Abstract
Background:
Aging alters biological processes resulting in body fat redistribution, loss of lean muscle mass, and reduced muscle strength, termed sarcopenia. Nutrition is an important modifiable risk factor in the development of sarcopenia. Food insecurity refers to limited or uncertain access to enough food for an active, healthy life, and is prevalent among older adults. The objective of this study was to examine the relationship between food insecurity and probable sarcopenia in older adults.
Methods
We examined 3,632 adults ≥60 years old from the 2011–2014 National Health and Nutrition Examination Surveys (NHANES). For our analysis food insecurity was identified using the Food Security Survey Module (FSSM). The primary outcome was based on the Sarcopenia Definitions and Outcomes consortium (SDOC) definition. Secondary outcomes were based on three other different grip strength cut-offs as there is debate within the field as to the optimal definition of sarcopenia. Consistent with the revised European consensus on the definition and diagnosis of Sarcopenia (EWGSOP2) recommendations, we used the term probable sarcopenia throughout this text as definitions were based on muscle strength alone and did not include an evaluation of muscle quality. Sensitivity analyses were performed using the standard four category definition of food security. We used logistic regression to examine the association between food insecurity and sarcopenia.
Results:
Using the Sarcopenia Definitions and Outcomes Consortium definition, 24.7% were classified as having probable sarcopenia (low grip strength); 5.5% had food insecurity and food insecurity was associated with probable sarcopenia (OR 1.51, 95%CI 1.03–2.22). Using three other definitions of probable sarcopenia, food insecurity was significantly associated with probable sarcopenia using the Foundation for the National Institute of Health definition using grip strength alone (OR 1.71, 95%CI 1.08–2.71), but food insecurity was not associated with food insecurity using definitions related to grip strength/BMI (OR 1.16, 95%CI 0.76–1.78) or grip strength/weight (OR 1.14, 95%CI 0.85–1.54).
Conclusions:
In this nationally representative cohort study, individuals classified as having food insecurity were more likely to have probable sarcopenia (low grip strength) compared to those with full food security. Future studies should examine whether food insecurity interventions may reduce probable sarcopenia and associated adverse outcomes.
Keywords: sarcopenia, food insecurity, epidemiology, aging
BACKGROUND
Sarcopenia is defined as a progressive loss of skeletal muscle mass, strength, and/or physical function.[1] Sarcopenia is an important aging syndrome that independently predicts multiple clinically relevant adverse outcomes, including increased risk of falls, fractures, mobility, and mortality.[2–4] The development of sarcopenia is likely multifactorial. Probable contributors include age-related changes in physiology, sedentary lifestyle, nutrition, and acute illness.[5] Lifestyle factors are the most common modifiable risk factors in the development of sarcopenia.[6] Multiple studies link malnutrition with the development of sarcopenia.[7] Recent consensus guidelines suggest that in order to make the diagnosis of malnutrition in older adults, one should identify at least one of three phenotypic criteria (non-volitional weight loss, reduced muscle mass, low body mass index) and one of two etiologic criteria (inflammation or disease burden and reduced food intake or assimilation).[8] A systematic review of studies in hospitalized older adults found considerable overlap (41.6%) between sarcopenia and malnutrition.[9] Further, a study of community-dwelling older adults found that the prevalence of sarcopenia was 31.4% in those with malnutrition and 6.1% in those without malnutrition.[10]
Older adults are at increased risk of developing malnutrition.[7] Previous studies estimate that 5–10% of community-dwelling older adults and up to 80% of those in a long-term care setting are malnourished.[11] Like sarcopenia, many factors contribute to the development of malnutrition.[12] In community-dwelling older adults, food insecurity plays a role in nutrition status.[13] Food insecurity is defined as limited or uncertain access to enough food for an active, healthy life.[14] Population-based estimates suggest that 10.5% of the United States population experienced food insecurity in 2020,[15] while a study that focused on older adults found that over a ten year period from 2007–2016 food insecurity increased from 5.5% to 12.4%.[15] Food insecurity is a major public health concern that persists despite major policy efforts including Supplemental Nutrition Assistance Program (SNAP),[16] Special Supplemental Nutrition Program for Women, Infants, and Children (WIC),[17] and Commodity Supplemental Food Program (CSFP).[18]
There is evidence to suggest that food insecurity can lead to malnutrition in older adults, and malnutrition is a risk factor for sarcopenia. Limited literature, however, has investigated the relationship between food insecurity and sarcopenia. To our knowledge, three prior studies have examined this relationship. All were based in low- and middle-income countries, and results were mixed.[19] There have been no prior studies which have evaluated this relationship in a US population. Developing a better understanding of this association has evident importance with implications for policymaking and clinical decision-making. This study analyzed data obtained from a nationally representative cohort of participants and assessed for an association between food insecurity and probable sarcopenia (i.e., low muscle strength indicated by low grip strength), as defined by the European Working Groups on Sarcopenia in Older People.
METHODS
Study Design and Population
All data were obtained through the National Health, and Nutrition Evaluation Surveys (NHANES) collected from the 2011–2012 and 2013–2014 surveys. NHANES is a program of the National Center for Health Statistics (NCHS) and data review was approved by the ethics review board of both the NCHS and the Centers for Disease Control (CDC). This was a cross-sectional survey including in-home interviews as well as physical examinations. Complex, multistage probability sampling of the non-institutionalized US population was utilized to obtain a nationally representative sample. Interviews included data on demographic, dietary, health, and socioeconomic questions. Examinations included physiologic and physical measurements. Participants provided written consent, and all interviews and examinations were performed by trained technicians as described in the standard operation manuals (available from NHANES at http://www.cdc.gov/nchs/nhanes.htm.) Data were deidentified. The Office of Human Research Ethics at the University of North Carolina determined that this secondary analyses of de-identified data was not human subjects research.
Of the 19,931 participants in these two survey cycles, we identified 3,632 aged ≥60 years old. Of this subset, 3,121 (86%) had complete grip strength data, and 3,104 (85%) of those had complete data on food security as well. Complete data on food security was defined as completing all parts from the 10-item United States Adult Food Security Module.[20] After considering covariates, the final analytical cohort was 2,781 persons.
Primary Exposure - Food Insecurity
The primary exposure variable was food insecurity. In NHANES, food insecurity was assessed through the 10-item United States Department of Agriculture Adult Food Security Survey Module (FSSM). This is a validated survey measuring food insecurity in adults over the past 12 months. Affirmative responses indicate greater food insecurity and are scored on 4 levels defined as full food security (no affirmative responses), marginal food security (1–2 affirmative responses), low food security (3–5 affirmative responses), and very low food security (6–10 affirmative responses.) To maximize power, we dichotomized results into either full food security (no affirmative responses) or food insecurity (≥1 affirmative response) for the purpose of our analysis. Food insecurity in NHANES was assessed at the household level and was used in this study as a surrogate for individual level food insecurity information.
Primary Outcome - Sarcopenia
Our primary outcome variable was probable sarcopenia defined using grip strength cutoffs. Grip strength was measured by a trained examiner using a handgrip dynamometer whose size was adjusted for the hand size of each participant. The examiner guided participants through the protocol for measuring grip strength and asked them to complete a practice trial. A total of three measurements were obtained with each hand with 60 seconds of rest between measurements on the same hand. Grip strength was measured with participants in the standing position unless they were unable to due to physical limitation. We excluded those with prior surgery of the hand/wrist, arthritis of the hand/wrist, or carpal tunnel, and any participants unable to complete testing on both hands for any reason. As sarcopenia definitions have differed and continue to be a source of debate,[21] we deliberately used different definitions. Four different definitions of sarcopenia used were (Appendix 1): (a) the SDOC definition using grip strength <35.5kg for men and <20kg for women; (b) grip strength divided by body mass index (BMI) <1.05 for men and <0.79 for women; (c) grip strength divided by body weight <0.45 for men and <0.34 for women; (d) and the previously published definition from FNIH - grip strength <26kg for men and <16kg for women. Height and weight data were obtained during the physical examination, as discussed below. The revised European consensus recommendations for the definition and diagnosis of Sarcopenia defined sarcopenia as the presence of low muscle strength and low muscle quality with sarcopenia being defined as severe if it impacts physical function. This group recognized the difficulties inherent in measuring muscle quality and thus recommended measuring muscle strength as an initial step in the path toward diagnosis before confirming the diagnosis with an assessment of muscle quality. Additionally, they recommended referring to low muscle strength in the absence of an assessment of muscle quality as probable sarcopenia which we have done in this study. We did not include specific cut-offs from this group in our definitions as they are very similar to the FNIH cut-offs (grip strength <27kg for men and <16kg for women).
Covariates
Based on available literature and our previously conducted analyses, covariates were chosen based on factors that may confound the association, if any, between probable sarcopenia and food insecurity. A self-reported questionnaire gathered the following information: age, sex, marital status (single, married or living with a partner, widowed/divorced/separated), education (non-high school graduate, high school graduate/GED, some college or associate degree, and college graduate or above), income expressed as a ratio to the federal poverty level (which accounts for inflation and household size), smoking status (never, current, former). As an indicator of the potential experience of racism, which may confound the association between probable sarcopenia and food insecurity, we also included data on race and ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, and other). Height was measured using a stadiometer with participants standing against a vertical background with an adjustable headpiece, and weight was measured using a digital scale with participants standing and wearing standardized examination gowns. Medical co-morbidity was also assessed using the questionnaire with the question “Have you ever been told by a doctor or other health professional that you had….”. For this analysis, we identified the following disorders: kidney disease, diabetes, heart failure, heart attack, and stroke. Each was dichotomized (yes/no).
Statistical Analysis
All analyses used weights to produce nationally-representative estimates, and we accounted for the complex sampling design in standard error estimation. Continuous variables are represented as means and standard errors, while categorical variables are represented as counts and weighted percentages. Chi-square and analysis of variance tests assessed differences in baseline characteristics. We evaluated the prevalence of food security by sarcopenia status based on the definitions previously outlined. Unadjusted and adjusted logistic regression models evaluated the relationship between food insecurity status (present/absent) as the primary predictor and probable sarcopenia status as the outcome. Adjusted models included co-variates defined above. All data was conducted using R (www-r-project.com). A p<0.05 was considered statistically significant.
RESULTS
Table 1 represents the baseline characteristics of the cohort, and Figure 1 demonstrates the identification of the cohort. Our final analytic cohort consisted of 2,781 older adults with complete data. Using the SDOC definition, the mean age of those not having probable sarcopenia (low grip strength) was 68.4 years (95% CI: 68.0–68.8) and 73.3 years (72.6–74.0) for those with probable sarcopenia. The proportion of participants characterized as having probable sarcopenia using the SDOC definition (Table 1) was 24.7%. Proportions differed using different definitions: grip strength/BMI definition (Definition #2, Appendix 2); grip strength/weight definition (Definition #3, Appendix 3); or the previous FNIH definition (Definition #4, Appendix 4) with 33.2%, 54.8%, and 9.0% respectively. Participants with probable sarcopenia had a larger proportion of medical comorbidities than those without probable sarcopenia, this was consistent across all definitions. Increasing severity of food insecurity was associated with multiple baseline characteristics including age (p=0.01), race (P=<0.001), education (P=<0.001), income (P=0.01), and certain co-morbidities (Appendix 4). The odds of probable sarcopenia were higher in those with marginal food insecurity (OR 1.4 95% CI 0.85–2.32) low food insecurity (OR 1.78, 95%CI: 1.07–2.96) and very low food insecurity (OR 1.33 95% CI 0.47–3.74) compared to those with and full food security (Appendix 5). However, a statistical difference was only observed for those with low food security (p=0.033)
Table 1:
Participant Characteristics By SDOC Sarcopenia Definition
| No Probable Sarcopenia | Probable Sarcopenia | p-value | |
|---|---|---|---|
| N = 2,094 | N = 687 | ||
| Age | 68.41 (68–68.82) | 73.27 (72.59–73.95) | <0.001 |
| Sex | - | - | <0.001 |
| Female | 1292 (61.5) | 121 (20.9) | - |
| Male | 802 (38.5) | 566 (79.1) | - |
| Race | - | - | 0.010 |
| Non-Hispanic White | 999 (80.1) | 335 (75.4) | - |
| Non-Hispanic Black | 554 (8.9) | 120 (7.3) | - |
| Hispanic | 369 (6.4) | 140 (9.6) | - |
| Other | 172 (4.5) | 92 (7.7) | - |
| Education | - | - | <0.001 |
| ≤12th grade | 517 (15.4) | 241 (25.9) | - |
| High school graduate/GED | 488 (21.8) | 157 (21) | - |
| Some college or AA degree | 622 (32.9) | 142 (24.1) | - |
| College graduate or above | 467 (29.9) | 147 (29) | - |
| Income Federal Poverty Level | 3.17 (3–3.34) | 2.64 (2.47–2.8) | <0.001 |
| Marital Status | - | - | 0.09 |
| Single | 114 (3.7) | 46 (6.7) | - |
| Widowed, divorced, or separated | 800 (31.3) | 241 (31.7) | - |
| Married or living with partner | 1180 (65) | 400 (61.6) | - |
| Smoking Status | - | - | 0.30 |
| Never smoker | 1060 (49.6) | 307 (46.9) | - |
| Former smoker | 764 (38.9) | 293 (42.5) | - |
| Current smoker | 270 (11.5) | 87 (10.6) | - |
| Body Mass Index | 29.32 (28.82–29.83) | 27.82 (27.02–28.63) | <0.001 |
| Kidney Condition | 112 (4.1) | 52 (7) | 0.007 |
| Diabetes | 0.002 | ||
| Borderline | 102 (4.5) | 25 (3.7) | - |
| Yes | 464 (18) | 200 (26.7) | - |
| Congestive heart failure | 127 (5.9) | 85 (13.2) | <0.001 |
| Myocardial infarction | 170 (8.1) | 86 (12.4) | 0.003 |
| Stroke | 134 (5.6) | 84 (11.5) | <0.001 |
Participant characteristics stratified by presence of probable sarcopenia as defined by SDOC cutoffs for grip strength <35.5kg for men and <20kg for women.
N: respondent counts
All values represented are weighted means (95% CI) or unweighted counts (weighted %)
Figure 1:
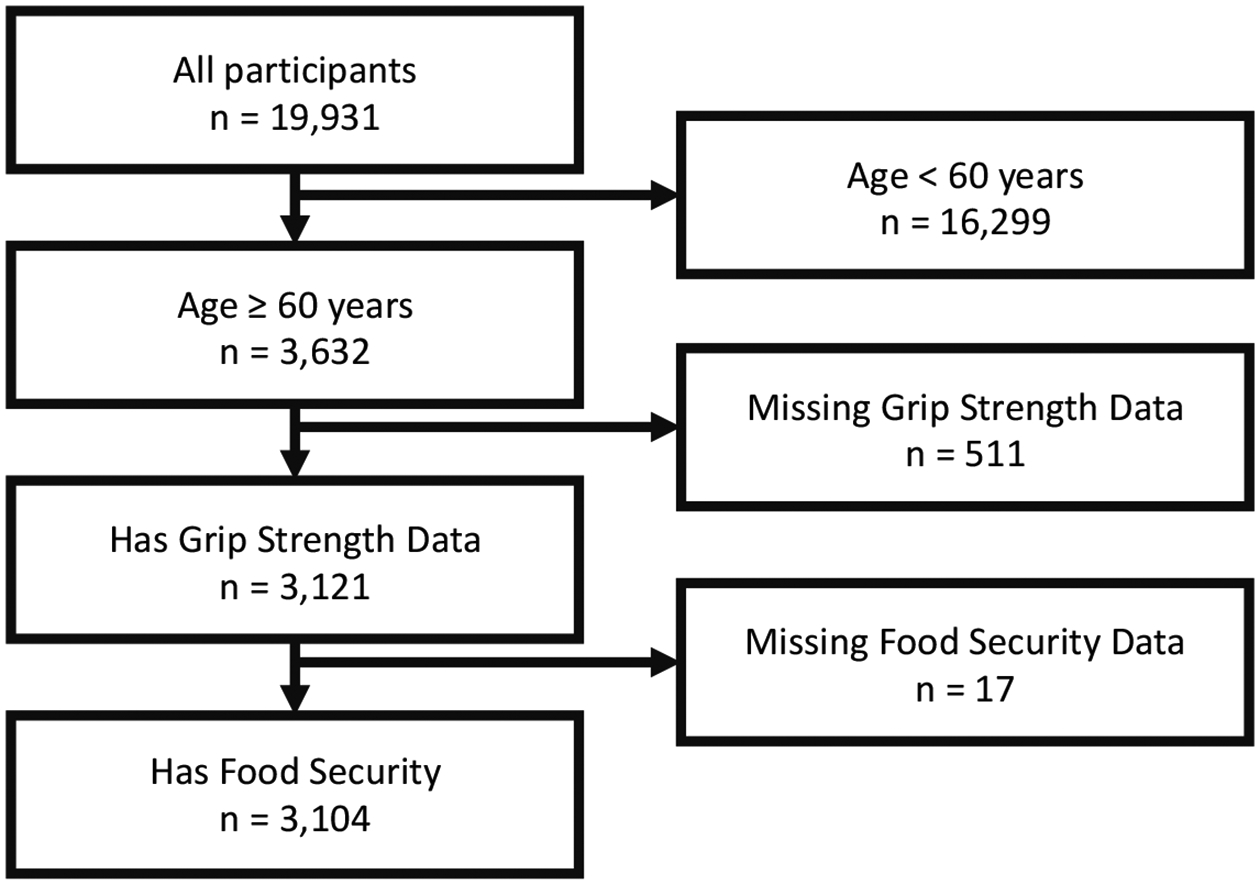
Cohort Definition
Table 2 represents the rates of food insecurity and probable sarcopenia (low grip strength) across four definitions of sarcopenia, while Fig 2. demonstrates the overlap in the prevalence of food insecurity using the four different definitions of sarcopenia. The rates of food insecurity were consistently higher in participants with probable sarcopenia as compared to those without probable sarcopenia (Table 2). Table 3 outlines the unadjusted and adjusted odds ratios for food security by probable sarcopenia based on the SDOC definition of grip strength (Definition 1). Utilizing the SDOC definition of probable sarcopenia based on grip strength alone, we found that food insecurity is significantly associated with probable sarcopenia, OR 1.51 (1.03–2.22) after adjusting for covariates. We repeated these analyses using additional sarcopenia definitions. While definition 4 (FNIH grip strength, OR 1.71 (1.08–2.71), appendix 9) was significant, none of the other definitions proved to be significantly related (definition 2 grip strength/BMI, OR 1.16 (0.76–1.78), appendix 7) or 3 (grip strength/weight, OR 1.14 (0.85–1.54), appendix 8).
Table 2:
Each Definition of Probable Sarcopenia By Food Security Status
| Definition | Probable Sarcopenia | Full food security | Food insecurity | |||
|---|---|---|---|---|---|---|
| Marginal | Low | Very low | Combined | |||
| N=2193 | N=228 | N=234 | N=126 | N=588 | ||
| SDOC grip strength | No sarcopenia | 1660 (75.7%) | 169 (74.1%) | 169 (72.2%) | 96 (76.2%) | 434 (73.8%) |
| Sarcopenia | 533 (24.3%) | 59 (25.9%) | 65 (27.8%) | 30 (23.8%) | 154 (26.2%) | |
| SDOC grip strength / BMI | No sarcopenia | 1522 (69.4%) | 134 (58.8%) | 126 (53.8%) | 77 (61.1%) | 337 (57.3%) |
| Sarcopenia | 671 (30.6%) | 94 (41.2%) | 108 (46.2%) | 49 (38.9%) | 251 (42.7%) | |
| SDOC grip strength / weight | No sarcopenia | 1023 (46.6%) | 95 (41.7%) | 89 (38.0%) | 49 (38.9%) | 233 (39.6%) |
| Sarcopenia | 1170 (53.4%) | 133 (58.3%) | 145 (62.0%) | 77 (61.1%) | 355 (60.4%) | |
| FNIH grip strength | No sarcopenia | 2012 (91.7%) | 203 (89.0%) | 205 (87.6%) | 112 (88.9%) | 520 (88.4%) |
| Sarcopenia | 181 (8.3%) | 25 (11.0%) | 29 (12.4%) | 14 (11.1%) | 68 (11.6%) | |
FNIH- Foundation for the National Institute of Health. SDOC- Sarcopenia Definitions and Outcomes consortium.
Prevalence of food insecurity based on presence or absence of probable sarcopenia for each definition: Definition 1 – SDOC defined grip strength <35.5kg for men and <20kg for women, Definition 2 – SDOC defined grip strength divided by BMI <1.05 for men and <0.79 for women, Definition 3 - SDOC defined grip strength divided by weight <0.45 for men and <0.34 for women, Definition 4 – FNIH defined grip strength <26kg for men and <16kg for women.
All values represented are weighted counts (%).
Figure 2:
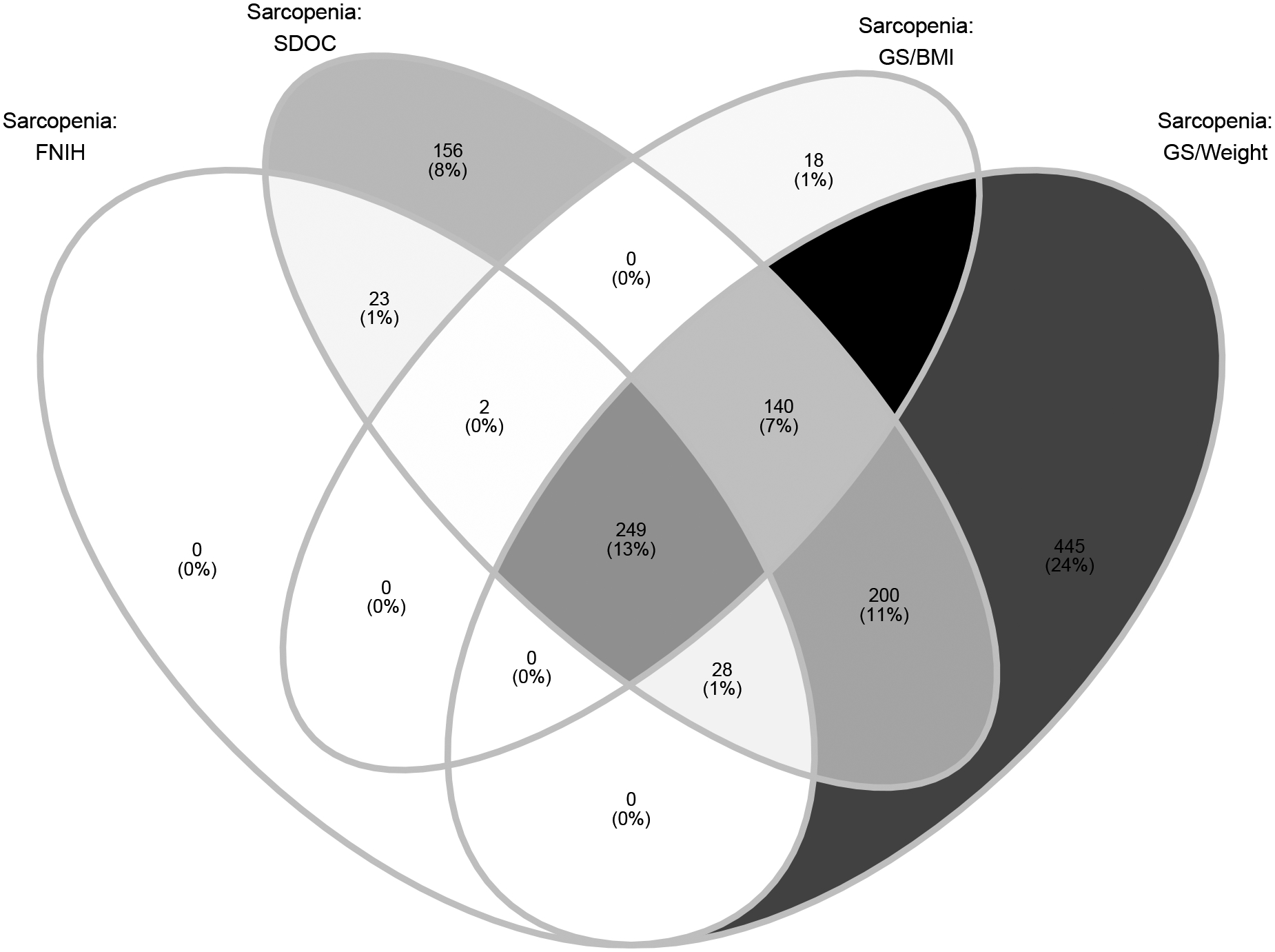
Overlap of food insecurity based on different definitions of sarcopenia
Venn diagram showing the overlap of prevalence of food insecurity in the presence of each analyzed definition of probable sarcopenia.
Table 3:
Univariate and Multivariable Associations of food security by SDOC defined probable sarcopenia status
| Unadjusted | Adjusted | |||
|---|---|---|---|---|
| Prevalence Odds Ratio | p-value | Prevalence Odds Ratio | p-value | |
| Food insecurity * | 1.43 (1.16–1.76) | 0.001 | 1.51 (1.03–2.22) | 0.038 |
| Male sex | 5.67 (4.28–7.5) | <0.001 | 15.34 (9.88–23.81) | <0.001 |
| Age | - | - | - | - |
| 60–69 | Reference | - | Reference | - |
| 70–79 | 2.07 (1.58–2.73) | <0.001 | 2.48 (1.79–3.43) | <0.001 |
| 80+ | 7.02 (5.22–9.42) | <0.001 | 11.84 (7.17–19.53) | <0.001 |
| Marriage status | - | - | - | - |
| Single | Reference | - | Reference | - |
| Widowed, divorced, or separated | 0.61 (0.37–1) | 0.052 | 0.48 (0.26–0.91) | 0.028 |
| Married or living with partner | 0.52 (0.3–0.91) | 0.023 | 0.35 (0.16–0.73) | 0.011 |
| Race/ethnicity | - | - | - | - |
| White | Reference | - | Reference | - |
| Non-Hispanic Black | 0.87 (0.62–1.22) | 0.406 | 0.68 (0.43–1.1) | 0.103 |
| Hispanic | 1.62 (1.22–2.14) | 0.001 | 1.67 (1.1–2.54) | 0.021 |
| Other | 1.8 (1.05–3.08) | 0.034 | 1.85 (1.02–3.35) | 0.045 |
| Education | - | - | - | - |
| ≤12th grade | Reference | - | Reference | - |
| High school graduate/GED | 0.52 (0.35–0.77) | 0.002 | 0.69 (0.43–1.11) | 0.108 |
| Some college or AA degree | 0.44 (0.32–0.61) | <0.001 | 0.78 (0.5–1.21) | 0.231 |
| College graduate or above | 0.55 (0.37–0.82) | 0.005 | 0.94 (0.5–1.76) | 0.814 |
| Income to federal poverty level ratio | 0.8 (0.74–0.86) | <0.001 | 0.83 (0.72–0.95) | 0.013 |
| Body mass index kg/m2 | - | - | - | - |
| 18.5–24.9 | Reference | - | Reference | - |
| <18.5 | 3.3 (1.33–8.18) | 0.012 | 8.71 (1.56–48.75) | 0.02 |
| 25–29.9 | 0.82 (0.61–1.09) | 0.16 | 0.69 (0.45–1.06) | 0.081 |
| ≥30 | 0.62 (0.46–0.84) | 0.003 | 0.7 (0.42–1.17) | 0.147 |
| Diabetes | - | - | - | - |
| No | Reference | - | Reference | - |
| Borderline | 0.86 (0.45–1.62) | 0.623 | 0.91 (0.31–2.71) | 0.854 |
| Yes | 1.59 (1.24–2.05) | 0.001 | 1.71 (1.13–2.58) | 0.018 |
| Smoking Status | - | - | - | - |
| Never smoker | Reference | - | Reference | - |
| Former smoker | 1.24 (1.02–1.49) | 0.029 | 0.71 (0.54–0.94) | 0.022 |
| Current smoker | 0.99 (0.74–1.32) | 0.922 | 0.67 (0.36–1.24) | 0.168 |
| Congestive heart failure | 2.58 (1.69–3.96) | <0.001 | 1.96 (1.14–3.36) | 0.02 |
| Myocardial infarction | 1.84 (1.37–2.47) | <0.001 | 0.72 (0.41–1.25) | 0.205 |
| Stroke | 2.2 (1.49–3.24) | <0.001 | 1.44 (0.98–2.12) | 0.061 |
| Kidney weak or failing | 1.83 (1.26–2.67) | 0.002 | 1 (0.58–1.73) | 0.99 |
Odds ratio for presence of food insecurity in presence of probable sarcopenia for each covariate based on sarcopenia as defined by SDOC cutoffs for grip strength <35.5kg for men and <20kg for women.
referent category is food secure.
DISCUSSION
This study found that in a cohort of older adult in the US, persons with food insecurity had a higher odds of being classified as probable sarcopenia based on standard grip strength cut-offs. This relationship was observed when probable sarcopenia was defined using grip strength cutoffs from both the former FNIH and the more recent SDOC definitions. If replicated in other studies and in different populations these findings may add to our understanding of the substantial public health impact of food insecurity and may highlight areas for future intervention.
Advances in the field of aging biology have demonstrated that sarcopenia is the result of complex underlying myocellular, inflammatory, and hormonal processes, which contribute to body fat redistribution, loss of lean muscle mass, and reduced muscle strength.[22] Translation of these advances into clinical practice has been impeded by an inability to identify and monitor sarcopenia in a cost- and time-efficient manner.[1] Objectively measured sarcopenia definitions using grip strength, while easy to use, are difficult to implement within practice-based settings with high volumes, reduced staff, and little time. This critical gap is broadened by the inability of current diagnostics to capture the heterogeneity within populations of patients with sarcopenia, which prohibits the design of targeted interventions.[23] Recent evidence suggests that malnutrition may contribute to the development of sarcopenia within certain groups of older adults, and additionally food insecurity may increase the risk of malnutrition in this demographic. In contrast to sarcopenia, food insecurity can easily be screened with a simple two-question survey in the clinical setting. This led us to hypothesize that if food insecurity in older adults leads to sarcopenia, screening for food insecurity may help to identify patients at risk for sarcopenia and facilitate the design of targeted nutrition interventions.
Our results suggest that food insecurity may be associated with an increased risk of probable sarcopenia (low grip strength) when using either the SDOC or the FNIH definitions. These definitions rely solely on grip strength and sex-specific cut offs to diagnose sarcopenia. Until recently, total muscle mass was considered an essential component of sarcopenia. Muscle mass is correlated with body size therefore previous definitions of sarcopenia included surrogates of body size such as BMI and weight. Consensus has since shifted to focus on muscle quality and function which in practice is measured as muscle strength. When we adjusted grip strength for BMI (definition 2, appendix 4) and weight (definition 3, appendix 5), there was no positive association with food insecurity. Therefore, the results of our study further support this change in practice and suggest that food insecurity may be associated with decreased muscle strength. We did examine the overlap of each definition of probable sarcopenia with only 13.3% of individuals consistently being defined as having probable sarcopenia or not (Figure 2). This degree of variability could lead to a meaningful number of individuals being misclassified depending on the definition used potentially leading to differential downstream treatment. As many have noted there is a need for global harmonization in the diagnosis and classification of sarcopenia.[5]
Importantly, sarcopenia is a major factor in the development of frailty, characterized by the loss of biological reserves and increased vulnerability to physiological stressors.[24] The burgeoning aging population places increasing numbers at risk for these syndromes and their associated adverse outcomes, including mortality, hospitalization, long-term care admission, loneliness, and reduced quality of life.[25–28] There is limited literature on the relationship between food insecurity and frailty. In one study published in 2013 frail older adults within a population of older adults in the US were more likely to report food insufficiency and lower energy intake than older adults who were not frail.[29] Understanding the relationships between food insecurity, sarcopenia, and frailty could offer targets for interventions to reduce adverse health outcomes in older adults. While our results are not causally related, they may provide insights into socio-behavioral mechanism leading to sarcopenia and frailty.
There are strengths and limitations of this study. Strengths include the size and diversity of the nationally representative sample, and the use of validated metrics to define food insecurity and sarcopenia. However, there are limitations as well. This study only focused on one component of the definition of sarcopenia, muscle strength. The revised European consensus on the definition and diagnosis of sarcopenia recommends a three-step process; 1) identification of probable sarcopenia by assessing muscle strength (e.g. grip strength) 2) confirmation of sarcopenia using measures of muscle quality (e.g. MRI) and 3) assess severity of sarcopenia by measuring it’s impact on function (e.g. 400 m walk).[30] There is a need for further studies that explore the relationship between food insecurity and sarcopenia in cohorts with data that allows for the exploration of the full spectrum of sarcopenia. This study focused on older adults, so whether results generalize to younger populations is not known. In addition, due to the cross-sectional study design, the observed association does not have a causal interpretation. In particular, reverse causality is possible - inadequate nutrition due to food insecurity could lead to sarcopenia or sarcopenia may lead to food insecurity through a decreased ability to obtain food for oneself. However, even if sarcopenia was the initial cause of food insecurity, given the relationship between food insecurity and nutrition, it is unlikely that sarcopenia will improve in the presence of food insecurity. This argues for addressing food insecurity among those with sarcopenia.
Findings in this study have potential implications for future research, clinical practice, and public health policy. As the population ages, geriatric syndromes such as sarcopenia and frailty will impose an even greater burden on the healthcare system. Translation of frailty and sarcopenia research into clinical practice has been slow due to difficulties with diagnosis and a lack of treatment options. The findings in this study suggest that screening for food insecurity may uncover a patient population at higher risk of probable sarcopenia (low grip strength), while also identifying a pathway for treatment to prevent future adverse events and incident disability. Specifically, we can impact food insecurity in older adults through increased services such as meals on wheels and helping older adults receive the nutrition that they need.[31,32] While nutrition and exercise interventions are the mainstay of sarcopenia prevention and treatment, additional evaluations are needed to determine the effectiveness of these strategies, particularly as they are related to the further development of frailty syndromes.
Funding:
Dr. Batsis’ has had his research supported in part by the National Institute on Aging and Office of Dietary Supplements of the National Institutes of Health under Award Number K23AG051681 and R01AG067416. Dr. Batsis also has equity in SynchroHealth LLC, a remote monitoring company. Mr. Petersen was supported by the Burroughs-Welcome Fund: Big Data in the Life Sciences at Dartmouth Dr Berkowitz reported receiving grants from the National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health and Blue Cross Blue Shield of North Carolina, and personal fees from the Aspen Institute and Rockefeller Foundation, outside the submitted work.
ABBREVIATIONS
- BMI
Body Mass Index
- CDC
Centers for Disease Control
- CSFP
Commodity Supplemental Food Program
- FNIH
Foundation for the National Institute of Health
- FSSM
Food Security Survey Module
- NCHS
National Center for Health Statistics
- NHANES
National Health and Nutrition Examination Surveys
- SDOC
Sarcopenia Definitions and Outcomes consortium
- SNAP
Supplemental Nutrition Assistance Program
- WIC
Special Supplemental Nutrition Program for Women, Infants, and Children
Appendix 1: Definitions of Probable Sarcopenia
| Definition | Probable Sarcopenia | |
|---|---|---|
| 1. | SDOC grip strength | Grip strength <35.5kg for men and <20kg for women |
| 2. | SDOC grip strength / BMI | Grip strength divided by body mass index <1.05 for men and <0.79 for women |
| 3. | SDOC grip strength / weight | Grip strength divided by body weight <0.45 for men and <0.34 for women |
| 4. | FNIH grip strength | Grip strength <26kg for men and <16kg for women |
FNIH- Foundation for the National Institute of Health. SDOC- Sarcopenia Definitions and Outcomes consortium.
Appendix 2: Participant Characteristics By Probable Sarcopenia Definition 2 (BMI)
| No Probable Sarcopenia | Probable Sarcopenia | p-value | |
|---|---|---|---|
| N = 1,859 | N = 922 | ||
| Age | 68.32 (67.88–68.75) | 71.65 (70.93–72.36) | <0.001 |
| Sex | - | - | <0.001 |
| Female | 759 (44.4) | 654 (75.7) | - |
| Male | 1100 (55.6) | 268 (24.3) | - |
| Race | - | - | <0.001 |
| Non-Hispanic White | 875 (80.5) | 459 (76.4) | - |
| Non-Hispanic Black | 481 (8.4) | 193 (9) | - |
| Hispanic | 300 (5.7) | 209 (10) | - |
| Other | 203 (5.4) | 61 (4.6) | - |
| Education | - | - | <0.001 |
| ≤12th grade | 443 (14.6) | 315 (23.7) | - |
| High school graduate/GED | 414 (19.4) | 231 (26.8) | - |
| Some college or AA degree | 524 (31.6) | 240 (30.4) | - |
| College graduate or above | 478 (34.4) | 136 (19.1) | - |
| Income Federal Poverty Level | 3.31 (3.16–3.46) | 2.5 (2.3–2.7) | <0.001 |
| Marital Status | - | - | <0.001 |
| Single | 108 (4.2) | 52 (4.4) | - |
| Widowed, divorced, or separated | 586 (25.4) | 455 (45.3) | - |
| Married or living with partner | 1165 (70.4) | 415 (50.3) | - |
| Smoking Status | - | - | 0.002 |
| Never smoker | 837 (46.2) | 530 (55.7) | - |
| Former smoker | 733 (40.9) | 324 (36.7) | - |
| Current smoker | 289 (12.9) | 68 (7.6) | - |
| Body Mass Index | 27.18 (26.79–27.57) | 33.34 (32.34–34.35) | <0.001 |
| Kidney Condition | 81 (3.6) | 83 (7) | <0.001 |
| Diabetes | - | - | <0.001 |
| Borderline | 83 (4.4) | 44 (4.2) | - |
| Yes | 351 (14.5) | 313 (31.5) | - |
| Congestive heart failure | 93 (4.5) | 119 (13.7) | <0.001 |
| Myocardial infarction | 153 (8.1) | 103 (10.7) | 0.07 |
| Stroke | 104 (4.4) | 114 (12) | <0.001 |
| Food insecurity | 337 (10.6) | 251 (18.6) | <0.001 |
Participant characteristics stratified by presence of probable sarcopenia as defined by SDOC cutoffs for grip strength divided by BMI <1.05 for men and <0.79 for women.
n: respondent counts
%: all percentages are weighted using NHANES defined weighting method
CI: confidence intervals are weighted using NHANES defined weighting method
mean: all means are weighted using NHANES defined weighting method
Appendix 3: Participant Characteristics By Probable Sarcopenia Definition 3 (Weight)
| No Sarcopenia | Sarcopenia | p-value | |
|---|---|---|---|
| N = 1,256 | N = 1,525 | ||
| Age | 67.79 (67.18–68.39) | 70.62 (70.09–71.14) | <0.001 |
| Sex | - | - | 0.12 |
| Female | 598 (51.3) | 815 (56) | - |
| Male | 658 (48.7) | 710 (44) | - |
| Race | - | - | 0.006 |
| Non-Hispanic White | 529 (78) | 805 (80.3) | - |
| Non-Hispanic Black | 332 (9) | 342 (8.3) | - |
| Hispanic | 220 (6.5) | 289 (7.5) | - |
| Other | 175 (6.5) | 89 (3.9) | - |
| Education | - | - | 0.01 |
| ≤12th grade | 318 (15.3) | 440 (19) | - |
| High school graduate/GED | 280 (20) | 365 (23) | - |
| Some college or AA degree | 337 (30.1) | 427 (32.2) | - |
| College graduate or above | 321 (34.5) | 293 (25.8) | - |
| Income Federal Poverty Level | 3.28 (3.07–3.49) | 2.89 (2.74–3.04) | <0.001 |
| Marital Status | - | - | 0.001 |
| Single | 82 (4.5) | 78 (4) | - |
| Widowed, divorced, or separated | 419 (26.2) | 622 (35.8) | - |
| Married or living with partner | 755 (69.3) | 825 (60.2) | - |
| Smoking Status | - | - | 0.008 |
| Never smoker | 588 (48.6) | 779 (49.5) | - |
| Former smoker | 450 (36.7) | 607 (42) | - |
| Current smoker | 218 (14.7) | 139 (8.5) | - |
| Body Mass Index | 25.54 (25.19–25.89) | 31.98 (31.34–32.63) | <0.001 |
| Kidney Condition | 58 (3.8) | 106 (5.3) | 0.11 |
| Diabetes | - | - | <0.001 |
| Borderline | 51 (3.6) | 76 (4.9) | - |
| Yes | 198 (10.8) | 466 (27) | -- |
| Congestive heart failure | 42 (3.4) | 170 (10.5) | <0.001 |
| Myocardial infarction | 83 (6.2) | 173 (11.1) | <0.001 |
| Stroke | 67 (4.4) | 151 (8.7) | <0.001 |
| Food insecurity | 67.79 (67.18–68.39) | 70.62 (70.09–71.14) | <0.001 |
Participant characteristics stratified by presence of probable sarcopenia as defined by SDOC cutoffs for grip strength divided by weight <0.45 for men and <0.34 for women.
n: respondent counts
%: all percentages are weighted using NHANES defined weighting method
CI: confidence intervals are weighted using NHANES defined weighting method
mean: all means are weighted using NHANES defined weighting method
Appendix 4: Participant Characteristics By Probable Sarcopenia Definition 4 (FNIH)
| No Sarcopenia | Sarcopenia | p-value | |
|---|---|---|---|
| N = 2,532 | N = 249 | ||
| Age | 68.84 (68.44–69.23) | 76.34 (75.6–77.09) | <0.001 |
| Sex | - | - | 0.10 |
| Female | 1292 (53.4) | 121 (60.7) | - |
| Male | 1240 (46.6) | 128 (39.3) | - |
| Race | - | - | 0.14 |
| Non-Hispanic White | 1206 (79.6) | 128 (74.1) | - |
| Non-Hispanic Black | 625 (8.5) | 49 (9.8) | - |
| Hispanic | 462 (6.8) | 47 (10.2) | - |
| Other | 239 (5.1) | 25 (5.9) | - |
| Education | - | - | <0.001 |
| ≤12th grade | 651 (16.3) | 107 (32.1) | - |
| High school graduate/GED | 585 (21.4) | 60 (24.8) | - |
| Some college or AA degree | 719 (31.7) | 45 (24.6) | - |
| College graduate or above | 577 (30.5) | 37 (18.5) | - |
| Income Federal Poverty Level | 3.12 (2.96–3.28) | 2.28 (2.02–2.55) | <0.001 |
| Marital Status | - | - | <0.001 |
| Single | 140 (4.1) | 20 (6.6) | - |
| Widowed, divorced, or separated | 918 (30.2) | 123 (49.3) | - |
| Married or living with partner | 1474 (65.8) | 106 (44.1) | - |
| Smoking Status | - | - | 0.21 |
| Never smoker | 1239 (48.7) | 128 (54.5) | - |
| Former smoker | 968 (39.9) | 89 (35.5) | - |
| Current smoker | 325 (11.4) | 32 (10) | - |
| Body Mass Index | 29.16 (28.7–29.63) | 27.26 (26.04–28.49) | 0.001 |
| Kidney Condition | 137 (4.1) | 27 (11.2) | <0.001 |
| Diabetes | - | - | <0.001 |
| Borderline | 117 (4.5) | 10 (2.5) | - |
| Yes | 578 (18.8) | 86 (31.2) | - |
| Congestive heart failure | 175 (6.7) | 37 (15.9) | <0.001 |
| Myocardial infarction | 222 (8.6) | 34 (13.1) | <0.001 |
| Stroke | 175 (6.1) | 43 (15.7) | <0.001 |
| Food insecurity | 520 (12.4) | 68 (21.4) | <0.001 |
Participant characteristics stratified by presence of probable sarcopenia as defined by FNIH defined grip strength <26kg for men and <16kg for women.
n: respondent counts
%: all percentages are weighted using NHANES defined weighting method
CI: confidence intervals are weighted using NHANES defined weighting method
mean: all means are weighted using NHANES defined weighting
Appendix 5: Associations For All Food Security Levels and Sarcopenia SDOC Definition
| Full | Marginal | Low | Very low | p-value | |
|---|---|---|---|---|---|
| Age n (%) | - | - | - | - | 0.01 |
| 60–69 | 1064 (54.9) | 134 (58.1) | 128 (57.6) | 84 (68.3) | - |
| 70–79 | 652 (29.4) | 58 (31.2) | 71 (34.3) | 26 (23.8) | - |
| 80+ | 414 (15.6) | 24 (10.7) | 20 (8.1) | 10 (7.9) | - |
| Sex n (%) | - | - | - | - | 0.006 |
| Female | 1056 (52.9) | 122 (62) | 128 (62.6) | 62 (53.3) | - |
| Male | 1074 (47.1) | 94 (38) | 91 (37.4) | 58 (46.7) | - |
| Race n (%) | - | - | - | - | <0.001 |
| Non-Hispanic White | 1140 (83) | 73 (61.7) | 53 (52.4) | 34 (54.9) | - |
| Non-Hispanic Black | 456 (6.8) | 76 (19.4) | 73 (20.1) | 39 (18.1) | - |
| Hispanic | 313 (5.1) | 50 (13.9) | 84 (24.7) | 41 (21.2) | - |
| Other | 221 (5.1) | 17 (5) | 9 (2.8) | 6 (5.9) | - |
| Education n (%) | - | - | - | - | <0.001 |
| ≤12th grade | 481 (13.8) | 83 (34.1) | 106 (45.7) | 54 (40.4) | - |
| High school graduate/GED | 473 (21.1) | 58 (20.9) | 61 (30.4) | 30 (26.4) | - |
| Some college or AA degree | 608 (31.8) | 59 (34) | 42 (20.8) | 28 (21.5) | - |
| College graduate or above | 568 (33.3) | 16 (11) | 10 (3.1) | 8 (11.7) | - |
| Income Federal Poverty Level n (%) | - | - | - | - | 0.01 |
| ≤1 | 246 (6.1) | 85 (32.5) | 89 (37.6) | 65 (43.2) | - |
| 1–2 | 585 (21) | 87 (42.5) | 89 (43) | 43 (39.5) | - |
| >2 | 1299 (72.9) | 44 (25) | 41 (19.4) | 12 (17.3) | - |
| Marital Status n (%) | - | - | - | - | <0.001 |
| Single | 110 (4.1) | 15 (4.3) | 16 (4.8) | 14 (7.4) | - |
| Widowed, divorced, or separated | 732 (28.3) | 103 (50.4) | 103 (49.8) | 61 (51.7) | - |
| Married or living with partner | 1288 (67.7) | 98 (45.3) | 100 (45.4) | 45 (40.9) | - |
| Smoking Status n (%) | - | - | - | - | 0.01 |
| Never smoker | 1075 (50.3) | 88 (37.4) | 96 (42.5) | 58 (41.8) | - |
| Former smoker | 827 (40.1) | 87 (42.3) | 80 (37.8) | 29 (28.3) | - |
| Current smoker | 228 (9.6) | 41 (20.3) | 43 (19.7) | 33 (29.9) | - |
| Body Mass Index n (%) | - | - | - | - | 0.21 |
| <18.5 | 29 (1.2) | 4 (2.7) | 4 (1) | 4 (2.8) | - |
| 18.5–24.9 | 575 (25.8) | 48 (18.4) | 45 (21.1) | 25 (21.9) | - |
| 25–29.9 | 759 (36.4) | 70 (35.1) | 69 (28.5) | 40 (31.2) | - |
| ≥30 | 767 (36.5) | 94 (43.9) | 101 (49.4) | 51 (44.1) | - |
| Diabetes n (%) | - | - | - | - | <0.001 |
| No | 1580 (78.2) | 134 (64.4) | 149 (67.8) | 71 (56.9) | - |
| Borderline | 95 (4.3) | 12 (5.1) | 10 (3.4) | 8 (4.2) | - |
| Yes | 455 (17.4) | 70 (30.5) | 60 (28.8) | 41 (38.9) | - |
| Congestive heart failure n (%) | 151 (6.8) | 17 (6.6) | 19 (10.2) | 16 (15.3) | 0.17 |
| Myocardial infarction n (%) | 186 (8.3) | 16 (6.4) | 28 (16.1) | 19 (17) | 0.06 |
| Stroke n (%) | 154 (5.9) | 16 (11) | 26 (12.8) | 10 (10.3) | 0.03 |
| Kidney Condition n (%) | 111 (3.9) | 13 (6) | 21 (10.3) | 10 (12.8) | 0.007 |
| Food security n (%) | - | - | - | - | 0.05 |
| No Sarcopenia | 1614 (82.1) | 165 (78.2) | 162 (77) | 93 (76.3) | - |
| Sarcopenia | 516 (17.9) | 51 (21.8) | 57 (23) | 27 (23.7) | - |
Food insecurity was assessed through the 10-item Food Security Survey Module. Marginal food security (1–2 affirmative responses), low food security (3–5 affirmative responses), and very low food security (6–10 affirmative 3 responses).
n: respondent counts
%: all percentages are weighted using NHANES defined weighting method
CI: confidence intervals are weighted using NHANES defined weighting method
mean: all means are weighted using NHANES defined weighting method
Appendix 6: Univariate and Multivariable Associations of food security and severity of food insecurity by SDOC defined sarcopenia status
| Unadjusted | Adjusted | |||
|---|---|---|---|---|
| Prevalence Odds Ratio | p-value | Prevalence Odds Ratio | p-value | |
| Food insecurity levels | ||||
| Full food security | Reference | - | Reference | - |
| Marginal food security | 1.39 (0.97–2.00) | 0.073 | 1.40 (0.85–2.32) | 0.153 |
| Low food security | 1.48 (1.10–2.00) | 0.012 | 1.78 (1.07–2.96) | 0.033 |
| Very low food security | 1.40 (0.71–2.75) | 0.321 | 1.33 (0.47–3.74) | 0.531 |
| Male sex | 5.67 (4.28–7.50) | <0.001 | 15.39 (9.69–24.43) | <0.001 |
| Age | - | - | - | - |
| 60–69 | Reference | - | Reference | - |
| 70–79 | 2.07 (1.58–2.73) | <0.001 | 2.48 (1.75–3.51) | 0.001 |
| 80+ | 7.02 (5.22–9.42) | <0.001 | 11.86 (6.94–20.24) | <0.001 |
| Marriage status | - | - | - | - |
| Single | Reference | - | Reference | - |
| Widowed, divorced, or separated | 0.61 (0.37–1.00) | 0.052 | 0.48 (0.25–0.94) | 0.036 |
| Married or living with partner | 0.52 (0.30–0.91) | 0.023 | 0.35 (0.16–0.76) | 0.016 |
| Race/ethnicity | - | - | - | - |
| White | Reference | - | Reference | - |
| Non-Hispanic Black | 0.87 (0.62–1.22) | 0.406 | 0.68 (0.41–1.13) | 0.115 |
| Hispanic | 1.62 (1.22–2.14) | 0.001 | 1.66 (1.07–2.58) | 0.03 |
| Other | 1.80 (1.05–3.08) | 0.034 | 1.85 (0.98–3.49) | 0.056 |
| Education | - | - | - | - |
| ≤12th grade | Reference | - | Reference | - |
| High school graduate/GED | 0.52 (0.35–0.77) | 0.002 | 0.69 (0.42–1.14) | 0.123 |
| Some college or AA degree | 0.44 (0.32–0.61) | <0.001 | 0.79 (0.49–1.25) | 0.253 |
| College graduate or above | 0.55 (0.37–0.82) | 0.005 | 0.94 (0.48–1.85) | 0.833 |
| Income to federal poverty level ratio | 0.72 (0.67–0.77) | <0.001 | 0.84 (0.72–0.97) | 0.025 |
| Body mass index kg/m2 | - | - | - | - |
| 18.5–24.9 | Reference | - | Reference | - |
| <18.5 | 3.30 (1.33–8.18) | 0.012 | 8.76 (1.42–53.96) | 0.027 |
| 25–29.9 | 0.82 (0.61–1.09) | 0.16 | 0.69 (0.44–1.09) | 0.093 |
| ≥30 | 0.62 (0.46–0.84) | 0.003 | 0.70 (0.40–1.21) | 0.16 |
| Diabetes | - | - | - | - |
| No | Reference | - | Reference | - |
| Borderline | 0.86 (0.45–1.62) | 0.623 | 0.92 (0.29–2.88) | 0.858 |
| Yes | 1.59 (1.24–2.05) | 0.001 | 1.72 (1.10–2.69) | 0.025 |
| Smoking Status | - | - | - | - |
| Never smoker | Reference | - | Reference | - |
| Former smoker | 1.24 (1.02–1.49) | 0.029 | 0.71 (0.53–0.96) | 0.032 |
| Current smoker | 0.99 (0.74–1.32) | 0.922 | 0.67 (0.35–1.29) | 0.186 |
| Congestive heart failure | 2.58 (1.69–3.96) | <0.001 | 1.98 (1.12–3.47) | 0.026 |
| Myocardial infarction | 1.84 (1.37–2.47) | <0.001 | 0.71 (0.40–1.28) | 0.209 |
| Stroke | 2.20 (1.49–3.24) | <0.001 | 1.44 (0.95–2.17) | 0.075 |
| Kidney weak or failing | 1.83 (1.26–2.67) | 0.002 | 1.00 (0.56–1.78) | 0.997 |
Participant characteristics stratified by presence of probable sarcopenia as defined by SDOC cutoffs for grip strength <35.5kg for men and <20kg for women.
n: respondent counts
All values represented are weighted means (95% CI) or unweighted counts (weighted %)
Appendix 7: Unadjusted and adjusted odds ratios for food security by probable sarcopenia status Definition 2 (BMI)
| Unadjusted | Adjusted | |||
|---|---|---|---|---|
| Prevalence Odds Ratio | p-value | Prevalence Odds Ratio | p-value | |
| Food insecurity | 1.91 (1.48–2.46) | <0.001 | 1.71 (1.08–2.71) | 0.027 |
| Male sex | 0.74 (0.54–1.03) | 0.074 | 1.1 (0.72–1.7) | 0.614 |
| Age | - | - | - | - |
| 60–69 | Reference | - | Reference | - |
| 70–79 | 4.34 (2.67–7.07) | <0.001 | 3.98 (2.37–6.69) | <0.001 |
| 80+ | 21.89 (14.61–32.81) | <0.001 | 18.91 (10.49–34.11) | <0.001 |
| Marriage status | - | - | - | - |
| Single | Reference | - | Reference | - |
| Widowed, divorced, or separated | 1.05 (0.54–2.02) | 0.883 | 0.51 (0.22–1.15) | 0.091 |
| Married or living with partner | 0.37 (0.18–0.76) | 0.009 | 0.4 (0.15–1.06) | 0.061 |
| Race/ethnicity | - | - | - | - |
| White | Reference | - | Reference | - |
| Non-Hispanic Black | 1.13 (0.7–1.83) | 0.602 | 1.01 (0.53–1.89) | 0.983 |
| Hispanic | 1.51 (1.09–2.1) | 0.015 | 1.56 (0.97–2.53) | 0.063 |
| Other | 1.34 (0.78–2.32) | 0.277 | 1.34 (0.61–2.95) | 0.42 |
| Education | - | - | - | - |
| ≤12th grade | Reference | - | Reference | - |
| High school graduate/GED | 0.51 (0.33–0.8) | 0.005 | 0.86 (0.49–1.53) | 0.574 |
| Some college or AA degree | 0.44 (0.29–0.67) | <0.001 | 0.84 (0.49–1.45) | 0.485 |
| College graduate or above | 0.33 (0.21–0.52) | <0.001 | 0.79 (0.41–1.52) | 0.435 |
| Income to federal poverty level ratio | 0.69 (0.62–0.78) | <0.001 | 0.89 (0.73–1.08) | 0.203 |
| Body mass index kg/m2 | - | - | - | - |
| 18.5–24.9 | Reference | - | Reference | - |
| <18.5 | 4.59 (1.83–11.52) | 0.002 | 5.64 (1.3–24.52) | 0.026 |
| 25–29.9 | 0.64 (0.44–0.92) | 0.019 | 0.65 (0.41–1.03) | 0.064 |
| ≥30 | 0.58 (0.38–0.88) | 0.012 | 0.76 (0.44–1.3) | 0.271 |
| Diabetes | - | - | - | - |
| No | Reference | - | Reference | - |
| Borderline | 0.62 (0.31–1.25) | 0.174 | 0.6 (0.19–1.95) | 0.347 |
| Yes | 1.78 (1.35–2.35) | <0.001 | 1.82 (1.15–2.9) | 0.017 |
| Smoking Status | - | - | - | - |
| Never smoker | Reference | - | Reference | - |
| Former smoker | 0.77 (0.56–1.06) | 0.106 | 0.76 (0.55–1.05) | 0.088 |
| Current smoker | 0.72 (0.48–1.09) | 0.114 | 1.05 (0.43–2.57) | 0.895 |
| Congestive heart failure | 2.72 (1.6–4.62) | 0.001 | 1.47 (0.73–2.97) | 0.238 |
| Myocardial infarction | 1.85 (1.35–2.53) | <0.001 | 0.81 (0.47–1.38) | 0.381 |
| Stroke | 3.11 (2.05–4.69) | <0.001 | 1.47 (0.87–2.47) | 0.126 |
| Kidney weak or failing | 2.59 (1.47–4.57) | 0.002 | 1.6 (0.69–3.7) | 0.234 |
Odds ratio for presence of food insecurity in presence of sarcopenia for each covariate based on sarcopenia as defined by SDOC cutoffs for grip strength divided by weight <0.45 for men and <0.34 for women
Appendix 8: Unadjusted and adjusted odds ratios for food security by sarcopenia status Definition 3 (Weight)
| Unadjusted | Adjusted | |||
|---|---|---|---|---|
| Prevalence Odds Ratio | p-value | Prevalence Odds Ratio | p-value | |
| Food insecurity | 1.37 (1.09–1.72) | 0.008 | 1.14 (0.85–1.54) | 0.336 |
| Male sex | 0.84 (0.66–1.06) | 0.137 | 0.87 (0.59–1.27) | 0.417 |
| Age | - | - | - | - |
| 60–69 | Reference | - | Reference | - |
| 70–79 | 1.84 (1.42–2.38) | <0.001 | 2.58 (1.85–3.6) | <0.001 |
| 80+ | 3.21 (2.29–4.52) | <0.001 | 7.2 (4.36–11.86) | <0.001 |
| Marriage status | - | - | - | - |
| Single | Reference | - | Reference | - |
| Widowed, divorced, or separated | 1.53 (0.97–2.4) | 0.064 | 1.1 (0.49–2.49) | 0.797 |
| Married or living with partner | 1 (0.64–1.56) | 0.992 | 0.93 (0.43–2.03) | 0.846 |
| Race/ethnicity | - | - | - | - |
| White | Reference | - | Reference | - |
| Non-Hispanic Black | 0.89 (0.74–1.07) | 0.204 | 0.55 (0.39–0.77) | 0.003 |
| Hispanic | 1.11 (0.92–1.34) | 0.267 | 0.96 (0.67–1.38) | 0.812 |
| Other | 0.58 (0.41–0.81) | 0.003 | 0.82 (0.52–1.29) | 0.337 |
| Education | - | - | - | - |
| ≤12th grade | Reference | - | Reference | - |
| High school graduate/GED | 0.86 (0.65–1.15) | 0.293 | 1.13 (0.73–1.73) | 0.541 |
| Some college or AA degree | 0.85 (0.65–1.11) | 0.213 | 1.01 (0.7–1.45) | 0.961 |
| College graduate or above | 0.59 (0.42–0.82) | 0.003 | 1.05 (0.66–1.67) | 0.806 |
| Income to federal poverty level ratio | 0.85 (0.79–0.92) | <0.001 | 0.95 (0.86–1.05) | 0.282 |
| Body mass index kg/m2 | - | - | - | - |
| 18.5–24.9 | Reference | - | Reference | - |
| <18.5 | 0.92 (0.33–2.56) | 0.867 | 0.81 (0.21–3.2) | 0.737 |
| 25–29.9 | 3.05 (2.15–4.31) | <0.001 | 4.13 (2.67–6.38) | <0.001 |
| ≥30 | 18.39 (12.91–26.2) | <0.001 | 32.13 (20.76–49.73) | <0.001 |
| Diabetes | - | - | - | - |
| No | Reference | - | Reference | - |
| Borderline | 1.73 (1.02–2.94) | 0.044 | 1.48 (0.73–3.02) | 0.237 |
| Yes | 3.16 (2.47–4.04) | <0.001 | 2.14 (1.54–2.98) | 0.001 |
| Smoking Status | - | - | - | - |
| Never smoker | Reference | - | Reference | - |
| Former smoker | 1.1 (0.86–1.39) | 0.442 | 0.9 (0.63–1.3) | 0.53 |
| Current smoker | 0.56 (0.35–0.89) | 0.016 | 0.9 (0.53–1.53) | 0.649 |
| Congestive heart failure | 3.36 (2.18–5.16) | <0.001 | 1.89 (1.12–3.21) | 0.024 |
| Myocardial infarction | 1.84 (1.35–2.52) | <0.001 | 1.05 (0.56–1.96) | 0.872 |
| Stroke | 2.2 (1.6–3.02) | <0.001 | 1.68 (1.06–2.66) | 0.033 |
| Kidney weak or failing | 1.67 (1.06–2.61) | 0.027 | 0.87 (0.38–1.98) | 0.702 |
Odds ratio for presence of food insecurity in presence of sarcopenia for each covariate based on sarcopenia as defined by SDOC cutoffs for grip strength divided by weight <0.45 for men and <0.34 for women.
Appendix 9: Unadjusted and adjusted odds ratios for food security by sarcopenia status Definition 4 (FNIH)
| Unadjusted | Adjusted | |||
|---|---|---|---|---|
| Prevalence Odds Ratio | p-value | Prevalence Odds Ratio | p-value | |
| Food insecurity | 1.91 (1.48–2.46) | <0.001 | 1.71 (1.08–2.71) | 0.027 |
| Male sex | 0.74 (0.54–1.03) | 0.074 | 1.1 (0.72–1.7) | 0.614 |
| Age | - | - | - | - |
| 60–69 | Reference | - | Reference | - |
| 70–79 | 4.34 (2.67–7.07) | <0.001 | 3.98 (2.37–6.69) | <0.001 |
| 80+ | 21.89 (14.61–32.81) | <0.001 | 18.91 (10.49–34.11) | <0.001 |
| Marriage status | - | - | - | - |
| Single | Reference | - | Reference | - |
| Widowed, divorced, or separated | 1.05 (0.54–2.02) | 0.883 | 0.51 (0.22–1.15) | 0.091 |
| Married or living with partner | 0.37 (0.18–0.76) | 0.009 | 0.4 (0.15–1.06) | 0.061 |
| Race/ethnicity | - | - | - | - |
| White | Reference | - | Reference | - |
| Non-Hispanic Black | 1.13 (0.7–1.83) | 0.602 | 1.01 (0.53–1.89) | 0.983 |
| Hispanic | 1.51 (1.09–2.1) | 0.015 | 1.56 (0.97–2.53) | 0.063 |
| Other | 1.34 (0.78–2.32) | 0.277 | 1.34 (0.61–2.95) | 0.42 |
| Education | - | - | - | - |
| ≤12th grade | Reference | - | Reference | - |
| High school graduate/GED | 0.51 (0.33–0.8) | 0.005 | 0.86 (0.49–1.53) | 0.574 |
| Some college or AA degree | 0.44 (0.29–0.67) | <0.001 | 0.84 (0.49–1.45) | 0.485 |
| College graduate or above | 0.33 (0.21–0.52) | <0.001 | 0.79 (0.41–1.52) | 0.435 |
| Income to federal poverty level ratio | 0.69 (0.62–0.78) | <0.001 | 0.89 (0.73–1.08) | 0.203 |
| Body mass index kg/m2 | - | - | - | - |
| 18.5–24.9 | Reference | - | Reference | - |
| <18.5 | 4.59 (1.83–11.52) | 0.002 | 5.64 (1.3–24.52) | 0.026 |
| 25–29.9 | 0.64 (0.44–0.92) | 0.019 | 0.65 (0.41–1.03) | 0.064 |
| ≥30 | 0.58 (0.38–0.88) | 0.012 | 0.76 (0.44–1.3) | 0.271 |
| Diabetes | - | - | - | - |
| No | Reference | - | Reference | - |
| Borderline | 0.62 (0.31–1.25) | 0.174 | 0.6 (0.19–1.95) | 0.347 |
| Yes | 1.78 (1.35–2.35) | <0.001 | 1.82 (1.15–2.9) | 0.017 |
| Smoking Status | - | - | - | - |
| Never smoker | Reference | - | Reference | - |
| Former smoker | 0.77 (0.56–1.06) | 0.106 | 0.76 (0.55–1.05) | 0.088 |
| Current smoker | 0.72 (0.48–1.09) | 0.114 | 1.05 (0.43–2.57) | 0.895 |
| Congestive heart failure | 2.72 (1.6–4.62) | 0.001 | 1.47 (0.73–2.97) | 0.238 |
| Myocardial infarction | 1.85 (1.35–2.53) | <0.001 | 0.81 (0.47–1.38) | 0.381 |
| Stroke | 3.11 (2.05–4.69) | <0.001 | 1.47 (0.87–2.47) | 0.126 |
| Kidney weak or failing | 2.59 (1.47–4.57) | 0.002 | 1.6 (0.69–3.7) | 0.234 |
Odds ratio for presence of food insecurity in presence of probable sarcopenia for each covariate based on sarcopenia as defined by FNIH defined grip strength <26kg for men and <16kg for women.
Footnotes
Ethics approval to consent to participate: This study was deemed to be non-human subjects research by the University of North Carolina at Chapel Hill (#20-3138.) Informed consent was obtained by all participants in this study in a written manner by the NHANES survey.
Competing interests: None
Availability of data and materials:
The datasets generated and/or analyzed during the current study are publicly available on the NHANES website.
REFERENCES
- [1].Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyère O, Cederholm T, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age and Ageing 2019;48:16–31. 10.1093/AGEING/AFY169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].de Buyser SL, Petrovic M, Taes YE, Toye KRC, Kaufman JM, Lapauw B, et al. Validation of the FNIH sarcopenia criteria and SOF frailty index as predictors of long-term mortality in ambulatory older men. Age Ageing 2016;45:603–9. 10.1093/AGEING/AFW071. [DOI] [PubMed] [Google Scholar]
- [3].Morley JE, Abbatecola AM, Argiles JM, Baracos V, Bauer J, Bhasin S, et al. Sarcopenia with limited mobility: an international consensus. J Am Med Dir Assoc 2011;12:403–9. 10.1016/J.JAMDA.2011.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Bischoff-Ferrari HA, Orav JE, Kanis JA, Rizzoli R, Schlögl M, Staehelin HB, et al. Comparative performance of current definitions of sarcopenia against the prospective incidence of falls among community-dwelling seniors age 65 and older. Osteoporos Int 2015;26:2793–802. 10.1007/S00198-015-3194-Y. [DOI] [PubMed] [Google Scholar]
- [5].Cruz-Jentoft AJ, Sayer AA. Sarcopenia. Lancet 2019;393:2636–46. 10.1016/S0140-6736(19)31138-9. [DOI] [PubMed] [Google Scholar]
- [6].Dent E, Morley JE, Cruz-Jentoft AJ, Arai H, Kritchevsky SB, Guralnik J, et al. International Clinical Practice Guidelines for Sarcopenia (ICFSR): Screening, Diagnosis and Management. Journal of Nutrition, Health and Aging 2018;22:1148–61. 10.1007/S12603-018-1139-9. [DOI] [PubMed] [Google Scholar]
- [7].Sieber CC. Malnutrition and sarcopenia. Aging Clin Exp Res 2019;31. 10.1007/S40520-019-01170-1. [DOI] [PubMed] [Google Scholar]
- [8].Cederholm T, Jensen GL, Correia MITD, Gonzalez MC, Fukushima R, Higashiguchi T, et al. GLIM criteria for the diagnosis of malnutrition - A consensus report from the global clinical nutrition community. Clin Nutr 2019;38:1–9. 10.1016/J.CLNU.2018.08.002. [DOI] [PubMed] [Google Scholar]
- [9].Ligthart-Melis GC, Luiking YC, Kakourou A, Cederholm T, Maier AB, de van der Schueren MAE. Frailty, Sarcopenia, and Malnutrition Frequently (Co-)occur in Hospitalized Older Adults: A Systematic Review and Meta-analysis. J Am Med Dir Assoc 2020;21:1216–28. 10.1016/J.JAMDA.2020.03.006. [DOI] [PubMed] [Google Scholar]
- [10].Liguori I, Curcio F, Russo G, Cellurale M, Aran L, Bulli G, et al. Risk of Malnutrition Evaluated by Mini Nutritional Assessment and Sarcopenia in Noninstitutionalized Elderly People. Nutr Clin Pract 2018;33:879–86. 10.1002/NCP.10022. [DOI] [PubMed] [Google Scholar]
- [11].Kaiser MJ, Bauer JM, Ramsch C, Uter W, Guigoz Y, Cederholm T, et al. Validation of the Mini Nutritional Assessment short-form (MNA®-SF): A practical tool for identification of nutritional status. JNHA - The Journal of Nutrition, Health and Aging 2009 13:9 2009;13:782–8. 10.1007/S12603-009-0214-7. [DOI] [PubMed] [Google Scholar]
- [12].Corish CA, Bardon LA. Malnutrition in older adults: screening and determinants. Proc Nutr Soc 2019;78:372–9. 10.1017/S0029665118002628. [DOI] [PubMed] [Google Scholar]
- [13].Pereira MHQ, Pereira MLAS, Campos GC, Molina MCB. Food insecurity and nutritional status among older adults: a systematic review. Nutrition Reviews 2022;80:631–44. 10.1093/NUTRIT/NUAB044. [DOI] [PubMed] [Google Scholar]
- [14].USDA ERS - Food Security in the U.S n.d. https://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-us/ (accessed November 20, 2021).
- [15].Coleman-Jensen A, Rabbitt MP, Gregory CA, Singh A. Household Food Security in the United States in 2020 2021.
- [16].Rivera RL, Maulding MK, Eicher-Miller HA. Effect of Supplemental Nutrition Assistance Program-Education (SNAP-Ed) on food security and dietary outcomes. Nutr Rev 2019;77:903–21. 10.1093/NUTRIT/NUZ013. [DOI] [PubMed] [Google Scholar]
- [17].About WIC - WIC at a Glance | Food and Nutrition Service n.d. https://www.fns.usda.gov/wic/about-wic-glance (accessed November 10, 2021).
- [18].Khan F, Andrew Schiff B;, Mello M. pOpulATION MEdICINE impact of Participation in the Commodity Supplemental Food Program on Food insecurity Among low-income elderly Rhode islanders n.d. [PubMed]
- [19].Smith L, Jacob L, Barnett Y, Butler LT, Shin J il, López-Sánchez GF, et al. Association between Food Insecurity and Sarcopenia among Adults Aged ≥65 Years in Low- and Middle-Income Countries. Nutrients 2021;13. 10.3390/NU13061879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].USDA ERS - Survey Tools n.d. https://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-u-s/survey-tools/#household (accessed May 26, 2022).
- [21].Bhasin S, Travison TG, Manini TM, Patel S, Pencina KM, Fielding RA, et al. Sarcopenia Definition: The Position Statements of the Sarcopenia Definition and Outcomes Consortium. J Am Geriatr Soc 2020;68:1410–8. 10.1111/JGS.16372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Batsis JA, Villareal DT. Sarcopenic obesity in older adults: aetiology, epidemiology and treatment strategies. Nat Rev Endocrinol 2018;14:513. 10.1038/S41574-018-0062-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Ferrucci L, Kuchel GA. Heterogeneity of Aging: Individual Risk Factors, Mechanisms, Patient Priorities, and Outcomes. J Am Geriatr Soc 2021;69:610–2. 10.1111/JGS.17011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Hoogendijk EO, Afilalo J, Ensrud KE, Kowal P, Onder G, Fried LP. Frailty: implications for clinical practice and public health. The Lancet 2019;394:1365–75. 10.1016/S0140-6736(19)31786-6. [DOI] [PubMed] [Google Scholar]
- [25].Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. The Lancet 2013;381:752–62. 10.1016/S0140-6736(12)62167-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Hoogendijk EO, Suanet B, Dent E, Deeg DJH, Aartsen MJ. Adverse effects of frailty on social functioning in older adults: Results from the Longitudinal Aging Study Amsterdam. Maturitas 2016;83:45–50. 10.1016/J.MATURITAS.2015.09.002. [DOI] [PubMed] [Google Scholar]
- [27].Kojima G, Iliffe S, Jivraj S, Walters K. Association between frailty and quality of life among community-dwelling older people: a systematic review and meta-analysis. J Epidemiol Community Health 2016;70:716–21. 10.1136/JECH-2015-206717. [DOI] [PubMed] [Google Scholar]
- [28].Dent E, Martin FC, Bergman H, Woo J, Romero-Ortuno R, Walston JD. Management of frailty: opportunities, challenges, and future directions. The Lancet 2019;394:1376–86. 10.1016/S0140-6736(19)31785-4. [DOI] [PubMed] [Google Scholar]
- [29].Smit E, Winters-Stone KM, Loprinzi PD, Tang AM, Crespo CJ. Lower nutritional status and higher food insufficiency in frail older US adults. British Journal of Nutrition 2013;110:172–8. 10.1017/S000711451200459X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyère O, Cederholm T, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age and Ageing 2019;48:601. 10.1093/ageing/afz046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Thomas KS, Mor V. Providing More Home-Delivered Meals Is One Way To Keep Older Adults With Low Care Needs Out Of Nursing Homes. 10.1377/Hlthaff20130390 2017;32:1796–802. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Berkowitz SA, Terranova J, Randall L, Cranston K, Waters DB, Hsu J. Association Between Receipt of a Medically Tailored Meal Program and Health Care Use. JAMA Internal Medicine 2019;179:786–93. 10.1001/JAMAINTERNMED.2019.0198. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and/or analyzed during the current study are publicly available on the NHANES website.


