Abstract
Background:
Nepal is preparing to eliminate malaria by 2026. To evaluate the progress of vector control and prioritize areas for targeted intervention, understanding the recent changing distribution of high and moderate malaria risk areas is vital.
Methods:
Patterns of designated high and moderate malaria risk wards in Nepal between 2018 and 2021 were analyzed to identify stable and newly generated high- and moderate-risk (HaMR) wards, using the Spatial Temporal Analysis of Moving Polygons (STAMP) method.
Results and Conclusions:
High-risk and moderate-risk wards decreased by about 55% and the number of districts containing these wards also decreased from 20 to 14. However, several stable and new HaMR wards, mostly in the northwest and the southwest of the country, are apparent, despite intervention efforts. Public health officials should prioritize those wards for malaria surveillance and vector control, and future studies should explore the underlying reasons for persistent risk wards.
Keywords: Nepal, risk stratification, malaria, spatial and temporal trend
Introduction
Malaria was a major public health issue in Nepal for much of the 20th century (Newby, 2015), but cases declined significantly in the past two decades, in response to concerted intervention efforts, as part of a push to elimination. Between 2010 and 2020, indigenous malaria declined by about 98% with only 73 cases reported in Nepal in 2020 (EDCD, 2021), and Nepal is preparing for malaria elimination by 2026. As malaria incidence decreases in response to intervention coverage, cases and transmission rates become heterogenous across the country.
In this phase, a key approach to optimize malaria intervention is “stratification” in which the country or region is divided into smaller units based on the malaria risk (WHO, 2015). Malaria risk stratification identifies geographical areas at potential risk of malaria transmission to guide targeted intervention and for an effective and efficient resource mobilization (EDCD, 2018a; EDCD, 2018b). Nepal conducted its first malaria risk stratification in 2010 at the district level based on annual parasite index (API), which is the total number of confirmed malaria cases per 1000 population at risk of malaria (DoHS, 2010; DoHS, 2009).
This stratification defined four risk categories: high-risk (HR), moderate-risk (MR), low-risk, and no-risk. With the large decline in burden, and evidence of malaria-endemic and malaria-free areas occurring within the same district, malaria stratification was refined to the subdistrict level (subdistrict geographic units called village development committees [VDCs]), in 2013. This stratification was based on disease burden, ecology, and vulnerability (Rijal et al., 2019). The continued declines showed that within a VDC, malaria activity is concentrated in some wards (subdivisions of VDCs), whereas others remain free. Risk stratification was refined to wards in 2016, and has been reported annually since 2018, using the same categories.
In this study, we analyzed the interannual spatiotemporal patterns of high- and moderate-risk (HaMR) wards from 2018 to 2021 by using the Spatial Temporal Analysis of Moving Polygons (STAMP) method. Identifying areas of stable or newly generated high- or moderate-risk areas identifies persistence of malaria or emergence of new risk areas. The objective was to identify priority areas for malaria surveillance and vector control as Nepal prepares for malaria elimination by 2026.
Materials and Methods
Malaria risk areas data
The names of HaMR malaria wards for the years 2018–2021 were obtained from reports published online by the Epidemiology and Disease Control Division (EDCD) of the Department of Health, Government of Nepal. Using a shapefile of the wards in Nepal (HES, 2020), we assigned the two categories of malaria risk to the wards: HR and MR wards and created a shapefile in ArcGIS 10.6.1 (ESRI, Redland, CA).
Spatial temporal analysis of moving polygons
To quantify patterns and changes of HaMR wards in Nepal, we used the STAMP algorithm (Robertson et al., 2007). STAMP overlays polygons from two time periods and evaluates changes in spatial position (Bezymennyi et al., 2014; Morris et al., 2013). The analysis includes the identification of regions newly generated (emerging risk), remaining stable (persistent risk) or disappeared (reduced risk). Polygons remaining at the same risk in two consecutive time periods are classified as “stable.” Polygons at risk in the first time but absent in the second are classified as “disappearance.”
Polygons at risk only in the second time are classified as “generation” (here “new”). Separate STAMP analyses were performed for each risk category: HR and MR for each interannual period: 2018–2019, 2019–2020, and 2020–2021. Risk category changes within wards were also identified, such as moderate to high or high to moderate between years, using STAMP across categories (Supplementary Data). STAMP analysis was performed in R version 4.1.3 (2022-03-10) using the “stampr” package. All final maps were produced in ArcGIS.
Results
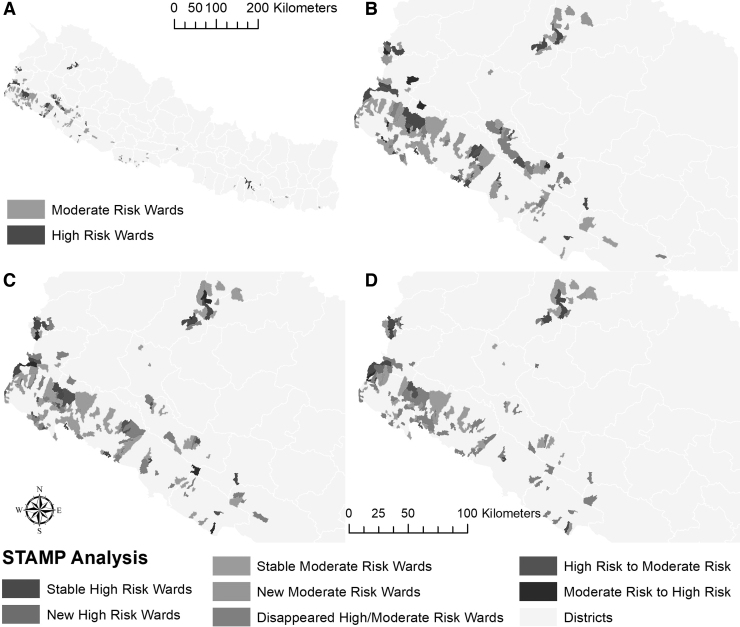
From 2018 to 2021, the number of HaMR wards decreased by about 55% in Nepal (Supplementary Table S1). There were 153 MR and 49 HR wards in 2018, which decreased to 68 MR and 22 HR wards in 2021. The HaMR wards were primarily concentrated in the southwest of Nepal in 2018 with very few HaMR wards in the northwest and the rest of the country (Fig. 1A). Between 2018 and 2019, several new MR wards appeared in the northwest (Fig. 1B) and remained stable. In the southwest region, several HaMR wards disappeared, whereas others persisted (Fig. 1B, D). MR wards were more widespread and persistent than HR wards in Nepal, and some wards changed from MR to HR and vice versa (Fig. 1B–D). The number of wards changing category decreased across the years of the study (Supplementary Table S4).
FIG. 1.
STAMP analysis for high- and moderate-risk malaria wards in Nepal between 2018 and 2021. (A) Distribution of high- and moderate-risk wards in 2018. (B) Results of STAMP analysis between 2018 and 2019 in western Nepal. (C) Results of STAMP analysis between 2019 and 2020 in western Nepal. (D) Results of STAMP analysis between 2020 and 2021 in western Nepal. The STAMP analysis for the whole country is presented in Supplementary Fig. S1. STAMP, Spatial Temporal Analysis of Moving Polygons.
There were 20 districts with HaMR wards in 2018. Humla and Achham districts had new HaMR wards in 2019, whereas Jhapa and Sarlahi became free of HaMR wards in the same year. In 2020, Bara, Dhanusha, Rupandehi, and Sindhuli became free of HaMR wards. In 2021, Dang, Nawalpur, and Salyan became free of HaMR wards, whereas Kalikot had new HR wards. This resulted in 2021 having 14 districts with HaMR wards. Humla and Achham had stable HaMR wards in 2021, which had been free of HaMR wards until 2018. Six HR wards in three districts and 20 MR wards in four districts remained consistently stable throughout the study period (Supplementary Table S5). The number of stable and new HaMR wards gradually decreased over the years, and disappeared HaMR wards increased (Supplementary Tables S2 and S3).
Discussion
Interannual patterns of malaria risk in Nepal between 2018 and 2021 were analyzed using the STAMP algorithm at the ward level. The implementation of vector control interventions has decreased the number of HaMR wards in Nepal, and the number of districts with HaMR wards has also decreased. This result is in agreement with studies done in other countries. For example, after vector control interventions, the number of high transmission districts dropped from 14.3% to 6.4% in Ethiopia between 2013 and 2016 (Taffese et al., 2018).
Similarly, in Bhutan, the geographical distribution of malaria infection decreased from 15 of the 20 districts in 2006 to only 2 districts in 2018 (Wangchuk et al., 2019). Although the number of HaMR wards decreased in Nepal, there were several stable HaMR wards throughout the study period, meaning malaria is still transmitted in these areas, despite vector control. Future studies should examine conditions associated with stability of these HaMR wards. In addition, we detected several new HaMR wards, mostly in the northwest and southwest.
In a previous study, we identified clusters of a significantly increasing trend of imported malaria in the southwest (Bhattarai et al., 2023), and the stable and new HaMR wards in the southwest may be due to imported malaria. Several other studies also have identified the high number of imported malaria cases in the western part of Nepal (Dhimal et al., 2014a; EDCD, 2018a; Rijal et al., 2018; Smith et al., 2019). Concurrently, several HaMR wards in the southwest disappeared during the study period, corroborating our previous study showing declining trends of several malaria indicators except imported malaria (Bhattarai et al., 2023). Some of this region may observe reduced transmission in the future with temperatures increasing to levels too high to be suitable for transmission (Bhattarai et al., 2022).
The generation of new HaMR wards in the northwest in 2019, and their stability throughout the study years is very concerning given this area falls in the hilly and mountainous region in Nepal, historically not endemic for malaria. This suggests malaria is becoming established in the mountainous area, which may be due to climate change. In a previous study, we found a significantly increasing trend of indigenous malaria in this same region (Bhattarai et al., 2023).
This area is projected to observe additional emergence and increase in season length of malaria transmission suitability in the future (Bhattarai et al., 2022), pointing to the need to prioritize these areas for surveillance, and vigilance in emerging new risk areas. Malaria transmission has increased in the highland areas in different parts of the world due to climate change (Loevinsohn, 1994; Siraj et al., 2014). In Nepal too, some studies have found that climate change has already affected malaria transmission (Badu, 2013; Bhandari et al., 2013; Dhimal et al., 2014b; Ghimire, 2016).
Few HR wards converted to MR; however, several MR wards converted to HR despite vector control intervention. Further study to understand where intervention succeeds and fails in an era of elimination, is needed.
Conclusions
High and moderate malaria risk areas in Nepal decreased significantly in Nepal between 2018 and 2021. However, there were several stable HaMR wards and some new HaMR wards, particularly in the northwest and southwest regions. Public health officials should focus on these areas to prioritize surveillance and vector control interventions. Future studies should explore the underlying reasons for persistent risk areas in these regions.
Supplementary Material
Acknowledgment
Thanks to the Department of Epidemiology and Disease Control Division, Government of Nepal for making malaria risk stratification data available online.
Authors' Contributions
Conceptualization (equal), methodology (equal), formal analysis (lead), writing original draft (lead), writing—review and editing (equal) by S.B. Conceptualization (equal), methodology (equal), writing—review and editing (equal) by J.K.B. and S.J.R.
Author Disclosure Statement
No conflicting financial interests exist.
Funding Information
No funding was received for this article.
Supplementary Material
References
- Badu M. Assessing the impact of climate change on human health: Status and trends of malaria and diarrhea with respect to temperature and rainfall variability in Nepal. Kathmandu Univ J Sci Eng Technol 2013;9:96–105. [Google Scholar]
- Bezymennyi M, Bagamian KH, Barro A, et al. Spatio-temporal patterns of livestock anthrax in Ukraine during the past century (1913–2012). Appl Geogr 2014;54:129–138; doi: 10.1016/j.apgeog.2014.07.016 [DOI] [Google Scholar]
- Bhandari GP, Dhimal M, Gurung S, et al. Climate change and malaria in Jhapa district of Nepal: Emerging evidences from Nepal. J Health Manag 2013;15(1):141–150; doi: 10.1177/0972063413486026 [DOI] [Google Scholar]
- Bhattarai S, Blackburn JK, McKune SL, et al. Spatio-temporal patterns of malaria in Nepal from 2005 to 2018: A country progressing towards malaria elimination. Spat Spatio Temporal Epidemiol 2023;45:100576; doi: 10.1016/j.sste.2023.100576 [DOI] [PubMed] [Google Scholar]
- Bhattarai S, Blackburn JK, Ryan SJ. Malaria transmission in Nepal under climate change: Anticipated shifts in extent and season, and comparison with risk definitions for intervention. Malar J 2022;21(1):390; doi: 10.1186/s12936-022-04417-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dhimal M, Ahrens B, Kuch U. Malaria control in Nepal 1963–2012: Challenges on the path towards elimination. Malar J 2014a;13(1):241; doi: 10.1186/1475-2875-13-241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dhimal M, O'Hara RB, Karki R, et al. Spatio-temporal distribution of malaria and its association with climatic factors and vector-control interventions in two high-risk districts of Nepal. Malar J 2014b;13(1):457; doi: 10.1186/1475-2875-13-457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- DoHS. Annual Report Department of Health Services 2065/66 (2008/2009). Department of Health Services, Ministry of Health & Population, Government of Nepal, Kathmandu, Nepal; 2009. [Google Scholar]
- DoHS. Annual Report Department of Health Services 2066/67 (2009/2010). Department of Health Services, Ministry of Health & Population, Government of Nepal, Kathmandu, Nepal; 2010. [Google Scholar]
- EDCD. 2016. Malaria Micro-Stratification. Epidemiology & Disease Control Division, Department of Health Services, Ministry of Health & Population, Government of Nepal, Kathmandu, Nepal; 2018a. [Google Scholar]
- EDCD. 2018. Malaria Micro-Stratification. Epidemiology & Disease Control Division, Department of Health Services, Ministry of Health & Population, Government of Nepal, Kathmandu, Nepal; 2018b. [Google Scholar]
- EDCD. Self-Audit of the National Malaria Program Using the Malaria Elimination Audit Tool 2021. Epidemiology & Disease Control Division, Department of Health Services, Ministry of Health & Population, Government of Nepal, Kathmandu, Nepal; 2021. [Google Scholar]
- Ghimire K. Geographic Distribution of Malaria in Nepal. 2016. Doctoral dissertation. Kansas State University. [Google Scholar]
- HES. GIS Map of Nepal. 2020. Available from: https://map.hermes.com.np [Last accessed: December 2, 2022].
- Loevinsohn ME. Climatic warming and increased malaria incidence in Rwanda. Lancet 1994;343(8899):714–718; doi: 10.1016/S0140-6736(94)91586-5 [DOI] [PubMed] [Google Scholar]
- Morris LR, Blackburn JK, Talibzade A, et al. Informing surveillance for the lowland plague focus in Azerbaijan using a historic dataset. Appl Geogr 2013;45:269–279; doi: 10.1016/j.apgeog.2013.09.014 [DOI] [Google Scholar]
- Newby G. Eliminating Malaria in Nepal. Global Health Group, UCSF: San Francisco, California, USA; 2015. [Google Scholar]
- Rijal KR, Adhikari B, Adhikari N, et al. Micro-stratification of malaria risk in Nepal: Implications for malaria control and elimination. Trop Med Health 2019;47(1):21; doi: 10.1186/s41182-019-0148-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rijal KR, Adhikari B, Ghimire P, et al. Epidemiology of Plasmodium Vivax malaria infection in Nepal. Am J Trop Med Hyg 2018;99(3):680–687; doi: 10.4269/ajtmh.18-0373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robertson C, Nelson TA, Boots B, et al. STAMP: Spatial–temporal analysis of moving polygons. J Geogr Syst 2007;9(3):207–227; doi: 10.1007/s10109-007-0044-2 [DOI] [Google Scholar]
- Siraj AS, Santos-Vega M, Bouma MJ, et al. Altitudinal changes in malaria incidence in highlands of Ethiopia and Colombia. Science 2014;343(6175):1154–1158; doi: 10.1126/science.1244325 [DOI] [PubMed] [Google Scholar]
- Smith JL, Ghimire P, Rijal KR, et al. Designing malaria surveillance strategies for mobile and migrant populations in Nepal: A mixed-methods study. Malar J 2019;18(1):158; doi: 10.1186/s12936-019-2791-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taffese HS, Hemming-Schroeder E, Koepfli C, et al. Malaria epidemiology and interventions in Ethiopia from 2001 to 2016. Infect Dis Poverty 2018;07(06):1–9; doi: 10.1186/s40249-018-0487-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wangchuk S, Gyeltshen S, Dorji K, et al. Malaria elimination in Bhutan: Asymptomatic malaria cases in the Bhutanese population living in malaria-risk areas and in migrant workers from India. Rev Inst Med Trop São Paulo 2019;61:e52; doi: 10.1590/S1678-9946201961052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO. Global Technical Strategy for Malaria 2016–2030. World Health Organization: Geneva, Switzerland; 2015. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.