Abstract
Background
Depression is associated with an increased risk for cardiovascular disease (CVD). Biological cardiac risk factors are already elevated in depressed patients without existing CVD. The purpose of this exploratory trial was to examine whether treating Major Depression (MD) with cognitive behavioral therapy (CBT) is associated with improvements in cardiac risk biomarkers and whether depressive symptom severity at baseline moderates treatment effects.
Methods
Eighty antidepressant-free patients with MD were randomly assigned to CBT or waiting list (WL). Biological outcomes included long-term recordings (24-h, daytime, nighttime) of heart rate, heart rate variability (HRV), and blood pressure, as well as inflammatory markers such as C-reactive protein (CRP), interleukin (IL)-6, and tumor necrosis factor (TNF)-α. A sample of 40 age- and sex-matched non-clinical controls was also involved to verify biological alterations in MD at study entry.
Results
Compared to WL, CBT was associated with a significant increase in overall HRV, as indexed by the 24-h and daytime HRV triangular index, as well as trend improvements in 24-h low-frequency HRV and daytime systolic blood pressure. Self-rated depressive symptom severity moderated (or tended to moderate) improvements in CBT for 24-h and daytime heart rate and several indices of HRV (especially daytime measures). Inflammatory treatment effects were not observed.
Conclusions
CBT increased overall HRV in patients with MD. Initially more depressed patients showed the most pronounced cardiovascular improvements through CBT. These exploratory findings may provide new insights into the biological effects of psychological treatment against depression and must be confirmed through future research.
Keywords: Blood pressure, Cognitive behavioral therapy, heart rate variability, inflammation, major depression
Introduction
Depression is associated with an increased risk for the development of cardiovascular disease (CVD) (Gan et al., 2014; Harshfield et al., 2020; Li et al., 2019; Wu & Kling, 2016) and future cardiovascular events in patients with existing CVD (Carney & Freedland, 2017; Goldston & Baillie, 2008; Pelle, Gidron, Szabó, & Denollet, 2008; Spaderna et al., 2017). Cardiac risk biomarkers are already prominent in patients with depression in the absence of CVD. These biological factors include autonomic dysregulation such as reduced heart rate variability (HRV) and increased heart rate (Kemp et al., 2010; Koch, Wilhelm, Salzmann, Rief, & Euteneuer, 2019; Lake et al., 1982; Lehofer et al., 1997), and possibly elevated blood pressure (Ginty, Carroll, Roseboom, Phillips, & de Rooij, 2013; Meng, Chen, Yang, Zheng, & Hui, 2012). In addition to autonomic dysregulation, depression is associated with elevated circulating levels of inflammatory immune markers such as interleukin (IL)-6, tumor necrosis factor (TNF)-α and C-reactive protein (CRP) (Dowlati et al., 2010; Howren, Lamkin, & Suls, 2009; Osimo et al., 2020). Based on these findings, it has been suggested that autonomic dysregulation and inflammation may partially mediate the link between depression and CVD (Musselman, Evans, & Nemeroff, 1998; Nicholson, Kuper, & Hemingway, 2006; Shaffer & Ginsberg, 2017; Sgoifo, Carnevali, de los Angeles Pico Alfonso, & Amore, 2015; Williams & Steptoe, 2007).
Previous studies suggest bidirectional associations of depression with autonomic and immunological alterations (Copeland, Shanahan, Worthman, Angold, & Costello, 2012; Deverts et al., 2010; Huang et al., 2018; 2019; Matthews et al., 2010; Valkanova, Ebmeier, & Allan, 2013). Cognitive behavioral therapy (CBT) is the most-studied form of psychotherapy for MD (Cuijpers et al., 2013; Cuijpers, Cristea, Karyotaki, Reijnders, & Huibers, 2016; David, Cristea, & Hofmann, 2018). By changing dysfunctional thoughts and behaviors, CBT may have the potential to reduce cardiac risk biomarkers via multiple stress-related and behavioral mechanisms. These potential mechanisms include factors which (i) are targeted by CBT and (ii) may interact with autonomic dysregulation and inflammation, such as negative mood, perceived stress and emotional stress reactivity, poor cognitive and behavioral skills to cope with stressors, social withdrawal, as well as inactivity (Allen, Kennedy, Cryan, Dinan, & Clarke, 2014; Audet, McQuaid, Merali, & Anisman, 2014; Eller, Kristiansen, & Hansen, 2011; Gerteis & Schwerdtfeger, 2016; Kemp, Koenig, & Thayer, 2017; Kiecolt-Glaser, Derry, & Fagundes, 2015; Lee & Way, 2019; Plaisance & Grandjean, 2006; Sin, Sloan, McKinley, & Almeida, 2016; Uchino et al., 2018; Yang, Schorpp, & Harris, 2014).
Although considered the gold-standard for the psychological treatment of MD, one important and understudied question is, however, whether CBT reduces cardiac risk biomarkers in populations with MD without CVD. In terms of HRV, two randomized controlled trials (RCT) indicated that short CBT interventions (i.e. 4–6 weeks) combined with HVR biofeedback (Caldwell & Steffen, 2018) or breathing exercises (Chien, Chung, Yeh, & Lee, 2015) may improve specific measures of HRV. Both studies have important limitations, such as a small sample size of younger females (Caldwell & Steffen, 2018), a short treatment duration (Caldwell & Steffen, 2018; Chien et al., 2015), the inclusion of patients with antidepressant medication (Chien et al., 2015), as well as the use of short-term measures of HRV (Caldwell & Steffen, 2018; Chien et al., 2015) instead of long-term HRV recordings which are more stable, less affected by placebo effects and more predictive for cardiovascular events in populations without known CVD (Hillebrand et al., 2013; Task Force of The European Society of Cardiology and The North American & Society of Pacing and Electrophysiology, 1996). In terms of inflammation, one previous RCT suggests that CBT lowers IL-6 and TNF-α in a sample of young adults (Moreira et al., 2015), while two trials did not observe an overall effect of CBT on inflammatory markers (Euteneuer et al., 2017; Taylor et al., 2009).
The present RCT examined whether established CBT for depression is accompanied by reductions in cardiac risk biomarkers in patients with MD without CVD. We aimed to extend previous research in several regards. First, we exploratory studied biological effects of CBT for a wide range of measures with predictive value for CVD, such as heart rate (Greenland et al., 1999; Kannel, Kannel, Paffenbarger, & Cupples, 1987), indices of HRV (Hillebrand et al., 2013), blood pressure (Lewington, Clarke, Qizilbash, Peto, & Rory, 2002), as well as inflammatory markers such as CRP, IL-6 and TNF-α (Avan et al., 2018; Pearson, 2003; Subirana et al., 2018). Second, this RCT only included patients without antidepressant medication. This point is important because antidepressants, in particular tricyclic antidepressants, may reduce HRV (Kemp et al., 2016, 2010; Kemp, Quintana, & Malhi, 2011; Yeh et al., 2016). Third, we used 24-h long-term recordings for cardiac measures instead of short-term recordings. Long-term recordings are more predictive for CVD (Hillebrand et al., 2013) and provide the possibility to analyze geometric indices of HRV such as the triangular index, which has been suggested for prospective research because of the highest reliability among all HRV indices (Ziegler, Piolot, Strassburger, Lambeck, & Dannehl, 1999). In addition, long-term recordings enable the possibility to consider circadian aspects of cardiac measures (Bilan, Witczak, Palusiński, Myśliński, & Hanzlik, 2005; Bonnemeier et al., 2003; Carney et al., 2000; Li et al., 2011; Ohkubo et al., 2002; Parati et al., 2014). Based on a pre-post study suggesting that CBT improved heart rate and daytime HRV in severely depressed patients but not in mildly depressed patients with coronary heart disease (Carney et al., 2000), we examined whether the intensity of depressive symptoms at study entry moderates potential effects on biological outcomes. This trial should be considered exploratory, because a wide range of biological markers were assessed, aiming to identify potential biological responsiveness for future research.
Materials and methods
This RCT was conducted from October 2015 to October 2019 in accordance with the World Medical Association Declaration of Helsinki and the ethical guidelines of the German Society for Psychology (see online Supplementary material for CONSORT 2010 checklist). The approval was given by the Institutional Review Board of the Department of Psychology at the University of Marburg (Approval number: 2014-26k). The study was funded by the German Research Foundation (DFG EU 154/2-1), and study registration took place (www.clinicaltrial.gov NCT 02787148).
Participants
Eighty antidepressant-free patients with MD according to DSM-IV were (1:1) urn randomized to 14 weeks of CBT or a waitlist control condition (see online Supplementary material for recruiting, setting and intervention). A sample of 40 (1:2) age- and sex-matched non-clinical controls from the same community was also involved to verify potential baseline alterations in biological markers in MD.
Depression assessment
Clinical diagnoses according to DSM-IV were verified using the SCID (Wittchen, Wunderlich, Gruschitz, & Zaudig, 1997). To verify the efficacy of the CBT intervention, the primary outcome was self-rated depressive symptom severity assessed with the Beck Depression Inventory (BDI)-II (Beck, Brown, & Steer, 1996; Hautzinger, Kühner, & Keller, 2006). Clinician-rated depressive symptom severity was also assessed using the Montgomery-Asberg Depression Rating Scale (MADRS) (Montgomery & Asberg, 1979; Schmidtke, Fleckenstein, Moises, & Beckmann, 1988). Clinical psychologists conducted clinical interviews and baseline MADRS assessments. MADRS assessment at the end of treatment was conducted by trained, supervised, and blinded research assistants.
Inflammatory markers
Non-fasting blood samples were collected in EDTA-treated tubes (S-Monovette, Sarstedt, Nümbrecht, Germany) between 8:00 AM and 11:00 AM. Before each blood sampling, participants were queried about acute infections during the last 14 days, chronic infections, and illness. Plasma for CRP and cytokine measurements were separated by centrifugation at 2000 × g for 10 min at 4 °C, and plasma was stored at −80 °C until analysis. CRP and cytokines were analyzed using the V-PLEX Human CRP Kit and MSD cytokine assays (Meso Scale Discovery, Rockville, USA) according to the manufacturer's instructions. The sensitivity of the assays was 1.33 pg/ml for CRP, 0.04 pg/ml for TNF-α, and 0.06 pg/ml for IL-6.
Ambulatory cardiovascular monitoring
Twenty-four-hour oscillometric blood pressure and electrocardiogram (ECG) monitoring for heart rate and HRV analyses was conducted during weekdays using a hybrid blood pressure/ECG monitor (card(X)plore, Meditech Ltd., Hungary). Participants were instructed to follow their typical daily activities but refrain from intense physical activity. Monitoring started between 8 AM and 11 AM. Considering circadian variations in heart rate, blood pressure, and HRV (Bilan et al., 2005; Bonnemeier et al., 2003; Li et al., 2011), these measures were calculated for the total 24-h recording and additionally for day- and nighttime. Using a fixed-narrow time interval approach, measures for day- and nighttime were calculated from standardized periods (i.e. daytime: 9 AM to 9 PM; nighttime: 1 AM to 6 AM) in which the retiring and rising periods (which are subject to considerable variation) were eliminated to increase reliability and comparability (Fagard, Brguljan, Thijs, & Staessen, 1996; O'Brien et al., 2013). CardioVisions 1.24 (Meditech Ltd., Hungary) was used to obtain parameters for heart rate, HRV, and blood pressure.
Heart rate was recorded continuously by a 3-channel Holter ECG at a sampling rate of 600 Hz using seven Ag/AgCl electrodes (Kendall H92SG, Cardinal Health Germany 507 GmbH, Germany) placed on the thoracic region. First, similar QRS complexes were automatically grouped and defined as normal or artifact beats. Next, QRS complexes were visually screened for incorrect beat detections and, in case of an incorrect reading, marked as artifact beat. All artifacts were excluded from the data. A minimum of 18 h of analyzable data and less than 5% artifacts of all analyzable beats were required for a recording to be accepted for further analyses (Crawford et al., 1999).
As recommended by common guidelines (Task Force of The European Society of Cardiology and The North American & Society of Pacing and Electrophysiology, 1996), the following time-domain HRV measures were assessed: the HRV triangular index and the standard deviation of all NN intervals (SDNN) for overall HRV, as well as the square root of the mean of the sum of the squares of differences between adjacent NN intervals (RMSSD) for estimating vagally mediated changes reflected in HRV. In terms of frequency-domain HRV, low-frequency (LF)-HRV (0.04–0.15 Hz) and high-frequency (HF)-HRV (0.15–0.4 Hz) were analyzed. HF-HRV reflects vagal modulation of HR. LF-HRV is more complex and may include both sympathetic and parasympathetic influences (Shaffer & Ginsberg, 2017; Task Force of The European Society of Cardiology and The North American & Society of Pacing and Electrophysiology, 1996). To determine LF and HF parameters, the software utilizes a Fast Fourier Transform (FFT) algorithm considering 4-min Hanning-windowed samples.
For ambulatory blood pressure monitoring (ABPM), the device was programmed to obtain blood pressure readings every 15 min during daytime (7 AM to 10 PM) and every 30 min during the night-time (10 PM to 7 AM). The inflatable cuff was placed on the participant's right arm. After the measurement, ABPM readings were manually screened for artifacts. As recommended, only strongly incorrect readings were deleted from recordings (O'Brien et al., 2003). Systolic blood pressure (SBP) values lower than 60 or higher than 260, and diastolic blood pressure (DBP) values lower than 40 and higher than 150 were defined as artificial readings and excluded. Daytime, nighttime and 24-h calculations based on weighted average blood pressure. Nocturnal SBP and DBP dipping was determined by subtracting the nighttime average blood pressure from the daytime average blood pressure. Thus, lower values on these different measures reflect lower nocturnal blood pressure dipping. This procedure yields adequate reliability for dipping values (Dimsdale et al., 2000).
Data analysis
Baseline measures are reported as means with SDs for continuous variables and as numbers with percentages for categorical variables. Data distributions were inspected, and screening for extreme outliers was conducted (i.e. values more than three interquartile ranges above quartile 3). Potential differences in study variables between patients with MD and non-clinical controls were examined using Welch's t tests and χ2 tests. Constrained longitudinal data analysis (cLDA) with linear mixed models (Coffman, Edelman, & Woolson, 2016; Fitzmaurice, Laird, & Ware, 2011; Liang & Zeger, 2000; Liu, Lu, Mogg, Mallick, & Mehrotra, 2009) was applied to examine differences in changes from baseline to the end of treatment between both treatment groups. Constrained linear mixed models incorporated baseline adjustment (i.e. baseline means are constrained to be equal between the randomized groups;) with time (baseline, end of treatment) and time × treatment interactions as fixed factors and with a random intercept at patient level. Longitudinal data were analyzed on an intention-to-treat base using maximum likelihood estimation to account for missing data and dropouts, respectively. To examine moderating effects of depressive symptom severity, time × treatment × baseline severity interactions, as well as corresponding lower-order terms, were added to constrained linear mixed models. Following common suggestions for exploratory research (Althouse, 2016; Bender & Lange, 2001; Rothman, 1990; Rubin, 2017), we report and interpret results without adjusting for multiple testing. All p-values are two-tailed and analyses were carried out with SPSS version 20.0 for Windows (Chicago, SPSS, Inc.) and Mplus7 (Muthén & Muthén, 1998–2012).
Results
Baseline and trial characteristics
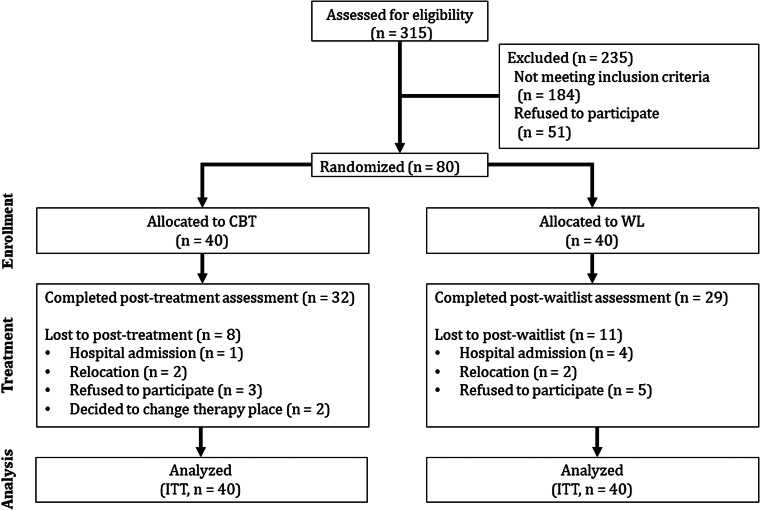
A total of 80 patients with MD and 40 non-clinical controls participated in this study. As illustrated in the study flow (shown in Fig. 1), dropout rates from baseline to the end of treatment were 20% for the CBT group and 27.5% for the WL group. Missing values occurred, and extreme outliers in biological variables were also considered missing values. Extreme outliers were observed for the following variables: CRP (non-clinical controls: 0%, CBT group: 5.6%, WL group: 5.8%), IL-6 (non-clinical controls: 0%, CBT group: 2.8%, WL group: 1.4%), nighttime heart rate (non-clinical controls: 0%, CBT group: 1.4%, WL group: 0%), daytime HF-HRV (non-clinical controls: 0%, CBT group: 1.4%, WL group: 1.4%), daytime LF-HRV (non-clinical controls: 0%, CBT group: 0%, WL group: 1.4%), nighttime HF-HRV (non-clinical controls: 2.5%, CBT group: 0%, WL group: 1.4%), and nighttime SBP (non-clinical controls: 0%, CBT group: 0%, WL group: 1.4%). Among those who completed the study, overall analyzable data were available as follows: BDI-II (non-clinical controls: 100%, CBT group: 100%, WL group: 96%), MADRS (non-clinical controls: 95%, CBT group: 94%, WL group: 94%), CRP (non-clinical controls: 95.0%, CBT group: 87.5%, WL group: 78.3%), IL-6 (non-clinical controls: 95.0%, CBT group: 90.3%, WL group: 82.6%), TNF-α (non-clinical controls: 95.0%, CBT group: 93.1%, WL group: 84.1%), heart rate and HRV measures (non-clinical controls: 92.5–95.0%, CBT group: 80.6–86.1%, WL group: 76.8–81.2%), and blood pressure measures (non-clinical controls: 95.0%, CBT group: 80.6–93.1%, WL group: 76.8–84.1%). Fisher's exact test did not indicate significant differences for any study variable when comparing proportions of outliers (all ps ⩾ 0.489) or total missing data (all ps ⩾ 0.114) between both treatment groups.
Fig. 1.
Flow of participants through each stage of the trial. CBT, cognitive-behavioral therapy; ITT, intention-to-treat; WL, waitlist.
Descriptive statistics for all groups and comparisons between patients with MD and non-clinical controls are presented in Table 1 (see online Supplementary material Table S1 for correlations between biological variables at study entry and Table S2 for correlations between changes in biological variables for each treatment group). Compared to non-clinical controls, patients with MD exhibited significantly higher levels in all inflammatory markers (i.e. CRP, IL-6 and TNF-α). Patients with MD showed significantly higher levels of 24-h and daytime heart rate, relative to non-clinical controls. With respect to HRV, patients had significantly lower levels of 24-h HRV triangular index, daytime HRV triangular index, daytime HF-HRV, daytime LF-HRV and daytime RMSSD, and a trend of reduced daytime SDNN. For blood pressure, higher levels of 24-SBP and daytime DBP, and a trend of higher daytime SBP and 24-h SBP, were observed in patients with MD compared to controls. There were no significant differences between groups for any other biological measures.
Table 1.
Baseline .characteristics of patients with Major Depression and comparison of study variables with a nonclinical age- and sex-matched non-clinical control sample
| Variable | Major depression | Non-clinical controls (n = 40) | Test statistics | ||
|---|---|---|---|---|---|
| CBT group (n = 40) | WL group (n = 40) | Total (n = 80) | |||
| Age | 30.73 (10.02) | 29.90 (10.27) | 30.31 (10.09) | 30.23 (9.63) | t(81.43) = 0.05, p = 0.963 |
| Female, number, n (%) | 26 (65.0) | 22 (55.0) | 48 (60.0) | 24 (60.0) | χ2 (1) = 0.00, p = 1.000 |
| Socioeconomic status1 | 8.89 (3.60) | 8.31 (3.58) | 8.60 (3.57) | 10.00 (3.48) | t(79.57) = –2.01, p = 0.048 |
| Body mass index, kg/m2 | 24.72 (4.36) | 24.90 (4.70) | 24.81 (4.50) | 22.72 (2.03) | t(108.73) = 3.38, p = 0.001 |
| Daily smoker, n (%) | 16 (40.0) | 17 (42.5) | 33 (41.3) | 5 (12.5) | χ2 (1) = 10.19, p = 0.001 |
| Age of depression onset | 21.53 (9.43) | 22.05 (11.10) | 21.78 (10.23) | N/A | N/A |
| Number of depressive episodes | 4.90 (4.58) | 4.05 (3.83) | 4.50 (4.23) | N/A | N/A |
| Chronic depression (⩾2 years), n (%) | 9 (22.5) | 6 (15.0) | 15 (18.8) | N/A | N/A |
| Depressive symptoms severity | |||||
| Self-rated, BDI-II | 28.24 (8.70) | 30.55 (8.07) | 29.40 (8.42) | 2.98 (2.84) | (107.77) = 25.33, p < 0.001 |
| Clinician-rated, MADRS | 28.48 (6.62) | 29.58 (6.49) | 29.04 (6.53) | 3.08 (2.91) | t(114.53) = 29.73, p < 0.001 |
| Immunological markers | |||||
| CRP, μg/ml2 | 0.56 (0.58) | 0.59 (0.59) | 0.57 (0.58) | 0.36 (0.33) | t(102.93) = 2.36, p = 0.020 |
| IL-6, pg/ml | 0.46 (0.27) | 0.58 (0.28) | 0.52 (0.28) | 0.36 (0.20) | t(96.48) = 3.34, p = 0.001 |
| TNF-α, pg/ml | 1.09 (0.32) | 1.04 (0.26) | 1.07 (0.29) | 0.96 (0.16) | t(106.97) = 2.55, p = 0.012 |
| Heart rate | |||||
| 24-h, beats/min | 77.43 (11.11) | 77.55 (7.18) | 77.49 (9.32) | 73.28 (6.58) | t(96.19) = 2.70, p = 0.008 |
| Daytime, beats/min | 84.80 (11.40) | 85.85 (8.63) | 85.33 (10.03) | 79.01 (7.03) | t(96.89) = 3.81, p < 0.001 |
| Nighttime, beats/min | 63.59 (10.95) | 64.18 (6.88) | 63.89 (9.08) | 63.22 (8.43) | t(78.92) = 0.38, p = 0.709 |
| Heart rate variability | |||||
| Triangular index | |||||
| 24-h | 32.38 (8.79) | 31.32 (7.15) | 31.85 (7.97) | 36.08 (9.92) | t(61.63) = −2.23, p = 0.029 |
| Daytime | 25.91 (7.35) | 23.92 (5.74) | 24.89 (6.60) | 28.08 (7.35) | t(66.87) = –2.21, p = 0.030 |
| Nighttime | 20.44 (6.90) | 19.47 (7.08) | 19.96 (6.95) | 22.30 (7.69) | t(67.92) = –1.54, p = 0.128 |
| HF-HRV | |||||
| 24-h, ms2 | 759.68 (547.51) | 851.38 (720.08) | 805.53 (636.53) | 902.59 (766.94) | t(63.27) = –0.66, p = 0.514 |
| Daytime, ms2 | 435.79 (282.00) | 432.20 (360.52) | 433.94 (322.40) | 637.38 (500.05) | t(52.68) = –2.24, p = 0.030 |
| Nighttime, ms2 | 1249.65 (1115.65) | 1288.97 (1107.37) | 1269.01 (1103.30) | 1184.97 (1115.78) | t(73.66) = 0.37, p = 0.713 |
| LF-HRV | |||||
| 24-h, ms2 | 1401.85 (677.78) | 1480.35 (799.32) | 1441.10 (736.56) | 1688.59 (927.21) | t(61.10) = –1.40, p = 0.166 |
| Daytime, ms2 | 1213.91 (569.95) | 1118.97 (492.50) | 1165.75 (530.29) | 1587.03 (868.30) | t(50.77) = –2.69, p = 0.010 |
| Nighttime, ms2 | 1684.59 (966.56) | 1706.41 (1083.42) | 1965.50 (1019.03) | 1821.11 (1152.38) | t(69.11) = –0.56, p = 0.577 |
| RMSSD | |||||
| 24-h, ms | 39.24 (15.08) | 40.50 (17.91) | 39.87 (16.45) | 42.41 (18.60) | t(66.65) = –0.70, p = 0.489 |
| Daytime, ms | 31.21 (12.12) | 30.11 (13.34) | 30.64 (12.68) | 36.05 (13.48) | t(69.58) = –2.02, p = 0.048 |
| Nighttime, ms | 52.94 (26.54) | 54.71 (29.10) | 53.82 (27.65) | 53.30 (29.28) | t(70.50) = 0.09, p = 0.929 |
| SDNN | |||||
| 24-h, ms | 161.00 (40.38) | 155.18 (34.25) | 158.09 (37.27) | 162.54 (40.46) | t(69.02) = –0.55, p = 0.582 |
| Daytime, ms | 121.12 (33.52) | 113.42 (29.90) | 117.16 (31.72) | 129.22 (34.02) | t(69.08) = –1.79, p = 0.079 |
| Nighttime, ms | 114.03 (35.65) | 108.21 (37.42) | 111.12 (36.39) | 124.35 (49.28) | t(57.80) = –1.44, p = 0.157 |
| Blood pressure | |||||
| Systolic blood pressure | |||||
| 24-h, mm Hg | 119.16 (12.56) | 123.72 (11.87) | 121.41 (12.36) | 117.32 (8.50) | t(100.59) = 2.05, p = 0.043 |
| Daytime, mm Hg | 124.71 (11.81) | 128.61 (12.99) | 126.61 (12.47) | 123.05 (9.04) | t(97.44) = 1.73, p = 0.088 |
| Nighttime, mm Hg | 107.64 (13.77) | 112.26 (8.61) | 109.99 (11.59) | 107.95 (11.29) | t(78.71) = 0.88, p = 0.381 |
| Nocturnal dipping, mm Hg | 15.18 (11.53) | 14.56 (10.14) | 14.87 (10.77) | 15.11 (10.16) | t(80.78) = –0.11, p = 0.910 |
| Diastolic blood pressure | |||||
| 24-h, mm Hg | 70.24 (9.37) | 72.00 (8.21) | 71.11 (8.80) | 68.66 (4.81) | t(108.70) = 1.90, p = 0.060 |
| Daytime, mm Hg | 75.24 (8.68) | 77.00 (8.87) | 76.09 (8.76) | 73.13 (6.18) | t(99.22) = 2.07, p = 0.041 |
| Nighttime, mm Hg | 59.00 (10.20) | 61.09 (8.41) | 60.07 (9.31) | 59.74 (6.44) | t(99.18) = 0.22, p = 0.827 |
| Nocturnal dipping, mm Hg | 15.00 (9.37) | 15.26 (7.80) | 15.13 (8.53) | 13.39 (8.10) | t(80.12) = 1.04, p = 0.302 |
BDI-II, Beck Depression Inventory-II; CBT, Cognitive behavioral therapy; CRP, C-reactive protein; HF-HRV, high-frequency heart rate variability; IL-6, interleukin 6; LF-HRV, low-frequency heart rate variability; MADRS, Montgomery–Asberg Depression Rating Scale; RMSSD, square root of the mean of the sum of the squares of differences between adjacent NN intervals; SDNN, a standard deviation of all NN intervals; TNF-α, tumor necrosis factor α; WL, waitlist.
Values are mean (s.d.) unless noted with percentage. Group differences were calculated using χ2 tests for categorical variables and t tests for continuous variables.
Winkler index for measuring individual socioeconomic status by combining information on education, income (monthly household net income), and occupation (ranging from 3 to 21).
Untransformed values are shown for ease of interpretation, although statistical comparisons were conducted on the square root transformed data.
Main treatment effects
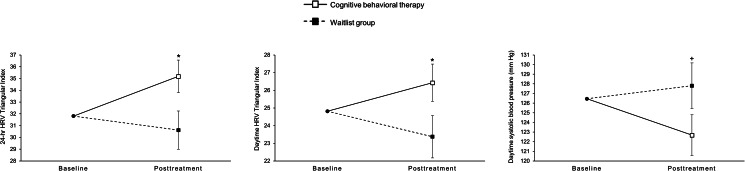
Table 2 reports test statistics for differences in changes from baseline to the end of treatment between both treatment groups. Compared to patients in the WL group, patients who received CBT had stronger reductions in self-rated depressive symptoms (d = 0.52) and in clinician-rated depressive symptoms (d = 0.61). Changes in inflammatory markers and measures of heart rate did not significantly differ between patients in the CBT group and patients in the WL group. In terms of HRV measures which were reduced in depressed patients at baseline, the CBT group showed a significant increase in 24-h HRV triangular index (d = 0.48) and in daytime HRV triangular index (d = 0.43) from baseline to the end of treatment, compared to the WL group (shown in Fig. 2). Although 24-h LF-HRV was not significantly reduced in depressed patients at baseline, there was a trend increase in 24-h LF-HRV (d = 0.35) in the CBT group, compared to the WL group (see online Supplementary material Fig. S1). With respect to blood pressure measures which were increased (or marginally increased) in depressed patients at baseline, the CBT group showed a trend decrease in daytime SBP (d = 0.36), compared to patients in the WL group (shown in Fig. 2). There was no evidence for the main treatment effect in other variables of HRV or blood pressure. Compared to intention-to-treat analyses, analyses per protocol (results not shown) did not provide any substantial changes in the estimates and showed the same pattern of significance for treatment effects with one exception: the treatment effect for 24-h LF-HRV became significant in the per-protocol analysis (Intention-to-treat: p = 0.051; per-protocol: p = 0.0499).
Table 2.
Associations between treatment groups and outcome measures over time. Results from constrained linear mixed models (Intention-to-treat analyses)
| Outcomes | Baselinea | Change from baseline to the end of treatment | Treatment effect | ||||
|---|---|---|---|---|---|---|---|
| Estimated mean (95% CI) | CBT group (n = 40) | WL group (n = 40) | Estimated differences in change (95% CI) | p value | |||
| Estimated Change (95% CI) | p value | Estimated Change (95% CI) | p value | ||||
| Depression severity | |||||||
| Self-rated, BDI-II | 29.22 (27.37–31.08) | ‒9.19 (‒12.27 to ‒6.12) | <0.001 | ‒3.38 (‒0.02 to 6.79) | 0.051 | ‒5.81 (‒10.36 to ‒1.26) | 0.013 |
| Clinician-rated, MADRS | 29.04 (27.59–30.49) | ‒12.38 (‒16.04 to ‒8.71) | <0.001 | ‒‒5.16 (‒9.08 to ‒1.21) | 0.011 | ‒7.22 (‒12.47 to ‒1.97) | 0.008 |
| Immunological markers | |||||||
| SQRT CRP, μg/ml | 0.67 (0.59–0.76) | ‒0.02 (‒0.13 to 0.09) | 0.722 | ‒0.05 (‒0.17 to 0.07) | 0.365 | 0.04 (‒0.12 to 0.19) | 0.642 |
| IL-6, pg/ml | 0.52 (0.45–0.59) | 0.11 (‒0.02 to 0.23) | 0.084 | 004 (‒0.09 to 0.17) | 0.561 | 0.07 (‒0.12 to 0.24) | 0.427 |
| TNF-α, pg/ml | 1.07 (1.00–1.13) | 0.01 (‒0.08 to 0.08) | 0.907 | ‒0.07 (‒0.16 to 0.02) | 0.112 | 0.08 (‒0.04 to 0.19) | 0.193 |
| Heart rate | |||||||
| 24-h, beats/min | 77.78 (75.57–79.98) | ‒3.31 (‒5.94 to ‒0.68) | 0.015 | ‒0.83 (‒3.89 to 2.23) | 0.589 | ‒2.49 (‒6.34 to 1.37) | 0.200 |
| Daytime, beats/min | 85.67 (83.33–88.02) | ‒3.24 (‒6.18 to ‒0.30) | 0.032 | ‒2.12 (‒5.48 to 1.25) | 0.213 | ‒1.12 (‒5.47 to 3.23) | 0.606 |
| Nighttime, beats/min | 64.31 (62.1–69.83) | 0.10 (‒3.15 to 3.34) | 0.953 | 1.46 (‒2.38 to 5.30) | 0.447 | ‒1.37 (‒6.31 to 3.58) | 0.580 |
| Heart rate variability | |||||||
| Triangular index | |||||||
| 24-h | 31.81 (29.91–33.72) | 3.37 (0.46–6.28) | 0.024 | ‒1.19 (‒4.58 to 2.20) | 0.483 | 4.56 (0.40–8.72) | 0.033b |
| Daytime | 24.81 (23.26–26.36) | 1.62 (‒0.54 to 3.77) | 0.139 | ‒1.44 (‒3.87 to 0.99) | 0.239 | 3.06 (0.02–6.10) | 0.049b |
| Nighttime | 20.03 (18.38–21.68) | 1.85 (‒0.66 to 4.35) | 0.145 | ‒1.03 (‒3.96 to 1.90) | 0.484 | 2.88 (‒0.80 to 6.55) | 0.122 |
| HF-HRV | |||||||
| 24-h, ms2 | 812.00 (662.62–961.38) | 58.96 (‒76.63 to 194.54) | 0.386 | ‒64.80 (‒224.28 to 94.69) | 0.418 | 123.75 (‒79.37 to 326.88) | 0.226 |
| Daytime, ms2 | 452.77 (372.78–532.76) | 141.84 (41.43–242.26) | 0.007 | 58.46 (‒56.03 to 172.96) | 0.308 | 83.381 (‒67.60 to 234.37) | 0.271 |
| Nighttime, ms2 | 1300.74 (1033.52–1567.96) | ‒73.97 (‒385.64 to 237.70) | 0.635 | ‒122.02 (‒487.08 to 243.04) | 0.504 | 48.05 (‒411.16 to 507.26) | 0.834 |
| LF-HRV | |||||||
| 24-h, ms2 | 1463.10 (1284.57–1641.63) | 107.87 (‒55.90 to 271.64) | 0.191 | ‒137.85 (‒330.92 to 55.22) | 0.157 | 245.72 (‒1.42 to 492.86) | 0.051 |
| Daytime, ms2 | 1200.61 (964.14–1337.09) | 120.77 (‒12.95 to 254.49) | 0.075 | 28.21 (‒126.15 to 182.56) | 0.731 | 92.57 (‒110.33 to 295.46) | 0.361 |
| Nighttime, ms2 | 1726.37 (1481.83–1970.90) | 183.54 (‒205.97 to 503.04) | 0.348 | ‒63.162 (‒523.32 to 397.00) | 0.783 | 246.70 (‒343.44 to 836.84) | 0.404 |
| RMSSD | |||||||
| 24-h, ms | 40.17 (36.28–44.07) | 2.22 (‒1.45 to 5.89) | 0.229 | ‒0.05 (‒4.38 to 4.29) | 0.982 | 2.27 (‒3.32 to 7.85) | 0.417 |
| Daytime, ms | 30.59 (27.63–33.55) | 3.38 (0.30–6.46) | 0.032 | 1.76 (‒1.71 to 5.22) | 0.313 | 1.63 (‒2.84 to 6.09) | 0.467 |
| Nighttime, ms | 54.75 (48.10–61.41) | ‒0.68 (‒7.91 to 6.55) | 0.851 | ‒1.52 (‒9.98 to 6.94) | 0.719 | 0.84 (‒9.77 to 11.46) | 0.873 |
| SDNN | |||||||
| 24-h, ms | 158.60 (149.72–167.49) | ‒0.11 (‒10.12 to 9.91) | 0.983 | ‒6.86 (‒18.62 to 4.90) | 0.246 | 6.75 (‒8.14 to 21.64) | 0.365 |
| Daytime, ms | 116.72 (109.27–124.16) | 6.51 (‒4.55 to 17.57) | 0.243 | ‒3.97 (‒16.47 to 8.53) | 0.527 | 10.48 (‒5.31 to 26.27) | 0.188 |
| Nighttime, ms | 111.92 (103.36–120.49) | 8.27 (‒4.84 to 21.43) | 0.210 | ‒0.17 (‒15.71 to 15.38) | 0.983 | 8.46 (‒11.58 to 28.51) | 0.400 |
| Blood pressure | |||||||
| Systolic blood pressure | |||||||
| 24-h, mm Hg | 121.04 (118.17–123.91) | ‒2.00 (‒5.13 to 1.12) | 0.204 | 0.92 (‒2.66 to 4.50) | 0.608 | ‒2.92 (‒7.59 to 1.74) | 0.213 |
| Daytime, mm Hg | 126.46 (123.59–129.32) | ‒3.78 (‒7.67 to 0.12) | 0.057 | 1.35 (‒3.14 to 5.84) | 0.549 | ‒5.13 (‒10.92 to 0.66) | 0.081 |
| Nighttime, mm Hg | 109.83 (107.04–112.62) | ‒0.87 (‒4.76 to 3.02) | 0.655 | 2.68 (‒1.82 to 7.17) | 0.237 | ‒3.55 (‒9.31 to 2.22) | 0.222 |
| Nocturnal dippingc, mm Hg | 14.79 (12.20–17.38) | ‒0.76 (‒4.90 to 3.38) | 0.594 | 1.16 (‒3.50 to 5.83) | 0.620 | ‒1.92 (‒7.61 to 3.76) | 0.500 |
| Diastolic blood pressure | |||||||
| 24-h, mm Hg | 70.91 (68.87–72.94) | ‒1.58 (‒3.96 to 0.79) | 0.187 | 0.02 (‒2.67 to 2.71) | 0.986 | ‒1.61 (‒5.00 to 1.79) | 0.347 |
| Daytime, mm Hg | 76.10 (74.08–78.11) | ‒2.89 (‒5.75 to ‒0.03) | 0.048 | 0.18 (‒3.12 to 3.48) | 0.914 | ‒3.07 (‒7.21 to 1.08) | 0.143 |
| Nighttime, mm Hg | 59.95 (57.72–62.18) | 0.27 (‒2.83 to 3.36) | 0.864 | 0.87 (‒2.59 to 4.33) | 0.617 | ‒0.61 (‒4.80 to 3.59) | 0.773 |
| Nocturnal dippingc, mm Hg | 15.20 (13.04–17.15) | ‒2.88 (‒6.29 to 0.53) | 0.097 | 0.97 (‒2.91 to 4.85) | 0.618 | ‒3.85 (‒8.66 to 0.96) | 0.114 |
BDI-II, Beck Depression Inventory-II; CBT, Cognitive behavioral therapy; CRP, C-reactive protein; HF-HRV, high-frequency heart rate variability; IL-6, interleukin 6; LF-HRV, low-frequency heart rate variability; MADRS, Montgomery–Asberg Depression Rating Scale; RMSSD, square root of the mean of the sum of the squares of differences between adjacent NN intervals; SDNN, standard deviation of all NN intervals; SQRT, square root transformed; TNF-α, tumor necrosis factor α; WL, waitlist.
Baseline-adjusted results; all patients are contained in one group at baseline.
A finding is not observed after adjustment with a false discovery rate of 10% (see methods section for details on false discovery adjustment).
Models include corresponding 24-h blood pressure as a time-varying covariate.
Fig. 2.
Treatment group differences in changes for cardiac measures from baseline to the end of treatment.
Note. Values are estimated marginal means (standard errors) from constrained linear mixed models (see Table 2 for test statistics). HRV, heart rate variability. +p < 0.10 *p < 0.05.
Moderated treatment effects
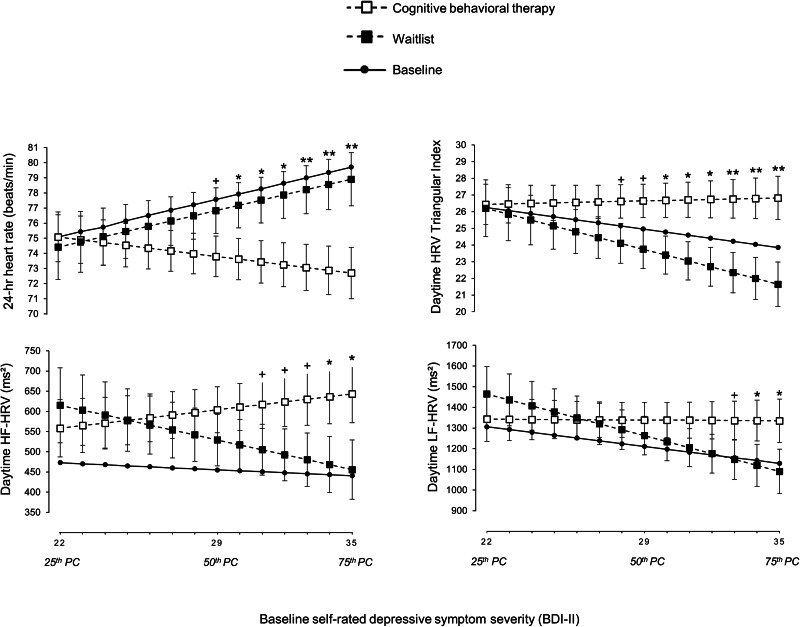
Table 3 shows results for moderation analyses with baseline self-rated (i.e. BDI-II) and clinician-rated (i.e. MADRS) depressive symptom severity as a predictor for changes in biological measures from baseline to the end of treatment. In cases where there were any significant or trend moderating effects (p < 0.10), differences between changes were plotted from lower (25th percentile) to higher (75th percentile) levels of the moderator to explore the nature of the moderation. Figure 3 plots moderating effects for biological measures which were altered in patients with MD at baseline (see online Supplementary material Fig. S2 for all other moderating effects).
Table 3.
Depressive symptom severity as moderator for associations between treatment groups and outcome measures over time. Results from constrained linear mixed models (Intention-to-treat analyses)
| Moderator | ||||
|---|---|---|---|---|
| Outcomes | Self-rated, BDI-II | Clinician rated, MADRS | ||
| Estimate (95% CI) | p value | Estimate (95% CI) | p value | |
| Immunological markers | ||||
| SQRT CRP, μg/ml | 0.01 (‒0.004 to 0.03) | 0.124 | 0.02 (‒0.07 to 0.04) | 0.175 |
| IL-6, pg/ml | ‒0.02 (‒0.04 to 0.01) | 0.147 | 0.01 (‒0.02 to 0.03) | 0.645 |
| TNF-α, pg/ml | ‒0.002 (‒0.02 to 0.01) | 0.782 | ‒0.001 (‒0.02 to 0.02) | 0.900 |
| Heart rate | ||||
| 24-h, beats/min | ‒0.53 (‒0.95 to ‒0.11) | 0.014a | ‒0.05 (‒0.60, to 0.51) | 0.862 |
| Daytime, beats/min | ‒0.41 (‒0.94 to 0.11) | 0.120 | 0.36 (‒0.28 to 1.00) | 0.261 |
| Nighttime, beats/min | ‒0.52 (‒1.10 to 0.07) | 0.081 | ‒0.03 (‒0.77 to 0.71) | 0.927 |
| Heart rate variability | ||||
| Triangular index | ||||
| 24-h | 0.49 (‒0.001 to 0.98) | 0.050 | ‒0.27 (‒0.89 to 0.35) | 0.389 |
| Daytime | 0.38 (0.01–0.75) | 0.043a | ‒0.34 (‒0.79 to 0.10) | 0.126 |
| Nighttime | 0.26 (‒0.20 to 0.71) | 0.260 | ‒0.15 (‒0.70 to 0.39) | 0.576 |
| HF-HRV | ||||
| 24-h, ms2 | 19.85 (‒3.00 to 41.99) | 0.078 | 10.70 (‒12.65 to 34.06) | 0.360 |
| Daytime, ms2 | 18.79 (0.66–36.93) | 0.043a | 3.02 (‒17.93 to 23.97) | 0.772 |
| Nighttime, ms2 | 35.65 (‒16.27 to 87.57) | 0.173 | 8.82 (‒50.91 to 68.54) | 0.767 |
| LF-HRV | ||||
| 24-h, ms2 | 17.24 (‒10.41 to 44.89) | 0.215 | 5.74 (‒26.94 to 38.42) | 0.724 |
| Daytime, ms2 | 28.24 (4.20–52.27) | 0.023a | 13.78 (‒12.75 to 40.31) | 0.299 |
| Nighttime, ms2 | 45.39 (‒22.03 to 112.81) | 0.181 | 5.82 (‒79.57 to 91.21) | 0.891 |
| RMSSD | ||||
| 24-h, ms | 0.52 (‒0.03 to 1.08) | 0.065 | 0.41 (‒0.28 to 1.10) | 0.235 |
| Daytime, ms | 0.46 (‒0.07 to 0.99) | 0.086 | ‒0.04 (‒0.67 to 0.59) | 0.908 |
| Nighttime, ms | 0.87 (‒0.28 to 2.02) | 0.136 | 0.51 (‒0.96 to 1.98) | 0.485 |
| SDNN | ||||
| 24-h, ms | 1.98 (0.23–3.67) | 0.023a | ‒0.23 (‒2.46 to 2.01) | 0.840 |
| Daytime, ms | 1.81 (‒0.11 to 3.73) | 0.065 | ‒1.96 (‒4.31 to 0.39) | 0.100 |
| Nighttime, ms | 3.00 (0.69–5.31) | 0.012a | 0.16 (‒2.88 to 3.21) | 0.916 |
| Blood pressure | ||||
| Systolic blood pressure | ||||
| 24-h, mm Hg | ‒0.14 (‒0.74 to 0.47) | 0.646 | ‒0.08 (‒0.83 to 0.66) | 0.822 |
| Daytime, mm Hg | ‒0.11 (‒0.87 to 0.65) | 0.771 | ‒0.30 (‒1.23 to 0.62) | 0.513 |
| Nighttime, mm Hg | 0.004 (‒0.68 to 0.69) | 0.991 | 0.03 (‒0.86 to 0.92) | 0.949 |
| Nocturnal dippingb, mm Hg | ‒0.23 (‒0.89 to 0.44) | 0.496 | ‒0.44 (‒1.29 to 0.41) | 0.303 |
| Diastolic blood pressure | ||||
| 24-h, mm Hg | ‒0.13 (‒0.57 to 0.31) | 0.555 | ‒0.01 (‒0.55 to 0.54) | 0.978 |
| Daytime, mm Hg | ‒0.04 (‒0.58 to 0.50) | 0.880 | ‒0.06 (‒0.72 to 0.60) | 0.866 |
| Nighttime, mm Hg | ‒0.07 (‒0.59 to 0.45) | 0.787 | 0.28 (‒0.36 to 0.92) | 0.381 |
| Nocturnal dippingb, mm Hg | 0.04 (‒0.53 to 0.62) | 0.882 | ‒0.36 (‒1.06 to 0.35) | 0.315 |
BDI-II, Beck Depression Inventory-II; CBT, Cognitive behavioral therapy; CRP, C-reactive protein; HF-HRV, high-frequency heart rate variability; IL-6, interleukin 6; LF-HRV, low-frequency heart rate variability; MADRS, Montgomery–Asberg Depression Rating Scale; RMSSD, square root of the mean of the sum of the squares of differences between adjacent NN intervals; SDNN, a standard deviation of all NN intervals; SQRT, square root transformed; TNF-α, tumor necrosis factor α; WL, waitlist.
A finding is observed after adjustment with a false discovery rate of 10% (see methods section for details on false discovery adjustment).
Models include corresponding 24-h blood pressure as a time-varying covariate.
Fig. 3.
Baseline self-rated depressive symptom severity (i.e. BDI-II) as moderator of differences in changes in cardiac measures from baseline to the end of treatment.
Note. Estimated marginal means (standard errors) from constrained linear mixed models are plotted from lower (25th percentile) to higher (75th percentile) levels of the moderator (see Table 3 for test statistics). HRV, heart rate variability; HF-HRV, high-frequency heart rate variability; LF-HRV, low-frequency heart rate variability. +p < 0.10 *p < 0.05 **p < 0.01.
Self-rated (but not clinician-rated) baseline depressive symptom severity significantly moderated differences between changes in 24-h heart rate. In patients with more severe depressive symptoms at study entry, there was a stronger decrease in 24-h heart rate from baseline to the end of treatment in the CBT group, compared to the WL group (see Fig. 3). A significant treatment effect on 24-h heart rate in favor of CBT over WL emerged with a baseline severity score of BDI-II = 30 (d = 0.39). At the 75th percentile (BDI = 35), the effect on 24-h heart rate was moderate (d = 0.57). Although not altered at study entry, there was also a trend for this moderating effect in terms of changes in nighttime heart rate (see online Supplementary material Fig. S2).
In terms of HRV measures which were impaired (or marginally impaired) in depressed patients at baseline, higher self-rated depressive symptom severity at baseline was associated with significant improvements in daytime HRV triangular index, daytime HF-HRV, and daytime LF-HRV from baseline to the end of treatment in the CBT compared to the WL group (see Fig. 3). A significant treatment effect in favor of CBT over WL emerged with a baseline severity score of BDI-II = 30 for daytime HRV triangular index (d = 0.48) and of BDI-II = 34 for daytime HF-HRV (d = 0.39) and daytime LF-HRV (d = 0.34). At the 75th percentile (BDI = 35), treatment effects were estimated to be moderate for daytime HRV triangular index (d = 0.62) and small for daytime HF-HRV (d = 0.41) and daytime LF-HRV (d = 0.37). There was also a trend for this moderating effect in 24-h HRV triangular index, daytime RMSSD and daytime SDNN (see online Supplementary material Fig. S2). Although not altered in depressed patients at baseline, similar moderating effects were observed for 24-h SDNN and nighttime SDNN. A significant treatment effect in favor of CBT over WL emerged with a baseline severity score of BDI-II = 34 for 24-h SDNN (d = 0.40) and nighttime SDNN (d = 0.43). At the 75th percentile (BDI = 35), treatment effects were estimated to be small for 24-h SDNN (d = 0.43) and nighttime SDNN (d = 0.46) (see online Supplementary material Fig. S2). Depressive symptom severity did not moderate the impact of treatment on inflammatory markers. Compared to intention-to-treat analyses, analyses per protocol (results not shown) did not provide any substantial changes in the estimates and showed the same pattern of significance for moderated treatment effects with one exception: the moderated treatment effect (i.e. self-rated depressive symptom severity) for 24-h HRV triangular index became significant in the per-protocol analysis (Intention-to-treat: p = 0.050; per-protocol: p = 0.049).
Correlations between changes in depressive symptom severity and biological outcomes
In cases where cLDA resulted in any significant or trend effects (p < 0.10), we performed post-hoc intention-to-treat correlational analyses with maximum likelihood estimation to examine whether a reduction in depressive symptom severity correlated with corresponding improvements in biological outcomes in the CBT group. A decline in self-rated depressive symptom severity from baseline to the end of CBT significantly correlated with a decrease in 24-h heart rate (r = 0.35; p = 0.010) and tended to correlate with a decrease in nighttime heart rate (r = 0.25; p = 0.076). In addition, decrease in self-rated depressive symptom severity significantly correlated with improvement in 24-h HF-HRV (r = −0.43; p < 0.001), daytime HF-HRV (r = −0.35; p = 0.004), 24-h RMSSD (r = −0.49; p < 0.001) and daytime RMSSD (r = −0.41; p = 0.001) but not with changes in measures of SDNN, LF-HRV and HRV triangular index, as well as daytime SBP (all ps ⩾ 0.1). Correlations between changes in clinician-rated depressive symptom severity and changes in cardiac measures were non-significant (all ps ⩾ 0.1).
A posterori multiplicity adjustments
As outlined in the methods section, all results are not adjusted for multiple testing and should be considered exploratory (Althouse, 2016; Bender & Lange, 2001; Rothman, 1990; Rubin, 2017). However, because there may not always be consensus on the need for multiplicity adjustment in exploratory studies, we decided to provide separate post-hoc multiplicity adjustments with a false discovery rate (FDR) of 10% in cases where at least one significant treatment effect was observed within a reasonable family of potentially interrelated HR and HRV outcomes. More specifically, we separately adjusted within the domain of 24-h HR and HRV measures, within the domain of daytime HR and HRV measures, as well as within the domain of nighttime HR and HRV measures via the less-conservative two-stage step-up method of Benjamini, Krieger, and Yekutieli (2006) using Prism 9 (GraphPad) for Windows. As shown in Table 2, the main treatments effects on 24-h and daytime HRV triangular index could not be observed after FDR adjustments. As seen in Table 3, all originally significant moderated treatment effects would also be prominent after FDR correction. Importantly, multiplicity adjustments were conducted a posteriori and thus the sample size in this study may not account for these adjustments.
Discussion
This exploratory RCT examined whether CBT is accompanied by reductions in cardiac risk biomarkers in antidepressant-free patients with MD. Biological outcomes included a wide range of measures with potential predictive value for CVD such as heart rate (Kannel et al., 1987), indices of HRV (Hillebrand et al., 2013), blood pressure (Lewington et al., 2002), as well as inflammatory markers (i.e. CRP, IL-6, and TNF-α) (Avan et al., 2018; Pearson, 2003; Subirana et al., 2018). Compared to WL, CBT was associated with a significant increase in 24-h and daytime HRV triangular index and a borderline significant increase in 24-h LF-HRV, as well as a trend decrease in daytime SBP. Self-rated depressive symptom severity at study entry moderated (or tended to moderate) improvements through CBT for 24-h and daytime heart rate, and for several indices of HRV, particularly those daytime measures which were altered in depressed patients at study entry. With increasing symptom severity, CBT increased or tended to increase these indices of HRV and reduced heart rate, compared to the control condition. Inflammatory effects were not observed in this trial.
At study entry, the 24-h and daytime HRV triangular index, a robust geometric measure of overall HRV (Stapelberg, Neumann, Shum, McConnell, & Hamilton-Craig, 2018; Vila, Lado, & Cuesta-Morales, 2019; Ziegler et al., 1999), was reduced in patients with MD. Compared to the control condition, CBT increased the 24-h and daytime HRV triangular index. Several studies suggest that overall HRV predict cardiovascular health outcomes in populations without known CVD at study entry, as well as in clinical populations (Fang, Wu, & Tsai, 2020a, 2020b; Hämmerle et al., 2020; Hillebrand et al., 2013). Although our finding needs confirmatory replication, an improvement of overall HRV during CBT may suggest that this common form of psychotherapy does not only improve depressive symptom severity but also cardiovascular health. Given the increased incidence of CVD in patients with MD, it is of clinical relevance whether common treatments affect cardiovascular health (Gan et al., 2014; Harshfield et al., 2020; Li et al., 2019; Wu & Kling, 2016). Our finding may thus inspire future research to include the HRV triangular index when evaluating biological effects of psychotherapy in MD, and also to examine whether potential improvements in overall HRV during treatment translate into reduced risk for CVD.
Although CBT numerically increased all other indices of HRV, differences in changes between CBT and WL were not significant. One explanation for this finding might be, that the triangular index is more reliable than non-geometric measures of HRV in terms of high intraindividual reproducibility and thus more appropriate for prospective research (Stapelberg et al., 2018; Vila et al., 2019; Ziegler et al., 1999). The major disadvantage of the triangular index is that time-consuming long-term recordings should be used to ensure valid calculation (Heart Rate Variability: Standards of Measurement, Physiological Interpretation and Clinical Use. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology, 1996). However, because of its robustness and responsiveness in this trial, the triangular index might be a good measure to evaluate changes in overall HRV through psychological treatment.
The observation that self-rated depressive symptom severity, assessed by the BDI, moderated treatment effects on heart rate and daytime HRV is in line with findings from an earlier pre-post study in depressed patients with coronary heart disease (Carney et al., 2000). In this previous work, patients were classified according to their BDI score as mildly depressed or moderately to severely depressed. The main result was that heart rate and daytime RMSSD improved significantly in the moderately to severely depressed patients but remained unchanged in the mildly depressed patients (Carney et al., 2000). This earlier study together with our present RCT suggests that potential changes in heart rate and especially in daytime measures of HRV are primarily observable in patients with more severe depressive symptoms. Patients with more severe depressive symptoms thus seem to improve their cardiovascular risk profile the most. This finding is of particular interest since also the risk for CVD increases with increasing self-rated depressive symptom severity (Harshfield et al., 2020) and an improvement of HRV during treatment might thus be of stronger prognostic relevance in more severe depression. Higher depression scores have greater potential for change than lower scores. If the degree of change in depressive symptoms relates to changes in heart rate and HRV, one would expect that a reduction in depressive symptom severity relates to improvements in heart rate and HRV during treatment. Indeed, the present study found that a reduction in self-rated depressive symptom severity through CBT significantly correlated with improvements in HF-HRV, RMSSD and heart rate. Importantly, clinician-rated depressive symptoms, as assessed by the MADRS, did neither moderate biological treatment effects nor correlate with changes in a cardiac measure in CBT. One explanation for these diverging findings may be that the BDI, in contrast to the MADRS, has been conceptualized to reflect outcomes of psychotherapy (Demyttenaere & De Fruyt, 2003) and may thus stronger relate to the biological effects of CBT. Moreover, expert ratings are prone to over-estimate clinical improvements (Cuijpers, Li, Hofmann, & Andersson, 2010; Rief et al., 2009). For future psychotherapeutic trials, we suggest considering moderating effects of patients’ self-rated symptom severity when studying changes in heart rate and HRV.
In the present study, patients exhibited increased levels of inflammatory levels at study entry. There was no evidence for reductions in these markers through CBT. A previous RCT with partially medicated patients with depression and elevated cardiovascular risk did also not observe an effect of CBT on CRP (Taylor et al., 2009). Another RCT with partially medicated patients found that CBT reduced CRP (but not IL-6) only in patients with increased baseline CRP levels, and only in combination with physical exercise (Euteneuer et al., 2017). On the other hand, reductions in IL-6 and TNF-α during CBT (but not during Narrative Cognitive Therapy) have been observed in a study with young patients with MD (18 to 29 years old), but this RCT did only analyze within-group changes and provided no intention-to-treat analyses for differences in changes between both treatment groups (Moreira et al., 2015). Based on all these findings, there may be little or no evidence for inflammatory effects of standard CBT in the context of depression, although some findings in other populations suggest that CBT may improve inflammation, for example, in insomnia (Irwin et al., 2015) or fibromyalgia (Zabihiyeganeh et al., 2019). Even if inflammation may neither be necessary nor sufficient to induce or sustain depression in general (Kiecolt-Glaser et al., 2015), a potential insufficiency of CBT to improve low-grade inflammation strengthens the importance of research efforts to develop more specific anti-inflammatory treatments for subgroups of patients (Jones et al., 2020).
Although findings for associations between depression and blood pressure alterations are mixed (Gould & Beaudreau, 2013; Hildrum et al., 2007; Rogeness, Cepeda, Macedo, Fisher, & Harris, 1990), depression has been shown to predict the development of hypertension (Ginty et al., 2013; Meng et al., 2012). In addition, research using long-term assessment of blood pressure (i.e. 7 days) suggests increased SBP and DBP, as well as reduced nocturnal blood pressure dipping in depressed individuals (Shinagawa et al., 2002). Compared to non-clinical controls, patients in the present study showed significantly increased 24-h SBP and daytime DBP, as well as marginally higher daytime SBP and 24-h DBP. Although these alterations numerically improved in the CBT group compared to the WL group, there was only a trend effect for daytime SBP. To the best of our knowledge, there are no previous RCTs that evaluate CBT effects on ambulatory blood pressure in patients with MD. So, this finding is of potential interest but needs further investigation.
Notwithstanding the strengths of the present study, such as the inclusion of a non-clinical control group, the randomized controlled design, the comprehensive assessment of potential cardiac risk biomarkers, the inclusion of patients without antidepressant medication, and the use of 24-h long-term recordings for cardiac measures instead of short-term recordings, limitations need to be reflected. First, given the exploratory nature of this trial, further research is necessary to confirm the observed findings. In particular, treatment effects for the HRV triangular index may have occurred by chance. Second, our sample consists of outpatients with MD who were eligible for psychological treatment. Thus, findings may not generalize to other samples of depressed patients (e.g. MD patients with psychotic features). Third, we did not assess patients` experience with CBT, a factor which might of relevance for treatment responsiveness. Fourth, although studies on depression and dysregulation of the hypothalamic–pituitary–adrenal (HPA) stress axis are less consistent (Dedovic & Ngiam, 2015; Psarraki et al., 2021; Stetler & Miller, 2011), there is meanwhile evidence for a prospective association between higher levels of morning plasma cortisol and incident CVD (Crawford et al., 2019). It might thus have been useful to include HPA-axis biomarkers in this study. Moreover, this RCT was not designed to examine specific mechanisms (as described in the introduction section) and the relative contribution of specific components of CBT to potential biological effects, which may be of interest for future dismantling studies. Finally, despite longitudinal evidence linking heart rate and HRV to cardiovascular risk, the clinical implications of the present study are not clear. The most important question is whether improving biological cardiac risk factors in patients with MD will translate into reduced risk for CVD. Given the lack of studies which focus on such long-term effects of psychological treatment, it is not possible to answer this question.
To conclude, this study found that CBT for MD is accompanied by an increase in overall HRV, as indexed by the triangular index. If this exploratory result is replicated in confirmatory studies, this could imply that the cardiovascular risk profile is reduced after successful CBT. Moreover, self-rated depressive symptom severity was identified as a potential moderator for improvements in several indices of heart rate and HRV. The findings provide new insights into biological effects of psychological treatment against depression.
Acknowledgements
We woud like to thank Dr Firouzeh Farahmand for conducting the biochemical analyses for this study.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S0033291722000447.
click here to view supplementary material
Financial support
This study was funded by the German Research Foundation DFG EU 154/2-1 with a grant for Dr Euteneuer.
Conflicts of interest
The authors declare no specific conflict of interest that could have influenced treatment results or the content of this paper.
References
- Allen, A. P., Kennedy, P. J., Cryan, J. F., Dinan, T. G., & Clarke, G. (2014). Biological and psychological markers of stress in humans: Focus on the trier social stress test. Neuroscience and Biobehavioral Reviews, 38, 94–124. doi: 10.1016/j.neubiorev.2013.11.005 [DOI] [PubMed] [Google Scholar]
- Althouse, A. D. (2016). Adjust for multiple comparisons? It's not that simple. The Annals of Thoracic Surgery, 101, 1644–1645. doi: 10.1016/j.athoracsur.2015.11.024 [DOI] [PubMed] [Google Scholar]
- Audet, M.-C., McQuaid, R. J., Merali, Z., & Anisman, H. (2014). Cytokine variations and mood disorders: Influence of social stressors and social support. Frontiers in Neuroscience, 8, 416. doi: 10.3389/fnins.2014.00416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Avan, A., Tavakoly Sany, S. B., Ghayour-Mobarhan, M., Rahimi, H. R., Tajfard, M., & Ferns, G. (2018). Serum C-reactive protein in the prediction of cardiovascular diseases: Overview of the latest clinical studies and public health practice. Journal of Cellular Physiology, 233, 8508–8525. doi: 10.1002/jcp.26791 [DOI] [PubMed] [Google Scholar]
- Beck, A. T., Brown, G., & Steer, R. A. (1996). Beck depression inventory II manual. The Psychological Corporation: San Antonio, TX. [Google Scholar]
- Bender, R., & Lange, S. (2001). Adjusting for multiple testing--when and how? Journal of Clinical Epidemiology, 54, 343–349. doi: 10.1016/s0895-4356(00)00314-0 [DOI] [PubMed] [Google Scholar]
- Benjamini, Y., Krieger, A. M., & Yekutieli, D. (2006). Adaptive linear step-up procedures that control the false discovery rate. Biometrika, 93, 491–507. doi: 10.1093/biomet/93.3.491 [DOI] [Google Scholar]
- Bilan, A., Witczak, A., Palusiński, R., Myśliński, W., & Hanzlik, J. (2005). Circadian rhythm of spectral indices of heart rate variability in healthy subjects. Journal of Electrocardiology, 38, 239–243. doi: 10.1016/j.jelectrocard.2005.01.012 [DOI] [PubMed] [Google Scholar]
- Bonnemeier, H., Wiegand, U. K. H., Brandes, A., Kluge, N., Katus, H. A., Richardt, G., & Potratz, J. (2003). Circadian profile of cardiac autonomic nervous modulation in healthy subjects: Differing effects of aging and gender on heart rate variability. Journal of Cardiovascular Electrophysiology, 14, 791–799. doi: 10.1046/j.1540-8167.2003.03078.x [DOI] [PubMed] [Google Scholar]
- Caldwell, Y. T., & Steffen, P. R. (2018). Adding HRV biofeedback to psychotherapy increases heart rate variability and improves the treatment of major depressive disorder. International Journal of Psychophysiology, 131, 96–101. doi: 10.1016/j.ijpsycho.2018.01.001 [DOI] [PubMed] [Google Scholar]
- Carney, R. M., & Freedland, K. E. (2017). Depression and coronary heart disease. Nature Reviews Cardiology, 14, 145–155. doi: 10.1038/nrcardio.2016.181 [DOI] [PubMed] [Google Scholar]
- Carney, R. M., Freedland, K. E., Stein, P. K., Skala, J. A., Hoffman, P., & Jaffe, A. S. (2000). Change in heart rate and heart rate variability during treatment for depression in patients with coronary heart disease. Psychosomatic Medicine, 62, 639–647. doi: 10.1097/00006842-200009000-00007 [DOI] [PubMed] [Google Scholar]
- Chien, H. C., Chung, Y. C., Yeh, M. L., & Lee, J. F. (2015). Breathing exercise combined with cognitive behavioural intervention improves sleep quality and heart rate variability in major depression. Journal of Clinical Nursing, 24, 3206–3214. doi: 10.1111/jocn.12972 [DOI] [PubMed] [Google Scholar]
- Coffman, C. J., Edelman, D., & Woolson, R. F. (2016). To condition or not condition? Analysing “change” in longitudinal randomised controlled trials. BMJ Open, 6, e013096. doi: 10.1136/bmjopen-2016-013096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Copeland, W. E., Shanahan, L., Worthman, C., Angold, A., & Costello, E. J. (2012). Cumulative depression episodes predict later C-reactive protein levels: A prospective analysis. Biological Psychiatry, 71, 15–21. doi: 10.1016/j.biopsych.2011.09.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crawford, A. A., Soderberg, S., Kirschbaum, C., Murphy, L., Eliasson, M., Ebrahim, S., … Walker, B. R. (2019). Morning plasma cortisol as a cardiovascular risk factor: Findings from prospective cohort and Mendelian randomization studies. European Journal of Endocrinology, 181, 429–438. doi: 10.1530/EJE-19-0161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crawford, M. H., Bernstein, S. J., Deedwania, P. C., DiMarco, J. P., Ferrick, K. J., Garson, A., … Smith, S. C. (1999). ACC/AHA guidelines for ambulatory electrocardiography: A report of the American college of cardiology/American heart association task force on practice guidelines (Committee to revise the guidelines for ambulatory electrocardiography). Journal of the American College of Cardiology, 34, 912–948. doi: 10.1016/S0735-1097(99)00354-X [DOI] [PubMed] [Google Scholar]
- Cuijpers, P., Berking, M., Andersson, G., Quigley, L., Kleiboer, A., & Dobson, K. S. (2013). A meta-analysis of cognitive-behavioural therapy for adult depression, alone and in comparison with other treatments. Canadian Journal of Psychiatry. Revue Canadienne de Psychiatrie, 58, 376–385. doi: 10.1177/070674371305800702 [DOI] [PubMed] [Google Scholar]
- Cuijpers, P., Cristea, I. A., Karyotaki, E., Reijnders, M., & Huibers, M. J. H. (2016). How effective are cognitive behavior therapies for major depression and anxiety disorders? A meta-analytic update of the evidence. World Psychiatry, 15, 245–258. doi: 10.1002/wps.20346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuijpers, P., Li, J., Hofmann, S. G., & Andersson, G. (2010). Self-reported versus clinician-rated symptoms of depression as outcome measures in psychotherapy research on depression: A meta-analysis. Clinical Psychology Review, 30, 768–778. doi: 10.1016/j.cpr.2010.06.001 [DOI] [PubMed] [Google Scholar]
- David, D., Cristea, I., & Hofmann, S. G. (2018). Why cognitive behavioral therapy Is the current gold standard of psychotherapy. Frontiers in Psychiatry, 9, 4. doi: 10.3389/fpsyt.2018.00004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dedovic, K., & Ngiam, J. (2015). The cortisol awakening response and major depression: Examining the evidence. Neuropsychiatric Disease and Treatment, 11, 1181–1189. doi: 10.2147/NDT.S62289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demyttenaere, K., & De Fruyt, J. (2003). Getting what you ask for: On the selectivity of depression rating scales. Psychotherapy and Psychosomatics, 72, 61–70. doi: 10.1159/000068690 [DOI] [PubMed] [Google Scholar]
- Deverts, D. J., Cohen, S., DiLillo, V. G., Lewis, C. E., Kiefe, C., Whooley, M., & Matthews, K. A. (2010). Depressive symptoms, race, and circulating C-reactive protein: The coronary artery risk development in young adults (CARDIA) study. Psychosomatic Medicine, 72, 734–741. doi: 10.1097/PSY.0b013e3181ec4b98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dimsdale, J. E., von Känel, R., Profant, J., Nelesen, R., Ancoli-Israel, S., & Ziegler, M. (2000). Reliability of nocturnal blood pressure dipping. Blood Pressure Monitoring, 5, 217–221. doi: 10.1097/00126097-200008000-00004 [DOI] [PubMed] [Google Scholar]
- Dowlati, Y., Herrmann, N., Swardfager, W., Liu, H., Sham, L., Reim, E. K., & Lanctot, L. K. (2010). A meta-analysis of cytokines in major depression. Biological Psychiatry, 67, 446–457. doi: 10.1016/j.biopsych.2009.09.033 [DOI] [PubMed] [Google Scholar]
- Eller, N. H., Kristiansen, J., & Hansen, ÅM (2011). Long-term effects of psychosocial factors of home and work on biomarkers of stress. International Journal of Psychophysiology, 79, 195–202. doi: 10.1016/j.ijpsycho.2010.10.009 [DOI] [PubMed] [Google Scholar]
- Euteneuer, F., Dannehl, K., Del Rey, A., Engler, H., Schedlowski, M., & Rief, W. (2017). Immunological effects of behavioral activation with exercise in major depression: An exploratory randomized controlled trial. Translational Psychiatry, 7, e1132. doi: 10.1038/tp.2017.76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fagard, R., Brguljan, J., Thijs, L., & Staessen, J. (1996). Prediction of the actual awake and asleep blood pressures by various methods of 24 h pressure analysis. Journal of Hypertension, 14, 557–563. doi: 10.1097/00004872-199605000-00003 [DOI] [PubMed] [Google Scholar]
- Fang, S.-C., Wu, Y.-L., & Tsai, P.-S. (2020a). Corrigendum to heart rate variability and risk of all-cause death and cardiovascular events in patients With cardiovascular disease: A meta-analysis of cohort studies. Biological Research for Nursing, 22, 423–425. doi: 10.1177/1099800420909152 [DOI] [PubMed] [Google Scholar]
- Fang, S.-C., Wu, Y.-L., & Tsai, P.-S. (2020b). Heart rate variability and risk of all-cause death and cardiovascular events in patients with cardiovascular disease: A meta-analysis of cohort studies. Biological Research for Nursing, 22, 45–56. doi: 10.1177/1099800419877442 [DOI] [PubMed] [Google Scholar]
- Fitzmaurice, G. M., Laird, N. M., & Ware, J. H. (2011). Applied longitudinal analysis (2nd ed.). Hoboken, New Jersey, USA: John Wiley & Sons. [Google Scholar]
- Gan, Y., Gong, Y., Tong, X., Sun, H., Cong, Y., Dong, X., … Lu, Z. (2014). Depression and the risk of coronary heart disease: A meta-analysis of prospective cohort studies. BMC Psychiatry, 14, 1–11. doi: 10.1186/s12888-014-0371-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerteis, A., & Schwerdtfeger, A. (2016). When rumination counts: Perceived social support and heart rate variability in daily life. Psychophysiology, 53, 1034–1043. doi: 10.1111/PSYP.12652. [DOI] [PubMed] [Google Scholar]
- Ginty, A. T., Carroll, D., Roseboom, T. J., Phillips, A. C., & de Rooij, S. R. (2013). Depression and anxiety are associated with a diagnosis of hypertension 5 years later in a cohort of late middle-aged men and women. Journal of Human Hypertension, 27, 187–190. doi: 10.1038/jhh.2012.18 [DOI] [PubMed] [Google Scholar]
- Goldston, K., & Baillie, A. J. (2008). Depression and coronary heart disease: A review of the epidemiological evidence, explanatory mechanisms and management approaches. Clinical Psychology Review, 28, 288–306. doi: 10.1016/j.cpr.2007.05.005 [DOI] [PubMed] [Google Scholar]
- Gould, C. E., & Beaudreau, S. A. (2013). Association between depression and anxiety on blood pressure dysregulation and pulse in the health and retirement study. International Journal of Geriatric Psychiatry, 28, 1045–1053. doi: 10.1002/gps.3926 [DOI] [PubMed] [Google Scholar]
- Greenland, P., Daviglus, M. L., Dyer, A. R., Liu, K., Huang, C. F., Goldberger, J. J., & Stamler, J. (1999). Resting heart rate is a risk factor for cardiovascular and noncardiovascular mortality: The Chicago heart association detection project in industry. American Journal of Epidemiology, 149, 853–862. doi: 10.1093/oxfordjournals.aje.a009901 [DOI] [PubMed] [Google Scholar]
- Hämmerle, P., Eick, C., Blum, S., Schlageter, V., Bauer, A., & Rizas, K. D., … Swiss-AF Study Investigators. (2020). Heart rate variability triangular index as a predictor of cardiovascular mortality in patients with atrial fibrillation. Journal of the American Heart Association, 9, e016075. doi: 10.1161/JAHA.120.016075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harshfield, E. L., Pennells, L., Schwartz, J. E., Willeit, P., Kaptoge, S., & Bell, S., … Emerging Risk Factors Collaboration. (2020). Association between depressive symptoms and incident cardiovascular diseases. JAMA, 324, 2396–2405. doi: 10.1001/jama.2020.23068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hautzinger, M., Kühner, C., & Keller, F. (2006). Das beck depressionsinventar II. Deutsche bearbeitung und handbuch zum BDI II. Frankfurt: Harcourt Test Services. [Google Scholar]
- Hildrum, B., Mykletun, A., Stordal, E., Bjelland, I., Dahl, A. A., & Holmen, J. (2007). Association of low blood pressure with anxiety and depression: The nord-trøndelag health study. Journal of Epidemiology and Community Health, 61, 53–58. doi: 10.1136/jech.2005.044966 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hillebrand, S., Gast, K. B., de Mutsert, R., Swenne, C. A., Jukema, J. W., Middeldorp, S., … Dekkers, O. M. (2013). Heart rate variability and first cardiovascular event in populations without known cardiovascular disease: Meta-analysis and dose–response meta-regression. EP Europace, 15, 742–749. doi: 10.1093/europace/eus341 [DOI] [PubMed] [Google Scholar]
- Howren, M. B., Lamkin, D. M., & Suls, J. (2009). Associations of depression with C-reactive protein, IL-1, and IL-6: A meta-analysis. Psychosomatic Medicine, 71, 171–186. doi: 10.1097/PSY.0b013e3181907c1b [DOI] [PubMed] [Google Scholar]
- Huang, M., Shah, A., Su, S., Goldberg, J., Lampert, R. J., Levantsevych, O. M., … Vaccarino, V. (2018). Association of depressive symptoms and heart rate variability in Vietnam war-era twins: A longitudinal twin difference study. JAMA Psychiatry, 75, 705–712. doi: 10.1001/jamapsychiatry.2018.0747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang, M., Su, S., Goldberg, J., Miller, A. H., Levantsevych, O. M., Shallenberger, L., … Vaccarino, V. (2019). Longitudinal association of inflammation with depressive symptoms: A 7-year cross-lagged twin difference study. Brain, Behavior, and Immunity, 75, 200–207. doi: 10.1016/j.bbi.2018.10.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irwin, M. R., Olmstead, R., Breen, E. C., Witarama, T., Carrillo, C., Sadeghi, N., … Cole, S. (2015). Cognitive behavioral therapy and tai chi reverse cellular and genomic markers of inflammation in late-life insomnia: A randomized controlled trial. Biological Psychiatry, 78, 721–729. doi: 10.1016/j.biopsych.2015.01.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones, B. D. M., Daskalakis, Z. J., Carvalho, A. F., Strawbridge, R., Young, A. H., Mulsant, B. H., … Husain, M. I. (2020). Inflammation as a treatment target in mood disorders: Review. BJPsych Open, 6, 1–10. doi: 10.1192/bjo.2020.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kannel, W. B., Kannel, C., Paffenbarger, R. S., & Cupples, L. A. (1987). Heart rate and cardiovascular mortality: The Framingham study. American Heart Journal, 113, 1489–1494. doi: 10.1016/0002-8703(87)90666-1 [DOI] [PubMed] [Google Scholar]
- Kemp, A. H., Fráguas, R., Brunoni, A. R., Bittencourt, M. S., Nunes, M. A., Dantas, E. M., … Lotufo, P. A. (2016). Differential associations of specific selective serotonin reuptake inhibitors with resting-state heart rate and heart rate variability. Psychosomatic Medicine, 78, 810–818. doi: 10.1097/PSY.0000000000000336 [DOI] [PubMed] [Google Scholar]
- Kemp, A. H., Koenig, J., & Thayer, J. F. (2017). From psychological moments to mortality: A multidisciplinary synthesis on heart rate variability spanning the continuum of time. Neuroscience & Biobehavioral Reviews, 83, 547–567. doi: 10.1016/j.neubiorev.2017.09.006 [DOI] [PubMed] [Google Scholar]
- Kemp, A. H., Quintana, D. S., Gray, M. A., Felmingham, K. L., Brown, K., & Gatt, J. M. (2010). Impact of depression and antidepressant treatment on heart rate variability: A review and meta-analysis. Biological Psychiatry, 67, 1067–1074. doi: 10.1016/j.biopsych.2009.12.012 [DOI] [PubMed] [Google Scholar]
- Kemp, A. H., Quintana, D. S., & Malhi, G. S. (2011). Effects of serotonin reuptake inhibitors on heart rate variability: Methodological issues, medical comorbidity, and clinical relevance. Biological Psychiatry, 69, e25–e26. doi: 10.1016/j.biopsych.2010.10.035 [DOI] [PubMed] [Google Scholar]
- Kiecolt-Glaser, J. K., Derry, H. M., & Fagundes, C. P. (2015). Inflammation: Depression fans the flames and feasts on the heat. American Journal of Psychiatry, 172, 1075–1091. doi: 10.1176/appi.ajp.2015.15020152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koch, C., Wilhelm, M., Salzmann, S., Rief, W., & Euteneuer, F. (2019). A meta-analysis of heart rate variability in major depression. Psychological Medicine, 49, 1948–1957. doi: 10.1017/S0033291719001351. [DOI] [PubMed] [Google Scholar]
- Lake, C. R., Pickar, D., Ziegler, M. G., Lipper, S., Slater, S., & Murphy, D. L. (1982). High plasma norepinephrine levels in patients with major affective disorder. The American Journal of Psychiatry, 139, 1315–1318. doi: 10.1176/ajp.139.10.1315 [DOI] [PubMed] [Google Scholar]
- Lee, D. S., & Way, B. M. (2019). Perceived social support and chronic inflammation: The moderating role of self-esteem. Health Psychology, 38, 563–566. doi: 10.1037/hea0000746 [DOI] [PubMed] [Google Scholar]
- Lehofer, M., Moser, M., Hoehn-Saric, R., McLeod, D., Liebmann, P., Drnovsek, B., … Zapotoczky, H. G. (1997). Major depression and cardiac autonomic control. Biological Psychiatry, 42, 914–919. doi: 10.1016/S0006-3223(96)00494-5 [DOI] [PubMed] [Google Scholar]
- Lewington, S., Clarke, R., Qizilbash, N., Peto, R., & Rory, C. (2002). Age-specific relevance of usual blood pressure to vascular mortality. The Lancet, 360, 1903–1913. doi: 10.1016/s0140-6736(02)11911-8 [DOI] [PubMed] [Google Scholar]
- Li, H., Zheng, D., Li, Z., Wu, Z., Feng, W., Cao, X., … Guo, X. (2019). Association of depressive symptoms with incident cardiovascular diseases in middle-aged and older Chinese adults. JAMA Network Open, 2, e1916591. doi: 10.1001/jamanetworkopen.2019.16591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, X., Shaffer, M. L., Rodriguez-Colon, S., He, F., Wolbrette, D. L., Alagona, P., … Liao, D. (2011). The circadian pattern of cardiac autonomic modulation in a middle-aged population. Clinical Autonomic Research, 21, 143–150. doi: 10.1007/s10286-010-0112-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang, K.-Y., & Zeger, S. L. (2000). Longitudinal data analysis of continuous and discrete responses for pre-post designs. Sankhy: The Indian Journal of Statistics, 62, 134–148. doi: 10.2307/25053123 [DOI] [Google Scholar]
- Liu, G. F., Lu, K., Mogg, R., Mallick, M., & Mehrotra, D. V. (2009). Should baseline be a covariate or dependent variable in analyses of change from baseline in clinical trials? Statistics in Medicine, 28, 2509–2530. doi: 10.1002/sim.3639 [DOI] [PubMed] [Google Scholar]
- Matthews, K. A., Schott, L. L., Bromberger, J. T., Cyranowski, J. M., Everson-Rose, S. A., & Sowers, M. (2010). Are there bi-directional associations between depressive symptoms and C-reactive protein in mid-life women? Brain, Behavior, and Immunity, 24, 96–101. doi: 10.1016/j.bbi.2009.08.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meng, L., Chen, D., Yang, Y., Zheng, Y., & Hui, R. (2012). Depression increases the risk of hypertension incidence: A meta-analysis of prospective cohort studies. Journal of Hypertension, 30, 842–851. doi: 10.1097/HJH.0b013e32835080b7 [DOI] [PubMed] [Google Scholar]
- Montgomery, S. A., & Asberg, M. (1979). A new depression scale designed to be sensitive to change. The British Journal of Psychiatry: The Journal of Mental Science, 134, 382–389. doi: 10.1192/bjp.134.4.382 [DOI] [PubMed] [Google Scholar]
- Moreira, F. P., de Cardoso, T. A., Mondin, T. C., de Souza, L. D. M., Silva, R., Jansen, K., … Wiener, C. D. (2015). The effect of proinflammatory cytokines in cognitive behavioral therapy. Journal of Neuroimmunology, 285, 143–146. doi: 10.1016/j.jneuroim.2015.06.004 [DOI] [PubMed] [Google Scholar]
- Musselman, D. L., Evans, D. L., & Nemeroff, C. B. (1998). The relationship of depression to cardiovascular disease: Epidemiology, biology, and treatment. Archives of General Psychiatry, 55, 580–592. doi: 10.1001/archpsyc.55.7.580 [DOI] [PubMed] [Google Scholar]
- Nicholson, A., Kuper, H., & Hemingway, H. (2006). Depression as an aetiologic and prognostic factor in coronary heart disease: A meta-analysis of 6362 events among 146 538 participants in 54 observational studies. European Heart Journal, 27, 2763–2774. doi: 10.1093/eurheartj/ehl338 [DOI] [PubMed] [Google Scholar]
- O'Brien, E., Asmar, R., Beilin, L., Imai, Y., Mallion, J.-M., & Mancia, G., … European Society of Hypertension Working Group on Blood Pressure Monitoring. (2003). European Society of hypertension recommendations for conventional, ambulatory and home blood pressure measurement. Journal of Hypertension, 21, 821–848. doi: 10.1097/01.hjh.0000059016.82022.ca [DOI] [PubMed] [Google Scholar]
- O'Brien, E., Parati, G., Stergiou, G., Asmar, R., Beilin, L., Bilo, G., … Zhang, Y. (2013). European Society of hypertension position paper on ambulatory blood pressure monitoring. Journal of Hypertension, 31, 1731–1768. doi: 10.1097/HJH.0b013e328363e964 [DOI] [PubMed] [Google Scholar]
- Ohkubo, T., Hozawa, A., Yamaguchi, J., Kikuya, M., Ohmori, K., Michimata, M., … Imai, Y. (2002). Prognostic significance of the nocturnal decline in blood pressure in individuals with and without high 24-h blood pressure: The Ohasama study. Journal of Hypertension, 20, 2183–2189. doi: 10.1097/00004872-200211000-00017 [DOI] [PubMed] [Google Scholar]
- Osimo, E. F., Pillinger, T., Rodriguez, I. M., Khandaker, G. M., Pariante, C. M., & Howes, O. D. (2020). Inflammatory markers in depression: A meta-analysis of mean differences and variability in 5166 patients and 5083 controls. Brain, Behavior, and Immunity, 87, 901–909. doi: 10.1016/j.bbi.2020.02.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parati, G., Stergiou, G., O'Brien, E., Asmar, R., Beilin, L., & Bilo, G., … European Society of Hypertension Working Group on Blood Pressure Monitoring and Cardiovascular Variability. (2014). European Society of hypertension practice guidelines for ambulatory blood pressure monitoring. Journal of Hypertension, 32, 1359–1366. doi: 10.1097/HJH.0000000000000221 [DOI] [PubMed] [Google Scholar]
- Pearson, T. A. (2003). Markers of inflammation and cardiovascular disease: Application to clinical and public health practice: A statement for healthcare professionals from the centers for disease control and prevention and the American heart association. Circulation, 107, 499–511. doi: 10.1161/01.CIR.0000052939.59093.45 [DOI] [PubMed] [Google Scholar]
- Pelle, A. J. M., Gidron, Y. Y., Szabó, B. M., & Denollet, J. (2008). Psychological predictors of prognosis in chronic heart failure. Journal of Cardiac Failure, 14, 341–350. doi: 10.1016/j.cardfail.2008.01.004 [DOI] [PubMed] [Google Scholar]
- Plaisance, E. P., & Grandjean, P. W. (2006). Physical activity and high-sensitivity C-reactive protein. Sports Medicine, 36, 443–458. doi: 10.2165/00007256-200636050-00006 [DOI] [PubMed] [Google Scholar]
- Psarraki, E. E., Kokka, I., Bacopoulou, F., Chrousos, G. P., Artemiadis, A., & Darviri, C. (2021). Is there a relation between major depression and hair cortisol? A systematic review and meta-analysis. Psychoneuroendocrinology, 124, 105098. doi: 10.1016/j.psyneuen.2020.105098 [DOI] [PubMed] [Google Scholar]
- Rief, W., Nestoriuc, Y., Weiss, S., Welzel, E., Barsky, A. J., & Hofmann, S. G. (2009). Meta-analysis of the placebo response in antidepressant trials. Journal of Affective Disorders, 118, 1–8. doi: 10.1016/j.jad.2009.01.029 [DOI] [PubMed] [Google Scholar]
- Rogeness, G. A., Cepeda, C., Macedo, C. A., Fisher, C., & Harris, W. R. (1990). Differences in heart rate and blood pressure in children with conduct disorder, major depression, and separation anxiety. Psychiatry Research, 33, 199–206. doi: 10.1016/0165-1781(90)90074-F [DOI] [PubMed] [Google Scholar]
- Rothman, K. J. (1990). No adjustments are needed for multiple comparisons. Epidemiology, 1, 43–46. doi: 10.1097/00001648-199001000-00010 [DOI] [PubMed] [Google Scholar]
- Rubin, M. (2017). Do p values lose their meaning in exploratory analyses? It depends how you define the familywise error rate. Review of General Psychology, 21, 269–275. doi: 10.1037/gpr0000123 [DOI] [Google Scholar]
- Schmidtke, A., Fleckenstein, P., Moises, W., & Beckmann, H. (1988). [Studies of the reliability and validity of the German version of the Montgomery-Asberg Depression Rating Scale (MADRS)]. Schweizer Archiv Für Neurologie Und Psychiatrie, 139, 51–65. [PubMed] [Google Scholar]
- Sgoifo, A., Carnevali, L., de los Angeles Pico Alfonso M., & Amore, M. (2015). Autonomic dysfunction and heart rate variability in depression. Stress, 18, 343–352. doi: 10.3109/10253890.2015.1045868 [DOI] [PubMed] [Google Scholar]
- Shaffer, F., & Ginsberg, J. P. (2017). An overview of heart rate variability metrics and norms. Frontiers in Public Health, 5, 258. doi: 10.3389/fpubh.2017.00258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shinagawa, M., Otsuka, K., Murakami, S., Kubo, Y., Cornelissen, G., Matsubayashi, K., … Halberg, F. (2002). Seven-day (24-h) ambulatory blood pressure monitoring, self-reported depression and quality of life scores. Blood Pressure Monitoring, 7, 69–76. doi: 10.1097/00126097-200202000-00015 [DOI] [PubMed] [Google Scholar]
- Sin, N. L., Sloan, R. P., McKinley, P. S., & Almeida, D. M. (2016). Linking daily stress processes and laboratory-based heart rate variability in a national sample of midlife and older adults. Psychosomatic Medicine, 78, 573. doi: 10.1097/PSY.0000000000000306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spaderna, H., Zittermann, A., Reichenspurner, H., Ziegler, C., Smits, J., & Weidner, G. (2017). Role of depression and social isolation at time of waitlisting for survival 8 years after heart transplantation. Journal of the American Heart Association, 6, 12. doi: 10.1161/JAHA.117.007016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stapelberg, N. J. C., Neumann, D. L., Shum, D. H. K., McConnell, H., & Hamilton-Craig, I. (2018). The sensitivity of 38 heart rate variability measures to the addition of artifact in human and artificial 24-h cardiac recordings. Annals of Noninvasive Electrocardiology, 23, e12483. doi: 10.1111/anec.12483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stetler, C., & Miller, G. E. (2011). Depression and hypothalamic-pituitary-adrenal activation: A quantitative summary of four decades of research. Psychosomatic Medicine, 73, 114–126. doi: 10.1097/PSY.0b013e31820ad12b [DOI] [PubMed] [Google Scholar]
- Subirana, I., Fitó, M., Diaz, O., Vila, J., Francés, A., Delpon, E., … Marrugat, J. (2018). Prediction of coronary disease incidence by biomarkers of inflammation, oxidation, and metabolism. Scientific Reports, 8, 3191. doi: 10.1038/s41598-018-21482-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology (1996). Heart rate variability: standards of measurement, physiological interpretation and clinical use. Circulation, 93, 1043–1065. [PubMed] [Google Scholar]
- Task Force of The European Society of Cardiology and The North American, & Society of Pacing and Electrophysiology (1996). Heart rate variability: Standards of measurement, physiological interpretation, and clinical use. European Heart Journal, 17, 354–381. [PubMed] [Google Scholar]
- Taylor, C. B., Conrad, A., Wilhelm, F. H., Strachowski, D., Khaylis, A., Neri, E., … Spiegel, D. (2009). Does improving mood in depressed patients alter factors that may affect cardiovascular disease risk? Journal of Psychiatric Research, 43, 1246–1252. doi: 10.1016/j.jpsychires.2009.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uchino, B. N., Trettevik, R., de Grey, K., Cronan, R. G., Hogan, S., & Baucom, J., & W, B. R. (2018). Social support, social integration, and inflammatory cytokines: A meta-analysis. Health Psychology, 37, 462–471. doi: 10.1037/hea0000594 [DOI] [PubMed] [Google Scholar]
- Valkanova, V., Ebmeier, K. P., & Allan, C. L. (2013). CRP, IL-6 and depression: A systematic review and meta-analysis of longitudinal studies. Journal of Affective Disorders, 150, 736–744. doi: 10.1016/j.jad.2013.06.004 [DOI] [PubMed] [Google Scholar]
- Vila, X. A., Lado, M. J., & Cuesta-Morales, P. (2019). Evidence based recommendations for designing heart rate variability studies. Journal of Medical Systems, 43, 311. doi: 10.1007/s10916-019-1437-8 [DOI] [PubMed] [Google Scholar]
- Williams, E. D., & Steptoe, A. (2007). The role of depression in the etiology of acute coronary syndrome. Current Psychiatry Reports, 9, 486–492. doi: 10.1007/s11920-007-0066-y [DOI] [PubMed] [Google Scholar]
- Wittchen, H.-U., Wunderlich, U., Gruschitz, S., & Zaudig, M. (1997). Strukturiertes Klinisches Interview für DSM-IV, Achse I (SKID-I). In Göttingen: Hogrefe.
- Wu, Q., & Kling, J. M. (2016). Depression and the risk of myocardial infarction and coronary death. Medicine, 95, e2815. doi: 10.1097/MD.0000000000002815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang, Y. C., Schorpp, K., & Harris, K. M. (2014). Social support, social strain and inflammation: Evidence from a national longitudinal study of U.S. Adults. Social Science & Medicine (1982), 107, 124–135. doi: 10.1016/j.socscimed.2014.02.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeh, T.-C., Kao, L.-C., Tzeng, N.-S., Kuo, T. B. J., Huang, S.-Y., Chang, C.-C., & Chang, H.-A. (2016). Heart rate variability in major depressive disorder and after antidepressant treatment with agomelatine and paroxetine: Findings from the Taiwan study of depression and anxiety (TAISDA). Progress in Neuro-Psychopharmacology & Biological Psychiatry, 64, 60–67. doi: 10.1016/j.pnpbp.2015.07.007 [DOI] [PubMed] [Google Scholar]
- Zabihiyeganeh, M., Vafaee Afshar, S., Amini Kadijani, A., Jafari, D., Bagherifard, A., Janbozorgi, M., … Mirzaei, A. (2019). The effect of cognitive behavioral therapy on the circulating proinflammatory cytokines of fibromyalgia patients: A pilot controlled clinical trial. General Hospital Psychiatry, 57, 23–28. doi: 10.1016/j.genhosppsych.2019.01.003 [DOI] [PubMed] [Google Scholar]
- Ziegler, D., Piolot, R., Strassburger, K., Lambeck, H., & Dannehl, K. (1999). Normal ranges and reproducibility of statistical, geometric, frequency domain, and non-linear measures of 24-h heart rate variability. Hormone and Metabolic Research, 31, 672–679. doi: 10.1055/s-2007-978819 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit https://doi.org/10.1017/S0033291722000447.
click here to view supplementary material