Although women appear less healthy according to the frailty index, they have lower death rates at all ages. This is known as the morbidity–mortality paradox and can be explained multifactorially by anatomic, behavioral, and social differences (1). Sex differences play an important role in medicine; for example, women with hip fractures are less likely to undergo surgery (2). The underlying mechanisms often remain unclear and are currently the subject of much debate (1, 3). Here, we describe sex differences in pelvic fractures and examine factors that may help explain the morbidity–mortality paradox.
Footnotes
Conflict of interest statement
The authors declare that no conflict of interest exists.
Methods
The German Pelvic Trauma Registry (GPR) is a multicenter registry of the German Trauma Society (Deutsche Gesellschaft für Unfallchirurgie, DGU) with 38 participating hospitals. Data on pelvic fractures are collected by means of a questionnaire-based survey with 231 categorical or numerical items. This retrospective analysis includes all data sets from 2003 (start of the registry) to 2017 (update of the questionnaire) (n = 16 359).
Sex differences were first examined observationally. Next, three logistic regression models with the dependent variables “surgery,” “complication,” and “mortality” were constructed. From these, adjusted odds ratios (AOR) were calculated for all independent variables in the models. The Akaike information criterion (AIC) relates the gain in accuracy yielded by including an independent variable to the additional complexity of a model. The AIC change was calculated for all three logistic regression models for the inclusion of the independent variable sex. Differences between men and women for categorical variables were evaluated using the chi² test.
Results
Epidemiology
Women are more commonly affected by pelvic fractures than men. Using the sex distribution obtained from the registry, an incidence of 33.4/100 000 for men and 38.4/100 000 for women can be calculated.
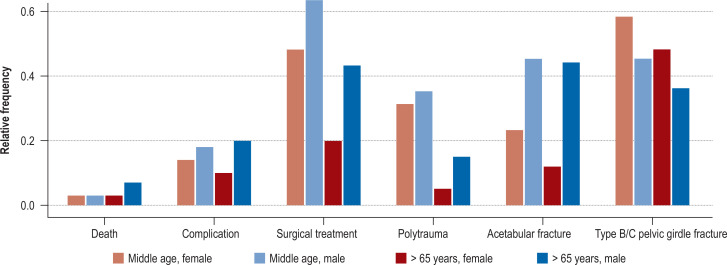
Analysis of three age groups (young < 35 years, middle-aged 35–65 years, old > 65 years) shows that men predominate in the two younger groups, whereas women predominate in the oldest group. In all three age groups, the proportion of acetabular fractures is higher in men, while the proportion of unstable pelvic girdle fractures is higher in women. The proportion of polytrauma as the cause of fractures is higher in men. The proportion was also higher in men than in women for surgery, morbidity, and mortality (figure).
Figure.
An overview of the epidemiological data and the proportion of cases according to factors and age groups (middle age 35–65 years [men n = 3433, women n = 1591]; old > 65 years [men n = 2389, women n = 6029])
Logistic regression analysis
All three models examined were significant. The AIC is reduced in all three models by adding the independent variable “sex”. Therefore “sex” improves all tested models and provides a partial explanation for the expression of the respective dependent variable. Multicollinearity was explicitly tested and ruled out. Female sex lowered the AOR for all three dependent variables, while age decreased the AOR for surgical treatment but increased the AOR for morbidity and mortality (table).
Table. Three evaluated models for the dependent variables “surgery,” “complication,” and “death”*.
| Factor | Surgery: adjusted OR [95% CI]/p | Complication: adjusted OR [95% CI]/p | Death: adjusted OR [95% CI]/p |
| Sex | |||
| Female | 0.58 [0. 53; 0.63] p < 0.001 | 0.74 [0. 67; 0.82] p < 0.001 | 0.82 [0.68; 0.98] p = 0.032 |
| Fracture | |||
| Acetabular involvement | 8.94 [8.05; 9.95] p < 0.001 | 2.59 [2.31; 2.89] p < 0.001 | 1.17 [0.95; 1.43] p = 0.146 |
| Type B/C pelvic girdle fracture | 5.12 [4.63; 5.67] p < 0.001 | 1.80 [1. 61; 2. 02] p < 0.001 | 0.96 [0.78; 1.17] p = 0.663 |
| Extent of injury | |||
| Polytrauma | 1.08 [0.95; 1.23] p = 0.101 | 1.48 [1.28; 1.72] p < 0.001 | 2.27 [1.73; 2.98] p < 0.001 |
| Continuous factors | |||
| ISS (Injury Severity Score) | 1.03 [1.02; 1.03] p < 0.001 | 1.04 [1.03; 1.04] p <0.001 | 1.09 [1.08; 1.10] p <0.001 |
| Age | 0.98 [0.98; 0.99] p < 0.001 | 1.01 [1.01; 1.02] p < 0.001 | 1.05 [1.04; 1.05] p < 0.001 |
* As well as the unadjusted and adjusted odds ratios (OR) of the independent variables.
The corresponding references for the discrete factors are: sex, male; fracture: no acetabular involvement or no type B/C pelvic girdle fracture; extent of injury: no polytrauma. CI, Confidence interval; OR, odds ratio
Conclusion
There are numerous sex differences that support and partially explain the morbidity–mortality paradox in pelvic fractures. “Sex” contributes to the predictive accuracy of the variables “surgery,” “complication,” and “mortality.” In summary, consistent with the morbidity–mortality paradox, women are more likely to suffer a pelvic fracture, but with lower injury severity and, despite higher age, with fewer complications and lower mortality. In contrast, men with a pelvic fracture are more likely than women to undergo surgery. Thus, “sex” remains an important determinant of the likelihood of surgical treatment and of morbidity and mortality.
Limitations and strengths
The large data set allows for small subgroup analyses. Only the acute and inpatient course is recorded, but this is documented in detail. Longer-term follow-up is missing. The data collection is biased in that only patients treated in specialized centers affiliated with the registry are included. Important additional factors such as pre-existing conditions, medications, and osteoporosis have only been included since the revision of the questionnaire in 2017.
The importance of this work
This can be summarized in three points:
Scientific: Documented yet unexplained sex differences, such as different fracture patterns, need to be validated and explained in future research.
Care planning: The data show that decision making is largely objective, but in part biased by sex. Therefore, decision making needs to be reevaluated in light of the expected pattern of injury and the question of which patient group will benefit from which treatment.
Prevention: Targeted prevention is certainly an important starting point. It includes education about risk behavior, particularly in young men, but also optimization of occupational health and safety, especially in the more dangerous manual labor occupations (4). In women, on the other hand, consistent and guideline-based postmenopausal osteoporosis therapy should be ensured.
References
- 1.Austad SN. Why women live longer than men: sex differences in longevity. Gend Med. 2006;3:79–92. doi: 10.1016/s1550-8579(06)80198-1. [DOI] [PubMed] [Google Scholar]
- 2.Audretsch C, Trulson A, Höch A, et al. Evaluation of decision-making in the treatment of acetabular fractures. EFORT Open Rev. 2022;7:84–94. doi: 10.1530/EOR-20-0149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schünemann J, Strulik H, Trimborn T. The gender gap in mortality: How much is explained by behavior? J Health Econ. 2017;54:79–90. doi: 10.1016/j.jhealeco.2017.04.002. [DOI] [PubMed] [Google Scholar]
- 4.Stergiou-Kita M, Mansfield E, Bezo R, et al. Danger zone: men, masculinity and occupational health and safety in high risk occupations. Saf Sci. 2015;80:213–220. doi: 10.1016/j.ssci.2015.07.029. [DOI] [PMC free article] [PubMed] [Google Scholar]