Abstract
Objective
To describe the impact of the COVID-19 pandemic on help-seeking behaviors among individuals with eating disorders and caregivers.
Methods
We analyzed service utilization data from the National Eating Disorder Information Centre (NEDIC). We compared the number of contacts and symptom frequency between the pandemic period and previous years.
Results
NEDIC was contacted 609 times during March 1–April 30, 2020 (72.1% individuals affected by disordered eating, 20.4% caregivers). The number of total contacts significantly increased from 2018 to 2019 and 2018 to 2020 (X2(3) = 50.34, p < .001). Among affected individuals (80.4% women), the number of contacts during the pandemic period was significantly higher (n = 439; X2(2) = 92.74, p < .001) compared to 2018 (n = 197) and 2019 (n = 312). There were higher rates of eating disorder symptoms, anxiety, and depression in 2020 compared to previous years. Thematic analysis of instant chats from the pandemic year revealed four emerging themes: 1) lack of access to treatment, 2) worsening of symptoms, 3) feeling out of control, and 4) need for support.
Conclusion
These findings point toward the impact of COVID-19 in individuals affected by disordered eating and hold implications for service delivery during times of crises.
Keywords: COVID-19, Eating disorder, Internet, Treatment, Psychotherapy
1. Introduction
Eating disorders (EDs) affect a significant portion of the global population, with lifetime prevalence rates ranging from 1% to 4% in epidemiological studies [1]. They are distinct disturbances in eating habits in the form of excessive or below optimal levels of food consumption, as well as distinct weight-control behaviors (e.g., frequent self-induced vomiting or laxative misuse) associated with an over-evaluation of body shape and/or weight [2]. EDs are chronic mental disorders associated with high relapse rates, high treatment costs, diminished quality of life [3] but also medical morbidity and mortality [4,5].
The COVID-19 pandemic has been assumed to have had an immediate impact on individuals suffering with eating disordered symptoms, both in terms of symptom aggravation as well as hampered access to treatments. The pandemic has disrupted typical modes of health care delivery such as face-to-face therapies with a professional caregiver. This situation has exacerbated the already pervasive problem of unmet treatment needs among individuals with eating disordered symptoms; it has repeatedly been shown that affected individuals either do not seek ED-specific treatment, or do not receive appropriate care when it is sought [6,7]. Additionally, the general anxiety-provoking atmosphere of the pandemic along with stay-at-home orders, at-home workouts, and threats of food shortages may exacerbate eating pathology [8]. Concerns about increases in the severity of ED symptomatology and caregiver burden have been raised [9,10]. ED-related cognitions and behaviors may even emerge in individuals who had thus far not been affected by symptoms [8].
The National Eating Disorder Information Centre (NEDIC) is a national non-profit organization that was founded in 1985. NEDIC operates Canada's only toll-free helpline and instant chat service pursuing the goal to provide information and resources to individuals, so they are empowered to make the decision best suited to their personal circumstances. NEDIC generally provides: a) in-the-moment support to those affected by food and weight concerns; b) information about eating disorders; c) resources, such as a guide for family members, checklists for discussing food and weight concerns with healthcare providers; and d) referral to a mental health or health professional that has experience treating EDs, as NEDIC has a service provider directory of 700 treatment and support options across the country. NEDIC supports over 3500 people each year on their helpline and instant chat service. Since 2004, NEDIC has educated more than 160,000 people through professional development and outreach initiatives [11].
Using anonymous data collected by NEDIC (helpline and instant chat), the primary objective of the present study was to assess and evaluate help-seeking behaviors in individuals suffering from eating disordered symptoms and their caregivers during the COVID-19 pandemic, and to compare help-seeking behaviors between 2020 and previous years. Furthermore, instant chat transcripts were hand-searched to identify emerging “themes” associated with the pandemic. We hypothesized that, in comparison to previous years, there would be an increase in both the number of individuals seeking help for eating disordered symptoms as well as their caregivers. We also anticipated that affected individuals would indicate higher symptom frequency and more difficulties accessing adequate support during the pandemic period compared to previous years. The present study directly answers Weissman et al.'s8 call to record the experiences of people experiencing EDs and their caregivers during the global COVID-19 crisis, as they may prove invaluable in formulating hypotheses for future studies to improve interventions and reduce the burden of suffering attributable to EDs during times of crises.
2. Methods
2.1. Service utilization
Using a retrospective design, we statistically analyzed anonymous NEDIC service utilization data comparing the “pandemic year” (March 1–April 30, 2020) with corresponding time periods in previous years (March 1–April 30, 2018 and 2019). Data were stratified according to a number of variables (gender, age, role, self-reported diagnosis, and reason for contacting NEDIC). Also, the rates of symptoms (over-eating/binge eating, over-exercising, dieting/restriction, weight preoccupation, perfectionism, purging, anxiety, and depression) among individuals who contacted NEDIC in the pandemic year and self-identified as being affected by eating disordered symptoms were assessed and compared across years. Symptoms were considered present (“yes”/“no”) based on the self-report of help-seekers. NEDIC helpline staff are trained to ask clients what behaviors/symptoms they are experiencing and systematically record the self-reported presence (or absence) of the above listed symptoms in standardized call statistics forms, which are completed for each contact. The questions in the call statistics form that pertain to symptoms are 1) “What behaviors are present (check all that apply)?” with the following options: dieting/restriction, overeating/binge eating, over-exercising, perfectionism, purging, weight pre-occupation; and 2) “Are co-morbid conditions or co-occurring concerns present (check all that apply)?” with the following options: anxiety, depression, other (please specify).
2.2. Emerging themes in chat transcripts during the pandemic
Furthermore, thematic analysis [12] was used to qualitatively analyze anonymous chat transcripts from the pandemic period containing COVID-19-related contents. Thematic analysis is useful in gaining an understanding of individual's unique experiences and offers an accessible and theoretically flexible approach to analyzing qualitative data [12]. Chat transcripts were read by two authors (CR, MP) who independently coded text into concepts; concepts were subsequently examined for their meanings, grouped into related themes, and named by both authors. Data were discussed between all authors to ensure they appropriately reflected the original data.
All individuals who contacted NEDIC through the helpline or instant chat function between March 1st and April 30th of 2018, 2019, or 2020 were included in the analysis. Data from each contact was analyzed as a separate case. The study was approved by the University Health Network Research Ethics Board. Statistical analyses were performed using SPSS (IBM SPSS Statistics for Windows, Armonk, NY: IBM Corp.). Descriptive statistics (means, standard deviations, percentages, etc.) were calculated to summarize demographic variables. Non-parametric chi-square tests were used to compare frequencies of help-seeking behaviors between years among the groups of interest. Chi-square tests were used to assess differences in symptom frequency between years; symptoms were defined as binary “yes”/“no” (i.e., present vs. absent) variables. Post-hoc tests were performed using pairwise comparisons between individual years.
3. Results
3.1. Service utilization data
NEDIC was contacted 609 times during the pandemic time period of March 1–April 30, 2020. Of these, 120 were calls, 418 were instant chats, and 71 were contacts via email or social media. The majority of contacts were for support (64.0%, n = 390) or referral (20.4%, n = 124), and 78.2% (n = 476) of help-seekers were women. The majority of help-seekers (72.1%, n = 439) were individuals affected by eating disordered symptoms, 20.4% (n = 124) were caregivers, 5.4% (n = 33) were professionals, and 2.1% (n = 13) were educators, students, or media requests. Chi-square tests showed that the number of contacts was significantly different between the years 2018, 2019, and 2020 (X2(3) = 50.34, p < .001). The number of total contacts received during the pandemic period (n = 609) was significantly higher than the volume seen in the corresponding time period in 2018 (n = 394; X2(1) = 46.09, p < .001) but was not significantly different than 2019 (n = 572; X2(1) = 1.16, p = .28).
3.2. Affected individuals vs. caregivers
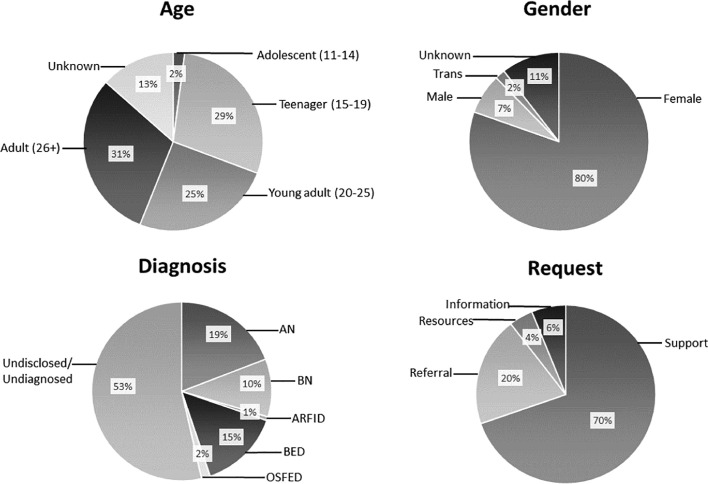
Among affected individuals (n = 439), the majority (80.4%, n = 353) were women, 7.3% (n = 32) were men, 1.8% (n = 8) were transgender, and 10.5% (n = 46) did not disclose. The majority of affected individuals were adults (age 26+; 30.5%, n = 134) or teenagers (ages 15–19; 28.7%, n = 126). Just under half of affected individuals (n = 204) self-disclosed an eating disorder diagnosis, of which AN (41.2%, n = 84) and BED (31.4%, n = 64) were the most prevalent; see Fig. 1 .
Fig. 1.
Self-reported age, gender identification, diagnosis, and request of affected individuals who contacted NEDIC in March/April 2020.
These findings are comparable with previous years, in which the majority of affected individuals were also women (86.8%, n = 173 in 2018; 77.6%, n = 242 in 2019), and the most prevalent self-reported diagnoses were AN (31.4%, n = 32 in 2018; 29.7%, n = 55 in 2019) and BED (41.2%, n = 42 in 2018; 43.8%, n = 81 in 2019). However, the majority of affected individuals in the prior two years were by far adults (48.2%, n = 95 in 2018; 47.8%, n = 149 in 2019) and young adults (age 20–25; 21.8%, n = 43 in 2018; 19.9%, n = 62 in 2019).
There were 124 caregivers, including parents, family members, and friends of affected individuals, who contacted NEDIC during the pandemic year. The majority of caregivers (72.6%, n = 90) were women, 21.0% (n = 26) were men, and 6.4% (n = 8) did not disclose their gender. Additionally, the majority of caregivers (67.7%, n = 84) were adults (age 26+).
Among affected individuals, the number of contacts differed significantly across the years (X2(2) = 92.74, p < .001), with the highest frequency of contacts in the pandemic period (n = 439), the lowest in 2018 (n = 197), and a moderate amount in 2019 (n = 312; 2020 > 2019, 2020 > 2018, 2019 > 2018). The number of contacts from caregivers was not significantly different across years (n = 132 in 2018, n = 156 in 2019, n = 124 in 2020; X2(2) = 4.04, p = .13). Of note, the number of teenagers who contacted NEDIC significantly differed between years (X2(2) = 87.56, p < .001), with the highest number (n = 126; 28.7%) in 2020, versus n = 25 in 2018 (12.7%) and n = 35 in 2019 (11.2%).
3.3. Symptom frequency among affected individuals
The proportion of affected individuals who reported dieting/restriction, over-exercising, perfectionism, purging, anxiety, and depression was significantly higher in the pandemic year than both 2018 and 2019. See Table 1 for rates and chi-square tests. The rates of reported overeating/binge eating and weight preoccupation did not vary between years.
Table 1.
Rates of self-reported symptom frequency among affected individuals presented by year.
|
Symptom Yes, n (%) No, n (%) |
2018 n = 197 |
2019 n = 312 |
2020 n = 439 |
Chi-square and Post-hoc tests |
|---|---|---|---|---|
| Overeating/Binge eating | 46 (23.4) 151 (76.6) |
88 (28.2) 224 (71.8) |
123 (28.0) 316 (72.0) |
X2(2) = 1.78 p < .410 |
| Dieting/Restriction | 47 (23.9) 150 (76.1) |
73 (23.4) 239 (76.6) |
154 (35.1) 285 (64.9) |
X2(2) = 15.19 p < .001 2020 > 18, 2020 > 19 |
| Over-exercising | 6 (3.0) 191 (97.0) |
8 (2.6) 304 (97.4) |
31 (7.1) 408 (92.9) |
X2(2) = 9.75 p = .008 2020 > 18, 2020 > 19 |
| Perfectionism | 1 (0.5) 196 (99.5) |
4 (1.3) 308 (98.7) |
25 (5.7) 414 (94.3) |
X2(2) = 17.32 p < .001 2020 > 18, 2020 > 19 |
| Purging | 15 (7.6) 182 (92.4) |
25 (8.0) 287 (92.0) |
61 (13.9) 378 (86.1) |
X2(2) = 9.04 p = .011 2020 > 18, 2020 > 19 |
| Weight pre-occupation | 43 (21.8) 154 (78.2) |
60 (19.2) 252 (80.8) |
111 (25.3) 328 (74.7) |
X2(2) = 3.90 p = .142 |
| Anxiety | 27 (13.7) 170 (86.3) |
26 (8.3) 286 (91.7) |
125 (28.5) 314 (71.5) |
X2(2) = 52.70 p < .001 2020 > 18, 2020 > 19 |
| Depression | 12 (6.1) 185 (93.9) |
11 (3.5) 301 (96.5) |
79 (18.0) 360 (82.0) |
X2(2) = 45.41 p < .001 2020 > 18, 2020 > 19 |
3.4. COVID-19-related emerging “themes”
Among all 418 chats in the pandemic period, 13.4% (n = 56) broached the issue of COVID-19. Among these 56 chats, four emerging themes were identified: 1) lack of access to treatment, 2) worsening of symptoms, 3) feeling out of control, and 4) need for support.
In detail, 46% of chatters (n = 26) experienced help-seeking delays and treatment program suspensions in the context of COVID-19 which left them with limited or no access to their regular supports. For example, one chatter wrote: “I'm currently getting outpatient treatment but […] my groups have been cancelled for the time being. I rely on the support and now I'm not sure what to do.” Another stated: “My doctor said I would be safer at home…safer from COVID maybe but not safer from myself”.
Furthermore, 73.2% of chatters (n = 41) identified that their symptoms have gotten worse in isolation/quarantine. These chatters disclosed experiencing a resurgence of ED symptoms and behaviors which were often used as a means of coping with changing routines, isolation, and working from home. For instance, one chatter stated: “I'm struggling during quarantine to not overeat out of stress and boredom. It's making my eating disorder spiral”. Similarly, another chatter described the effect of isolation on their ED as follows: “I have been in recovery from AN and BN for about two years now, and ever since this whole isolation thing started, my symptoms have come back, and worsened almost immediately.”
Furthermore, 14.3% of chatters (n = 8) identified feeling overwhelmed or “out of control” and turning to ED behaviors for a sense of normalcy. For instance, one chatter stated: “I guess I am feeling out of control of life's circumstances right now. And eating and weight is what I can control”. Finally, 32.1% of chatters (n = 18) requested referrals for support options.
4. Discussion
We assessed the demand for support in individuals dealing with eating disordered symptoms, as well as their caregivers, during the pandemic months of March/April 2020. We used a retrospective methodology and analyzed NEDIC service utilization data comparing the pandemic period with corresponding time periods in previous years, assessed self-reported symptom frequency across the years (ED-related symptoms and anxiety/depression as a proxy for general psychopathology), and qualitatively described emerging themes in anonymous chat transcripts that addressed the pandemic.
As main results, we found a significant increase in help-seeking rates during the pandemic months compared to corresponding periods in previous years among individuals affected by eating disordered symptoms. The proportion of affected individuals who reported dieting/restriction, over-exercising, perfectionism, purging, anxiety, and depression was also significantly higher in the pandemic year than both 2018 and 2019. The impact of the pandemic was addressed in numerous instant chats; qualitative analysis of these chat transcripts revealed four pandemic-related emerging themes: 1) lack of access to treatment, 2) worsening of symptoms, 3) feeling out of control, and 4) need for support. Among these themes, worsening of symptoms was the most prevalent.
While the majority of help-seekers were affected individuals (72.1%), one-fifth of contacts to NEDIC was initiated by a caregiver (20.4%). Both among affected individuals and caregivers, women-initiated contacts were seen in the vast majority of cases (80.4% and 72.6%, respectively); on the other hand, 21% of caregiver contacts were initiated by men (compared to 7.3% of men among affected individuals). Among both groups, adult help-seekers (26+ years of age) were the most prevalent (30.5% in the affected group vs. 66.9% in the caregiver group). Interestingly, a significant percentage of affected teenagers (28.70%; age 15–19) also contacted NEDIC in March/April 2020 (compared to 12.69% in 2018 and 11.22% in 2019). A possible explanation may be that teenagers were not attending school in person during the pandemic period, and thus did not have regular access to their usual support network and structure (e.g., guidance counsellors, teachers). Problematic home life with no respite and lack of routine may also be factors. This finding could be reflective of increased needs for support in this age group during the pandemic.
Moreover, despite the higher general prevalence of BED compared to other types of EDs, BED was only the second most prevalent (14.6%) self-reported diagnosis among affected individuals, following AN (19.8%). In line with this finding, dieting/restriction was reported significantly more often in 2020 compared to the two years prior. General psychopathology frequency (anxiety, depression) was also significantly higher in 2020 compared to both 2018 and 2019.
Our results are in line with pre-existing evidence showing that the COVID-19 pandemic has raised individual's perceived stress, anxiety, and depression levels [10]. Individuals with pre-existing mental disorders may be at especially high risk of experiencing deterioration of their mental well-being during the time of the pandemic [13]. In a pilot study, Fernández-Aranda et al. surveyed 32 patients with EDs to measure the impact of confinement during the first two weeks of the pandemic. They found most patients presented worries about increased uncertainty in their lives, 12 patients (out of 32) reported increased ED symptomatology, and 18 reported increased anxiety symptoms [14].
The increases we saw in our sample are in line with, or slightly higher than, the currently available reports of increases in prevalence of mental health issues more broadly during COVID-19. For instance, we found anxiety symptoms increased from an 8.3% low in 2019 to 28.5% in 2020, and depression symptoms from a 3.5% low in 2019 to 18.0% in 2020. Whereas, in a longitudinal study examining the impact of the COVID-19 pandemic on population mental health among adults in the United Kingdom, Pierce et al. [15] found that the population prevalence of clinically significant levels of mental distress rose about 10%, from 18.9% in 2018–19 to 27.3% in April 2020. Similarly, in a systematic review of the impact of the COVID-19 pandemic on mental health in the general population, Xiong et al. [16] found that a high prevalence of adverse psychiatric symptoms was reported in most studies conducted across eight countries. In a separate analysis of five of the nineteen included studies -deemed to be more representative of the general population based on quality appraisal- the rates of anxiety symptoms ranged from 6.33% to 18.7%, depressive symptoms from 14.6% to 32.8%, stress symptoms were 27.2%, and PTSD symptoms were 7%. However, there was notably high heterogeneity across studies in the assessment tools used and primary outcomes measured. It is unclear whether these rates translate to a Canadian context as the majority of studies were conducted in China and Europe.
Additionally, the COVID-19 pandemic has caused a shift in prioritization of healthcare delivery. Worldwide, healthcare delivery services deemed “non-essential” were either shut down completely or significantly reduced, and healthcare professionals were redeployed to COVID-19-related areas where they were urgently needed. Eating disorder programs, especially outpatient programs, were among the services deemed “non-essential”. As a result, a significant number of affected individuals were suddenly left with no access to treatment. These patients may be at heightened physical risk due to health complications associated with their disorder, and experience psychological stress due to confinement and lack of access to their usual supports [8]. Here, we provide empirical evidence that the needs of a significant portion of individuals suffering from eating disordered symptoms remained unmet during the pandemic. These results answer Weissman et al.'s [8] call to record the experiences of people experiencing EDs and their caregivers during the global COVID-19 crisis, as they may provide information needed to improve future interventions. Greater attention to and understanding of the impact of the pandemic on individuals affected by eating disordered symptoms and their caregivers is warranted. Being prepared for similar crises will guarantee that affected individuals get the support they require. In an effort to mitigate disruptions in ED treatment due to the pandemic, virtualized forms of care that can replace face-to-face interventions have been initiated globally. While e-health interventions may bear great potential in times of crises, such as that of the COVID-19 pandemic, both the acceptability and effectiveness of such interventions in the field of EDs has been shown to be limited and in need of significant improvement [17]. Moreover, while several recent papers [18,19] have been published about the online delivery of evidence-based treatments for eating disorders, these treatments are not available or accessible to all patients. While many private-practice clinicians rapidly shifted toward online-delivery methods, the provision of government-funded treatment options have taken longer to implement, leaving many patients without the financial means to pay for treatment, without access to accessible care [20].
Several strengths and limitations of this study need to be considered. Strengths of this study include: the collection of anonymous data, which may be regarded as facilitating unbiased responses; the assessment of a significant number of contacts, including all ages (from adolescents to adults) as well as both affected individuals and caregivers; and the comparison between corresponding time periods in three consecutive years. Given the anonymous nature of NEDIC's services, we were unable to determine if the same individual(s) contacted NEDIC multiple times. Thus, each contact was considered to be a separate case, which may be considered a limitation. Symptoms were assessed based on a standardized call statistics form which may have not accurately reflected the entire spectrum of symptoms experienced by clients. Furthermore, ED diagnoses were self-reported and -due to the voluntary and anonymous disclosure of information- a significant percentage of affected individuals did not disclose a diagnosis and/or had not been formally diagnosed with an ED. Thus, while only 2% of affected individuals self-disclosed to suffer from OSFED, 53% reported to be undiagnosed or did not want to disclose their diagnosis. Presumably, the distribution of diagnoses might have been different if all affected individuals had received a formal ED diagnosis. Finally, there is a possibility that the increases in total contacts to NEDIC between 2018 and 2020 were caused by a natural trend toward increased symptoms rather than the pandemic, specifically. The provision of NEDIC services has changed significantly after December 2017 (structural changes). Thus, data before this timeframe cannot be effectively compared to data gathered afterwards. On the other hand, the differences in symptom frequencies are driven by differences between 2020 > 2018 and 2020 > 2019; the changes between 2018 and 2019 were not significant. Thus, we have reason to believe that the pandemic year 2020 differed than the two years before with regard to symptom burden in individuals with eating disorders.
5. Conclusion
The COVID-19 pandemic has significantly disrupted health care delivery. We provide evidence for the impact of the pandemic in the vulnerable population of individuals affected by disordered eating. Adult women who self-reported suffering from AN accounted for the largest group contacting NEDIC during the pandemic and reported worsening of dieting/restriction and increases in anxiety and depression. Our findings add to the scarce existing knowledge regarding help-seeking behaviors in individuals with eating disordered symptoms as well as their caregivers during COVID-19. These findings may serve as evidence for the demand for support during this and future pandemic(s) and may help make necessary future adjustments to the support provided during times of crises.
Funding
G.P. was supported by the Loretta Anne Rogers Chair in Eating Disorders Fund at University Health Network and the University of Toronto.
Data availability
Data are available upon reasonable request.
Author statement
All authors have sufficiently contributed to and approved the final version of the manuscript that has not been previously published. C.R. and M.P. were involved in statistical analyses and analyses of the qualitative data and wrote the first draft of the paper. S.P. and G.P. critically evaluated and edited the manuscript, and provided input for subsequent paper versions. G.P. conceptualized the paper and supervised the project.
Declaration of Competing Interest
None.
References
- 1.Smink F.R.E., van Hoeken D., Hoek H.W. Epidemiology of eating disorders: incidence, prevalence and mortality rates. Curr Psychiatry Rep. 2012;14(4):406–414. doi: 10.1007/s11920-012-0282-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.American Psychiatric Association . 5th ed. 2013. Diagnostic and Statistical Manual of Mental Disorders. Washington, DC. [Google Scholar]
- 3.Hay P., Mitchison D., Collado A.E.L., González-Chica D.A., Stocks N., Touyz S. Burden and health-related quality of life of eating disorders, including avoidant/restrictive food intake disorder (ARFID), in the Australian population. J Eat Disord. 2017;5(1):21. doi: 10.1186/s40337-017-0149-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rosling A.M., Sparén P., Norring C., Von Knorring A.L. Mortality of eating disorders: a follow-up study of treatment in a specialist unit 1974-2000. Int J Eat Disord. 2011;44(4):304–310. doi: 10.1002/eat.20827. [DOI] [PubMed] [Google Scholar]
- 5.Gibson D., Workman C., Mehler P.S. Medical complications of anorexia nervosa and bulimia nervosa. Psychiatr Clin North Am. 2019;42(2):263–274. doi: 10.1016/j.psc.2019.01.009. [DOI] [PubMed] [Google Scholar]
- 6.Hart L.M., Granillo M.T., Jorm A.F., Paxton S.J. Unmet need for treatment in the eating disorders: a systematic review of eating disorder specific treatment seeking among community cases. Clin Psychol Rev. 2011 doi: 10.1016/j.cpr.2011.03.004. [DOI] [PubMed] [Google Scholar]
- 7.Striegel Weissman R., Rosselli F. Reducing the burden of suffering from eating disorders: unmet treatment needs, cost of illness, and the quest for cost-effectiveness. Behav Res Ther. 2017;88:49–64. doi: 10.1016/j.brat.2016.09.006. [DOI] [PubMed] [Google Scholar]
- 8.Weissman R.S., Bauer S., Thomas J.J. Access to evidence-based care for eating disorders during the COVID-19 crisis. Int J Eat Disord. 2020;53(5):369–376. doi: 10.1002/eat.23279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Peckmezian T., Paxton S.J. A systematic review of outcomes following residential treatment for eating disorders. Eur Eat Disord Rev. 2020;28(3):246–259. doi: 10.1002/erv.2733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Torales J., O’Higgins M., Castaldelli-Maia J.M., Ventriglio A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int J Soc Psychiatry. 2020 doi: 10.1177/0020764020915212. [DOI] [PubMed] [Google Scholar]
- 11.NEDIC About NEDIC. nedic.ca. https://nedic.ca/about/ Published 2019. Accessed June 1, 2020.
- 12.Braun V., Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. doi: 10.1191/1478088706qp063oa. [DOI] [Google Scholar]
- 13.Wang C., Pan R., Wan X., et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. 2020;17(5):1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fernández-Aranda F., Casas M., Claes L., et al. COVID-19 and implications for eating disorders. Eur Eat Disord Rev. 2020;28(3):239–245. doi: 10.1002/erv.2738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pierce M., Hope H., Ford T., et al. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatry. 2020;7(10):883–892. doi: 10.1016/S2215-0366(20)30308-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Xiong J., Lipsitz O., Nasri F., et al. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J Affect Disord. 2020;277:55–64. doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ahmadiankalati M., Steins-Loeber S., Paslakis G. Review of randomized controlled trials using e-health interventions for patients with eating disorders. Front Psychiatry. 2020;11:568. doi: 10.3389/fpsyt.2020.00568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Waller G., Pugh M., Mulkens S., et al. Cognitive-behavioral therapy in the time of coronavirus: clinician tips for working with eating disorders via telehealth when face-to-face meetings are not possible. Int J Eat Disord. 2020;53(7):1132–1141. doi: 10.1002/eat.23289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Matheson B.E., Bohon C., Lock J. Family-based treatment via videoconference: clinical recommendations for treatment providers during COVID-19 and beyond. Int J Eat Disord. 2020;53(7):1142–1154. doi: 10.1002/eat.23326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gaind K. Mental health and healthcare in Canada during the COVID-19 epidemic: a social perspective. World Soc Psychiatry. 2020;2(2):106–108. doi: 10.4103/WSP.WSP_45_20. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available upon reasonable request.