Abstract
BACKGROUND
With the recent improvement of endoscopic techniques, endoscopic ultrasound-guided fine needle aspiration and endoscopic submucosal tunnel dissection (ESTD) have been widely used for accurate diagnosis and dissection acceleration of esophageal tumors.
CASE SUMMARY
We used a modified submucosal tunnel technique during endoscopic en bloc resection in a 58-year-old man with large esophageal submucosal gland duct adenoma (ESGDA). During modified ESTD, the oral end of the involved mucosa was cut transversely, followed by a submucosal tunnel created from the proximal to the distal end, and the anal end of the involved mucosa blocked by the tumor was incised. As a result of retaining submucosal injection solutions using the submucosal tunnel technique, it was possible to reduce the amount of injection required and increase the efficiency and safety of dissection.
CONCLUSION
Modified ESTD is an effective treatment strategy for large ESGDAs. Single-tunnel ESTD appears to be a time-saving procedure compared with conventional endoscopic submucosal dissection.
Keywords: Esophageal submucosal gland duct adenoma, Endoscopic ultrasound-guided fine needle aspiration, Endoscopic submucosal tunnel dissection, Case report
Core Tip: With the recent improvement of endoscopic techniques, endoscopic ultrasound-guided fine needle aspiration and endoscopic submucosal tunnel dissection (ESTD) have been widely used for accurate diagnosis and dissection acceleration. Here we used a modified submucosal tunnel technique during endoscopic en bloc resection in a 58-year-old man with large esophageal submucosal gland duct adenoma (ESGDA) 3.5 cm × 2.2 cm in size with negative margins. Modified ESTD is an effective treatment strategy for large ESGDAs. Single-tunnel ESTD appears to be a time-saving procedure compared with conventional ESD.
INTRODUCTION
The esophageal glands reside in the submucosal layer of the upper and lower segments of the esophagus, opening at the esophageal lumen by tortuous tubules. The glands play a role in protecting the esophagus from damage caused by acid exposure through the secretion of bicarbonate and prostaglandin. Esophageal submucosal gland duct adenoma (ESGDA) is quite rare and usually presents as a submucosal lesion with or without a central depression[1-2]. This is the first report of the successful resection of a large esophageal submucosal tumor (SMT) using endoscopic-related techniques.
METHODS
As described in the published literature, single-tunnel ESTD[3] has shown greater efficiency for large superficial esophageal squamous cell neoplasms. In contrast to conventional ESTD, modified ESTD does not begin with cutting the distal end of the involved mucosa, which is occluded by a large esophageal SMT. First, the oral end of the involved mucosa was cut transversely. Subsequently, a submucosal tunnel was created from the proximal to the distal end. After completion of the tunnel, the lateral mucosa was incised, followed by the anal end of the involved mucosa, until complete removal of the tumor was achieved. Modified ESTD can be faster than conventional ESD for large esophageal tumors.
CASE PRESENTATION
Chief complaints
A 58-year-old man was referred to our hospital with a complaint of gastro-esophageal reflux symptoms for one month.
History of present illness
Symptoms started 1 mo before presentation with recurrent retro-sternal heartburn.
History of past illness
He was made a definite diagnosis of hypertension, and his blood pressure control is steady by oral anti-hypertensive drugs.
Personal and family history
The patient denied any family history of malignant tumors.
Physical examination
On physical examination, the vital signs were as follows: Body temperature, 36.5℃; blood pressure, 140/85 mmHg; heart rate, 85 beats per min; respiratory rate, 18 breaths per min. Furthermore, no enlargement was found in superficial lymph nodes. There was no obvious redness and swelling. Digital anal examination was not performed.
Laboratory examinations
Levels of serum tumor markers were normal (carcinoembryonic antigen, 2.8 ng/mL; carbohydrate antigen 12-5, 12 U/mL; carbohydrate antigen 724, 0.33 U/mL), except elevated carbohydrate antigen 19-9 at the level of 45.25 U/mL. No abnormality was found in routine blood, stool and urine analyses.
Imaging examinations
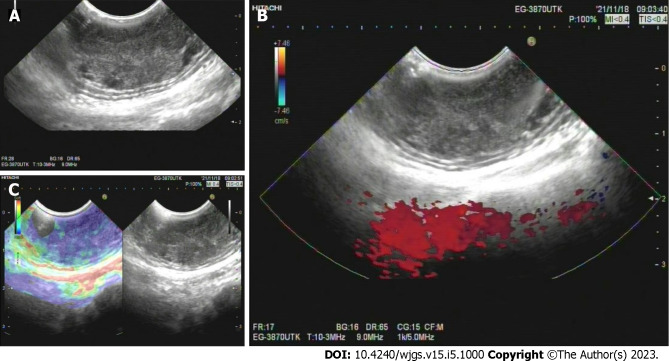
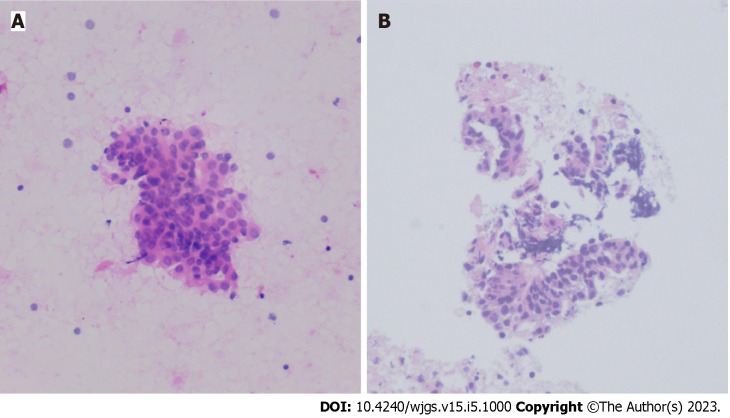
White-light endoscopy showed one 35-mm SMT located in the lower thoracic esophagus, with a central depression with a reddish appearance, just above the squamous-columnar epithelium junction (Figure 1). Endoscopic ultrasound (EUS) showed that the SMT was a well-defined heterogeneous, hypoechoic lesion with scattered small anechoic areas in the third layer (Figure 2A). No vascular flow was noted on color Doppler within the lesion (Figure 2B). Elastography revealed a hard mass (Figure 2C). Both cytological and histological analysis of fine-needle aspiration (FNA) specimens reported atypical glandular epithelial cells, ruling out squamous carcinoma (Figure 3). Thorax computed tomography (CT) revealed an eccentric soft tissue density mass in the esophagus.
Figure 1.
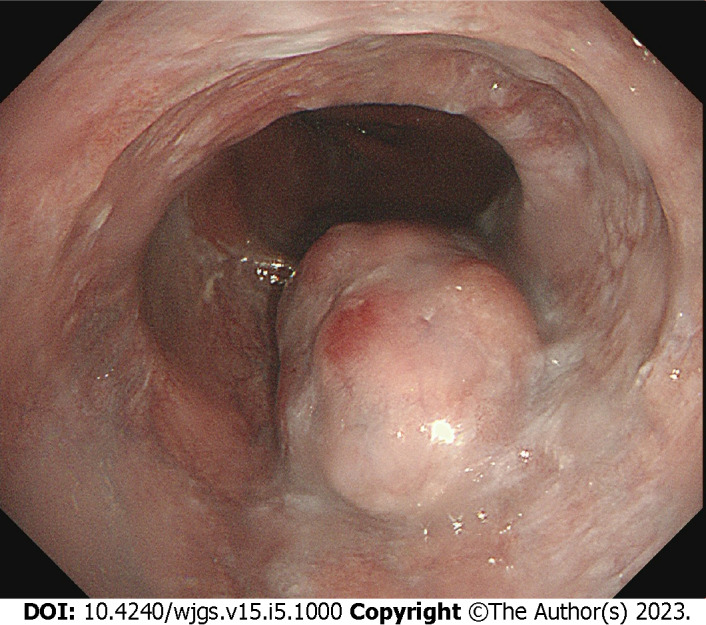
Endoscopic findings. One 35-mm submucosal tumor was located in the lower thoracic esophagus, with a central depression with a reddish appearance.
Figure 2.
Endoscopic ultrasound findings. A: A well-defined heterogeneous, hypoechoic lesion with scattered small anechoic areas in the third layer; B: No vascular flow within the lesion; C: A hard mass revealed by elastography.
Figure 3.
Endoscopic ultrasound - fine-needle aspiration findings. A: Cytological analysis; B: Histological analysis.
FINAL DIAGNOSIS
Combined with the patient’s medical history, the final diagnosis was esophageal benign submucosal mesenchymal tumor.
TREATMENT
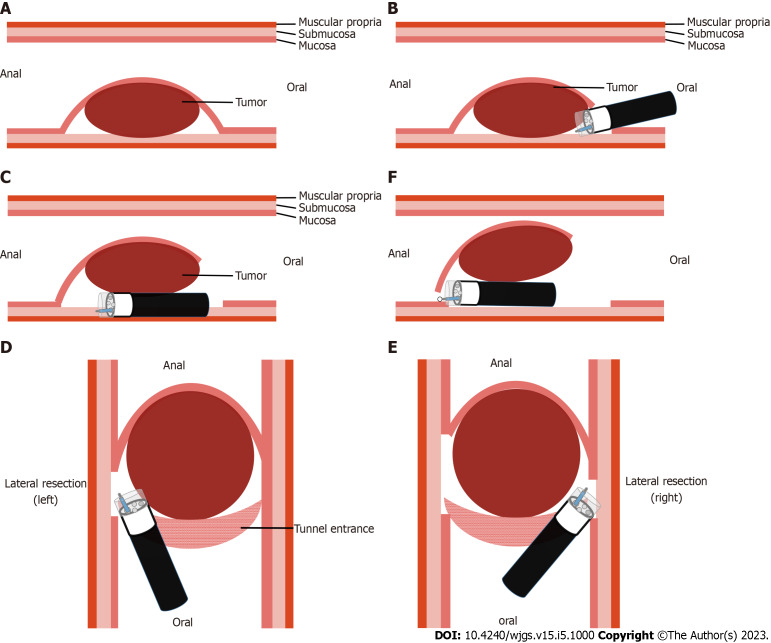
Given that the mass did not involve the muscularis propria, modified ESTD was performed using a single-accessory channel endoscope with a transparent cap attached to the front. First, the oral end of the involved mucosa was cut transversely. Subsequently, a submucosal tunnel was created from the proximal end to the distal end. After completion of the tunnel, the lateral mucosa was incised, followed by the anal end of the involved mucosa, until complete removal of the tumor was achieved (Figure 4). The post-ESTD defect was closed using repositionable clips in the distal–proximal sequence.
Figure 4.
Schema of modified endoscopic submucosal tunnel dissection. A: Endoscopic submucosal tunnel dissection located in the submucosal layer; B: Oral end of the involved mucosa cut transversely; C: Submucosal tunnel created from the proximal end to the distal end; D: One lateral mucosa resected; E: The other lateral mucosa resected; F: Anal end of the involved mucosa resected.
Subsequently, cefazolin sodium 1 g was administered intravenously twice a day for three days from the day of the resection.
OUTCOME AND FOLLOW-UP
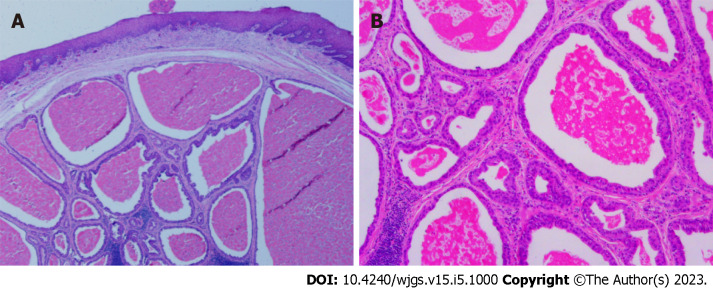
The procedure was completed without any adverse events, and the patient was discharged on postoperative day 7. Post-ESTD pathology confirmed an ESGDA 3.5 cm × 2.2 cm in size with negative margins. A cystic pattern with distinct 2-cell layers was observed, and the inner luminal cells were eosinophilic (Figure 5). Immunohistochemical staining showed the positive expression of P63, CK7, CK8/18, and Ki-67.
Figure 5.
Post-Endoscopic submucosal tunnel dissection pathology. A: A cystic pattern with distinct 2-cell layers; B: Eosinophilic inner luminal cells.
At 12 mo postoperatively, the patient received gastroscopy showing the esophageal wound healed well.
DISCUSSION
To the best of our knowledge, this present study represents the largest ESGDA treated by modified ESTD to be reported in the literature. Published literature reports suggest a potential biological pathway for ESGDA to progress to malignancy; thus, resection of these tumors is recommended if possible.
As an esophageal subepithelial tumor, ESGDA is extremely easily mistaken for esophageal carcinoma. EUS evaluation is essential for evaluating subepithelial lesions. The typical EUS feature of ESGDA is a heterogeneous hypoechoic submucosal tumor located in the third sonographic layer, with a few cystic lesions, considered dilated adenomatous gland ducts[4]. Differentiation through EUS-guided FNA is helpful to judge the origin of pathology and make the decision for conservative management vs endoscopic or thoracoscopic intervention[5]. In our case, both cytological and histological analyses showed atypical glandular epithelial cells, so modified ESTD was selected for resection.
As reported previously[3], the major advantage of ESTD over ESD for large superficial esophageal squamous cell neoplasms is that most submucosal injection solutions can be retained in the submucosal layer, resulting in increased efficiency and safety of dissection. Also tunnel endoscopy can be used to expose the intact submucosal lesion between the mucosa and muscular layer of the esophagus. In view of the aforementioned advantages, we performed ESTD for en bloc resection of the large ESGDA, rather than conventional ESD that was be adopted in the literature on ESGDA[1,2,4,6-8]. During routine ESTD, the distal end of the involved mucosa was first cut transversely. In this case, the obstruction caused by a large esophageal tumor made it difficult to cut the distal end of the involved mucosa at the beginning of the operation. An adjustment of the operative sequence was made in the modified ESTD. The oral end of the involved mucosa was first cut transversely, then the lateral mucosa was incised, followed by the anal end of the involved mucosa, after completion of the tunnel.
With regard to the disadvantages of ESTD, they include visual field loss when arterial bleeding requiring immediate endoscopic hemostasis occurs, due to the limited tunnel space. Furthermore, arterial bleeding in ESTD for lower esophageal tumors is relatively more common, differing from that involving the upper and middle esophagus.
CONCLUSION
Modified ESTD is an effective treatment strategy for large ESGDAs. Single-tunnel modified ESTD appears to be a time-saving procedure compared with conventional ESD[9-10].
Footnotes
Informed consent statement: Informed written consent was obtained from the patient for publication of this report and any accompanying images.
Conflict-of-interest statement: The authors declare that they have no conflict of interest to disclose.
CARE Checklist (2016) statement: The authors have read the CARE Checklist (2016), and the manuscript was prepared and revised according to the CARE Checklist (2016).
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Peer-review started: January 16, 2023
First decision: February 1, 2023
Article in press: March 30, 2023
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Atanasova EG, Bulgaria; Atqiaee K, Iran; Mokhtar MN, Malaysia; Piltcher-da-Silva R, Brazil S-Editor: Ma YJ L-Editor: A P-Editor: Zhao S
Contributor Information
Su-Yu Chen, Department of Endoscopy Center, Clinical Oncology School of Fujian Medical University, Fujian Cancer Hospital, Fuzhou 350014, Fujian Province, China.
Zhao-Fei Xie, Department of Endoscopy Center, Clinical Oncology School of Fujian Medical University, Fujian Cancer Hospital, Fuzhou 350014, Fujian Province, China.
Yan Jiang, Department of Endoscopy Center, Clinical Oncology School of Fujian Medical University, Fujian Cancer Hospital, Fuzhou 350014, Fujian Province, China.
Juan Lin, Department of Endoscopy Center, Clinical Oncology School of Fujian Medical University, Fujian Cancer Hospital, Fuzhou 350014, Fujian Province, China.
Hong Shi, Department of Endoscopy Center, Clinical Oncology School of Fujian Medical University, Fujian Cancer Hospital, Fuzhou 350014, Fujian Province, China. endoshihong@126.com.
References
- 1.Yamamoto M, Nishida T, Nakamatsu D, Adachi S, Inada M. Endoscopic findings of esophageal gland duct adenoma resected by endoscopic submucosal dissection. Gastrointest Endosc. 2020;92:961–962. doi: 10.1016/j.gie.2020.04.053. [DOI] [PubMed] [Google Scholar]
- 2.Nie L, Wu HY, Shen YH, Fan XS, Sun Q, Huang Q, Chen J. Esophageal submucosal gland duct adenoma: a clinicopathological and immunohistochemical study with a review of the literature. Dis Esophagus. 2016;29:1048–1053. doi: 10.1111/dote.12442. [DOI] [PubMed] [Google Scholar]
- 3.Zhang W, Zhai Y, Chai N, Linghu E, Li H, Feng X. Single- and double-tunnel endoscopic submucosal tunnel dissection for large superficial esophageal squamous cell neoplasms. Endoscopy. 2018;50:505–510. doi: 10.1055/s-0043-122384. [DOI] [PubMed] [Google Scholar]
- 4.Agawa H, Matsushita M, Kusumi F, Nishio A, Takakuwa H. Esophageal submucosal gland duct adenoma: characteristic EUS and histopathologic features. Gastrointest Endosc. 2003;57:983–985. doi: 10.1016/s0016-5107(03)70058-3. [DOI] [PubMed] [Google Scholar]
- 5.Nashed B, Ayas MF, Gharib H, Issa M, Fatouh K, Sebastian F, Backer Z, Mahat K, Barawi M. Esophageal Schwannoma: An Important Differential Diagnosis for Esophageal Subepithelial Lesions. Cureus. 2022;14:e27168. doi: 10.7759/cureus.27168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shibata M, Kusafuka K, Ono H. A Rare Submucosal Tumor of the Esophagus. Gastroenterology. 2017;152:e6–e7. doi: 10.1053/j.gastro.2016.08.017. [DOI] [PubMed] [Google Scholar]
- 7.Matsushita M, Okazaki K. Esophageal, submucosal, gland duct adenoma: role of EUS for endoscopic removal. Gastrointest Endosc. 2005;61:790; author reply 790–790; author reply 791. doi: 10.1016/s0016-5107(05)00142-2. [DOI] [PubMed] [Google Scholar]
- 8.Chinen T, Misawa T, Yoshida K, Nasu T, Kubo S, Toyoshima S, Yao T, Harada N. Esophageal submucosal gland duct adenoma. Gastrointest Endosc. 2004;60:798–799. doi: 10.1016/s0016-5107(04)02026-7. [DOI] [PubMed] [Google Scholar]
- 9.Fan X, Wu Q, Li R, Chen W, Xie H, Zhao X, Zhu S, Fan C, Li J, Liu M, Liu Z, Han Y. Clinical benefit of tunnel endoscopic submucosal dissection for esophageal squamous cancer: a multicenter, randomized controlled trial. Gastrointest Endosc. 2022;96:436–444. doi: 10.1016/j.gie.2022.04.016. [DOI] [PubMed] [Google Scholar]
- 10.Zou J, Chai N, Linghu E, Li H, Chai M, Shi Y, Wang Z, Li L. Autologous skin-grafting surgery to prevent esophageal stenosis after complete circular endoscopic submucosal tunnel dissection: a case-matched controlled study. Surg Endosc. 2021;35:5962–5970. doi: 10.1007/s00464-020-08081-7. [DOI] [PubMed] [Google Scholar]