Abstract
Objective:
The objective of this review was to examine existing literature and conceptually map the evidence for school-based obesity prevention programs implemented in rural communities, as well as identify current gaps in the literature.
Introduction:
Pediatric obesity is a significant public health condition worldwide. Rural residency places children at increased risk of obesity. Schools have been identified as an avenue for obesity prevention in rural communities.
Inclusion criteria:
We considered citations focused on children (5 to 18 years of age) enrolled in a rural educational setting. We included obesity prevention programs delivered in rural schools that focused on nutrition or dietary changes, physical activity or exercise, decreasing screen time, or combined nutrition and physical activity that aimed to prevent childhood obesity. We included all quantitative, qualitative, and mixed methods research designs, as well as text and opinion data.
Methods:
A search was conducted of published and unpublished studies in English from 1990 through April 2020 using PubMed, CINAHL Complete, ERIC, Embase, Scopus, Academic Search Premier, Cochrane Register of Controlled Trials, and ClinicalTrials.gov. Gray literature was also searched. After title and abstract review, potentially relevant citations were retrieved in full text. The full texts were assessed in detail against the inclusion criteria by 2 independent reviewers. Included citations were reviewed and data extracted by 2 independent reviewers and captured on a spreadsheet targeting the review objectives.
Results:
Of the 105 studies selected for full-text review, 72 (68.6%) were included in the final study. Most of the studies (n = 50) were published between 2010 and 2019 and were conducted in the United States (n = 57). Most studies included children in rural elementary or middle schools (n = 57) and targeted obesity prevention (n = 67). Teachers implemented the programs in half of the studies (n = 36). Most studies included a combination of physical activity and nutrition components (n = 43). Other studies focused solely on nutrition (n = 9) or physical activity (n = 9), targeted obesity prevention policies (n = 9), or other components (n = 8). Programs ranged in length from weeks to years. Overall, weight-related, physical activity–specific, and nutrition-specific outcomes were most commonly examined in the included citations.
Conclusions:
Obesity prevention programs that focused on a combination of physical activity and nutrition were the most common. Multiple outcomes were examined, but most programs included weight-specific and health behavior–specific outcomes. The length and intensity of rural school-based obesity prevention programs varied. More research examining scientific rigor and specific outcomes of rural school-based obesity prevention programs is needed.
Keywords: child health, pediatric obesity, preventive health programs, rural health, school health promotion
Introduction
High prevalence rates of pediatric overweight and obesity are global concerns because of their associations with poor health in childhood and adulthood.1–11 Recent data from some countries reveal that prevalence rates of obesity in disadvantaged subpopulations continue to increase,1 and rates of severe obesity in youth are growing.12 It is recognized that people living in rural-designated areas are one of the largest medically under-served populations.13 People living in rural areas encompasses a substantial portion of the world’s population. In 2016, approximately 19% of Americans (60 million), including 13 million children under 18 years of age, lived in a rural area.13 Worldwide, it is estimated that more than 45% of the population, or about 3.5 billion people, live in rural areas.14
Although findings are mixed, living in a rural community has been identified as a risk factor for overweight (ie, body mass index [BMI] greater than or equal to the 85th percentile for age and sex) and obesity (ie, BMI greater than or equal to the 95th percentile for age and sex) in adults and children,15–18 even after adjusting for poverty.17 Multiple factors related to rurality may increase the risk of obesity in adults and children. Residents living in rural areas are more likely to experience economic problems and have limited access to quality physical and mental health care.19 Some findings also suggest higher prevalence of diabetes, stroke, and cancer, as well as worse morbidity and mortality, among individuals living in rural compared with non-rural communities.20,21 Multiple sources indicate that youth from rural areas may engage in more unhealthy behaviors,22 such as spending more time in sedentary activities compared to those living in urban areas.15,16
Additional intersecting features that may influence health disparities in rural communities should also be considered. In some Western countries, such as the United States (US), there is evidence that rural communities are becoming increasingly more racially and ethnically diverse,23 which may result in additional disparity given that the prevalence of overweight and obesity in racial and ethnic minority youth is increasing, while stabilizing in non-Hispanic Whites in the US.12 The intersection between rurality and structural factors, such as minority vs. majority culture, should be considered in the context of obesity risk worldwide.
Prevention efforts in rural and under-served communities are needed to combat obesity in these high-risk groups.24 Schools are one avenue for intervening, given that children spend a large amount of time attending school each week; many children eat multiple meals at school each day, such as breakfast and lunch; and education about healthy nutrition and physical activity (PA) can be incorporated into academic classes. In addition, schools in rural communities and school personnel are well-respected and viewed by parents as important sources of information.25 In addition to educating students, schools may be an avenue to facilitate community health17 by providing parents with education regarding current nutrition and PA recommendations for children, which may not otherwise be available because of limited access and availability of primary care medical services in rural areas.
The role of schools has been recognized in the World Health Organization’s (WHO) Commission on Ending Childhood Obesity, which provided 6 recommendations for policy makers worldwide. One recommendation was specific to the ways schools can be involved to reduce the prevalence of obesity in youth. The school-specific recommendation is to: “Implement comprehensive programmes that promote healthy school environments, health and nutrition literacy and PA among school-age children and adolescents.”26(p.xi) In addition to worldwide efforts, specific countries have also recognized how schools promote improvements in child health. The US Centers for Disease Control and Prevention’s Whole School, Whole Community, Whole Child model27 also emphasizes the role schools play in promoting health in children and adolescents by facilitating the adaptation of health behaviors throughout life, with the recognition that health behaviors are easier to modify—and more effectively modified—when addressed in youth as opposed to changing unhealthy behaviors in adults.27
Given the importance of schools in promoting health in children, in recent years researchers have developed, implemented, and evaluated school-based obesity prevention programs focused on lifestyle behaviors and the school environment, such as healthy diet, increased PA, a motivating environment, educational curricula, and training teachers28–30; however, it is unclear what obesity prevention strategies have been implemented in schools in rural communities. Programs implemented in rural communities may need to take into account limited access to heathy foods and places to engage in safe PA, transportation and time-related issues (eg, need to travel farther distances), and economic-related issues.31 A preliminary search for existing systematic and scoping reviews was conducted in January 2018 to locate literature related to rural school-based obesity prevention programs, and no systematic reviews were identified. Thus, the current review was needed to increase understanding about the types of school-based obesity prevention programs that have been implemented in rural schools in order to inform future development of school-based obesity prevention programs in rural communities.
The objective of this scoping review was to examine the existing literature related to school-based obesity prevention programs implemented in rural communities, conceptually map the evidence, and identify current gaps in the literature.
Review questions
What types of school-based obesity prevention programs have been implemented in rural schools?
What specific elements/components of school-based obesity prevention programs have been implemented in rural schools?
What outcomes have been reported regarding school-based obesity prevention programs that have been implemented in rural schools?
Inclusion criteria
Participants
This review considered studies that included children aged 5 to 18 years of age who were enrolled in an institution that provided instruction and teaching of children, such as elementary, middle, or high school, and were conducted in a rural setting. Elementary schools were considered those that generally provided instruction to children in the first 4 years of formal education and also included schools that taught children through the first 8 years of instruction and self-identified as elementary. High school was defined as schools that included grades 9–12 or 10–12. Middle schools usually included grades 5–8 or 6–8, and were defined as such for this study. Schools included those classified as private, parochial, or publicly funded. Private schools were defined as schools that were supported by a non-governmental agency; public schools were free, tax-supported, and controlled by a local governmental authority; and parochial schools were defined as private schools maintained by a religious body. Children who were home-schooled or in an alternative setting, such as juvenile detention or hospitalized for prolonged periods, were excluded.
Concept
This scoping review considered studies about school-based obesity prevention programs implemented in rural schools, including, but not limited to, those focused on nutrition and dietary changes, PA or exercise, decreasing screen time, or mixed nutrition and PA programs aimed at childhood obesity prevention. Physical activity was defined as bodily movement produced by skeletal muscle contraction with increased energy expenditure, whereas exercise, a kind of PA, is planned, structured, repetitive movement that is often intentional and aimed at improving or maintaining health or fitness. We also considered whether the school-based obesity prevention programs implemented in rural schools incorporated behavioral components. Behavioral components included goal-setting, monitoring, self-regulation strategies, rewards/incentives, time management skills, counseling, and/or strategies to improve body image.
The school-based programs could be designed and delivered by health professionals, members of a community organization, or educators whose occupation is to teach; however, programs had to be delivered in the school setting. Health professionals could be registered dietitians, occupational therapists, physical therapists, public health practitioners, licensed nurses, dentists, physicians, pharmacists, nutritionists, mental health providers (eg, counselors, psychologists), or health educators. Studies that focused on physical fitness as an outcome and those conducted by health paraprofessionals, such as dental hygienists or nursing assistants, were excluded. Studies with obesity programs delivered to children outside of elementary, middle, or high schools, or programs offered at community facilities were also excluded.
Context
The context for this scoping review focused on schools in rural settings in any country. “Rural” is usually defined by individual countries13,14,32,33 and is often defined by exclusion, such that any area that is not urban is considered rural.34,35 This review considered any study in which the authors conducting the study classified the area as rural, as well as any study in an area designated as rural by the country’s census geographic entity.
Types of sources
This scoping review considered quantitative, qualitative, and text and opinion data. For quantitative studies, the review considered both experimental and quasi-experimental quantitative study designs including randomized controlled trials, non-randomized controlled trials, before and after studies, and interrupted time-series studies. In addition, analytical observational studies, including prospective and retrospective cohort studies, case-control studies, analytical cross-sectional studies, and systematic reviews were considered for inclusion. This review also considered descriptive observational study designs including case series, individual case reports, descriptive cross-sectional studies, and gray literature for inclusion.
Qualitative studies that focused on qualitative data, including, but not limited to, designs such as phenomenology, grounded theory, ethnography, qualitative description, action research, and feminist research were considered. Text and opinion papers were also considered for inclusion.
Methods
This review was conducted in accordance with an a priori protocol36 and the JBI methodology for scoping reviews.37
Search strategy
The search strategy aimed to find both published and unpublished studies. A three-step strategy was used, and included electronic and manual searches of reference lists, as well as government or agency websites for gray literature. The initial step included a limited search of MEDLINE (PubMed) and CINAHL, and an analysis of the text words contained in the title and abstract and of the index terms used to describe the articles. This informed the development of the search strategy, which was tailored for each information source. The second step was a search using all keywords and index terms identified in the electronic databases listed below. The third step was to search reference lists of included studies, trial registers, and unpublished studies.
Studies published in English since 1990 were included, as the rise in prevalence of childhood obesity began to be recognized during the 1980s in the US, closely followed by recognized increases in trends in other developed countries. In addition, surveillance data and analysis of rates frequently use the baseline comparator of 1990 or later.26,38–40
The databases searched included PubMed (US National Library of Medicine), CINAHL Complete (EBSCO), ERIC (EBSCO), Embase (Elsevier), Scopus (Elsevier), and Academic Search Premier (EBSCO). The trial registers searched included Cochrane Register of Controlled Trials (Wiley) and ClinicalTrials.gov. The search for unpublished studies included ProQuest Dissertations and Theses Sciences and Engineering Collection (ProQuest), OpenGrey, Open Access Theses and Dissertations, Directory of Open Access Journals, and OCLC PapersFirst. Organization websites searched included the Centers for Disease Control and Prevention (MedNar), and the US Department of Education. All searches were performed in April 2019 and updated in April 2020. The full search strategies are presented in Appendix I.
Study selection
Following the search, all identified citations were imported into EndNote v.20 (Clarivate Analytics, PA, USA) and duplicates were removed. Titles and abstracts of citations were screened by 2 independent reviewers (CL, JR, XG, MH) and compared to the inclusion criteria for the scoping review. Potentially relevant studies were retrieved in full and their citation details imported into the data extraction spreadsheet in MS Excel (Redmond, Washington, USA). The full text of selected citations was assessed in detail against the inclusion criteria by 2 independent reviewers (CL, JR, XG, AG, CC, MR). Full-text studies that did not meet inclusion criteria were excluded. Reasons for their exclusion are reported in Appendix II. Disagreements that arose between the reviewers at each stage of the study selection process were resolved through consensus or by a third reviewer (CL, JR). The results of the search are reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram.41
Data extraction
Data were extracted from studies included in the scoping review by 2 independent reviewers using an a priori data extraction tool that was modified from the JBI extraction tool (CL, JR, XG, AG, CC, MR). The data extracted included specific author details, year and country of publication, defined rural designation, type of school-based prevention or intervention used, intervention components, duration of intervention, provider of the intervention, study sample and size (when reported), types of outcomes, and key findings. Any disagreements that arose between the reviewers were resolved through discussion or with a third reviewer (CL, JR).
Data analysis and presentation
While addressing the objectives proposed in the scoping review protocol, common groupings across the included articles were analyzed. The first and second authors (CL and JR) reviewed the data extracted from each included study to identify key features of school-based obesity prevention programs in rural communities. Results were later verified by co-authors. Aligned with the PCC mnemonic (participants, concept, context), only 2 of the components were appropriate for analysis and discussion based on the review questions and literature analysis. “Participants” and “concept” were analyzed and discussed because context was limited to rural school settings and invariant given the inclusion criteria for this review.
Results
Source inclusion
Through database searches conducted in April 2019 and updated in April 2020, 3368 records were identified, and 1310 duplicates were removed. An additional 13 records were identified through reference list searches. A total of 2071 studies were screened by title and abstract for inclusion. Of those, 1966 were excluded. The remaining 105 records were assessed for inclusion based on full-text review, and 33 full-text records were excluded (see Appendix II for reasons for exclusion). The final data set consisted of 72 citations for data extraction. The search results are summarized in a PRISMA flow diagram (Figure 1).41
Figure 1:
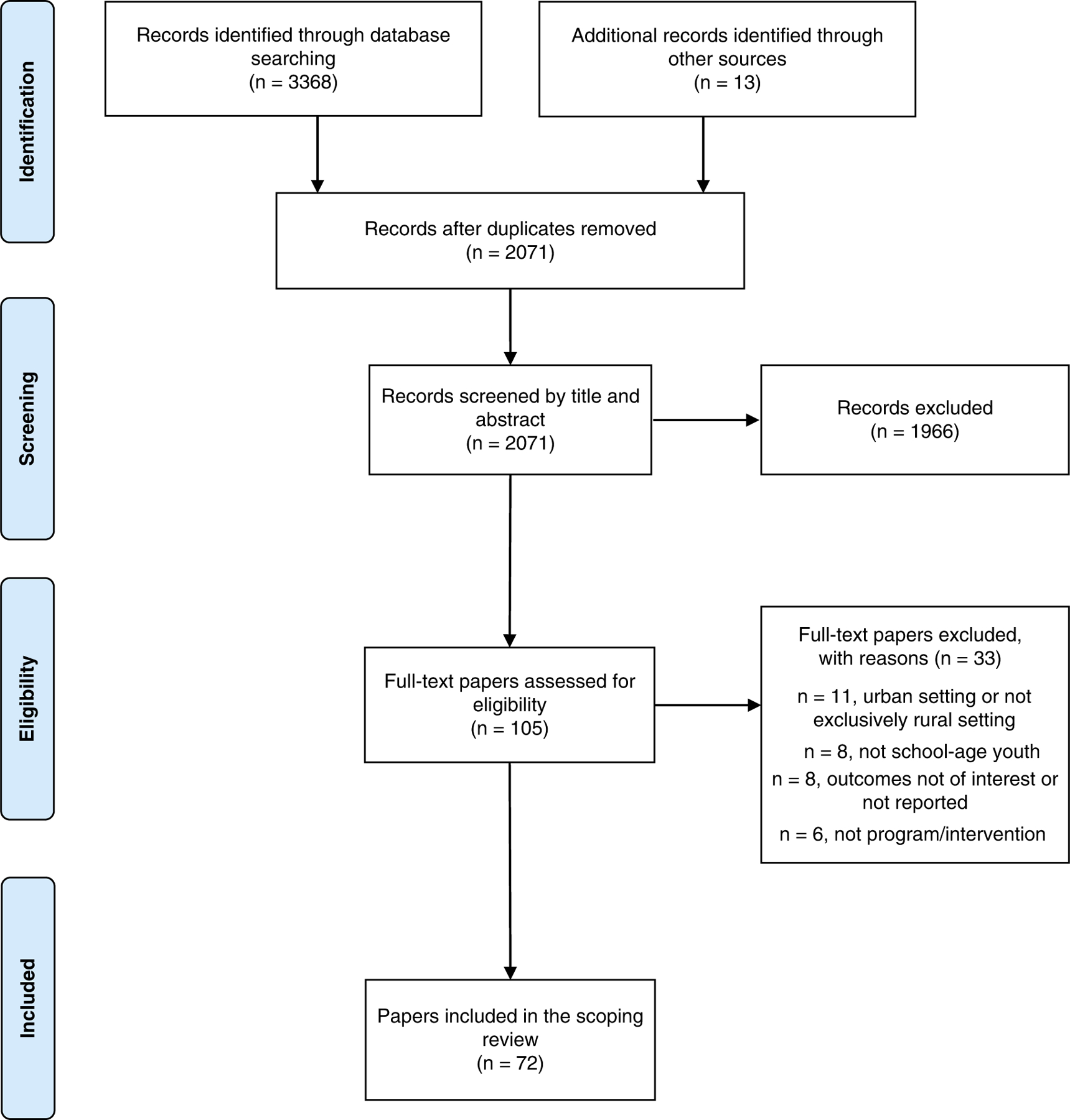
Search results and source selection and inclusion process41
Characteristics of included sources
Three studies (4.2%) were published in the 1990s,42–44 18 (25.0%) were published between 2000 and 2009,45–62 50 (69.4%) were published between 2010 and 2019,63–112 and 1 (1.4%) was published in 2020.113
Fifty-seven (79.2%) of the studies were conducted in the US,43–55,57–63,65–71,75–81,84,85,87,89–104,106,108,109,113 four (5.6%) in Australia,56,73,107,112 3 in Canada (4.2%),64,74,82 2 in China (2.8%),8,110 1 each in Chile,83 Italy,42 New Zealand,72 Spain,86 and Taiwan,111 and 1 additional study105 that was conducted in multiple countries (US, Australia, and England).
In regard to definition of rurality, most authors reported that participants lived in a rural community or attended a rural school but did not provide a definition of how rurality was identified in their manuscript. Specifically, only 14 articles (19.4%) defined or described how rurality was determined in their manuscript. In terms of study designs, 27 (37.5%) used pre-post designs, 21 (29.2%) implemented a randomized controlled trial (RCT) design, 11 (15.3%) reported using quasi-experimental designs, 5 (6.9%) used qualitative methods,62,67,71,98,107 3 (4.2%) used both pre-post and qualitative designs,48,59,64 3 (4.2%) used cross-sectional designs,42,89,90 1 (1.4%) used both RCT and quasi-experimental designs,105 and 1 (1.4%) study was descriptive.81
Extracted data from each of the included citations are presented in Appendix III.
Review findings
Review question #1: What types of school-based obesity prevention programs have been implemented in rural schools?
Population: children or adolescents
Of the 72 manuscripts, the majority (n = 57; 79.2%) were implemented with children, conceptualized as elementary or middle school students. Additionally, 9 (12.5) studies targeted high school students or adolescents,55,66,69,73,91,99,102,106,113 and 6 (8.3%) were obesity prevention programs that included both children and adolescents (elementary, middle, and high school students).64,74,81,82,88,97
Concept: program type (prevention vs. intervention)
Of the school-based obesity programs, the majority (n = 67; 93.1%) were identified as prevention programs.42–44,46–104,106,108,109,111,112 Four (5.6%) were identified as intervention programs targeting student participants with overweight or obesity, or their engagement in specific health-related behaviors,45,107,110,113 such as reported time engaged in moderate to vigorous PA or recreational screen time.107 One (1.4%) additional study was a systematic review that included a combination of prevention and intervention programs.105
Concept: program providers
Teachers were identified as implementing the obesity prevention program in half of the studies (n = 36; 50%). Of the programs implemented by teachers, 7 were specifically identified as physical education teachers.49,53,59,87,90,100,110 Twelve manuscripts reported researchers or study staff as the primary providers of the obesity prevention program.56,57,60,65,71,74–76,84,104,109,111 Other providers included peers, such as older students serving as mentors (n = 8; 11.1%),54,55,77,82,94,106,107,113 nutritionists or dietitians (n = 7; 9.7%),44,46,61,66,97,105,110 community member volunteers (n = 4; 5.6%),43,49,61,105 members of county extension offices (n = 3; 4.2%),47,61,98 college undergraduate or graduate students (n = 3; 4.2%),44,86,95 trained lifestyle coaches (n = 2; 2.8%),78,85 school nurses (n = 1; 1.4%),95 and other health care professionals (n = 5; 6.9%).46,56,63,69,92 It is important to note that some of the articles reported including multiple types of program providers (eg,66,91); thus, those articles are included more than once in the numbers reported here. However, 13 articles (18.1%) did not provide specific information on who implemented or provided the school-based obesity prevention program in rural schools.51,52,58,62,73,79,81,83,88,89,99,102,112
Review question #2: What specific elements/components of school-based obesity prevention programs have been implemented in rural schools?
Concept: program components
With regard to the program component concept, some of the articles included in this scoping review were categorized as including multiple components; thus, they may be included and discussed under more than one component category.
Exercise/physical activity.
Specific to program components, only 9 (12.5%) studies focused on exercise or PA as an obesity prevention program.53,55,71,87,89,90,100,106,113 Several of the studies also included a PA policy or program evaluation component, such as consistency of schools’ implementation of PA mandates90 and Walk to School Programs.89 Two of the programs focusing on PA also incorporated behavioral components.71,113 The school-based intervention program developed by Smith et al.113 taught self-regulation skills (eg, goal-setting, self-monitoring, time management, self-reward) related to PA in mentored and non-mentored groups. The program by Conway et al.71 consisted of setting goals and keeping logs (ie, behavioral components).
Dietary/nutrition.
Nine (12.5%) of the included studies primarily focused on nutrition or dietary behaviors as the prevention component.42,54,75,79,91,92,97,98,102 Two of the dietary interventions also incorporated behavioral components.79,97 Murimi and colleagues’97 program included medical screening for obesity, diabetes, cholesterol, and high blood pressure; individualized nutrition education and action plans based on screening findings; and group nutrition education classes for rural middle school and high school students. Moss et al.79 implemented nutrition education via the dietary traffic light system and farm tour, and outcomes primarily focused on specific nutritional components, such as fiber and eating vegetables at school.
Combined dietary and physical activity.
Forty-three (59.7%) of the included citations incorporated both nutrition and PA in the school-based obesity prevention program. Seven of the reviewed studies included behavioral components, as well as PA and nutrition, in their prevention programs.48,61,64,70,82,101,111
Policy.
Nine (12.5%) articles focused on policy related to PA or diet as the pediatric obesity prevention component.58,62,69,78,81,85,89–91
Other obesity prevention programs.
Eight (11.1%) articles included in the review did not focus on diet, PA, combination of diet and PA, or policy and were classified as “other.”51,56,63,73,88,105,109,112
As described previously, 12 (16.7%) citations included behavioral components, 7 (9.7%) were in programs with a combined focus on nutrition and PA,48,61,64,70,82,101,111 2 (2.8%) focused on combined nutrition and behavioral components,79,97 2 (2.8%) programs included PA and behavioral components,71,113 and 1 (1.4%) included policy and behavioral aspects.69
Concept: length of prevention programs
The length of the prevention programs was typically implemented according to the school/academic calendar in the rural community. Specifically, 9 out of 72 (12.5%) reported being implemented across 1 school year or 2 academic semesters. In addition, 10 (13.9%) were described as being implemented during 1 semester, 22 (30.6%) reported that the prevention program was less than 1 semester in length, and 1 study74 reported being conducted over more than 1 semester but not the entire school year. Other prevention programs were reported as being conducted over the course of multiple school or calendar years (n = 20; 27.8%). Ten articles (13.9%) did not include information regarding the length of the prevention program described/evaluated.
Review question #3: What outcomes have been reported regarding school-based obesity prevention programs that have been implemented in rural schools?
Concept: outcomes by program components
Exercise/physical activity.
Of the 9 PA programs, 6 examined weight-related outcomes, which were conceptualized as weight, height, BMI, BMI percentiles, BMI z-scores, relative BMI, body fat percentage, or waist circumference. PA-specific outcomes, such as pedometer steps, self-reported PA, and physical fitness, were also included as outcomes in 5 of these programs.53,55,87,89,90 Self-efficacy and barriers to PA were also outcomes included in 3 the programs.53,55,87 Conway and colleagues71 conducted focus groups about their PA and behavioral program; thus, their reported outcomes were qualitative.
Dietary/nutrition.
Of the 9 dietary/nutrition interventions and related policies, 3 included weight-related outcomes42,97,102 and 1 assessed other related health outcomes,97 specifically outcomes from blood work examining cholesterol and triglycerides. Some programs also included nutrition consumption54,75,79,92,102 and/or nutrition knowledge54,75,79,97 as specific outcomes. One of the combined nutrition and policy programs specifically included water and sugar-sweetened beverage consumption as their outcomes of interest.91 In addition to dietary-specific outcomes, Muth and colleagues also included PA-related outcomes in their study.54 Rodriguez and colleagues98 conducted focus groups that qualitatively examined students’ perceptions of a school garden program.
Combined dietary and physical activity.
Of the 43 studies reviewed of combined PA and dietary programs, 33 examined BMI or other weight-related outcomes. In addition, 33 incorporated outcomes specific to PA and diet, 9 included health-related outcomes,44–46,49,60,74,77,94,103 and 5 examined outcomes focused on psychological functioning, such as body image, self-esteem, and depressive symptoms.49,65,82,93,101 Two citations reported qualitative outcomes.64,67 The seven combined PA and nutrition programs that also included behavioral components all examined multiple outcomes.48,61,64,70,82,101,111
Policy.
Three of the policy-focused studies examined weight-related outcomes.69,81,90 Ling and colleagues78,85 implemented a multicomponent, school-level intervention, and focused on PA and dietary behavior outcomes. Three additional citations also included PA- and dietary-specific outcomes to examine policy-related programs. Schetzina and colleagues62 described the design of an obesity-prevention program in response to a new state policy and included outcomes from a qualitative community-needs assessment. Belansky et al.58 included the results of key informant interviews after the implementation of their policy-specific prevention program in rural elementary schools. Ritchie’s69 policy intervention also incorporated behavioral components (eg, cognitive-behavioral skill building), and examined beliefs and perceived difficulties related to healthy lifestyle behaviors.
Other obesity prevention programs.
Five of the other programs incorporated weight-related outcomes.56,73,88,105,112 Some citations also included dietary- and PA-specific outcomes.88,105,109,112 Schiller and colleagues’51 Program ENERGY included outcomes specific to health and science knowledge, and interest in science and health-related careers. Other policy-related programs included outcomes from qualitative interviews with school stakeholders.109,112 Gabriele and colleagues63 described treatment implementation information from an internet educational intervention that incorporated brief behavioral counseling related to weight management depending on the weight status of the student (non-overweight vs. overweight) and only reported implementation related outcomes.
Discussion
Pediatric overweight and obesity are a significant public health burden, and youth in rural areas worldwide are disproportionately impacted. Rural schools are one potential avenue for pediatric obesity prevention and intervention efforts. However, little is known about the components and effectiveness of rural school-based obesity prevention and treatment programs. The purpose of the current scoping was to answer the following questions: i) what types of school-based obesity prevention programs have been implemented in rural schools, ii) what specific elements/components of school-based obesity prevention programs have been implemented in rural schools, and iii) what outcomes have been reported regarding school-based obesity prevention programs that have been implemented in rural schools?
Summary of evidence
We identified 72 citations for inclusion in this scoping review. The majority of the included programs conducted in rural schools were implemented in North America during or after 2010. Among the other studies reviewed, 21 were published before 2009. Five were conducted in Australia or New Zealand, 3 were conducted in Asia, 2 in Europe, 1 in South America, and 1 in multiple countries. Only 14 of the included citations specifically described how rurality was defined or conceptualized in their study. The remaining reported the participants or the schools were located in a rural community.
Review question #1: what types of school-based obesity prevention programs have been implemented in rural schools?
Most of the studies included in this scoping review were implemented with children (elementary and middle school students) and focused on prevention (ie, included children with varying weight status) rather than treatment interventions (ie, included only those who were overweight or obese). Teachers were the primary interventionists, which is not surprising given that the programs were implemented in the school setting. Teachers implementing prevention programs in rural schools could potentially help with program sustainability. The length of the programs implemented in rural schools varied, with most lasting either less than 1 semester in length or over several years.
Review question #2: What specific elements/components of school-based obesity prevention programs have been implemented in rural schools?
The most common elements of school-based obesity prevention programs implemented in rural schools included a combination of nutrition and PA components. Some studies included solely nutrition or PA, and a small number focused on upstream programs aimed at policy changes locally within schools or more broadly with mandates that affected all schools.
Review question #3: What outcomes have been reported regarding school-based obesity prevention programs that have been implemented in rural schools?
Most of the studies reviewed examined multiple outcomes, with weight-related outcomes and PA/nutrition-specific outcomes being the most commonly examined. Several studies reported outcomes from blood work, such as high-density lipoproteins or triglycerides, and some examined psychological outcomes (eg, self-esteem, depressive symptoms), which are associated with pediatric overweight and obesity.
Additional information
While conducting this scoping review, we identified an exploratory interest in understanding characteristics of obesity prevention programs in rural schools that resulted in weight improvements. Therefore, we examined the articles that reported weight changes in more detail. Of the 72 articles included in this review, 14 (19.4%) reported improvements in weight-related outcomes.45,56,57,68,73,82–84,91,95,99,108,110,112 Two of these programs were identified as treatment programs that only included children who were overweight or obese.45,110 The majority of these programs included components focusing on nutrition and exercise, and a few described the inclusion of family involvement and community-based aspects. The programs ranged in length from 2 months to 6 years, but also ranged in intensity from every school day to weekly and monthly implementation.
Overall, conclusions cannot be made from this information because this review did not assess the quality of the research evidence or systematically examine outcomes. There was also variability in the programs that indicated significant improvements in weight outcomes. However, in general, it appears that in rural school-based settings, combined nutrition and PA obesity prevention programs that provide a high dose of prevention/intervention (length, intensity) may be the most effective at impacting weight-related outcomes. Future meta-analytic research is needed to confirm this finding.
Limitations
There are limitations of the current scoping review that are important to consider. First, the lack of information presented in some of the citations made it difficult to determine inclusion/exclusion criteria, as well as to extract data of interest. For example, most of the included citations did not use a specific definition of rurality, but instead the authors reported the school was located in a rural area or community. The definition of what constitutes a rural area is often ambiguous, and standards are not consistent across counties, given that it is often defined by each country differently.32,33 Many definitions of rurality are based on exclusion, such that any area not considered urban is considered rural.35 In addition, our search included “rural” as a term, which may have impacted our ability to include some studies if they were conducted in a rural community but were not identified as such by the authors. Whether the prevention programs were identified as school-based was also at times unclear during the initial citation review. For example, prevention programs that were implemented after school were not included, although they may have been identified as a school-based obesity prevention program by the authors. In addition, extracting specific information about the school-based prevention programs, such as treatment components, was difficult due to limited descriptions or information provided.
Second, we extracted data regarding the providers of the prevention programs but did not extract data on the training the providers may have received or their educational backgrounds. This information would be helpful for those interested in developing obesity prevention programs in rural schools, but it was often not described in the included citations. Also, regarding length of the programs, based on information included in the citations and what was able to be extracted, it was difficult to determine the intensity or dose of the reviewed prevention programs, such as frequency of treatment or hours of prevention/treatment received by students. Because there are specific recommendations regarding pediatric obesity treatment dose (eg, US Preventive Services Task force recommends 26 or more hours of treatment in one year114), this information could be helpful to extract in future scoping and systematic reviews of school-based obesity prevention programs. This could provide additional information regarding the potential impact of dose- and weight-related outcomes and allow comparisons to expert recommendations.
Third, although this information was not specifically intended to be extracted, some authors included information about specific theories that informed their obesity prevention program.66,80,102 For many of the other articles, it was difficult to determine what theories, if any, had guided program development and implementation. It is unclear how this may impact program components or weight-related outcomes in school-based obesity prevention programs in rural communities.
Fourth, although examining the scientific rigor of the included citations was beyond the scope of this scoping review, it is important to consider both the statistical and clinical significance of the findings reported in the included studies. Many of the studies included multiple weight-related, dietary, and PA outcomes requiring multiple statistical analyses and comparisons. Overall, there were limited significant findings across all the reviewed citations, and some of the differences reported could be considered secondary outcomes (ie, the study was not powered to determine differences in specific secondary outcome). Thus, some of the findings could be the result of error due to multiple comparisons. Methodological and statistical rigor of school-based obesity prevention programs in rural communities are needed to guard against exaggerated effectiveness or ineffectiveness of these interventions (for example, see Brown et al.115). Future systematic reviews and meta-analyses are needed to better understand the methodological rigor of research previously conducted in this area.
Conclusions
This scoping review identifies and describes school-based obesity prevention programs that have been implemented in rural communities. Despite the heterogeneity of the programs reviewed, prevention programs that focus on a combination of PA and nutrition appear to be the most common. The length and intensity of the school-based obesity prevention programs reviewed varied. This scoping review provides important directions for future research.
Implications for research
First, future researchers should provide more specific information about obesity prevention programs and the schools and communities where they are implemented. Specifically, understanding how rurality is conceptualized is important because there is increasing recognition that the extent of rurality in the community is associated with poor health outcomes.116 This could impact the implementation and effectiveness of school-based obesity prevention programs. Additionally, there is a need for better reporting of the specific characteristics of programs implemented in rural schools, such as the training of providers, theories that informed program development, specific program components (including behavioral components utilized), and amount of time students are exposed to the prevention program. In addition, it would be helpful for authors to identify what specific aspects of their prevention programs have been modified due to being implemented in a rural location. School-based obesity prevention programs implemented in rural areas could help inform programs in other under-served and under-resourced communities, even if they are not located in a rural community.
Second, because the majority of programs included multiple components, it was difficult to ascertain critical components of school-based obesity prevention programs in rural areas. The studies in this review reported that few (if any) PA, dietary, or policy programs alone impacted weight status. However, more dismantling studies via meta-analyses should be conducted to determine if critical components of these programs can be identified. This would potentially save resources (eg, time, money) as a result of implementing future programs that have limited evidence of success.
Third, more rigorous research designs and outcome assessments should be included in future research, particularly RCTs, and future meta-analyses should focus on synthesizing the specific health- and school-related outcomes of the interventions. In addition, long-term follow-up of outcomes are needed given that weight and other related outcomes may take longer to change after the implementation of prevention programs.
Finally, given the structural nature of conditions that shape health in rural areas, including the increasing risk of obesity in adults and youth, multi-level structural interventions that target root causes of disparities (eg, socioeconomic factors, limited access to physical and mental health care) should be developed and evaluated in under-served rural community-based settings.
Funding
Research reported in this publication was supported by the National Institute of General Medical Sciences of the National Institutes of Health under Award Number 5U54GM115428. The authors participated in the Community Engagement and Outreach Core Working Group, a resource of this award. JR, AG, and CC received funding support though this award. CL received partial funding support through the Federal Office of Rural Health Policy (FORHP), Health Resources and Services Administration (HRSA), US Department of Health and Human Services (HHS) under cooperative agreement award no. 6 U66RH31459-02-03, and partial funding support from NIH/ECHO/ISPCTN 8UG1OD024942-02 and U24 OD02495. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Appendix I: Search strategy
PubMed (US National Library of Medicine)
Search conducted: April 27, 2020
| Search | Query |
|---|---|
| #1 | prevent*[tw] OR intervention[tw] OR program[tw] OR “Health Promotion”[Mesh] OR “health promotion”[tw] |
| #2 | “rural population”[MeSH] OR rural[tw] |
| #3 | schools[MeSH] OR “school based”[tw] OR school-based[tw] OR “school health services”[MeSH] OR school*[tw] |
| #4 | obes*[tw] OR obesity[MeSH] OR “pediatric obesity”[MeSH] |
| #5 | teen*[tw] OR child[tw] OR children[tw] OR “school age”[tw] OR “school aged”[tw] OR child[MeSH] OR “child, preschool”[MeSH] OR adolescent [MeSH] OR adolescen*[tw] OR “high school”[tw] OR “middle school”[tw] OR “elementary school”[tw] OR “pre k”[tw] OR preschool[tw] OR “primary school”[tw] OR youth[tw] OR pediatric[tw] OR paediatric[tw] OR “secondary school”[tw] OR “head start”[tw] OR “nursery school”[tw] OR “Schools, Nursery”[Mesh] |
| #6 | #1 AND #2 AND #3 AND #4 AND #5 |
Limited to English language and years 1990—present
413 results
CINAHL Complete (EBSCO)
Search conducted: April 23, 2020
| Search | Query |
|---|---|
| #1 | prevent* OR intervention OR program OR “health promotion” OR (MH “Health Promotion”) |
| #2 | (MH “Rural Areas”) OR (MH “Rural Population”) OR rural |
| #3 | (MH “Schools”) OR “school based” OR school-based OR school* |
| #4 | obes* OR (MH “Obesity”) OR (MH “Pediatric Obesity”) |
| #5 | (MH “Adolescence”) OR (MH “Child”) OR (MH “Child, Preschool”) OR teen* OR child OR children OR “school age” OR “school aged” OR adolescen* OR “high school” OR “middle school” OR “elementary school” OR “pre k” OR preschool OR “primary school” OR youth OR pediatric OR paediatric OR (MH “Students, High School”) OR (MH “Schools, Middle”) OR (MH “Schools, Secondary”) OR “secondary school” OR (MH “Schools, Elementary”) OR (MH “Students, Elementary”) OR “head start” OR “nursery school” OR (MH “Schools, Nursery”) |
| #6 | #1 AND #2 AND #3 AND #4 AND #5 |
Limited to English language and years 1990—present
255 results
ERIC (EBSCO)
Search conducted: April 23, 2020
| Search | Query |
|---|---|
| #1 | prevent* OR intervention OR program OR DE “Prevention” OR DE “Health Programs” OR DE “Programs” OR DE “Health Promotion” OR DE “Intervention” |
| #2 | rural OR DE “Rural Areas” OR DE “Rural Environment” OR DE “Rural Population” OR DE “Rural Schools” |
| #3 | DE “Schools” OR “school based” OR school-based OR school* |
| #4 | obes* OR DE “Obesity” |
| #5 | teen* OR child OR children OR “school age” OR “school aged” OR adolescen* OR “high school” OR “middle school” OR “elementary school” OR “pre k” OR preschool OR “primary school” OR youth OR pediatric OR paediatric OR “secondary school” OR DE “Adolescents” OR DE “Children” OR DE “Early Adolescents” OR DE “Preadolescents” OR DE “Late Adolescents” OR DE “Youth” OR DE “High School Students” OR DE “Secondary School Students” OR DE “Young Children” OR DE “Preschool Children” OR DE “Middle School Students” OR DE “Middle Schools” OR DE “Secondary School Students” OR DE “Secondary Schools” OR DE “Elementary School Students” OR DE “Elementary Schools” OR “head start” OR “nursery school” OR DE “Nursery Schools” |
| #6 | #1 AND #2 AND #3 AND #4 AND #5 |
Limited to English language and years 1990—present
55 results
Embase (Elsevier)
Search conducted: April 28, 2020
| Search | Query |
|---|---|
| #1 | prevention:ti,ab OR prevent:ti,ab OR ‘prevention and control’/exp OR ‘prevention’/exp OR intervention:ti,ab OR program:ti,ab OR ‘health program’/exp OR ‘health promotion’/exp |
| #2 | ‘rural area’/exp OR ‘rural population’/exp OR ‘rural health care’/exp OR ‘rural health’/exp OR rural:ti,ab |
| #3 | ‘school’/exp OR “school based”:ti,ab OR “school-based”:ti,ab OR school:ti,ab OR ‘school health service’/exp |
| #4 | ‘obesity’/exp OR ‘adolescent obesity’/exp OR ‘childhood obesity’/exp OR obese:ti,ab OR obesity:ti,ab |
| #5 | ‘juvenile’/exp OR ‘adolescent’/exp OR ‘child’/exp OR ‘preschool child’/exp OR ‘school child’/exp OR teen:ti,ab OR teenager:ti,ab OR teenaged:ti,ab OR adolescent:ti,ab OR adolescence:ti,ab OR children:ti,ab OR child:ti,ab OR ‘school age’/exp OR ‘school age population’/exp OR “school aged”:ti,ab OR “school age”:ti,ab OR ‘high school’/exp OR ‘high school student’/exp OR ‘middle school’/exp OR ‘middle school student’/exp OR ‘primary school’/exp OR ‘elementary student’/exp OR “elementary school”:ti,ab OR “pre k”:ti,ab OR ‘preschool’/exp OR ‘preschoolers’/exp OR youth:ti,ab OR pediatric:ti,ab OR paediatric:ti,ab OR ‘secondary schools’/exp OR “head start”:ti,ab OR ‘nursery school’/exp |
| #6 | #1 AND #2 AND #3 AND #4 AND #5 |
Limited to English language and years 1990—present
421 results
Scopus (Elsevier)
Searched conducted: April 28, 2020
| Search | Query |
|---|---|
| #1 | prevent* OR intervention OR program OR “health promotion” |
| #2 | rural |
| #3 | “school based” OR school-based OR school* |
| #4 | obes* |
| #5 | teen* OR child OR children OR “school age” OR “school aged” OR adolescen* OR “high school” OR “middle school” OR “elementary school” OR “pre k” OR preschool OR “primary school” OR youth OR pediatric OR paediatric OR “secondary school” OR “head start” OR “nursery school” |
| #6 | #1 AND #2 AND #3 AND #4 AND #5 |
Limited to English language and years 1990—present
653 results
Academic Search Premier (EBSCO)
Search conducted: April 24, 2020
| Search | Query |
|---|---|
| #1 | prevent* OR intervention OR program OR “health promotion” OR DE “PREVENTION” OR DE “HEALTH promotion” |
| #2 | Rural OR DE “RURAL geography” OR DE “RURAL health” OR DE “RURAL population” OR DE “RURAL schools” OR DE “RURAL youth” OR DE “RURAL teenagers” |
| #3 | “school based” OR school-based OR school* OR DE “SCHOOLS” |
| #4 | obes* OR DE “OBESITY” OR DE “OBESITY in adolescence” OR DE “OBESITY in children” |
| #5 | teen* OR child OR children OR “school age” OR “school aged” OR adolescen* OR “high school” OR “middle school” OR “elementary school” OR “pre k” OR preschool OR “primary school” OR youth OR pediatric OR paediatric OR “secondary school” OR DE “CHILDREN” OR DE “YOUTH” OR DE “ADOLESCENCE” OR DE “TEENAGERS” OR DE “HIGH school students” OR DE “SECONDARY school students” OR DE “HIGH schools” OR DE “MIDDLE school students” OR DE “MIDDLE schools” OR DE “SCHOOL children” OR DE “KINDERGARTEN children” OR DE “ELEMENTARY schools” OR DE “PRIMARY schools” OR DE “PRESCHOOL children” OR DE “SECONDARY schools” OR “head start” OR “nursery school” OR DE “HEAD Start programs” OR DE “NURSERY school education (Great Britain)” OR DE “NURSERY schools (Great Britain)” |
| #6 | #1 AND #2 AND #3 AND #4 AND #5 |
Limited to English language and years 1990—present
557 results
Cochrane Central Register of Controlled Trials (Wiley)
Search conducted: April 24, 2020
| Search | Query |
|---|---|
| #1 | prevent* OR intervention OR program OR “health promotion” |
| #2 | rural |
| #3 | “school based” OR school-based OR school* |
| #4 | obes* |
| #5 | teen* OR child OR children OR “school age” OR “school aged” OR adolescen* OR “high school” OR “middle school” OR “elementary school” OR “pre k” OR preschool OR “primary school” OR youth OR pediatric OR paediatric OR “secondary school” OR “head start” OR “nursery school” |
| #6 | #1 AND #2 AND #3 AND #4 AND #5 |
Limited to English language and years 1990—present
95 results
ClinicalTrials.gov
Search conducted on April 24, 2020
| Search | Query |
|---|---|
| #1 | Advanced Search: |
| Condition or disease: obesity | |
| Other terms: school AND rural | |
| Study type: All | |
| Study results: All | |
| Age: Child | |
| Sex: All |
Study Start: From 01/01/1990-present
10 results
ProQuest Dissertations and Theses Sciences and Engineering Collection (ProQuest)
Search conducted: April 23, 2020
| Search | Query |
|---|---|
| #1 | Exact(“Rural” OR “RURAL” OR “Rural adolescents” OR “rural populations” OR “rural adolescents” OR “rural” OR “Rural adolescent females” OR “Rural population” OR “Rural populations” OR “Rural schools”) AND (obesity OR obese) AND (teen* OR child OR children OR “school age” OR “school aged” OR adolescen* OR “high school” OR “middle school” OR “elementary school” OR “pre k” OR preschool OR “primary school” OR youth OR pediatric OR paediatric OR “secondary school” OR “head start” OR “nursery school”) AND (“school based” OR school-based OR school*) |
Limited to English language and years 1990—present
207 results
OpenGrey (opengrey.eu)
Search conducted: April 23, 2020
| Search | Query |
|---|---|
| #1 | (prevention OR intervention) AND rural AND school AND (obesity OR obese) AND (child OR children OR teen) |
Limited to English language and years 1990—present
0 results
Open Access Theses and Dissertations (oatd.org)
Search conducted: April 23, 2020
| Search | Query |
|---|---|
| #1 | (prevention OR intervention) AND rural AND school AND (obesity OR obese) AND (child OR children OR teen) |
Limited to English language and years 1990—present
22 results
Directory of Open Access Journals (doaj.org)
Search conducted: April 23, 2020
| Search | Query |
|---|---|
| #1 | (prevention OR intervention) AND rural AND school AND (obesity OR obese) AND (child OR children OR teen) |
Limited to English language and years 1990—present
21 results
PapersFirst (OCLC)
Search conducted: April 23, 2020
| Search | Query |
|---|---|
| #1 | (prevention OR intervention) AND rural AND school AND (obesity OR obese) AND (child OR children OR teen) |
Limited to English language and years 1990—present
0 results
Centers for Disease Control and Prevention (MedNar)
Search conducted: April 24, 2020
| Search | Query |
|---|---|
| #1 | prevention AND rural AND school-based AND obesity AND child |
Limited to English language and years 1990—present
99 results
US Department of Education (ed.gov)
Search conducted: April 23, 2020
| Search | Query |
|---|---|
| #1 | prevention AND rural AND school-based AND obesity AND child |
Limited to English language and years 1990—present
560 results
Appendix III: Characteristics of included studies, organized by program components
| Study, year, location | Method of rural designation | Study type (design) | Intervention components | Intervention frequency/length | Provider | Sample | Type of outcomes | Key findings |
|---|---|---|---|---|---|---|---|---|
| Exercise/physical activity (n = 9) | ||||||||
| Conway et al.71 2012 US (North Dakota) | Author reported rural county | Prevention (qualitative) | PA (and behavioral)a | 5 weeks in winter | 3 member evaluation team | N = 81 5th and 6th grade students |
5 focus groups, qualitative data | Students thought setting goals and keeping logs supported participation in PA; logs helpful but not consistently completed; some students wanted them to be electronic but also to be private; described support from parents and teachers and role models; increasing level and variety of PA was recommendation for change. |
| Eichner et al.100 2016 US (Oklahoma) | Author reported rural school | Prevention (pre-post design) | PA | 2 school semesters (daily PA on school days) | PE teacher | N = 66 Middle school: 6th, 7th, and 8th grade students, 12–15 years old |
BMI z-scores pre- and post-assessments | Significant group differences in BMI z-scores, with participating students staying the same and nonparticipating students increasing; BMI decreased among boys who participated and was stable among girls. |
| Manley53 2008 US (Kentucky) | Author reported rural | Prevention (RCT) | PA | 12 weeks (wore pedometer every day and 10 minutes of moderate to vigorous PA) | PE teacher | N = 116 6th and 7th grade students Intervention n = 55 Control n = 61 |
Self-efficacy levels, PA (pedometers), aerobic fitness (1 mile walk test), and body composition (height, weight, BMI, BMI %ile, relative BMI) pre- and postassessments | No Tx effects—no statistical difference between Tx and control school; Tx school had significantly higher weight status (BMI and relative BMI); Tx school had significantly lower PA and aerobic fitness compared to control school; noteworthy that Tx group had greater improvements in self-efficacy, aerobic fitness levels, and relative BMI than control group. |
| Manley et al.87 2014 US (Kentucky) | Author reported rural | Prevention (RCT) | PA | 12 weeks (wore pedometer every day and 10 minutes of moderate to vigorous PA) | PE teacher | N = 116 11- and 13-year-olds (mean age 11.7 years) Intervention n = 55 Control n = 61 |
Self-efficacy levels, PA (pedometers), aerobic fitness (1 mile walk test), and body composition (BMI, BMI %ile, relative BMI) pre- and postassessments | No significant difference between Tx and control groups; those with optimal relative BMI levels had higher self-efficacy, PA, and aerobic fitness levels. Although not statistically significant, Tx group had greater improvements in mean self-efficacy scores, aerobic fitness levels, and relative BMI. |
| Oluyomi et al.89 2014 US (Texas) | Definition not included (home addresses were geocoded) | Prevention (cross-sectional) | PA (and policy)b | 5-year implementation project | Not described | N = 830 parent-student dyads (4th grade) | Self-reported child walking to school; perceived traffic and personal safety concerns for neighborhood, en route to school, school environments; social capital | Odds of walking to school were higher with no problems related to traffic speed, amount of traffic, sidewalks, intersection safety, crossing guards; odds of walking to school were lower with stray animals and concerns with no walking partner. |
| Robinson et al.90 2014 US (Alabama) | Author reported 1 county in Black Belt Region | Prevention (cross-sectional) | PA (and policy)b | Daily PE for 30 minutes | Certified PE instructor | 5 elementary schools; N = 683 school-age children (341 female; 342 male); mean age 8.22 years; 99.9% Black | BMI; weight status; waist circumference; PA behavior (pedometer step count, System for Observing Fitness Instruction Time, and the System for Observing Play and Leisure Activity in Youth) | Overall, PE and PA state-level policies were only partially implemented; large discrepancy between what is scheduled at school level and what is actually being implemented; PA during PE was students’ only opportunity for school PA. |
| Rye et al.55 2008 US (West Virginia) | Definition not included; state is in Appalachia and ranks 3rd highest among all states on % rural population | Prevention (pre-post design) | PA | 2 academic years | 2 secondary teachers and high school students | Y1, N = 16 Y2, N = 15 + 3 repeaters from Y1, faculty, staff, parents, community members High school focus group: Health Sciences and Technology Academy students Y1, N = 12 Y2, N = 5 Adult focus group participants: teachers, parents, community members | Daily step count (pedometer); perceptions of barriers to PA; self-efficacy; outcome expectations | Pre to post-decreases in Y2 mean scores were statistically significant for total barriers, as well as lack of energy, time, and willpower. |
| Smith et al.113 2020 US (Ohio) | Author reported rural Appalachian high schools in Southern Ohio (based on population density, housing, and territory) | Intervention (RCT) | PA (and behavioral)a | 10 weeks (10 40-minute weekly lessons) | Trained peer mentors and teachers | N = 190 (n = 106 obese and n = 84 extremely obese) in 9th-11th grades Mean age 15.03 years (standard deviation = 0.84) | Conducted baseline, 3-month follow-up, and 6-month postintervention of raw body weight, height, BMI, body fat %, BMI % | All youth lost an average of 7.3 lb from baseline to 3-month follow-up and 10.8 lb from baseline to 6-month follow-up; Obese Mentored Planning to be Active group lost 77.5% more weight by 6-month follow-up compared to the Planning to be Active group. Extremely obese in the Mentored Planning to be Active group lost 80% more weight compared to the Planning to be Active group. Extremely obese females lost more weight compared to males; BMI and body fat had similar results; youth in the Mentored Planning to be Active group had most improvements. |
| Smith et al.106 2018 US (Ohio) | School districts in rural Appalachia counties | Prevention (RCT) | PA | 10 40-minute sessions (2 possible sessions each week) | Teachers and trained teen mentors | N = 654 9th and 10th graders N = 119 older peer mentors N = 8 teachers N = 20 schools |
BMI, height, weight | Peer-to-peer mentoring by local high school students and school-based tailored support strengthens sustainable behavioral change. |
| Dietary/nutrition (n = 9) | ||||||||
| Angelico et al.42 1991 Italy (Sezze Romano) | Author reported small town (70 miles outside Rome) | Prevention (cross-sectional) | Nutrition | 5 years (3 teacher trainings, 6 parent/community interactions); frequency of nutrition education in classroom unclear | Trained school teachers | N = 150 children aged 6–7 years attending rural elementary school | Height, weight, BMI | Height, weight, and BMI increased over time. |
| Moss et al.79 2013 US (Illinois) | US Department of Agriculture Rural designation | Prevention (pre-post design) | Nutrition (and behavioral)a | 4-week intervention (2 30-minute lessons one week apart; 120-minute farm tour in week 4) | Unclear | N = 65 3rd grade students from one elementary school |
Nutrition knowledge; fruit/vegetable consumption, farm exposure; Go, Slow, Whoa foods | Positive eating fiber, fruits/vegetables contain vitamins, eating more vegetables at school; non-significant relationship between fruit/vegetable and farm tour. |
| Murimi et al.97 2015 US (Louisiana) | Definition not included | Prevention (pre-post design) | Nutrition (and behavioral)a | Screening and point-of-testing counseling sessions offered every 6 months for 3 years; 6 possible testing and counseling session opportunities; 2040 minutes per counseling session; nutrition education 1 hour/week for 12 weeks | Registered dietitian, registered nurse, dietetic students | N = 233 6th-12th grade students (11–19 years old), 51% female, 58% White, 51% overweight or obese |
BMI, BP, total cholesterol, HDL, LDL, triglycerides, student food knowledge | Significantly increased HDL and nutrition knowledge (7th and 8th grade), non-significant but stabilized weight and blood values. Participants who attended 4 sessions maintained their weight at 76th %ile; highest-risk participants, systolic BP, total cholesterol, and triglycerides lowered. |
| Muth et al.54 2008 US (North Carolina) | Definition not included | Prevention (RCT) | Nutrition | 12-week curriculum, 60-minute lessons; 15-hour high school student training | Peer modeling by medical and high school students | 1 high school; 8 students trained as health educators, 10 medical students 1 elementary school, 4th grade classrooms, 2 intervention (38 students) and 2 control (37 students) classrooms |
Nutrition servings per day: fruit/vegetable, calcium foods, grains, sweet beverages, fried foods, sweets; nutrition knowledge and attitudes, PA score, sedentary score | Increased fruit/vegetable intake and nutrition knowledge. |
| Nanney et al.102 2016 US (Minnesota) | 50% rural town fringe and 50% rural using National Center for Education Statistics and rural-urban commuting area codes | Prevention (RCT) | Nutrition | 1 academic year; School Breakfast Expansion Team met 5 times; Tx or delayed Tx; block randomization with 4 Tx and 4 control in each wave | School personnel implemented school-level changes; no other detail about provider | 8 schools in Wave 1; 3 schools in Wave 2; all 9th and 10th graders screened for eligibility; 904 enrolled; 54% girls and 30% non-White | Increase systolic BP participation (primary), diet quality, intention to eat school breakfast; decrease calories, BMI, body fat | Community-based approach to translate best practices; study successfully recruited 16 schools and exceeded student enrollment; few results on the intervention; schools did initiate a second chance grab and go breakfast. |
| Rodriguez et al.98 2015 US (Florida) | Author reported Florida Panhandle | Prevention (qualitative) | Nutrition | Not provided | Florida A&M Extension agents | N = 60 3 focus groups; 20 participants per group; 9–12 years |
Student thoughts, feelings, and perceptions of school garden program | Students reported greater technical knowledge and liked spending time outside; talked about growing vegetables and opinions of the different vegetables grown; some participants described having tried new vegetables; however, participants did not speak about an increase in household vegetable consumption. |
| Smith et al.91 2014 US (Ohio) | Author reported a rural Appalachian county | Prevention (pre-post design) | Nutrition (and policy)b | 30-day | Teen Advisory Council (teachers and students from 9th-12th grades) | N = 186 high school students in 9th-12th grades from 2 schools (mean age = 15.85 years) |
Sugar-sweetened beverage consumption and water consumption: pre, post, and 30-day follow-up | Sugar-sweetened beverage consumption decreased significantly, and water consumption increased 19% from baseline to post-intervention. |
| Struempler et al.92 2014 US (Alabama) | Participants from schools eligible for SNAP-Ed, with over 50% students receiving free or reduced-price lunch | Prevention (pre-post design) | Nutrition | Weekly for 17 weeks, 45-minute classes | SNAP-Ed educators | N = 2477 3rd grade students eligible for SNAP-Ed |
Fruit and vegetable consumption during lunch (self-reported food consumption) | School-based childhood obesity prevention programs as means to moderately increase fruit and vegetable consumption through the school lunch program. |
| Tussing-Humphreys et al.75 2012 US (Mississippi) | Author reported “rural Lower Mississippi Delta” Hollandale, MS | Prevention (pre-post design) | Nutrition | 3 times per week over a 6-week period | Research staff, teachers | N = 187 4th-6th graders completed the study |
Fruit and vegetable recognition, willingness to try, and fruit and vegetable consumption pre- and postintervention | A fruit and vegetable snack feeding intervention can increase familiarity, and potentially, the amount of fruits and vegetables consumed by school children. |
| Combined nutrition and physical activity (n = 43) | ||||||||
| Bergan77 2013 US (South Dakota) | Author reported “rural” students (125-mile radius from Brookings, South Dakota) | Prevention (RCT) | Combined nutrition and PA | 6-month program; 6 40-minute lessons (6-month follow-up assessment) 2 interventions compared to control: KidsQuest (Intervention 1) and KidsQuest plus Family Fun Packs and Take 10! Activities (Intervention 2) | Trained teen teachers | N = 91 5th and 6th grade students. Mean age ranged from 10.85 to 11.04 years (128 invited to participate, 91 started the program, and 79 completed the whole study) |
Total cholesterol, triglycerides, LDL, HDL, BMI (assessed pre-, post-, and 6 month [12-month] follow-up) | No significant group difference in total cholesterol, triglycerides, and HDL from pre to post and pre to follow-up; significant decrease in LDL from pre to post in Intervention 2 group; significant increase in BMI for Tx Group 1 pre to post and pre to follow-up for Tx groups 1 and 2. |
| Brown103 2018 US (Washington) | Author reported rural community in eastern Washington | Prevention (quasi-experimental) | Combined nutrition and PA | 6 months | Teachers; provider of child and family intervention unclear | N = 665 (Tx = 282, control = 383) 3rd-5th grade students N = 205 (Tx = 104 and control = 101) 3rd and 4th graders assessed for nutrition and PA for comparison |
Height, weight, BMI z-scores, dietary intake, PA, sedentary behavior (assessed baseline and 6-month follow-up) | Significant improvement in light and moderate PA for the intervention group compared to control group from pre- to postassessment, and significant decrease in moderate and vigorous PA in control group; no significant group difference in dietary behaviors (fruit, vegetable, and sugar consumption) or sedentary behavior. |
| Bumaryoum94 2015 US (South Dakota) | Author reported rural schools | Prevention (RCT) | Combined nutrition and PA | 6 50-minute sessions over 4–6 months | Trained teen teachers and SNAP-Ed educators | N = 254 5th and 6th grade students |
Nutrition, PA, BMI (height, weight), BP, total cholesterol, HDL, hemoglobin (assessed pre and 6 months after initiation) | No significant change in BMI, BP, total cholesterol, HDL, hemoglobin. Significant reduction in eating candy in intervention groups and increases in whole grain consumption. |
| Canavera et al.59 2009 US (Kentucky) | Author reported rural Kentucky | Prevention (qualitative and pre-post design) | Combined nutrition and PA | 12-week intervention (plus focus groups conducted before) | PE and health teachers (no specialized training) | N = 122 5th grade students (mean age not reported) N = 36 focus group parent and child dyads |
PA, watching TV, drinking water, eating fruits and vegetables (pre- and post-assessments); focus group data | Generally no significant pre-post difference with exception of significant pre-post differences for expectations for watching TV, expectations for drinking water, and number of glasses of water consumed. |
| Carrel et al.45 2005 US (Wisconsin) | Author reported rural | Intervention (RCT) | Combined nutrition and PA | 5 times every 2 weeks for 45 minutes; 9 months (school year) | Instructors | N = 50 obese middle school students (mean age 12 years) |
BMI, fasting glucose, insulin, body fat, fat-free mass, cardiovascular fitness (maximal oxygen consumption) | Compared with the control group, treatment group had significant decrease in body fat %, significant improvements in cardiovascular fitness, and significant improvement in fasting insulin level. |
| Cason et al.47 2006 US (South Carolina) | Author reported rural underserved communities | Prevention (quasi-experimental) | Combined nutrition and PA | 7 1-hour sessions over 14 weeks | University Cooperative extension educator | N = 130 4th grade students (mean age 9 years); n = 72 control, n = 58 intervention |
PA and dietary intake knowledge and behavior, 21 items (pre, post, and 5-month follow-up) | Significant group differences (Tx group better) in washing hands, choosing healthy snacks, eating vegetables every day, trying new foods, thinking about foods being healthy, doing moderate PA, working on getting stronger, PA until sweating, exercising or dancing during TV commercials, enjoying being physically active, matching muscle group to body parts, keep-away strategies. |
| Craven et al.66 2011 US (North Carolina) | Author reported rural high schools | Prevention (quasi-experimental) | Combined nutrition and PA | 4 90-minute lessons (6 hours) of nutrition education and 6 hours of PA instruction in one semester | Nutritionist and classroom teacher | N = 399 9th graders (mean age = 14.7 years) N = 214 Tx group and N = 185 control group |
Height, weight, BMI, self- reported eating behaviors (fruits, vegetables, dairy, sweet beverages, fast food), pre and post | No significant group difference in mean BMI change, but mean BMI decreased in Tx group; increases in fruit and vegetable intake for intervention group but not statistically significant (P = 0.09 and 0.08). |
| Culbertson49 2007 US (Colorado) | Author reported rural | Prevention (quasi-experimental) | Combined nutrition and PA | Bimonthly classroom; 1 hour long; 11 hours total intervention time; 2 years | Grad student and community volunteers (PE teacher, high school and nursing students, police officer, veterinarian) |
N = 82 2nd and 3rd graders; Cohort A = 37 2nd graders completing Year 1, Cohort B = 40 3rd graders completing Year 2, Cohort C = 29 2nd and 3rd graders who completed both years |
Food and PA knowledge, attitude and behavior, BMI, waist circumference, body image, pedometer step counts; pre- and post-assessments | Significant improvement in PA attitude and knowledge in Tx group compared to control group; significant improvement in dietary intake pre- and post-Tx group but no significant difference from control group; significant improvement in body image especially for females in Tx group; overall no significant change in BMI z-score; no significant group differences in pedometer steps. |
| Davis et al.43 1993 US (New Mexico) | Author reported rural schools | Prevention (RCT) | Combined nutrition and PA | 5 units; 18 hours of curriculum in one semester | Classroom teachers, older members of community | N = 1543 5th grade students, 9–13 years old (participated over 5-year period) |
Health knowledge and attitudes, dietary habits, exercise behavior; height, weight, BMI, skin folds; pre and post | Significant improvement in overall knowledge in intervention schools vs. control schools; significant increase in exercise in intervention vs. control schools; significant decrease in use of butter or tortillas in intervention vs. control schools. |
| Donnelly et al.44 1996 US (Nebraska) | Author reported rural | Prevention (quasi-experimental) | Combined nutrition and PA | 2 years; nutrition: 18 modules (9 modules per school year) PA: 3 days per week for 30–40 minutes |
Existing classroom teachers | 3rd and 5th grade elementary school students; N = 200 to collect lab data | Aerobic capacity, body composition, blood chemistry, nutrition knowledge, energy intake, and PA | No significant difference in Tx and control schools in weight, BMI, fat %, maximal oxygen consumption, BP, insulin, or glucose; via 24-hour recall, students in Tx schools consumed significantly less sodium vs. control schools at post; no other significant dietary difference, although lunches had less fat, sodium, and total energy; HDL cholesterol and the ratio of cholesterol to HDL significantly improved for Tx vs. control group; Tx group significantly more active at school but significantly less active outside of school vs. control schools. |
| Gittelsohn and Rowan67 2011 US (Native American) | Author reported rural areas (American Indian and First Nation communities) | Prevention (qualitative) | Combined nutrition and PA | Unknown | Teachers | Elementary schools; 3rd-5th grade |
Qualitative/descriptive | Positive change in psychosocial measures and improvements in diet; no significant improvements in PA or obesity (primary outcome). |
| Gombosi et al.50 2007 US (Pennsylvania) | Author reported rural county | Prevention (pre-post design) | Combined nutrition and PA | 5 years | Teachers, guest teachers, health curriculum coordinator | N = 4804 K-8th grade (ages 5–14 years) | BMI %, health assessments at health fairs; pre- and postassessments | Minority of teachers used provided kits; increased incidence of overweight and obesity over time; no treatment effect. |
| Hao et al.110 2019 China | Author reported rural (one district of Benxi City, Liaoning Province, in Northeast China) | Intervention (RCT) | Combined nutrition and PA | Exercise Tx: every school day for 30 minutes for 2 months; skipping rope, 3 times for 10 minutes; nutrition education, 8 45-minute meetings for 2 months (total of 6 hours) | Nutritionist, PE teacher | N = 229; n = 104 girls, n = 125 boys Overweight or obese primary school children 9–12 years of age | Anthropometric assessments (weight, height), dietary survey, nutrition knowledge, daily energy intake at baseline, after 2 months Tx (post), and 1 year follow-up | Compared to baseline, BMI significantly decreased for all 3 groups at post-intervention and follow-up; nutrition knowledge significantly improved for 2 groups who received nutrition education at both post-Tx and follow-up vs. baseline; significant decrease in energy intake post-Tx and follow-up in those who received nutrition education; significant changes in BMI standard deviation scores in exercise and nutrition education intervention, nutrition education intervention, exercise intervention, and control groups, from highest to lowest; combination Tx had best short- and long-term outcomes. |
| Harrell et al.46 2005 US (Mississippi) | Author reported rural southern community (Scott County, MS) | Prevention (quasi-experimental) | Combined nutrition and PA | 16 weeks; 4 monthly sessions | Health care Professionals (pediatrician, pharmacist, Exercise physiologist, and registered dietitian) |
N = 205 5th graders (mean age 11.9 years) |
Health knowledge, height, weight, BMI, body fat %, waist circumference, dietary intake, blood lipids, blood glucose, and BP; pre and post test | Students in intervention school increased health knowledge compared to control school; significant increases in height, weight, and waist circumference over time; significant increase in vegetable consumption and decrease in soft drink consumption in Tx group compared to control group; no significant difference in other outcomes. |
| Harwood60 2009 US (Ohio) | Author reported rural Appalachia (federally designated, <2500 people) | Prevention (quasi-experimental) | Combined nutrition and PA | 16 weeks: 6 45–60 minutes each (child part); parents (3 nutrition education, 5 packets); rowing twice a week for 30 minutes for 16 weeks | Research teachers |
N = 35 (n = 19 Tx group and n = 16 control group) 2nd grade students (7 and 8 years old) |
Dietary behaviors (nutrients, food groups): 3-day food log, height, weight, BMI, body fat % (skin fold), exercise test (aerobic fitness, BP, heart rate, respiratory function); pre- and postassessments | Children in Tx group significantly increased milk and magnesium compared to control group; no other significant difference in nutrition; no significant difference between groups in BMI and body fat %. |
| Hawkins et al.104 2018 US (Louisiana) | Author reported rural | Prevention (RCT) | Combined nutrition and PA | 28 months | Research personnel | N = 1626 4th-6th graders (mean age = 10.5 years); n = 1195 Tx and n = 431 control |
Sodium, added sugars in lunches (baseline, 18 months, and 28 months); food selection and consumption based on digital photography | No significant group difference in energy intake at 18 months, but at 28 months, Tx group consumed significantly fewer kcals; at 18 months, sodium selection and consumption significantly increased in control group vs. Tx group and at 28 months, control group consumed more sodium compared to the Tx group; at 18 months, added sugar consumption increased in control group compared to Tx group and at 28 months, added sugar consumption significantly decreased in Tx group vs. control group; plate waste did not decrease. |
| Hawley et al.48 2006 US (Kansas) | Author reported rural | Prevention (qualitative and pre-post design) | Combined nutrition and PA (and behavioral)a | Five 40-minute session classroom program over 6 weeks | Unclear | N = 65 6th graders (and 25 families) 11–12 years old |
Nutrition and exercise knowledge; self-reported PA and eating behavior; BMI (height and weight) | No significant change in child health attitudes and behaviors; significant change in goal of eating healthfully; families significantly increased PA and significantly improved PA knowledge; no significant change in knowledge of nutrition and goal setting or importance of PA. |
| Heelan et al.95 2015 US (Nebraska) | Author reported rural community (~30,000) | Prevention (pre-post design) | Combined nutrition and PA | Tx phased over 6 years | School nurses, trained university volunteers | N = 2400 each year, K-5th grade, across 9 schools | Student measurements: weight, height, BMI; implementation data (frequency, duration, and magnitude of change); reach and strength of Tx strategies; behavioral outcomes included increasing PA, decreasing unhealthy/high-calorie foods, and increasing healthy food consumption | Prevalence of overweight decreased 1.2% and obesity decreased 2.5% over 6-year period; inverse relationship between the number of strategies implemented and prevalence of overweight and obesity over time. |
| Hoying et al.101 2016 US | Author reported Appalachian | Prevention (pre-post design) | Combined nutrition and PA (and behavioral)a | 15 sessions during one academic year | Trained health teacher | N = 24 8th grade students (mean age = 13.6 years) completed Tx |
Healthy lifestyle behaviors, physical health (BMI), and mental health symptoms, parent program evaluation; pre- and post-assessments | Significant improvement in healthy lifestyle behavioral scale at post-Tx; approaching significant improvement in self-concept at post-Tx; no significant change in anxiety, depression, anger, or disruptive behavior (greater effect size found for those who were overweight/obese). |
| Langham96 2015 US (Alabama) | Author reported rural school system and medically under-served community | Prevention (pre-post design) | Combined nutrition and PA | One 30-minute session | Nursing students | N = 57 3rd graders (8 to 9 years old) |
Height, weight, BMI, knowledge of nutrition, PA, and healthy behaviors (pre and post, 10 weeks) | Significant improvement in nutrition and health behavior knowledge pre and post; no significant change in BMI %ile. |
| Lazorick et al.84 2014 US (North Carolina) | Author reported designed to reach rural youth | Prevention (pre-post design) | Combined nutrition and PA | 55 contact hours over 14–16 weeks | Trained research team member | N = 106 participated as 7th graders and 8th graders who were retained at 11th and 12th grade (originally N = 195) | Weight category, BMI, BMI z-score, BMI %ile, rates of change in BMI per month | At follow-up, Tx group decreased % overweight but comparison group increased; Tx group had higher decrease in BMI z-scores and BMI %ile than comparison; comparison group had higher increase in % overweight after 5 years compared to Tx group. |
| Lazorick et al.68 2011 US (North Carolina) | Author reported rural school/county | Prevention (pre-post design) | Combined nutrition and PA | 55 contact hours over 14 weeks | Classroom teachers | N = 197 7th graders (mean age 13 years) Cohort 1: n = 92 Cohort 2: n = 102 |
BMI z-scores and BMI %ile (pre, post, 15 months, and 30 months) | Slight decrease in BMI for both cohorts; in overweight group significant reductions in BMI z-score and BMI %ile; little change in healthy weight subgroup post. |
| Lin et al.111 2019 Taiwan | Author reported remote rural areas of Northern Taiwan | Prevention (RCT) | Combined nutrition and PA (and behavioral)a | 8 weeks, 8 sessions, 40 minutes | Research group | N = 201 3rd and 4th graders from 8 elementary schools (8 to 12 years old) |
Conducted before and after Tx; child interest in space exploration, satisfaction, healthy eating, and PA behaviors, knowledge, height and weight to calculate BMI; teachers and PE teachers evaluated sessions; appropriateness of content, relevance to space exploration, willingness to apply program to class | Compared to control, Tx group had significant increase in healthy diet but no significant difference in healthy eating behaviors; Tx group had significantly higher active lifestyle knowledge but no significant difference in active lifestyle behaviors; no significant difference in body weight outcomes; increase in interest in space and 90% students were happy to participate. |
| Ling78 2013 US (Kentucky) | Author reported rural | Prevention (pre-post design) | Combined nutrition and PA (and policy)b | 5 months | Trained healthy lifestyle coaches |
N = 1508 K-5th grade (mean age 8.32 years) |
PA (pedometer) and eating behavior (dietary recall) | Significant improvement in % of children meeting PA recommendations after the Tx; significant improvement in % of children meeting nutrition recommendations after Tx; significant Tx effects on PA behavior and increased consumption of fruits and vegetables; effects on nutrition and PA depended on school, age, and grade. |
| Ling et al.85 2014 US (Kentucky) | School rural based on rural-urban commuting areas using census tract-level demographic and work-commuting data, and economic integration with urban areas | Prevention (pre-post design) | Combined nutrition and PA (and policy)b | 5 months | Trained healthy lifestyle coaches |
N = 1508 K-5th grade students (mean age 8.3 years) |
Nutrition (dietary recall) and PA (pedometer) | Intervention had significant effects on % of children meeting nutrition recommendations and intervention had significant effects on % of children who met PA recommendations; effects on nutrition and PA depended on school, age, and grade; increasing linear trend of PA and increasing quadratic trend of nutrition over time. |
| Llaurado et al.86 2014 Spain | Author reported semi-rural town (minimum of 500 7- and 8-year-olds) | Prevention (RCT) | Combined nutrition and PA | 12 1-hour sessions implemented over 3-year period (22 months of Tx) | Health promoting agents (college students) | N = 690 primary school students (2nd and 3rd grade) mean age 8.04 years Intervention: n = 320, Control: n = 370 | Obesity prevalence, BMI, dietary habits and lifestyles; pre- and postassessments | No significant group difference in obesity prevalence or BMI, BMI z-score between Tx or control group post-Tx; boys in Tx group performed more PA (4 or more hours a week after school) post-Tx compared to control group; boys in Tx group also watched less TV (2 hours or less per day) post- Tx compared to boys in control group; no sign group differences found for girls. |
| Naylor et al.64 2010 Canada (British Columbia) | Population and distance from nearest city (Prince Rupert); author reported Aboriginal communities in northern British Columbia | Prevention (pre-post design and qualitative) | Combined nutrition and PA (and behavioral)a | 15 minutes extra PA/day; ≥ 1 healthy eating activity per month | Teachers (received 2 half-days of training) | 3 schools (K to 10th grade) | Action plans; type, frequency, duration of PA and healthy eating; minutes of PA and healthy eating; activities counted and categorized; qualitative feasibility of implementation | Logging was 34% for all weeks but varied across schools; 140 minutes of PA average, scheduled PE average 1.75 times/week; healthy eating 2.27 times/week with 15.6 minutes each session; healthy eating average was 55 min/week with 4.6 activities/week; overall, acceptable to teachers and administrators; cultural adaptations recommended. |
| Puma et al.80 2013 US (Colorado) | < 15,000 population; south-central Colorado | Prevention (quasi-experimental) | Combined nutrition and PA | Implementation in 3rd grade; 28 lessons in each grade for 2 years (3rd and 4th grades); followed for ~6 years | Trained resource teacher or regular classroom teacher |
1 school district; 173 2nd graders; 190 2nd graders as controls; follow-up in 8th grade (N = 190) |
Nutrition and PA knowledge, self-efficacy, attitudes and behaviors, BMI | Increase in nutrition-related knowledge and attitudes; no effect on self-efficacy or behavior change including more fruit/vegetable consumption. |
| Ronsley et al.82 2013 Canada (British Columbia) | Identified as remote; communities only accessible by boat or plane; author reported Aboriginal communities in northern British Columbia | Prevention (quasi-experimental) | Combined nutrition and PA (and behavioral)a | 10-month study; 21 lessons, each for 30 minutes; 6 fitness loops, 2 conducted per week with 2 classes at one time | Older students trained to teach younger students | 2 intervention schools (N = 118); 1 control school (N = 61); K-12th grades |
BMI, waist circumference, BP, food frequency, PA frequency, sedentary and screen time, healthy living knowledge, selfesteem | Significant decrease in BMI z-score (1.10 to 1.04, P = .028) and waist circumference (77.1 to 75.0 cm, P < .0001) and BP z-score in the Healthy Buddies (control group increased); overall, intervention was successful at decreasing BMI z-score and waist circumference; BP remained stable but increased in control group. |
| Rush et al.72 2012 New Zealand (Waikato District) | Not defined, author reported | Prevention (RCT) | Combined nutrition and PA | Weekly newsletter with healthy eating nuggets; 2 academic-year study | Trained change agent (teachers or graduates in exercise and nutrition, or physical education) | 124 schools, stratified by rurality; 62 control schools (N = 692; 5–7 years old), 62 intervention schools (N = 660; 10–12 years old) | BMI, BP, and body composition | Intervention had a more favorable, but not statistically significant, effect in rural schools; systolic BP standard deviation score was nonsignificantly lower in rural children than urban; 5–7 year olds’ body fat % significantly lower and 10–12 year olds’ systolic BP significantly lower until school clustering was controlled for (then nonsignificant). |
| Schetzina et al.61 2009 US (Tennessee) | Author reported Appalachia | Prevention (pre-post design) | Combined nutrition and PA (and beha- vioral)a | Pre-post evaluation conducted over 18-month period | Registered dietitian, teachers, extension agents; school health staff, parent teacher organization | 114 students (53% female; 94% White); teachers (98% of K-4th grade teachers); 1 elementary school; impact of school-wide program (K-4th) on 3rd and 4th graders | BMI, diet, PA (pedometer), knowledge attitudes, perceptions, acceptability, feasibility, sustainability | No significant changes in students’ BMI z-score during the first 7 months of program evaluation; 4th graders had higher increase in BMI z-score and if overweight at start, no decrease in BMI; PA increased; fewer Whoa foods served in cafeteria; no significant changes for GO or SLOW foods. |
| Schetzina et al.70 2011 US (Tennessee) | Author reported Appalachia | Prevention (pre-post design) | Combined nutrition and PA (and behavioral)a | 1 academic year; 4-year follow-up of 1 academic year pilot study | School personnel (teachers and staff) | Follow-up, N = 65 4th grade students (45% female; 90.9% White); teachers (N = 23) | Diet, PA (pedometer), cafeteria offerings, teacher implementation, teacher perception of obesity as a problem | Improved in healthy eating food score, steps/day, green and yellow foods in cafeteria, fewer red foods served (per Go, Slow, Whoa food chart); teachers’ perceptions of PA and healthy eating changed. |
| Slawson et al.99 2015 US (Tennessee) | Author reported rural Appalachia in northeastern Tennessee | Prevention (RCT [abstract]) | Combined nutrition and PA | 3 months; 8 40-minute sessions | Not specified | N = 1509 high school students | BMI | Positive impact on standardized BMI z-score at 3 months post-baseline for the treatment arm. |
| Smith et al.52 2007 US (Colorado, Texas, and West Virginia) | Author reported suburban/rural public schools | Prevention (pre-post design) | Combined nutrition and PA | One school year | Not specified | 2nd-6th grade children in 40 classrooms in 3 states (more than 800 participants, total unknown) | Food knowledge, health knowledge, PA (steps/day), scientific knowledge of type 2 diabetes; pre and post school year | Significant increase in knowledge related to food, health, diabetes, and prevention increase and PA significantly increased. |
| Tomlin et al.74 2012 Canada (British Columbia) | Author reported rural and remote communities | Prevention (pre-post design) | Combined nutrition and PA | 7 months | Researchers (collaborated with schools, families and communities) | N = 148 children and youth, ages 12.5 ± 2.2 years | BMI z-score, waist circumference, aerobic fitness, PA, dietary intake (healthy eating) and cardiovascular risk; pre- and post-measurements | BMI z-score remained unchanged while waist circumference z-score increased. No change was detected in PA or cardiovascular risk but aerobic fitness increased. There was an increase in variety of vegetables consumed but otherwise no dietary changes were detected. |
| Valenzuela et al.83 2013 Chile (Pumanque, VI Region) | Author reported rural school | Prevention (pre-post design) | Combined nutrition and PA | 8 educational sessions | Not reported | N = 94 students in 1st-5th year of primary school | Malnutrition rate, obesity rate, breakfast/snack eating practices; pre and post | Obesity decreased by 2.1% after the educational program. There was a decrease of 10.6% of students who ate breakfast twice. The prevalence of school children who took a snack from home, and also bought another at school decreased. |
| van Dongen et al.107 2018 Australia (New South Wales) | Author reported areas of social disadvantage | Intervention (qualitative) | Combined nutrition and PA | One 90-minute PA session per week, 20 weeks in total; teacher professional development: 2 full-day workshops (pre- and mid-program) | Teachers (teacher-led PA), students (selfmonitoring), peers (peer-mentoring) | 361 boys in year 7 (eligible if self-reported less than 60 minutes of moderate to vigorous PA/day or more than two hours of recreational screen time per day) | BMI, waist circumference, percentage body fat or for overall activity; boys’ attitudes and behaviors relating to PA and nutrition; need-support practices and self-reported effects | Students reported increased feelings of autonomy, competence, and relatedness; for intervention, no significant effects for BMI, waist circumference, percentage body fat, or for overall activity (see Smith et al., 2014117). However, there was a significant intervention effect for reduced screen time, upper body muscular endurance, and resistance training skill competency. |
| Vogeltanz-Holm and Holm108 2018 US (North Dakota) | Author reported rural schools in the US upper Midwest | Prevention (pre-post design) | Combined nutrition and PA | 3 years | Trained teachers | N = 308 students followed from 3rd-5th grades, ages 6–11 years | BMI z-score (height and weight), assessments beginning of school year, end of school year, and yearly for 2 additional years | There was a significant decrease in BMI z-score across the 3-year study period. Ethnicity analyses showed that White students had overall decreases in BMI z-scores whereas American Indian students’ BMI z-scores remained stable across the program. |
| Williamson et al.57 2008 US (Louisiana) | Author reported rural schools | Prevention (RCT) | Combined nutrition and PA | 28-month; weekly lessons | Research staff and teachers | N = 2097 children in 4th-6th grades (mean age 10.5 years) | Body weight, body fat, food intake, PA, sedentary behavior, and social support: assessed at 18 and 28 months | Primary prevention program resulted in prevention of weight/fat gain in White boys and girls but not in minority children. Addition of the secondary prevention program to the primary prevention program yielded some behavioral changes, but had minimal effects on measures of adiposity. |
| Williamson et al.65 2010 US (Louisiana) | Author reported rural schools | Prevention (RCT) | Combined nutrition and PA | 3 years; weekly lessons of 20–25 minutes, PA of 30 minutes | Research staff and teachers | 17 school clusters; N = 2102 students from 4th-6th grades | BMI z-scores, BMI %ile, body fat, food selections, food intakes, PA, sedentary behavior, psychosocial variables (mood, eating attitudes, and social support for diet and PA) | No results provided; research was ongoing and no results available. |
| Williamson et al.76 2012 US (Louisiana) | Author reported rural communities | Prevention (RCT) | Combined nutrition and PA | 28-month; weekly lessons of 20–25 minutes, PA of 30 minutes | Research staff and teachers | N = 2060 children 4th-6th grades | Body fat, BMI z-scores, dietary intake, PA, and sedentary behavior | Changes in percent body fat % and BMI z-scores, and changes in behaviors related to energy balance were observed. Prevention program was effective for reducing body fat % in boys and attenuating body fat % gain in girls. Comparisons of two treatment arms and control on changes in body fat and BMI z-scores found no differences. |
| Zaremba Morgan et al.93 2014 US (Alabama) | Author reported rural elementary schools | Prevention (quasi-experimental) | Combined nutrition and PA | 10-week | Trained teachers | N = 85 4th graders | Anthropometric measures: height, weight, and BMI; nutrition-related knowledge, attitudes, and behaviors; food self-efficacy, PA self-efficacy, and PA knowledge; healthy body image and attempted weight loss, healthy body size perception, food intake, self-perceptions, avatar assessment | Intervention improved nutrition knowledge and attitudes but no significant changes in anthropometric measures, food intake, selfperceptions. |
| Policy (n = 9) | ||||||||
| Belansky et al.58 2009 US (Colorado) | Author defined rural and low-income schools (outside urban areas) | Prevention (pre-post design) | Policy | Not specified | Not specified | 45 rural elementary schools | School environment and health policy survey: PA and nutrition, presence and enforcement of policies; key informant interviews | Compared 2005–06 school year to 2007–08 school year, time in PA increased 14 minutes/week (not significant change), time for recess decreased 19 minutes/week (not significant change); policies did not change participation; barriers identified included competing pressures, lack of resources devoted to policy, principals being unfamiliar with policy, lack of accountability mechanisms. |
| Ling78 2013 US (Kentucky) | Author reported rural | Prevention (pre-post design) | Policy (and combined nutrition and PA)b | 5 months | Trained healthy lifestyle coaches |
N = 1508 K-5th grade (mean age 8.3 years) |
PA (pedometer) and eating behavior (dietary recall) | Significant improvement in % of children meeting PA recommendations after treatment; significant improvement in % of children meeting nutrition recommendations after treatment; significant treatment effects on PA behavior and increased consumption of fruits and vegetables; effects on nutrition and PA depended on school, age, and grade. |
| Ling et al.85 2014 US (Kentucky) | School rural based on rural-urban commuting areas, using census tract-level demographic and work-commuting data, and economic integration with urban areas | Prevention (pre-post design) | Policy (and combined nutrition and PA)b | 5 months | Trained healthy lifestyle coaches |
N = 1508 K-5th grade students (mean age 8.3 years) |
Nutrition (dietary recall) and PA (pedometer) | Intervention had significant effects on % of children meeting nutrition recommendations and on % of children who met PA recommendations; effects on nutrition and PA depended on school, age, and grade; increasing linear trend of PA and increasing quadratic trend of nutrition over time. |
| Oluyomi et al.89 2014 US (Texas) | Definition not included (home addresses were geocoded) | Prevention (cross-sectional) | Policy (and PA)b | 5 year implementation project; Texas Childhood Obesity Prevention Policy Evaluation; cross- sectional study | Not described | N = 830 parent-student (4th grade) dyads | Self-reported child walking to school; perceived traffic and personal safety concerns for neighborhood, en route to school, school environments, social capital | Odds of walking to school were higher with no problems related to traffic speed, amount of traffic, sidewalks, intersection safety, crossing guards; odds of walking to school were lower with stray animals and concerns with no walking partner. |
| Ramirez and Stafford81 2013 US (California) | Stated rural region, town of < 6000 population) | Prevention (descriptive) | Policy | state-wide; ongoing | Policy implementation at school level | Students in San Joaquin Valley, CA | Weight, decrease in sugar-sweetened beverage, increased water consumption | Some schools have to buy water because tap is contaminated; overall, in addition to policy, need to address infrastructure for providing students with free, clean drinking water in order to prevent disparities in access. |
| Ritchie69 2011 US (West Virginia) | Not defined | Prevention (pre-post design) | Policy (and behavioral)a | 15 weeks; 30 minutes of cognitive behavior skills building education, followed by 20 minutes of PA; parental newsletter every 4 weeks during 15 week intervention | Nurse practitioner or registered nurse | N = 55 9th graders |
BMI, BMI %, teen healthy lifestyle behavior, cognitive beliefs, perceived difficulty in leading a healthy lifestyle, self-esteem, and parent’s healthy lifestyle behaviors, beliefs, and perceived difficulty in leading a healthy lifestyle | Students’ healthy behavior improved from Time 1 (mean = 51.32, standard deviation = 11.15) to Time 2 (mean = 57.45, standard deviation = 9.71), t (43) 3.93, P = 0.000. Subgroup with low self-esteem improved. 49% lost weight, 6% maintained their weight. BMI % improved in 7 teens (moving from obese to overweight or overweight to healthy weight); 1 increased BMI%. |
| Robinson et al.90 2014 US (Alabama) | Author reported 1 county in Black Belt Region | Prevention (cross-sectional) | Policy (and PA)b | Alabama requires daily PE for 30 minutes per day by certified PE teacher; recess and other activities are not included and are considered extra | Certified PE instructor | 5 elementary schools; N = 683 school-age children (341 female; 342 male); mean age 8.2 years; 99.9% Black | BMI, weight status, waist circumference; PA behavior (pedometer step count, System for Observing Fitness Instruction Time, and the System for Observing Play and Leisure Activity in Youth) | Overall, PE and PA state-level policies were only partially implemented; large discrepancy between what is scheduled at school level and what is actually being implemented; PA during PE was students’ only opportunity for school PA. |
| Schetzina et al.62 2009 US (Tennessee) | Author reported Appalachia | Prevention (qualitative) | Policy | Not applicable | Not applicable | 60–90 minute focus groups with adults (23 teachers, 12 parents), and 30–40 minute focus groups with students (19 4th grade students) | Community-needs assessment; qualitative outcomes from focus groups using open-ended questions about school nutrition and PA practices and resources, perceptions of student overweight/obesity; outcomes analyzed using the Coordinated School Health Program model as an analysis framework | Community concerned about obesity, and supports schools doing more; all thought there was a need for healthy eating and PA; parents worried about kid hunger and not in favor of measuring BMI; kids and parents wanted more PA in school; noted school environment, academic pressure, and lack of parental support as barriers. |
| Smith and Holloman91 2014 US (Ohio) | Author reported a rural Appalachian county | Prevention (pre-post design) | Policy (and nutrition)b | 30-day | Teen advisory council (teachers and students from 9th-12th grades) | N = 186 high school students 9th-12th grades from 2 schools (mean age 15.85 years) |
Sugar-sweetened beverage consumption and water consumption pre, post, and 30-day follow-up | Sugar-sweetened beverage consumption decreased significantly, and water consumption increased 19% from baseline to post-intervention. |
| Other (n = 8) | ||||||||
| Askelson et al.109 2019 US (Iowa) | Author reported 5 schools located in rural areas | Prevention (pre-post design) | other | 1 school year | Nutrition researchers | 6 middle schools: 5 rural schools and 1 non-rural school; food service director and staff and student group | Lunchroom perception assessment completed by students, online survey (student, parents, and food service staff), production records (fruit, vegetable, and milk) and telephone interviews with food service directors | 5 out of 6 schools improved lunchroom assessment; 2 out of 5 schools increased servings of fruit; and 3 out of 5 increased servings of vegetables and milk; all food service directors described treatment as successful, and improved communication with students was an important outcome. |
| Gabriele et al.63 2010 US (Louisiana) | Author reported rural school | Prevention (RCT, secondary) | Other (program evaluation) | Weekly for 2.5 school- year period (32 lessons, 5 were repeated = total of 37 lessons); new lesson every 2 weeks | Internet counselor (had bachelor’s degree or higher degree in nutrition, health behavior, psychology, or exercise and sport science); teachers did classroom activities | N = 773 students in 4th-6th grades from 14 schools (mean age 10.5 years) | Treatment implementation information presented; BMI not reported | 12 of 14 schools participated; 763 students accessed site at least 1 time; required 1174 hours of internet counselor coverage to implement. |
| Muzaffar et al.105 2018 Multiple countries (US, Australia, England) | Definition not included | Combined prevention and intervention (RCT and quasi-experimental) | Other (systematic review) | 3–5 sessions | Registered dietitian, trained staff, teachers, parents, volunteers, chefs, and undetermined | 6 intervention studies; included children and early adolescents | Food prep, cooking confidence, trying new foods, cooking attitudes, behaviors, behavioral intentions, fruit and vegetable preference, theoretical constructs (perceptions), anthropometrics (BMI), BP, diet intake, visual estimate intake whole grains and vegetables | Improvement in cooking and healthy eating, cooking self-efficacy, cooking behavioral intentions, food-prep frequency, knowledge, healthy diet intake, BMI, BP. |
| Ning et al.88 2014 China (Qingdao) | Not defined | Prevention (RCT) | Other | Information not provided | Information not provided | 15,095 primary and secondary school children/adolescents | Prevalence of overweight/obesity, PA, sedentary time | No difference in overweight/obesity prevalence between health education and control groups; weight, BMI, TV time, homework significantly lower in education group (P < 0.001); increased awareness of type 2 diabetes mellitus and risk factors higher in education group. |
| Sanigorski et al.56 2008 Australia (Colac, Victoria) | Author reported town of about 11,000 inhabitants in rural area | Prevention (quasi-experimental) | Other (Community Capacity Building) | 3 years | Colac Area Health, Colac Otway Shire and Colac Neighborhood Renewal; Deakin University provided support | 4 preschools and 6 primary schools at baseline (2003, N = 1001) and follow-up (2006, N = 839) Controls: 4 preschools and 12 primary schools baseline (N = 1183) and follow-up in (2006, N = 979) | Differences in the increases in anthropometry (weight, waist, waist-to-height ratio and BMI z-score) over time and the relationship between baseline indicators of children’s household socioeconomic status | Intervention significantly lower increases in body weight, waist, and BMI z-score. |
| Schiller et al.51 2007 US (Colorado) | Author reported, Fort Collins, CO | Prevention (pre-post design [abstract]) | Other (body science focus) | 8-week program | Not determined | Teachers and 6th grade students from 1 school; specifics not included | Knowledge, attitudes, body acceptance, interest in science-health careers | Better health and science knowledge (brain science), attitudes (mental illness), behaviors (sensory physiology, increased body acceptance), and increased interest in science/health-related careers. |
| Slaney et al.73 2012 Australia (Mansfield in NE Victoria) | Author reported rural campus near Mansfield in NE Victoria, Australia | Prevention (pre-post design) | Other (residential school program) | 10 months (Feb-Nov) | Not specified | N = 1021 year 9 students (mean age 14.9 years) | BMI pre and post | Participation in program reduced BMI of boys who were in normal to obese range but not in girls. |
| Whelan et al.112 2019 Australia (Victoria) | Author reported rural and remote | Prevention (pre-post design) | Other (communityled local determinants) | 3.5 years | Communityled | Community; workplaces and children in kindergarten | Community readiness assessments, community-based systems dynamics, workforce audit, policy audit and changes in kindergartens, workplaces, schools, food supply audit, preexisting anthropometric data analysis, sales data, lunchbox audits and key informant interviews | Local children at 3.5 years recorded a lower prevalence of overweight and obesity compared to state’s average (11.4% vs. 20%). Discretionary foods in kindergarten lunchboxes was significantly reduced. Workforce audits revealed 1.3 full time equivalent available for obesity prevention (7000 km2). |
%ile, percentile; BMI, body mass index; BP, blood pressure; HDL, high-density lipoprotein; K, kindergarten; LDL, low-density lipoprotein; PA, physical activity; PE, physical education; RCT, randomized controlled trial; SNAP-Ed, Supplemental Nutrition Assistance Program Education; Tx, treatment; US, United States
The prevention program also included behavioral components.
The prevention program is listed in the table under more than one component.
Footnotes
The authors declare no conflict of interest.
References
- 1.Bauman A, Rutter H, Baur L. Too little, too slowly: International perspectives on childhood obesity. Public Health Res Pract 2019;29(1):1–5. [DOI] [PubMed] [Google Scholar]
- 2.Daniels SR. The consequences of childhood overweight and obesity. Future Child 2006;16(1):47–67. [DOI] [PubMed] [Google Scholar]
- 3.Estrada E, Eneli I, Hampl S, Mietus-Snyder M, Mirza N, Rhodes E, et al. Children’s Hospital Association consensus statements for comorbidities of childhood obesity. Child Obes 2014;10(4):304–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Morrison KM, Shin S, Tarnopolsky M, Taylor VH. Association of depression & health related quality of life with body composition in children and youth with obesity. J Affect Disord 2015;172:18–23. [DOI] [PubMed] [Google Scholar]
- 5.Schwimmer JB, Burwinkle TM, Varni JW. Health-related quality of life of severely obese children and adolescents. JAMA 2003;289(14):1813–9. [DOI] [PubMed] [Google Scholar]
- 6.Lim CS, Espil FM, Viana AG, Janicke DM. Associations between anxiety symptoms and child and family factors in pediatric obesity. J Dev Behav Pediatr 2015;36(9):664–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Puhl RM, Luedicke J. Weight-based victimization among adolescents in the school setting: emotional reactions and coping behaviors. J Youth Adolesc 2012;41(1):27–40. [DOI] [PubMed] [Google Scholar]
- 8.Reilly JJ, Kelly J. Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: systematic review. Int J Obes 2011;35(7):891–8. [DOI] [PubMed] [Google Scholar]
- 9.Cawley J The economics of childhood obesity. Health Aff (Millwood) 2010;29(3):364–71. [DOI] [PubMed] [Google Scholar]
- 10.Seidell JC, Halberstadt J. The global burden of obesity and the challenges of prevention. Ann Nutr Metab 2015;66:(Suppl 2):7–12. [DOI] [PubMed] [Google Scholar]
- 11.Wang Y, Beydoun MA, Liang L, Caballero B, Kumanyika SK. Will all Americans become overweight or obese? Estimating the progression and cost of the US obesity epidemic. Obesity 2008;16(10):2323–30. [DOI] [PubMed] [Google Scholar]
- 12.Skinner AC, Ravanbakht SN, Skelton JA, Perrin EM, Armstrong SC. Prevalence of obesity and severe obesity in US children, 1999–2016. Pediatrics 2018;141(3):e20173459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Agency for Healthcare Research and QualityNational Healthcare Quality and Disparities Report Chartbook on Rural Health Care. Rockville, MD: Agency for Healthcare Research and Quality; 2017. [Google Scholar]
- 14.World Bank Group. Rural population [internet]. The World Bank Group; 2019. [cited 2019 Apr 16]. Available from: https://data.worldbank.org/indicator/sp.rur.totl.zs. [Google Scholar]
- 15.Johnson JA 3rd, Johnson AM. Urban-rural differences in childhood and adolescent obesity in the United States: a systematic review and meta-analysis. Child Obes 2015;11(3):233–41. [DOI] [PubMed] [Google Scholar]
- 16.Lemas DJ, Cardel MI, Filipp SL, Hall J, Essner RZ, Smith SR, et al. Objectively measured pediatric obesity prevalence using the OneFlorida Clinical Research Consortium. Obes Res Clin Pract 2019;13(1):12–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Todic J, Scott J. Unincorporated health: understanding residents’ perspectives on factors impacting their health and emergent place-based solutions. Soc Work Public Health 2021;36(3):317–29. [DOI] [PubMed] [Google Scholar]
- 18.Befort CA, Nazir N, Perri MG. Prevalence of obesity among adults from rural and urban areas of the United States: findings from NHANES (2005–2008). J Rural Health 2012;28(4):392–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mohatt NV, Kreisel CJ, Hoffberg AS, Mph LW, Beehler SJ. A systematic review of factors impacting suicide risk among rural adults in the United States. J Rural Health 2021;37(3):565–75. [DOI] [PubMed] [Google Scholar]
- 20.Scott J, Dardas L, Sloane R, Wigington T, Noonan D, Simmons LA. Understanding social determinants of cardiometabolic disease risk in rural women. J Community Health 2020;45(1):1–9. [DOI] [PubMed] [Google Scholar]
- 21.Weeks KS, Lynch CF, West M, McDonald M, Carnahan R, Stewart SL, et al. Impact of rurality on stage IV ovarian cancer at diagnosis: a Midwest Cancer Registry Cohort Study. J Rural Health 2020;36(4):468–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Davis AM, Bennett KJ, Befort C, Nollen N. Obesity and related health behaviors among urban and rural children in the United States: data from the National Health And Nutrition Examination Survey 2003–2004 and 2005–2006. J Pediatr Psychol 2011;36(6):669–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lichter DT. Immigration and the new racial diversity in rural America. Rural Sociol 2012;77(1):3–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Broskey NT, Wang P, Li N, Leng JH, Li WQ, Wang LS, et al. Early pregnancy weight gain exerts the strongest effect on birth weight, posing a critical time to prevent childhood obesity. Obesity 2017;25(9):1569–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Witte AL, Sheridan SM. Family engagement in rural schools. In: Redding S, Murphy M, Sheley P, eds. Handbook on Family and Community Engagement. Charlotte, NC: Information Age Publishing, Inc; 2011. 153–6. [Google Scholar]
- 26.World Health Organization. Report of the Commission on Ending Childhood Obesity [internet]. WHO; 2017. [cited 2018 May 15]. Available from: http://apps.who.int/iris/bitstream/10665/204176/1/9789241510066_eng.pdf?ua=1. [Google Scholar]
- 27.Centers for Disease Control and Prevention. Whole School, Whole Community, Whole Child (WSCC) [internet]. CDC; 2018. [updated 2018 Nov 14; cited 2019 Apr 16]. Available from: https://www.cdc.gov/healthyschools/wscc/index.htm. [Google Scholar]
- 28.Hu Y, He JR, Liu FH, Li WD, Lu JH, Xing YF, et al. Effectiveness of a kindergarten-based intervention for preventing childhood obesity. Pediatrics 2017;140(6):e20171221. [DOI] [PubMed] [Google Scholar]
- 29.Wang Y, Wu Y, Wilson RF, Bleich S, Cheskin L, Weston C, et al. Childhood obesity prevention programs: comparative effectiveness review and meta-analysis. AHRQ Comparative Effectiveness Reviews. Rockville, MD: AHRQ; 2013. [PubMed] [Google Scholar]
- 30.Yang Y, Kang B, Lee EY, Yang HK, Kim HS, Lim SY, et al. Effect of an obesity prevention program focused on motivating environments in childhood: a school-based prospective study. Int J Obes 2017;41(7):1027–34. [DOI] [PubMed] [Google Scholar]
- 31.Lim CS, Janicke DM. Barriers related to delivering peditric weight management interventions to children and families from rural communities. Child Health Care 2013;42:214–30. [Google Scholar]
- 32.Rural Health Information Hub. What is rural? [internet]. U.S. Department of Health and Human Services. RHIhub; n.d. [cited 2019 Apr 17]. Available from: https://www.ruralhealthinfo.org/topics/what-is-rural. [Google Scholar]
- 33.United Nations. Population density and urbanization [internet]. United Nations; 2017. [cited 2019 Apr 17]. Available from: https://unstats.un.org/UNSD/demographic/sconcerns/densurb/densurbmethods.htm. [Google Scholar]
- 34.UK Department for Environment, Food & Rural Affairs. Defining rural areas. England: Office for National Statistics Rural Urban Classification [internet]. Crown; 2017. [cited 2019 Apr 19]. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/597751/Defining_rural_areas__Mar_2017_.pdf. [Google Scholar]
- 35.Ratcliffe M, Burd C, Holder K, Fields A. Defining rural at the U.S. Census Bureau. Washington, DC: U.S. Census Bureau; 2016. [Google Scholar]
- 36.Robinson JC, Lim CS, Hinton E, Pintado I, Gamble A, Compretta C, et al. School-based obesity prevention programs in rural communities: a scoping review protocol. JBI Database System Rev Implement Rep 2019;17(7):1326–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Peters MDJ, Marnie C, Tricco AC, Pollock D, Munn Z, Alexander L, et al. Updated methodological guidance for the conduct of scoping reviews. JBI Evid Synth 2020;18(10):2119–26. [DOI] [PubMed] [Google Scholar]
- 38.von Hippel PT, Nahhas RW. Extending the history of child obesity in the United States: the Fels Longitudinal Study, Birth Years 1930–1993. Obesity 2013;21(10):2153–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Martinez-Vizcaino V, Sanchez Lopez M, Moya Martinez P, Solera Martinez M, Notario Pacheco B, Salcedo Aguilar F, et al. Trends in excess weight and thinness among Spanish schoolchildren in the period 1992–2004: the Cuenca study. Public Health Nutr 2009;12(7):1015–8. [DOI] [PubMed] [Google Scholar]
- 40.Lazzeri G, Rossi S, Pammolli A, Pilato V, Pozzi T, Giacchi MV. Underweight and overweight among children and adolescents in Tuscany (Italy). Prevalence and short-term trends. J Prev Med Hyg 2008;49(1):13–21. [PubMed] [Google Scholar]
- 41.Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 2018;169(7):467–73. [DOI] [PubMed] [Google Scholar]
- 42.Angelico F, Del Ben M, Fabiani L, Lentini P, Pannozzo F, Urbinati GC, et al. Management of childhood obesity through a school-based programme of general health and nutrition education. Public Health 1991;105(5):393–8. [DOI] [PubMed] [Google Scholar]
- 43.Davis S, Gomez Y, Lambert L, Skipper B. Primary prevention of obesity in American Indian children. Ann NY Acad Sci 1993;699(1):167–80. [DOI] [PubMed] [Google Scholar]
- 44.Donnelly JE, Jacobsen DJ, Whatley JE, Hill JO, Swift LL, Cherrington A, et al. Nutrition and physical activity program to attenuate obesity and promote physical and metabolic fitness in elementary school children. Obes Res 1996;4(3):229–43. [DOI] [PubMed] [Google Scholar]
- 45.Carrel AL, Clark RR, Peterson SE, Nemeth BA, Sullivan J, Allen DB. Improvement of fitness, body composition, and insulin sensitivity in overweight children in a school-based exercise program: a randomized, controlled study. Arch Pediatr Adolesc Med 2005;159(10):963–8. [DOI] [PubMed] [Google Scholar]
- 46.Harrell TK, Davy BM, Stewart JL, King DS. Effectiveness of a school-based intervention to increase health knowledge of cardiovascular disease risk factors among rural Mississippi middle school children. South Med J 2005;98(12):1173–80. [DOI] [PubMed] [Google Scholar]
- 47.Cason KL, Logan BN. Education intervention improves 4th-grade schoolchildren’s nutrition and physical activity knowledge and behaviors. Top Clin Nutr 2006;21(3):234–40. [Google Scholar]
- 48.Hawley SR, Beckman H, Bishop T. Development of an obesity prevention and management program for children and adolescents in a rural setting. J Community Health Nurs 2006;23(2):69–80. [DOI] [PubMed] [Google Scholar]
- 49.Culbertson DL. Mini-Program ENERGY Cortez: obesity and type 2 diabetes prevention through science enrichment for elementary school children in rural southwestern Colorado [thesis]. Colorado State University; 2007. [Google Scholar]
- 50.Gombosi RL, Olasin RM, Bittle JL. Tioga County Fit for Life: a primary obesity prevention project. Clin Pediatr 2007;46(7):592–600. [DOI] [PubMed] [Google Scholar]
- 51.Schiller K, Suchor L, Smith F, Porter D, Murt L, Allen J, et al. Program ENERGY: an extension focusing on brain and nervous system science for 6th-grade elementary school children. Appetite 2007;49(1):328. [Google Scholar]
- 52.Smith FJ, Porter D, Holliday A, Durham S, Murt L, Allen J, et al. Program ENERGY: scientists and students in the classroom tackle type 2 diabetes and obesity in elementary schools in three states. Appetite 2007;49(1):332. [Google Scholar]
- 53.Manley D Self-efficacy, physical activity, and aerobic fitness in middle school children: examination of a pedometer intervention program University of Tennessee Health Science Center; 2008. [DOI] [PubMed]
- 54.Muth ND, Chatterjee A, Williams D, Cross A, Flower K. Making an IMPACT: effect of a school-based pilot intervention. N C Med J 2008;69(6):432–40. [PubMed] [Google Scholar]
- 55.Rye J, Tompkins NO, McClure D, Aleshire J. Adolescents and teachers as partners in a school-based research project to increase physical activity opportunities in a rural community. Rural Educator 2008;30(1):39–48. [Google Scholar]
- 56.Sanigorski AM, Bell AC, Kremer PJ, Cuttler R, Swinburn BA. Reducing unhealthy weight gain in children through community capacity-building: results of a quasi-experimental intervention program, Be Active Eat Well. Int J Obes 2008; 32(7):1060–7. [DOI] [PubMed] [Google Scholar]
- 57.Williamson DA, Champagne CM, Harsha D, Han H, Martin CK, Newton R Jr, et al. Louisiana (LA) Health: design and methods for a childhood obesity prevention program in rural schools. Contemp Clin Trials 2008;29(5):783–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Belansky ES, Cutforth N, Delong E, Ross C, Scarbro S, Gilbert L, et al. Early impact of the federally mandated Local Wellness Policy on physical activity in rural, low-income elementary schools in Colorado. J Public Health Policy 2009;30(Suppl 1):S141–60. [DOI] [PubMed] [Google Scholar]
- 59.Canavera M, Sharma M, Murnan J. Development and pilot testing a social cognitive theory-based intervention to prevent childhood obesity among elementary students in rural Kentucky. Int Q Community Health Educ 2009;29(1):57–70. [DOI] [PubMed] [Google Scholar]
- 60.Harwood TM. School based exercise and nutrition intervention: effects on health measures in rural children [thesis]. Ohio University; 2009. [Google Scholar]
- 61.Schetzina KE, Dalton WT 3rd, Lowe EF, Azzazy N, Von-Werssowetz KM, Givens C, et al. A coordinated school health approach to obesity prevention among Appalachian youth: the Winning with Wellness Pilot Project. Fam Community Health 2009;32(3):271–85. [DOI] [PubMed] [Google Scholar]
- 62.Schetzina KE, Dalton WT 3rd, Lowe EF, Azzazy N, Vonwerssowetz KM, Givens C, et al. Developing a coordinated school health approach to child obesity prevention in rural Appalachia: results of focus groups with teachers, parents, and students. Rural Remote Health 2009;9(4):1157. [PubMed] [Google Scholar]
- 63.Gabriele JM, Stewart TM, Sample A, Davis AB, Allen R, Martin CK, et al. Development of an internet-based obesity prevention program for children. J Diabetes Sci Technol 2010;4(3):723–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Naylor PJ, Scott J, Drummond J, Bridgewater L, McKay HA, Panagiotopoulos C. Implementing a whole school physical activity and healthy eating model in rural and remote first nations schools: a process evaluation of action schools! BC. Rural Remote Health 2010;10(2):1296. [PubMed] [Google Scholar]
- 65.Williamson DA, Champagne CM, Harsha D, Han H, Martin CK, Newton R, et al. Efficacy of two obesity prevention programs in rural schools: primary outcomes for the Louisiana (LA) health study. Obes Rev 2010;11:59. [Google Scholar]
- 66.Craven KW, Moore JB, Swart AS, Keene AF, Kolasa KM. School-based nutrition education intervention: effect on achieving a healthy weight among overweight ninth-grade students. J Public Health Manag Pract 2011;17(2):141–6. [DOI] [PubMed] [Google Scholar]
- 67.Gittelsohn J, Rowan M. Preventing diabetes and obesity in American Indian communities: the potential of environmental interventions. Am J Clin Nutr 2011;93(5):1179S–83S. [DOI] [PubMed] [Google Scholar]
- 68.Lazorick S, Hardison GT Jr, Esserman DA, Perrin EM. Sustained body mass index changes one and two years post MATCH: a school-based wellness intervention in adolescents. Child Obes 2011;7(5):372–8. [Google Scholar]
- 69.Ritchie T Evaluation of the impact of the Creating Opportunity for Personal Empowerment (COPE) Healthy Lifestyles Thinking, Emotions, Exercise, and Nutrition (TEEN) program in a rural high school health class [dissertation]. West Virginia University; 2011. [Google Scholar]
- 70.Schetzina KE, Dalton WT 3rd, Pfortmiller DT, Robinson HF, Lowe EF, Stern HP. The Winning with Wellness pilot project: rural Appalachian elementary student physical activity and eating behaviors and program implementation 4 years later. Fam Community Health 2011;34(2):154–62. [DOI] [PubMed] [Google Scholar]
- 71.Conway P, Haller IV, Lutfiyya MN. School-aged overweight and obese children in rural America. Dis Mon 2012;58(11):639–50. [DOI] [PubMed] [Google Scholar]
- 72.Rush E, Reed P, McLennan S, Coppinger T, Simmons D, Graham D. A school-based obesity control programme: Project Energize. Two-year outcomes. Br J Nutr 2012;107(4):581–7. [DOI] [PubMed] [Google Scholar]
- 73.Slaney G, Salmon J, Weinstein P. Can a school based programme in a natural environment reduce BMI in overweight adolescents? Med Hypotheses 2012;79(1):68–70. [DOI] [PubMed] [Google Scholar]
- 74.Tomlin D, Naylor PJ, McKay H, Zorzi A, Mitchell M, Panagiotopoulos C. The impact of Action Schools! BC on the health of Aboriginal children and youth living in rural and remote communities in British Columbia. Int J Circumpolar Health 2012;71:17999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Tussing-Humphreys L, Thomson J, McCabe-Sellers B, Strickland E, Lovera D, Bogle M. A school-based fruit and vegetable snacking pilot intervention for lower Mississippi Delta children. Infant Child Adolesc Nutr 2012;4(6):340–7. [Google Scholar]
- 76.Williamson DA, Champagne CM, Harsha DW, Han H, Martin CK, Newton RL Jr, et al. Effect of an environmental school-based obesity prevention program on changes in body fat and body weight: a randomized trial. Obesity 2012;20(8):1653–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Bergan T Low density lipoprotein cholesterol decreases in fifth-grade students following the teen taught KidQuest Program [thesis]. South Dakota State University; 2013. [Google Scholar]
- 78.Ling J Preliminary assessment of a school-based healthy lifestyle program among rural children [thesis]. University of Louisville; 2013. [Google Scholar]
- 79.Moss A, Smith S, Null D, Long Roth S, Tragoudas U. Farm to school and nutrition education: positively affecting elementary school-aged children’s nutrition knowledge and consumption behavior. Child Obes 2013;9(1):51–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Puma J, Romaniello C, Crane L, Scarbro S, Belansky E, Marshall JA. Long-term student outcomes of the integrated nutrition and physical activity program. J Nutr Educ Behav 2013;45(6):635–42. [DOI] [PubMed] [Google Scholar]
- 81.Ramirez SM, Stafford R. Equal and universal access? Water at mealtimes, inequalities, and the challenge for schools in poor and rural communities. J Health Care Poor Under-served 2013;24(2):885–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Ronsley R, Lee AS, Kuzeljevic B, Panagiotopoulos C. Healthy buddies™ reduces body mass index z-score and waist circumference in aboriginal children living in remote coastal communities. J Sch Health 2013;83(9):605–13. [DOI] [PubMed] [Google Scholar]
- 83.Valenzuela C, Gonzalez ML, Vielma B. Intervention in rural school to promote healthy lifestyles. Ann Nutr Metab 2013;63:1025. [Google Scholar]
- 84.Lazorick S, Crawford Y, Gilbird A, Fang X, Burr V, Moore V, et al. Long-term obesity prevention and the Motivating Adolescents with Technology to CHOOSE Health program. Child Obes 2014;10(1):25–33. [DOI] [PubMed] [Google Scholar]
- 85.Ling J, King KM, Speck BJ, Kim S, Wu D. Preliminary assessment of a school-based healthy lifestyle intervention among rural elementary school children. J Sch Health 2014;84(4):247–55. [DOI] [PubMed] [Google Scholar]
- 86.Llaurado E, Tarro L, Morina D, Queral R, Giralt M, Sola R. EdAl-2 (Educacio en Alimentacio) programme: reproducibility of a cluster randomised, interventional, primary-school-based study to induce healthier lifestyle activities in children. BMJ Open 2014;4(11):e005496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Manley D, Cowan P, Graff C, Perlow M, Rice P, Richey P, et al. Self-efficacy, physical activity, and aerobic fitness in middle school children: examination of a pedometer intervention program. J Pediatr Nurs 2014;29(3):228–37. [DOI] [PubMed] [Google Scholar]
- 88.Ning F, Wang YM, Wang SJ, Sun JP, Ren J, Gao WG, et al. Lifestyle education on diabetes in children and in adolescents: Results from school-based settings in China. Diabetes Res Clin Pract 2014;106:S207–8. [Google Scholar]
- 89.Oluyomi AO, Chanam L, Nehme E, Dowdy D, Ory MG, Hoelscher DM. Parental safety concerns and active school commute: correlates across multiple domains in the home-to-school journey. Int J Behav Nutr Phys Act 2014;11:1–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Robinson LE, Wadsworth DD, Kipling Webster E, Bassett DR Jr. School reform: the role of physical education policy in physical activity of elementary school children in alabama’s black belt region. Am J Health Promot 2014;28:(Suppl 3):S72–6. [DOI] [PubMed] [Google Scholar]
- 91.Smith LH, Holloman C. Piloting “sodabriety”: a school-based intervention to impact sugar-sweetened beverage consumption in rural Appalachian high schools. J Sch Health 2014;84(3):177–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Struempler BJ, Parmer SM, Mastropietro LM, Arsiwalla D, Bubb RR. Changes in fruit and vegetable consumption of third-grade students in body quest: food of the warrior, a 17-class childhood obesity prevention program. J Nutr Educ Behav 2014;46(4):286–92. [DOI] [PubMed] [Google Scholar]
- 93.Zaremba Morgan A, Ulrich P, Simmons KP, Gropper SS, Connell LJ, Daniels MK, et al. Effectiveness of a multifaceted, school-based health intervention program with 4th graders in Alabama. Child Youth Serv Rev 2014;37:46–54. [Google Scholar]
- 94.Bumaryoum N Kidquest Childhood Obesity Prevention program: analysis of its influence on health of rural South Dakota 5th and 6th grade children [dissertation]. South Dakota State University; 2015. [Google Scholar]
- 95.Heelan KA, Bartee RT, Nihiser A, Sherry B. Healthier school environment leads to decreases in childhood obesity: the Kearney Nebraska Story. Child Obes 2015;11(5):600–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Langham G A community-academic collaboration to impact childhood obesity. Int J Health Wellness Soc 2015;5(3):43–58. [Google Scholar]
- 97.Murimi MW, Chrisman MS, Hughes K, Taylor C, Kim Y, McAllister TL. Effects of school-based point-of-testing counselling on health status variables among rural adolescents. Health Educ J 2015;74(5):557–67. [Google Scholar]
- 98.Rodriguez MT, Lamm AJ, Odera E, Owens C, Thompson S. Evaluating impacts of school-based extension garden programs from a child’s perspective. J Extension 2015;53(1): [Google Scholar]
- 99.Slawson DL, Dalton WT 3rd, Dula TM, Southerland J, Wang L, Littleton MA, et al. Team Up for Healthy Living: cross-peer obesity prevention intervention has positive impact for high school students in rural Appalachia. J Acad Nutr Diet 2015;115(9 suppl):A51. [Google Scholar]
- 100.Eichner JE, Folorunso OA, Moore WE. A physical activity intervention and changes in body mass index at a middle school with a large American Indian population, Oklahoma, 2004–2009. Prev Chronic Dis 2016;13:E163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Hoying J, Melnyk BM, Arcoleo K. Effects of the COPE cognitive behavioral skills building TEEN program on the healthy lifestyle behaviors and mental health of Appalachian early adolescents. J Pediatr Health Care 2016;30(1):65–72. [DOI] [PubMed] [Google Scholar]
- 102.Nanney MS, Shanafelt A, Wang Q, Leduc R, Dodds E, Hearst M, et al. Project BreakFAST: rationale, design, and recruitment and enrollment methods of a randomized controlled trial to evaluate an intervention to improve school breakfast program participation in rural high schools. Contemp Clin Trials Commun 2016;3:12–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Brown E Impact of a community-wide multi-level obesity prevention intervention for children in rural communities [thesis]. University of Washington; 2018. [Google Scholar]
- 104.Hawkins KR, Burton JH, Apolzan JW, Thomson JL, Williamson DA, Martin CK. Efficacy of a school-based obesity prevention intervention at reducing added sugar and sodium in children’s school lunches: the LA Health randomized controlled trial. Int J Obes 2018;42(11):1845–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Muzaffar H, Metcalfe JJ, Fiese B. Narrative review of culinary interventions with children in schools to promote healthy eating: directions for future research and practice. Curr Dev Nutr 2018;2(6):nzy016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Smith LH, Petosa RL, Shoben A. Peer mentor versus teacher delivery of a physical activity program on the effects of BMI and daily activity: protocol of a school-based group randomized controlled trial in Appalachia. BMC Public Health 2018;18(1):633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.van Dongen B, Finn T, Hansen V, Wagemakers A, Lubans D, Dally K. The ATLAS school-based health promotion programme. Eur Phy Educ Rev 2018;24(3):330–48. [Google Scholar]
- 108.Vogeltanz-Holm N, Holm J. Changes in body mass index during a 3-year elementary school-based obesity prevention program for American Indian and White rural students. Health Educ Behav 2018;45(2):277–85. [DOI] [PubMed] [Google Scholar]
- 109.Askelson NM, Brady P, Ryan G, Meier C, Ortiz C, Scheidel C, et al. Actively involving middle school students in the implementation of a pilot of a behavioral economics-based lunchroom intervention in rural schools. Health Promot Pract 2019;20(5):675–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Hao M, Han W, Yamauchi T. Short-term and long-term effects of a combined intervention of rope skipping and nutrition education for overweight children in Northeast China. Asia-Pacific J Public Health 2019;31(4):348–58. [DOI] [PubMed] [Google Scholar]
- 111.Lin YC, Chen HJ, Wang Y, Min J, Wu HC, Carvajal NA, et al. NASA Mission X Program for healthy eating and active living among Taiwanese elementary school students. J Pediatr Nurs 2019;49:e8–14. [DOI] [PubMed] [Google Scholar]
- 112.Whelan J, Love P, Millar L, Allender S, Bell C. Can the community of a rural and remote Australian local government area lead and sustain obesity prevention? Obes Res Clin Pract 2019;13(3):273. [Google Scholar]
- 113.Smith LH, Petosa RL, Laurent D. Efficacy of “Mentoring to Be Active” on weight loss, body mass index, and body fat among obese and extremely obese youth in rural Appalachia. J Rural Health 2020;36(1):77–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.US Preventive Services Task ForceScreening for obesity in children and adolescents: US Preventive Services Task Force Recommendation Statement. JAMA 2017;317(23):2417–26. [DOI] [PubMed] [Google Scholar]
- 115.Brown AW, Altman DG, Baranowski T, Bland JM, Dawson JA, Dhurandhar NV, et al. Childhood obesity intervention studies: a narrative review and guide for investigators, authors, editors, reviewers, journalists, and readers to guard against exaggerated effectiveness claims. Obes Rev 2019;20(11):1523–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Zahnd WE, Mueller-Luckey GS, Fogleman AJ, Jenkins WD. Rurality and health in the United States: do our measures and methods capture our intent? J Health Care Poor Underserved 2019;30(1):70–9. [DOI] [PubMed] [Google Scholar]
- 117.Smith JJ, Morgan PJ, Plotnikoff RC, et al. (2014b) Smartphone obesity prevention trial for adolescent boys in low-income communities: the ATLAS RCT. Pediatrics 134(3):e723–e731. [DOI] [PubMed] [Google Scholar]
Appendix II: Studies ineligible following full-text review
- 1.Adom T, De Villiers A, Puoane T, Kengne AP. School-based interventions targeting nutrition and physical activity, and body weight status of African children: a systematic review. Nutrients. 2019;12(1). [DOI] [PMC free article] [PubMed] [Google Scholar]; Reason for exclusion: ineligible context – included both rural and urban settings
- 2.Baker K, Hagedorn RL, Hendricks T, Clegg EN, Joseph L, McGowan M, et al. Katalyst: development of a fifth-grade novel approach to health and science experiential learning. Sci Act. 2018;55(3–4):127–39. [PMC free article] [PubMed] [Google Scholar]; Reason for exclusion: ineligible concept – no outcomes reported
- 3.Hosseini H, Yilmaz A. Using telehealth to address pediatric obesity in rural Pennsylvania. Hosp Top. 2019;97(3):107–18. [DOI] [PubMed] [Google Scholar]; Reason for exclusion: ineligible concept – no outcomes reported
- 4.Lyders S Evaluation of a daily activity program for early school-age children in a rural setting. 2019.; Reason for exclusion: ineligible population – adults
- 5.Marchetti D, Fraticelli F, Polcini F, Fulcheri M, Mohn AA, Vitacolonna E. A school educational intervention based on a serious game to promote a healthy lifestyle. Mediterranean J Clin Psychol. 2018;6(3):1–16. [Google Scholar]; Reason for exclusion: ineligible context – both rural and urban settings
- 6.Mitchell B, McLennan S, Latimer K, Graham D, Gilmore J, Rush E. Improvement of fundamental movement skills through support and mentorship of class room teachers. Obes Res Clin Pract. 2013;7(3):e230–e4. [DOI] [PubMed] [Google Scholar]; Reason for exclusion: ineligible concept – outcomes
- 7.Morshed AB, Davis SM, Keane PC, Myers OB, Mishra SI. The impact of the CHILE Intervention on the food served in Head Start centers in rural New Mexico. J Sch Health. 2016;86(6):414–23. [DOI] [PMC free article] [PubMed] [Google Scholar]; Reason for exclusion: ineligible population – younger children
- 8.ClinicalTrials.gov. Families and schools for health [internet]. 2016. [cited 2019 Jul 22]. Available from: https://clinicaltrialsgov/show/nct02659319.; Reason for exclusion: ineligible concept – no outcomes reported
- 9.ClinicalTrials.gov. Rural disparities in pediatric obesity: the iAmHealthy Intervention [internet]. 2017. [cited 2019 Jul 22]. Available from: https://clinicaltrialsgov/show/nct03304249.; Reason for exclusion: ineligible concept – no outcomes reported
- 10.ClinicalTrials.gov. Systems-oriented school healthy weight promotion based on NASA Mission X Campaign [internet]. 2017. [cited 2019 Jul 22]. Available from: https://clinicaltrialsgov/show/nct03355131.; Reason for exclusion: ineligible concept – no outcomes reported
- 11.Raczynski JM, Thompson JW, Phillips MM, Ryan KW, Cleveland HW. Arkansas Act 1220 of 2003 to reduce childhood obesity: its implementation and impact on child and adolescent body mass index. J Public Health Policy. 2009;30 Suppl 1:S124–40. [DOI] [PubMed] [Google Scholar]; Reason for exclusion: ineligible context – both rural and urban settings
- 12.Richards K, Slawson DL, Johns-Wommack R, Smith S. Identifying demographic risk factors for pediatric obesity: a multitvariate analysis of Tennessee coordinated school health BMI reports for 2007–2008. Obesity. 2011;19:S127–S8. [Google Scholar]; Reason for exclusion: ineligible concept – not program/intervention
- 13.Roche E, Kolodinsky JM, Johnson RK, Pharis M, Banning J. School gardens may combat childhood obesity. Choices. 2017;32(1):1–6. [Google Scholar]; Reason for exclusion: ineligible context – both rural and urban settings
- 14.Rush E, Reed PW, Simmons D, Coppinger T, McLennan S, Graham D. Baseline measures for a school-based obesity control programme: Project Energize: differences by ethnicity, rurality, age and school socio-economic status. J Paediatr Child Health. 2013;49(4):E324–31. [DOI] [PubMed] [Google Scholar]; Reason for exclusion: ineligible concept – no outcomes reported
- 15.Sadeghi B, Kaiser LL, Hanbury MM, Tseregounis IE, Shaikh U, Gomez-Camacho R, et al. A three-year multifaceted intervention to prevent obesity in children of Mexican-heritage. BMC Public Health. 2019;19(1):1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]; Reason for exclusion: ineligible population – younger children
- 16.Samuels CA. Studies evaluate school wellness policies. Education Week. 2009;28(23):4. [Google Scholar]; Reason for exclusion: ineligible concept – not program/intervention
- 17.Shephard RJ, Trudeau F. Quality daily physical education for the primary school student: a personal account of the Trois-Rivières Regional Project. Quest. 2013;65(1):98–115. [Google Scholar]; Reason for exclusion: ineligible context – both rural and urban settings
- 18.Silva Silveira D, Barbosa Ferreira Lemos LFG, Miranda Tassitano R, Teresa Cattuzzo M, Pereira Feitoza AH, Moreira Carneiro Aires LMS, et al. Effect of a pilot multi-component intervention on motor performance and metabolic risks in overweight/obese youth. J Sports Sci. 2018;36(20):2317–26. [DOI] [PubMed] [Google Scholar]; Reason for exclusion: ineligible context – urban setting
- 19.Slawson DL, Dalton WT 3rd, Dula TM, Southerland J, Wang L, Littleton MA, et al. College students as facilitators in reducing adolescent obesity disparity in Southern Appalachia: Team Up for Healthy Living. Contemp Clin Trials. 2015;43:39–52. [DOI] [PMC free article] [PubMed] [Google Scholar]; Reason for exclusion: ineligible concept – no outcomes reported
- 20.Smith LH, Holloman C. Comparing the effects of teen mentors to adult teachers on child lifestyle behaviors and health outcomes in Appalachia. J Sch Nurs. 2013;29(5):386–96. [DOI] [PMC free article] [PubMed] [Google Scholar]; Reason for exclusion: ineligible concept – after school program
- 21.Southerland J, Slawson DL, Schetzina KE, Dalton WT 3rd. Implementation of the go slow whoa meal pattern in schools through the winning with wellness project: food service workers’ perceptions of implementation feasibility and impact. Obesity. 2011;19:S150. [Google Scholar]; Reason for exclusion: ineligible population – adults
- 22.National Center for Education Statistics. Nutrition education in public elementary and secondary schools [internet]. 1996. [cited 2019 Nov 14]. Available from: https://nces.ed.gov/pubs/96852.pdf.; Reason for exclusion: ineligible context – both rural and urban settings
- 23.National Center for Education Statistics. National Center for Education Statistics (NCES) Data Sources [internet]. 2012. [cited 2019 Dec 17]. Available from: https://nces.ed.gov/pubs2012/2012046/sources.asp.; Reason for exclusion: ineligible concept – no program/intervention
- 24.Stewart TM, Martin C, Han H, Newton R, Allen HR, Williamson D. Sustained utilization of internet-based weight management programs can be achieved. Obesity. 2011;19:S121. [Google Scholar]; Reason for exclusion: ineligible concept – abstract, not enough details about program/intervention
- 25.Sussman AL, Davis SM. Integrating formative assessment and participatory research: building healthier communities in the CHILE Project. Am J Health Educ. 2010;41(4):244–9. [DOI] [PMC free article] [PubMed] [Google Scholar]; Reason for exclusion: ineligible population – younger children
- 26.Swinburn B, Malakellis M, Moodie M, Waters E, Gibbs L, Millar L, et al. Large reductions in child overweight and obesity in intervention and comparison communities 3 years after a community project. Pediatr Obes. 2014;9(6):455–62. [DOI] [PubMed] [Google Scholar]; Reason for exclusion: ineligible population – younger children
- 27.Terry-McElrath YM, O’Malley PM, Johnston LD. Foods and beverages offered in US public secondary schools through the National School Lunch Program from 2011–2013: early evidence of improved nutrition and reduced disparities. Prev Med. 2015;78:52–8. [DOI] [PubMed] [Google Scholar]; Reason for exclusion: ineligible context – both rural and urban settings
- 28.Watts AW, DeNiet J, Masse LC. Vending machine access and characteristics of the school environment in British Columbia elementary schools. Can J Diabetes. 2011;35(2):217. [Google Scholar]; Reason for exclusion: ineligible population – adults
- 29.Wilson AM, Magarey AM, Dollman J, Jones M, Mastersson N. The challenges of quantitative evaluation of a multi-setting, multi-strategy community-based childhood obesity prevention programme: lessons learnt from the eat well be active Community Programs in South Australia. Public Health Nutr. 2010;13(8):1262–70. [DOI] [PubMed] [Google Scholar]; Reason for exclusion: ineligible context – both rural and urban settings
- 30.Wilson DK, Lawman HG, Segal M, Chappell S. Neighborhood and parental supports for physical activity in minority adolescents. Am J Prev Med. 2011;41(4):399–406. [DOI] [PMC free article] [PubMed] [Google Scholar]; Reason for exclusion: ineligible population – adults
- 31.Wyatt K, Lloyd J, Creanor S, Green C, Dean SG, Hillsdon M, et al. Cluster randomised controlled trial and economic and process evaluation to determine the effectiveness and cost-effectiveness of a novel intervention [Healthy Lifestyles Programme (HeLP)] to prevent obesity in school children. Public Health Res. 2018;6(1). [PubMed] [Google Scholar]; Reason for exclusion: ineligible context – both rural and urban settings
- 32.Yoost JL, Hensley C, Woodall B. Use of telehealth to teach healthy life skills to rural adolescent females. J Adolesc Health. 2016;58(2):S31–S2. [Google Scholar]; Reason for exclusion: ineligible concept – after school program
- 33.Zahner L, Puder JJ, Roth R, Schmid M, Guldimann R, Puhse U, et al. A school-based physical activity program to improve health and fitness in children aged 6–13years (“Kinder-Sportstudie KISS”): study design of a randomized controlled trial [ISRCTN15360785]. BMC Public Health. 2006;6:147. [DOI] [PMC free article] [PubMed] [Google Scholar]; Reason for exclusion: ineligible context – both rural and urban settings


