakos AE, Vemula SP, Domb BG. Does Robotic-Assisted Computer Navigation Affect Acetabular Cup Positioning in Total Hip Arthroplasty in the Obese Patient? A Comparison Study. J Arthroplasty 2015;30:2204–7. https://doi.org/10.1016/j.arth.2015.06.062. |
|
| 94 | St Mart J-P, de Steiger RN, Cuthbert A, Donnelly W. The 3-year survivorship of robotically assisted versus non-robotically assisted unicompartmental knee arthroplasty. Bone Joint J 2020;102-B:319–28. https://doi.org/10.1302/0301-620X.102B3.BJJ-2019-0713.R1. |
|
| 95 | Burger JA, Kleeblad LJ, Laas N, Pearle AD. Mid-term survivorship and patient-reported outcomes of robotic-arm assisted partial knee arthroplasty. Bone Joint J 2020;102-B:108–16. https://doi.org/10.1302/0301-620X.102B1.BJJ-2019-0510.R1. |
|
| 96 | Sires JD, Craik JD, Wilson CJ. Accuracy of Bone Resection in MAKO Total Knee Robotic-Assisted Surgery. J Knee Surg 2021;34:745–8. https://doi.org/10.1055/s-0039-1700570. |
|
| 97 | Khlopas A, Sodhi N, Hozack WJ, Chen AF, Mahoney OM, Kinsey T, et al. Patient-Reported Functional and Satisfaction Outcomes after Robotic-Arm-Assisted Total Knee Arthroplasty: Early Results of a Prospective Multicenter Investigation. J Knee Surg 2020;33:685–90. https://doi.org/10.1055/s-0039-1684014. |
|
| 98 | Kayani B, Konan S, Ayuob A, Ayyad S, Haddad FS. The current role of robotics in total hip arthroplasty. EFORT Open Rev 2019;4:618–25. https://doi.org/10.1302/2058-5241.4.180088. |
|
| 99 | Karunaratne S, Duan M, Pappas E, Fritsch B, Boyle R, Gupta S, et al. The effectiveness of robotic hip and knee arthroplasty on patient-reported outcomes: A systematic review and meta-analysis. Int Orthop 2019;43:1283–95. https://doi.org/10.1007/s00264-018-4140-3. |
|
| 100 | Perets I, Walsh JP, Close MR, Mu BH, Yuen LC, Domb BG. Robot-assisted total hip arthroplasty: Clinical outcomes and complication rate. Int J Med Robot 2018;14:e1912. https://doi.org/10.1002/rcs.1912. |
|
Discussion
The field of robotic arthroplasty is young and rapidly growing. The oldest article included in this analysis was published in 1995, representing only 27 years of research history. The novelty of this surgical technique within orthopaedic surgery is reflected by the fact that the 100 most influential studies in robotic arthroplasty are primarily composed of comparative studies (36) and case series (20) and are level IV (33) and III (23) evidence. This relatively short history of research and development likely explains the predominance of comparative studies and case series. However, a reasonable proportion of studies (15%) were randomized controlled trials. Despite the novelty of robotics in orthopaedic surgery, several high-level evidence studies have been published and serve as the foundation that has supported the expeditious adoption and growth of this surgical technique worldwide [10,40]. We postulate that more reports with level I evidence will emerge as the field of robotic arthroplasty continues to mature. Publication of high-quality studies will become increasingly important as the debate surrounding the cost-effectiveness and associated outcomes of robotic arthroplasty systems progresses [41]. For these platforms to continue their swift adoption and utilization growth, additional high-quality evidence in the form of randomized controlled trials with specific analyses of patient-reported outcomes will be necessary.
Notably, we observed an exponential rise in citation generation by year for the top 100 most influential papers in robotic arthroplasty (Fig. 2). Between 1997 and 2021, 5770 total citations were accumulated by these 100 articles. However, nearly one-half of these citations were generated in the past 2 years (2790 between 2020 and 2021), and over two-thirds of the citations were accumulated in the past 4 years (3940 between 2018 and 2021). While similar bibliometric analyses analyzing orthopaedic procedures such as knee arthroscopy, hip arthroscopy, total hip arthroplasty, and ankle arthroplasty found rapid growth in citation accumulation, no other topic areas have observed the same high rate of growth as seen in robotic arthroplasty [20,21,23,42]. The difference noted between this study and other similar bibliometric analyses regarding citation accumulation may be attributed to the novelty of this surgical technique. Commonly used orthopaedic techniques like arthroscopy and joint arthroplasty have been in existence for many decades [43,44]. However, robotically assisted arthroplasty has only been used for approximately 25 years [1] with more widespread adoption taking place in the past 10-20 years.
The country of origin of the top 100 most cited articles was quite varied, with the United States possessing the most publications (49). The United Kingdom had the second most with 19 publications, followed by Korea and Germany with 8 and 6, respectively. These findings are consistent with previous orthopaedic bibliometric analyses. Moore et al. and Murphy et al. found that within shoulder and knee arthroscopy research, the United States was responsible for 62% and 52% of article generation, respectively [21,42]. Additionally, Zhang et al. found that 37% of the top 100 most cited hip arthroplasty articles originated in the United States [23]. Similarly to other fields within orthopaedic surgery, the research generation for robotic arthroplasty has been a global effort led by the United States and supported by many other European and Asian countries.
Among the top 100 most influential robotic arthroplasty articles, a few specific institutions and authors were well represented. Specifically, the University College of London, the Hospital for Special Surgery, and the Cleveland Clinic were responsible for approximately 20% of all articles included. Institutional origin is likely to play a substantial role in the citation generation and subsequent influence an article has in its field. In a study by Abed et al., the authors found that the institution of origin and the prestige of an affiliated medical school or university were significantly correlated with citation generation and citation rate for orthopaedic sports medicine journals specifically [45]. This is evidenced in our analysis as well, with many highly prestigious institutions being responsible for several of the most influential robotic arthroplasty research items. However, it is difficult to determine causation in this situation. Perhaps prestige and reputation were less important for citation generation but allowed the authors access to high-quality data and resources to publish highly impactful research.
The content of the articles included in this analysis was also quite varied. Regarding the joint of focus, 68 studies analyzed only the knee, 27 focused on only the hip, and 3 focused on both the knee and hip. Interestingly, no studies were included analyzing robotic ankle, shoulder, or elbow arthroplasty. While robotic arthroplasty technology exists for each of these joints, hip and knee arthroplasty comprise the vast majority of all arthroplasty procedures worldwide and are more readily studied. As robotic systems become more advanced, cheaper, and widespread, studies in these other arthroplasty procedures are anticipated.
Additionally, a total of 5 different robotic arthroplasty technology platforms were represented in the top 100 articles, with MAKO (38) being the most common. Currently, Stryker and their MAKO robotic arthroplasty system are the leaders in the robotic arthroplasty market due to their rapid expansion and growth to metropolitan surgical centers capable of purchasing their $1 million device [46]. However, as the technology continues to advance and becomes more ubiquitous, in addition to eventual patent expiration, new companies are likely to enter the market and may offer lower price points and different technological features.
Notably, 64 of 89 studies (71.9%) with relevant information available were associated with and/or funded by industry. This reveals how the industry has had a large influence on the research landscape of robotic arthroplasty thus far. We speculate that as robotic arthroplasty becomes less novel, more and more industry-independent studies will be conducted.
Finally, the clinical findings of the top 100 most-cited robotic arthroplasty studies indicate a predominating focus within the literature on improved radiographic outcomes when assessing robotic arthroplasty techniques. While other studies in the top 100 demonstrate mixed results, it is clear that more studies exploring long-term clinical outcomes with robotic arthroplasties are necessary to definitively evaluate this newer technique.
Limitations
This study has several limitations. First, while the selection criteria used to obtain the top 100 articles in robotic arthroplasty were well-defined and very comprehensive, they were partially subjective in nature. However, the authors maintained objectivity as much as possible in the review and selection of articles by having multiple authors involved in the selection process. Secondly, while citation accumulation is an important metric that can objectively assess an article’s influence on a specific field, it is not the only factor that contributes to an article’s impact. Other factors influencing citation frequency include research funding disparities, positive outcome bias, time since the publication date, institutional prestige, and dissemination bias. Therefore, articles with fewer total citations but a substantial impact on clinical and surgical practice may have been overlooked in the present analysis. However, total number of citations serves as an objective metric that can be used to stratify the literature and avoid as much ambiguity as possible. Finally, the Web of Knowledge Database that was used for this analysis, while comprehensive, may have excluded certain articles by either search criteria discrepancies or the tabulation of article citations.
Conclusions
Research on robotic arthroplasty is rapidly growing and originates from a wide variety of countries, academic institutions, and with significant industry influence. This article serves as a reference to direct orthopaedic practitioners to the 100 most influential studies in robotic arthroplasty. We hope that these 100 studies and the analysis we provide aid healthcare professionals in efficiently assessing consensus, trends, and needs within the field.
Appendix
The final Boolean search terms used to generate the largest number of results were: “(arthroplasty (OR) joint arthroplasty (OR) joint replacement (OR) knee arthroplasty (OR) knee replacement (OR) hip arthroplasty (OR) hip replacement (OR) shoulder arthroplasty (OR) shoulder replacement (OR) ankle arthroplasty (OR) ankle replacement (OR) joint reconstruction (OR) total knee arthroplasty (OR) total knee replacement (OR) total hip arthroplasty (OR) total hip replacement (OR) total ankle arthroplasty (OR) total ankle replacement (OR) total shoulder arthroplasty (OR) total shoulder replacement (OR) partial knee arthroplasty (OR) unicompartmental knee arthroplasty (OR) partial knee replacement (OR) unicompartmental knee replacement) AND (robotic surgery (OR) robotic technology (OR) robotic systems (OR) robotics (OR) robot-assisted surgery (OR) robot assisted surgery (OR) robotic-arm assisted surgery (OR) robotic arm assisted surgery (OR) robotic (OR) robot)”.
Conflicts of interest
The authors declare there are no conflicts of interest.
For full disclosure statements refer to https://doi.org/10.1016/j.artd.2023.101153.
Appendix A. Supplementary Data
References
- 1.Jacofsky D.J., Allen M. Robotics in arthroplasty: a comprehensive review. J Arthroplasty. 2016;31:2353–2363. doi: 10.1016/j.arth.2016.05.026. [DOI] [PubMed] [Google Scholar]
- 2.Faust R.A. Robotics in surgery: history, current and future applications. Nova Publishers; Hauppauge, New York: 2007. [Google Scholar]
- 3.Gilmour A., MacLean A.D., Rowe P.J., Banger M.S., Donnelly I., Jones B.G., et al. Robotic-arm-assisted vs conventional unicompartmental knee arthroplasty. The 2-year clinical outcomes of a randomized controlled trial. J Arthroplasty. 2018;33:S109–S115. doi: 10.1016/j.arth.2018.02.050. [DOI] [PubMed] [Google Scholar]
- 4.Li C., Wang L., Perka C., Trampuz A. Clinical application of robotic orthopedic surgery: a bibliometric study. BMC Musculoskelet Disord. 2021;22:968. doi: 10.1186/s12891-021-04714-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bargar W.L. Robots in orthopaedic surgery: past, present, and future. Clin Orthop Relat Res. 2007;463:31–36. [PubMed] [Google Scholar]
- 6.Deckey D.G., Rosenow C.S., Verhey J.T., Brinkman J.C., Mayfield C.K., Clarke H.D., et al. Robotic-assisted total knee arthroplasty improves accuracy and precision compared to conventional techniques. Bone Joint J. 2021;103-B:74–80. doi: 10.1302/0301-620X.103B6.BJJ-2020-2003.R1. [DOI] [PubMed] [Google Scholar]
- 7.Ng N., Gaston P., Simpson P.M., Macpherson G.J., Patton J.T., Clement N.D. Robotic arm-assisted versus manual total hip arthroplasty : a systematic review and meta-analysis. Bone Joint J. 2021;103-B:1009–1020. doi: 10.1302/0301-620X.103B6.BJJ-2020-1856.R1. [DOI] [PubMed] [Google Scholar]
- 8.de Steiger R.N., Liu Y.-L., Graves S.E. Computer navigation for total knee arthroplasty reduces revision rate for patients less than sixty-five years of age. J Bone Joint Surg Am. 2015;97:635–642. doi: 10.2106/JBJS.M.01496. [DOI] [PubMed] [Google Scholar]
- 9.Agarwal N., To K., McDonnell S., Khan W. Clinical and radiological outcomes in robotic-assisted total knee arthroplasty: a systematic review and meta-analysis. J Arthroplasty. 2020;35:3393–3409.e2. doi: 10.1016/j.arth.2020.03.005. [DOI] [PubMed] [Google Scholar]
- 10.Brinkman J.C., Christopher Z.K., Moore M.L., Pollock J.R., Haglin J.M., Bingham J.S. Patient interest in robotic total joint arthroplasty is exponential: a 10-year google trends analysis. Arthroplast Today. 2022;15:13–18. doi: 10.1016/j.artd.2022.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jeon S.-W., Kim K.-I., Song S.J. Robot-assisted total knee arthroplasty does not improve long-term clinical and radiologic outcomes. J Arthroplasty. 2019;34:1656–1661. doi: 10.1016/j.arth.2019.04.007. [DOI] [PubMed] [Google Scholar]
- 12.Sherman W.F., Wu V.J. Robotic surgery in total joint arthroplasty: a survey of the AAHKS membership to understand the utilization, motivations, and perceptions of total joint surgeons. J Arthroplasty. 2020;35:3474–3481.e2. doi: 10.1016/j.arth.2020.06.072. [DOI] [PubMed] [Google Scholar]
- 13.Antonios J.K., Korber S., Sivasundaram L., Mayfield C., Kang H.P., Oakes D.A., et al. Trends in computer navigation and robotic assistance for total knee arthroplasty in the United States: an analysis of patient and hospital factors. Arthroplast Today. 2019;5:88–95. doi: 10.1016/j.artd.2019.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Adams A.B., Simonson D. Publication, citations, and impact factors of leading investigators in critical care medicine. Respir Care. 2004;49:276–281. [PubMed] [Google Scholar]
- 15.Garfield E. Citation analysis as a tool in journal evaluation. Science. 1972;178:471–479. doi: 10.1126/science.178.4060.471. [DOI] [PubMed] [Google Scholar]
- 16.Merigó J.M., Núñez A. Influential journals in health research: a bibliometric study. Global Health. 2016;12:46. doi: 10.1186/s12992-016-0186-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Garfield E. Which medical journals have the greatest impact? Ann Intern Med. 1986;105:313–320. doi: 10.7326/0003-4819-105-2-313. [DOI] [PubMed] [Google Scholar]
- 18.McQuivey K.S., Moore M.L., Pollock J.R., Hassebrock J.D., Patel K.A., Chhabra A. Top-100 most-cited sports-related concussion articles focus on symptomatology, epidemiology, and demographics. Arthrosc Sports Med Rehabil. 2021;3:e1585–e1597. doi: 10.1016/j.asmr.2021.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Huo Y., Pan X., Li Q., Wang X., Jiao X., Jia Z., et al. Fifty top-cited classic papers in orthopedic elbow surgery: a bibliometric analysis. Int J Surg. 2015;18:28–33. doi: 10.1016/j.ijsu.2015.03.020. [DOI] [PubMed] [Google Scholar]
- 20.Malik A.T., Noordin S. The Top 50 most-cited articles on Total Ankle Arthroplasty: a bibliometric analysis. Orthop Rev (Pavia) 2018;10:7498. doi: 10.4081/or.2018.7498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moore M.L., Pollock J.R., McQuivey K.S., Bingham J.S. The top 50 most-cited shoulder arthroscopy studies. Arthrosc Sports Med Rehabil. 2021;3:e277–e287. doi: 10.1016/j.asmr.2020.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yakkanti R., Greif D.N., Wilhelm J., Allegra P.R., Yakkanti R., Hernandez V.H. Unicondylar knee arthroplasty: a bibliometric analysis of the 50 most commonly cited studies. Arthroplast Today. 2020;6:931–940. doi: 10.1016/j.artd.2020.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhang W., Tang N., Li X., George D.M., He G., Huang T. The top 100 most cited articles on total hip arthroplasty: a bibliometric analysis. J Orthop Surg Res. 2019;14:412. doi: 10.1186/s13018-019-1476-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Griffin Z.D., Pollock J.R., Moore M.L., McQuivey K.S., Arthur J.R., Chhabra A. The most highly cited publications on basketball originate from English-speaking countries, are published after 2000, are focused on medicine-related topics, and are level III evidence. Arthrosc Sports Med Rehabil. 2022;4:e891–e898. doi: 10.1016/j.asmr.2021.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ahmad S.S., Evangelopoulos D.S., Abbasian M., Röder C., Kohl S. The hundred most-cited publications in orthopaedic knee research. J Bone Joint Surg Am. 2014;96:e190. doi: 10.2106/JBJS.N.00029. [DOI] [PubMed] [Google Scholar]
- 26.Cassar Gheiti A.J., Downey R.E., Byrne D.P., Molony D.C., Mulhall K.J. The 25 most cited articles in arthroscopic orthopaedic surgery. Arthroscopy. 2012;28:548–564. doi: 10.1016/j.arthro.2011.08.312. [DOI] [PubMed] [Google Scholar]
- 27.Lefaivre K.A., Shadgan B., O’Brien P.J. 100 most cited articles in orthopaedic surgery. Clin Orthop Relat Res. 2011;469:1487–1497. doi: 10.1007/s11999-010-1604-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Holzer L.A., Holzer G. The 50 highest cited papers in hip and knee arthroplasty. J Arthroplasty. 2014;29:453–457. doi: 10.1016/j.arth.2013.07.022. [DOI] [PubMed] [Google Scholar]
- 29.Baldwin K.D., Kovatch K., Namdari S., Sankar W., Flynn J.M., Dormans J.P. The 50 most cited articles in pediatric orthopedic surgery. J Pediatr Orthop B. 2012;21:463–468. doi: 10.1097/BPB.0b013e328354b0cf. [DOI] [PubMed] [Google Scholar]
- 30.To P., Atkinson C.T., Lee D.H., Pappas N.D. The most cited articles in hand surgery over the past 20-plus years: a modern-day reading list. J Hand Surg Am. 2013;38:983–987. doi: 10.1016/j.jhsa.2013.02.004. [DOI] [PubMed] [Google Scholar]
- 31.Barbera J., Selverian S., Courington R., Mikhail C., Colvin A. The top 50 most influential articles in hip arthroscopy. Arthroscopy. 2020;36:716–722. doi: 10.1016/j.arthro.2019.09.031. [DOI] [PubMed] [Google Scholar]
- 32.Namdari S., Baldwin K., Kovatch K., Huffman G.R., Glaser D. Fifty most cited articles in orthopedic shoulder surgery. J Shoulder Elbow Surg. 2012;21:1796–1802. doi: 10.1016/j.jse.2011.11.040. [DOI] [PubMed] [Google Scholar]
- 33.Wright J.G., Swiontkowski M.F., Heckman J.D. Introducing levels of evidence to the journal. J Bone Joint Surg Am. 2003;85:1–3. [PubMed] [Google Scholar]
- 34.Kayani B., Konan S., Tahmassebi J., Pietrzak J.R.T., Haddad F.S. Robotic-arm assisted total knee arthroplasty is associated with improved early functional recovery and reduced time to hospital discharge compared with conventional jig-based total knee arthroplasty: a prospective cohort study. Bone Joint J. 2018;100-B:930–937. doi: 10.1302/0301-620X.100B7.BJJ-2017-1449.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sires J.D., Craik J.D., Wilson C.J. Accuracy of Bone resection in MAKO total knee robotic-assisted surgery. J Knee Surg. 2021;34:745–748. doi: 10.1055/s-0039-1700570. [DOI] [PubMed] [Google Scholar]
- 36.Bach C.M., Winter P., Nogler M., Göbel G., Wimmer C., Ogon M. No functional impairment after Robodoc total hip arthroplasty. Acta Orthop Scand. 2002;73:386–391. doi: 10.1080/00016470216316. [DOI] [PubMed] [Google Scholar]
- 37.Börner M., Bauer A., Lahmer A. Computer-guided robot-assisted hip endoprosthesis. Orthopade. 1997;26:251–257. doi: 10.1007/s001320050092. [DOI] [PubMed] [Google Scholar]
- 38.Siebel T., Käfer W. Clinical outcome following robotic assisted versus conventional total hip arthroplasty: a controlled and prospective study of seventy-one patients. Z Orthop Ihre Grenzgeb. 2005;143:391–398. doi: 10.1055/s-2005-836776. [DOI] [PubMed] [Google Scholar]
- 39.Kazanzides P., Mittelstadt B.D., Musits B.L., Bargar W.L., Zuhars J.F., Williamson B., et al. An integrated system for cementless hip replacement. IEEE Eng Med Biol Mag. 1995;14:307–313. doi: 10.1109/51.391772. [DOI] [Google Scholar]
- 40.Chen X., Deng S., Sun M.-L., He R. Robotic arm-assisted arthroplasty: the latest developments. Chin J Traumatol. 2022;25:125–131. doi: 10.1016/j.cjtee.2021.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.St Mart J.-P., Goh E.L. The current state of robotics in total knee arthroplasty. EFORT Open Rev. 2021;6:270–279. doi: 10.1302/2058-5241.6.200052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Murphy S.N., Moore M.L., Pollock J.R., McQuivey K.S., Bingham J.S. The top 50 most-cited knee arthroscopy studies. Arthrosc Sports Med Rehabil. 2021;3:e1243–e1253. doi: 10.1016/j.asmr.2021.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Jackson R.W. A history of arthroscopy. Arthroscopy. 2010;26:91–103. doi: 10.1016/j.arthro.2009.10.005. [DOI] [PubMed] [Google Scholar]
- 44.Steinberg D.R., Steinberg M.E. The early history of arthroplasty in the United States. Clin Orthop Relat Res. 2000;374:55–89. doi: 10.1097/00003086-200005000-00007. [DOI] [PubMed] [Google Scholar]
- 45.Abed V., Koolmees D.S., Elhage K., Hessburg L., Makhni E.C. Institution origin and medical school rank impact the citation frequency and publication rate in orthopaedic sports medicine journals. Arthrosc Sports Med Rehabil. 2022;4:e295–e300. doi: 10.1016/j.asmr.2021.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Clarivate DBM Expert Orthopedic surgical robotics market: competitive landscape. 2021. https://clarivate.com/blog/orthopedic-surgical-robotics-market-competitive-landscape/
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.