Abstract
BACKGROUND
Cesarean delivery is a major source of maternal morbidity, and repeat cesarean delivery accounts for 40% of cesarean delivery, but recent data on the trial of labor after cesarean and vaginal birth after cesarean are limited.
OBJECTIVE
This study aimed to report the national rates of trial of labor after cesarean and vaginal birth after cesarean by number of previous cesarean deliveries and examine the effect of demographic and clinical characteristics on these rates.
STUDY DESIGN
This was a population-based cohort study using the US natality data files. The study sample was restricted to 4,135,247 nonanomalous singleton, cephalic deliveries between 37 and 42 weeks of gestation, with a history of previous cesarean delivery and delivered in a hospital between 2010 and 2019. Deliveries were grouped by number of previous cesarean deliveries (1, 2, or ≥3). The trial of labor after cesarean (deliveries with labor among deliveries with previous cesarean delivery) and vaginal birth after cesarean (vaginal deliveries among trial of labor after cesarean) rates were computed for each year. The rates were further subgrouped by history of previous vaginal delivery. Year of delivery, number of previous cesarean deliveries, history of previous cesarean delivery, age, race and ethnicity, maternal education, obesity, diabetes mellitus, hypertension, inadequate prenatal care, Medicaid payer, and gestational age were examined concerning the trial of labor after cesarean and vaginal birth after cesarean using multiple logistic regression. SAS software (version 9.4) was used for all analyses.
RESULTS
The trial of labor after cesarean rates increased from 14.4% in 2010 to 19.6% in 2019 (P<.001). This trend was seen in all categories of number of previous cesarean deliveries. Moreover, vaginal birth after cesarean rates increased from 68.5% in 2010 to 74.3% in 2019. The trial of labor after cesarean and vaginal birth after cesarean rates were the highest for deliveries with a history of both 1 previous cesarean delivery and a vaginal delivery (28.9% and 79.7%, respectively) and the lowest for those with a history of ≥3 previous cesarean deliveries and no history of vaginal delivery (4.5% and 46.9%, respectively). Factors associated with the trial of labor after cesarean and vaginal birth after cesarean rates are similar, but several factors have different directions of effect, such as non-White race and ethnicity, which is associated with a higher likelihood of trial of labor after cesarean but a lower likelihood of successful vaginal birth after cesarean.
CONCLUSION
More than 80% of patients with a history of previous cesarean delivery deliver by repeat scheduled cesarean delivery. With vaginal birth after cesarean rates increasing among those who attempt a trial of labor after cesarean, emphasis should be put on safely increasing the trial of labor after cesarean rates.
Key words: cesarean, trial of labor after cesarean, vaginal birth after cesarean, vaginal delivery
AJOG Global Reports at a Glance.
Why was this study conducted?
This study aimed to evaluate recent trends in the trial of labor after cesarean (TOLAC) and vaginal birth after cesarean (VBAC) and to investigate the predictors of TOLAC and VBAC.
Key findings
The TOLAC and VBAC rates increased from 2010 to 2019. TOLAC occurred in 21.9%, 7.1%, and 4.8% of deliveries with 1, 2, and ≥3 previous cesarean deliveries (CDs), respectively. Among patients with 1 previous CD and a history of vaginal delivery, 28.9% of patients underwent TOLAC.
What does this add to what is known?
The TOLAC rates are low but are increasing since 2010, countering the decrease that occurred in the 2000s.
Introduction
Cesarean delivery (CD) is a lifesaving procedure, and in a worldwide analysis, the national rates of CD of up to 19% were associated with lowered maternal and neonatal mortality rates.1 However, in a given delivery, CD is associated with an elevated risk of maternal mortality compared with vaginal delivery (VD).2 In the United States, where the CD rate is 30% (range, 7%–56%), an increase of 1% in the hospital CD rate was associated with a 3.3% increase in severe maternal morbidity.3 In addition to these immediate risks of CD, the risks of multiple repeat CD include placenta accreta spectrum disorders, unplanned hysterectomy, blood transfusion, cystotomy, bowel injury, ureteral injury, placenta previa, ileus, need for maternal mechanical ventilation, or intensive care unit admission.4 Placenta accreta spectrum disorders account for most morbidities, and their incidence is increasing secondary to the increased rate of multiple repeat CD.5
More than one-fifth of all deliveries in the United States are by primary CD, and most pregnant individuals with a previous CD undergo repeat CD.6 Trial of labor after cesarean (TOLAC) is considered safe, and the American College of Obstetricians and Gynecologists states that most women with 1 previous CD with a low transverse incision are candidates for TOLAC. However, in the most recent meta-analysis published in 2010, the TOLAC rate among eligible candidates was only 47% (95% confidence interval [CI], 37%–58%).7 Sargent and Caughey8 discussed historical reasons for the fluctuation in vaginal birth after cesarean (VBAC) rates over the past 40 years, which ranged from 3% in 1981 to 28% in 1996 and a nadir of 9% in 2006. Although the US Centers for Disease Control and Prevention publishes regular birth data updates, they and others only provide VBAC rates without TOLAC rates9,10 or do not analyze trends over multiple years.11 In addition, no recent article provides TOLAC or VBAC rates by number of previous CDs, although the recommendations for the management differ based on number of previous CDs.12 Secondary to these data limitations, a recently published VBAC calculator used data from 20 years ago.13
TOLAC is 1 way to reduce the sequelae of multiple repeat CD, but appropriate decision-making and patient counseling require up-to-date and accurate data. This study aimed to report the national rates of TOLAC and VBAC by number of previous CDs and examine the effect of demographic and clinical characteristics on these rates.
Materials and Methods
Overview
This was a population-based cohort study using the natality data files of the US Vital Statistics Data. The study sample was restricted to in-hospital, nonanomalous singleton, cephalic deliveries between 37 and 42 weeks of gestation from 2010 to 2019 with a history of at least 1 previous CD. Only states using the 2003 birth certificate revision were included because only with this revision was information included on history of previous CD and number of previous CDs.14 The 2003 revision was used by 33 states and the District of Columbia in 2010, 36 states and the District of Columbia in 2011, 38 states and the District of Columbia in 2012, 41 states and the District of Columbia in 2013, 47 states and the District of Columbia in 2014, 48 states and the District of Columbia in 2015, and 50 states and the District of Columbia in 2016–2019. The percentage of live births captured by this revision ranged from 65% in 2010 to 100% in 2019. The sample size was determined by the number of available deliveries. This study did not include personally identifiable information and was exempt from institutional review board review. We followed the Strengthening the Reporting of Observational Studies in Epidemiology guidelines.15
Predictor variables
Deliveries were grouped by number of previous CDs (1, 2, or ≥3). Deliveries with ≥3 CDs were included as a “negative control,” which is expected to rarely attempt TOLAC. Previous VD was defined as records with parity greater than the number of previous CDs. Maternal education was defined as less than high school, high school or more, or unknown. A prepregnancy body mass index of ≥30 kg/m2 was defined as obese. Pregestational and gestational diabetes mellitus were combined into a single diabetes mellitus category, and pregestational and gestational hypertension and eclampsia were combined into a single hypertension category (the birth certificate includes preeclampsia with gestational hypertension). Inadequate prenatal care was defined as fewer than 6 visits.16 Gestational age was based on the variable “obstetrical estimate of gestation.” Induction or augmentation of labor was used only in VBAC models.
Statistical analysis
The TOLAC (VDs and deliveries with CD after TOLAC among deliveries with previous CD) and VBAC rates (VD among TOLAC) rates were computed for each year. The TOLAC and VBAC rates were further subgrouped by number of previous CDs and history of previous VD. Chi-square tests were used for bivariate associations. Multivariable logistic regression models were used to explore the association between demographic and clinical characteristics (year of delivery, number of previous CDs, history of previous VD, age, race and ethnicity, maternal education, obesity, diabetes mellitus, hypertension, inadequate prenatal care, Medicaid payer, and gestational age) and TOLAC and VBAC. Models included demographic and clinical characteristics selected a priori through literature review and expert clinical consensus as potential predictors. Cases with missing data were excluded from the models. SAS software (version 9.4; SAS Institute, Cary, NC) was used for all analyses.
Results
From 2010 to 2019, there were 39,236,775 live births in the United States recorded into the national database, of which 36,714,578 (93.6%) used the 2003 revised birth certificate. The study population included 4,135,247 deliveries (11.3%). Table 1 presents the maternal characteristics among the study population by number of previous CDs. The number of deliveries among people with 1 previous CD increased from 224,205 in 2010 to 311,410 in 2019 (39% increase), and the number of deliveries among people with ≥3 previous CDs increased from 18,781 in 2010 to 35,489 in 2019 (89% increase). Increasing age at delivery, higher parity, and previous VD were associated with higher numbers of previous CDs (P<.001). Race and ethnicity were associated with number of previous CDs, with higher proportions of non-Hispanic Black and Hispanic among those with ≥3 previous CDs (19.2% and 32.2%, respectively) than among those with 1 CD (14.0% and 23.9%, respectively) or 2 previous CDs (15.9% and 29.9%, respectively). Obesity, diabetes mellitus, hypertension, Medicaid payer, and inadequate prenatal care were associated with higher numbers of previous CDs (P<.001). Gestational age was inversely related to number of previous CDs (P<.001). Induction or augmentation occurred in 10.9%, 3.6%, and 2.4% of those with 1, 2, or ≥3 previous CDs (P<.001).
Table 1.
Demographic and clinical characteristics by number of previous CDs
| Characteristic | 1 previous CD (n=2,922,602) | 2 previous CDs (n=951,875) | ≥3 previous CDs (n=293,358) | P value |
|---|---|---|---|---|
| Birth year | <.001 | |||
| 2010 | 224,205 (7.7) | 69,216 (7.3) | 18,781 (6.4) | |
| 2011 | 254,282 (8.7) | 78,993 (8.3) | 21,839 (7.4) | |
| 2012 | 265,724 (9.1) | 84,023 (8.8) | 23,909 (8.2) | |
| 2013 | 276,866 (9.5) | 88,294 (9.3) | 25,797 (8.8) | |
| 2014 | 302,984 (10.4) | 97,900 (10.3) | 29,754 (10.1) | |
| 2015 | 317,392 (10.9) | 104,270 (11.0) | 32,097 (10.9) | |
| 2016 | 327,496 (11.2) | 108,196 (11.4) | 34,557 (11.8) | |
| 2017 | 322,887 (11.0) | 107,989 (11.3) | 35,163 (12.0) | |
| 2018 | 319,356 (10.9) | 108,292 (11.4) | 35,972 (12.3) | |
| 2019 | 311,410 (10.7) | 104,702 (11.0) | 35,489 (12.1) | |
| Age (y) | <.001 | |||
| <20 | 41,154 (1.4) | 3551 (0.4) | 288 (0.1) | |
| 20–34 | 2,208,248 (75.6) | 699,070 (73.4) | 204,185 (69.6) | |
| ≥35 | 673,200 (23.0) | 249,254 (26.2) | 88,885 (30.3) | |
| Race and ethnicity | <.001 | |||
| Non-Hispanic White | 1,518,583 (52.0) | 450,912 (47.4) | 124,999 (42.6) | |
| Non-Hispanic Black | 409,004 (14.0) | 151,312 (15.9) | 56,244 (19.2) | |
| Non-Hispanic Asian or Pacific Islander | 221,682 (7.6) | 38,293 (4.0) | 6153 (2.1) | |
| Hispanic | 699,283 (23.9) | 284,873 (29.9) | 94,592 (32.2) | |
| Other or unknown | 74,050 (2.5) | 26,485 (2.8) | 11,370 (3.9) | |
| Parity | <.001 | |||
| 1 | 1,610,187 (55.1) | 832 (0.1) | 68 (0.0) | |
| 2 | 682,631 (23.4) | 528,685 (55.5) | 371 (0.1) | |
| ≥3 | 608,151 (20.8) | 415,618 (43.7) | 29,0621 (99.1) | |
| Previous vaginal delivery | 1,290,782 (44.2) | 415,618 (43.7) | 138,636 (47.3) | <.001 |
| Gestational age at delivery (wk) | <.001 | |||
| 37–38 | 912,923 (31.2) | 325,920 (34.2) | 113,036 (38.5) | |
| 39–40 | 1,773,504 (60.7) | 564,555 (59.3) | 162,225 (55.3) | |
| 41–42 | 236,175 (8.1) | 61,400 (6.5) | 18,097 (6.2) | |
| Obesity | 948,138 (32.4) | 358,191 (37.6) | 123,398 (42.1) | <.001 |
| Diabetes mellitus | 245,273 (8.4) | 88,560 (9.3) | 29,214 (10.0) | <.001 |
| Hypertension | 189,450 (6.5) | 62,955 (6.6) | 20,800 (7.1) | <.001 |
| Medicaid | 1,181,616 (40.4) | 483,742 (50.8) | 179,837 (61.3) | <.001 |
| Inadequate prenatal care | 164,628 (5.6) | 67,919 (7.1) | 31,072 (10.6) | <.001 |
| Induction or augmentation | 320,012 (10.9) | 34,598 (3.6) | 7083 (2.4) | <.001 |
Data are presented as number (percentage), unless otherwise indicated. P values were calculated using chi-square tests for independence between the number of previous CDs and the clinical and demographic characteristics.
CD, cesarean delivery.
Pineles. Trial of labor after cesarean rates and success. Am J Obstet Gynecol Glob Rep 2023.
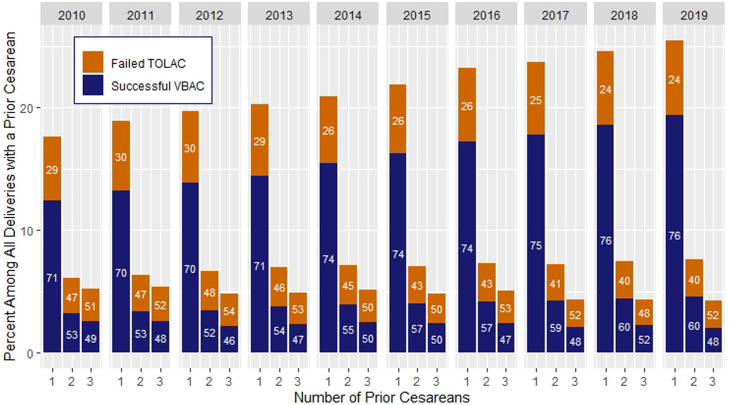
The TOLAC rates among all deliveries with a previous CD increased from 14.4% in 2010 to 19.6% in 2019 (36% increase; P<.001) (Figure). This trend was seen in all categories of number of previous CDs. Moreover, the VBAC rates increased from 68.5% in 2010 to 74.3% in 2019 (8% increase; P<.001) (Figure).
Figure.
Rates of TOLAC and VBAC by number of previous CDs
CD, cesarean delivery; TOLAC, trial of labor after cesarean; VBAC, vaginal birth after cesarean.
Pineles. Trial of labor after cesarean rates and success. Am J Obstet Gynecol Glob Rep 2023.
TOLAC occurred in 21.9%, 7.1%, and 4.8% of deliveries with 1, 2, and ≥3 previous CDs, respectively. Among TOLAC, VBAC occurred in 73.5%, 56.6%, and 48.6% of deliveries with 1, 2, and ≥3 previous CDs, respectively. The TOLAC and VBAC rates were the highest for deliveries with a history of both 1 previous CD and a VD (28.9% and 79.7%, respectively) and the lowest for those with a history or ≥3 previous CDs and no history of VD (4.5% and 46.9%, respectively).
In the multivariable model, the odds of TOLAC and VBAC were elevated with more recent year of delivery, previous VD, and inadequate prenatal care (Table 2). Of note, 2 and ≥3 previous CDs, obesity, hypertension, diabetes mellitus, government insurance, and maternal age of ≥35 years were associated with lower odds of TOLAC and VBAC. Maternal age of <20 years was associated with lower odds of TOLAC but higher odds of VBAC. Non-White race and ethnicity were associated with higher odds of TOLAC but were associated with lower odds of VBAC. Induction or augmentation of labor was associated with higher odds of successful VBAC.
Table 2.
Multivariable model for TOLAC and successful VBAC among deliveries with a history of previous CD
| Variable | TOLAC (n=3,970,990) | Successful VBAC (n=683,002) |
|---|---|---|
| aOR (95% CI) | aOR (95% CI) | |
| Year of deliverya | 1.05 (1.05–1.05) | 1.04 (1.04–1.04) |
| Number of previous CDs | ||
| 1 | Reference | Reference |
| 2 | 0.27 (0.27–0.27) | 0.52 (0.51–0.53) |
| 3 | 0.17 (0.17–0.17) | 0.41 (0.40–0.43) |
| Previous vaginal delivery | 2.02 (2.01–2.03) | 2.15 (2.13–2.18) |
| Maternal age (y) | ||
| <20 | 0.84 (0.82–0.86) | 1.14 (1.08–1.20) |
| 20–34 | Reference | Reference |
| ≥35 | 0.90 (0.89–0.90) | 0.86 (0.85–0.87) |
| Maternal race and ethnicity | ||
| Non-Hispanic White | Reference | Reference |
| Non-Hispanic Black | 1.28 (1.26–1.29) | 0.65 (0.64–0.66) |
| Hispanic | 1.05 (1.04–1.06) | 0.85 (0.84–0.87) |
| Non-Hispanic Asian | 1.03 (1.02–1.05) | 0.74 (0.72–0.75) |
| Other or unknown | 1.23 (1.21–1.25) | 0.99 (0.96–1.03) |
| Inadequate prenatal care | 1.36 (1.35–1.38) | 1.12 (1.10–1.15) |
| Gestational age at delivery (wk) | ||
| 37–38 | 1.04 (1.03–1.05) | 0.92 (0.91–0.93) |
| 39–40 | Reference | Reference |
| 41–42 | 2.05 (2.04–2.07) | 0.90 (0.89–0.92) |
| Obesity | 0.67 (0.66–0.67) | 0.68 (0.67–0.69) |
| Diabetes mellitus | 0.86 (0.85–0.86) | 0.86 (0.84–0.88) |
| Hypertension | 0.88 (0.87–0.89) | 0.71 (0.69–0.72) |
| Medicaid | 0.97 (0.96–0.98) | 0.94 (0.93–0.95) |
| Induction or augmentation | Not included | 1.31 (1.30–1.33) |
aOR, adjusted odds ratio; CD, cesarean delivery; CI, confidence interval; OR, odds ratio; TOLAC, trial of labor after cesarean; VBAC, vaginal birth after cesarean.
The ORs are per each 1-year increase.
Pineles. Trial of labor after cesarean rates and success. Am J Obstet Gynecol Glob Rep 2023.
Discussion
Principal findings
TOLAC and VBAC have both increased over the past decade; however, the TOLAC rate remains below 20% in 2019 and was only 29% for patients with 1 previous CD and a history of VD. The rate of successful VBAC was much higher, at 74% in 2019 after increasing since 2010.
Results
The most recent analysis of TOLAC trends, from 1990 to 2009, showed that the TOLAC rate peaked at 51.8% in 1995 and had a nadir of 15.9% in 2006.17 Since then, the rate increased by 1.6% per year to 2009. The increase in rates from 2010 to 2019 shown in the current article continues this trend. An analysis of 2016 US birth data found the same predictors of TOLAC and VBAC as the current article.18 They found that lack of a high school degree and inadequate prenatal care were associated with a higher likelihood of both TOLAC and VBAC. Non-Hispanic Black women were more likely to undergo TOLAC but less likely to have a successful VBAC than non-Hispanic White women. To reduce the perpetuation of these disparities, a recent calculator to predict successful VBAC eliminated race and ethnicity from the predictive model.13
Clinical implications
These data have implications for reducing the national rate of CD and reducing maternal morbidity and mortality. This analysis shows an 80% likelihood of successful VBAC among TOLAC with 1 previous CD and a previous VD, but only a 29% rate of attempted TOLAC. Thus, the decision to undergo TOLAC is the limiting step for even the best candidates. Even among patients with 2 previous CDs, more than one-half of those who undergo TOLAC have a successful VBAC. Despite guidelines, recommendations, and advocacy to “prevent the primary cesarean,” CD rates have been stable in the United States over the past 10 years.19,20 In 2020, 42% of all CDs were repeat CD, and thus, preventing the second and third CDs are also crucial in reducing CD rates.21 The current article shows that those with 2 previous CDs have a <10% chance of undergoing a TOLAC, and those with ≥3 previous CDs have a <5% chance of undergoing a TOLAC. This is consistent with existing guidelines that recommend offering most patients with 1 previous CD the option to undergo TOLAC based on strong evidence, considering patients with 2 previous CDs as candidates for TOLAC based on weaker evidence, and offering no recommendation for patients with ≥3 previous CDs based on limited data on risks of uterine rupture and overall safety.12 In most cases, TOLAC has been shown to be more cost-effective than elective repeat CD.22 This is especially true when considering the risks to future pregnancies. The risks of multiple repeat CD are well documented and include placenta accreta spectrum disorders, blood transfusion, adjacent organ injury, and hysterectomy.4,23 The cost-effectiveness of a TOLAC increases with the number of subsequent VDs.24
Research implications
This study is a descriptive analysis, and research in several directions would contribute to the field: (1) analyzing the reasons behind changes in the TOLAC and VBAC rates, (2) correlation between maternal morbidity rates and TOLAC and VBAC rates, (3) effective implementation of policies that affect TOLAC and VBAC rates, and (4) a predictive model for successful VBAC using recent US birth data, which has been performed in the subgroup undergoing induction of labor.25
Strengths and limitations
The limitations of this study include the lack of data on the planned mode of delivery, with information only on whether or not TOLAC occurred. In addition, the data do not include information on previous classical CD or other risk factors that make TOLAC less safe or on local policies regarding TOLAC. We did not analyze morbidity because it is poorly captured in US birth data, with the sensitivity of severe maternal morbidity indicators ranging from 0.11 to 0.52 (0.26 for ruptured uterus) and the positive predictive value of these indicators ranging from 0.03 to 0.77 (0.18 for ruptured uterus).26 Only term deliveries were included because of the heterogeneity of clinical scenarios in preterm delivery that may reduce the propensity toward TOLAC, such as preeclampsia and placental abruption. The strengths of this study include the use of recent national data with multiple years to analyze trends. The data were standardized, all collected with the 2003 revision of the US birth certificate, and missing data were rare. Although the state of the birth was not available, the increases in TOLAC and VBAC were noted both from 2010 to 2013 when up to one-third of jurisdictions did not use the 2003 revision and from 2014 to 2019 when nearly all jurisdictions used the 2003 revision. The primary birth certificate variables used (method of delivery, history of previous CD, and trial of labor attempted) had high or substantial agreement compared with medical records in a published validation study.27
Conclusions
The TOLAC rates were low but increasing. Among those who underwent TOLAC, successful VBAC rates were high and increasing. Our data provide a benchmark for counseling patients with a history of previous CD about the mode of delivery.
Footnotes
The authors report no conflict of interest.
This study did not received external funding.
This study was presented at the Society for Maternal-Fetal Medicine 42nd Annual Pregnancy Meeting that was held virtually on January 31, 2022, to February 5, 2022.
Patient consent is not required because no personal information or detail is included.
Cite this article as: Pineles BL, Buskmiller CM, Qureshey EJ, et al. Recent trends in term trial of labor after cesarean by number of prior cesarean deliveries. Am J Obstet Gynecol Glob Rep 2023;XX:x.ex–x.ex.
References
- 1.Molina G, Weiser TG, Lipsitz SR, et al. Relationship between cesarean delivery rate and maternal and neonatal mortality. JAMA. 2015;314:2263–2270. doi: 10.1001/jama.2015.15553. [DOI] [PubMed] [Google Scholar]
- 2.Balayla J, Lasry A, Badeghiesh A, Volodarsky-Perel A, Gil Y. Mode of delivery is an independent risk factor for maternal mortality: a case-control study. J Matern Fetal Neonatal Med. 2022;35:1962–1968. doi: 10.1080/14767058.2020.1774874. [DOI] [PubMed] [Google Scholar]
- 3.Clapp MA, James KE, Little SE, Robinson JN, Kaimal AJ. Association between hospital-level cesarean delivery rates and severe maternal morbidity and unexpected newborn complications. Am J Obstet Gynecol MFM. 2021;3 doi: 10.1016/j.ajogmf.2021.100474. [DOI] [PubMed] [Google Scholar]
- 4.Silver RM, Landon MB, Rouse DJ, et al. Maternal morbidity associated with multiple repeat cesarean deliveries. Obstet Gynecol. 2006;107:1226–1232. doi: 10.1097/01.AOG.0000219750.79480.84. [DOI] [PubMed] [Google Scholar]
- 5.Matsuzaki S, Mandelbaum RS, Sangara RN, et al. Trends, characteristics, and outcomes of placenta accreta spectrum: a national study in the United States. Am J Obstet Gynecol. 2021;225 doi: 10.1016/j.ajog.2021.04.233. 534.e1–38. [DOI] [PubMed] [Google Scholar]
- 6.Martin JA, Hamilton BE, Osterman MJK, Driscoll AK. Births: final data for 2019. Natl Vital Stat Rep. 2021;70:1–51. [PubMed] [Google Scholar]
- 7.Guise JM, Eden K, Emeis C, et al. Vaginal birth after Cesarean: new insights. Evid Rep Technol Assess (Full Rep) 2010:1–397. [PMC free article] [PubMed] [Google Scholar]
- 8.Sargent J, Caughey AB. Vaginal birth after cesarean trends: which way is the pendulum swinging? Obstet Gynecol Clin North Am. 2017;44:655–666. doi: 10.1016/j.ogc.2017.08.006. [DOI] [PubMed] [Google Scholar]
- 9.Osterman MJK. Recent trends in vaginal birth after cesarean delivery: United States, 2016-2018. NCHS Data Brief. 2020:1–8. [PubMed] [Google Scholar]
- 10.Triebwasser JE, Kamdar NS, Langen ES, et al. Hospital contribution to variation in rates of vaginal birth after cesarean. J Perinatol. 2019;39:904–910. doi: 10.1038/s41372-019-0373-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Greene M, Hsiang-Hui DK, Hartenbach E, Shrider E, Ehrenthal D. Attempted and successful VBAC across geographic areas in the United States [25H] Obstet Gynecol. 2019;133:91S. [Google Scholar]
- 12.ACOG Practice Bulletin No. 205: vaginal birth after cesarean delivery. Obstet Gynecol. 2019;133 doi: 10.1097/AOG.0000000000003078. e110–27. [DOI] [PubMed] [Google Scholar]
- 13.Grobman WA, Sandoval G, Rice MM, et al. Prediction of vaginal birth after cesarean delivery in term gestations: a calculator without race and ethnicity. Am J Obstet Gynecol. 2021;225:664. doi: 10.1016/j.ajog.2021.05.021. e1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Methodological issues and the 2003 revision of standard instruments . National Academies Press. United States of America; Washington, DC: 2009. United States of America: National Research Council Committee on National Statistics. Vital Statistics. Summary of a Workshop. [Google Scholar]
- 15.von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med. 2007;147:573–577. doi: 10.7326/0003-4819-147-8-200710160-00010. [DOI] [PubMed] [Google Scholar]
- 16.American Academy of Pediatrics, American College of Obstetricians and Gynecologists . 8th ed. The American College of Obstetricians and Gynecologists; Washington, DC: 2017. Guidelines for perinatal care. Elk Grove Village. IL: American Academy of Pediatrics. [Google Scholar]
- 17.Uddin SF, Simon AE. Rates and success rates of trial of labor after cesarean delivery in the United States, 1990-2009. Matern Child Health J. 2013;17:1309–1314. doi: 10.1007/s10995-012-1132-6. [DOI] [PubMed] [Google Scholar]
- 18.Attanasio LB, Paterno MT. Correlates of trial of labor and vaginal birth after cesarean in the United States. J Womens Health (Larchmt) 2019;28:1302–1312. doi: 10.1089/jwh.2018.7270. [DOI] [PubMed] [Google Scholar]
- 19.American College of Obstetricians and Gynecologists (College), Society for Maternal-Fetal Medicine. Caughey AB, Cahill AG, Guise JM, Rouse DJ. Safe prevention of the primary cesarean delivery. Am J Obstet Gynecol. 2014;210:179–193. doi: 10.1016/j.ajog.2014.01.026. [DOI] [PubMed] [Google Scholar]
- 20.Osterman M, Hamilton B, Martin JA, Driscoll AK, Valenzuela CP. Births: final data for 2020. Natl Vital Stat Rep. 2021;70:1–50. [PubMed] [Google Scholar]
- 21.Natality, 2016-2020 expanded. 2020. Available at: https://wonder.cdc.gov/natality.html. Accessed April 4, 2022.
- 22.Rogers AJ, Rogers NG, Kilgore ML, Subramaniam A, Harper LM. Economic evaluations comparing a trial of labor with an elective repeat cesarean delivery: a systematic review. Value Health. 2017;20:163–173. doi: 10.1016/j.jval.2016.08.738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Klahr R, Cheung K, Markovic ES, Naert M, Rebarber A, Fox NS. Maternal morbidity with repeated cesarean deliveries. Am J Perinatol. 2021 doi: 10.1055/s-0041-1736183. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 24.Wymer KM, Shih YC, Plunkett BA. The cost-effectiveness of a trial of labor accrues with multiple subsequent vaginal deliveries. Am J Obstet Gynecol. 2014;211:56. doi: 10.1016/j.ajog.2014.01.033. e1–12. [DOI] [PubMed] [Google Scholar]
- 25.Rossi RM, Requarth E, Warshak CR, Dufendach KR, Hall ES, DeFranco EA. Risk calculator to predict cesarean delivery among women undergoing induction of labor. Obstet Gynecol. 2020;135:559–568. doi: 10.1097/AOG.0000000000003696. [DOI] [PubMed] [Google Scholar]
- 26.Luke B, Brown MB, Liu CL, Diop H, Stern JE. Validation of Severe Maternal Morbidity on the US Certificate of Live Birth. Epidemiology. 2018;29 doi: 10.1097/EDE.0000000000000828. e31–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gregory ECW, Martin JA, Argov EL, Osterman MJK. Assessing the quality of medical and health data from the 2003 birth certificate revision: results from New York City. Natl Vital Stat Rep. 2019;68:1–20. [PubMed] [Google Scholar]