Abstract
BACKGROUND:
Early sexual reproductive health (SRH) education is linked to a reduction in risky sexual behaviors. Sexually transmitted infections (STIs) are rising at alarming rates. Risky sexual behaviors, including initiation of sex before age 13, having more than four sexual partners, and lack of use of condoms, increase the chance of infection and cancer. Informing students about the link between risky behaviors and cancer is vital to reduce morbidity and mortality.
METHODS:
A trend analysis of the Youth Risk Behavior Surveillance System (YRBSS) data between 2001 and 2019 was conducted. Results from four survey responses related to sexual risk behaviors among 9th to 12th grade in Mississippi students are compared with their US peers.
RESULTS:
Between 2001 and 2019, favorable declines in 3 out of 4 sexual risk behaviors were observed. Declining prevalence was reported for “ever had sexual intercourse,” “age of sexual initiation at age 13 or younger,” and “having 4 or more sexual partners in their lifetime” are promising. However, fewer students report using condoms. The adjusted prevalence rates for Mississippi students in all 4 measures were higher than the national responses.
CONCLUSIONS:
Our analysis supports the need for early skill-based sex education to promote health. States with increased behavioral risk among students should consider trends in data to improve education and policy.
Keywords: sexual reproductive education, youth risk, sexual risk, cancer, human papillomavirus, sexually transmitted infection
Across the United States, there are declining state-level trends in US school-based sexual reproductive health (SRH) instruction, and efforts to strengthen curriculums are critical.1,2 Risky sexual behaviors among youth and young adults have been associated with rising rates of sexually transmitted infections (STIs) in the United States. Of the 26 million new STI diagnoses in the United States in 2018, almost half were among youth aged 15 to 24.3 Human papillomavirus (HPV) causes cancer and is the most common STI in the United States with over 80 million people infected, including 14 million teenagers.3 There is no cure for HPV, only treatment or prevention with vaccination and behavioral risk reduction. School-based SRH instruction adds to health promotion efforts to reduce risky behaviors and reduce cancer.
Persistent HPV infection causes genital warts in the oral cavity, reproductive tract, and nearly all cervical cancers. Each year, in the United States, an estimated 36,500 new HPV-attributable cancers occur, and the majority are preventable.3 Of these cancers, 21,400 occur in females and 15,100 in males.4 Regional disparities in the rates of other new STIs and HPV-related cancers are the highest in the southern United States, where regional rates of the uptake of HPV vaccination are the lowest.5 Accordingly, Mississippi (MS) bears a high burden of HPV prevalence and these preventable HPV-related cancers are acquired at early ages.6,7 Acquiring HPV at an early age increases one’s risk of developing cancer.8 Early sexual debut (having sexual intercourse before age 13) has been associated with increased risky sexual behaviors and early pregnancy and may increase cancer risk.9 An increased number of lifetime sexual partners (4 or more sexual partners) presents multiple opportunities for exposure to HPV, which can also contribute to developing cervical cancer in females and even higher rates of oral cancers in males.3,9 HPV vaccination and education prior to sexual debut or age 12 may prevent most cervical cancers, but the benefits decrease if delayed until age 16.10
An analysis of the 2019 Youth Risk Behavior Surveillance System (YRBSS) data comparing MS students to students in the United States identified a higher percentage of MS students who initiated sex prior to age 13 (5.4% vs 3.0%) and those reporting more than 4 sexual partners (10.1% vs 8.6%) in their lifetime.6 Therefore, to inform educators and cancer control programs, this study aimed to assess additional YRBSS data and the trends in the sexual risk behaviors between 2001 and 2019 and compare the responses from US students to those in MS.
A goal of this study was to further understand trends in risky sexual behaviors among adolescents in regions of the United States, such as MS, with increased cancer incidences. Understanding data about population behaviors can help direct community initiatives to prevent cancer.11 To that end, an epidemiologic analysis of trends in sexual risk behaviors in high school students using responses from the YRBSS was performed.
METHODS
Data were drawn from the survey responses within the Youth Risk Behavior Surveillance System (YRBSS) from the years 2001 to 2019.11–13 The YRBSS is self-reported data from minors attending participating high schools to monitor health-related behaviors that lead to death and disability. The Centers for Disease Control and Prevention (CDC) directs the US school-based survey with national, state, territorial, and tribal governments. It contains representative samples of 9th through 12th-grade students and is conducted every 2 years, usually during the spring semester of the odd years. A detailed description of methods is found at cdc.gov.10–13
Participants
The responses in this study included those from students attending public high schools in MS and were compared to the responses from the other 44 participating states across the United States. Study participants self-reported their gender (female or male), grade (from 9th to 12th), ethnicity (Hispanic/Latino), and race (American Indian or Alaska Native, Asian, Black or African American, Native Hawaiian or Other Pacific Islander, and White).
Instrumentation
Data related to behavior of the student respondents were determined by the survey asking the following questions and re-coding the responses for further analysis: (1) “Have you ever had sexual intercourse?” (2) “How old were you when you had sexual intercourse for the first time?” (These two questions were created to assess those who had sexual intercourse for the first time before age 13), (3) “During your life, with how many people have you had sexual intercourse?” (This survey question was created to re-code the variable, ‘among students who were currently sexually active, who had sexual intercourse with four or more persons during their lifetime’), and (4) “Who did not use a condom during last sexual intercourse?”
Procedure
The YRBSS questionnaire is conducted every odd year,11 except in MS for years 2005 and 2015, when the survey did not reach a 60% response rate. Therefore, we used data for 2001, 2003, 2007, 2009, 2011, 2013, 2015, and 2019 (8 data points). The survey uses standardized complex sampling methods and requires an overall response rate of 60% or higher to be a representative sample.12,13 The use of complex sampling methods of applying weighting, stratum, and primary sampling unit (PSU), produced a well-defined probability sample and was determined to be representative high-school students across the nation.14 The US weighted measures were applied to adjust for nonresponse and the distribution of students by sex, race, and grade in each record. Responses having a cell size of <50 respondents for the subgroup may not be reliable and were not included in this analysis. A detailed description of the survey method can be found in other sources.10–13
Parents of the teenagers had to consent to the study, and the teens had the choice to refuse participation.10 The use of this survey data was considered exempt from the Institutional Review Board by the University of Mississippi Medical Center as data is accessible in the public domain.
Data Analysis
Summary statistics and trends were compared with four survey responses related to sexual risk behaviors from MS students and aggregated responses from the 44 states reporting in the United States. The average annual adjusted prevalence and adjusted percentage change were reported, and longitudinal trends using Joinpoint trend analysis software15 of two segments of time for the following questions were calculated. Then, the associations of four behaviors were examined to provide estimates of differences between main effects within subgroups.
Statistical analysis was conducted using IBM SPSS Statistics—Complex Samples version 23 (Armonk, NY: IBM Corp., 2016) to calculate summary statistics and a weighted average annual percentage change (AAPC) and their 95% confidence intervals (CIs). A chi-square test was used to investigate if the prevalence of specific sexual risk behavioral responses differed between the United States and MS. Statistical software called Joinpoint version 4.9 was downloaded from the National Institutes of Health, National Cancer Institute, Division of Cancer Control and Population Sciences and used in all trend analyses.14 For the Joinpoint trend analysis, segments 1 and 2 are defined based on the availability of the dates. The survey responses are provided (Figure 1).
Figure 1.
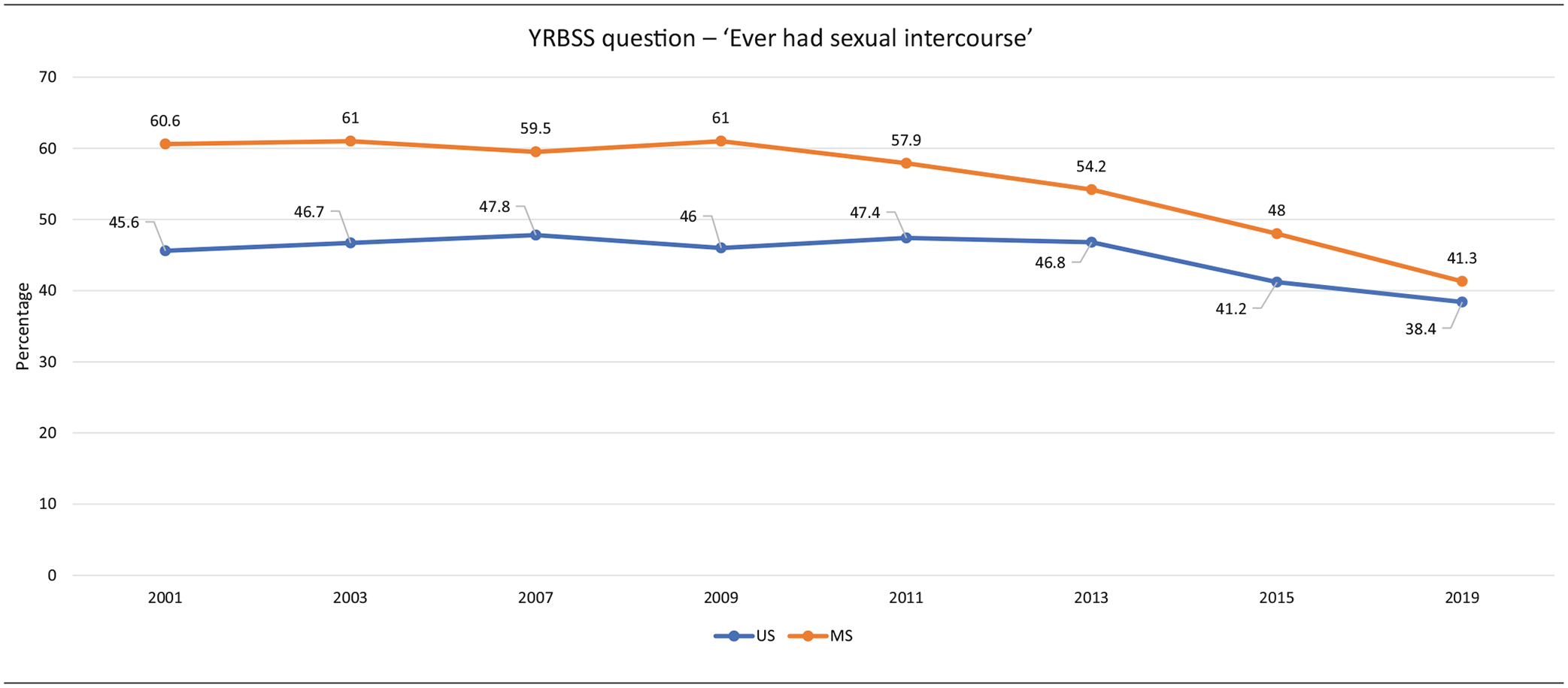
Prevalence change from 2001 to 2019
RESULTS
US Sample Characteristics
The 2019 US sample consisted of more than 13,000 students.14 According to the demographics, males and females were about equally represented at 50.6% male and 49.4% female. Most US students reported their race as White (51.2%) while 12.2% reported being Black, and 10.5% other races; 26.1% of the students named their ethnicity Hispanic. Those recorded in the aggregated “other” category for race/ethnicities include American Indian or Alaska Native, Asian, Native Hawaiian or other Pacific Islander, and multiple races (non-Hispanic). The US YRBSS sample demographics are consistent with the distribution of the US population data. Participants were distributed among grades with 26.6% in grade 9, 25.5% in grade 10, 24.2% in grade 11, and 23.5% in grade 12.
Mississippi Sample Characteristics
The 2019 MS YRBS sample consisted of 1767 MS students.13 According to the demographics, males and females were equally represented at 50.1% and 49.9%, respectively. Among all participants, 47.1% were Black students and 44.9% were White. The small proportion of all “other” race/ethnicities category responses was too small in MS for separate subgroup analysis, and data were not included in the overall comparison. In the overall population in MS, the US Census reports, 58.8% of individuals were White, 38% were Black, and 3.2% were from another race.16 Participants also were distributed among grades with 27.7% in grade 9, 26.3% in grade 10, 23.8% in grade 11, and 22.0% in grade 12.
Prevalence of Risk Factors in 2019
The prevalence of sexual risk behaviors in 2019 by selected factors in the United States and MS for the four variables is presented in Table 1. The overall comparison showed a statistically significant higher prevalence of having first sexual intercourse before the age of 13 (5.4% vs 3.0%; p < .001) and not using a condom during the last sexual intercourse (51.6% vs 45.7%; p = .04), for MS compared to US students.
Table 1.
Youth Risk Behavioral Survey (YRBS) 2019 Prevalence for Sexual Risk Behaviors by Selected Factors in the United States (US) and Mississippi (MS)
| Question (QN) | QN58— “Who Ever Had Sexual Intercourse?” | QN59—“Who Had Sexual Intercourse for the First Time Before the Age of 13 years?” | QN60—“Who Had Sexual Intercourse with Four or More Persons During Their Lifetime?” | QN63—“Who Did Not use a Condom during Last Sexual Intercourse?” | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Percent prevalence | US (95% CI) | MS (95% CI) | p-value | US (95% CI) | MS (95% CI) | p-value | US (95% CI) | MS (95% CI) | p-value | US (95% CI) | MS (95% CI) | p-value |
| Total overall prevalence | 38.4 (35.4–41.6) | 41.3 (36.8–46.0) | .29 | 3.0 (2.5–3.6) | 5.4 (4.1–7.0) | <.001 | 8.6 (7.5–9.9) | 10.1 (8.4–12.1) | .16 | 45.7 (43.4–48.0) | 51.6 (46.4–56.8) | .04 |
| Gender | ||||||||||||
| Male | 39.2 (35.9–42.7) | 44.8 (39.0–50.7) | .10 | 3.9 (3.2–4.7) | 8.3 (6.1–11.1) | <.001 | 10.0 (8.5–11.7) | 12.7 (10.0–16.0) | .10 | 40.0 (37.0–43.0) | 40.1 (31.8–49.0) | .98 |
| Female | 37.6 (34.2–41.1) | 38.2 (32.7–44.0) | .86 | 2.1 (1.5–2.9) | 2.7 (1.5–4.8) | .45 | 7.2 (6.1–8.5) | 7.6 (5.4–10.8) | .76 | 63.2 (55.5–70.2) | 50.4 (46.4–54.4) | <.001 |
| Race | ||||||||||||
| Black | 42.3 (36.2–48.5) | 46.8 (41.3–52.4) | .27 | 7.9 (6.2–10.0) | 6.9 (5.5–8.7) | .44 | 13.3 (10.1–17.2) | 13.0 (10.5–15.9) | .88 | 51.8 (46.7–56.8) | 48.4 (41.9–55.0) | .42 |
| White | 38.0 (34.6–41.4) | 37.6 (32.1–43.5) | .92 | 3.0 (1.7–5.1) | 1.9 (1.4–2.4) | .18 | 7.7 (6.5–9.1) | 7.3 (5.4–9.7) | .72 | 44.2 (41.4–47.1) | 55.5 (45.7–64.9) | .03 |
| Grade | ||||||||||||
| 9th | 19.2 (16.0–22.9) | 23.5 (18.8–28.9) | .16 | 3.7 (2.9–4.7) | 5.7 (3.8–8.5) | .09 | 2.7 (2.0–3.6) | 5.1 (3.4–7.7) | .03 | 38.7 (32.5–45.4) | N/A | N/A |
| 10th | 33.6 (29.4–38.0) | 36.7 (28.5–45.8) | .51 | 3.2 (2.3–4.3) | 7.1 (4.3–11.5) | .03 | 5.7 (4.5–7.2) | 9.3 (5.6–14.8) | .13 | 44.6 (39.6–49.8) | N/A | N/A |
| 11th | 46.5 (42.4–50.7) | 48.6 (39.8–57.5) | .67 | 3.0 (2.2–4.1) | 3.0 (1.6–5.6) | .96 | 10.6 (8.6–13.0) | 10.2 (6.6–15.4) | .85 | 43.7 (39.4–48.1) | N/A | N/A |
| 12th | 56.7 (53.1–60.2) | 60.1 (52.4–67.4) | .4 | 2.0 (1.4–2.7) | 5.7 (2.8–11.2) | .06 | 16.0 (13.6–18.8) | 16.8 (11.8–23.3) | .80 | 49.7 (46.2–53.1) | 57.0 (46.9–66.6) | .16 |
YRBS, Youth Risk Behavioral Survey, QN, YRBS question, US, United States aggregated YRBS responses, MS, Mississippi YRBS responses, Other race, Asian, Pacific Islander, American Indian, Alaska Native, Mixed Race.
Bold p-values are statistically significant.
Comparing MS and US students’ responses indicated several significant differences among gender, race, ethnicity, and grade subgroups. Compared to the United States, MS male students reported a significantly higher prevalence of having first sexual intercourse before the age of 13 (8.3% vs 3.9%; p<.001). The same results were reported for grade 9 (MS = 5.7% vs US = 3.7%, p = .09); grade 10 (MS = 7.1% vs US = 3.2%, p = .03), and grade 12 (MS = 5.7% vs US = 2.0%, p = .06). When comparing race/ethnicity groups in MS to the United States, MS White students reported a higher prevalence of not using a condom in their last sexual intercourse compared to the United States White students (55.5% vs 44.2%; p = .03).
Sub-Group Analysis of Risk Factors
Comparing being sexually active before age 13 within-group in MS, males were more likely to report being sexually active before age 13 than females (8.3% vs 2.7%, p < .000). However, within the US group, statistical differences were not observed. Next, within MS, when comparing Black versus White respondents, Black students were more likely to have sex prior to age 13, (6.9% vs 1.9%, p < .000). At the national level, similar results occurred (Table 1).
Prevalence Change from 2001 to 2019 MS
Table 2 summarizes 2001 to 2019 annual prevalence changes for each response and the results of the factors as they relate to one another. The Joinpoint trend and logistic regression linear and quadratic trends are shown. Responses from MS students to aggregated responses from other US students are compared. For three questions: “Who ever had sexual intercourse?,” “Who had sexual intercourse for the first time before the age of 13 years?,” “Who had sexual intercourse with four or more persons during their lifetime?,” a favorable significant decreasing linear trend is shown in sexual risk behaviors. However, for “Who did not use a condom during last sexual intercourse?,” a significant unfavorable increase occurs in students reporting the lack of use of condoms at last intercourse in MS.
Table 2.
Trends in the Youth Risk Behavioral Survey (YRBS) 2001–2019, Mean Prevalence for Sexual Risk Behaviors by Selected Factors in the United States (US) and Mississippi (MS)—Joinpoint Trend and Logistic Regression Analysis of Linear and Quadratic
| YRBS Question | AP | AAPC | p-value | ||||
|---|---|---|---|---|---|---|---|
| 2001 | 2019 | Joinpoint | Linear* | Quadratic* | |||
| QN 58—who ever had sexual intercourse | US | 46.9 | 38.0 | −1.3 (−1.9, −0.6) | .0001 | .0001 | <.0001 |
| MS | 60.9 | 41.1 | −2.2 (−2.4, −1.9) | <.0001 | <.0001 | <.0001 | |
| QN 59—who had sexual intercourse for the first time before age 13 years | US | 7.0 | 3.0 | −5.3 (−7.5, −3.1) | <.0001 | <.0001 | <.0001 |
| MS | 13.8 | 5.6 | −4.6 (−7.5, −1.7) | .0020 | <.0001 | <.0001 | |
| Q.N. 60—who had sexual intercourse with four or more people during their life | US | 15.0 | 8.4 | −3.3 (−4.6, −2.0) | <.0001 | <.0001 | <.0001 |
| MS | 25.8 | 9.9 | −5.1 (−6.2, −4.0) | <.0001 | <.0001 | <.0001 | |
| QN 63—who did not use a condom during last sexual intercourse | US | 42.4 | 44.0 | 0.4 (−0.3,1.2) | .2592 | <.0001 | <.0001 |
| MS | 34.9 | 50.1 | 2.0 (1.8, 2.2) | <.0001 | <.0001 | .0007 | |
YRBS, Youth Risk Behavioral Survey; AP, adjusted prevalence; AAPC, average annual percent change calculated using joinpoint trend analysis, QN, YRBS Question; US, United States aggregated YRBS responses; MS, Mississippi YRBS responses.
Results of the logistic regression analysis.
Figures 1, 2, 3 and 4 present the linear trends from 2001 to 2019. Figure 1 indicates a significant favorable linear decrease in the prevalence of sexual intercourse (AAPC, −2.2; 95% CI, −2.4, −1.9) in MS participants. An average of 2.2% decrease per year from 2001 to 2019. The same results were found at the national level (AAPC, −1.3; 95% CI, −1.9, −0.6). There was an average of 1.3% decrease per year from 2001 to 2019.
Figure 2.
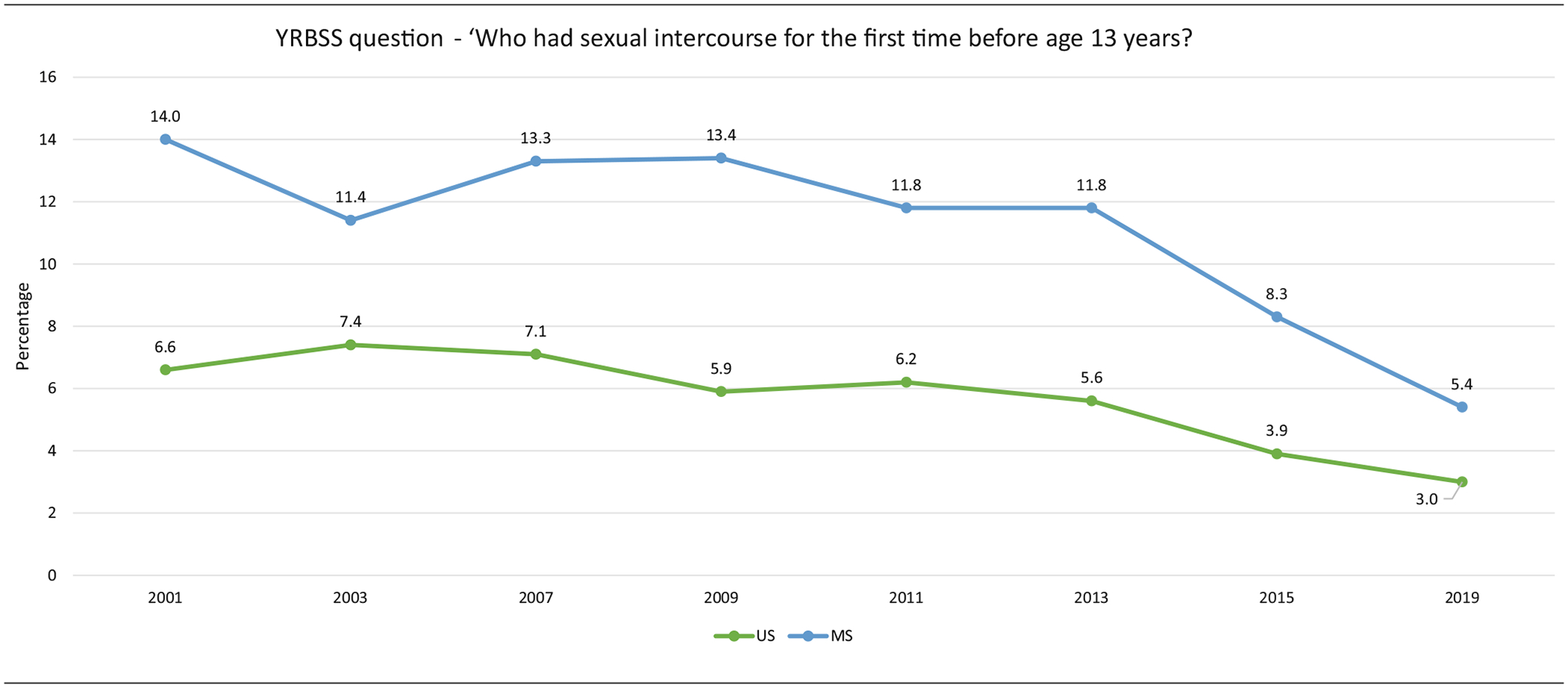
Prevalence change from 2001 to 2019
Figure 3.
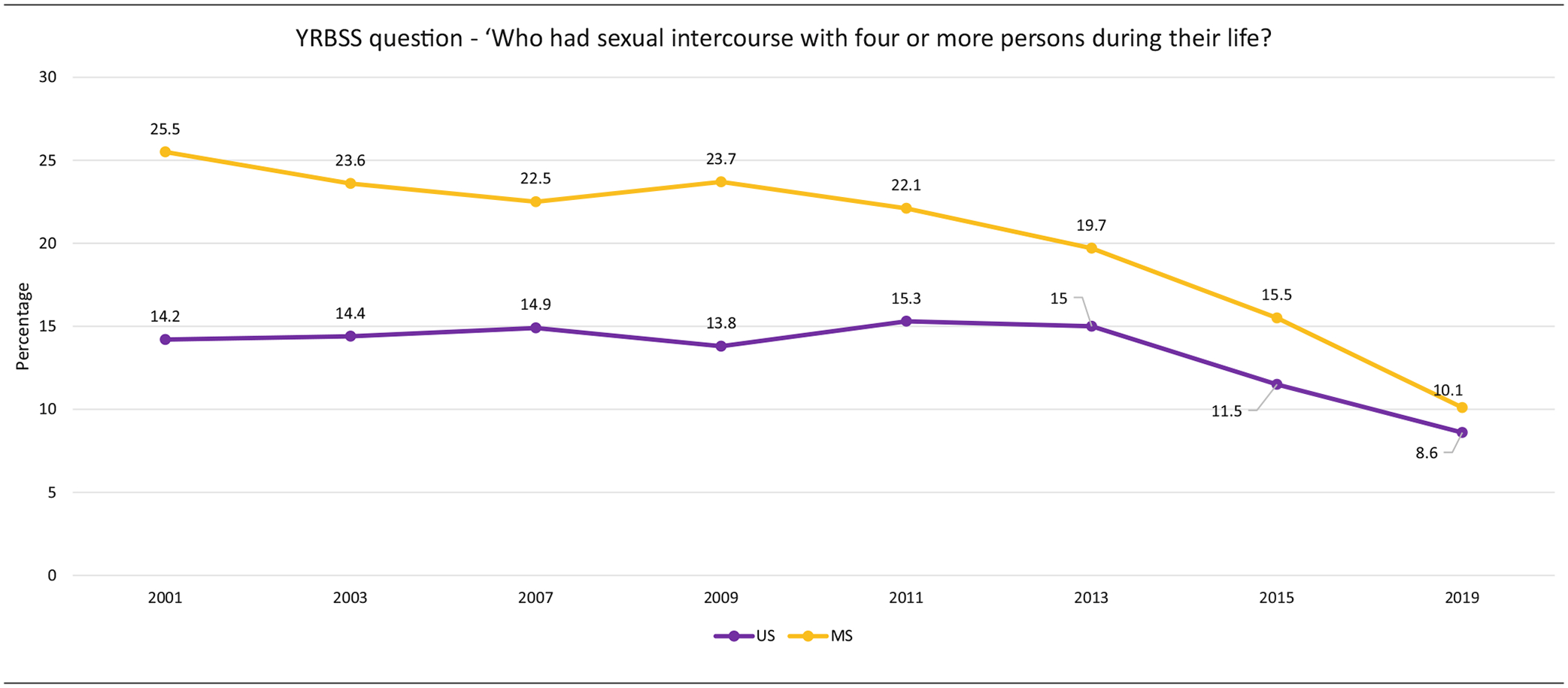
Prevalence change from 2001 to 2019
Figure 4.
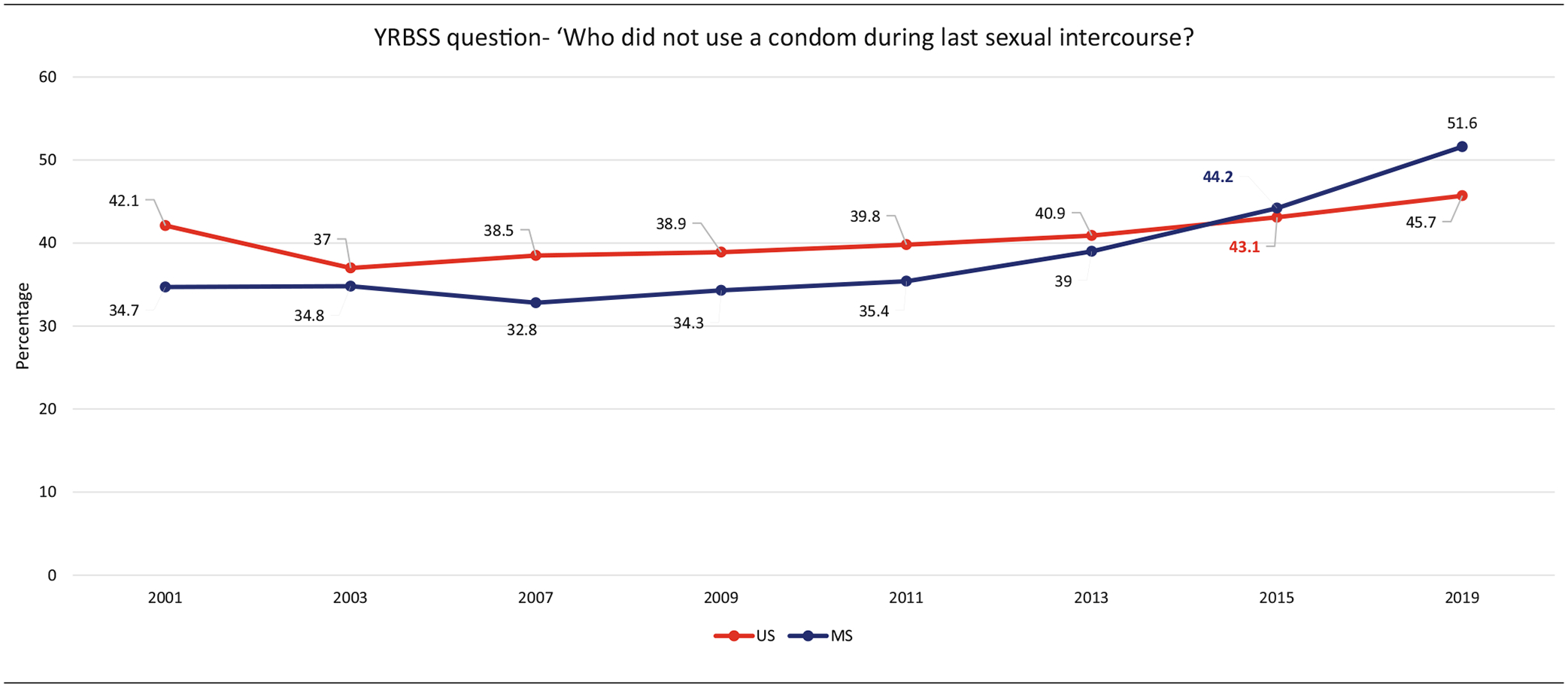
Prevalence change from 2001 to 2019
Figure 2 indicates a significant favorable linear decrease in the prevalence of having first sexual intercourse before the age of 13 (AAPC, −4.6; 95% CI, −7.5, −1.7) in MS participants. There was an average of 4.6% decrease per year from 2001 to 2019. The same results were found at the national level (AAPC, −5.3; 95% CI, −7.5, −3.1). There was an average of 5.3% decrease per year from 2001 to 2019.
Figure 3 indicates a significant favorable linear decrease in the prevalence of having sexual intercourse with multiple partners (AAPC, −5.1; 95% CI, −6.2, −4.0) in MS participants. There was an average of 5.1% decrease per year from 2001 to 2019. The same results were found at the national level (AAPC, −3.3; 95% CI, −4.6, −2.0). There was an average of 3.3% decrease per year from 2001 to 2019.
Figure 4 indicates an unfavorable increase in the prevalence of not having used a condom during last sexual intercourse (AAPC, +2.0; 95% CI, +1.8, +2.2) in MS participants. There was an average of 2% increase per year from 2001 to 2019. The same results were found at the national level (AAPC, +0.4; 95% CI, −0.3, +1.2). There was an average of 0.4% increase per year from 2001 to 2019. Results of the joinpoint trend analysis indicated an increase in the number of US students who reported not using a condom which was not statistically significant (p = .2592) compared to the MS students’ report (p < .0001).
DISCUSSION
This epidemiologic analysis of the YRBSS trends over 2001 to 2019 showed favorable declines in risky sexual risk behaviors in the United States and MS in 3 out of 4 measures. Declining prevalence and trends are reported for “ever had sexual intercourse,” “age of sexual initiation at age 13 or younger,” and “having four or more sexual partners in their lifetime,” are promising. Nevertheless, early sexual debut is still highly prevalent, and the number of those who reported not using condoms is significantly increasing and may offset those benefits.
This study shows a high prevalence of sexual debut before age 13 occurs nationally. However, individual state laws vary according to when it is “age-appropriate” to introduce sex education,17 and curriculums that include sexual risk behaviors are not standardized within or throughout the states.2 Furthermore, avoiding unplanned pregnancies, in addition to reducing STIs and cancer, is of paramount importance. In MS, where the content of SRH education is limited and controlled,17 the adjusted prevalence rates of risky sexual behavior were higher in MS than in the United States for each response and year. These high prevalence rates are comparable to the rates seen in its neighboring southern states (data not shown).10 Fortunately, sex education in MS, as well as in other US states, allows education for dating sexual violence prevention but further measures to expand content to reduce disease are required.
Despite favorable US trends in reduced sexual risk, the CDC reports marked increases in STIs in the 15–24-year-old age groups, especially in the southern US states. MS, Louisiana, South Carolina, and Alabama are consistently ranked in the top 5 for the highest rates of Chlamydia and Gonorrhea infections (Rates of HPV are not reported.).3 STIs are associated with an increased risk of hepatitis, HIV infection, and cancer. The YRBSS data reinforces starting SRH education for boys and girls before the onset of sexual activity, as well as initiating HPV vaccination at age 9 to best prevent cancer.10
Primary cancer prevention information regarding vaccination can be included in SRH education. HPV vaccination is safe and effective in preventing HPV-related cancer.3 However, HPV vaccination rates fail to achieve community immunity to eliminate cancers, and completion rates are lowest in the southern states with the highest cancer rates.4,5 Disparities in HPV vaccine non-completion are higher among rural students versus urban.18 Therefore, to reduce cancer, school-based education coupled with vaccine programs,19 as well as local pharmacy distribution20 are encouraged to conveniently increase vaccine uptake in rural areas.18 However, misinformation regarding HPV vaccination abounds. Studies show HPV vaccination is not associated with increased sexual behavior among young sexually active women in the United States.21 Educators, clergy, and all community groups are encouraged to seek and disseminate evidence-based data.22
The alarming increase in the reported lack of use of condoms brings to light the issue of variations in sex education content in the United States, and in this case, MS. The federal government has advocated, through funding, the use of evidence-based sex education programs; however, individual state policies vary regarding content and life skills within programs. For example, Mississippi laws require sex education but demand parents’ notification and consent, which may result in lower student participation.17 Sex education in MS stresses abstinence and the importance of sex only in marriage. Of note, contraception can only be discussed. Demonstrations or instructions related to the application of condoms are prohibited. A recent trend analysis of 35 states showed a decreased linear trend in SRH instruction, especially in grades 6–8; strengthening education efforts are suggested.2
Peer and parental involvement have a strong influence on risky behaviors. Parental monitoring and communication are directly related to reduced risky sexual behaviors.23,24 Huebner and Howell examined the relationship between adolescent risky sexual behaviors and perception of parental monitoring, communication, and parenting style and found they can be significant predictors of sexual risk-taking.25
Understanding that sexual debut during adolescence is prevalent allows lawmakers, teachers, health care providers, and other adults in their lives to provide essential information to promote healthy sexual behaviors. This information should include waiting until older to have sex and promoting the use of condoms. Saint-Eloi Cadely et al found adolescents who had healthy sex attitudes were more likely to initiate sex at an older age, had fewer lifetime sexual partners, and knew their sexual partners longer.26
Similarly, lawmakers should consider addressing structural disadvantages that increase risky behaviors, such as lack of employment opportunities and safer neighborhoods. When both issues are met, it allows parents opportunities to be more involved in their teen’s day-to-day life.
IMPLICATIONS FOR SCHOOL HEALTH
Risky health behaviors are often started in early childhood or adolescence.1 Some state education policies limit SRH content. Educators, parents, and communities should advocate for policy change.
Limitations
This study had several limitations. First, because the MS YRBSS only contained students from public high schools, adolescents who attend private schools or who are homeschooled were omitted. Next, secondary to the small sample size, only responses from White and Black students were analyzed. Nevertheless, the YRBSS survey has proven reliable over time.
Conclusions
This YRBSS trend analysis produces sound information for educators, health care providers, and local leaders to develop community prevention initiatives to promote health, avoid unplanned pregnancies, and prevent cancer. However, some state education laws remain unchanged despite support for early skills-based instruction in sex education that prevents teen pregnancy, dating violence, disease, and cancer. Law-makers can also use the YRBSS data to rate health policy to influence funding and changes in programs to promote healthy behaviors. Advocacy organizations, such as the CDC, the American Cancer Society, and other local groups are available to assist citizens in providing standardized material for public education programs.
ACKNOWLEDGMENTS
This work was supported by a grant from the Mississippi Nurses Foundation, the University of Mississippi Medical Center School of Nursing and School of Medicine Department of Pathology, the Mississippi Center for Translational Research (National Institute of General Medical Sciences/National Institutes of Health award 1U54GM115428), and the National Institutes of Health Graduate Partnership Program.
Footnotes
Human Subjects Approval Statement. The use of this survey data was deemed exempt from the Institutional Review Board by the University of Mississippi Medical Center as data is accessible in the public domain.
Conflict of Interest
All authors must declare that they have no conflicts of interest.
REFERENCES
- 1.Kann L, Kinchen SA, Williams BI, et al. Youth risk behavior surveillance system (YRBSS)—United States, 1997. State and local YRBSS coordinators. J Sch Health. 1998;68(9):355–369. 10.1111/j.1746-1561.1998.tb07202.x. [DOI] [PubMed] [Google Scholar]
- 2.Young E, Demissie Z, Brener ND, Benes S, Szucs LE. Trends in teaching sexual and reproductive health skills in U.S. secondary schools in 35 states, 2008 to 2018. J Sch Health. 2022. Jul;92(7):711–719. 10.1111/josh.13179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. Sexually Transmitted Diseases (STDs) STI Prevalence, Incidence, and Cost Estimates. https://www.cdc.gov/std/statistics/prevalence-incidence-cost-2020.htm. Accessed June 15, 2022.
- 4.Saraiya M, Unger ER, Thompson TD, et al. U.S. assessment of HPV types in cancers: implications for current and 9-valent HPV vaccines. J Natl Cancer Inst. 2015;107(6):djv086. 10.1093/jnci/djv086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Reagan-Steiner S, Yankey D, Jeyarajah J, et al. National, regional, state, and selected local area vaccination coverage among adolescents aged 13–17 years - United States, 2015. MMWR Morb MortalWkly Rep. 2016;65(33):850–858. 10.15585/mmwr.mm6533a4. [DOI] [PubMed] [Google Scholar]
- 6.Risley C, Stewart MW, Geisinger KR, et al. STRIDES—STudying risk to improve DisparitiES in cervical cancer in Mississippi—design and baseline results of a statewide cohort study. Prev Med. 2021;153:106740. 10.1016/j.ypmed.2021.106740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Clarke MA, Risley C, Stewart MW, et al. Age-specific prevalence of human papillomavirus and abnormal cytology at baseline in a diverse statewide prospective cohort of individuals undergoing cervical cancer screening in Mississippi. Cancer Med. 2021;10(23):8641–8650. 10.1002/cam4.4340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.de Sanjosé S, Brotons M, Pavón MA. The natural history of human papillomavirus infection. Best Pract Res Clin Obstet Gynaecol. 2018;47:2–13. 10.1016/j.bpobgyn.2017.08.015. [DOI] [PubMed] [Google Scholar]
- 9.Schiffman M, Doorbar J, Wentzensen N, et al. Carcinogenic human papillomavirus infection. Nat Rev Disease Primers. 2016;2:16086. 10.1038/nrdp.2016.86. [DOI] [PubMed] [Google Scholar]
- 10.Egemen D, Katki HA, Chaturvedi AK, Landy R, Cheung LC. Variation in human papillomavirus vaccination effectiveness in the US by age at vaccination. JAMA Netw Open. 2022;5(10):e2238041. 10.1001/jamanetworkopen.2022.38041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention. Adolescent and school health—youth risk behavior surveillance system (YRBSS). Data & Documentation 2020. https://www.cdc.gov/healthyyouth/data/yrbs/data.htm. Accessed June 15, 2022.
- 12.Centers for Disease Control and Prevention. 2019. Youth Risk Behavior Surveillance System (YRBSS) Overview. https://www.cdc.gov/healthyyouth/data/yrbs/overview.htm. Accessed June 15, 2022.
- 13.Centers for Disease Control and Prevention. 2019. High School YRBS Mississippi 2019 Results. https://nccd.cdc.gov/youthonline/App/Results.aspx?LID=MS. Accessed June 15, 2022.
- 14.Underwood JM, Brener N, Thornton J, et al. Overview and methods for the youth risk behavior surveillance system -United States, 2019. MMWR Morb MortalWkly. 2020;69(1):1–10. 10.15585/mmwr.su6901a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.National Institutes of Health National Cancer Institute. Division of Cancer Control and Population Sciences. Joinpoint Trend Analysis Softward. Rockville, MD: Joinpoint Trend Analysis Software, Download Joinpoint Desktop Software; 2021. https://surveillance.cancer.gov/joinpoint/download Accessed June 15, 2022. [Google Scholar]
- 16.U.S. Census. Rockville, MD: Quick Facts Mississippi. 2021. https://www.census.gov/quickfacts/MS. Accessed March 3, 2023.
- 17.Mississippi Department of Education. Health Education School-Based Prevention Education. 2021. http:/mdek12.org. Accessed June 15, 2022
- 18.Swiecki-Sikora AL, Henry KA, Kepka D. HPV vaccination coverage among U.S. teens across the rural-urban continuum. J Rural Health. 2019;35(4):506–517. 10.1111/jrh.12353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Centers for Disease Control and Prevention. 2021. Considerations for Planning School-Located Vaccination Clinics https://www.cdc.gov/vaccines/covid-19/planning/school-located-clinics.html. Accessed June 15, 2022
- 20.National Conference of State Legislature. 2020. HPV Vaccine: State Legislation and Regulation. https://www.ncsl.org/research/health/hpv-vaccine-state-legislation-and-statutes.aspx. Accessed June 15, 2022.
- 21.Leidner AJ, Chesson HW, Talih M. HPV vaccine status and sexual behavior among young sexually-active women in the U.S.: evidence from the National Health and Nutrition Examination Survey, 2007–2014. Health Econ Policy Law. 2020;15(4):477–495. 10.1017/s1744133119000136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Duck A, Hall K, Douglas K, Price T. Potential influencers of COVID-19 vaccine acceptance among adults living in the United States who have accepted or plan to accept the COVID-19 vaccine: an online survey. Am J Health Promot. 2022;36:1193–1199. 10.1177/08901171221095351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stattin H, Kerr M. Parental monitoring: A reinterpretation. Child Dev. 2000;71:1072–1085. [DOI] [PubMed] [Google Scholar]
- 24.Santa Maria D, Guilamo-Ramos V, Jemmott LS, Derouin A, Villarruel A. Nurses on the front lines: improving adolescent sexual and reproductive health across health care settings. American journal of nursing. Am J Nursing. 2017;117:42–51. 10.1097/01.NAJ.0000511566.12446.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Huebner AJ, Howell LW. Examining the relationship between adolescent sexual risk-taking and perceptions of monitoring, communication, and parenting styles. J Adolesc Health. 2003;33(2):71–78. 10.1016/s1054-139x(03)00141-1. [DOI] [PubMed] [Google Scholar]
- 26.Saint-Eloi Cadely H, Finnegan V, Spears EC, Kerpelman JL. Adolescents and sexual risk-taking: the interplay of constraining relationship beliefs, healthy sex attitudes, and romantic attachment insecurity. J Adolesc. 2020;84:136–148. 10.1016/j.adolescence.2020.08.010. [DOI] [PubMed] [Google Scholar]


