Abstract
Background
Glottic insufficiency, or glottic gap as it is commonly called, is a common cause of dysphonia, producing symptoms of soft voice, decreased projection, and vocal fatigue. The etiology of glottic gap can occur from issues related to muscle atrophy, neurologic impairment, structural abnormalities, and trauma related causes. Treatment of glottic gap can include surgical and behavioral therapies or a combination of the two. When surgery is chosen, closure of the glottic gap is the primary goal. Options for surgical management include injection medialization, thyroplasty, and other methods of medializing the vocal folds.
Methods
This manuscript reviews the current literature regarding the options for treatment of glottic gap.
Discussion
This manuscript discusses options for treatment of glottic gap, including the indications for temporary and permanent treatment modalities; the differences between the available materials for injection medialization laryngoplasty and how they affect the vibratory function of the vocal folds and vocal outcome; and the evidence that supports an algorithm for treatment of glottic gap.
Level of Evidence
3a—Systematic review of case–control studies.
Keywords: glottic gap, injection laryngoplasty, thyroplasty, vocal paresis
This article reviews the options for treatment of glottic gap. The article explores the various etiologies as well as the available materials for medialization.

1. INTRODUCTION
Small areas of glottic insufficiency in the adult patient can cause symptomatic dysphonia, including vocal fatigue, and can result from several different etiologies. In treating patients with small glottic gaps, it is important to understand the etiology of the symptoms, the likelihood of improvement spontaneously or with voice therapy alone, the differences between the available materials for vocal fold medialization, and the impact of patient preference in management decisions.
2. SYMPTOMS OF SMALL GLOTTIC GAP
The symptoms of a small glottic gap derive from the loss of subglottic pressure during phonation secondary to glottic insufficiency. During normal phonation, the vocal folds move through a vibratory cycle in which the overlying mucosa of the vocal folds goes through open and closed phases initiated by a stream of air from the lungs. During the vibratory cycle, the muscles of phonation hold the vocal folds in an adducted position. Once the subglottic pressure reaches a certain threshold, the mucosa of the vocal folds are forced to move into lateral positions (while the vocal ligament remains in the adducted position), opening slightly the space between the vocal folds (Figure 1). The opening of the mucosa occurs from inferior to superior, then closes from inferior to superior as the pressure below and above the vocal folds begins to equilibrate. The cycle then repeats. The amount of tension in the vocal ligament determines the frequency of the vibratory cycle. This frequency then determines the pitch of the voice.
FIGURE 1.
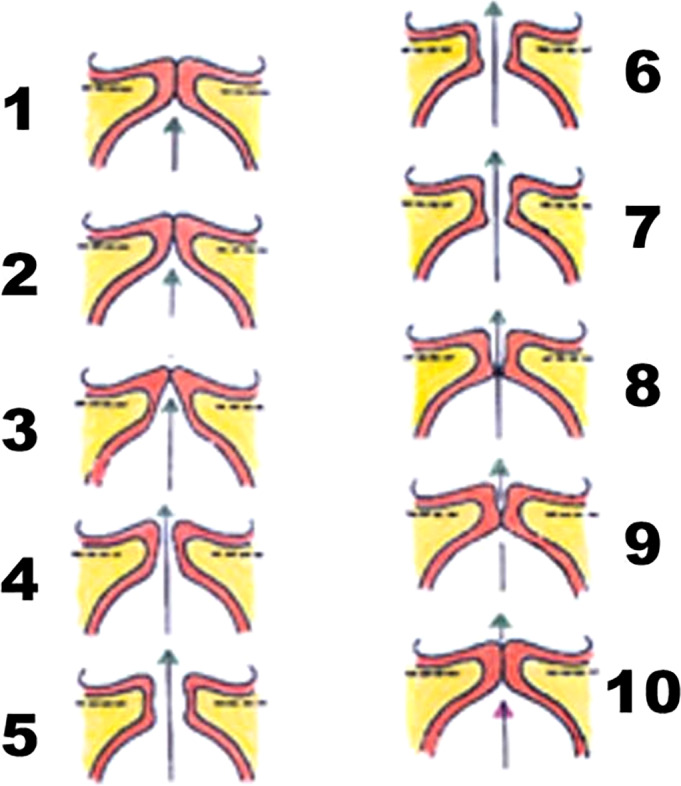
Vibratory cycle. From the Voice Foundation Website. https://voicefoundation.org/health‐science/voice‐disorders/anatomy‐physiology‐of‐voice‐production/understanding‐voice‐production/
When the vocal folds are unable to adduct completely, more subglottic pressure is needed to entrain the vocal fold mucosa into a vibratory cycle. Additionally, a greater subglottic pressure is needed to create a pressure differential between the subglottic and supraglottic regions. Depending upon the degree of subglottic pressure, the width of the glottic gap, and the ability of the patient to compensate for these issues by manipulating the remainder of the vocal tract, the resulting voice can be breathy, soft, raspy, not project as well, or tire easily.
3. ETIOLOGY OF SMALL GLOTTIC GAP
Glottic gap can occur from structural issues with the vocal fold or from neurologic issues with the vocal fold.
3.1. Volume loss
Among the structural issues that can cause glottic gap are tissue loss of the vocal ligament and/or vocalis muscle. Such tissue loss can occur as a result of aging (presbyphonia), rapid weight loss (related to carcinoma, gastric bypass/sleeve surgeries, hyperthyroidism, etc.), or can be congenital (bilateral vocal fold bowing; Figure 2). The glottic insufficiency from bilateral vocal fold bowing is usually spindle shaped. The onset of the dysphonia is usually gradual and associated with the progression of the underlying cause. Some individuals with bilateral vocal fold bowing will respond well to voice therapy aimed at improving breath support, projection, and resonance and others will not.
FIGURE 2.
Presbyphonia.
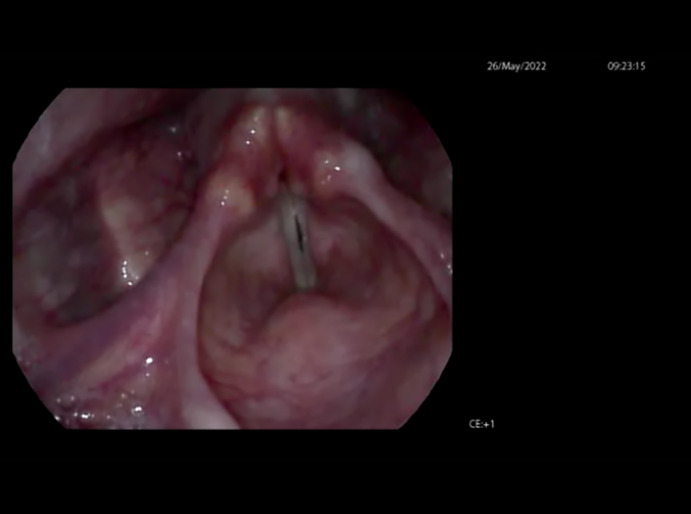
3.2. Sulcus vocalis
Sulcus vocalis can also cause a glottic gap (Figure 3). The underlying issue in all forms of sulcus is loss of lamina propria, and as a general rule, the greater the loss of lamina propria, the greater the impact of the sulcus on both voice and vocal fold closure. There is no singularly accepted nomenclature for sulcus. For the purposes of this discussion, type I, II, and III sulcus as described in Ford et al. will be used 1 (Figure 4). Type I is typically invagination of the epithelium into the superficial lamina propria (SLP; Figure 5). Type II is invagination all the way to the vocal ligament with the loss of the intermediate tissue. Type III is more limited in the distance along the vocal fold, often described as a pit, but may extend deeper into the vocal fold with loss of tissue layers.
FIGURE 3.

Bilateral sulcus vocalis.
FIGURE 4.
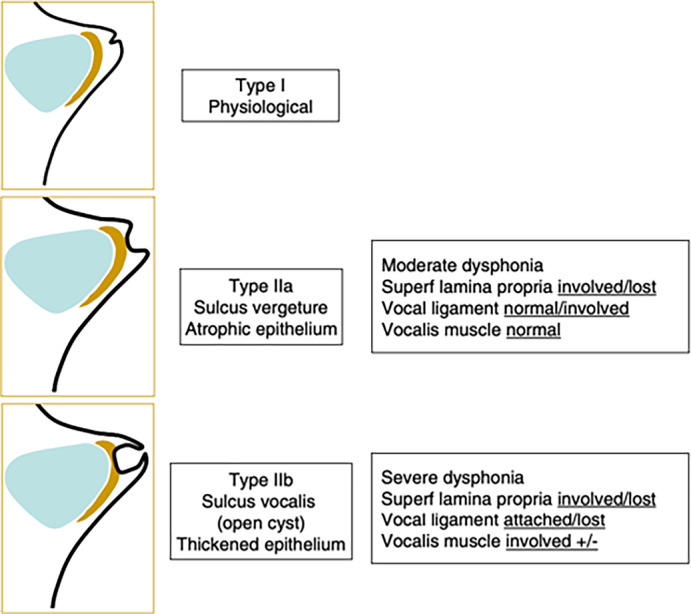
Ford's sulcus vocalis classification.
FIGURE 5.
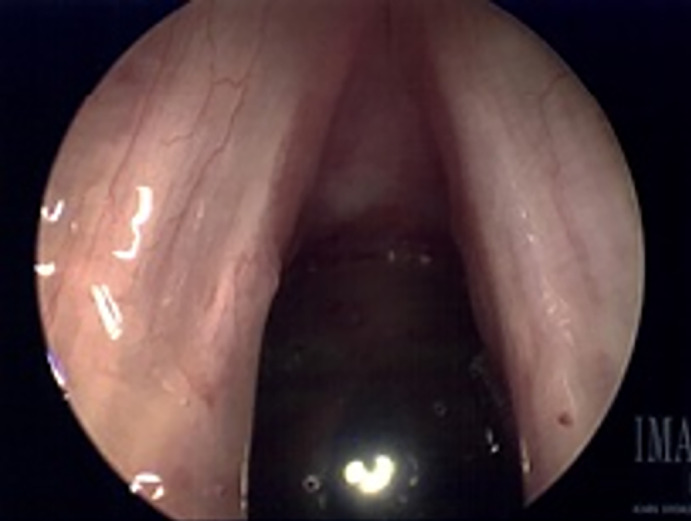
Bilateral type I sulcus vocalis intraoperative photo.
When the structured layer of the vocal fold is altered the mucosal wave is no longer able to propagate normally. The tissue loss in type II and III sulci is often accompanied by scar and effectively binds the mucosa to deeper structures and disallows the body and the cover of the mucosa to move separately. The impact of this scarring is to thin the vocal mucosa, thus causing bowing and open phase predominance when evaluated strobovideolaryngoscopically. This decreased vocal closure causes mild glottic incompetence which necessitates increased muscle tension for secondary compensation.
Patients with sulcus have voice complaints similar to those with other forms of minimal glottic incompetence, including rough vocal quality (hoarseness), early vocal fatigue, and the feeling of straining or pushing with speaking/singing. 2 It is rare for patients to complain of a breathy voice, but more common to have difficulty projecting or speaking in louder environments. Because sulcus is extremely hard to visualize without strobovideolaryngoscopy, and sometimes challenging to visualize even with strobovideolaryngoscopy, it is often difficult to diagnose. Sulcus was one of the most common diagnoses added after operative microscopic direct laryngoscopy, suggesting that it is often missed on preoperative evaluation of benign mucosal lesions. 3 , 4
3.3. Vocal fold scar
Scarring of the vocal fold from trauma, prior vocal fold surgery, inflammatory laryngeal masses (such as vocal fold polys, nodules, or cysts), or other iatrogenic sources (intubation, prolonged ventilation) can also cause a localized glottic gap (Figure 6). The scarring exists because there has been trauma to the vocal fold deep to the superficial layer of lamina propria. The biological response to the trauma is to increase procollagen in the deeper layers of lamina propria, which histologically results in a disorganized collagen scaffolding that has less collagen and less elastin than the native vocal fold. 5 Physiologically, the result is stiffness of the lamina propria, with tethering of the mucosal layer to the deep layers of lamina propria and loss of the more elastic superficial layer of lamina propria. 6 In these cases, voice therapy may have a more limited role in improving the glottic gap itself, but a greater role in ameliorating those intrinsic behaviors that led to the formation or perpetuation of the scarring.
FIGURE 6.
Right vocal fold scar.
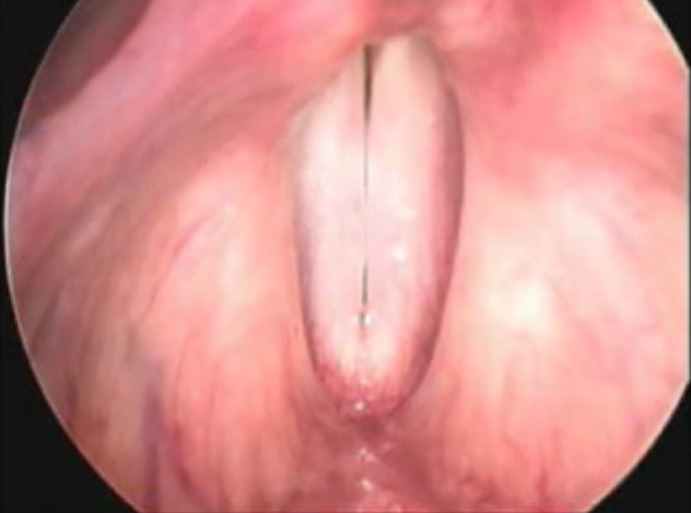
3.4. Mild vocal fold paresis
Mild vocal fold paresis can cause glottic insufficiency by decreasing the ability of the vocal folds to achieve full adduction during phonation (Figure 7). The most common nerve involved in symptomatic mild vocal fold paresis, where the vocal fold is mobile but sluggish in mobility, is the superior laryngeal nerve. 7 , 8 The superior laryngeal nerve is paretic in approximately 98% of the individuals with a glottic gap due to mild vocal fold paresis and the recurrent laryngeal nerve is involved approximately 17.5%. 7 , 8 There is bilateral nerve involvement in 25%–27.9% of those with a symptomatic glottic gap due to mild vocal fold paresis. 7 , 8
FIGURE 7.

Left superior laryngeal nerve paresis.
In studies evaluating symptoms of individuals presenting with dysphonia, those with a small glottic gap associated with vocal fold paresis were more likely to complain of vocal fatigue, decreased range, decreased volume, diplophonia, odynophonia, and effortful phonation than individuals with other causes of dysphonia or those without dysphonia. 7 , 9 , 10 Voice therapy alone will improve the symptoms associated with a small glottic gap due to vocal fold paresis in approximately 70% of those presenting to a laryngologist with complaints. 7 , 8 , 9
4. TREATMENT OF SMALL GLOTTIC GAP
The options for treatment of small glottic gap include voice therapy, injection medialization laryngoplasty, and type I thyroplasty. Medialization via an innervated myofascial flap, laryngeal reinnervation, and arytenoid adduction are typically reserved for issues related to a large glottic gap from vocal fold immobility or a large paraglottic space defect and are not indicated for treatment of small glottic gap. In a systematic review of the literature looking at injection medialization laryngoplasty, type I thyroplasty, arytenoid adduction, and laryngeal reinnervation for treatment of large glottic gaps due to vocal fold paralysis, no significant difference in the voice outcome was found between the treatment groups. 11 The outcome measures evaluated in this study included perceptual analyses (both patient and clinician), acoustic analyses, quality of life assessments, and strobovideolaryngoscopic assessment of glottic closure. These findings, however, should be viewed with caution because none of the studies in the literature looking that treatment outcomes in management of glottic gap have been randomized controlled studies or prospective in design. All of the studies have evaluated treatment outcomes after a decision was made to use one technique or another based on individual patient situational factors and the surgeon's experience in treating a particular configuration of glottic insufficiency. It likely is more the case that as anecdotal experience has shown, certain treatments work best in certain situations. Additionally, there is less data in the literature regarding treatment outcomes for the types of small glottic gaps addressed in this manuscript.
4.1. Voice therapy
Voice therapy is an important part of the treatment algorithm of all patients with a small glottic gap. In almost all of the patients, because of the glottic insufficiency, the subglottic pressure needed to entrain the vocal folds into the vibratory cycle is increased above that needed to entrain them if they had the ability to close completely. Early on in the development of the glottic gap, many people do not develop maladaptive compensatory behaviors. Voice therapy is beneficial here because it can be used to teach the patient safe ways in increasing the subglottic pressure through a focus on improving breath support, decreasing supraglottic resistance by improving resonance in the upper vocal tract, maximizing resistance at the level of the glottis, and improving vocal projection with other postural mechanisms. When the glottic gap has been present for some time, maladaptive behaviors form, most commonly supraglottic hyperfunction and muscle tension dysphonia. Voice therapy then focuses on alleviating these maladaptive behaviors and then teaching the rehabilitative behaviors.
The response to voice therapy can vary from individual to individual, but should be tried as the initial step in treatment in everyone. In many patients, it is the only treatment that is needed. It is only after voice therapy fails that surgical management should be entertained. Even when a “quick fix” is desired by the patient, the clinician should stress the importance of the need for voice therapy postoperatively for rehabilitation and the fact that postoperative voice therapy usually works better and faster if the individual has learned some of the positive rehabilitative techniques prior to the surgical intervention.
4.2. Injection medialization laryngoplasty
The options for injection medialization laryngoplasty can be described as temporary, semi‐permanent, and permanent. The goal of injection medialization laryngoplasty is to medialize the vocal fold by increasing the volume in the paraglottic space. This is performed by placing a needle lateral to the vocalis muscle, just medial to the inner perichondrium of the thyroid lamina and injecting injectable implant material. The material will fill the paraglottic space, and in doing so will both provide volume through bulk and will medialize the vocal fold undergoing injection. Care should be taken not to inject into the vocalis muscle itself or into the vocal ligament with the injectables. Doing so can result in sluggishness of the muscle and stiffness and inflammation of the vocal fold, causing worsening symptoms of dysphonia instead of improvement.
4.2.1. Temporary injectables
Temporary injectables for vocal fold medialization are those materials that will likely resorb within 4–6 weeks after injection. Carboxymethylcellulose falls into this category of injectable. It is most commonly used in patients who are hesitant to proceed with surgery and want a nonpermanent procedure to demonstrate the potential benefit of a more lasting procedure. It also is often used when the surgeon is unsure whether or not medialization will improve the patient's dysphonia symptoms and wants to use a temporary injectable to see whether medialization at a particular spot along the vocal fold will improve the voice. 12
4.2.2. Semi‐permanent injectables
Semi‐permanent injectables include those materials that are likely to resorb somewhat or completely but act as a scaffolding so that the body's own tissues may fill the space occupied by the filler when it is resorbed. The traditional materials that fall into this category include hyaluronic acid, fascia lata, and fat. Silk hydroxyapatite is the newest material that has been FDA approved as a semi‐permanent injectable as well.
Hyaluronic acid comes in small, medium, and large particle gels. Hyaluronic acid injections tend to last for 6–12 months after injection, with the large particle gels lasting longer than the small particle gels. 13 A slight overcorrection of the vocal folds is needed when injecting Hyaluronic acid, and it is best injected lateral to the vocal folds.
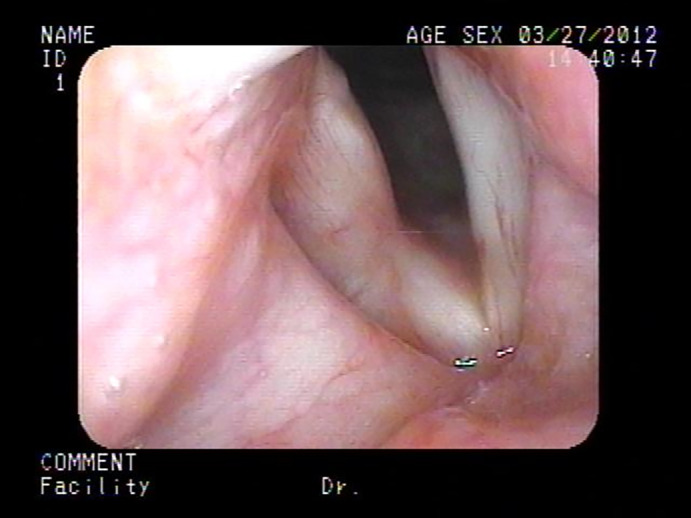
Homologous fat, derived either through liposuction or directly excised from the patient's abdomen, can be injected to medialize the vocal folds. The fat requires some preparation prior to injecting to help minimize resorption. There are various techniques for washing the fat. The issue is ridding the fat of associated blood cells. After washing, the fat is loaded into a Bruening syringe and injected lateral to the vocal fold to medialize it. Because approximately 50% of the fat will resorb, most surgeons inject 200% of the needed medialization with the expectation that after a typical resorption, the desired medialization will result (Figure 8). The resorption period with fat can take anywhere from 4 weeks to 6 months, which can be frustrating for the patient because the voice will sound strained during the period where the glottic gap has been overclosed. 14 Whatever fat is still present after 12 months, typically does not resorb further.
FIGURE 8.
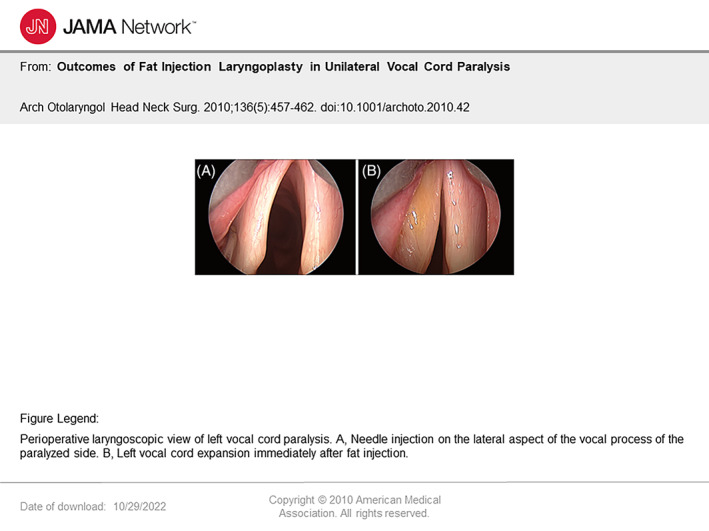
Fat injection into left vocal fold. From Arch Otolaryngol Head Neck Surg. 2010;136 (5):457‐462. doi:10.1001/archoto.2010.42.
Fascia is readably obtained homologously, is easily morselized, made into a paste, and injected either as the sole substrate for medialization or in combination with fat for injection. 15 , 16 It provides long‐term vocal fold medialization by serving as a matrix for collagen formation. 16
Silk particles suspended in hyaluronic acid (silk‐HA) is made from the Bombyx mori silk worm, and is the from the same silk protein material that has been used as suture for centuries. 17 It has recently been formulated into an injectable filler for use in vocal fold augmentation and medialization to treat small glottic gaps. It has good biocompatibility is mechanically tunable, and degrades slowly. 17 Unlike calcium hydroxyapatite, it does not migrate, which makes it more desirable for use in the larynx. 18 Because the particles are porous, they promote collagen ingrowth and support the potential for long‐lasting medialization even after the silk microparticles themselves have resorbed. 17 Although silk‐HA is a promising injectable that has been FDA approved, the experience using this material as an injectable in the laryngology community is very low. The manufacturers state that the effects of the silk‐HA injection last at least 18 months and that the voice effect may even be permanent. The silk‐HA microparticles, themselves, resorb but provide an environment that favors cellular infiltration that lends itself to a permanent bulking result. There is more general experience with the other injectable materials, and the long‐term outcomes with the other materials are better established.
4.2.3. Permanent injectables
Permanent injectables are those in which the material injected is expected to remain within the body indefinitely, whether or not the material migrates to another area of the body. Calcium hydroxyapatite is FDA approved for permanent vocal fold medialization. However, it tends to cause issues with vocal fold inflammation and vocal fold stiffness if injected near the vocal ligament. 18 Additionally, the particles tend to migrate within the neck to regional lymph nodes and at times to other areas within the larynx, including the vibratory margin. 19 These side effects can happen unpredictably and at times can be undesirable.
4.3. Type I thyroplasty
Type I thyroplasty is advantageous because it is a permanent method of medializing the vocal fold. It can be performed unilaterally or bilaterally. Several commercial prefabricated implants are available and made of either silicone or Titanium. These are best used in cases of unilateral vocal fold paralysis in which there is a sizeable vocal fold gap and tend to be less useful in patients with small glottic gaps and mobile but sluggish vocal folds. 20 Similarly, silastic can be carved to create a thyroplasty implant. However, thyroplasties for patients with small glottic gaps and mobile vocal folds are most easily performed using an expanded polytetrafluoroethylene (commonly marketed as Gore‐Tex®) implant. Because the amount of closure needed to ameliorate the symptoms of a small glottic gap is itself small, silastic implants can be difficult to carve in the configuration needed to effectuate a mild degree of closure. Similarly, prefabricated thyroplasty implants are designed to close larger glottic gaps and are less useful in the treatment of small glottic gaps.
Type I thyroplasty is performed by making a horizontal incision in the neck at the level of the thyroid cartilage. The strap muscles are divided in the midline, and the outer perichondrium of the thyroid cartilage is incised also in the midline. A lateral perichondrial flap is elevated on the side that the implant will be placed. A thyroplasty window is created at the level of the vocal folds, and the implant is positioned to medialize the vocal folds.
4.3.1. Gore‐Tex® thyroplasty
When a Gore‐Tex® implant is used, the window is no bigger than the width of a 4 mm round diamond bur, and it is positioned 3 mm superior to the inferior border of the thyroid ala and 7 mm posterior to the midline in females and 9 mm posterior to the midline in males. The inner perichondrium is not incised but is elevated off the thyroid cartilage. A thyroplasty implant, cut from a 0.6 mm thickness Gore‐Tex® cardiac patch, is trimmed to be 6 mm wide and 10–15 cm in length. The position of the vocal fold is assessed by applying medial pressure on the vocalis muscle through the thyroplasty window. The implant is folded on itself in lengths of 7–9 mm and placed into the thyroplasty window to medialize the vocal fold (Figure 9). The voice is assessed and more implant is added medial to the last layering of implant until optimal medialization is achieved (Figure 10). With each layering of implant, it should be firmly positioned against the thyroid cartilage to minimize implant migration or shift. Once the optimal voice is obtained, the vocal folds should be visualized through a flexible laryngoscope to ensure that the position of the implant is at the level of the vocal folds and that there has been no penetration of the ventricle.
FIGURE 9.

Thyroplasty insertion.
FIGURE 10.

Thyroplasty configuration to glottic gap.
Gore‐Tex is an ideal material for type I thryoplasty because it can be molded to fit the exact configuration of the patient's glottic gap. It is performed with the patient awake so that the voice can be assessed during implant placement and so that the implant position can be modified to match the exact position needed to produce the optimal voice. 21 An additional benefit of Gore‐Tex® as a thyroplasty implant is that it is both permanent and reversible. If, for some reason, the patient decides that they do not like their voice, it can be easily removed. 22
5. DISEASE SPECIFIC SURGICAL TREATMENT
5.1. Volume loss
Volume loss of the tissues of the vocal ligament and/or the vocalis muscle from presbyphonia or bilateral vocal fold bowing secondary to rapid weight loss is best surgically treated with a medialization procedure that will also provide bulk to the vocal folds (Figures 11 and 12). For most of these individuals, the loss of volume is likely permanent, so the treatment should also be permanent. Many of the individuals suffering from volume loss are not ideal candidates for general anesthesia, so consideration for the risks of general anesthesia versus the risks of cardiovascular instability from patient intolerance to an in‐office intralaryngeal injection must be weighed for each individual patient. The ideal substrate is one that is semi‐permanent or permanent. Among the available options, large particle hyaluronic acid, silk hydroxyapatite, and calcium hydroxyapatite will likely pose the best option for most patients because they are semi‐permanent to permanent; they can be injected in the office or with 5–10 minutes of general anesthesia in the operating room; and they both bulk and medialize the vocal folds in a manner that compensates for the volume loss.
FIGURE 11.
Presbyphonia preoperative.
FIGURE 12.
Presbyphonia post hyaluronic acid injection medialization laryngoplasty.
5.2. Sulcus vocalis
Once recognized as the likely cause for minimal glottic incompetence, sulcus is unfortunately not an easy condition to correct. In most cases simply lifting the epithelium is not sufficient, as it is the intermediate tissue loss that is the crux of the issue. To complicate matters further, surgical intervention also creates scar tissue that can secondarily fix the epithelium to the underlying structures, and perhaps even worsen the stiffness of the vocal fold. While there are many techniques described in the literature to attempt to improve sulcus, there is currently no accepted gold standard treatment. 23 Surgical outcomes for patients with both vocal atrophy and sulcus have been shown to be poorer than for patients with vocal atrophy alone. 24 Current research includes cell therapy to attempt regeneration of the lost vocal fold lamina and layered anatomy. 25
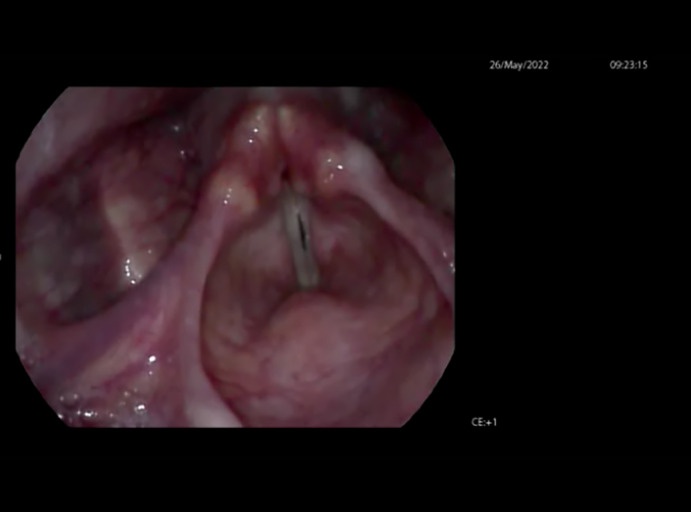
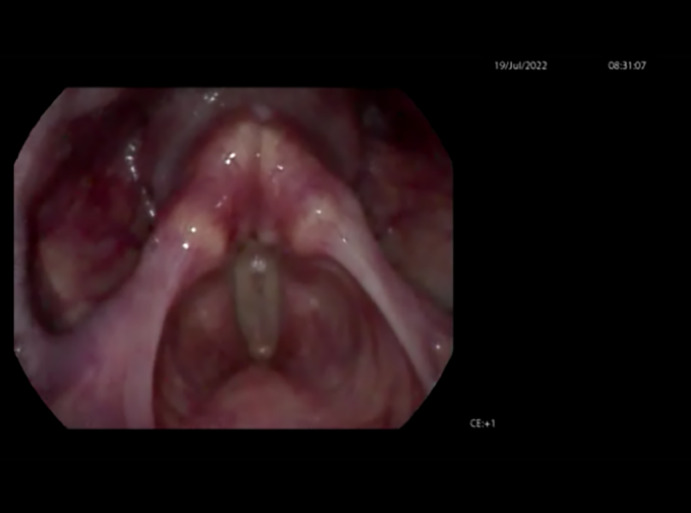
Instead of directly addressing the sulcus, intervention is often aimed at decreasing the minimal glottic insufficiency instead of improving mucosal wave propagation or stiffness caused by the underlying tissue loss (Figure 13). Procedures to close the glottic gap improve loudness, projection, and can partially relieve vocal fatigue. Rough vocal quality is often still noted due to the unresolved sulcus. At times temporary injection laryngoplasty using carboxymethylcellulose or small particle hyaluronic acid is performed for patients with sulcus (Figure 14). Even though it will not permanently improve the condition, it can be easily performed in the office or at the time of microscopic direct laryngoscopy for diagnosis. This may allow the patient to experience the effect of glottic closure on their voice. Patients may be more confident going forward with a permanent procedure after they understand how such an intervention will affect their function.
FIGURE 13.

Bilateral sulcus vocalis.
FIGURE 14.

Bilateral sulcus vocalis post carboxymethylcellulose injection medialization laryngoplasty.
Speech therapy has been infrequently utilized to attempt improvement in vocal function for patients with sulcus. Most often therapy has been performed as a safe and useful adjunct to surgical interventions, as it cannot directly address the sulcus. The main goals are to decrease compensatory hyperfunction and retrain compensatory skills to improve vocal output. 26 Therapy may also include vocal relaxation exercises and stress reduction training. It can also aid in postoperative functional recovery.
Because sulcus does not have the possibility for recovery like a vocal fold weakness may, permanent surgical interventions are preferable to temporary ones. Most commonly, a type I thyroplasty is performed with Gore‐Tex®. Fat injection medialization laryngoplasty with or without fascia lata or injection medialization laryngoplasty using silk hydroxyapatite would also be appropriate.
5.3. Vocal fold scar
Like sulcus vocalis, treatment of the glottic gap caused by vocal fold scarring is difficult. The treatment that is chosen should be aimed at both loosening the scar tissue itself and at medializing the vocal fold. Attempts to loosen the scar tissue can include local injection directly into the scar with dexamethasone to soften the scar or hydro‐dissection with dexamethasone to elevate the scar. In many of these patients, the configuration of the glottis is irregular because of the scar, and a very localized injection medialization procedure just lateral to the “divot” in the vocal fold from the scar is the best option for treatment. One approach is to do such an injection with a temporary injectable such as carboxymethylcellulose or small particle hyaluronic acid to see if adequate medialization can be obtained to improve the voice. 27 If so, then a return to the operating room to do a more permanent medialization with either fat, a large particle hyaluronic acid, or silk hydroxyapatite once the temporary injectable resorbs would be the favored approach. Type I thyroplasty is not a good option in these patients because it is difficult to fashion the implant in the disfigured configuration caused by the scarring.
5.4. Mild vocal fold paresis
The options for treatment of mild vocal fold paresis are many. If the paresis is relatively new in onset and induced by a viral illness or other cause that may spontaneously resolve, consideration may be given for a temporary or semi‐permanent injection medialization laryngoplasty using either carboxymethyl cellulose or a small particle hyaluronic acid injectable. If it appears as though the paresis is permanent (either through diagnostic testing with laryngeal electromyography or based on symptoms that have persisted for 6–12 months or longer), then consideration can be given for a more permanent injection medialization laryngoplasty using a larger particle hyaluronic acid, silk hydroxyapatite, or fat. Fat is helpful if there is associated volume loss. If there is not significant atrophy of the vocal folds, then a large particle hyaluronic acid or silk hydroxyapatite would be advised. Although hyaluronic acid injections tend to result in permanent medialization even after the material itself is resorbed, approximately 15% of the patients who undergo vocal fold injection require another medialization procedure after resorption. For some patients, the possibility of needing a more permanent procedure in the future is less preferable than performing only one permanent procedure, and these individuals may choose to have a type I thyroplasty with Gore‐Tex® in lieu of an injection medialization laryngoplasty (Figures 15 and 16). Those who need a revision after an injection medialization laryngoplasty are also candidates for the permanent type I thyroplasty procedure.
FIGURE 15.

Left superior laryngeal nerve paresis.
FIGURE 16.
Left superior laryngeal nerve paresis post type I thyroplasty with Gore‐Tex®.
6. CONCLUSION
The algorithm for treatment of a small glottic gap is influenced by the medical issue that is causing the glottic gap, the response of the patient to an initial trial of voice therapy, and patient factors that may favor temporary, semi‐permanent, or permanent solutions.
CONFLICT OF INTEREST STATEMENT
Yolanda Heman‐Ackah and Chandra Ivey have nothing to disclose. Ronda Alexander discloses that she is a consultant for Smith and Nephew and receives consulting fees or honoraria as an independent contractor/speakers bureau/advisory committees/review panels.
Heman‐Ackah YD, Ivey CM, Alexander R. Options for treatment of a small glottic gap. Laryngoscope Investigative Otolaryngology. 2023;8(3):720‐729. doi: 10.1002/lio2.1060
The content of this article was presented at the American Academy of Otolaryngology‐Head and Neck Surgery Meeting in Philadelphia, PA on September 14, 2022.
REFERENCES
- 1. Ford C, Inagi K, Khidr A, Bless D, Gilchrist K. Sulcus vocalis: a rational analytical approach to diagnosis and management. Ann Otol Rhinol Laryngol. 1996;105(3):189‐200. [DOI] [PubMed] [Google Scholar]
- 2. Soni R, Dailey S. Sulcus vocalis. Otolaryngol Clin North Am. 2019;52:735‐743. [DOI] [PubMed] [Google Scholar]
- 3. Dailey S, Spanou K, Zeitels S. The evaluation of benign glottic lesions: rigid telescopic stroboscopy versus suspension microlaryngoscopy. J Voice. 2007;21(1):112‐118. [DOI] [PubMed] [Google Scholar]
- 4. Akbulut S, Sltintas H, Oguz H. Videolaryngostroboscopy versus microlaryngoscopy for the diagnosis of benign vocal cord lesions: a prospective clinical study. Eur Arch Oto‐Rhino‐Laryngol. 2015;272(1):131‐136. [DOI] [PubMed] [Google Scholar]
- 5. Thibeault S, Gray S, Bless D, Chan R, Ford C. Histologic and rheologic characterization of vocal fold scarring. J Voice. 2002;16(1):96‐104. [DOI] [PubMed] [Google Scholar]
- 6. Hansen J, Thibeault S. Current understanding and review of the literature: vocal fold scarring. J Voice. 2006;20(1):110‐120. [DOI] [PubMed] [Google Scholar]
- 7. Heman‐Ackah Y, Joglekar S, Caroline M, et al. The prevalence of undiagnosed thyroid disease in patients with symptomatic vocal fold paresis. J Voice. 2011;25(4):496‐500. [DOI] [PubMed] [Google Scholar]
- 8. Sataloff R, Praneetvatakul P, Heuer R, et al. Laryngeal electromyography: clinical application. J Voice. 2010;24(2):228‐234. [DOI] [PubMed] [Google Scholar]
- 9. Koufman J, Postma G, Cummins M, Blalock P. Vocal fold paresis. Otolaryngol Head Neck Surg. 2000;122(4):537‐541. [DOI] [PubMed] [Google Scholar]
- 10. Dursun G, Sataloff R, Spiegel J, Mandel S, Heuer R, Rosen D. Superior laryngeal nerve paresis and paralysis. J Voice. 1996;10(2):206‐211. [DOI] [PubMed] [Google Scholar]
- 11. Siu J, Tam S, Fung K. A comparison of outcomes in interventions for unilateral vocal fold paralysis: a systematic review. Laryngoscope. 2016;126(7):1616‐1624. [DOI] [PubMed] [Google Scholar]
- 12. Carroll T, Dezube A, Bauman L, Mallur P. Scar patients who may benefit from more durable augmentation. Ann Otol Rhinol Laryngol. 2018;127(2):105‐112. [DOI] [PubMed] [Google Scholar]
- 13. Svejdova A, Drsata J, Mejzlik J, et al. Injection laryngoplasty with hyaluronic acid for glottic insufficiency in unilateral vocal fold paralysis: a systematic review of the literature. Eur Arch Oto‐Rhino‐Laryngol. 2022;279(11):5071‐5079. [DOI] [PubMed] [Google Scholar]
- 14. Fang T, Li H, Gliklich R, Chen Y, Wang P, Chuang H. Outcomes of fat injection laryngoplasty in unilateral vocal cord paralysis. Arch Otolaryngol Head Neck Surg. 2010;136(5):457‐462. [DOI] [PubMed] [Google Scholar]
- 15. Cheng Y, Li Z, Huang J, et al. Combination of autologous fascia lata and fat injection into the vocal fold via the cricothyroid gap for unilateral vocal fold paralysis. Arch Otolaryngol Head Neck Surg. 2009;135(8):759‐763. [DOI] [PubMed] [Google Scholar]
- 16. Tsunoda K, Baer T, Niimi S. Autologous transplantation of fascia into the vocal fold: long‐term results of a new phonosurgical technique for glottal incompetence. Laryngoscope. 2001;111(3):453‐457. [DOI] [PubMed] [Google Scholar]
- 17. Brown J, Gulka C, Giordano J, Montero M, Hoang A, Carroll T. Injectable silk protein microparticle‐based fillers: a novel material for potential use in glottic insufficiency. J Voice. 2019;33(5):773‐780. [DOI] [PubMed] [Google Scholar]
- 18. Rosen C, Gartner‐Schmidt J, Casiano R, et al. Vocal fold augmentation with calcium hydroxylapatite: twelve‐month report. Laryngoscope. 2009;119(5):1033‐1041. [DOI] [PubMed] [Google Scholar]
- 19. Gulka C, Brown J, Giordano J, Hickey JM, Hoang A, Carroll T. A novel silk‐based vocal fold augmentation material: 6‐month evaluation in a canine model. Laryngoscope. 2019;129(8):1856‐1862. [DOI] [PubMed] [Google Scholar]
- 20. Laccourreye O, Rubin F, van Lith‐Bijl J, Desuter G. Keys to successful type‐I thyroplasty with Montgomery® implant for unilateral laryngeal immobility in adults. Eur Ann Otorhinolaryngol Head Neck Dis. 2021;138(3):191‐194. [DOI] [PubMed] [Google Scholar]
- 21. Selber J, Sataloff R, Spiegel J, Heman‐Ackah Y. Gore‐Tex medialization thyroplasty: objective and subjective evaluation. J Voice. 2003;17(1):88‐95. [DOI] [PubMed] [Google Scholar]
- 22. Cohen J, Bates D, Postma G. Revision Gore‐Tex medialization laryngoplasty. Otolaryngol Head Neck Surg. 2004;131(3):236‐240. [DOI] [PubMed] [Google Scholar]
- 23. Medeiros N, Castro M, van Lith‐Bijl J, Desuter G. A systematic review on surgical treatments for sulcus vocalis and vocal fold scar. Laryngoscope. 2022;132(4):822‐830. [DOI] [PubMed] [Google Scholar]
- 24. Isshiki N, Shoji K, Kojima H, Hirano S. Vocal fold atrophy and its surgical treatment. Ann Otol Rhinol Laryngol. 1996;105(3):182‐188. [DOI] [PubMed] [Google Scholar]
- 25. Mattei A, Magalon J, Bertrand B, Philandrianos C, Veran J, Giovanni A. Cell therapy and vocal fold scarring. Eur Ann Otorhinolaryngol Head Neck Dis. 2017;134(5):339‐345. [DOI] [PubMed] [Google Scholar]
- 26. Giovanni A, Chanteret C, Lagier A. Sulcus vocalis: a review. Eur Arch Oto‐Rhino‐Laryngol. 2007;264(4):337‐344. [DOI] [PubMed] [Google Scholar]
- 27. Dumberger L, Overton L, Buckmire R, Shah R. Trial vocal fold injection predicts thyroplasty outcomes in nonparalytic glottic incompetence. Ann Otol Rhinol Laryngol. 2017;126(4):279‐283. [DOI] [PubMed] [Google Scholar]


