Abstract
B cells occupy a vital role in the functioning of the immune system, working in tandem with T cells to either suppress or promote tumor growth within the tumor microenvironment(TME). In addition to direct cell-to-cell communication, B cells and other cells release exosomes, small membrane vesicles ranging in size from 30-150 nm, that facilitate intercellular signaling. Exosome research is an important development in cancer research, as they have been shown to carry various molecules such as major histocompatibility complex(MHC) molecules and integrins, which regulate the TME. Given the close association between TME and cancer development, targeting substances within the TME has emerged as a promising strategy for cancer therapy. This review aims to present a comprehensive overview of the contributions made by B cells and exosomes to the tumor microenvironment (TME). Additionally, we delve into the potential role of B cell-derived exosomes in the progression of cancer.
Keywords: B cell, B cell-derived exosome, therapy, TME, anti-tumor
1. Introduction
Cancer remains a significant global cause of mortality (1). Historically, cancer research solely emphasized studying cancer cells. However, with the introduction of the “seed and soil” concept (2), researchers have redirected their focus towards investigating the development of cancer cells within TME. The TME fosters cancer cell growth and progression through its complex composition of ECM, neuroendocrine cells, immune cells, stromal cells, fibroblasts, and lymphatic networks (3, 4). Immune cells play a significant role in the survival of tumors, as cancer cell metabolites and secretions from specific TME cells can influence the activation, proliferation, differentiation, and function of immune cells (5).
Reports suggest that extracellular vesicles (EVs), particularly exosomes, hold significant potential as a cancer treatment (6). Standard chemotherapy methods may cause harm to normal cells, resulting in detrimental side effects (7, 8). In contrast, Targeted therapy has become a more appealing approach to combatting tumors as it offers greater specificity and can spare adjacent healthy tissues (9). The idea of utilizing exosomes for targeted therapy is intriguing, given that almost all cells produce exosomes (10). Bioengineered exosomes have garnered considerable attention due to their exceptional stability, extensive tissue penetrability, potent targeting capability, and precise drug modulatory properties (11). Although there are no standardized protocols for exosome isolation and purification (12), their potential role in cancer therapy warrants further investigation into their biological functions.
B cells are present in both secondary lymphoid organs (SLOs) and tertiary lymphoid structures(TLSs). TLSs, which represent lymphoid neogenesis sites that occur in most solid tumors (13), primarily consist of B cell follicles and T cell zones, along with mature dendritic cells (DCs) (14, 15). Within these lymphoid structures, there is a rich signaling crosstalk between B cell-derived exosomes and other cells.
2. B cells and the tumor microenvironment
In the past decade, immune cells have gained significant attention in TME research due to their capacity to regulate tumor growth (16). Despite incomplete comprehension of the role of B cells in cancer research, their heterogeneity has been demonstrated as indispensable in the TME (17). B cells are also involved in the formation of TLSs, which has been instrumental in advancing cancer research (18).
2.1. Immunomodulatory functions of B cells
B cells are a component of the adaptive immune system that can differentiate into various subsets when subjected to diverse stimuli and stress conditions (19). The multifaceted nature of B cell subsets, which is primarily due to the absence of a precise definition of their transcription factors, makes comprehending their functions a difficult and complicated process (17).
B cells assume a pivotal role in antibody production and antigen presentation to facilitate effective immune responses among other immune cells (20, 21). After antigen recognition, B cell activation occurs through activation of B cell receptors (BCRs) and Toll-like receptors present on the surface of them. Subsequently, activated B cells differentiate into plasma cells through two distinct pathways. In the first pathway, plasma cells differentiate outside the lymphoid follicle, exhibit lower affinity for antigens, and have shorter lifespans. In the second pathway, B cells migrate into the follicle and establish a germinal center (GC) that differentiates into long-lived plasma cells and memory B cells (22–24). Plasma cells produce IgM antibodies that contribute to humoral immune responses. Moreover, B-cell-associated immunoglobulins, including IgG, IgE, and IgA, have been extensively reviewed in the literature with respect to their subclasses (21). IL-10 promotes plasma cell production through CD40 activation and is superior to IL-4 (25). Recent studies have found that tumour-associated neutrophils in TME rely on TNF-α to recruit B cells and regulate B cell differentiation into plasma cells via the BAFF pathway (26).
Memory B cells exhibit signaling molecules, such as MHC and co-stimulatory molecules, along with cytokines (IL-6, TNF, GM-CSF) on their surface, which stimulate T cells, thereby amplifying the immune response (24). Upon a second exposure to antigens, memory B cells produce high-quality antibodies (27).
B regulatory (Breg) cells are distinct in that their primary function is to suppress the immune system (28). Breg subsets containing IL-10 and IL-35 have the ability to suppress effector T cells (both CD4 and CD8), NK cells, and neutrophils (29). Additionally, Bregs regulate levels of extracellular metabolites such as ATP, ADP, AMP, and adenosine in TME, resulting in the suppression of T and B cell proliferation, forming a complex network (30, 31).
Tumor-infiltrating B cells (TIBs) participate in the development of TLSs, which stimulate an active anti-tumor response via antigen presentation (32, 33). Activated TIBs release enzymes or receptors to kill cancerous cells, leading to their lysis (34). B cells secrete angiogenic factors to stimulate the activation of STAT3 and facilitate angiogenesis (35). In prostate cancer, TIBs may produce lymphotoxin (LT), and high levels of LT can lead to CR-CAP and adversely affect treatment outcomes (36).
2.2. B cells in cancer therapy
Surface markers CD19, CD20, and CD37 are expressed at varying levels by B cells during development. Although studies indicate that targeting these molecules therapeutically holds promise for B-cell cancers (37), their potential efficacy against other cancer types remains largely unexplored. Mediation by CD19 increases antigen presentation by B cells, consequently improving the T cell response (38). Attracting B cells, CXCL13 functions as a chemokine (36, 39). Tumor-induced Bregs (tBregs) serve as a marker of tumor persistence (40). CD20 is expressed on both anti-tumor B cells and tBregs, and targeting CD20 B cells with CXCL13-coupled CpG-ODN can enrich and inactivate tBregs, thereby controlling tumor immune escape (41). This approach minimizes the potential side effects of B-cell depletion methods. In bladder cancer, CXCL13 expression can be used as a surrogate marker for tumor TLSs and correlates with the response to immune checkpoint inhibitors (ICIs) in patients (42). Additionally, in a subset of patients with soft tissue sarcoma, B-cell-enriched TLSs was associated with a better response to anti-PD-1 blockade therapy and increased survival rates (43).
However, the inhibitory mechanisms of tumors mediated by TLSs and B cells in ICI therapy remain poorly understood (44). It is noteworthy that within GCs, B cells are activated to produce antibodies, while Bregs and Tregs produce cytokines such as IL-10, IL-35, and TGF-β to suppress T cell function (18). Furthermore, chemotherapy (45) and vaccination (46) have also demonstrated associations with TLSs.
B cell-enriched TLSs have been found to exhibit tumor-suppressing properties (47). Infiltration of CD19/CD20 B cells has now emerged as a promising target for immunotherapy of hepatocellular carcinoma (48). Thus, combining immunotherapies such as cancer vaccines, cytokine therapies, and immune checkpoint inhibitors (ICIs) with strategies targeting B cells and TLSs may represent promising new anti-tumor approaches.
3. Exosomes and tumor microenvironment
Exosomes facilitate substance transfer between cells, activating signaling pathways (49). The secretion of exosomes by B cells is among the most important ways in which they influence the TME. Additionally, exosomes secreted by other cells and cancer cells also play pivotal roles (50, 51). Therefore, it can be speculated that exosomes hold great potential for advancing the exploration of new therapeutic pathways in cancer ( Figure 1A ).
Figure 1.
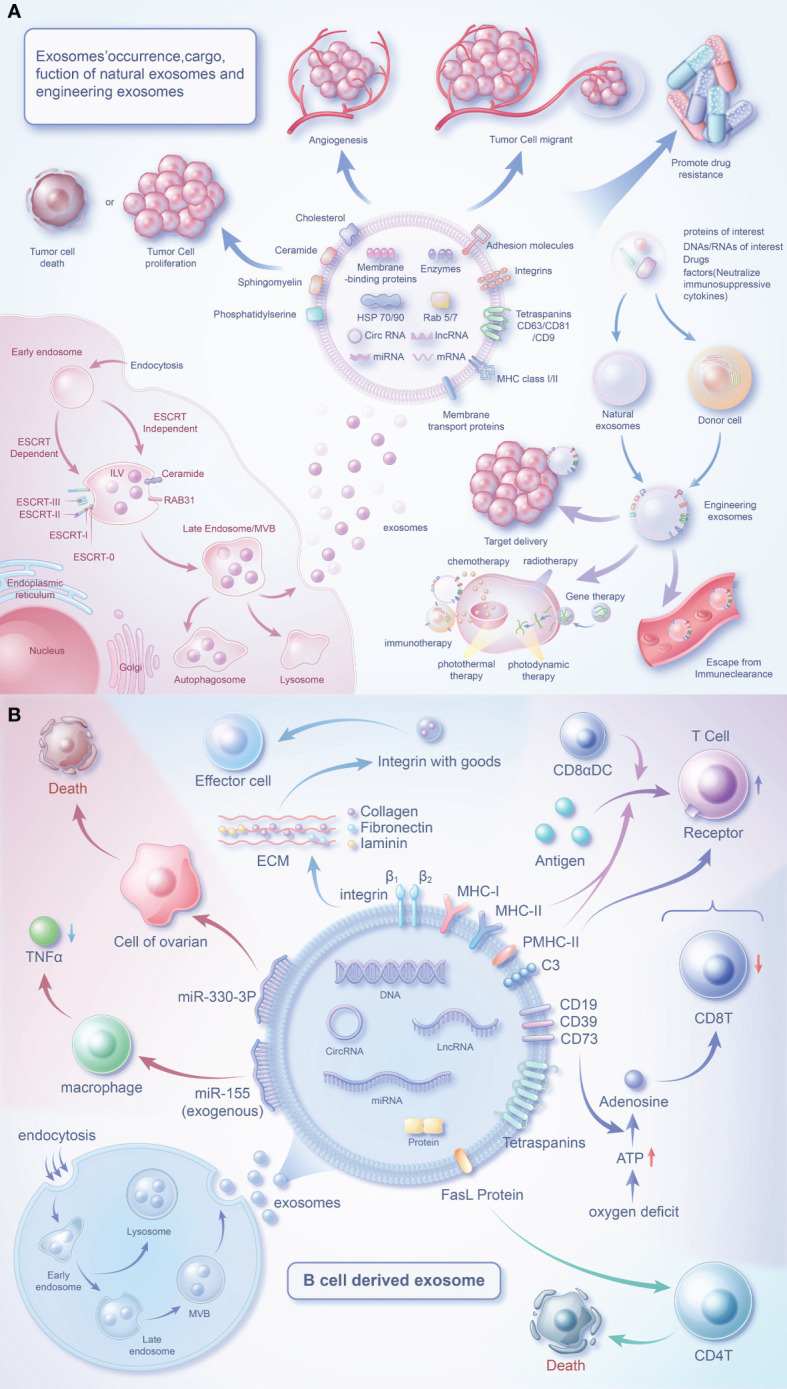
Biology of exosomes and the role of their cargo in the tumor microenvironment. (A) Exosomes are produced in dependence on the ESCRT mechanism or a RAB31-mediated pathway independent of the ESCRT mechanism. Exosomes carry a variety of proteins and effector molecules that can determine the direction of tumour development and tumour metastasis, promote tumour angiogenesis and participate in tumour drug resistance.Engineered exosomes carry cargoes of interest that also have multiple roles closely related to tumours. (B) B cells release exosomes through endocytosis of the plasma membrane, the formation of early endosomes and late endosomes, and fusion of polyvesicular bodies with the plasma membrane. In addition to MHC protein and quadruple transmembrane protein, the surface of B cell-derived exosomes contains special FasL proteins, integrins, C3, CD19, CD39, CD73, etc., which can regulate immune cells (T cells) or affect the survival of tumor cells through special factors.
3.1. The biological characteristics and functions of exosomes
Exosomes, a type of extracellular vesicles, have been extensively studied (52–55). Exosomes are generated through the intracellular process of inward budding of multivesicular bodies, followed by their subsequent release into the extracellular space through fusion events with the plasma membrane (56). The secretion of exosomes is regulated by the RAB family (57, 58). Secretion of exosomes can be divided into an ESCRT mechanism and a RAB31-mediated mechanism independent of ESCRT (59). Despite being previously viewed as waste materials, exosomes are now acknowledged as vital components of the intercellular communication network (60). Exosomes, containing biologically active substances can be found in bodily fluids and are discharged by originating cells (54, 61). Exosomes are structurally more stable than parent cells due to their higher concentration of lipid components (62). CD81 and CD63 are common exosome markers, and along with CD82 and CD37, are highly abundant transmembrane proteins in exosomes. Exosomes also carry a diverse range of membrane signaling proteins (63). These signaling molecules can be delivered to target cells by exosomes (64), making them an integral component of TME communication.
As researchers continue to investigate exosomes, their overall functions have become increasingly evident. In a normal physiological context, exosomes contribute to the maintenance of immune response, cell proliferation, maturation, and homeostasis (65). Exosomes have been identified to play crucial roles in various processes within TME, including but not limited to immune regulation, promotion of cancer cell proliferation, metastasis, drug resistance, and angiogenesis (66, 67).
Exosomes can facilitate crosstalk between B cells and other cells, making them a potent target for cancer treatment ( Table 1 ).
Table 1.
Exosome crosstalk between B cells and other cells.
| Other cell-derived exosomes act on B cells | ||||||
|---|---|---|---|---|---|---|
| Tumor type | Source | In vivo/in vitro | Action type/specific axis | Effect | Effects on tumors | Ref. |
| —— | DC | In vivo | Stimulate B cell proliferation | CD8 + T cell response was induced | Kill cancer cells | (68) |
| —— | Mature DC | In vivo | Binds to B cell receptors | Induces T cell proliferation | —— | (69) |
| —— | T cells | In vivo | —— | Promote B cell proliferation and differentiation | —— | (70) |
| —— | Mesenchymal cells | —— | TGF-β1 is produced | Regulates B cell proliferation and survival | —— | (71) |
| HCC | Tumor cells | In vitro | HMGB1-TLR2/4-MAPK | Induction of B cells to become TIM-1Breg, impairing CD 8T cell function | Promote HCC progression | (72) |
| HNSCC | plasma | In vitro | —— | Inhibits the proliferation, viability and function of B cells | Helps immune escape | (73) |
| B-cell-derived exosomes act on other cells | ||||||
| Tumor type | Target cells | In vivo/in vitro | Action type/specific axis | Effect | Effects on tumors | Ref. |
| Ovarian cancer | cancer cell | In vitro | miR-330-3p/JAM2 axis | Inducing mesenchymal procedures | Promote the growth of cancer cells | (74) |
| —— | T cell | In vivo | Rab27a expression is up-regulated | Impaired CD8T cell response | Promote tumor survival | (75) |
| —— | T cell | In vivo | C3 fragments are deposited on the surface of the cell membrane | Enhance T cell response, conducive to the development of immune response | Inhibits tumors | (76) |
| —— | Macrophages | In vivo | Enhances lipopolysaccharide stimulation | Reduces the release of TNFα | Promote tumor survival | (77) |
3.2. application of exosomes in cancer therapy
Exosomes are widely recognized as significant biomarkers for cancer diagnosis, prediction, and monitoring (78). Due to their stability and prevalence in circulation, they serve as valuable indicators for liquid biopsy techniques (79), enabling more accurate and less invasive treatments (80). Considering the active cross-talk of exosomes between immune and cancer cells, they can be utilized for immunotherapy to promote (81, 82) or suppress (83, 84) tumor proliferation. Additionally, cancer vaccines based on exosomes have also been developed (85).
Compared to other types of extracellular vesicles (microvesicles, membrane particles, apoptotic bodies), the majority of the biological components, lipids, and proteins of exosomes are relatively clear (86). In comparison to synthetic nanovesicles (polymeric nanoparticles, liposomes, and solid lipid nanoparticles), exosomes possess more membrane proteins, stronger biocompatibility, and a longer circulation half-life naturally (87). They can easily pass through the plasma membrane, blood, and blood-brain barrier (88) to infiltrate tumor tissues (89), which allows for precise and targeted therapeutic interventions (90). Consequently, emerging research is focused on the development and design of bioengineered exosomes.
Bioengineered exosomes can be designed to target specific cells, provide therapeutic cargo, and regulate the immune system (11).
Certain surface-adhesive proteins and carrier ligands allow exosomes to attach to target cell surfaces and efficiently deliver them into the cells (91). Exosomes can efficiently deliver drugs like paclitaxel (92), transport siRNA (93, 94). But the presence of the blood-brain barrier (BBB) limits the access of small molecule drugs to glioma tissue (95). Exosomes derived from brain endothelial cells can transport drugs to BBB, which may become a breakthrough for the treatment of brain cancer (96).
Immune suppressive factors can inhibit the function of immune cells (97–100). By transporting cargo that neutralizes these immune suppressive factors, exosomes can enhance the body’s anti-tumor immune response and improve the efficacy of cancer immunotherapy. An investigation has demonstrated that the T-cell suppressive effects of exosomes can be mitigated by the administration of anti-TGF-β (101). Franz L and colleagues conducted a PD-1 blockade experiment using EV secreted by glioblastoma, which almost reactivated T cells and suppressed tumor progression (102). In the HNSCC microenvironment, the T-cell inhibitory effect of circulating PD-L1 exosomes can be blocked by PD-1 antibodies (103). However, the interference of molecules carried by exosomes in immunotherapy may be related to mechanisms of drug resistance (104, 105).
4. B-cell-derived exosomes and the tumor microenvironment
The investigation of B cell-derived exosomes initiated with the initial characterization of these vesicles in 1996 (106). Through their surface effector molecules, these exosomes can signal to various cells to regulate the TME ( Figure 1B ).
4.1. The biological components of exosomes released by B cells
Mass spectrometry analysis has uncovered a wealth of constituents in exosomes originating from B cells, including MHC-I, MHC-II, CD20, CD45, and BCR complexes (comprising surface Ig, CD19, and Tetraspanins), as well as chaperones such as heat shock protein 70 and 90, integrins and other proteins (107–109). Furthermore, these exosomes also express cholesterol, sphingomyelin, and ganglioside GM3 (107). Addition of macrophage-derived exosomes to naive monocytes induces cell differentiation (110), however this mechanism is unclear in B cells and B cell exosomes. When B cells are activated, they release a greater amount of exosomes (111, 112), which carry more effector molecules (77, 108, 109). CD45 is a key positive regulator of the BCR-mediated signalling pathway (113, 114) and, interestingly, is absent from T-cell-derived exosomes (115, 116). Triggering the classical NF-κB pathway via downstream of BCR is able to increase HLA expression in B-cell exosomes (111). However, these two regulatory pathways may be linked and need to be explored in further experimental studies.
4.2. Mechanism of involvement of components of B cell-derived exosomes in the tumour process
4.2.1. Proteins
MHC-II molecules in exosomes are predominantly located in SLOs and are expressed exclusively by professional APCs, including B cells (117). The presence of CD20, CD81, and HSC70 is associated with MHC-II on the plasma membrane, which promotes antigen presentation and T cell activation (118). CD20 can form complexes with both MHC-II and CD40 (119), while the R21 monoclonal antibody selectively recognizes CD20 on B cells. Additionally, R21 mAb can induce lfa-1-dependent cell adhesion but inhibits MHC-II-mediated lfa-1-dependent cell adhesion. It’s worth noting that CD40 may interfere with mAb binding to CD20 by competitively binding with it (119).
It is not surprising that exosomes are present in TLSs, as B cells are abundant in these structures (120). CD20 can form complexes with BCR to participate in signal transduction (121), ultimately initiating immune responses. Additionally, CD20 can activate B cells through calcium channels (122), and the resulting stimulated calcium channels may induce the release of a large number of exosomes (108). Some of the mechanisms of CD20 are not yet clear (37). The augmented abundance of CD20-positive B lymphocytes in sentinel lymph nodes is indicative of a favorable prognosis in cases of breast cancer (123). CD20 accumulates at the tumour-liver border in patients with colorectal cancer (124), where it may act as a prognostic marker for the tumour.
These indications suggest that these complexes may be crucial factors in MHC-II or antigen-mediated B cell responses.
B cell-derived exosomes express MHC-II and form a complex (PMHC-II) with peptide antigens. The notion that B-cell exosomal exosomes may transport PMHC-II, proposed more than 20 years ago (106), is confirmed. Exosomes released by most primary B cells express PMHC-II. When antigen-loaded B cells meet specific T cells, B cell activation stimulates exosome release, while stimulating pMHC-II to escape intracellular degradation. pMHC-II interacts with the TCR and activates naive CD4 T cells to initiate an immune response (125). However, exosomes from mature DCs only activate naïve T cells as inefficient APCs (126).
4.2.2. ncRNAs
B-cell exosomes have emerged as viable candidates for the delivery of miRNA-155. When miRNA-155 inhibitor-loaded exosomes were administered to miRNA-155 knockout mice, a notable reduction in TNF-α production was observed in mouse RAW macrophages (77). After treatment with rituximab, a downregulation of miR-155 levels in exosomes was observed (127). This study highlights the potential of B cell-derived exosomes as therapeutic vehicles.
MiR-330-3p has been identified as a key factor in tumor progression. It targets TPX2, which negatively regulates TPX2 expression to inhibit melanoma cell proliferation (128). In addition, miR-330-3p from plasma cell-derived exosomes is a critical regulator of ovarian cancer stroma and promotes tumor metastasis through the JAM2 pathway (74). TPX2 (129) and JAM2 (130, 131) have been described as associated with cancer progression. However, the ability of miR-330-3p to target these proteins may suggest a potentially important role for our B-cell exosome miR-330-3p.
4.3. B cell-derived exosomes are taken up by other cells
4.3.1. Follicular dendritic cells
In vitro isolated B cell-derived exosomes specifically bind follicular dendritic cells (FDC) (132). The fate of B cells in GC depends on the adhesion of the VCAM-1 pathway and is associated with FDC (133). More importantly, FDC themselves do not express MHC-II, but rather pick up peptide-loaded MHC-II on the surface of B cells (134). Exosome binding to FDC may be through interaction with VCAM-1, which then stimulates T helper cells. Additionally, tumor-associated FDCs express CXCL13, which effectively recruits lymphocytes (135). We postulate that in tumor tissues, FDCs may attract B cells, which then bind to the released exosomes, leading to antigen presentation. Therefore, FDCs may represent a physiological target for B cell-derived exosomes (132).
4.3.2. Fibroblasts
Compared to FDCs, fibroblasts exhibit a limited expression of leukocyte adhesion molecules on their surface (132). Treatment of fibroblasts with TNF-α induces the upregulation of ICAM-1 expression on their surface, thereby enhancing the adhesion of B cell-derived exosomes to fibroblast surfaces (136). TNF-α may be a key factor in inducing exosomes to be adsorbed.
4.3.3. Macrophages
In the subcapsular sinus of the lymph node, B-cell-derived exosomes are captured by CD169 macrophages, which then penetrate deep into the paracortex (137). CD169+ cells are present within B-cell follicles (138) and the T-B cell zone boundary of the GC (139). The presentation of antigens by CD169+ cells to CD8 T cells and/or B cells causes them to being activated (140). Activated B cells may release more exosomes. Exosome-induced CTL responses (141) are enhanced in CD169+ mice in cooperation with T and B cells, suggesting that exosomes enter lymphoid organs possibly to reduce the immune response to autoantigens (137).
5. Discussion
In recent years, exosomes have gained increasing attention as important mediators of intercellular communication. While many studies have focused on cancer cell-derived exosomes for diagnosis, prognostic testing, and drug delivery, less is known about exosomes derived from B cells. Fortunately, there are still some relevant studies targeting B-cell-derived exosomes, as outlined in our earlier discussion.
As previously outlined, the effective delivery of miRNA-155 by B cell-derived exosomes has been established. For the delivery of miR-330-3p, researchers may consider the design of a B cell (142) transfected with the V600E mutation. Subsequently, lipid transfection or electroporation can be employed to introduce the miR-330-3p construct into B cells. In addition, the design of a short hairpin RNA (shRNA) or small interfering RNA (siRNA) targeting TPX2 is essential. These molecules should be transfected into B cells along with miR-330-3p for culture, followed by the isolation of exosomes. To enhance the yield of exosomes, researchers can employ additional stimuli, such as TLR3, TLR7, TLR9, and other motifs discussed earlier.It is crucial to emphasize that researchers must continually optimize and thoroughly validate the experimental design at each stage to ensure the exosomes effectively downregulate TPX2 and inhibit melanoma growth. It should be noted that miR-330-3p and TPX2 are merely two components of a complex regulatory network, and their specific roles and effects on tumor growth are contingent upon various factors in the experimental context. Furthermore, although the production of exosomes with multiple engineered cargoes is theoretically feasible, it may induce cellular stress or potentially cytotoxic effects, thereby posing challenges for manipulation.
The study of B-cell-derived exosomes for cancer therapy presents a number of challenges, including inadequate comprehension of their interactions within the complex milieu of TME and insufficient clinical investigations to verify their functionality and potential side effects. We anticipate that with increasing research into B-cell-derived exosomes, their functions and the mechanisms underlying their biological components will soon become clearer.
Author contributions
JX, FY and GT conceived the study. JX, HC and GY drafted the manuscript. JX, SZ, JZ, LT and ZX performed the literature search and collected the data. ZX, FY and GT helped with the final revision of this manuscript. All authors contributed to the article and approved the submitted version.
Funding Statement
This study was supported by grants from the Luzhou Science and Technology Department Applied Basic Research program (No: 2022-JYJ-145), the Sichuan Province Science and Technology Department of foreign (border) high-end talent introduction project (No: 2023JDGD0037), and Sichuan Provincial Medical Association (No: Q22027).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fimmu.2023.1188760/full#supplementary-material
There can be many types of B cells (plasma cells, memory B cells, breg, TIL-B). In their respective ways, they regulate the tumor microenvironment and affect tumor growth.
References
- 1. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin (2021) 71:209–49. doi: 10.3322/caac.21660 [DOI] [PubMed] [Google Scholar]
- 2. Paget S. The distribution of secondary growths in cancer of the breast. 1889. Cancer Metastasis Rev (1989) 8:98–101. [PubMed] [Google Scholar]
- 3. Chen F, Zhuang X, Lin L, Yu P, Wang Y, Shi Y, et al. New horizons in tumor microenvironment biology: challenges and opportunities. BMC Med (2015) 13:45. doi: 10.1186/s12916-015-0278-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bejarano L, Jordāo MJC, Joyce JA. Therapeutic targeting of the tumor microenvironment. Cancer Discov (2021) 11:933–59. doi: 10.1158/2159-8290.CD-20-1808 [DOI] [PubMed] [Google Scholar]
- 5. Xia L, Oyang L, Lin J, Tan S, Han Y, Wu N, et al. The cancer metabolic reprogramming and immune response. Mol Cancer (2021) 20:28. doi: 10.1186/s12943-021-01316-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Dai J, Su Y, Zhong S, Cong L, Liu B, Yang J, et al. Exosomes: key players in cancer and potential therapeutic strategy. Signal Transduct Target Ther (2020) 5:145. doi: 10.1038/s41392-020-00261-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Qin SY, Zhang AQ, Cheng SX, Rong L, Zhang XZ. Drug self-delivery systems for cancer therapy. Biomaterials (2017) 112:234–47. doi: 10.1016/j.biomaterials.2016.10.016 [DOI] [PubMed] [Google Scholar]
- 8. Wei G, Wang Y, Yang G, Wang Y, Ju R. Recent progress in nanomedicine for enhanced cancer chemotherapy. Theranostics (2021) 11:6370–92. doi: 10.7150/thno.57828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ke X, Shen L. Molecular targeted therapy of cancer: the progress and future prospect. Front Lab Med (2017) 1:69–75. doi: 10.1016/j.flm.2017.06.001 [DOI] [Google Scholar]
- 10. Choi H, Choi Y, Yim HY, Mirzaaghasi A, Yoo JK, Choi C. Biodistribution of exosomes and engineering strategies for targeted delivery of therapeutic exosomes. Tissue Eng Regener Med (2021) 18:499–511. doi: 10.1007/s13770-021-00361-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Zhang X, Zhang H, Gu J, Zhang J, Shi H, Qian H, et al. Engineered extracellular vesicles for cancer therapy. Adv Mater (2021) 33:e2005709. doi: 10.1002/adma.202005709 [DOI] [PubMed] [Google Scholar]
- 12. Yang D, Zhang W, Zhang H, Zhang F, Chen L, Ma L, et al. Progress, opportunity, and perspective on exosome isolation - efforts for efficient exosome-based theranostics. Theranostics (2020) 10:3684–707. doi: 10.7150/thno.41580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Dieu-Nosjean MC, Giraldo NA, Kaplon H, Germain C, Fridman WH, Sautès-Fridman C. Tertiary lymphoid structures, drivers of the anti-tumor responses in human cancers. Immunol Rev (2016) 271:260–75. doi: 10.1111/imr.12405 [DOI] [PubMed] [Google Scholar]
- 14. Deguchi S, Tanaka H, Suzuki S, Natsuki S, Mori T, Miki Y, et al. Clinical relevance of tertiary lymphoid structures in esophageal squamous cell carcinoma. BMC Cancer (2022) 22:699. doi: 10.1186/s12885-022-09777-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ruffin AT, Cillo AR, Tabib T, Liu A, Onkar S, Kunning SR, et al. B cell signatures and tertiary lymphoid structures contribute to outcome in head and neck squamous cell carcinoma. Nat Commun (2021) 12:3349. doi: 10.1038/s41467-021-23355-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Yadav D, Puranik N, Meshram A, Chavda V, Lee PC, Jin JO. How advanced are cancer immuno-nanotherapeutics? a comprehensive review of the literature. Int J Nanomed (2023) 18:35–48. doi: 10.2147/IJN.S388349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Downs-Canner SM, Meier J, Vincent BG, Serody JS. B cell function in the tumor microenvironment. Annu Rev Immunol (2022) 40:169–93. doi: 10.1146/annurev-immunol-101220-015603 [DOI] [PubMed] [Google Scholar]
- 18. Fridman WH, Meylan M, Petitprez F, Sun CM, Italiano A, Sautès-Fridman C. B cells and tertiary lymphoid structures as determinants of tumour immune contexture and clinical outcome. Nat Rev Clin Oncol (2022) 19:441–57. doi: 10.1038/s41571-022-00619-z [DOI] [PubMed] [Google Scholar]
- 19. Ghamlouch H, Ouled-Haddou H, Guyart A, Regnier A, Trudel S, Claisse JF, et al. TLR9 ligand (CpG oligodeoxynucleotide) induces CLL b-cells to differentiate into CD20(+) antibody-secreting cells. Front Immunol (2014) 5:292. doi: 10.3389/fimmu.2014.00292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. LeBien TW, Tedder TF. B lymphocytes: how they develop and function. Blood (2008) 112:1570–80. doi: 10.1182/blood-2008-02-078071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Sharonov GV, Serebrovskaya EO, Yuzhakova DV, Britanova OV, Chudakov DM. B cells, plasma cells and antibody repertoires in the tumour microenvironment. Nat Rev Immunol (2020) 20:294–307. doi: 10.1038/s41577-019-0257-x [DOI] [PubMed] [Google Scholar]
- 22. Kim SS, Sumner WA, Miyauchi S, Cohen EEW, Califano JA, Sharabi AB. Role of b cells in responses to checkpoint blockade immunotherapy and overall survival of cancer patients. Clin Cancer Res (2021) 27:6075–82. doi: 10.1158/1078-0432.CCR-21-0697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Palm AE, Henry C. Remembrance of things past: long-term b cell memory after infection and vaccination. Front Immunol (2019) 10:1787. doi: 10.3389/fimmu.2019.01787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Cencioni MT, Mattoscio M, Magliozzi R, Bar-Or A, Muraro PA. B cells in multiple sclerosis - from targeted depletion to immune reconstitution therapies. Nat Rev Neurol (2021) 17:399–414. doi: 10.1038/s41582-021-00498-5 [DOI] [PubMed] [Google Scholar]
- 25. Rousset F, Peyrol S, Garcia E, Vezzio N, Andujar M, Grimaud JA, et al. Long-term cultured CD40-activated b lymphocytes differentiate into plasma cells in response to IL-10 but not IL-4. Int Immunol (1995) 7:1243–53. doi: 10.1093/intimm/7.8.1243 [DOI] [PubMed] [Google Scholar]
- 26. Shaul ME, Zlotnik A, Tidhar E, Schwartz A, Arpinati L, Kaisar-Iluz N, et al. Tumor-associated neutrophils drive b-cell recruitment and their differentiation to plasma cells. Cancer Immunol Res (2021) 9:811–24. doi: 10.1158/2326-6066.CIR-20-0839 [DOI] [PubMed] [Google Scholar]
- 27. Packard TA, Cambier JC. B lymphocyte antigen receptor signaling: initiation, amplification, and regulation. F1000Prime Rep (2013) 5:40. doi: 10.12703/P5-40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Vitale G, Mion F, Pucillo C. Regulatory b cells: evidence, developmental origin and population diversity. Mol Immunol (2010) 48:1–8. doi: 10.1016/j.molimm.2010.09.010 [DOI] [PubMed] [Google Scholar]
- 29. Peng B, Ming Y, Yang C. Regulatory b cells: the cutting edge of immune tolerance in kidney transplantation. Cell Death Dis (2018) 9:109. doi: 10.1038/s41419-017-0152-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Rosser EC, Mauri C. Regulatory b cells: origin, phenotype, and function. Immunity (2015) 42:607–12. doi: 10.1016/j.immuni.2015.04.005 [DOI] [PubMed] [Google Scholar]
- 31. Rosser EC, Mauri C. The emerging field of regulatory b cell immunometabolism. Cell Metab (2021) 33:1088–97. doi: 10.1016/j.cmet.2021.05.008 [DOI] [PubMed] [Google Scholar]
- 32. Siliņa K, Soltermann A, Attar FM, Casanova R, Uckeley ZM, Thut H, et al. Germinal centers determine the prognostic relevance of tertiary lymphoid structures and are impaired by corticosteroids in lung squamous cell carcinoma. Cancer Res (2018) 78:1308–20. doi: 10.1158/0008-5472.CAN-17-1987 [DOI] [PubMed] [Google Scholar]
- 33. Neyt K, Perros F, GeurtsvanKessel CH, Hammad H, Lambrecht BN. Tertiary lymphoid organs in infection and autoimmunity. Trends Immunol (2012) 33:297–305. doi: 10.1016/j.it.2012.04.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Wang SS, Liu W, Ly D, Xu H, Qu L, Zhang L. Tumor-infiltrating b cells: their role and application in anti-tumor immunity in lung cancer. Cell Mol Immunol (2019) 16:6–18. doi: 10.1038/s41423-018-0027-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Yang C, Lee H, Pal S, Jove V, Deng J, Zhang W, et al. B cells promote tumor progression via STAT3 regulated-angiogenesis. PloS One (2013) 8:e64159. doi: 10.1371/journal.pone.0064159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Ammirante M, Luo JL, Grivennikov S, Nedospasov S, Karin M. B-cell-derived lymphotoxin promotes castration-resistant prostate cancer. Nature (2010) 464:302–5. doi: 10.1038/nature08782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Pavlasova G, Mraz M. The regulation and function of CD20: an “enigma” of b-cell biology and targeted therapy. Haematologica (2020) 105:1494–506. doi: 10.3324/haematol.2019.243543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Ding C, Wang L, Marroquin J, Yan J. Targeting of antigens to b cells augments antigen-specific T-cell responses and breaks immune tolerance to tumor-associated antigen MUC1. Blood (2008) 112:2817–25. doi: 10.1182/blood-2008-05-157396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Pylayeva-Gupta Y, Das S, Handler JS, Hajdu CH, Coffre M, Koralov SB, et al. IL35-producing b cells promote the development of pancreatic neoplasia. Cancer Discovery (2016) 6:247–55. doi: 10.1158/2159-8290.CD-15-0843 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. He Y, Qian H, Liu Y, Duan L, Li Y, Shi G. The roles of regulatory b cells in cancer. J Immunol Res (2014) 2014:215471. doi: 10.1155/2014/215471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Bodogai M, Lee Chang C, Wejksza K, Lai J, Merino M, Wersto RP, et al. Anti-CD20 antibody promotes cancer escape via enrichment of tumor-evoked regulatory b cells expressing low levels of CD20 and CD137L. Cancer Res (2013) 73:2127–38. doi: 10.1158/0008-5472.CAN-12-4184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Groeneveld CS, Fontugne J, Cabel L, Bernard-Pierrot I, Radvanyi F, Allory Y, et al. Tertiary lymphoid structures marker CXCL13 is associated with better survival for patients with advanced-stage bladder cancer treated with immunotherapy. Eur J Cancer (2021) 148:181–9. doi: 10.1016/j.ejca.2021.01.036 [DOI] [PubMed] [Google Scholar]
- 43. Petitprez F, de Reyniès A, Keung EZ, Chen TW, Sun CM, Calderaro J, et al. B cells are associated with survival and immunotherapy response in sarcoma. Nature (2020) 577:556–60. doi: 10.1038/s41586-019-1906-8 [DOI] [PubMed] [Google Scholar]
- 44. Lauss M, Donia M, Svane IM, Jönsson G. B cells and tertiary lymphoid structures: friends or foes in cancer immunotherapy? Clin Cancer Res (2022) 28:1751–8. doi: 10.1158/1078-0432.CCR-21-1130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Lu Y, Zhao Q, Liao JY, Song E, Xia Q, Pan J, et al. Complement signals determine opposite effects of b cells in chemotherapy-induced immunity. Cell (2020) 180:1081–1097.e1024. doi: 10.1016/j.cell.2020.02.015 [DOI] [PubMed] [Google Scholar]
- 46. Lutz ER, Wu AA, Bigelow E, Sharma R, Mo G, Soares K, et al. Immunotherapy converts nonimmunogenic pancreatic tumors into immunogenic foci of immune regulation. Cancer Immunol Res (2014) 2:616–31. doi: 10.1158/2326-6066.CIR-14-0027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Tokunaga R, Naseem M, Lo JH, Battaglin F, Soni S, Puccini A, et al. B cell and b cell-related pathways for novel cancer treatments. Cancer Treat Rev (2019) 73:10–9. doi: 10.1016/j.ctrv.2018.12.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Feng Y, Liu L, Li J, Huang J, Xie JH, Menard L, et al. Systematic characterization of the tumor microenvironment in Chinese patients with hepatocellular carcinoma highlights intratumoral b cells as a potential immunotherapy target. Oncol Rep (2022) 47 (2): 38. doi: 10.3892/or.2021.8249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Gurunathan S, Kang M-H, Jeyaraj M, Qasim M, Kim J-H. Review of the isolation, characterization, biological function, and multifarious therapeutic approaches of exosomes. Cells (2019) 8:307. doi: 10.3390/cells8040307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Yan W, Jiang S. Immune cell-derived exosomes in the cancer-immunity cycle. Trends Cancer (2020) 6:506–17. doi: 10.1016/j.trecan.2020.02.013 [DOI] [PubMed] [Google Scholar]
- 51. Mashouri L, Yousefi H, Aref AR, Ahadi AM, Molaei F, Alahari SK. Exosomes: composition, biogenesis, and mechanisms in cancer metastasis and drug resistance. Mol Cancer (2019) 18:75. doi: 10.1186/s12943-019-0991-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Samuel M, Gabrielsson S. Personalized medicine and back-allogeneic exosomes for cancer immunotherapy. J Intern Med (2021) 289:138–46. doi: 10.1111/joim.12963 [DOI] [PubMed] [Google Scholar]
- 53. Nam GH, Choi Y, Kim GB, Kim S, Kim SA, Kim IS. Emerging prospects of exosomes for cancer treatment: from conventional therapy to immunotherapy. Adv Mater (2020) 32:e2002440. doi: 10.1002/adma.202002440 [DOI] [PubMed] [Google Scholar]
- 54. Huang T, Deng CX. Current progresses of exosomes as cancer diagnostic and prognostic biomarkers. Int J Biol Sci (2019) 15:1–11. doi: 10.7150/ijbs.27796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Wu M, Wang G, Hu W, Yao Y, Yu XF. Emerging roles and therapeutic value of exosomes in cancer metastasis. Mol Cancer (2019) 18:53. doi: 10.1186/s12943-019-0964-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Zhang L, Yu D. Exosomes in cancer development, metastasis, and immunity. Biochim Biophys Acta Rev Cancer (2019) 1871:455–68. doi: 10.1016/j.bbcan.2019.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Ostrowski M, Carmo NB, Krumeich S, Fanget I, Raposo G, Savina A, et al. Rab27a and Rab27b control different steps of the exosome secretion pathway. Nat Cell Biol (2010) 12:19–30. doi: 10.1038/ncb2000 [DOI] [PubMed] [Google Scholar]
- 58. Hsu C, Morohashi Y, Yoshimura S, Manrique-Hoyos N, Jung S, Lauterbach MA, et al. Regulation of exosome secretion by Rab35 and its GTPase-activating proteins TBC1D10A-c. J Cell Biol (2010) 189:223–32. doi: 10.1083/jcb.200911018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Wei D, Zhan W, Gao Y, Huang L, Gong R, Wang W, et al. RAB31 marks and controls an ESCRT-independent exosome pathway. Cell Res (2021) 31:157–77. doi: 10.1038/s41422-020-00409-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Milane L, Singh A, Mattheolabakis G, Suresh M, Amiji MM. Exosome mediated communication within the tumor microenvironment. J Control Release (2015) 219:278–94. doi: 10.1016/j.jconrel.2015.06.029 [DOI] [PubMed] [Google Scholar]
- 61. Tan S, Xia L, Yi P, Han Y, Tang L, Pan Q, et al. Exosomal miRNAs in tumor microenvironment. J Exp Clin Cancer Res (2020) 39:67. doi: 10.1186/s13046-020-01570-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Kalluri R, LeBleu VS. The biology, function, and biomedical applications of exosomes. Science (2020) 367 (6478):eaau6977. doi: 10.1126/science.aau6977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Pegtel DM, Gould SJ. Exosomes. Annu Rev Biochem (2019) 88:487–514. doi: 10.1146/annurev-biochem-013118-111902 [DOI] [PubMed] [Google Scholar]
- 64. Tkach M, Théry C. Communication by extracellular vesicles: where we are and where we need to go. Cell (2016) 164:1226–32. doi: 10.1016/j.cell.2016.01.043 [DOI] [PubMed] [Google Scholar]
- 65. Li J, Li S, Guo J, Li Q, Long J, Ma C, et al. Natural product micheliolide (MCL) irreversibly activates pyruvate kinase M2 and suppresses leukemia. J Med Chem (2018) 61:4155–64. doi: 10.1021/acs.jmedchem.8b00241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Shao Y, Shen Y, Chen T, Xu F, Chen X, Zheng S. The functions and clinical applications of tumor-derived exosomes. Oncotarget (2016) 7:60736–51. doi: 10.18632/oncotarget.11177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Yang K, Zhou Q, Qiao B, Shao B, Hu S, Wang G, et al. Exosome-derived noncoding RNAs: function, mechanism, and application in tumor angiogenesis. Mol Ther Nucleic Acids (2022) 27:983–97. doi: 10.1016/j.omtn.2022.01.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Näslund TI, Gehrmann U, Qazi KR, Karlsson MC, Gabrielsson S. Dendritic cell-derived exosomes need to activate both T and b cells to induce antitumor immunity. J Immunol (2013) 190:2712–9. doi: 10.4049/jimmunol.1203082 [DOI] [PubMed] [Google Scholar]
- 69. Segura E, Nicco C, Lombard B, Véron P, Raposo G, Batteux F, et al. ICAM-1 on exosomes from mature dendritic cells is critical for efficient naive T-cell priming. Blood (2005) 106:216–23. doi: 10.1182/blood-2005-01-0220 [DOI] [PubMed] [Google Scholar]
- 70. Tay NQ, Lee DCP, Chua YL, Prabhu N, Gascoigne NRJ, Kemeny DM. CD40L expression allows CD8(+) T cells to promote their own expansion and differentiation through dendritic cells. Front Immunol (2017) 8:1484. doi: 10.3389/fimmu.2017.01484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Bruno S, Deregibus MC, Camussi G. The secretome of mesenchymal stromal cells: role of extracellular vesicles in immunomodulation. Immunol Lett (2015) 168:154–8. doi: 10.1016/j.imlet.2015.06.007 [DOI] [PubMed] [Google Scholar]
- 72. Ye L, Zhang Q, Cheng Y, Chen X, Wang G, Shi M, et al. Tumor-derived exosomal HMGB1 fosters hepatocellular carcinoma immune evasion by promoting TIM-1(+) regulatory b cell expansion. J Immunother Cancer (2018) 6:145. doi: 10.1186/s40425-018-0451-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Schroeder JC, Puntigam L, Hofmann L, Jeske SS, Beccard IJ, Doescher J, et al. Circulating exosomes inhibit b cell proliferation and activity. Cancers (Basel) (2020) 12 (8): 2110. doi: 10.3390/cancers12082110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Yang Z, Wang W, Zhao L, Wang X, Gimple RC, Xu L, et al. Plasma cells shape the mesenchymal identity of ovarian cancers through transfer of exosome-derived microRNAs. Sci Adv (2021) 7 (9): eabb0737. doi: 10.1126/sciadv.abb0737 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Zhang F, Li R, Yang Y, Shi C, Shen Y, Lu C, et al. Specific decrease in b-Cell-Derived extracellular vesicles enhances post-chemotherapeutic CD8(+) T cell responses. Immunity (2019) 50:738–750.e737. doi: 10.1016/j.immuni.2019.01.010 [DOI] [PubMed] [Google Scholar]
- 76. Papp K, Végh P, Prechl J, Kerekes K, Kovács J, Csikós G, et al. B lymphocytes and macrophages release cell membrane deposited C3-fragments on exosomes with T cell response-enhancing capacity. Mol Immunol (2008) 45:2343–51. doi: 10.1016/j.molimm.2007.11.021 [DOI] [PubMed] [Google Scholar]
- 77. Momen-Heravi F, Bala S, Bukong T, Szabo G. Exosome-mediated delivery of functionally active miRNA-155 inhibitor to macrophages. Nanomedicine (2014) 10:1517–27. doi: 10.1016/j.nano.2014.03.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Zhu L, Sun HT, Wang S, Huang SL, Zheng Y, Wang CQ, et al. Isolation and characterization of exosomes for cancer research. J Hematol Oncol (2020) 13:152. doi: 10.1186/s13045-020-00987-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Ma S, Zhou M, Xu Y, Gu X, Zou M, Abudushalamu G, et al. Clinical application and detection techniques of liquid biopsy in gastric cancer. Mol Cancer (2023) 22:7. doi: 10.1186/s12943-023-01715-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Nikanjam M, Kato S, Kurzrock R. Liquid biopsy: current technology and clinical applications. J Hematol Oncol (2022) 15:131. doi: 10.1186/s13045-022-01351-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Filipazzi P, Bürdek M, Villa A, Rivoltini L, Huber V. Recent advances on the role of tumor exosomes in immunosuppression and disease progression. Semin Cancer Biol (2012) 22:342–9. doi: 10.1016/j.semcancer.2012.02.005 [DOI] [PubMed] [Google Scholar]
- 82. Whiteside TL. Immune modulation of T-cell and NK (natural killer) cell activities by TEXs (tumour-derived exosomes). Biochem Soc Trans (2013) 41:245–51. doi: 10.1042/BST20120265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Wolfers J, Lozier A, Raposo G, Regnault A, Théry C, Masurier C, et al. Tumor-derived exosomes are a source of shared tumor rejection antigens for CTL cross-priming. Nat Med (2001) 7:297–303. doi: 10.1038/85438 [DOI] [PubMed] [Google Scholar]
- 84. Zhang HG, Zhuang X, Sun D, Liu Y, Xiang X, Grizzle WE. Exosomes and immune surveillance of neoplastic lesions: a review. Biotech Histochem (2012) 87:161–8. doi: 10.3109/10520291003659042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Zuo B, Zhang Y, Zhao K, Wu L, Qi H, Yang R, et al. Universal immunotherapeutic strategy for hepatocellular carcinoma with exosome vaccines that engage adaptive and innate immune responses. J Hematol Oncol (2022) 15:46. doi: 10.1186/s13045-022-01266-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. van der Pol E, Böing AN, Harrison P, Sturk A, Nieuwland R. Classification, functions, and clinical relevance of extracellular vesicles. Pharmacol Rev (2012) 64:676–705. doi: 10.1124/pr.112.005983 [DOI] [PubMed] [Google Scholar]
- 87. Mondal J, Pillarisetti S, Junnuthula V, Saha M, Hwang SR, Park IK, et al. Hybrid exosomes, exosome-like nanovesicles and engineered exosomes for therapeutic applications. J Control Release (2023) 353:1127–49. doi: 10.1016/j.jconrel.2022.12.027 [DOI] [PubMed] [Google Scholar]
- 88. Liu C, Su C. Design strategies and application progress of therapeutic exosomes. Theranostics (2019) 9:1015–28. doi: 10.7150/thno.30853 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Prajapati S, Hinchliffe T, Roy V, Shah N, Jones CN, Obaid G. Biomimetic nanotechnology: a natural path forward for tumor-selective and tumor-specific NIR activable photonanomedicines. Pharmaceutics (2021) 13 (6) :786. doi: 10.3390/pharmaceutics13060786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Turturici G, Tinnirello R, Sconzo G, Geraci F. Extracellular membrane vesicles as a mechanism of cell-to-cell communication: advantages and disadvantages. Am J Physiol Cell Physiol (2014) 306:C621–633. doi: 10.1152/ajpcell.00228.2013 [DOI] [PubMed] [Google Scholar]
- 91. Batrakova EV, Kim MS. Using exosomes, naturally-equipped nanocarriers, for drug delivery. J Control Release (2015) 219:396–405. doi: 10.1016/j.jconrel.2015.07.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Saari H, Lázaro-Ibáñez E, Viitala T, Vuorimaa-Laukkanen E, Siljander P, Yliperttula M. Microvesicle- and exosome-mediated drug delivery enhances the cytotoxicity of paclitaxel in autologous prostate cancer cells. J Control Release (2015) 220:727–37. doi: 10.1016/j.jconrel.2015.09.031 [DOI] [PubMed] [Google Scholar]
- 93. Zhang Y, Li L, Yu J, Zhu D, Zhang Y, Li X, et al. Microvesicle-mediated delivery of transforming growth factor β1 siRNA for the suppression of tumor growth in mice. Biomaterials (2014) 35:4390–400. doi: 10.1016/j.biomaterials.2014.02.003 [DOI] [PubMed] [Google Scholar]
- 94. Zhao L, Gu C, Gan Y, Shao L, Chen H, Zhu H. Exosome-mediated siRNA delivery to suppress postoperative breast cancer metastasis. J Control Release (2020) 318:1–15. doi: 10.1016/j.jconrel.2019.12.005 [DOI] [PubMed] [Google Scholar]
- 95. Lockman PR, Mittapalli RK, Taskar KS, Rudraraju V, Gril B, Bohn KA, et al. Heterogeneous blood-tumor barrier permeability determines drug efficacy in experimental brain metastases of breast cancer. Clin Cancer Res (2010) 16:5664–78. doi: 10.1158/1078-0432.CCR-10-1564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Yang T, Martin P, Fogarty B, Brown A, Schurman K, Phipps R, et al. Exosome delivered anticancer drugs across the blood-brain barrier for brain cancer therapy in danio rerio. Pharm Res (2015) 32:2003–14. doi: 10.1007/s11095-014-1593-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Casey TM, Eneman J, Crocker A, White J, Tessitore J, Stanley M, et al. Cancer associated fibroblasts stimulated by transforming growth factor beta1 (TGF-beta 1) increase invasion rate of tumor cells: a population study. Breast Cancer Res Treat (2008) 110:39–49. doi: 10.1007/s10549-007-9684-7 [DOI] [PubMed] [Google Scholar]
- 98. Fridlender ZG, Sun J, Kim S, Kapoor V, Cheng G, Ling L, et al. Polarization of tumor-associated neutrophil phenotype by TGF-beta: “N1” versus “N2” TAN. Cancer Cell (2009) 16:183–94. doi: 10.1016/j.ccr.2009.06.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Chen Y, Zheng X, Wu C. The role of the tumor microenvironment and treatment strategies in colorectal cancer. Front Immunol (2021) 12:792691. doi: 10.3389/fimmu.2021.792691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Ren B, Cui M, Yang G, Wang H, Feng M, You L, et al. Tumor microenvironment participates in metastasis of pancreatic cancer. Mol Cancer (2018) 17:108. doi: 10.1186/s12943-018-0858-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Rong L, Li R, Li S, Luo R. Immunosuppression of breast cancer cells mediated by transforming growth factor-β in exosomes from cancer cells. Oncol Lett (2016) 11:500–4. doi: 10.3892/ol.2015.3841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Ricklefs FL, Alayo Q, Krenzlin H, Mahmoud AB, Speranza MC, Nakashima H, et al. Immune evasion mediated by PD-L1 on glioblastoma-derived extracellular vesicles. Sci Adv (2018) 4:eaar2766. doi: 10.1126/sciadv.aar2766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Theodoraki MN, Yerneni SS, Hoffmann TK, Gooding WE, Whiteside TL. Clinical significance of PD-L1(+) exosomes in plasma of head and neck cancer patients. Clin Cancer Res (2018) 24:896–905. doi: 10.1158/1078-0432.CCR-17-2664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Turiello R, Capone M, Morretta E, Monti MC, Madonna G, Azzaro R, et al. Exosomal CD73 from serum of patients with melanoma suppresses lymphocyte functions and is associated with therapy resistance to anti-PD-1 agents. J Immunother Cancer (2022) 10:e004043. doi: 10.1136/jitc-2021-004043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Theodoraki MN, Yerneni S, Gooding WE, Ohr J, Clump DA, Bauman JE, et al. Circulating exosomes measure responses to therapy in head and neck cancer patients treated with cetuximab, ipilimumab, and IMRT. Oncoimmunology (2019) 8:1593805. doi: 10.1080/2162402X.2019.1593805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Raposo G, Nijman HW, Stoorvogel W, Liejendekker R, Harding CV, Melief CJ, et al. B lymphocytes secrete antigen-presenting vesicles. J Exp Med (1996) 183:1161–72. doi: 10.1084/jem.183.3.1161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Wubbolts R, Leckie RS, Veenhuizen PT, Schwarzmann G, Möbius W, Hoernschemeyer J, et al. Proteomic and biochemical analyses of human b cell-derived exosomes. Potential implications their Funct multivesicular body formation. J Biol Chem (2003) 278:10963–72. doi: 10.1074/jbc.M207550200 [DOI] [PubMed] [Google Scholar]
- 108. Clayton A, Court J, Navabi H, Adams M, Mason MD, Hobot JA, et al. Analysis of antigen presenting cell derived exosomes, based on immuno-magnetic isolation and flow cytometry. J Immunol Methods (2001) 247:163–74. doi: 10.1016/S0022-1759(00)00321-5 [DOI] [PubMed] [Google Scholar]
- 109. Saunderson SC, Schuberth PC, Dunn AC, Miller L, Hock BD, MacKay PA, et al. Induction of exosome release in primary b cells stimulated via CD40 and the IL-4 receptor. J Immunol (2008) 180:8146–52. doi: 10.4049/jimmunol.180.12.8146 [DOI] [PubMed] [Google Scholar]
- 110. Ismail N, Wang Y, Dakhlallah D, Moldovan L, Agarwal K, Batte K, et al. Macrophage microvesicles induce macrophage differentiation and miR-223 transfer. Blood (2013) 121:984–95. doi: 10.1182/blood-2011-08-374793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Arita S, Baba E, Shibata Y, Niiro H, Shimoda S, Isobe T, et al. B cell activation regulates exosomal HLA production. Eur J Immunol (2008) 38:1423–34. doi: 10.1002/eji.200737694 [DOI] [PubMed] [Google Scholar]
- 112. Calvo V, Izquierdo M. Inducible polarized secretion of exosomes in T and b lymphocytes. Int J Mol Sci (2020) 21 (7) :2631. doi: 10.3390/ijms21072631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Penninger JM, Irie-Sasaki J, Sasaki T, Oliveira-dos-Santos AJ. CD45: new jobs for an old acquaintance. Nat Immunol (2001) 2:389–96. doi: 10.1038/87687 [DOI] [PubMed] [Google Scholar]
- 114. Hermiston ML, Xu Z, Weiss A. CD45: a critical regulator of signaling thresholds in immune cells. Annu Rev Immunol (2003) 21:107–37. doi: 10.1146/annurev.immunol.21.120601.140946 [DOI] [PubMed] [Google Scholar]
- 115. Blanchard N, Lankar D, Faure F, Regnault A, Dumont C, Raposo G, et al. TCR activation of human T cells induces the production of exosomes bearing the TCR/CD3/zeta complex. J Immunol (2002) 168:3235–41. doi: 10.4049/jimmunol.168.7.3235 [DOI] [PubMed] [Google Scholar]
- 116. Richmond A, Nf-kappa B. Chemokine gene transcription and tumour growth. Nat Rev Immunol (2002) 2:664–74. doi: 10.1038/nri887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Lindenbergh MFS, Stoorvogel W. Antigen presentation by extracellular vesicles from professional antigen-presenting cells. Annu Rev Immunol (2018) 36:435–59. doi: 10.1146/annurev-immunol-041015-055700 [DOI] [PubMed] [Google Scholar]
- 118. Buschow SI, van Balkom BW, Aalberts M, Heck AJ, Wauben M, Stoorvogel W. MHC class II-associated proteins in b-cell exosomes and potential functional implications for exosome biogenesis. Immunol Cell Biol (2010) 88:851–6. doi: 10.1038/icb.2010.64 [DOI] [PubMed] [Google Scholar]
- 119. Léveillé C, AL-D R, Mourad W. CD20 is physically and functionally coupled to MHC class II and CD40 on human b cell lines. Eur J Immunol (1999) 29:65–74. doi: [DOI] [PubMed] [Google Scholar]
- 120. Munoz-Erazo L, Rhodes JL, Marion VC, Kemp RA. Tertiary lymphoid structures in cancer - considerations for patient prognosis. Cell Mol Immunol (2020) 17:570–5. doi: 10.1038/s41423-020-0457-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. Polyak MJ, Li H, Shariat N, Deans JP. CD20 homo-oligomers physically associate with the b cell antigen receptor. dissociation upon receptor engagement and recruitment of phosphoproteins and calmodulin-binding proteins. J Biol Chem (2008) 283:18545–52. doi: 10.1074/jbc.M800784200 [DOI] [PubMed] [Google Scholar]
- 122. Bubien JK, Zhou LJ, Bell PD, Frizzell RA, Tedder TF. Transfection of the CD20 cell surface molecule into ectopic cell types generates a Ca2+ conductance found constitutively in b lymphocytes. J Cell Biol (1993) 121:1121–32. doi: 10.1083/jcb.121.5.1121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Sato Y, Shimoda M, Sota Y, Miyake T, Tanei T, Kagara N, et al. Enhanced humoral immunity in breast cancer patients with high serum concentration of anti-HER2 autoantibody. Cancer Med (2021) 10:1418–30. doi: 10.1002/cam4.3742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Meshcheryakova A, Tamandl D, Bajna E, Stift J, Mittlboeck M, Svoboda M, et al. B cells and ectopic follicular structures: novel players in anti-tumor programming with prognostic power for patients with metastatic colorectal cancer. PloS One (2014) 9:e99008. doi: 10.1371/journal.pone.0099008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Muntasell A, Berger AC, Roche PA. T Cell-induced secretion of MHC class II-peptide complexes on b cell exosomes. EMBO J (2007) 26:4263–72. doi: 10.1038/sj.emboj.7601842 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126. Knight AM. Regulated release of b cell-derived exosomes: do differences in exosome release provide insight into different APC function for b cells and DC? Eur J Immunol (2008) 38:1186–9. doi: 10.1002/eji.200838374 [DOI] [PubMed] [Google Scholar]
- 127. Liao TL, Hsieh SL, Chen YM, Chen HH, Liu HJ, Lee HC, et al. Rituximab may cause increased hepatitis c virus viremia in rheumatoid arthritis patients through declining exosomal MicroRNA-155. Arthritis Rheumatol (2018) 70:1209–19. doi: 10.1002/art.40495 [DOI] [PubMed] [Google Scholar]
- 128. Yao Y, Zuo J, Wei Y. Targeting of TRX2 by miR-330-3p in melanoma inhibits proliferation. BioMed Pharmacother (2018) 107:1020–9. doi: 10.1016/j.biopha.2018.08.058 [DOI] [PubMed] [Google Scholar]
- 129. Ma Y, Lin D, Sun W, Xiao T, Yuan J, Han N, et al. Expression of targeting protein for xklp2 associated with both malignant transformation of respiratory epithelium and progression of squamous cell lung cancer. Clin Cancer Res (2006) 12:1121–7. doi: 10.1158/1078-0432.CCR-05-1766 [DOI] [PubMed] [Google Scholar]
- 130. Arcangeli ML, Frontera V, Bardin F, Thomassin J, Chetaille B, Adams S, et al. The junctional adhesion molecule-b regulates JAM-c-dependent melanoma cell metastasis. FEBS Lett (2012) 586:4046–51. doi: 10.1016/j.febslet.2012.10.005 [DOI] [PubMed] [Google Scholar]
- 131. Costa A, Kieffer Y, Scholer-Dahirel A, Pelon F, Bourachot B, Cardon M, et al. Fibroblast heterogeneity and immunosuppressive environment in human breast cancer. Cancer Cell (2018) 33:463–479.e410. doi: 10.1016/j.ccell.2018.01.011 [DOI] [PubMed] [Google Scholar]
- 132. Denzer K, van Eijk M, Kleijmeer MJ, Jakobson E, de Groot C, Geuze HJ. Follicular dendritic cells carry MHC class II-expressing microvesicles at their surface. J Immunol (2000) 165:1259–65. doi: 10.4049/jimmunol.165.3.1259 [DOI] [PubMed] [Google Scholar]
- 133. Koopman G, Keehnen RM, Lindhout E, Newman W, Shimizu Y, van Seventer GA, et al. Adhesion through the LFA-1 (CD11a/CD18)-ICAM-1 (CD54) and the VLA-4 (CD49d)-VCAM-1 (CD106) pathways prevents apoptosis of germinal center b cells. J Immunol (1994) 152:3760–7. doi: 10.4049/jimmunol.152.8.3760 [DOI] [PubMed] [Google Scholar]
- 134. Gray D, Kosco M, Stockinger B. Novel pathways of antigen presentation for the maintenance of memory. Int Immunol (1991) 3:141–8. doi: 10.1093/intimm/3.2.141 [DOI] [PubMed] [Google Scholar]
- 135. Vermi W, Lonardi S, Bosisio D, Uguccioni M, Danelon G, Pileri S, et al. Identification of CXCL13 as a new marker for follicular dendritic cell sarcoma. J Pathol (2008) 216:356–64. doi: 10.1002/path.2420 [DOI] [PubMed] [Google Scholar]
- 136. Clayton A, Turkes A, Dewitt S, Steadman R, Mason MD, Hallett MB. Adhesion and signaling by b cell-derived exosomes: the role of integrins. FASEB J (2004) 18:977–9. doi: 10.1096/fj.03-1094fje [DOI] [PubMed] [Google Scholar]
- 137. Saunderson SC, Dunn AC, Crocker PR, McLellan AD. CD169 mediates the capture of exosomes in spleen and lymph node. Blood (2014) 123:208–16. doi: 10.1182/blood-2013-03-489732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138. Berney C, Herren S, Power CA, Gordon S, Martinez-Pomares L, Kosco-Vilbois MH. A member of the dendritic cell family that enters b cell follicles and stimulates primary antibody responses identified by a mannose receptor fusion protein. J Exp Med (1999) 190:851–60. doi: 10.1084/jem.190.6.851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139. Martínez-Pomares L, Kosco-Vilbois M, Darley E, Tree P, Herren S, Bonnefoy JY, et al. Fc chimeric protein containing the cysteine-rich domain of the murine mannose receptor binds to macrophages from splenic marginal zone and lymph node subcapsular sinus and to germinal centers. J Exp Med (1996) 184:1927–37. doi: 10.1084/jem.184.5.1927 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140. Martinez-Pomares L, Gordon S. CD169+ macrophages at the crossroads of antigen presentation. Trends Immunol (2012) 33:66–70. doi: 10.1016/j.it.2011.11.001 [DOI] [PubMed] [Google Scholar]
- 141. Qazi KR, Gehrmann U, Domange Jordö E, Karlsson MC, Gabrielsson S. Antigen-loaded exosomes alone induce Th1-type memory through a b-cell-dependent mechanism. Blood (2009) 113:2673–83. doi: 10.1182/blood-2008-04-153536 [DOI] [PubMed] [Google Scholar]
- 142. Menzer C, Menzies AM, Carlino MS, Reijers I, Groen EJ, Eigentler T, et al. Targeted therapy in advanced melanoma with rare BRAF mutations. J Clin Oncol (2019) 37:3142–51. doi: 10.1200/JCO.19.00489 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
There can be many types of B cells (plasma cells, memory B cells, breg, TIL-B). In their respective ways, they regulate the tumor microenvironment and affect tumor growth.


